Have you ever wondered why some people suddenly develop dry eyes, a dry mouth, and feel tired all the time? What if your immune system turns against you? These are more than just daily annoyances, they could be signs of something deeper. What causes Sjogren’s syndrome is one of the most asked questions in neurology and immunology clinics, yet most explanations barely scratch the surface.
In this blog, we will break it down in the simplest way possible. We’ll explore what causes Sjogren’s syndrome, the role of your immune system, genes, viruses, hormones, and more. This article is backed by science and simplified by Dr. Chandril Chugh, a board-certified U.S.-trained neurologist who makes complex conditions easy to understand.
Let’s understand what causes Sjogren’s syndrome and why knowing this could change how we diagnose and treat it.
Table of Contents
ToggleWhat is Sjogren’s Syndrome?
Sjogren’s Syndrome is an autoimmune gland disorder. This means your immune system, which normally protects you, starts attacking healthy parts of your body, especially the glands that make moisture.
- It mostly affects the eyes, mouth, nose, throat, and even internal organs.
- It often comes with dry eyes, dry mouth, tiredness, and joint pain.
- It can show up by itself or along with other autoimmune diseases.
It’s more than just dryness, it can affect your whole body.
A Look at Primary vs Secondary Sjogren’s
There are two main types:
| Type | Description |
|---|---|
| Primary | Happens on its own without other autoimmune diseases |
| Secondary | Happens along with diseases like lupus or rheumatoid arthritis |
Knowing the type helps doctors plan the right treatment.
Prevalence and Who It Affects
- Over 4 million people in the U.S. have it (source: NIH)
- 90% of patients are women
- Most people get diagnosed between the ages of 40 and 60
- It often goes undiagnosed for years
This makes it one of the most common autoimmune gland disorders that people haven’t heard enough about.
What Causes Sjogren’s Syndrome?
Let’s get to the heart of the matter: what causes Sjogren’s syndrome? It’s not just one thing. Doctors believe it’s a mix of genes, immune system problems, environmental factors, and hormones.
Is Sjogren’s Syndrome an Autoimmune Disorder?
Yes, Sjogren’s syndrome immune system behavior is the core issue.
- The body mistakenly attacks glands that produce saliva and tears.
- Immune cells invade these glands and reduce their function.
- This leads to the dry symptoms seen in most patients.
So, when people ask what causes Sjogren’s syndrome, the immune system is the first place to look.
Genetic Factors
There is a clear genetic link to Sjogren’s syndrome.
- Specific genes like HLA-DR and HLA-DQ are more common in patients.
- Family history increases your risk.
- Twin studies show that if one twin has it, the other has a higher chance too.
Genetics alone won’t cause it, but it sets the stage.
Environmental Triggers
Many researchers believe viral causes of Sjogren’s play a key role.
- Viruses like Epstein-Barr virus (EBV) and Hepatitis C may trigger the disease.
- Some bacteria could be involved, but the evidence isn’t as strong.
- The virus may wake up immune cells that then attack the glands.
So, catching certain viruses could be a trigger.
Hormonal Influence
This is why 90% of Sjogren’s cases are in women.
- Hormones, especially estrogen, might protect the glands.
- After menopause, estrogen drops, and symptoms often worsen.
- Some researchers think estrogen helps regulate the immune system.
So, hormones may explain both timing and severity.
Other Risk Factors
Age and other health issues can increase your risk:
- Most people get it between ages 40 and 60.
- Having other autoimmune diseases like lupus or rheumatoid arthritis raises your risk.
- Smoking or chronic stress may make it worse, but they are not direct causes.
These factors don’t cause the disease alone, but they add fuel to the fire.
Is Sjogren’s Syndrome Hereditary?
People often ask: is it passed down in families?
Twin Studies and Family History Insights
- Identical twins show a higher match rate for Sjogren’s.
- If you have a family member with it, you’re at greater risk.
But not everyone with the genes will get the disease.
Differences Between Genetic Predisposition and Actual Onset
- Genes can make you prone to it.
- But something needs to “turn it on” (like a virus or hormone change).
- This is why two people in the same family can have very different health.
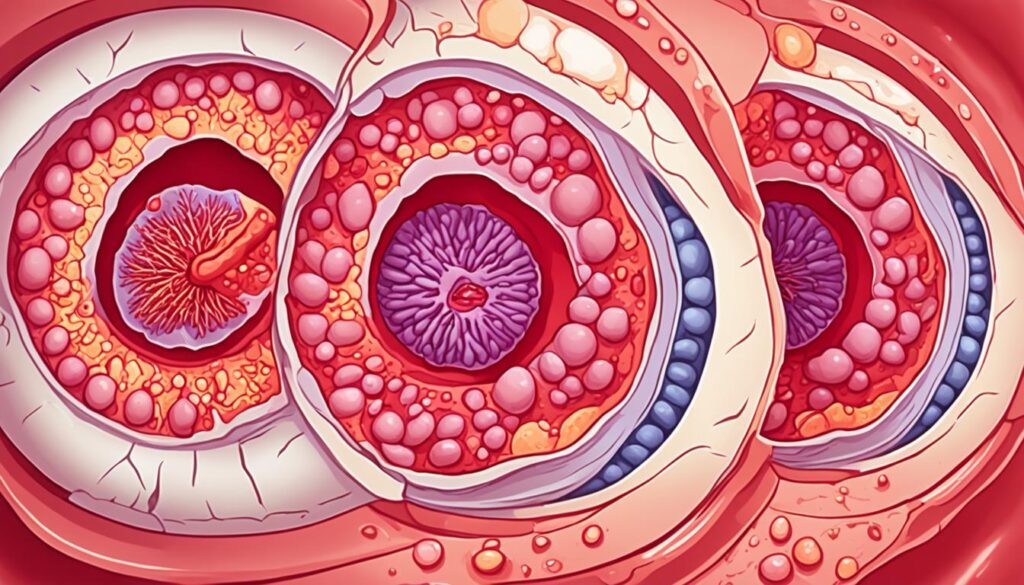
Mechanisms Affecting Moisture-Producing Glands
In Sjogren’s syndrome, the immune system mistakenly attacks the exocrine glands. These include the lacrimal (tear) and salivary glands. Decreased tears and saliva are the result, leading to dry eyes and dry mouth. The immune system damages the glandular tissue with inflammation, which affects their normal tasks. This causes the dryness symptoms in Sjogren’s.
Dysfunction of Lacrimal and Salivary Glands
Faulty immune reactions harm the lacrimal and salivary glands. This damage reduces tear and saliva production. Hence, Sjogren’s patients face dry eye and dry mouth problems.
Aquaporin Degradation and Impaired Function
Aquaporins are key for creating tears and saliva. But, in Sjogren’s, the body attacks these proteins. This hit affects mainly aquaporin-5 (AQP5), found in these glands. The attack makes tear and saliva production go down, causing the syndrome’s dryness.
Inflammation and Glandular Damage
In Sjogren’s syndrome, the body’s defense system mistakenly attacks its own glands. This leads to the release of substances that cause swelling and harm to the salivary and tear glands. These substances pull in immune system cells. Over time, this ongoing swelling stops glands from working as they should.
Role of Inflammatory Mediators
Sjogren’s syndrome pushes the body to make things like cytokines. These substances help kick off swelling and injuries in the mouth and eye glands. They draw in immune cells, such as B and T cells, crowding the glands with them. This swelling is long-lasting and hampers gland performance.
Involvement of Toll-Like Receptors
Toll-like receptors (TLRs) are key in spotting threats and starting the immune response. In Sjogren’s syndrome, TLR3 is especially important in starting gland inflammation. By sensing harmful signals from both inside and outside the body, TLRs can make the situation worse. They do this by turning on the production of more swelling substances, worsening gland damage and troubles.
Hormonal Imbalances and Sjogren’s Syndrome
Sjogren’s syndrome may be linked to not having enough of a hormone called dehydroepiandrosterone (DHEA). This hormone helps control the immune system. If someone with Sjogren’s doesn’t have enough DHEA, it might lead to immune system problems. Not being able to use DHEA well in the salivary glands could be why this happens.
Dehydroepiandrosterone (DHEA) Deficiency
Research shows that DHEA-S levels are lower in people with Sjogren’s compared to those without it. DHEA is important for how our immune system works. If there’s not enough DHEA, it might play a part in causing Sjogren’s. The salivary glands might not work right with DHEA for those with Sjogren’s.
When estrogen levels go down in menopause, the chance of getting Sjogren’s might go up. This points to how important hormones are in this disease. On the other hand, since men have more testosterone, and that can turn into a strong hormone called dihydrotestosterone (DHT), they’re less likely to get Sjogren’s. But, it seems that everyone with Sjogren’s doesn’t change testosterone to DHT very well. This could also add to the hormone problems in the condition.
Autonomic Nervous System Dysfunction
Sjogren’s syndrome is linked to a problem with your body’s autonomic nervous system. This system controls things you don’t think about, like making tears and saliva. When this system doesn’t work right, people with Sjogren’s have trouble making tears and saliva.
They often have issues with their blood vessels not reacting as they should. This can make dry eyes and mouth worse. In simple terms, their body doesn’t manage these things as it normally would.
Experts have done a lot of research on how Sjogren’s affects the autonomic nervous system. They found that many patients in a 2012 study had common problems. These problems were connected to how sick they felt and how active their Sjogren’s seemed to be. A later study in 2017 also found issues with the autonomic system in people with Sjogren’s.
Looking more closely, Sjogren’s seems to affect the heart too. A study in 1998 showed that the autonomic system can mess with how the heart works in Sjogren’s syndrome. Similarly, another study in 2000 looked at heart rate changes in these patients.
These studies suggest that people with Sjogren’s might have trouble with how their blood vessels work. This could be because their autonomic system isn’t managing things correctly. Basically, their body’s system for controlling blood flow isn’t doing its job right.
Recent research points to bigger health risks from this autonomic imbalance. It could signal problems like heart disease and diabetes. A study in 2015 put a spotlight on these risks. Then, in 2018, researchers did a deep dive into how autonomic dysfunction is tied to Sjogren’s disease. They looked at how it connects with the signs of the disease and the body’s immune reactions.
Muscarinic Receptor Autoantibodies
In Sjogren’s syndrome, the body’s defense attacks itself. It makes autoantibodies that target muscarinic acetylcholine receptors. These are found a lot in the salivary and lacrimal glands. The antibodies affect these receptors, leading to dry mouth and eyes.
Anti-Muscarinic Antibodies and Glandular Dysfunction
When looking at people with Sjögren’s syndrome, their anti-M3R levels were high. This was more than in healthy people or those with lupus or arthritis.
There was a strong link between how much anti-M3R someone had and the seriousness of their Sjögren’s syndrome. More anti-M3R meant a worse condition.
Animal Models of Sjogren’s Syndrome
Animal models play a key role in Sjogren’s syndrome research. The NOD mouse model stands out. It naturally develops a condition like human Sjogren’s, affecting salivary and lacrimal glands.
NOD Mouse Model
The NOD mouse model is invaluable for understanding Sjogren’s syndrome. It shows symptoms similar to the human disease. This includes gland damage and autoantibody production, helping scientists explore the disease’s roots.
MRL/lpr Mouse Model
Next, the MRL/lpr mouse model is also critical. It mimics systemic autoimmune disorders, like Sjogren’s. These mice have gland damage and produce autoantibodies. This model aids in studying genetic and immune system influences on Sjogren’s development.
Gene Expression Profiles in Sjogren’s Syndrome
Salivary Gland Gene Expression
Experts have checked how genes work in the salivary glands of those with Sjogren’s syndrome. This shows the key ways our body’s reactions can cause the disease. They found changes in genes linked to fighting off illnesses, swelling, and harming tissue. This helps us see how Sjogren’s syndrome messes with the salivary glands.
Peripheral Blood Gene Expression
Furthermore, scientists looked at how genes act in the blood of Sjogren’s patients. They found unique signs in the blood that could show disease levels and how it goes forward. Looking at gene activities in both key areas and all through the body offers deep insights into Sjogren’s syndrome’s causes.
Role of Type I Interferons
New findings show that type I interferons are crucial in the early immune response. They are linked to the development of Sjogren’s syndrome. In this condition, Sjogren’s patients show a distinct pattern known as an “interferon signature.” This means they have more interferon-regulated genes active in their tissues and blood. This overactive immune response likely leads to the damage seen in their glands and the overall dysfunction of the condition.
B-Cell Activating Factor (BAFF)
BAFF Expression in Salivary Gland Epithelial Cells
The B-cell activating factor (BAFF) is important for keeping B cells healthy and active. It’s also known as B lymphocyte stimulator (BLyS). In Sjogren’s syndrome, BAFF is made too much in the salivary gland cells. This overproduction messes with how BAFF should work, leading to issues with the immune system.
This extra BAFF can make B cells that attack the body live longer and work better. These are common features of Sjogren’s syndrome. People with this disease have fewer special memory B cells. Yet, their types of B cells in the blood can help doctors diagnose the illness.
Too much BAFF in the salivary glands seems to make B cells overly active in Sjogren’s. This has been shown by other studies. Also, comparing B cell behavior from the blood and salivary glands gives us interesting details about how Sjogren’s affects B cells.
Lymphoproliferation and Lymphoma Risk
Sjogren’s syndrome can increase the chance of getting lymphoma, a blood cancer. This risk is higher because of the ongoing stimulation of B cells. These cells may change and grow abnormally, leading to lymphoma in some Sjogren’s patients.
Prelymphomatous Stages
Sjogren’s syndrome’s risk of lymphoma is tied to its early stages. In these phases, there is a big growth and change in B cells. This can later turn into lymphoma for a few with Sjogren’s. Figuring out how this happens is key. It can help find those at risk and start the right care early.
Association with Hepatitis C Virus
Hepatitis C virus (HCV) infection may also matter for Sjogren’s. Many who have symptoms like Sjogren’s are found to have HCV. This link hints that viruses might help start or worsen Sjogren’s. So, it’s critical to check for HCV in those dealing with Sjogren’s.
Treatment Implications
It’s key to understand Sjogren’s syndrome to make better treatments. Scientists are looking at many ways to target the autoimmune issues and poor gland function. They plan to cut down on inflammation, fix how interferon works, slow down B-cells, and more. All this could help lessen how bad Sjogren’s is and slow how quickly it gets worse.
Targeting Specific Pathways
For instance, a drug called etanercept can tackle a protein called tumor necrosis factor-alpha (TNF-α). But, studies say it can’t stop the interferon signature in Sjogren’s patients. This shows the need to dig deeper. We need to find and aim at the pathways most important in causing Sjogren’s.
Etanercept and Interferon Pathway Activation
The fact that etanercept doesn’t fully stop the interferon signature says a lot. It tells us the interferon pathway might be crucial in Sjogren’s. This drives the push for more research. By hitting the main pathways, scientists hope to make treatments that really work, easing symptoms and maybe even turning back the harm of autoimmunity in Sjogren’s.
Final Thoughts from Dr. Chugh
As a U.S.-trained neurologist, I’ve seen the confusion and delays people face with this disease. The earlier you understand what causes Sjogren’s syndrome, the better your chances of managing it.
Dry eyes, a tired body, or mouth discomfort may seem minor. But when these persist, they need attention.
If you or someone in your family is showing signs, don’t wait.
Book your consultation with Dr. Chandril Chugh and get clarity on what’s happening inside your body.
FAQ
What is Sjogren’s syndrome?
Sjogren’s syndrome is when the body’s immune system attacks its own cells. This often happens to glands making tears and saliva. It causes symptoms like dry eyes and mouth.
What are the symptoms of Sjogren’s syndrome?
The key signs of Sjogren’s syndrome are dry eyes and mouth. It happens because the immune system attacks the glands. Joints, lungs, kidneys, and nerves can also be affected.
Who is at risk of developing Sjogren’s syndrome?
It’s more common in women, usually after they’re 40. Risk goes up if you have other autoimmune diseases like rheumatoid arthritis. Being female and older also add to the risk.
What causes Sjogren’s syndrome?
Sjogren’s is an autoimmune problem with different causes. Genes, hormones, and the environment play a part. They make the immune system harm moisture glands.
How does the immune system contribute to Sjogren’s syndrome?
The immune system targets and damages tear and salivary glands in Sjogren’s. This causes less tears and saliva, leading to dry eyes and mouth.
What genetic factors are associated with Sjogren’s syndrome?
Gene variants, especially in the HLA system, relate to a higher Sjogren’s risk. These genes control the immune system’s actions.
How does the dysfunction of aquaporins contribute to Sjogren’s syndrome?
Aquaporins help make tears and saliva. But in Sjogren’s, the body attacks them. This affects how moisture is made, leading to dry eyes and mouth.
What is the role of inflammation in Sjogren’s syndrome?
In Sjogren’s, the immune system starts an inflammatory reaction. This harms moisture glands. It leads to problems producing saliva and tears.
How do Toll-like receptors (TLRs) influence Sjogren’s syndrome?
Some TLRs, like TLR3, start inflammation in Sjogren’s. They can make the glands more damaged, worsening the condition.
What is the role of hormonal factors in Sjogren’s syndrome?
DHEA, an adrenal hormone, is low in Sjogren’s patients. It helps control the immune system. Its drop might make the disease worse.
How does the autonomic nervous system dysfunction affect Sjogren’s syndrome?
Sjogren’s can mess with the autonomic nervous system. It controls things like tears and saliva. This causes more severe dry mouth and eyes.
What is the role of muscarinic receptor autoantibodies in Sjogren’s syndrome?
In Sjogren’s, the immune system can make autoantibodies that block muscarinic receptors. These are important for moisture glands. This leads to the dryness in the mouth and eyes.
What are the environmental triggers for Sjogren’s syndrome?
Besides genes, infections can start Sjogren’s. Viruses like Epstein-Barr and hepatitis C might play a role.
What animal models are used to study Sjogren’s syndrome?
The NOD and MRL/lpr mouse models help study the disease. They showcase what happens in Sjogren’s accurately – from gland issues to autoantibodies.
How are gene expression profiles used to understand Sjogren’s syndrome?
Scientists find Sjogren’s clues by looking at genes in saliva and blood. This shows what’s going wrong, helping understand the disease better.
What is the role of type I interferons in Sjogren’s syndrome?
Interferons, proteins in the immune system, heavily influence Sjogren’s. They’re in high amounts in patients, possibly causing gland harm.
How does B-cell activating factor (BAFF) contribute to Sjogren’s syndrome?
BAFF overactivity in glands is a key part of Sjogren’s. It helps B-cells survive and work too much. This might worsen the disease.
What is the link between Sjogren’s syndrome and lymphoma?
People with Sjogren’s have a higher lymphoma risk. This might be because their immune system is too active, putting them at risk.
How is the treatment of Sjogren’s syndrome being targeted?
Scientists are looking into ways to fix key issues in Sjogren’s, like too much inflammation and autoimmunity. New treatments are on the horizon.
Source Links
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/symptoms-causes/syc-20353216
- https://www.ncbi.nlm.nih.gov/books/NBK459485/
- https://www.niams.nih.gov/health-topics/sjogrens-syndrome
- https://www.webmd.com/a-to-z-guides/sjogrens-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8863725/
- https://www.ncbi.nlm.nih.gov/books/NBK431049/
- https://versusarthritis.org/about-arthritis/conditions/sjoegrens-syndrome/
- https://www.womensinternational.com/blog/sjogrens-syndrome/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6928446/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9248235/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8350514/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5036946/
- https://www.nature.com/articles/3700173
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4425610/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7338666/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6917337/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3273959/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3778845/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7916411/
- https://www.jrheum.org/content/50/9/1103
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6819875/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998301/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8328496/
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/diagnosis-treatment/drc-20353221
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5410683/
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




