Table of Contents
ToggleWhat is Amyotrophic Lateral Sclerosis (ALS)?
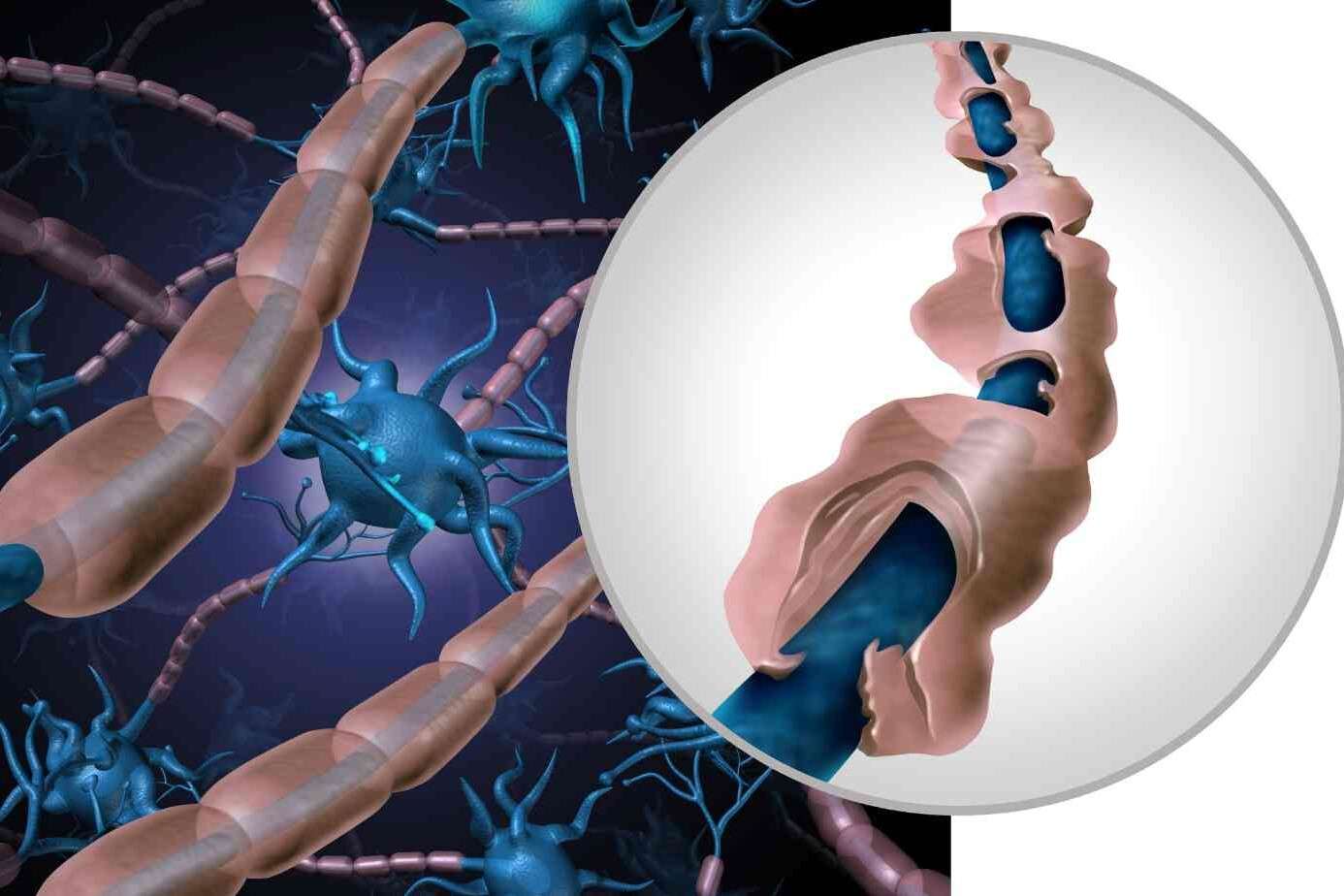
Amyotrophic Lateral Sclerosis, or ALS, is a disease of spinal cord motor cells. Here’s a closer look:
- A Nerve Disease: ALS is a condition that affects the nerves in our body, specifically the ones that control our muscles. Think of these nerves as tiny messengers that tell our muscles to move. It primarily affects the motor cells in the spinal cord.
- Muscle Weakness: People with ALS find it increasingly hard to move their arms legs, and even to talk or breathe. It’s like the messages to the muscles get lost.
- Progressive Condition: ALS gets worse over time. This means Amyotrophic Lateral Sclerosis Symptoms start mild but gradually become more severe.
- Not Very Common: ALS is a rare disease. It only happens to a few people, but understanding it is still essential.
- Two Types: There are two main types of ALS – sporadic (the most common, and it can happen to anyone) and familial (which is inherited and happens in families).
Named After a Baseball Player, It’s also known as Lou Gehrig’s disease, named after a famous baseball player with ALS.
In ALS, the nerve cells (neurons) that control muscles weaken and die. This means the muscles don’t receive the signals they need to move, leading to muscle weakness. It’s like having a remote control that slowly stops working.
Who Gets Amyotrophic Lateral Sclerosis ALS?
Understanding who can get Amyotrophic Lateral Sclerosis (ALS)
- Mainly Affects Adults: ALS is more common in adults, typically showing up between the ages of 40 and 70. The disease usually chooses to visit people in the middle or later part of their life journey.
- Slightly More Common in Men: While both men and women can get ALS, it’s a bit more common in men. Think of it like flipping a coin where heads (men getting ALS) come up just a few times more often than tails.
- Familial and Sporadic Types: Most cases are sporadic, which means they happen randomly without an apparent reason. A smaller number, about 5-10%, are familial, meaning the disease runs in the family.
- Geographic and Occupational Factors: Some studies suggest that where you live and your job might play a role, but this is like having only a few pieces of a big puzzle.
- We Don’t Know Why for Sure: The exact cause of ALS is still a mystery. Scientists believe it’s a mix of genetics and environmental factors.
What Happens in Amyotrophic Lateral Sclerosis ALS?
Let’s dive into what happens in the body when someone has Amyotrophic Lateral Sclerosis (ALS).

- Nerve Cells Break Down: In ALS, the nerve cells (neurons) in the brain and spinal cord that tell muscles to move start to weaken and eventually die. It’s as if the body’s internal telephone lines are getting disconnected.
- Muscles Get Weaker: As these nerves stop working, the muscles don’t receive the messages they need to move. Gradually, the muscles weaken, shrink, and become less able to do their job. Imagine a muscle is like a balloon slowly losing air.
- Different Symptoms for Everyone: Like everyone is unique, ALS affects people differently. One person might have trouble holding a pencil, while another might find speaking more challenging.
- Difficulty with Daily Tasks: As the muscles get weaker, simple things like walking, talking, eating, and even breathing can become challenging. The body’s muscles slowly forget how to do their everyday jobs.
- Affects Voluntary Muscles: ALS mainly impacts the muscles we can control, like those in our arms, legs, and face. This is different from involuntary muscles, which do things like keep our heart beating without us thinking about it.
Amyotrophic Lateral Sclerosis Symptoms
- Nerve Damage: ALS mainly happens because the nerves that control muscles start to weaken.
- Muscle Weakness: A common early sign. People might find it hard to:
- Use their hands and fingers, Like having trouble buttoning a shirt or writing.
- Moving arms and legs easily: Difficulty climbing stairs or lifting things.
- Muscles Get Smaller: The muscles might look smaller because they’re not used as much.
- Stiff Muscles and Overactive Reflexes: Muscles might feel tight, and reflexes, like the knee-jerk reaction, could be stronger.
- The trouble with Speaking and Swallowing: Speaking might become unclear, and swallowing food can be hard. Some people might drool more or find it hard to control their emotions.
- Muscle Twitching: Tiny, involuntary muscle movements, often in the arms or legs.
- Breathing Issues: It can become hard to breathe deeply, especially as ALS gets more advanced.
- Thinking and Behavior Changes: Some people might experience changes in thinking or acting.
- Feeling Tired: Tiredness can happen, even without much activity.
- Occasional Pain and Unusual Sensations: Some people might feel muscle cramps or a sort of pins-and-needles feeling, but it’s not very common.
How Neurologists Diagnose Amyotrophic Lateral Sclerosis ALS
Diagnosing Amyotrophic Lateral Sclerosis (ALS) is a complex process. Doctors have to look at lots of clues because there isn’t just a straightforward test for ALS. Here’s how they do it:
- Check Symptoms: First, doctors listen to the person’s symptoms – like muscle weakness, trouble speaking, or twitching.
- Physical Exam: They do a physical check to see how the muscles and reflexes work.
- Medical History: Doctors ask about the person’s health history and if anyone in their family has had similar problems.
- Muscle and Nerve Tests: Special tests, like EMG (electromyography), check how well the nerves and muscles work.
- Imaging Tests: Sometimes, they do MRI scans or blood tests to ensure the symptoms aren’t caused by something else.
- Rule Out Other Diseases: ALS can look like other diseases, so doctors check to ensure it’s not something else. It’s like making sure they have the right puzzle piece.
- Repeat Tests: Sometimes, doctors need to do tests more than once over time to see how symptoms are changing.
Amyotrophic Lateral Sclerosis Diagnosis takes time and careful checking. No single test can tell for sure, so doctors look at all the different information they gather to make a diagnosis. Be patient and trust your neurologist.
Living with Amyotrophic Lateral Sclerosis ALS
Living with Amyotrophic Lateral Sclerosis (ALS) is a big challenge, both for the person who has it and their family. Since there’s no cure for ALS right now, the focus is on making life as comfortable and fulfilling as possible. Here’s how people manage life with ALS

- Medications: Doctors may prescribe medicines. These can’t cure ALS, but they can slow it down a bit and help with some symptoms, like muscle cramps or stiffness.
- Physical Therapy: This is like a particular exercise with a therapist. It helps keep the muscles as strong as possible and makes moving around easier.
- Speech Therapy: If talking gets hard, speech therapists can help. They teach different communication methods, like using a computer or a particular board.
- Eating Changes: Dietitians can suggest softer foods or even special nutritional drinks if swallowing food becomes tough. It’s all about ensuring the person gets enough to eat without trouble.
- Breathing Support: Sometimes, people with ALS need help with breathing. Doctors might give them a machine to help get more air into their lungs.
- Home Modifications: Making changes at home, like ramps for wheelchairs or grab bars in the bathroom, can make daily life safer and more accessible.
- Support Groups: Talking with others who understand what it’s like can be helpful. Support groups offer a place to share tips and encouragement.
- Caregiver Support: Family members and caregivers also need support. It’s a tough job, and getting help, taking breaks, and looking after their health is super important.
How Can We Help Someone with ALS?
Helping someone with Amyotrophic Lateral Sclerosis (ALS) is about understanding, patience, and kindness. Here are some ways we can support and help make their life easier and more comfortable:
- Understanding and Patience: Understand that things they used to do easily might now be difficult or take longer. Be patient when they need more time to speak or move.
- Lend a Hand: Offer help with everyday tasks and let them do what they can by themselves. It’s about finding the right balance between helping and encouraging independence.
- Listening is Caring: Sometimes, being there to listen can mean a lot. Give them your full attention if they want to talk about their feelings or frustrations.
- Educate Yourself: Learn more about ALS. The more you know, the better you can understand what they’re going through.
- Make Their Space Comfortable: Adjust their living space so it’s safe and easy to get around. Moving furniture to create clear paths and adding grab bars in the bathroom can make a big difference.
- Join in Activities: Share activities they enjoy and can still participate in. It could be watching their favourite movie together or listening to music.
- Support with Communication: If they have trouble speaking, learn their communication methods, like alphabet boards or speech-generating devices.
- Plan for the Future: Talk about what they want regarding care and support as ALS progresses. It’s important to respect their wishes and make plans together.
- Take Care of Yourself: Supporting someone with ALS can be challenging. Make sure you also take time to rest and do things you enjoy. It’s like putting on your oxygen mask first before helping others.
Helping someone with ALS is about providing support, love, and understanding. It’s not just about physical help; it’s also about emotional support. Remember, your care and presence can make a big difference in their life.
FAQs
Can ALS be cured?
Currently, there is no cure for ALS. But doctors and scientists are working hard to find one.
Can ALS kill you?
Yes, ALS is a severe disease that eventually leads to death, often due to breathing problems.
Can ALS be prevented?
Right now, we don’t know how to prevent ALS because we don’t fully understand what causes it.
Can ALS symptoms come and go?
Generally, ALS symptoms don’t come and go. Once they start, they usually continue and often get worse over time.
Can ALS be hereditary?
In some cases, yes. About 5-10% of ALS cases are familial, which means they can be inherited from parents.
Can ALS go into remission?
No, ALS does not go into remission. Symptoms usually get steadily worse.
Can ALS be reversed?
Currently, there’s no way to reverse the damage caused by ALS.
How do ALS patients die?
Many people with ALS die from respiratory failure, which means their lungs stop working correctly.
How do ALS patients communicate?
They might use speech-generating devices, computer programs, or boards with letters or pictures to communicate.
How do ALS patients use the bathroom?
They might need help from others or use special equipment to help them use the bathroom as the disease progresses.
How is ALS diagnosed?
Doctors use a combination of physical exams, medical history, and tests like EMG (to check muscle activity) and MRI to diagnose ALS.
How does ALS affect the body?
ALS affects the nerves that control muscles, leading to muscle weakness, difficulty moving, speaking, swallowing, and eventually breathing.
Why does ALS happen?
We need to understand why fully. It might be a mix of genetic and environmental factors.
ALS and dementia:
Some people with ALS can also develop problems with thinking and memory, similar to dementia.
ALS and MS (Multiple Sclerosis):
Both affect the nervous system, but they are different diseases. MS affects the brain and spinal cord’s protective covering, while ALS affects nerve cells that control muscles.
ALS and COVID:
People with ALS may be more vulnerable to complications if they get COVID due to their weakened respiratory systems.
ALS and exercise:
Exercise can help maintain muscle strength and mobility in ALS, but it should be gentle and supervised by a healthcare professional.
ALS and co (companionship or cohabitation):
Support and companionship are essential for people with ALS, as the disease can be isolating.
ALS and Lyme disease:
Lyme disease can sometimes mimic ALS symptoms, but they are different conditions.
ALS and constipation:
Constipation can be a problem for people with ALS, often due to reduced mobility and changes in diet.
ALS compared to MS:
ALS primarily causes muscle weakening and loss, while MS can cause a broader range of symptoms, including vision problems and numbness.
ALS compared to Parkinson’s:
Parkinson’s mainly affects movement, causing tremors and stiffness. ALS leads to muscle weakening and loss.
How is MS different from ALS?
MS can be managed and sometimes goes into remission, which doesn’t happen with ALS. MS symptoms vary more and include problems with vision and balance.
Is ALS similar to MS?
They have similarities in affecting the nervous system, but their causes and progression differ.
ALS-like diseases:
There are other motor neuron diseases similar to ALS, like progressive bulbar palsy and primary lateral sclerosis.
Is ALS like Parkinson’s?
They both affect movement but in different ways. Parkinson’s usually starts with tremors, while ALS begins with muscle weakness.
Is ALS like Huntington’s disease?
Both are neurodegenerative, but Huntington’s disease also affects mental abilities and behaviour, which is less common in ALS.
ALS specialist near me:
Contact Dr. Chandril Chugh, American Trained Adult Neurologist.
ALS with dementia:
Some people with ALS can develop symptoms like dementia, affecting their thinking and memory.
ALS without weakness:
ALS almost always causes muscle weakness. If there’s no weakness, it might be a different condition.
ALS with normal EMG:
It’s rare, but some early cases of ALS might have a normal EMG (a test that checks muscle activity) initially.
ALS with bulbar onset:
Bulbar onset ALS means the symptoms start with speech and swallowing difficulties.
ALS with sensory symptoms:
ALS usually doesn’t cause sensory symptoms like numbness or tingling, which are more common in diseases like MS.
ALS with bulbar involvement:
This means ALS is affecting the muscles used for speaking and swallowing.
ALS with Parkinson’s:
It’s uncommon, but someone can have both ALS and Parkinson’s disease.
ALS without muscle weakness:
ALS always involves muscle weakness; if there’s no weakness, it’s likely not ALS.
ALS without fasciculations:
Muscle twitching (fasciculations) is common in ALS but might not be present in every case.
ALS without feeding tube:
Some people with ALS might not need a feeding tube, especially in earlier stages or if swallowing isn’t severely affected.
ALS without treatment:
Without treatment, ALS symptoms will progress. While there’s no cure, treatments can help manage symptoms and improve quality of life.
ALS without bulbar symptoms:
ALS can occur without initially affecting speech and swallowing (bulbar muscles).
ALS without upper motor neuron signs:
ALS usually involves both upper and lower motor neurons, but in some cases, the signs might be more subtle.
ALS without spasticity:
Spasticity (muscle stiffness) is common in ALS but not always present.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.