Complex regional pain syndrome (CRPS) is a neuropathic pain disorder that affects individuals worldwide. To fully comprehend this condition, it’s essential to understand its critical stages.
CRPS progresses through distinct stages, each associated with unique clinical features. These stages include the acute stage, the dystrophic stage, and the atrophic stage. Each stage presents with specific symptoms and challenges, requiring tailored treatment approaches.
In this article, I will explain these stages in-depth, shedding light on the complexities of CRPS and providing insights into its diagnosis and treatment.
Table of Contents
ToggleWhat is Complex Regional Pain Syndrome?
Complex regional pain syndrome (CRPS) is a rare neuropathic pain disorder characterized by ongoing pain that is disproportionate to the initial injury. It is accompanied by sensory, motor, and autonomic abnormalities. The pain in CRPS is often described as burning or electrical shocks. Other clinical features include:
- Allodynia (pain due to stimuli that should not be painful).
- Hyperalgesia (increased pain sensitivity).
- Sudomotor and vasomotor abnormalities.
- Trophic changes (changes in skin, hair, and nails).
CRPS can affect any body part but most commonly affects the arms, legs, hands, or feet.
| CRPS Characteristics | Descriptions |
|---|---|
| Pain | Ongoing pain disproportionate to the initial injury |
| Allodynia | Pain due to stimuli that should not be painful |
| Hyperalgesia | Increased pain sensitivity |
| Sudomotor and Vasomotor Abnormalities | Changes in sweating and blood flow |
| Trophic Changes | Changes in skin, hair, and nails |
Key Stages of CRPS
Complex regional pain syndrome (CRPS) progresses through three main stages: the acute stage, the dystrophic stage, and the atrophic stage. Distinct symptoms and changes in the affected area characterize each stage.
1. Acute Stage
In the acute stage of CRPS, which typically lasts for a few weeks, individuals experience severe pain, inflammation, and hypersensitivity to touch. The affected area may appear red, swollen, and warm. The pain can be intense and may spread beyond the initial injury site. During this stage, seeking medical attention for appropriate management and treatment is essential.
2. Dystrophic Stage
The dystrophic stage of CRPS can last for several months. During this stage, changes in the affected area become more apparent. The skin may take on a mottled appearance, with red, purple, or blue discoloration patches. The area’s temperature may fluctuate, making the skin dry and thin. Stiffness and limited range of motion in the joints may also be present. Physical therapy and other interventions to improve circulation and joint mobility are often recommended during this stage.
3. Atrophic Stage
Long-term changes in the affected area typically characterize the atrophic stage of CRPS. It can last for years and is marked by muscle atrophy, contractures (tightening of the muscles and tendons), and irreversible changes in the skin and bones. The affected area may become thinner, and the bones may become more brittle. The pain may persist but might not be as severe as in the earlier stages. Management strategies during this stage focus on pain relief, maintaining mobility, and preventing further complications.
| CRPS Stage | Main Features | Duration |
|---|---|---|
| Acute Stage | Severe pain, inflammation, hypersensitivity | A few weeks |
| Dystrophic Stage | Changes in skin color, temperature, texture; joint stiffness | Several months |
| Atrophic Stage | Muscle atrophy, contractures; irreversible skin and bone changes | Years |
Causes and Risk Factors of CRPS
Complex regional pain syndrome (CRPS) can have various causes and risk factors contributing to its development. While the exact cause of CRPS is unknown, it often occurs following an injury, trauma, or surgical procedure. Additionally, CRPS can also manifest spontaneously without any apparent trigger.
CRPS is believed to involve a complex interplay between the immune system, nervous system, and genetic factors. The immune system’s response to an injury or trauma may contribute to the development and progression of CRPS. Abnormalities in the nervous system, including heightened sensitivity to pain and changes in nerve signaling, are also thought to play a role.
Various risk factors increase the likelihood of developing CRPS. Individuals with a history of trauma, such as fractures or sprains, are more susceptible to developing the condition. Similarly, those who have undergone surgery, particularly orthopedic procedures, are at an increased risk. Prolonged immobilization, such as cast or prolonged bed rest, can also contribute to the onset of CRPS.
Psychological factors, such as anxiety and depression, can influence the development and progression of CRPS. Stress and emotional distress may exacerbate symptoms or make them more challenging to manage. Additionally, individuals with certain medical conditions like fibromyalgia and migraines may have a higher risk of developing CRPS.
To summarize, the causes of CRPS are multifactorial and involve a combination of trauma, surgery, immune and nervous system abnormalities, and genetic factors. Understanding these causes and risk factors is essential in identifying individuals more susceptible to developing CRPS and implementing preventive measures.
Risk Factors for CRPS:
- History of trauma, fractures, or sprains
- Prior surgical procedures
- Prolonged immobilization
- Psychological factors, such as anxiety or depression
- Medical conditions like fibromyalgia and migraines
| Causes | Risk Factors |
|---|---|
| Trauma | History of trauma, fractures, or sprains |
| Surgery | Prior surgical procedures |
| Immobilization | Prolonged immobilization |
| Psychological Factors | Psychological factors, such as anxiety or depression |
| Medical Conditions | Medical conditions like fibromyalgia and migraines |
Diagnosis of CRPS
Diagnosing complex regional pain syndrome (CRPS) involves comprehensively evaluating clinical signs, symptoms, and diagnostic criteria. Clinicians commonly use the Budapest Criteria to guide the complex regional pain syndrome diagnosis. These criteria include:
- Continuing pain that is disproportionate to the initial injury
- Sensory changes such as allodynia (pain due to non-painful stimuli) and hyperalgesia (increased pain sensitivity)
- Vasomotor changes like temperature asymmetry and skin color changes
- Sudomotor/edema changes such as excessive sweating and edema
- Motor/trophic changes like decreased range of motion and trophic skin changes
A thorough clinical examination is essential in the diagnosis of CRPS. The examination may include:
- Assessing pain levels.
- Evaluating sensory abnormalities.
- Measuring skin temperature and color.
- Assessing motor function and trophic changes in the affected limb.
While clinical evaluation is crucial, specific diagnostic tests may be used to support the diagnosis of CRPS and rule out other conditions. These tests may include:
- Blood tests to rule out underlying medical conditions
- Thermography to evaluate temperature changes in the affected area
- Nerve conduction studies to assess nerve function
- Imaging tests such as X-rays, MRI, or bone scans to detect any structural abnormalities
These diagnostic tests help provide a comprehensive understanding of the condition and assist in formulating an appropriate treatment plan.

Treatment Options for CRPS
A multi-modal approach is often necessary when treating complex regional pain syndrome (CRPS). The treatment plan is tailored to meet each patient’s specific needs and may include a combination of physical therapy, medication, nerve stimulation, and surgery.
Physical Therapy
Physical therapy is critical in managing CRPS, helping patients regain function, and alleviating pain. Physical therapists employ various techniques and exercises to improve blood flow, restore range of motion, and prevent muscle wasting. These exercises target the affected areas and help patients regain strength and mobility.
Medication
Medications are commonly prescribed to manage the pain and other symptoms associated with CRPS. Non-steroidal anti-inflammatory drugs (NSAIDs), anticonvulsants, and antidepressants may be used to alleviate pain, reduce inflammation, and improve mood. The specific medications prescribed will depend on the individual’s symptoms and needs.
Nerve Stimulation
Nerve stimulation techniques can provide significant pain relief for individuals with CRPS. Transcutaneous electrical nerve stimulation (TENS) involves applying electrical impulses to the affected area using adhesive electrodes. This technique helps to disrupt pain signals and promote circulation. Spinal cord stimulation is another option in which electrodes are placed near the spinal cord to control pain signals.
Surgery
In severe cases of CRPS, surgical interventions may be considered. Sympathectomy, a surgical procedure that involves cutting or blocking the nerves responsible for pain transmission, may be recommended to alleviate pain and improve function. Decompression surgery, which consists of relieving pressure on nerves or blood vessels, can also be an option to reduce pain.
Prognosis and Complications of CRPS
Managing complex regional pain syndrome (CRPS) can be challenging due to the varying prognosis and potential complications associated with the condition. The outlook for CRPS differs from person to person and is influenced by several factors, including the stage of the condition, response to treatment, and coexisting medical conditions.
Some individuals with CRPS may experience spontaneous remission or significant improvement over time, while others may face a chronic and debilitating course. It’s essential to understand that each individual’s journey with CRPS is unique.
Complications of CRPS:
- Chronic Pain: Ongoing and persistent pain is a hallmark symptom of CRPS. It can significantly impact a person’s quality of life and ability to engage in daily activities.
- Muscle Weakness and Atrophy: CRPS can lead to muscle weakness and wasting. Reduced muscle strength and loss of tone may affect mobility and overall physical function.
- Bone Loss: CRPS can cause bone demineralization, weakening bones, and increased risk of fractures.
- Skin Problems: Skin color, texture, and temperature changes are expected in CRPS. The affected area may appear blotchy, shiny, or thin and more susceptible to infections.
- Cardiovascular and Respiratory Issues: In rare cases, CRPS can affect the cardiovascular system, leading to complications such as increased heart rate, changes in blood pressure, or difficulty breathing.
- Psychological Distress: Living with chronic pain and the impact of CRPS on daily life can cause psychological distress, including anxiety, depression, and social isolation.
Individuals with CRPS must work closely with their healthcare team to manage symptoms, prevent complications, and improve overall well-being.

| Complication | Description |
|---|---|
| Chronic Pain | Ongoing and persistent pain that can significantly impact quality of life. |
| Muscle Weakness and Atrophy | Reduction in muscle strength and loss of muscle tone due to CRPS. |
| Bone Loss | Weakening of bones and increased risk of fractures. |
| Skin Problems | Changes in skin color, texture, and temperature, which may lead to skin infections. |
| Cardiovascular and Respiratory Issues | Potential complications affecting the cardiovascular system and respiratory function. |
| Psychological Distress | Anxiety, depression, and social isolation resulting from the impact of CRPS on daily life. |
Epidemiology of CRPS
Understanding the epidemiology of complex regional pain syndrome (CRPS) can provide valuable insights into the incidence, gender, age distribution, and regional distribution of this condition.
The incidence of CRPS varies across different studies and geographical locations. In the United States, the estimated incidence is around 5.5 cases per 100,000 person-years. This highlights the significance of CRPS as a relatively rare pain disorder.
When considering gender distribution, CRPS is more commonly diagnosed in females, with a female-to-male ratio of approximately 4:1. This gender disparity emphasizes the potential influence of biological and hormonal factors in the development of CRPS.
While CRPS can affect individuals of any age, it is most commonly seen in adults between 40 and 70. This age distribution indicates that CRPS is more prevalent among middle-aged and older adults.
CRPS follows a regional distribution and commonly affects the distal extremities, such as the hands and feet. However, it is essential to note that CRPS can also involve other parts of the body.
| CRPS Incidence | Gender Distribution | Age Distribution | Regional Distribution |
|---|---|---|---|
| Varies across studies and locations | More common in females (4:1 ratio) | Most commonly seen in adults aged 40-70 | Affects distal extremities, can involve other body parts |
Pathophysiology of CRPS
The exact pathophysiology of complex regional pain syndrome (CRPS) has yet to be fully understood. However, it is believed to involve inflammatory changes, neural sensitization, and genetic factors.
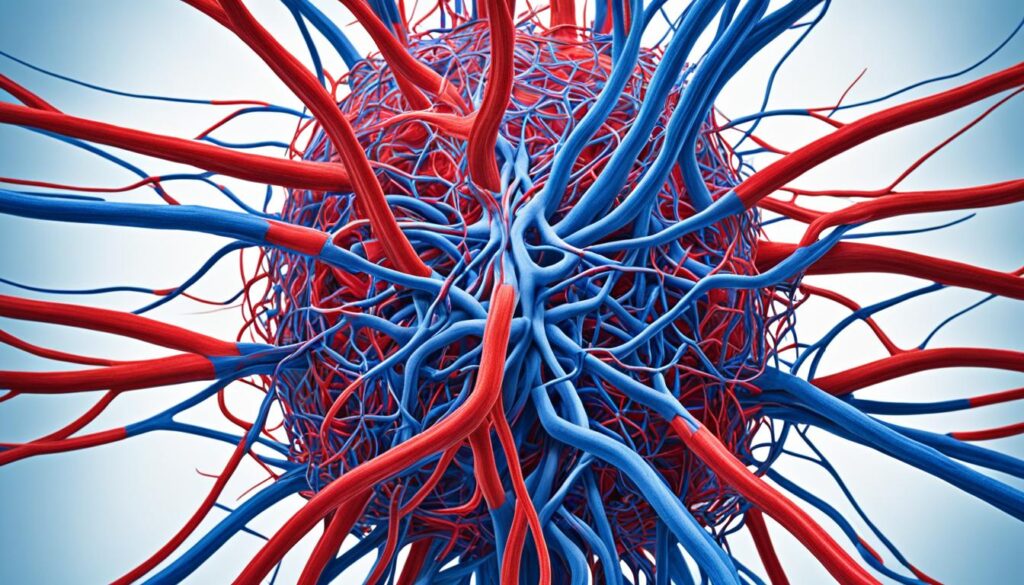
Inflammation plays a crucial role in CRPS, with elevated levels of pro-inflammatory cytokines and neuropeptides found in affected individuals. These inflammatory changes contribute to the pain and other symptoms experienced in CRPS.
Additionally, the peripheral and central nervous systems undergo significant changes in CRPS. Neural sensitization is a process in which the nerves become more responsive to pain signals, increase pain sensitivity, and develop symptoms such as allodynia and hyperalgesia.
Abnormalities in the sympathetic nervous system, which controls involuntary functions such as blood flow, also play a role in CRPS. Dysregulation of sympathetic activity further contributes to the pain, temperature abnormalities, and skin changes observed in CRPS.
Furthermore, genetic factors may influence an individual’s susceptibility to developing CRPS and the severity of the condition. Research suggests that certain genetic variations may predispose some individuals to CRPS or affect their response to treatment.
Inflammatory Changes in CRPS
| Inflammatory Changes | Effects |
|---|---|
| Elevated levels of pro-inflammatory cytokines | Contribute to inflammation and pain |
| Increased neuropeptide release | Amplify pain signals |
| Leukocyte infiltration | Trigger immune response and further inflammation |
Understanding the underlying pathophysiological mechanisms of CRPS is essential for developing targeted therapies to alleviate pain, reduce inflammation, and improve overall outcomes for individuals living with this complex condition.
Prevention and Management Strategies for CRPS
While there is no surefire way to prevent complex regional pain syndrome (CRPS), early intervention and appropriate management can significantly improve outcomes. CRPS can be a debilitating condition, but taking proactive measures can help individuals effectively manage their symptoms and regain control of their lives.
Preventive Measures
Although preventing CRPS altogether may not be possible, specific preventive measures can be taken to reduce the risk of its development. For instance, in the case of particular fractures, vitamin C may help promote proper healing and minimize the chances of CRPS occurrence. Additionally, avoiding tight dressings and prolonged immobilization can help prevent the condition from setting in.
Interdisciplinary Approach to Management
The management of CRPS requires a comprehensive and interdisciplinary approach involving a team of healthcare professionals with expertise in different areas. By collaborating and coordinating their efforts, these professionals can provide a holistic and personalized treatment plan tailored to the individual’s needs.
The interdisciplinary team may include:
- Neurologists
- Pain specialists
- Physical therapists
- Psychologists
- Occupational therapists
Each healthcare professional plays a unique role in managing CRPS. Neurologists and pain specialists can provide medical interventions, including medications, nerve blocks, and other pain management techniques. Physical therapists focus on physical rehabilitation, providing exercises to improve mobility, strengthen muscles, and enhance overall function. Psychologists can offer psychological support, helping individuals cope with the emotional impact of CRPS. Occupational therapists aid individuals in regaining independence and improving their ability to perform daily activities.
Treatment Strategies
Treatment strategies for CRPS aim to address pain relief, restore function, provide psychological support, and enhance overall quality of life. They may include:
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs), anticonvulsants, and antidepressants may be prescribed to manage pain and other symptoms associated with CRPS.
- Physical Therapy: Physical therapy is crucial in managing CRPS by improving blood flow, restoring range of motion, and preventing muscle wasting.
- Nerve Stimulation: Techniques such as transcutaneous electrical nerve stimulation (TENS) and spinal cord stimulation can relieve pain and help manage CRPS symptoms.
- Surgical Interventions: In severe cases of CRPS, surgical interventions like sympathectomy or decompression may be considered to alleviate pain and improve function.
It is essential to work closely with the healthcare team to determine the most appropriate treatment options based on individual needs and circumstances.
By following preventive measures, seeking early intervention, and embracing an interdisciplinary approach to management, individuals with CRPS can significantly improve their quality of life and regain control over their pain and symptoms. Although living with CRPS can be challenging, with the right strategies and support, it is possible to minimize the impact of the condition and thrive.
Conclusion
Living with complex regional pain syndrome (CRPS) can be challenging, but understanding the stages of this condition and the available treatment options is crucial for managing pain and improving quality of life. Early diagnosis and intervention play a vital role in preventing the progression of CRPS and minimizing its impact on daily life.
CRPS progresses through distinct stages, including the acute, dystrophic, and atrophic stages. Specific symptoms characterize each stage and require tailored approaches for treatment. Physical therapy, medication, nerve stimulation techniques, and surgery are commonly used to manage pain and improve function in individuals with CRPS.
Managing pain in CRPS requires a multidisciplinary approach involving various healthcare professionals, such as neurologists, pain specialists, physical therapists, and psychologists. The goal is to alleviate pain and restore mobility, enhance mental well-being, and support overall quality of life.
While there is still much to learn about CRPS, ongoing research is focused on understanding the underlying mechanisms of the condition and developing more effective treatments. By staying informed and working closely with healthcare providers, individuals with CRPS can take steps toward managing their pain and living a fulfilling life.
FAQ
What is complex regional pain syndrome (CRPS)?
Complex regional pain syndrome (CRPS) is a rare neuropathic pain disorder characterized by ongoing pain that is disproportionate to the initial injury. It is accompanied by sensory, motor, and autonomic abnormalities.
What are the critical stages of CRPS?
CRPS progresses through three main stages: the acute stage, the dystrophic stage, and the atrophic stage. Each stage is characterized by different symptoms and changes in the affected area.
What are the causes and risk factors of CRPS?
CRPS often develops after an injury, trauma, or surgery but can also occur spontaneously. Risk factors for developing CRPS include a history of trauma, fractures, surgery, prolonged immobilization, psychological factors, and certain medical conditions.
How is CRPS diagnosed?
The diagnosis of CRPS is primarily based on clinical evaluation and the presence of specific signs and symptoms. Diagnostic tests may be used to support the diagnosis and rule out other conditions.
What are the treatment options for CRPS?
The treatment of CRPS is multi-modal and individualized. It may include physical therapy, medication, nerve stimulation techniques, and surgery, depending on each patient’s specific needs.
What is the prognosis, and what complications can arise from CRPS?
The prognosis of CRPS varies widely. Some individuals may experience significant improvement, while others may have a chronic and debilitating course. Complications of CRPS can include chronic pain, muscle weakness and atrophy, bone loss, skin problems, and psychological distress.
What is the epidemiology of CRPS?
The incidence of CRPS varies across different studies and geographical locations. It is more commonly diagnosed in females and can affect individuals of any age, but it is most commonly seen in adults between 40 and 70.
What is the pathophysiology of CRPS?
The exact pathophysiology of CRPS is not fully understood, but it is believed to involve a combination of inflammatory changes, neural sensitization, and genetic factors.
Can CRPS be prevented, and how is it managed?
While there is no surefire way to prevent CRPS, early intervention and appropriate management can help improve outcomes. The management of CRPS requires a comprehensive and interdisciplinary approach involving multiple healthcare professionals.
What is the conclusion on CRPS?
Understanding the stages and treatment options for CRPS is essential for individuals with this condition and their healthcare providers. Early diagnosis and intervention and a personalized and interdisciplinary treatment approach can help manage pain, improve function, and enhance the quality of life for those living with CRPS.
Source Links

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | YouTube | Linkedin
Related Blog Posts
CRPS Treatment: Physical Therapy Solutions
May 23, 2024
Relief for CRPS: Sympathetic Nerve Block Info
April 16, 2024