Basilar artery migraine, also known as basilar migraines or migraines with brainstem aura, is a unique type of migraine that originates in the brainstem. It is characterized by aura symptoms originating from the brainstem, such as vertigo, double vision, difficulty speaking, and lack of coordination. These symptoms can occur 10 minutes to 45 minutes before the onset of a headache. It is important to be able to recognize these specific symptoms in order to properly identify and manage basilar artery migraines.
Key Takeaways:
- Basilar artery migraines are a subtype of migraines with aura.
- Symptoms originate from the brainstem and include vertigo, difficulty speaking, double vision, and coordination problems.
- Recognition of these symptoms is crucial for accurate diagnosis and effective management.
- A proper understanding of basilar artery migraine symptoms aids in identifying triggers and implementing preventive measures.
- Consultation with a healthcare professional is recommended for diagnosis and treatment.
Table of Contents
ToggleWhat is Basilar Migraine?
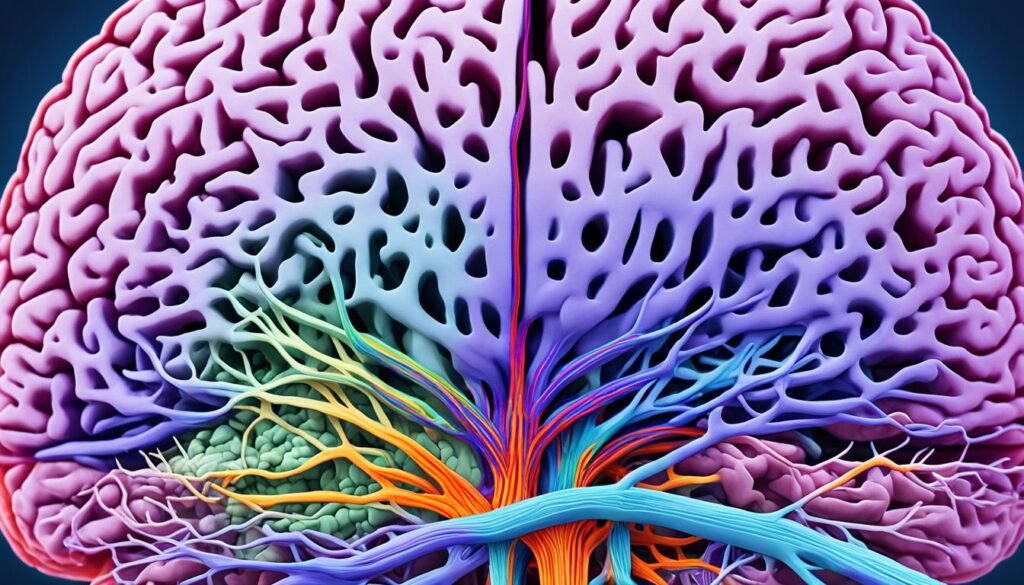
Basilar migraine, also known as basilar artery migraine, brainstem migraine, or vertebrobasilar migraine, is a subtype of migraine with aura. It was originally believed to be caused by spasms of the basilar artery, but it is now understood to be due to the firing of nerves in the brainstem. Basilar migraines are characterized by aura symptoms originating from the brainstem or both cerebral hemispheres, along with typical symptoms of a migraine, such as headache pain and sensitivity to light and sound.
During a basilar migraine episode, individuals may experience a range of symptoms that can be debilitating. These symptoms can include vertigo, difficulty speaking, double vision, impaired coordination, and other sensory disturbances. The aura symptoms are usually followed by the onset of a throbbing headache, often accompanied by sensitivity to light and sound.
Basilar migraines are often mistaken for other types of migraines or neurological conditions due to the similarity of symptoms. However, the distinctive feature of basilar migraines is the involvement of the brainstem, which sets it apart from other types of migraines.
Etiology of Basilar Migraine
The etiology of basilar migraines is still not fully understood. However, researchers believe that a combination of environmental factors and genetic predisposition contribute to the development of this condition. Understanding the causes and triggers of basilar migraines is important for managing and preventing future episodes.
Common triggers for basilar migraines include:
- Strong smells
- Loud noises
- Weather changes
- Sleep disturbances
- Stress
- Physical exertion
- Certain foods
- Hormonal changes in females
These triggers can vary from person to person, and identifying individual triggers can help manage and reduce the frequency of basilar migraines.
While the genetic basis of basilar migraines is not yet well understood, some studies suggest a potential genetic involvement, particularly in genes associated with migraine with typical aura. Further research is needed to fully elucidate the genetic factors contributing to basilar migraines.
Risk Factors for Basilar Migraine
Though the exact cause of basilar migraines remains uncertain, certain risk factors have been identified. These include:
| Risk Factors | Description |
|---|---|
| Gender | Basilar migraines are more common in females than males. |
| Age | Basilar migraines typically manifest in adolescence and young adulthood, with an age of onset between 7 and 20 years old. |
| Family history | A family history of migraines, particularly migraines with aura, may increase the risk of developing basilar migraines. |
| Hormonal changes | Fluctuations in hormone levels, such as those that occur during menstruation, pregnancy, or menopause, may trigger or worsen basilar migraines. |
While these risk factors may increase the likelihood of developing basilar migraines, it’s important to note that not everyone with these risk factors will develop the condition. Basilar migraines can also occur in individuals without any known risk factors.
Epidemiology of Basilar Migraine
Understanding the epidemiology of basilar migraine can provide valuable insights into the prevalence and age of onset for this unique type of migraine. While the exact numbers are unknown, basilar migraine is believed to be more commonly seen in females than males. It can occur at any age, but it is most frequently observed in adolescence and young adults, with the age of onset typically ranging from 7 to 20 years old.
Prevalence of Basilar Migraine
The exact prevalence and incidence rates of basilar migraine are yet to be determined. However, studies suggest that it accounts for only a small portion of all migraines, estimated to be around 4% to 12%. Because basilar migraines are relatively rare, they require a unique set of diagnostic criteria to differentiate them from other types of migraines.
Age of Onset for Basilar Migraine
Basilar migraines can manifest at any age, but they are more commonly observed in younger individuals. The adolescent and young adult age groups are particularly susceptible to experiencing basilar migraines. The fact that basilar migraines tend to occur during these developmental stages highlights the importance of early recognition and effective management for improved quality of life.
| Characteristics | Females | Males |
|---|---|---|
| Prevalence | Higher | Lower |
| Age of Onset | Adolescence and Young Adults | Varied |
Note: The data in the table above is for illustrative purposes and may not reflect precise statistics.
Understanding the epidemiology of basilar migraine, including its prevalence and age of onset, is crucial for healthcare professionals and individuals affected by this condition. By recognizing the demographic characteristics associated with basilar migraines, appropriate diagnosis, management, and support can be provided, leading to improved outcomes and a better quality of life.
Pathophysiology of Basilar Migraine
Basilar migraine, previously believed to be caused by vascular pathology involving spasms of the basilar artery, is now understood differently. Research has found no evidence to support this theory, leading to a new understanding of the pathophysiology. It is now known that basilar migraines are related to the firing of nerves in the brainstem, specifically the brainstem aura symptoms seen in basilar migraines are believed to be a result of cortical spreading depression.
Cortical spreading depression refers to a wave of depolarization that spreads across the cerebral cortex, affecting both neurons and glia. This depolarization leads to the development of aura symptoms commonly seen in basilar migraines.
Understanding the pathophysiology of basilar migraines can help in the development of targeted therapeutic approaches and enhance our knowledge of this complex neurological disorder.
Basilar Artery Migraine Symptoms
Basilar migraines are characterized by a range of symptoms that can vary from person to person. These symptoms, also known as aura symptoms, are generally reversible and may occur before the onset of a headache. It is important to recognize and understand these symptoms in order to properly identify and manage basilar migraines.
The most common symptom of basilar migraines is vertigo, a sensation of spinning or dizziness. Other aura symptoms that may occur include:
- Dysarthria (difficulty speaking)
- Diplopia (double vision)
- Tinnitus (ringing in the ears)
- Impaired hearing
- Lack of coordination
- Confusion
- Loss of consciousness (in some cases)
These aura symptoms are usually followed by an occipital headache, which is characterized by pain at the back of the head. The headache can last for hours to days and can be accompanied by sensitivity to light and sound.
If you experience any weakness or visual loss along with these symptoms, it is important to seek medical evaluation to rule out other potential causes.

Diagnosis of Basilar Migraine
The diagnosis of basilar migraine involves the assessment of specific criteria outlined by the International Classification of Headache Disorders. These criteria help healthcare professionals identify and confirm the presence of basilar migraine based on distinctive characteristics. To make a diagnosis of basilar migraine, the following criteria should be met:
- Aura symptoms originating from the brainstem:
- Dysarthria (difficulty speaking)
- Vertigo (spinning sensation)
- Tinnitus (ringing in the ears)
- Hearing impairment
- Diplopia (double vision)
- Ataxia (impaired coordination)
- Decreased level of consciousness
- Bilateral paresthesia (abnormal skin sensations)
- Aura symptoms lasting for more than 5 minutes
- Aura symptoms followed by a headache that begins either during the aura or within 1 hour
In addition to these criteria, healthcare providers may perform diagnostic tests to rule out other potential causes of the symptoms and further support the diagnosis of basilar migraine. These diagnostic tests can include:
- Brain imaging (MRI or CT scans): These tests can help identify any abnormalities, such as tumors or vascular malformations, which may be causing the symptoms.
- EEG (Electroencephalogram): This test measures the electrical activity of the brain and can help rule out seizures or other brain abnormalities.
| Diagnostic Criteria | Presence |
|---|---|
| Aura symptoms originating from the brainstem | Present |
| Aura symptoms lasting for more than 5 minutes | Present |
| Aura symptoms followed by a headache within 1 hour | Present |
| Brain imaging (MRI or CT scans) | Performed |
| EEG (Electroencephalogram) | Performed |
The diagnostic criteria and tests help healthcare professionals accurately diagnose basilar migraine and differentiate it from other conditions with similar symptoms. Through proper diagnosis, individuals with basilar migraine can receive appropriate treatment and management strategies to effectively alleviate their symptoms and improve their quality of life.
Evaluation of Basilar Migraine
When diagnosing and evaluating basilar type migraine, several tests and procedures can provide valuable insights. Brain imaging, such as MRI or CT scans, are commonly employed to rule out other potential causes of the symptoms. These imaging techniques help identify conditions such as stroke, arteriovenous malformations, or brain tumors that may mimic basilar migraines.
In addition to brain imaging, an electroencephalogram (EEG) may be performed to evaluate brain activity and detect any abnormalities. This test is particularly useful in cases where there is confusion or a decreased level of consciousness, as it helps rule out seizures as a cause of the symptoms.
In some instances, 24-hour Holter monitoring may be recommended to assess the heart’s electrical activity and evaluate for arrhythmias. This monitoring device records the heart’s rhythm continuously for 24 hours, providing valuable information on any irregularities that may contribute to the occurrence of basilar migraines.
These evaluation procedures help healthcare professionals establish an accurate diagnosis and better understand the underlying mechanisms of basilar migraines, enabling them to develop a targeted treatment plan specific to each individual.
Treatment and Management of Basilar Migraine
When it comes to the basilar artery migraine treatment and management, the focus is on providing symptomatic relief and implementing preventive measures to reduce the frequency and severity of episodes. By effectively addressing both acute symptoms and long-term prevention, individuals can better navigate the challenges associated with basilar migraines.
For immediate relief from headache pain and associated symptoms, several medication options can be considered:
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen sodium, can help alleviate mild to moderate headache pain and reduce inflammation.
- Anti-emetics: Anti-emetic medications like metoclopramide or prochlorperazine can offer relief from nausea and vomiting, which are common symptoms during a basilar migraine attack.
- Pain relievers: Over-the-counter pain relievers like acetaminophen or aspirin may be effective in reducing headache pain.
However, it’s important to note that triptans and ergotamines, which are commonly used to treat other types of migraines, are generally avoided in basilar migraines due to the potential risk of increasing cerebral ischemia.
Preventive therapy plays a crucial role in managing basilar migraines and reducing their frequency. This involves identifying and modifying triggers that may precipitate an attack. By keeping a headache diary and tracking factors like stress, sleep patterns, diet, and hormonal changes, individuals can gain insights into their unique triggers and make lifestyle adjustments accordingly.
Medications can also be prescribed for preventive therapy:
- Verapamil: This medication, typically used for heart conditions, is often effective in preventing basilar migraines by regulating blood pressure and blood flow in the brain.
- Topiramate: An anticonvulsant drug, topiramate has shown efficacy in reducing the frequency and severity of migraine attacks, including basilar migraines.
Non-pharmacological therapies can complement medication-based treatments or be used as standalone options for prevention:
- Relaxation techniques: Practices like deep breathing, progressive muscle relaxation, and guided imagery can help manage stress and promote overall well-being.
- Acupuncture and massage: These alternative therapies have been used to alleviate migraine symptoms and promote relaxation. Acupuncture involves the insertion of thin needles at specific points on the body, while massage focuses on relieving muscle tension and improving blood flow.
- Cognitive behavior therapy: This form of therapy can help individuals recognize and modify negative thought patterns, leading to improved coping strategies and better migraine management.
- Biofeedback: This technique utilizes instruments that measure physiological responses, such as muscle tension or skin temperature, to provide real-time feedback. By learning to control these responses, individuals may experience a reduction in migraine symptoms.
By combining medication, preventive measures, and non-pharmacological therapies, individuals with basilar migraines can take charge of their condition and adopt a comprehensive approach to treatment and management.
Differential Diagnosis of Basilar Migraine
When diagnosing basilar migraines, it is essential to consider other conditions that may present with similar symptoms. Some of these conditions include:
- Hemiplegic migraines: These migraines are characterized by temporary paralysis or weakness on one side of the body, which can be mistaken for the impaired coordination seen in basilar migraines.
- Meniere’s disease: Meniere’s disease is a disorder of the inner ear that can cause dizziness, hearing loss, and ringing in the ears, symptoms that can overlap with those of basilar migraines.
- Vestibular disease: Vestibular disorders affect the inner ear and can cause vertigo, a common symptom of basilar migraines.
- Transient ischemic attacks (TIAs) and strokes: Both TIAs and strokes can produce neurological symptoms similar to those seen in basilar migraines, including double vision, difficulty speaking, and lack of coordination.
- Brainstem arteriovenous (AV) malformations: These abnormalities in blood vessels in the brainstem can lead to symptoms similar to basilar migraines, such as vertigo, impaired hearing, and diplopia.
- Tumors: Tumors in the brainstem can cause a variety of symptoms, including vertigo, vision changes, and impaired coordination, which can be mistaken for basilar migraines.
- Meningitis: Meningitis is an infection that causes inflammation of the membranes surrounding the brain and spinal cord. Some of its symptoms, such as headache, confusion, and coordination difficulties, can mimic those of basilar migraines.
It is crucial to rule out these conditions before making a definitive diagnosis of basilar migraines. This typically requires a thorough examination, review of medical history, and diagnostic tests such as brain imaging (MRI or CT scans) and nerve tests. These evaluations can help differentiate basilar migraines from other conditions and ensure appropriate management and treatment.
| Condition | Key Symptoms | Diagnostic Tests |
|---|---|---|
| Hemiplegic migraines | Temporary paralysis or weakness on one side of the body | No specific diagnostic tests Diagnosis based on symptoms and exclusion of other causes |
| Meniere’s disease | Dizziness, hearing loss, ringing in the ears | Audiometry (hearing test) Electronystagmography (ENG) Magnetic resonance imaging (MRI) of the inner ear |
| Vestibular disease | Vertigo, balance problems | Electronystagmography (ENG) Vestibular evoked myogenic potentials (VEMP) |
| Transient ischemic attacks (TIAs) and strokes | Temporary neurological deficits such as double vision, difficulty speaking, lack of coordination | Computed tomography (CT) scan of the head Magnetic resonance imaging (MRI) of the brain Cerebral angiography |
| Brainstem arteriovenous (AV) malformations | Vertigo, impaired hearing, diplopia | Magnetic resonance imaging (MRI) or computed tomography (CT) angiography Digital subtraction angiography (DSA) |
| Tumors | Vertigo, vision changes, impaired coordination | Magnetic resonance imaging (MRI) of the brain |
| Meningitis | Headache, confusion, coordination difficulties | Lumbar puncture (CSF analysis) Blood cultures Computed tomography (CT) scan or magnetic resonance imaging (MRI) of the brain |
Prognosis and Complications of Basilar Migraine
Basilar migraines can have a significant impact on your daily life, as they tend to be more disabling than other types of migraines. These migraines are characterized by increased severity, longer duration of symptoms, and a range of aura symptoms originating from the brainstem. However, there is some good news. The frequency of basilar migraine episodes tends to decrease with age, and they often evolve into more typical patterns of migraines.
While it is known that migraines with aura, including basilar migraines, have a slightly higher risk of stroke compared to migraines without aura, it’s important to note that the overall risk of stroke in basilar migraines is not significantly higher than in migraines with typical aura. However, it is crucial to address modifiable risk factors that can further increase the risk of stroke.
Some common complications associated with basilar migraine include:
- Disruption of daily activities and reduced quality of life
- Impaired cognitive function during and after migraine attacks
- Mental health challenges, such as anxiety and depression
- Increased risk of stroke, especially in individuals who smoke or use estrogen contraceptives
Managing and minimizing the risk of complications involves:
- Working closely with your healthcare provider to develop an individualized treatment plan
- Identifying and avoiding triggers that may precipitate basilar migraines
- Implementing lifestyle modifications, such as maintaining a regular sleep schedule, managing stress, and staying hydrated
- Using preventive medications, as prescribed by your healthcare provider, to reduce the frequency and severity of the migraines
- Monitoring and addressing modifiable risk factors for stroke, such as smoking and the use of estrogen contraceptives
Comparison of Basilar Migraine with Typical Migraine and Risk of Stroke
| Factor | Basilar Migraine | Typical Migraine |
|---|---|---|
| Risk of Stroke | Slightly higher compared to migraines without aura | Slightly higher compared to migraines without aura |
| Risk Factors for Stroke | Can be further increased by modifiable risk factors such as smoking and estrogen contraceptive use | Can be further increased by modifiable risk factors such as smoking and estrogen contraceptive use |
Conclusion
Basilar artery migraines, also known as basilar migraines or migraines with brainstem aura, are a unique subtype of migraines that originate from the brainstem. They are characterized by a range of symptoms such as vertigo, difficulty speaking, double vision, and impaired coordination. These symptoms can occur prior to the onset of a headache.
While the exact cause of basilar migraines is unknown, environmental triggers and genetic factors may contribute to their development. Diagnosis is based on specific criteria, and it is crucial to rule out other potential causes of similar symptoms. Treatment and management strategies primarily focus on providing symptom relief and implementing preventive measures, which may include lifestyle modifications and the use of medications.
Basilar migraines generally have a favorable prognosis. However, it is important to note that they carry a slightly increased risk of stroke compared to migraines without aura. Addressing modifiable risk factors and seeking timely medical attention are essential in the proper diagnosis and management of this condition.
FAQ
What are the basilar artery migraine symptoms?
The symptoms of basilar artery migraine include vertigo, difficulty speaking, double vision, impaired coordination, and headache pain.
What is basilar migraine?
Basilar migraine, also known as basilar artery migraine, brainstem migraine, or vertebrobasilar migraine, is a subtype of migraine with aura that originates from the brainstem.
What are the triggers for basilar migraine?
Common triggers for basilar migraine include strong smells, loud noises, weather changes, sleep disturbances, stress, physical exertion, certain foods, and hormonal changes in females.
What is the age of onset for basilar migraine?
Basilar migraine can occur at any age, but it is more commonly seen in adolescence and young adults, typically between 7 and 20 years old.
What is the pathophysiology of basilar migraine?
Basilar migraine is believed to be related to the firing of nerves in the brainstem and the development of aura symptoms due to cortical spreading depression, a wave of depolarization across the cerebral cortex.
What are the symptoms of basilar migraine?
The symptoms of basilar migraine include vertigo, dysarthria (difficulty speaking), diplopia (double vision), tinnitus (ringing in the ears), impaired hearing, lack of coordination, confusion, and sometimes loss of consciousness.
How is basilar migraine diagnosed?
Basilar migraine is diagnosed based on specific criteria outlined by the International Classification of Headache Disorders, which include the presence of aura symptoms originating from the brainstem, lasting for more than 5 minutes, followed by a headache within 1 hour.
What tests are performed to evaluate basilar migraine?
Diagnostic tests, such as brain imaging (MRI or CT scans) and EEG, may be performed to rule out other potential causes of the symptoms and assess brain activity.
How is basilar migraine treated and managed?
Treatment focuses on symptomatic relief and may involve the use of NSAIDs, anti-emetics, and pain relievers. Preventive therapy includes identifying and modifying triggers, lifestyle changes, and the use of medications such as verapamil and topiramate.
What conditions should be considered in the differential diagnosis of basilar migraine?
Conditions with symptoms similar to basilar migraine include hemiplegic migraines, Meniere’s disease, vestibular disease, transient ischemic attacks (TIAs), strokes, brainstem AV malformations, tumors, and meningitis.
What is the prognosis and risk of complications in basilar migraine?
Basilar migraines can be more disabling, but the frequency of episodes tends to decrease with age. While there is a slightly increased risk of stroke compared to migraines without aura, the risk of stroke in basilar migraines is not significantly higher than in migraines with typical aura.
Source Links
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




