Table of Contents
ToggleHow to take care of someone with Amyotrophic Lateral Sclerosis?
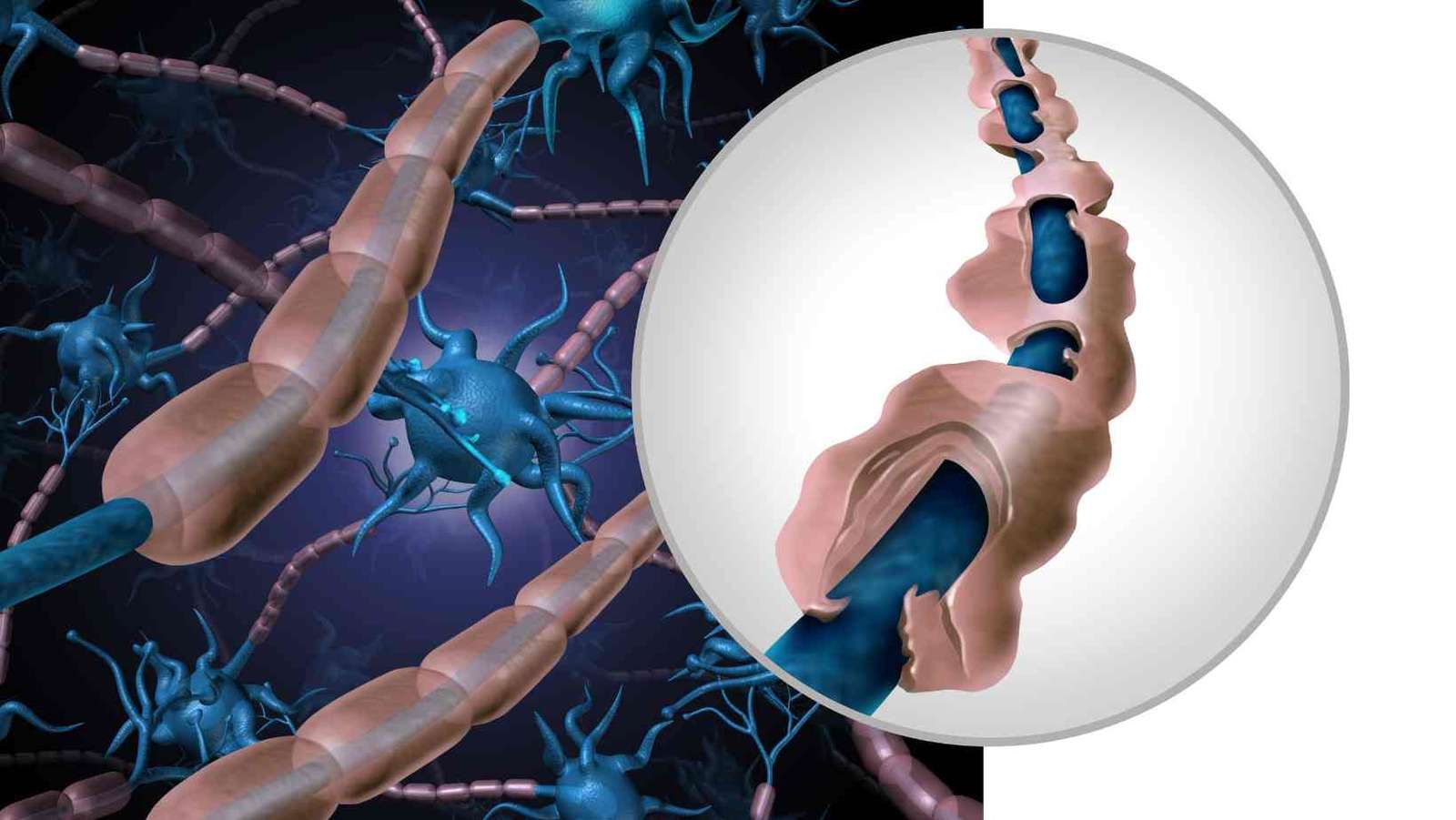
Today, we’re going to talk about a condition called ALS, or Amyotrophic Lateral Sclerosis. ALS is a disease that affects the nerves in our body that help us move our muscles. Imagine the nerves as electric wires and muscles as light bulbs. When the wires don’t work well, the light bulbs don’t light up. That’s kind of what happens in ALS.
What is ALS?
- Amyotrophic Lateral Sclerosis ALS is a disease that makes it hard for people to move their muscles.
- It mostly affects adults, but it’s very rare in kids.
- Neuroscientists are trying to understand why it happens.
What Happens in ALS?
- Muscles Get Weaker: Over time, people with ALS find it hard to walk, talk, eat, and even breathe.
- Different for Everyone: Each person with ALS has a different experience. Some might have trouble holding a pencil, while others might find it hard to speak clearly.
Is There a Cure for ALS?
- No Cure Yet: Sadly, we don’t have a cure for ALS right now.
- Research is Ongoing: Many smart scientists are working hard to find a cure.
Living with ALS

Living with ALS is a journey that requires a lot of care, patience, and understanding. We want to give you a deeper insight into how we can support those living with this condition. Remember, each person with ALS is unique, and their needs can change over time.
Helping with Movement
- Wheelchairs: Customized for comfort and mobility. Helps in moving around when walking becomes difficult.
- Braces and Walkers: Provide support to weakened limbs and help maintain balance.
- Physical Therapy: Gentle exercises to keep muscles as strong and flexible as possible.
- Home Modifications: Ramps, stairlifts, and modified bathrooms for easier access.
Assisting with Communication
- Speech Therapy: Techniques to maintain as much speech function as possible.
- Communication Devices: Such as tablets and computers that can be operated with minimal movement.
- Eye-Tracking Technology: Allows communication by tracking eye movements for those who can’t speak or type.
- Family Education: Teaching family members how to understand and communicate effectively with their loved one.
Eating and Nutrition
- Nutritional Advice: Tailored diets to meet individual health needs and maintain weight.
- Soft or Pureed Foods: Easier to swallow for those with difficulty in chewing.
- Feeding Tubes: In advanced stages, they provide necessary nutrition directly to the stomach.
- Hydration Management: Ensuring adequate fluid intake to prevent dehydration.
Breathing Support
- Breathing Exercises: To strengthen the muscles used for breathing.
- Non-Invasive Ventilation: Machines to assist breathing without needing a tube in the windpipe.
- Cough Assist Devices: Help in clearing the airway.
- Regular Monitoring: Checking lung function and making adjustments to care as needed.
Emotional and Psychological Support
- Counseling Services: For both patients and families to cope with emotional challenges.
- Support Groups: Connecting with others who are going through similar experiences.
- Recreational Therapy: Engaging in enjoyable activities to improve mood and mental health.
- End-of-Life Care Planning: Discussing and planning for future care preferences and decisions.
Supporting Daily Activities
- Occupational Therapy: To maintain independence in daily activities as much as possible.
- Adaptive Equipment: Special tools to help with dressing, eating, and other personal care tasks.
- Personal Care Assistance: Home health aides to assist with daily living activities.
- Family Training: Educating family members on how to provide practical support.
Community Involvement and Resources
- Local ALS Associations: Provide resources, information, and support services.
- Educational Workshops: For patients and caregivers to learn about managing ALS.
- Transportation Services: Special transportation options for medical appointments and outings.
- Financial and Legal Advice: Guidance on managing the financial and legal aspects of living with ALS.
Continuous Medical Care
- Regular Medical Checkups: To monitor the progression of Amyotrophic Lateral Sclerosis Symptoms.
- Medication Management: To address symptoms like muscle stiffness, cramps, or excess saliva.
- Team Approach: Collaboration between neurologists, therapists, nurses, and other specialists for comprehensive care.
- Research and Clinical Trials: Information about the latest ALS research and potential participation in trials.
Encouraging Independence and Quality of Life
- Empowering Patients: Encouraging self-care and decision-making as much as possible.
- Personalized Care Plans: Tailoring care to each individual’s preferences and needs.
- Promoting Social Interaction: Encouraging involvement with family and community to maintain social connections.
- Spiritual Support: Addressing spiritual needs and concerns as part of holistic care.
Taking Care of Personal Needs for ALS Patients
Caring for personal needs is a crucial aspect of supporting someone with ALS. Here’s a guide to help caregivers and family members provide the best care for their loved ones.
Personal Hygiene
- Bathing: Use of shower chairs and handheld showers. Assistance with bathing while ensuring safety and dignity.
- Skin Care: Regular skin checks to prevent sores, especially for those who are bedridden.
- Oral Care: Gentle brushing and mouthwash to maintain oral hygiene, even if the person can’t spit out water.
- Hair and Nail Care: Regular hair washing and grooming, along with nail care to prevent ingrown nails and infections.
Dressing
- Adaptive Clothing: Clothes with Velcro or snaps that are easier to put on and take off.
- Dressing Aids: Tools like dressing sticks and zipper pullers for those who can dress with minimal assistance.
- Assistance Techniques: Caregivers should learn proper techniques to assist with dressing while minimizing discomfort.
Toileting
- Accessible Toilets: Raised toilet seats or commode chairs for easier access.
- Incontinence Care: Use of absorbent products and skin protection creams as needed.
- Routine Schedule: Establishing a regular toileting schedule to reduce accidents.
Eating and Drinking
- Assistive Eating Tools: Utensils with larger handles, plate guards, and non-slip mats.
- Feeding Assistance: Gentle, patient assistance with feeding, ensuring the person is in an upright position to prevent choking.
- Hydration Strategies: Offering small sips of fluids frequently, using straws or special cups if needed.
Mobility
- Transfers: Safe techniques for moving the person from bed to chair and vice versa.
- Position Changes: Regularly changing the person’s position to avoid pressure sores and improve comfort.
- Mobility Aids: Using walkers, wheelchairs, or scooters as appropriate for the person’s mobility level.
Communication
- Communication Boards or Devices: For those who struggle with speech, using alternative communication methods.
- Patience in Conversation: Giving the person time to express themselves, not rushing or finishing sentences for them.
- Eye Contact: Maintaining eye contact and showing attentiveness to non-verbal cues.
Sleep
- Comfortable Bedding: Ensuring a comfortable mattress and pillows to prevent sores and aid in better sleep.
- Sleep Aids: Using devices like CPAP machines if there are breathing issues during sleep.
- Nighttime Care: Arranging for assistance during the night if needed, for bathroom trips or repositioning.
Emotional Support
- Encouraging Independence: Allowing the person to do as much as they can by themselves to promote a sense of control.
- Listening and Empathy: Being an understanding listener, validating their feelings and frustrations.
- Privacy and Respect: Maintaining their dignity and privacy, especially during personal care tasks.
Living with ALS is about adapting to changes and focusing on what can be done. With the right support and care, people with ALS can lead meaningful and fulfilling lives.

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | YouTube | Linkedin