If you experience migraines with aura symptoms originating from the brainstem, you may be suffering from basilar type migraines. This subtype of migraines is characterized by a range of symptoms, including vertigo, impaired coordination, confusion, and even loss of consciousness. Understanding the symptoms and available relief options is crucial in managing this condition effectively.
Key Takeaways:
- Basilar type migraines are a subtype of migraines with aura originating from the brainstem.
- Common symptoms include vertigo, impaired coordination, confusion, and loss of consciousness.
- Triggers for basilar migraines can include strong smells, loud noises, weather changes, lack of sleep, stress, certain foods, and hormonal changes.
- Treatment options for basilar type migraines include NSAIDs, anti-emetics, and lifestyle modifications such as stress management and trigger avoidance.
- Preventive therapies and medications may also be recommended for frequent and disabling migraines.
Table of Contents
ToggleUnderstanding Basilar Migraine
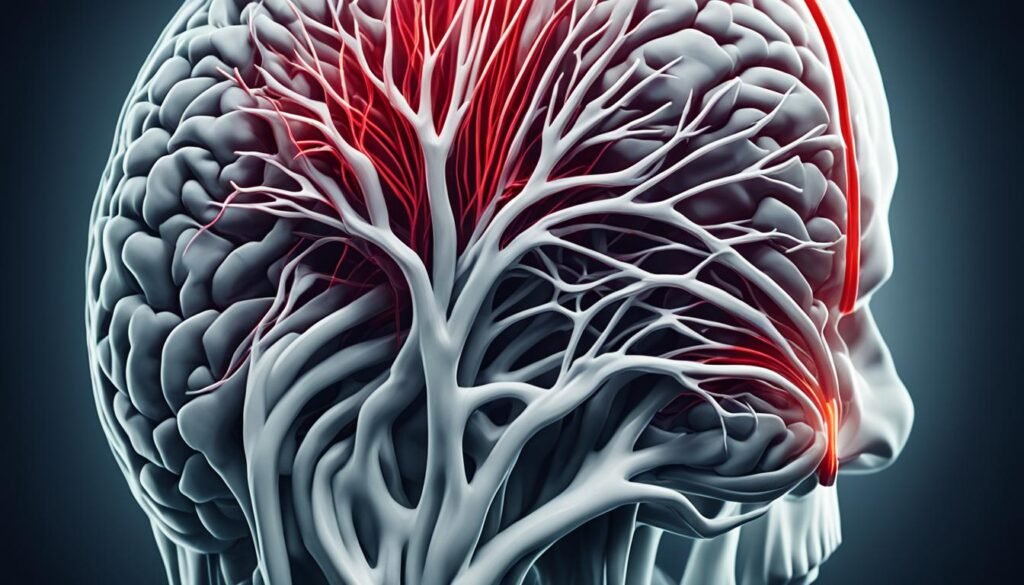
Basilar artery migraine, also known as migraine with brainstem aura, is a rare type of migraine that originates in the brainstem. This condition is characterized by the occurrence of aura symptoms before or during a migraine episode.
Aura symptoms associated with basilar migraines can manifest as various sensory and motor changes. These can include alterations in speech, hearing, and vision. Individuals may also experience vertigo, tinnitus, double vision, impaired muscle control, and a reduced level of consciousness. It is important to note that while these symptoms can be frightening, they are completely reversible.
Basilar migraines can persist for a few hours to several days, significantly impacting the individual’s daily life. The frequency and severity of episodes can be influenced by various factors, including stress, lack of sleep, certain foods, hormonal changes, and environmental stimuli.
It is crucial to understand the symptoms associated with basilar migraines to differentiate them from other types of migraines and seek appropriate treatment. Early recognition and management can significantly enhance the quality of life for individuals affected by this condition.
| Aura Symptoms | Key Features |
|---|---|
| Changes in speech | Altered speech patterns, difficulty finding words |
| Hearing changes | Impaired hearing, hypersensitivity to sound (phonophobia) |
| Vision changes | Visual disturbances such as blurred vision, seeing flashing lights or zigzag lines |
| Vertigo | Sensation of spinning or dizziness |
| Tinnitus | Ringing or buzzing sound in the ears |
| Double vision | Seeing two overlapping images |
| Impaired muscle control | Difficulty with coordination and fine motor skills |
| Reduced level of consciousness | Feeling disoriented, confused, or experiencing temporary loss of consciousness |
Etiology and Pathophysiology
The exact cause of basilar migraines is still unknown, but researchers believe that both genetic and environmental factors contribute to its development. Basilar migraines are now recognized as a subtype of migraines with aura and are commonly referred to as “migraines with brainstem aura.”
The basilar artery migraine symptoms experienced during basilar migraines are believed to be caused by cortical spreading depression. This phenomenon refers to a self-propagating wave that spreads across the cerebral cortex due to the depolarization of neurons and glia. The firing of nerves in the brainstem is thought to play a significant role in triggering basilar migraines.
Contrary to previous beliefs, there is no proven evidence of vascular pathology involved in basilar migraines. Instead, it is the abnormal firing of nerves in the brainstem that leads to the characteristic aura symptoms.

Diagnosis and Evaluation
Diagnosing basilar migraine involves a thorough evaluation based on specific criteria outlined by the International Classification of Headache Disorders. These criteria are essential for distinguishing basilar migraine from other conditions with similar symptoms. The diagnosis relies on the presence of aura symptoms originating from the brainstem or both occipital hemispheres, the duration and characteristics of the aura symptoms, and the association of migraine without aura beginning during or within 1 hour of the aura.
While basilar migraine diagnosis is primarily based on clinical criteria, additional tests may be ordered to rule out other potential causes and ensure accurate evaluation. Imaging studies such as MRI or CT scans may be performed to exclude conditions like stroke, tumors, or infections that can present with similar symptoms. In some cases, an electroencephalogram (EEG) may be necessary to assess brain activity and rule out seizures, particularly in instances where confusion and decreased level of consciousness occur.
Evaluating basilar migraine requires a comprehensive approach that combines clinical assessment, patient history, and appropriate basilar type migraine diagnostic criteria tests. This ensures an accurate diagnosis and enables healthcare professionals to develop an effective treatment plan tailored to the individual’s needs.
Treatment and Management
The basilar artery migraine treatment focuses on relieving symptoms and effectively managing the condition. Acute attacks are typically managed with medications such as NSAIDs (nonsteroidal anti-inflammatory drugs) and anti-emetics to alleviate pain and reduce nausea. Recent studies have shed light on the potential benefits of triptans and ergotamines in providing headache relief, despite their traditionally avoided status in basilar migraines due to concerns of increased cerebral ischemia.
Preventive therapy may be recommended for individuals experiencing frequent and disabling migraines. Medications like verapamil and topiramate are commonly prescribed for their ability to reduce the frequency and severity of migraines. However, it’s essential to consult with a healthcare professional to determine the most suitable preventive treatment plan based on individual needs and medical history.
While medications play a critical role in managing basilar migraines, lifestyle modifications are equally important for long-term management and prevention. Making specific changes to your daily routine can help reduce the frequency of migraine attacks. It is recommended to:
- Avoid known triggers such as strong smells, loud noises, and certain foods.
- Practice stress management techniques, such as meditation and deep breathing exercises.
- Engage in regular exercise to promote overall well-being and reduce stress levels.
Incorporating these lifestyle modifications can significantly contribute to the prevention of migraine attacks and improve overall quality of life. Consulting with a healthcare professional is essential to develop an individualized treatment plan that addresses the specific needs and triggers of each person with basilar migraines.
Prognosis and Complications
Basilar migraines can have a significant impact on your daily life, as they tend to be more disabling than migraines without aura or migraines with typical aura. The severity and longer duration of symptoms can make it challenging to carry out your usual activities. However, there is some good news – the frequency of basilar migraines typically decreases with age, and they often evolve into more typical patterns.
While migraines with aura, including basilar migraines, have a slightly higher risk of stroke compared to migraines without aura, the specific risk remains unclear. It’s important to note that the overall risk of stroke associated with migraines is still relatively low. However, certain factors such as smoking and the use of estrogen contraceptives can further increase this risk. Therefore, it’s essential to address these risk factors and make necessary lifestyle changes to reduce the likelihood of complications.
Potential Complications of Basilar Migraines
Basilar migraines can have various complications or associated conditions. These may include:
- Increased risk of stroke
- Disruption of daily activities
- Interference with work or school
- Physical and emotional distress
- Decreased quality of life
These complications can be significant, underscoring the importance of effective migraine management and preventive strategies. By working closely with your healthcare provider and making the necessary lifestyle modifications, you can reduce the frequency and severity of basilar migraines, improving your overall well-being.
Managing Basilar Migraines for Better Prognosis
While basilar migraines can be challenging to deal with, a proactive approach to management can lead to a better prognosis. Here are some strategies that may help:
- Identify and manage triggers: Keep a headache diary to track potential triggers and avoid them as much as possible.
- Practice stress management: Engage in relaxation techniques, such as deep breathing, meditation, or yoga, to reduce stress levels.
- Consider preventive medications: Consult your healthcare provider about preventive medications to reduce the frequency of basilar migraines.
- Make lifestyle modifications: Maintain a balanced diet, exercise regularly, prioritize quality sleep, and limit alcohol and caffeine intake.
By taking these steps, you can actively participate in the management of basilar migraines and improve your overall prognosis. Remember, it’s crucial to work closely with your healthcare provider to tailor a treatment plan that suits your specific needs and ensures the most effective management of your migraines.
Triggers and Prevention
Basilar migraines, like other types of migraines, can be triggered by various factors. Identifying these triggers and taking preventive measures can help reduce the frequency and severity of migraine attacks. Here are some common triggers to be aware of:
- Stress: Emotional and physical stress can trigger basilar migraines. Finding effective stress management techniques such as deep breathing exercises, meditation, or yoga can help prevent migraines.
- Alcohol and Caffeine: Excessive consumption of alcohol and caffeine can trigger migraines. Limiting or avoiding these substances may help prevent migraine attacks.
- Hormonal Changes: Fluctuations in hormone levels, particularly estrogen, can trigger migraines in some individuals. Understanding your hormonal patterns and discussing hormone-based treatments with your healthcare provider may be beneficial.
- Lack of Sleep: Irregular sleep patterns or lack of sufficient sleep can trigger migraines. Establishing a regular sleep schedule and practicing good sleep hygiene can contribute to preventing migraines.
- Strong Smells: Certain strong smells, such as perfumes, chemicals, or even strong cooking odors, can trigger migraines in some individuals. Minimizing exposure to these triggers or using scent-free products can help prevent migraines.
- Certain Foods: Some foods can act as triggers for migraines, including aged cheeses, processed meats, chocolate, and foods containing monosodium glutamate (MSG). Keeping a headache diary and avoiding known trigger foods can aid in preventing migraines.
In addition to identifying and avoiding triggers, preventive medications may be prescribed for individuals with frequent and disabling migraines. These medications are designed to reduce the frequency and severity of migraine attacks. Discussing preventive options with a healthcare professional can help determine the most suitable preventive medication for you.
Preventing Basilar Migraine Attacks
Preventing basilar migraines involves a combination of trigger management and lifestyle modifications. Here are some strategies to consider:
- Keep a Headache Diary: Tracking your migraines and potential triggers in a headache diary can help you identify patterns and avoid triggers in the future.
- Practice Stress Management: Finding effective stress management techniques, such as regular exercise, deep breathing exercises, or engaging in hobbies, can help reduce stress levels and prevent migraines.
- Maintain a Regular Sleep Schedule: Establishing a consistent sleep routine, including going to bed and waking up at the same time every day, can help regulate your body’s internal clock and prevent migraines.
- Avoid Known Triggers: If certain triggers consistently lead to migraines, it’s important to avoid or minimize exposure to them. This may include avoiding certain foods, limiting alcohol and caffeine intake, and managing environmental triggers.
By being proactive and making necessary lifestyle modifications, you can take control of your basilar migraines and reduce their impact on your daily life.

Lifestyle Modifications
In addition to trigger avoidance, making certain lifestyle modifications can help manage basilar migraines effectively. By incorporating the following habits into your everyday life, you can significantly reduce the frequency and severity of your migraines:
- Maintain a balanced diet, focusing on nutritious foods.
- Avoid the consumption of drugs and alcohol.
- Ensure you do not skip meals and maintain a regular eating schedule.
- Limit your caffeine intake, as it can act as a trigger for migraines.
- Avoid specific trigger foods such as dairy, wheat, chocolate, and citrus fruits.
- Engage in regular exercise to promote overall physical and mental well-being.
- Practice relaxation techniques, like deep breathing exercises and meditation, to reduce stress levels.
- Consider alternative therapies such as acupuncture and massage to alleviate migraine symptoms.
- Explore cognitive-behavioral therapy to develop effective coping strategies for dealing with migraines.
- Try biofeedback techniques to gain better control over your body’s responses to stress and pain.
By embracing these lifestyle modifications, you can proactively manage your basilar migraines and improve your quality of life.
Conclusion
Basilar migraines, with their distinct brainstem aura symptoms, are a rare subtype of migraines. Although the exact cause is still unknown, various triggers such as stress, lack of sleep, certain foods, and hormonal changes can contribute to the occurrence of these migraines. Diagnosis is based on specific criteria and requires ruling out other potential causes to ensure accurate identification.
Treatment options for basilar migraines focus on relieving symptoms and may include medications, lifestyle modifications, and preventive therapies. By understanding their triggers and making appropriate lifestyle changes, individuals with basilar migraines can effectively manage their condition and reduce both the frequency and severity of their migraines.
It is crucial for people experiencing basilar migraines to work closely with their healthcare providers in order to develop a personalized treatment plan that suits their specific needs. By staying informed, seeking appropriate medical guidance, and adopting necessary lifestyle modifications, individuals can improve their quality of life and find relief from the symptoms of basilar migraines.
FAQ
What is a basilar migraine?
A basilar migraine, also known as migraine with brainstem aura, is a rare type of migraine that starts in the brainstem. It is characterized by aura symptoms that occur before or during the migraine episode.
What are the symptoms of a basilar migraine?
Symptoms of a basilar migraine can include changes in speech, hearing, and vision, as well as vertigo, tinnitus, double vision, impaired muscle control, and a reduced level of consciousness.
What causes basilar migraines?
The exact cause of basilar migraines is unknown, but it is believed to have a genetic and environmental component. Trigger factors such as stress, lack of sleep, certain foods, hormonal changes, and environmental stimuli can contribute to the occurrence of basilar migraines.
How are basilar migraines diagnosed?
The diagnosis of basilar migraine is based on specific criteria outlined by the International Classification of Headache Disorders. Imaging studies such as MRI or CT scans may be ordered to rule out other conditions, and an EEG may be necessary to rule out seizures.
What are the treatment options for basilar migraines?
Treatment options for basilar migraines include medications such as NSAIDs and anti-emetics to alleviate pain and nausea. Preventive therapy may be recommended for frequent and disabling migraines, and lifestyle modifications such as trigger avoidance and stress management can also help prevent migraine attacks.
How can basilar migraines be differentiated from other conditions?
Basilar migraines can mimic other conditions such as hemiplegic migraines, Meniere’s disease, vestibular disorders, transient ischemic attacks (TIAs), strokes, brainstem AV malformations, tumors, and meningitis. A thorough evaluation, including a physical examination and appropriate imaging and testing, is necessary to differentiate basilar migraines from other potential causes of similar symptoms.
Are basilar migraines more severe than other types of migraines?
Basilar migraines can be more disabling than migraines without aura or migraines with typical aura due to the increased severity and longer duration of symptoms. However, the frequency of basilar migraines tends to decrease with age, and they often evolve into more typical patterns.
Can basilar migraines be prevented?
Basilar migraines can be triggered by various factors, including stress, alcohol, caffeine, hormonal changes, lack of sleep, strong smells, and certain foods. Identifying and avoiding these triggers, along with lifestyle modifications such as maintaining a balanced diet, regular exercise, and stress management, can help prevent migraine attacks.
What lifestyle modifications can help manage basilar migraines?
In addition to trigger avoidance, maintaining a balanced diet, avoiding drugs and alcohol, not skipping meals, limiting caffeine intake, and avoiding specific trigger foods like dairy, wheat, chocolate, and citrus fruits can all contribute to preventing migraine attacks. Regular exercise, relaxation techniques, acupuncture, massage, cognitive-behavioral therapy, and biofeedback techniques may also help reduce the frequency and severity of basilar migraines.
What is the prognosis for basilar migraines?
Basilar migraines can be disabling, but the frequency tends to decrease with age. While migraines with aura have a slightly higher risk of stroke compared to migraines without aura, the specific risk for basilar migraines is unclear. Risk factors like smoking and the use of estrogen contraceptives can further increase the risk of stroke, and risk factor modification should be reinforced.
Source Links
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




