Table of Contents
ToggleWhat Is Subarachnoid Hemorrhage?
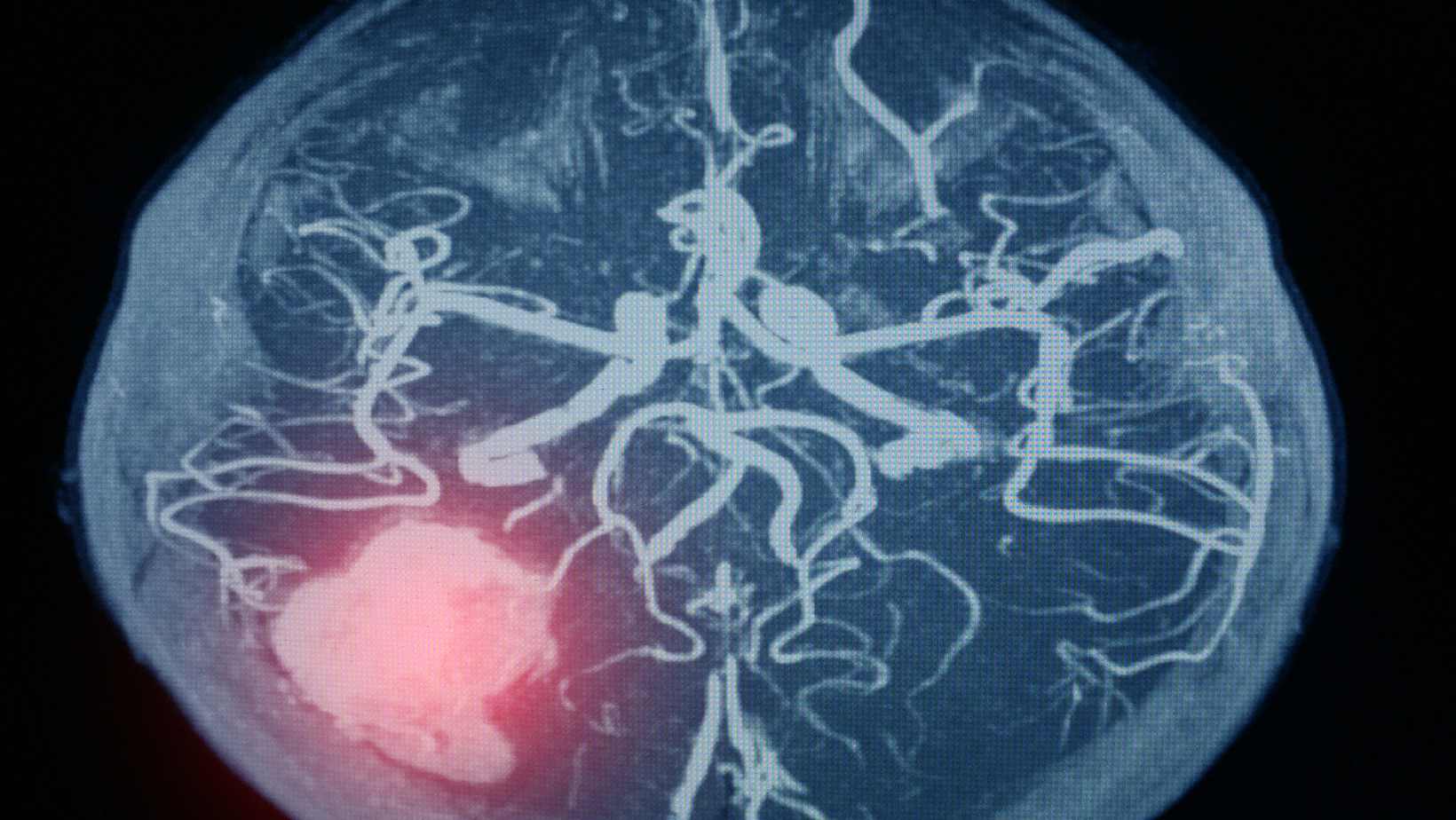
Subarachnoid hemorrhage (SAH) is a medical emergency that often results from a ruptured brain aneurysm. This critical condition involves bleeding into the space surrounding the brain, leading to severe complications, including death or long-term health issues. Understanding the treatment of a ruptured aneurysm is essential for improving outcomes and managing this life-threatening condition.
To learn more about what a brain aneurysm is, you can visit What is a Brain Aneurysm?.
Initial Steps in SAH Management
When a patient arrives at a healthcare facility with symptoms of SAH, the first priority is stabilizing their condition. This involves:
- Ensuring the patient can breathe: In severe cases, intubation and mechanical ventilation may be necessary.
- Stabilizing heart function: Maintaining stable heart function is crucial.
- Seizure management: Immediate treatment of seizures, if present, is essential.
Assessing the Severity of SAH
Healthcare professionals use specific grading systems to determine the severity of SAH. These systems assess the neurological impact and the extent of bleeding, guiding the approach to treatment.
Critical Care Management Strategies
The treatment of a ruptured aneurysm in a critical care setting involves several key strategies:
- Blood Pressure Control: Controlling blood pressure is vital to prevent further bleeding and ensure adequate blood flow to the brain.
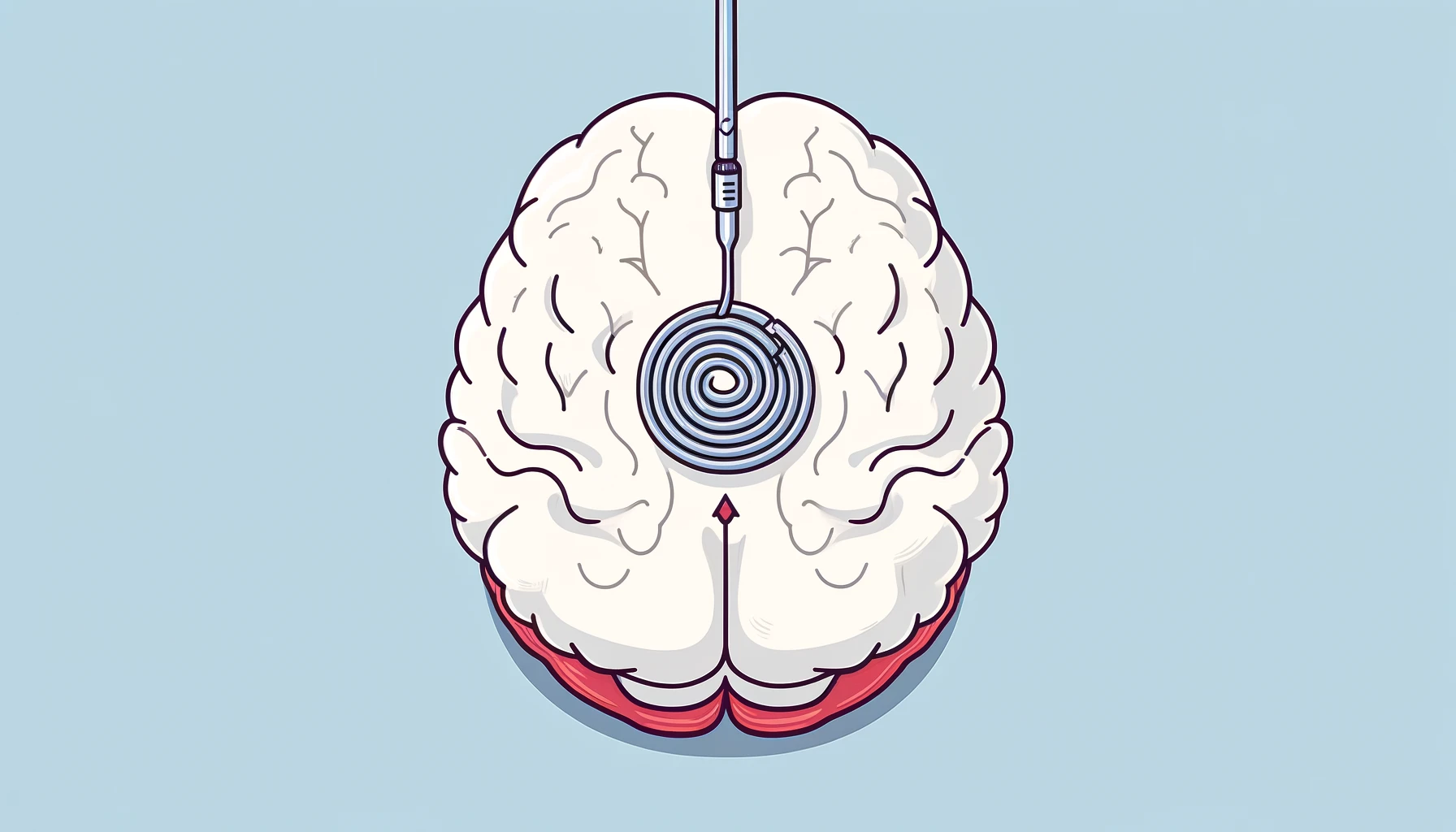
- Aneurysm Repair: The primary goal is to secure the aneurysm through surgical clipping or endovascular coiling to prevent rebleeding. To understand these methods in detail, visit Endovascular Aneurysm Repair Coiling VS Clipping.
- Monitoring and Prevention of Complications: Continuous monitoring for neurological changes is essential, as is the prevention of complications like vasospasm, a condition where blood vessels constrict, reducing blood flow to the brain.
- Fluid Management: Maintaining proper fluid and electrolyte balance is crucial to prevent dehydration and other complications.
- Medication: Medications such as Nimodipine are used to improve outcomes, even though their exact mechanism in SAH treatment is not fully understood.
- Pain Control: Effective pain management is crucial for patient comfort and recovery.
Treating the Aneurysm
The risk of rebleeding after an aneurysmal SAH is significant, making the treatment of a ruptured aneurysm an urgent priority. Ideally, the aneurysm should be repaired within the first 24 hours after admission. Two main approaches are used:
- Surgical Clipping: A small clamp is placed at the base of the aneurysm to isolate it from normal blood flow.
- Endovascular Coiling: This less invasive method involves inserting coils into the aneurysm to induce clotting and seal it off.
For more information on the various methods, you can read about Endovascular Aneurysm Repair Coiling VS Clipping.
In cases where immediate surgery is not possible, medications like tranexamic acid or aminocaproic acid may be used temporarily, but typically not for more than 72 hours.

Early Complications of SAH
Rebleeding
One of the most severe early complications is rebleeding, which can occur within the first 24 hours after the initial hemorrhage. Factors that increase the risk of rebleeding include:
- Delay in treating the aneurysm
- Poor neurological status upon admission
- Large aneurysm size
- High blood pressure
- Presence of blood within the brain or ventricles
- Incomplete obliteration of the aneurysm during treatment
Rebleeding often leads to worse outcomes and can be fatal.
Vasospasm and Delayed Cerebral Ischemia
Another significant complication is delayed cerebral ischemia, often resulting from vasospasm. This typically occurs between 4 and 14 days after the SAH. Managing vasospasm involves several strategies:
- Nimodipine: Used to reduce the risk of poor outcomes.
- Euvolemia Maintenance: Ensuring the right balance of body fluids.
- Hemodynamic Augmentation: Increasing blood pressure to improve blood flow to the brain.
- Balloon Angioplasty and Vasodilators: Used in severe cases to open narrowed blood vessels.
Managing Elevated Intracranial Pressure (ICP)
When bleeding increases pressure inside the skull, known as elevated intracranial pressure (ICP), it can be dangerous and requires prompt management:
- Draining Excess Fluid (CSF): Doctors may use an external ventricular drain (EVD) to remove fluid buildup in the brain.
- Medication to Reduce Fluid: Certain medications help draw out fluid from the brain.
- Surgery: In severe cases, part of the skull may be temporarily removed to relieve pressure.
- Long-Term Solutions: If the problem persists, a permanent drainage solution like a shunt might be necessary.

What Is Hydrocephalus?
Hydrocephalus, where fluid becomes trapped in the brain, can affect about 1 in 5 SAH patients. Treatment options include using drains or closely monitoring the patient to determine if surgery is needed.
The Salt and Water Balance: Managing Hyponatremia
Hyponatremia, a condition characterized by low sodium levels in the blood, is a common complication after a brain hemorrhage. Managing this condition involves restoring the salt-water balance, often with the help of salt solutions.
When Seizures Strike
Types Of Seizures can occur after SAH, especially if the bleeding was significant or if the aneurysm was located in certain areas of the brain. Doctors use carefully selected medications to prevent further seizures without worsening the patient’s condition.
Understanding the Impact of SAH: What Are the Long-Term Effects?
Early Challenges and Survival
- Immediate Risks: SAH can be life-threatening, with some patients not surviving long enough to receive hospital care.
- Early Hospital Mortality: The first few days in the hospital are critical, with complications like rebleeding, vasospasm, increased intracranial pressure, seizures, and heart issues posing significant risks.
Long-Term Outlook
Surviving SAH is just the first step. While survival rates have improved, SAH survivors often face a higher risk of health problems compared to the general population.
Dealing with Long-Term Effects
- Brain and Cognitive Challenges: Memory problems and difficulties with thinking and decision-making are common after SAH.
- Mood and Sleep: Depression, anxiety, and sleep problems can significantly affect the quality of life.
- Seizures and Epilepsy: A small number of survivors may develop epilepsy.
- Sense of Smell: Some patients may lose their sense of smell, especially after aneurysm surgery.
The Risk of Another Bleed
There’s a small chance of developing another aneurysm or experiencing a rebleed. Regular check-ups and monitoring are crucial. Learn more about Brain Aneurysms and related complications here.
Screening for Family Members
If you’ve had a SAH, your close family members might have a higher risk of experiencing it too. Doctors may suggest screening for them, especially if there’s a family history of brain aneurysms.
Final Thoughts
Dealing with SAH and its aftermath is a complex and challenging journey. However, with modern medical care, the chances of surviving and living a fulfilling life after SAH are better than ever. It’s important to stay hopeful, remain connected with your medical team, and understand that each person’s journey is unique. For more information on the treatment of a ruptured aneurysm, please visit What is a Brain Aneurysm?.

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | YouTube | Linkedin
Related Blog Posts
Aneurysmal Subarachnoid Hemorrhage (SAH)
May 31, 2024
What is a Brain Aneurysm?
April 3, 2024