Guillain-Barré syndrome or GBS is a rare disorder linked with infections. It happens when the immune system reacts too much and attacks its own self. There are types of GBS that need to be understood for its treatment. It can weaken or paralyze the body, making it hard to breathe.
GBS is usually caused after an infection, either bacterial or viral. It’s important to know the 4 types of Guillain-Barre syndrome. This knowledge helps doctors give the right care. This leads to the best chances for a patient’s recovery.
Table of Contents
ToggleIntroduction to Guillain-Barré Syndrome (GBS)
Guillain-Barré Syndrome: An Overview
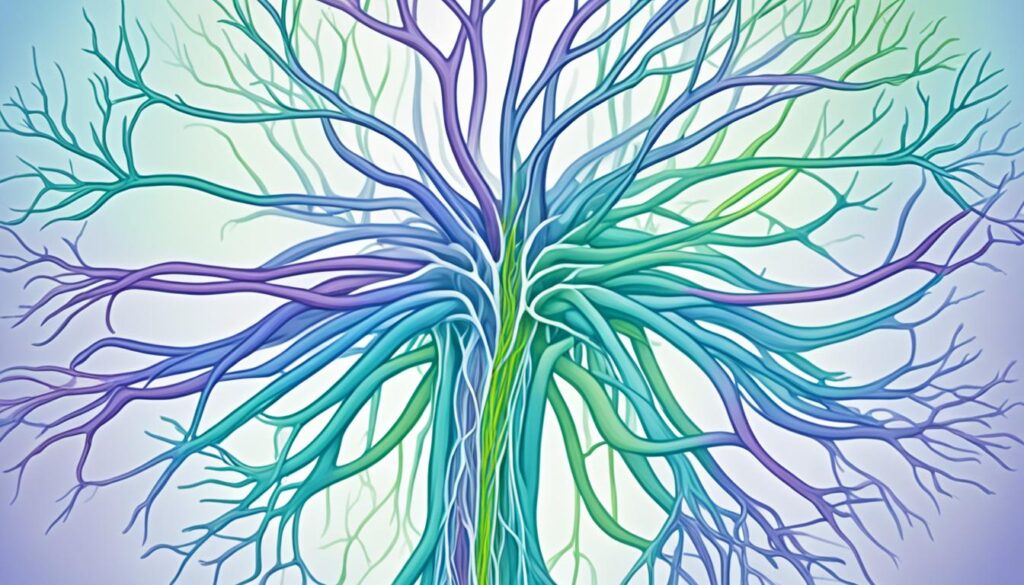
Guillain-Barré syndrome (GBS) is a rare disorder. It affects the peripheral nerves. These nerves help the brain, skin, and muscles talk to each other. The immune system mistakenly attacks these nerves. This causes inflammation and damage.
GBS and the Peripheral Nervous System
The peripheral nervous system is a network of nerves. It goes from the brain and spinal cord to the body. In GBS, the immune system damages these nerves. This disruption causes problems in sending signals. As a result, people may feel weak, tingle, or even become paralyzed.
Acute Inflammatory Demyelinating Polyneuropathy (AIDP)
AIDP is the main Guillain-Barré Syndrome (GBS) type in America. It damages the myelin sheaths on nerves. People with AIDP suddenly feel weak on both sides of their body. This weak feeling starts in the toes and moves up. They might also have trouble moving their face, speaking, or swallowing. Their reflexes can be low or not work at all.
Symptoms of AIDP
The main signs of AIDP are quick muscle weakness or not being able to move. This usually starts in the legs and goes up. The person might feel numb, tingly, or in pain in their arms or legs. They could find it hard to move their face, speak, or swallow. Their reflexes might be weak too.
Progression of AIDP
AIDP gets worse fast, with the strongest signs in the first two to four weeks. Someone might lose muscle strength very quickly. This might lead to not being able to move at all in severe cases. How fast it gets worse can change. Getting diagnosed and treated early is very important.
AIDP and Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
AIDP is a fast-moving GBS type. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is another kind but it gets worse over time. In CIDP, there’s almost always some loss of myelin. It can take months to get very bad. Jumping on diagnosis and treatment is key to stop disability and get better in both AIDP and CIDP people.

Acute Motor and Sensory Axonal Neuropathy (AMSAN)
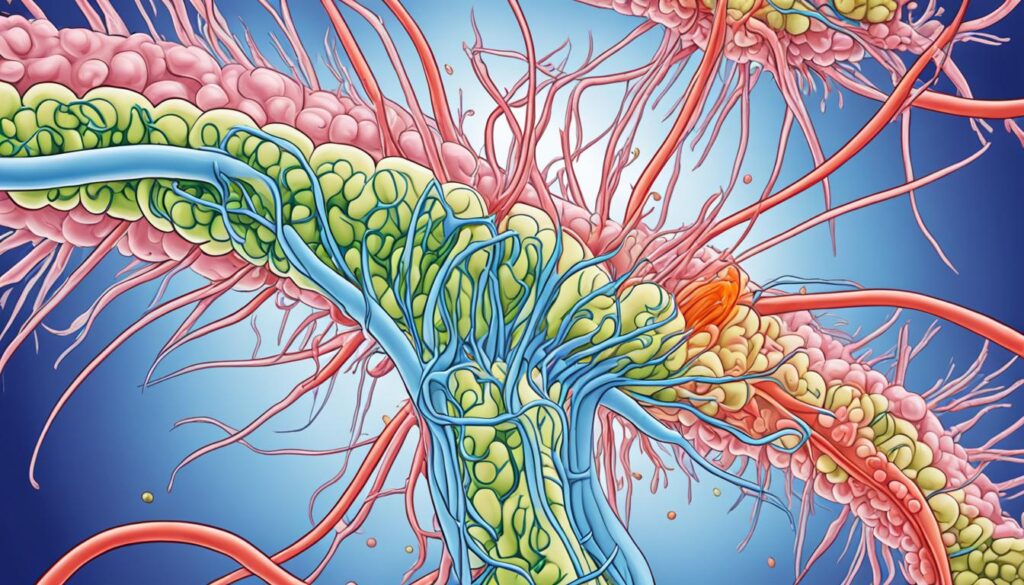
Acute Motor and Sensory Axonal Neuropathy (AMSAN) is a rare, severe type of Guillain-Barré syndrome (GBS). It affects the axons, or the nerves’ message-carrying parts for both movement and sensation. Unlike other GBS forms, AMSAN targets both sensory and motor fibers’ axonal degeneration.
Distinguishing Features of AMSAN
AMSAN shows in numbness and tingling in feet and hands, leading to limb weakness and walking difficulty within 10 days. Such a quick start and progression are typical for AMSAN. It can also affect automatic processes, like breathing, putting lives at risk.
Recovery from AMSAN
Healing from AMSAN is slow due to the needed axonal damage repair and regeneration. Patients might need a long time on mechanical ventilation and tracheostomy, along with extended care for nerve and muscle issues. With correct support and therapy, most regain some functionality. Yet, the path to recovery is long and tough, unlike other GBS types.
Acute Motor Axonal Neuropathy (AMAN)
Acute Motor Axonal Neuropathy (AMAN) is a rare type of Guillain-Barré syndrome (GBS). It mainly affects the motor nerves for movement. This form makes up 5-10% of GBS cases in the U.S.
Campylobacter jejuni and AMAN
Campylobacter jejuni bacteria plays a big role in AMAN’s development. If someone gets infected with it, their body may react in a harmful way. This can cause problems and even harm the motor nerves. Studies have shown that Campylobacter jejuni is linked to some AMAN cases.
| GBS Variant | Percentage of Cases in the U.S. |
|---|---|
| Acute Inflammatory Demyelinating Polyneuropathy (AIDP) | 85-90% |
| Acute Motor Axonal Neuropathy (AMAN) | 5-10% |
| Acute Motor Sensory Axonal Neuropathy (AMSAN) | Rare |
Miller-Fisher Syndrome (MFS)
Miller-Fisher Syndrome (MFS) is very rare. It’s a kind of Guillain-Barré Syndrome (GBS) that affects the nerves in your head. People with MFS have three main symptoms: weak eye muscles, no reflexes, and unsteady movements.
Cranial Nerve Involvement in MFS
MFS especially affects the cranial nerves. This can cause many problems. For example, eye muscle weakness can make you see double or cause your eyelids to droop. You might also have a weak face, find it hard to swallow, or move unsteadily.
Prognosis of Miller-Fisher Syndrome
Most people with MFS get better in 8 to 12 weeks, often without special treatment. Only a few may have symptoms come back. These symptoms usually go away in about six months. In some cases, doctors might use special treatments like IVIg or plasmapheresis.
| Characteristic | Statistic |
|---|---|
| Worldwide incidence of MFS | 1 to 2 per 1,000,000 people |
| Gender ratio (male to female) | 2:1 |
| Mean age at onset | 43.6 years |
| Incidence in Asians | 15% to 25% of GBS cases |
| Incidence in Western populations | 5% of GBS cases |
| Preceding viral infection | 72% of MFS cases |
| Positive for anti-GQ1b antibodies | 70% to 90% of MFS patients |
| Classic triad presentation | 90% of MFS patients |
| Albuminocytologic dissociation | 90% of MFS patients |
4 types of guillain barre syndrome
Guillain-Barré syndrome (GBS) is a rare disorder that affects the nerves. It shows up in four main types:
- Acute Inflammatory Demyelinating Polyneuropathy (AIDP): This is the most seen type in the U.S. It damages the myelin sheaths that cover nerves.
- Acute Motor and Sensory Axonal Neuropathy (AMSAN): A rare, severe form that mainly harms the axons. Axons are nerves that help us move and feel.
- Acute Motor Axonal Neuropathy (AMAN): This type only affects nerves that control movement. It makes up 5-10% of cases.
- Miller-Fisher Syndrome (MFS): A very rare kind that mostly affects facial nerves. It leads to issues with moving and eating, and weakens the face.
Each type of GBS has its own symptoms and ways of progressing. Knowing these differences helps healthcare providers treat GBS better.
| GBS Subtype | Prevalence | Key Features | Recovery Timeline |
|---|---|---|---|
| AIDP | Most seen in the U.S. | Hurts myelin sheaths of nerves | Most people walk again within 6 months |
| AMSAN | Rare, severe | Targets axons of nerves for movement and sensation | Recovery can be a year or more |
| AMAN | 5-10% of cases | Only affects nerves controlling movement | – |
| MFS | Very rare, affects 1-2 per million in the U.S. | Affects facial nerves, leading to problems with movement and coordination | – |
Diagnosis and Treatment Approaches
Doctors use your medical past, a checkup, and special tests to find out if you have Guillain-Barré syndrome. These tests show the kind of GBS and tell if it’s something else.
Electrodiagnostic Testing for GBS
Tests like nerve conduction studies and electromyography are key in figuring out Guillain-Barré syndrome. They look at the nerves’ electric activity to see the damage. This info helps doctors choose the right way to treat you.
Treatment Options for GBS
The main goals of treating Guillain-Barré syndrome are to ease symptoms and support recovery. Treatments include IVIG and plasma exchange to help your immune system and lower nerve inflammation. Sometimes, you might need help breathing with a machine. Fortunately, most people can walk on their own after six months. And around 60% get back full muscle strength a year later.
FAQ
What is Guillain-Barré syndrome (GBS)?
Guillain-Barré syndrome (GBS) is a rare nerve disorder. It can happen after someone gets sick. The body’s immune system acts too much. This can make arms and legs weak. In bad cases, it can even make breathing hard.
What are the different types of Guillain-Barré syndrome?
There are four types of Guillain-Barré syndrome:
– Acute Inflammatory Demyelinating Polyneuropathy (AIDP)
– Acute Motor and Sensory Axonal Neuropathy (AMSAN)
– Acute Motor Axonal Neuropathy (AMAN)
– Miller-Fisher Syndrome (MFS)
What are the symptoms of Acute Inflammatory Demyelinating Polyneuropathy (AIDP)?
With AIDP, you might suddenly feel weak on both body sides. This weakness usually starts in the toes and moves up. You might also face weak facial muscles, have trouble speaking or swallowing, and show reduced reflexes.
How is Acute Motor and Sensory Axonal Neuropathy (AMSAN) different from other types of GBS?
AMSAN is rare and serious. It mainly affects the nerves’ axons that control feeling and motion. Symptoms start with tingling in hands and feet. This can become limb weakness and trouble walking over 10 days. Breathing problems may also arise.
What causes Acute Motor Axonal Neuropathy (AMAN)?
Sometimes, AMAN happens because of Campylobacter jejuni. This bacteria causes a few AMAN cases. It’s a rare GBS type that only affects nerves for movement.
How does Miller-Fisher Syndrome (MFS) differ from other GBS variants?
MFS is very rare and targets the head’s nerves. It starts with eye muscle weakness. Symptoms may grow to include movement problems, weak face muscles, and trouble swallowing.
How is Guillain-Barré syndrome diagnosed?
Doctors find GBS through a person’s health story, checkup, and special tests. Tests like nerve studies and muscle checks help to diagnose GBS. They also exclude other illnesses.
What are the treatment options for Guillain-Barré syndrome?
GBS can be treated with drugs that calm the immune system. Treatments like IVIG or plasma exchange help. In tough cases, a person might need help breathing.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939842/
- https://medlineplus.gov/genetics/condition/guillain-barre-syndrome/
- https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/symptoms-causes/syc-20362793
- https://www.ncbi.nlm.nih.gov/books/NBK532254/
- https://www.verywellhealth.com/introduction-to-guillain-barre-syndrome-2488658
- https://www.uofmhealth.org/conditions-treatments/brain-neurological-conditions/guillain-barre-syndrome-GBS-and-chronic-inflammatory-demyelinating-polyneuropathy-CIDP
- https://emedicine.medscape.com/article/1169959-overview
- https://www.medicalnewstoday.com/articles/types-of-guillain-barre-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7189311/
- https://www.ncbi.nlm.nih.gov/books/NBK507717/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7676442/
- https://rarediseases.org/rare-diseases/miller-fisher-syndrome/
- https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/diagnosis-treatment/drc-20363006
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6821638/
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




