Table of Contents
ToggleUnderstanding Myoclonus
What is Myoclonus?
Myoclonus is sudden jerks in your body. Myoclonus is characterized by short, involuntary muscle twitches that resemble shocks. These jerks may occur individually or in a series.
They may be mild, like a quick leg twitch, or strong enough to throw objects from the hands. Unlike regular movements, they are sudden and not under voluntary control.
What is the Cause of Myoclonus?
The cause of myoclonus depends on context. It can occur due to neurological disorders, brain injury, metabolic imbalance, or drug side effects. Sometimes, it results from electrical misfiring within the brain’s motor control areas. Drugs are one of the most overlooked contributors. Patients often mistake drug-induced jerks for worsening illness, though the actual cause may be their medication.
What is Myoclonus Jerk?
A myoclonus jerk describes that sudden, involuntary twitch. It might be as simple as a hand snapping shut or a leg jumping when sitting still. These jerks often appear without warning and can interfere with daily life.
What is Sleep Myoclonus?
Sleep myoclonus refers to those sudden jerks that happen as someone falls asleep. For most people, these jerks are harmless. But in patients on certain drugs, sleep jerks can be exaggerated and disturbing, leading to poor sleep quality.
Types of Myoclonus
There are different types of myoclonus. They include physiological, like hiccups or sleep jerks; essential, when jerks happen without underlying disease; symptomatic, when related to conditions like epilepsy or metabolic disorders; and drug-induced, where medications are responsible. Each type has distinct triggers, duration, and severity.
Symptoms of Myoclonus
The symptoms of myoclonus include sudden jerks, brief spasms, or repeated muscle twitching. They can vary in intensity, being either mild or severe, and may appear random or follow a specific pattern.
Sometimes they occur during movement, other times at rest. Unlike tremors, they are quick, shock-like, and disruptive.
Drugs That Cause Myoclonus

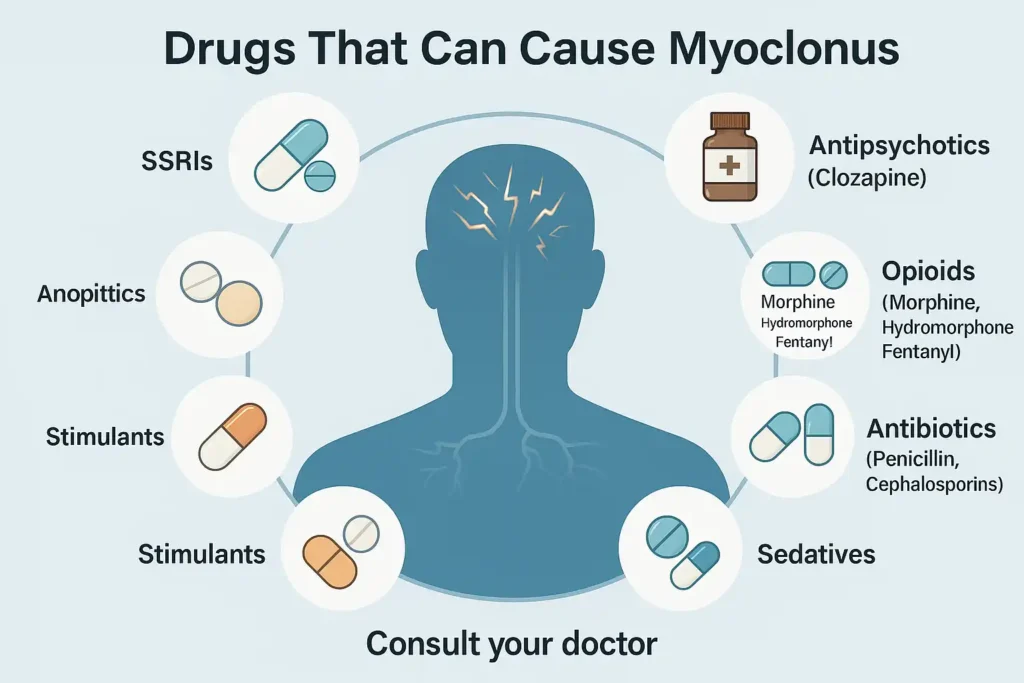
Several classes of medications are linked to drugs causing myoclonic jerks. Knowing which drugs may cause problems helps patients and doctors make informed choices.
Antiepileptic Drugs Causing Myoclonic Jerks
Ironically, some antiepileptics can trigger myoclonus. Valproate and levetiracetam are known culprits. Although these drugs control seizures, they can paradoxically increase jerks in sensitive patients.
The effect often depends on dosage and pre-existing neurological conditions. This highlights the complexity of anticonvulsants and myoclonus.
Antidepressant Medications That Cause Myoclonus
Some antidepressants may lead to abnormal jerks. SSRIs, like sertraline or fluoxetine, have been reported to cause muscle twitches. The mechanism is tied to serotonin pathways, which influence motor control.
For some people, these jerks are mild; for others, they disrupt sleep and daily activities. This aligns with the association between antidepressants and involuntary jerks.
Antipsychotic Drugs Causing Myoclonus
Certain antipsychotics, including clozapine, can trigger myoclonus. They alter dopamine and serotonin balance in the brain.
Patients using them for schizophrenia or mood disorders may suddenly experience jerks. These are often overlooked as part of the underlying illness but are actually neurological drug side effects.
Opioids and Other Drugs Causing Myoclonic Jerks
High doses of opioids are strongly linked to jerks. Opioids such as morphine, hydromorphone, and fentanyl can lead to myoclonus. These jerks usually appear in hospitalized patients receiving pain treatment. They often worsen with prolonged use or kidney dysfunction. Other drugs, like antibiotics (penicillin, cephalosporins), also contribute.
Medications That Cause Myoclonus: Detailed Overview
Medications that cause myoclonus include a wide range of drugs. Besides antiepileptics, antidepressants, antipsychotics, and opioids, sedatives, stimulants, and even some antibiotics can trigger jerks.
What makes it challenging is that not all patients develop symptoms. Individual brain chemistry, dosage, and other health issues determine who is at risk. This is why drug-induced myoclonus must be carefully understood in clinical settings.
Mechanisms Behind Drug-Induced Myoclonus
The brain’s motor control areas depend on balanced neurotransmitters. When drugs disturb serotonin, dopamine, or GABA pathways, abnormal firing occurs. This causes sudden jerks.
For instance, while SSRIs increase serotonin levels, they might also overstimulate motor circuits. Opioids, when broken down, leave by-products that irritate neurons. Antiepileptics may alter electrical stability, leading to paradoxical effects. These mechanisms explain why drug-induced jerks appear unpredictable.
Risk Factors for Myoclonus Caused by Drugs
Age and Susceptibility to Drug-Induced Myoclonus
Older adults are more vulnerable. Their kidneys and liver process drugs more slowly, causing buildup in the body. Children, especially those with neurological disorders, may also react more strongly.
Underlying Medical Conditions and Myoclonus
Patients with epilepsy, dementia, or kidney disease have higher risks. Damaged brain circuits are more prone to drug-induced jerks. For example, those with Alzheimer’s may develop sudden twitching after new prescriptions.
Drug Interactions as Myoclonus Causes
Mixing medications increases risk. SSRIs with opioids, or antipsychotics with antiepileptics, may amplify jerks. Doctors must carefully review prescriptions to avoid dangerous myoclonus and central nervous system drugs combinations.
Diagnosis of Drug-Induced Myoclonus

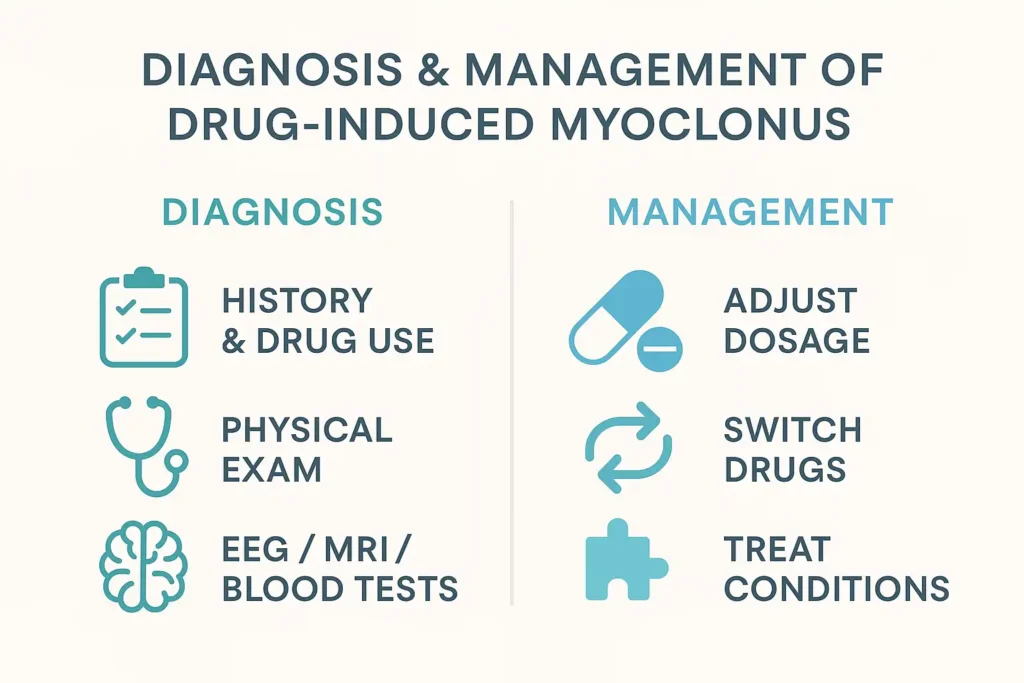
Medical History and Drug Use
Doctors start by reviewing medication history. A detailed record of when jerks began compared to new prescriptions is critical.
Physical Examination
A doctor observes the jerks, checks reflexes, and examines muscle tone. This helps distinguish myoclonus from tremors or seizures.
Diagnostic Tests for Myoclonus
EEG can reveal abnormal brain activity. Blood tests check for drug buildup or metabolic issues. MRI may identify underlying brain damage. Together, these confirm symptoms of medication-related myoclonus.
Managing Myoclonus Caused by Drugs
Adjusting Medication Dosages
Sometimes lowering the dose reduces jerks without losing drug effectiveness. This requires medical supervision.
Switching Medications Causing Myoclonus
If lowering the dose fails, switching to a different drug is often needed. Doctors may choose alternatives less likely to cause jerks.
Treating Underlying Conditions
Addressing epilepsy, dementia, or kidney disease helps reduce drug sensitivity. This approach is part of the treatment of drug-induced myoclonus.
Preventive Measures for Myoclonus Caused by Drugs
Medication Monitoring
Routine drug level checks are crucial. Early detection prevents jerks from worsening.
Lifestyle Modifications
Good hydration, regular sleep, and avoiding unnecessary drug combinations lower risk. Patients should always report new jerks immediately.
When to Seek Medical Attention for Drug-Induced Myoclonus
Persistent jerks, especially if they affect daily life, require medical review. Confusion, worsening spasms, or drug changes are red flags. Knowing when to see a doctor for myoclonus can prevent complications.
Living with Myoclonus
Coping Strategies
Patients benefit from stress control, physiotherapy, and clear communication with doctors. Accepting that some jerks may persist helps people adjust emotionally while focusing on long-term health.
The Bottom Line
Drugs that cause myoclonus are more common than most people realize. The jerks may be mild or highly disruptive. Recognizing links between myoclonus causes drugs and daily medications prevents confusion. The best outcomes happen when patients speak openly with doctors, monitor medications, and report changes early. Drug-induced jerks are not always a sign of worsening illness; often, they are side effects that can be controlled.
FAQs
What is the main cause of myoclonus?
The main cause is abnormal electrical activity in the brain. It can arise from neurological disease, metabolic imbalance, or medications that cause myoclonus.
What does a myoclonus look like?
It looks like a sudden, brief muscle jerk. It may affect one body part or spread widely, resembling a shock-like spasm.
Is myoclonus harmful?
Most cases are not life-threatening. However, severe drug-induced jerks can interfere with daily tasks and sleep, requiring medical adjustment of prescriptions.
Is myoclonus caused by anxiety?
Anxiety does not directly cause it. Stress may worsen twitching, but drug effects or neurological conditions are usually the root cause.
How to check for myoclonus?
Doctors confirm it through physical exams, EEGs for brain activity, and reviewing drug use. Blood tests also detect underlying contributors.
What deficiency causes myoclonus?
Magnesium or calcium deficiency can cause jerks. Vitamin B12 deficiency is another common factor linked to twitching.
What can be mistaken for myoclonus?
Tremors, tics, or seizures are often confused with myoclonus. Careful medical evaluation ensures accurate diagnosis.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.