Childhood trauma refers to distressing or harmful experiences that overwhelm your ability to feel safe, supported, or protected during early development.
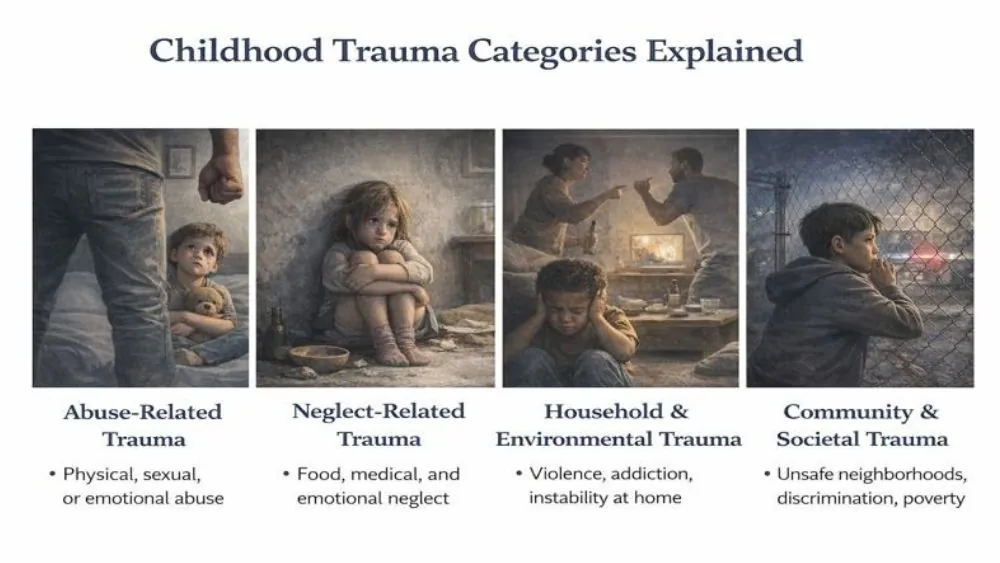
The types of childhood trauma fall into clear patterns based on where harm comes from and how often it occurs. Abuse-related trauma includes physical, emotional, or sexual harm that directly triggers fear and pain.
Neglect-related trauma develops when basic emotional or physical needs go unmet, quietly limiting brain growth and emotional skills. Household trauma grows from ongoing exposure to violence, addiction, mental illness, or instability at home, keeping the stress response constantly active.
Community trauma comes from unsafe environments, discrimination, or chronic poverty that place daily pressure on a child’s sense of security. Medical trauma occurs through repeated illness, painful procedures, or loss of control during care, even when treatment is necessary.
These types of childhood trauma often overlap, and the combined exposure increases the risk of long-term emotional, physical, and relational difficulties later in life.
Childhood Trauma Categories Explained
Childhood trauma is not one single experience. Doctors and researchers group it into clear categories to understand risk and outcomes. These categories of childhood trauma help explain why two people exposed to stress may show very different symptoms as adults.
Abuse-Related Trauma
Abuse-related trauma happens when someone causes direct harm. This includes physical abuse, sexual abuse, and emotional abuse. Repeated abuse keeps a child’s stress response switched on. That constant alert state affects memory, sleep, and immune function.
Among all types of childhood trauma , abuse has one of the strongest links to post-traumatic stress disorder, also called PTSD, which means the brain stays stuck in survival mode even after danger ends.
Neglect-Related Trauma
Neglect-related trauma occurs when basic needs are not met. Food, medical care, supervision, comfort, and emotional support may be missing. Neglect can slow development in areas that control planning, focus, and emotional control. These types of childhood trauma are often overlooked because there are no visible injuries. The harm still runs deep.
Household And Environmental Trauma
This category includes domestic violence, caregiver addiction, untreated mental illness, incarceration, or constant instability at home. A child may not be hit directly, but living in fear changes brain wiring. These different types of childhood trauma teach the nervous system that danger is unpredictable.
Community And Societal Trauma
Community trauma includes exposure to violence, discrimination, unsafe neighborhoods, poverty, or war. The WHO reports that chronic community stress increases anxiety and depression rates in children, even without direct abuse. These categories of childhood trauma pile stress onto a developing brain every single day.
Physical Abuse Childhood Trauma
Physical harm during development forces the nervous system into constant survival mode. Repeated injury alters pain perception, stress hormone release, and impulse control, increasing both physical illness and behavioral risk later in life.
What Counts As Physical Abuse In Childhood
Physical abuse includes hitting, kicking, burning, shaking, choking, or using objects to cause pain. It also includes extreme punishment that leads to injury. Even a single severe incident can alter stress hormone regulation. Repeated incidents greatly increase risk.
Common Signs And Behavioral Indicators
You may notice frequent injuries with unclear explanations. Some children flinch when touched or stay unusually alert. Others act aggressively or withdraw. These signs are survival responses, not behavior problems. They reflect how types of childhood trauma train the brain to expect harm.
Short-Term And Long-Term Health Consequences
Short-term effects include pain, sleep problems, headaches, and fear. Long-term outcomes are higher rates of heart disease, autoimmune illness, substance use, and depression in adults with physical abuse histories. These outcomes explain many long-term effects of childhood trauma seen in medical care.
Emotional And Psychological Abuse In Childhood
Emotional harm reshapes self-belief and emotional control rather than causing visible injury. Long-term exposure interferes with how the brain processes self-worth, trust, and threat, often leading to internalized distress rather than outward behavior
Verbal Abuse And Emotional Neglect
Constant criticism, threats, yelling, and rejection count as emotional abuse. Emotional neglect happens when caregivers ignore feelings or provide no comfort. These types of childhood trauma can lead to changes in the brain areas that manage self-worth and emotional balance.
Gaslighting, Humiliation, And Fear-Based Control
Gaslighting means being told your feelings or memories are wrong. Humiliation attacks dignity. Fear-based control uses threats to force obedience. These patterns teach you to doubt yourself. Among different types of childhood trauma , emotional abuse strongly predicts anxiety disorders in adulthood.
Impact On Self-Esteem And Emotional Regulation
Children exposed to emotional abuse often feel shame without knowing why. They may struggle to calm anger or sadness. These struggles explain many long-term effects of childhood trauma , including unstable moods and chronic self-criticism.
Adverse Childhood Experiences (ACEs)
ACEs represent cumulative stress exposure rather than isolated events. Research shows a clear dose-response pattern, meaning each added experience increases the likelihood of mental illness, chronic disease, and reduced life expectancy.
What Are ACEs?
Adverse childhood experiences (ACEs) are a set of ten exposures identified by large CDC studies. They include abuse, neglect, and household dysfunction. ACEs do not measure personality or strength. They measure exposure.
Common ACE Categories (Abuse, Household Dysfunction, Loss)
ACE categories include physical, emotional, and sexual abuse. They also include caregiver addiction, mental illness, violence, separation, or incarceration. These categories of childhood trauma often overlap, which increases harm.
ACE Score And Cumulative Trauma Risk
Each exposure adds one point to your ACE score. Higher scores raise the risk of heart disease, stroke, depression, addiction, and early death. This dose-response pattern proves that types of childhood trauma accumulate in the body over time. Evidence is strong, but researchers note that resilience factors can reduce impact.
Medical Trauma In Childhood
Medical trauma affects children even when treatment is necessary and life-saving. Repeated pain, loss of control, and fear during care can sensitize stress pathways, especially when emotional support is limited or inconsistent.
Chronic Illness And Repeated Hospitalizations
Children with chronic illness face repeated procedures, separation from caregivers, and loss of control. Higher anxiety and PTSD symptoms in these children. These types of childhood trauma happen even when care is lifesaving.
Painful Or Invasive Medical Procedures
Procedures without adequate pain control or explanation can overwhelm a child’s coping ability. Memory of pain can trigger fear responses years later. Doctors now stress trauma-informed care, but research notes gaps in practice.
Trauma Related To Disability Or Developmental Disorders
Children with disabilities often face bullying, isolation, and medical stress. WHO disability research shows higher trauma exposure in this group. These different types of childhood trauma increase emotional strain and health risk over time.
Long-Term Effects Of Childhood Trauma
Types of childhood trauma do not stop affecting you when childhood ends. The brain and body adapt to early danger in ways meant to protect you. Those same changes can cause problems years later.
Early trauma changes stress hormones, immune responses, and emotional control systems. These changes explain why the long-term effects of childhood trauma often appear slowly over time.
Impact On Mental Health (Anxiety, Depression, PTSD)
When you grow up in constant stress, your brain learns to expect threat. This increases the risk of anxiety disorders, depression, and post-traumatic stress disorder, which means your body reacts as if danger is still present. Nightmares, panic, emotional numbness, and sudden fear are common.
Among all types of childhood trauma , repeated exposure raises the highest risk. Evidence is strong, but researchers note that not everyone exposed develops mental illness due to protective factors like support and early care.
Effects On Physical Health And Chronic Disease Risk
Childhood trauma affects more than emotions. It increases inflammation, raises blood pressure, and disrupts metabolism. Adults with high trauma exposure show higher rates of heart disease, diabetes, autoimmune illness, and chronic pain. These findings explain why doctors now screen for adverse childhood experiences (ACEs) during medical care. The body keeps score even when memories fade.
Relationship, Attachment, And Trust Difficulties
Early trauma teaches you how relationships work. If care felt unsafe, closeness may feel risky. You may avoid intimacy or fear abandonment. Some people cling to relationships, while others stay distant. These patterns reflect different types of childhood trauma shaping attachment and trust.
Signs Of Unresolved Childhood Trauma In Adults
Unresolved trauma often appears as patterns rather than memories. Emotional overreactions, avoidance, chronic tension, or shutdown responses signal a nervous system shaped by early threat rather than present danger.
Emotional Regulation Issues
You may feel emotions intensely or struggle to calm down. Small stress can trigger strong reactions. This happens because types of childhood trauma train the nervous system to stay alert.
Hypervigilance And Avoidance Behaviors
Hypervigilance means always scanning for danger. Avoidance means staying away from reminders, people, or places. Both are survival responses learned early.
Trauma-Related Coping Patterns
Some people cope through overwork, food, substances, or emotional shutdown. These behaviors often link to long-term effects of childhood trauma , not personal failure.
How Childhood Trauma Is Diagnosed
Diagnosis relies on pattern recognition across symptoms, history, and behavior. Trauma often mimics other conditions, so clinicians assess timing, triggers, and stress responses rather than relying on one test.
Clinical Assessment And Trauma History
Clinicians start with detailed interviews. They ask about early experiences, symptoms, and timing. Trust matters because many types of childhood trauma involve secrecy or shame.
Role Of Screening Tools And ACE Questionnaires
Screening tools help identify risk. Adverse childhood experiences (ACEs) questionnaires measure exposure, not diagnosis. They guide care planning and prevention.
Differential Diagnosis Considerations
Doctors rule out ADHD, mood disorders, thyroid disease, and sleep disorders. Trauma can mimic these conditions, so careful evaluation matters.
Treatment And Healing Options For Childhood Trauma
Effective treatment targets both thought patterns and nervous system responses. Combining psychological therapy with body-based regulation strategies leads to better long-term outcomes than talk therapy alone.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
TF-CBT helps children and adults change trauma-driven thoughts and behaviors. It teaches coping skills and emotional regulation. Caregivers often join treatment for younger patients.
EMDR And Somatic Therapies
EMDR uses guided eye movements to process traumatic memories. Somatic therapies focus on body sensations, which helps when words feel hard. These approaches work well for types of childhood trauma stored in the nervous system.
Family-Based And Supportive Interventions
Stable relationships support healing. Family therapy, school support, and community care reduce stress and improve outcomes linked to the long-term effects of childhood trauma .
Can Childhood Trauma Be Prevented?
Prevention focuses on reducing chronic stress and increasing safety. Consistent caregiving, emotional validation, and early intervention can buffer the brain against lasting damage even in high-risk environments.
Protective Factors In Early Life
Safe adults, routines, and emotional support protect brain development. Teaching coping skills early reduces risk from different types of childhood trauma .
Role Of Caregivers, Schools, And Communities
Trauma-informed caregiving and education reduce punishment and increase safety. Schools that understand categories of childhood trauma respond with support instead of blame.
Early Intervention And Trauma-Informed Care
Early help limits long-term damage. Trauma-informed care recognizes stress responses and avoids retraumatization.
When To Seek Professional Help
Professional help is needed when stress responses interfere with daily life. Persistent anxiety, emotional numbness, physical symptoms without a clear cause, or unstable relationships signal unresolved trauma requiring support.
Warning Signs In Children
Seek help for sleep problems, fear, aggression, withdrawal, or sudden school decline. These signs often follow types of childhood trauma .
When Adult Symptoms Require Clinical Support
Panic, depression, substance use, or relationship breakdown signal the need for care. These are common long-term effects of childhood trauma .
How To Find Trauma-Informed Professionals
Look for licensed providers trained in trauma care. Ask about experience with adverse childhood experiences (ACEs) and evidence-based methods.
FAQs
How Many Types Of Childhood Trauma Are There?
Experts group types of childhood trauma into abuse, neglect, household dysfunction, community stress, and medical trauma. These groups overlap and often occur together, increasing long-term health and emotional risk across the lifespan.
Can Childhood Trauma Affect Adulthood Even If Forgotten?
Yes. Even without clear memories, the brain and body store stress responses. These hidden effects explain many long-term effects of childhood trauma , including anxiety, chronic illness, and relationship struggles.
Are ACEs The Same As Childhood Trauma?
No. Adverse childhood experiences (ACEs) measure exposure to early stress. Trauma describes how those experiences affect your nervous system, emotions, and health over time.
Can Childhood Trauma Be Fully Healed?
Healing is possible, but it does not erase the past. With therapy, support, and safety, many people reduce symptoms and build stable lives after different types of childhood trauma .
What Does A Clinical Trauma Assessment Involve?
Assessment includes interviews, symptom review, and screening tools. Clinicians look at patterns across time while ruling out medical or psychiatric conditions that mimic trauma responses.
How Are Screening Tools And ACE Questionnaires Used?
ACE tools help identify risk and guide care. They do not label you. They support early intervention and prevention for types of childhood trauma .
What Conditions Must Be Ruled Out During Diagnosis?
Doctors rule out ADHD, depression, anxiety disorders, sleep disorders, and medical causes. Trauma can mimic these, so careful diagnosis matters.
What Treatment Options Are Available For Childhood Trauma?
Treatment includes TF-CBT, EMDR, somatic therapy, family support, and medication when needed. Choice depends on age, symptoms, and trauma history.
What Healing Approaches Help Children Recover From Trauma?
Safety, stable caregiving, emotional skills training, and therapy help children recover. These steps reduce the lasting impact of categories of childhood trauma and support healthy development.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.