Table of Contents
ToggleIntroduction: Understanding Meningitis and Its Treatment
Meningitis is a serious infection that causes inflammation of the meninges, the protective membranes covering the brain and spinal cord. It can be caused by bacteria, viruses, fungi, or parasites. While most cases are treated with medications, some severe cases require surgical intervention.
Key Takeaways:
- What is surgical management of meningitis and when is it needed?
- How is tuberculous (TB) meningitis treated surgically?
- What are the first steps in managing meningitis?
- What is the role of nurses in meningitis care?
Let’s explore when surgery becomes necessary and what procedures are used to treat meningitis complications.
What is Surgical Management of Meningitis?
Surgical management of meningitis involves surgical procedures to treat complications caused by the infection. While most cases of meningitis are treated with antibiotics or antiviral drugs, surgery may be required in severe cases, such as:
- Hydrocephalus (excess fluid in the brain)
- Brain abscess (pus-filled swelling in the brain)
- Spinal cord compression
- Severe sinus or ear infections spreading to the brain
How Does Surgery Help?
- Drains excess fluid (to relieve pressure on the brain)
- Removes abscesses or infected tissue
- Prevents permanent brain damage
Now, let’s look at the specific conditions that may require surgery.
When is Surgery Needed for Meningitis?
Surgery is only recommended when meningitis leads to serious complications that cannot be controlled with medications alone.
1. Hydrocephalus (Excess Fluid in the Brain)

Meningitis can block the normal flow of cerebrospinal fluid (CSF), causing fluid buildup in the brain. This leads to dangerous brain pressure, headaches, and confusion.
Surgical Treatment:
Ventriculoperitoneal (VP) Shunt – A small tube is inserted to drain excess fluid from the brain into the abdomen.
2. Brain Abscess (Pus in the Brain)
A brain abscess occurs when pus collects inside the brain, leading to severe infections and swelling. This can cause seizures, headaches, and confusion.
Surgical Treatment:
Craniotomy & Abscess Drainage – A part of the skull is temporarily removed, and the abscess is drained to prevent further infection.
3. Spinal Cord Compression (Due to Epidural Abscess)

In some cases, meningitis causes pus or swelling around the spinal cord, leading to severe pain and paralysis.
Surgical Treatment:
Laminectomy & Abscess Drainage – A small section of the vertebra is removed to relieve pressure and allow the pus to drain.
4. Severe Skull or Sinus Infections

Bacterial meningitis can sometimes spread from ear or sinus infections, damaging nearby bones.
Surgical Treatment:
Debridement Surgery – The infected bone or tissue is removed to stop the infection from spreading further.
What is the Surgical Management of TB Meningitis?
Tuberculous (TB) meningitis is a severe form of meningitis caused by tuberculosis bacteria. It can cause brain swelling, hydrocephalus, and tissue damage.
Surgical Procedures for TB Meningitis:
- VP Shunt Surgery – To relieve fluid buildup in the brain.
- Craniotomy – To drain abscesses and reduce pressure.
- Meningeal Biopsy – A sample is taken from the meninges to confirm TB meningitis if diagnosis is unclear.
What is the First Step in Managing Meningitis?
The first and most critical step in meningitis management is early diagnosis and immediate treatment.
Key Early Actions:
- Hospitalization – Immediate medical care is needed.
- Lumbar Puncture (Spinal Tap) – A test to confirm meningitis by analyzing cerebrospinal fluid.
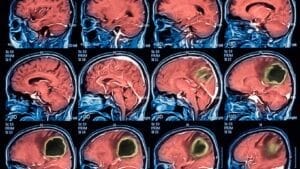
- Blood Tests & Brain Imaging (MRI/CT Scan) – To check for infection severity.
- Empirical Antibiotics – Doctors start treatment immediately, even before confirming bacterial type.
Early treatment saves lives! Delays can lead to severe brain damage or death.
What is the Early Management of Meningitis?
Once diagnosed, meningitis treatment focuses on controlling the infection and preventing complications.
- IV Antibiotics (for bacterial meningitis) – To kill the infection.
- Steroids – To reduce inflammation and brain swelling.
- Oxygen Therapy – Helps breathing in critical cases.
- Pain Management – Controls headaches and discomfort.
If complications like brain abscesses develop, surgical intervention is required.
What is the Management of Surgical Infections in Meningitis?
If surgery is needed, post-operative infection control is essential.
Key Steps:
- Sterile Surgical Techniques – To avoid spreading infection.
- Post-Surgical Antibiotics – To kill remaining bacteria.
- Regular CSF Monitoring – To check for new infections.
- Proper Wound Care – Prevents post-surgical complications.
What is the Role of Nurses in Meningitis Management?
Nurses play a vital role in meningitis care, ensuring early detection and patient recovery.
Key Nursing Responsibilities:
- Monitor Neurological Status – Check for seizures, consciousness, and brain swelling.
- Control Fever & Pain – Medications help manage symptoms.
- Prevent Infection Spread – Proper hygiene and isolation if needed.
- Educate Patients & Families – About treatment, recovery, and prevention.
What Are 5 Symptoms of Meningitis?
- Severe Headache – Constant and worsening.
- High Fever & Chills – Especially in bacterial meningitis.
- Stiff Neck – A classic meningitis symptom.
- Sensitivity to Light – Bright light causes discomfort.
- Seizures or Loss of Consciousness – Occurs in severe cases.
Seek medical help immediately if you notice these symptoms!
Final Thoughts: When is Surgery Needed for Meningitis?
Meningitis is a medical emergency that requires quick action. While most cases can be treated with medications, surgery is necessary in cases of:
- Brain abscesses
- Hydrocephalus (fluid buildup in the brain)
- Spinal cord compression
Early detection and timely treatment are critical! If you suspect meningitis, see a doctor immediately.
Looking for expert medical advice? Stay informed with the latest updates in neurology and infectious disease management!
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




