What if your newborn couldn’t move their arm right after birth? For any parent, that’s a terrifying thought. When a baby enters the world, we expect all their little limbs to work perfectly. But sometimes, complications during delivery can hurt the delicate nerves in a baby’s shoulder, leading to what doctors call a brachial plexus injury at birth.
If you’re a parent looking for answers, you’re not alone. This blog, written by Dr. Chandril Chugh, a US-trained neurologist, breaks down everything you need to know about this condition.
In this blog, we will explain what causes a brachial plexus injury at birth, what signs to look for, what recovery looks like, and what parents can do to help. We will also look at the latest treatments and research helping babies recover better.
Table of Contents
ToggleWhat is a Brachial Plexus Injury at Birth?
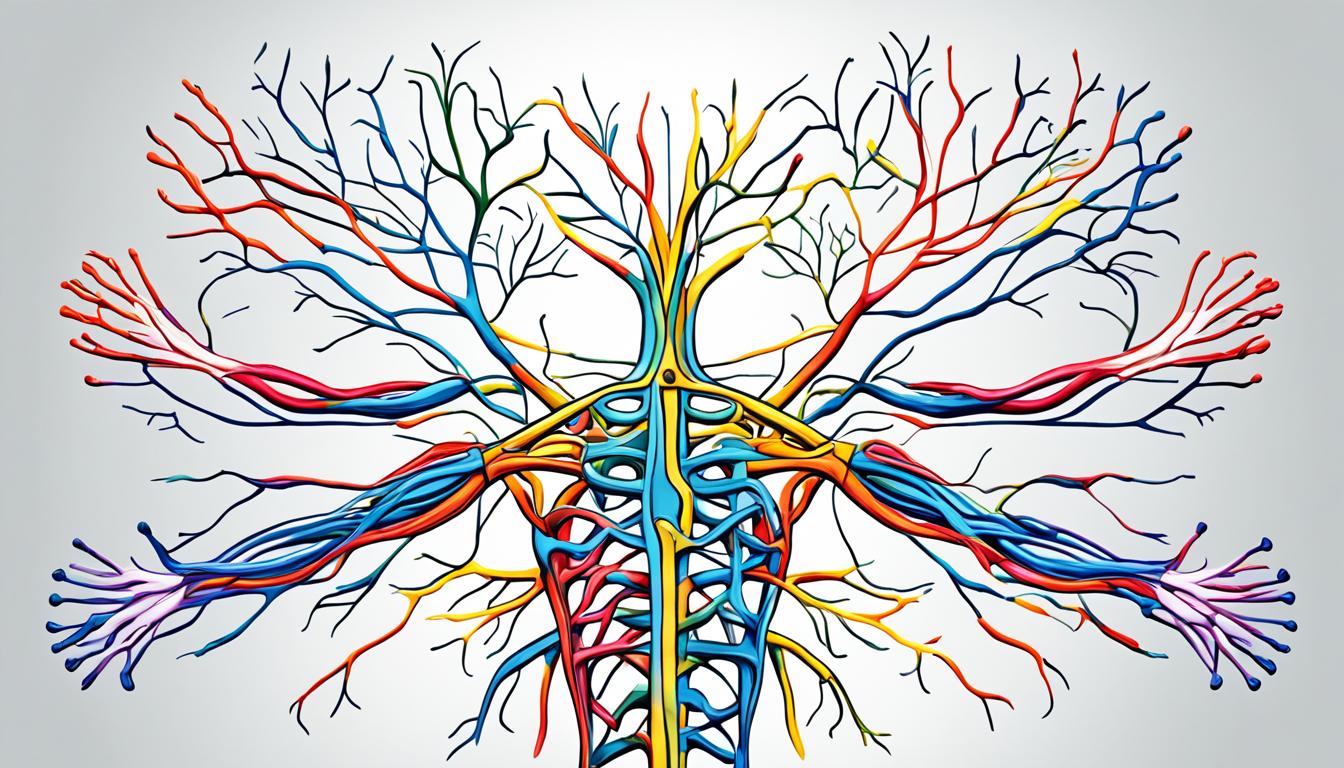
The brachial plexus is a group of nerves that starts near the neck and goes down into the shoulder and arm. These nerves help move the muscles and feel things in the arm, hand, and fingers. A brachial plexus injury at birth happens when these nerves are stretched, torn, or pulled away from the spinal cord during delivery.
This kind of injury often occurs when the baby’s shoulder gets stuck during birth, or if the baby is very large, making delivery harder. The more pressure on the baby’s shoulder, the higher the risk of nerve damage.
How Does This Nerve Injury Occur During Delivery?
Several events during labor can damage the nerves of the brachial plexus:
Common causes:
- Shoulder dystocia: when the baby’s shoulder gets stuck behind the mother’s pelvic bone.
- Breech delivery: when the baby is delivered feet or bottom first.
- Large birth weight: babies weighing more than 4,000 grams (about 8.8 pounds) are more likely to suffer this injury.
Types of injuries include:
- Erb’s palsy in newborns: affects the upper part of the brachial plexus, causing weakness in the shoulder and elbow.
- Klumpke’s palsy: affects the lower nerves, often causing hand and wrist problems.
- Total plexus palsy: all the nerves in the brachial plexus are affected, leading to complete paralysis of the arm.
Each of these conditions varies in severity and treatment needs.
Read: Sleep Hygiene with a Newborn: Moving Beyond “Sleep When Baby Sleeps”
How Common is Brachial Plexus Injury in Newborns?
Brachial plexus injury at birth is not very common, but it does happen.
According to the American College of Obstetricians and Gynecologists (ACOG), this injury occurs in about 0.5 to 2 out of every 1,000 live births.
Risk factors include:
- Prolonged labor
- Use of forceps or vacuum during delivery
- Maternal diabetes
- High birth weight
- Breech position
Here’s a quick table showing some of the data:
| Risk Factor | How It Increases Risk |
|---|---|
| Shoulder dystocia | Increases pulling on neck/shoulder during delivery |
| High birth weight (>8.8 lbs) | More difficult delivery; nerves are under more pressure |
| Breech birth | Arms may be pulled during delivery |
| Long labor | More stress and possible intervention |
What are the Signs and Symptoms Parents Should Watch For?
Early signs can be easy to miss, especially for first-time parents. Knowing what to look for is important.
How Can You Tell If Your Baby Has a Brachial Plexus Injury?
If your baby has a brachial plexus injury at birth, symptoms may show up right away or within the first few days.
Signs to look out for:
- One arm doesn’t move while the other does
- Baby does not grip with the affected hand
- Weak or limp arm hanging by the side
- No shoulder or elbow movement on one side
Severity levels:
- Mild: minor stretching of the nerve, may heal on its own
- Moderate: some damage, but still connected; needs therapy
- Severe: nerves are torn; may require surgery
When symptoms appear: Usually noticeable immediately, but sometimes they appear over the first week.
When Should You Seek a Medical Diagnosis?
If your baby shows any of the above signs, do not wait.
Early diagnosis is important because:
- Treatment works best when started early
- Helps prevent long-term weakness or disability
Doctors may use:
- Imaging (like ultrasound or MRI) to look at soft tissues
- EMG (electromyography) to test how nerves and muscles are working
Always get a pediatric neurologist to check your baby if symptoms last more than a week.
Long-Term Outlook and Prognosis
The long-term outlook for individuals with brachial plexus birth injury depends on various factors, including the severity of the injury, the effectiveness of treatment, and individual factors such as age and overall health. While some individuals may experience near-complete recovery and regain full motor function, others may have residual deficits that require ongoing care and accommodations.
It is essential to manage expectations and approach the recovery journey with patience and realistic goals. Open communication with healthcare providers, adherence to treatment plans, and ongoing therapy can greatly influence the long-term prognosis and overall quality of life for individuals with brachial plexus birth injury.
| Severity of BPBI | Potential Long-Term Outcomes |
|---|---|
| Mild | Spontaneous recovery with minimal to no long-term deficits. Ongoing rehabilitation may be required to optimize function and prevent future complications. |
| Moderate | Partial recovery with residual deficits. Ongoing therapy and supportive care interventions may be necessary for functional independence. |
| Severe | Significant and persistent motor impairment, potentially requiring ongoing medical management and adaptive strategies for daily activities. |
Individuals with brachial plexus birth injury should work closely with a multidisciplinary team, including pediatric neurologists, orthopedic surgeons, physical therapists, and occupational therapists, to determine the most appropriate treatment plan and optimize long-term outcomes.
Advances in the Management of Brachial Plexus Birth Injury
Over the past decade, there have been significant advances in the management of brachial plexus birth injury (BPBI). These advancements have allowed for improved understanding of shoulder pathology and its impact on motor recovery, the development of novel surgical techniques, a focus on sensory function and pain management, and global efforts to standardize outcomes assessment scales.
One major area of progress in the management of BPBI is the improved understanding of shoulder pathology and its correlation with motor recovery. Researchers and clinicians now have a more comprehensive understanding of the complex mechanisms involved in brachial plexus injuries and how they contribute to functional limitations in the affected limb.
Surgical intervention has also witnessed notable advancements, with the development of innovative techniques aimed at optimizing motor recovery. Microsurgical nerve reconstruction, for instance, has shown promising results in restoring nerve functionality and improving motor outcomes in patients with brachial plexus birth injuries. Additionally, distal nerve transfers have proven to be effective in cases where the proximal nerves are severely damaged, providing new neural pathways for motor function.
Furthermore, there has been a growing emphasis on addressing sensory function and pain management in the management of BPBI. It is now widely recognized that optimal recovery goes beyond motor function alone, and includes sensory outcomes and pain relief. This holistic approach ensures a comprehensive management plan that considers the overall quality of life for individuals with brachial plexus birth injuries.
Lastly, there is a concerted effort to standardize outcomes assessment scales in order to better evaluate the efficacy of different management strategies and interventions. The use of standardized assessment tools allows for more accurate monitoring of progress and comparison of outcomes across different treatment facilities and research studies.
These advances in the management of brachial plexus birth injury have resulted in more effective strategies for improving outcomes and enhancing recovery. By combining a deeper understanding of shoulder pathology, innovative surgical techniques, a holistic approach to sensory function and pain management, and standardized outcomes assessment, healthcare professionals are better equipped to provide comprehensive care and support for individuals with brachial plexus birth injuries.

| Treatment Advances | Benefits |
|---|---|
| Improved understanding of shoulder pathology | Enhanced motor recovery outcomes |
| Development of novel surgical techniques | Optimized nerve reconstruction and motor function |
| Focus on sensory function and pain management | Improved quality of life and overall outcomes |
| Standardization of outcomes assessment scales | Accurate evaluation of treatment effectiveness and comparison of outcomes |
Treatment Options for Brachial Plexus Birth Injury
The treatment options for brachial plexus birth injury (BPBI) vary based on the severity of the injury and the extent of motor impairment. Depending on the individual case, both nonsurgical and surgical approaches can be considered to improve motor function and facilitate a successful recovery.
Nonsurgical Strategies:
- Physical therapy – specialized exercises and movements tailored to the individual’s needs can help strengthen muscles, improve range of motion, and enhance functional abilities.
- Occupational therapy – focuses on developing fine motor skills and enhancing independence in daily activities.
- Hydrotherapy – water-based therapy can provide a supportive environment for exercise and promote relaxation, flexibility, and overall physical well-being.
- Botox injections – when used strategically, can help relieve muscle tightness and spasms, allowing for improved movement and function.
Surgical Procedures:
If nonsurgical options do not yield significant improvement or if the injury is severe, surgical intervention may be recommended. Two commonly performed surgical procedures for BPBI are microsurgical nerve reconstruction and distal nerve transfers.
| Surgical Procedure | Description |
|---|---|
| Microsurgical nerve reconstruction | As the name suggests, this procedure involves meticulous microsurgical techniques to repair or graft damaged brachial plexus nerves. It aims to restore nerve function and promote motor recovery. |
| Distal nerve transfers | This procedure involves transferring less critical, but still functional, nerves from other parts of the body to the affected area. It allows for the rerouting of nerve signals and promotes functional restoration. |

Both nonsurgical and surgical approaches have their benefits and considerations. The choice of treatment options depends on factors such as the individual’s age, the extent of damage to the brachial plexus, and the presence of associated conditions. It is essential to consult with a healthcare professional specializing in BPBI to determine the most suitable treatment plan for optimal recovery.
Rehabilitation and Supportive Care for Brachial Plexus Birth Injury
Rehabilitation and supportive care are essential in the recovery journey of individuals with brachial plexus birth injury (BPBI). With the right approaches, physical therapy and occupational therapy can significantly improve strength, flexibility, and functional abilities. Additionally, effective pain management strategies contribute to enhanced comfort and an improved quality of life.
Physical therapy: Physical therapy is a cornerstone of rehabilitation for BPBI. It focuses on improving motor function, range of motion, and overall physical well-being. It typically includes targeted exercises and activities designed to strengthen muscles and enhance coordination.
Occupational therapy: Occupational therapy aims to optimize daily living skills, such as self-care, fine motor skills, and sensory integration. Therapists work closely with individuals with BPBI to develop strategies and provide specialized tools or adaptive equipment that promote independence and functional abilities.
Pain management: Effective pain management is crucial for individuals with BPBI, as it can significantly impact their daily lives. Various strategies, including medication, nerve blocks, and alternative therapies, can help alleviate discomfort and improve overall well-being.
| Rehabilitation and Supportive Care Strategies for BPBI | Benefits |
|---|---|
| Physical therapy |
|
| Occupational therapy |
|
| Pain management |
|
Together, these rehabilitation and supportive care strategies empower individuals with BPBI to regain function and independence. By focusing on physical therapy, occupational therapy, and effective pain management, individuals can enhance their recovery and achieve a higher quality of life.
Prognosis and Long-Term Outcomes of Brachial Plexus Birth Injury
After a brachial plexus birth injury (BPBI), the prognosis and long-term outcomes can vary depending on the severity of the injury and the effectiveness of treatment. While many infants experience spontaneous motor recovery within three to six months, others may require additional interventions for optimal outcomes. It is crucial to consider sensory outcomes and pain management in the long-term management of individuals with BPBI.
Motor Recovery
In most cases, motor recovery in infants with BPBI occurs naturally within the first six months of life. As the nerves heal, gradual improvement in muscle strength and movement becomes evident. Early intervention and dedicated physical therapy can further enhance motor recovery. However, in severe cases, where significant nerve damage has occurred, surgical procedures such as microsurgical nerve reconstruction or distal nerve transfers may be necessary to facilitate motor recovery.
Sensory Outcomes
Beyond motor function, sensory outcomes are essential in assessing the overall progress of individuals with BPBI. Sensory deficits in the affected arm can range from mild to severe and may require ongoing management. Strategies such as sensory reeducation and sensory integration therapy can help individuals with BPBI optimize their sensory function and adapt to their unique sensory challenges.
Pain Management
Pain management is a crucial aspect of the long-term care for individuals with BPBI. Nerve pain, muscle tightness, and discomfort in the affected arm are common challenges. Medications, nerve blocks, and alternative therapies such as acupuncture and massage can be effective in alleviating pain and improving quality of life for individuals with BPBI.
| Outcome | Percentage of Recovered Cases |
|---|---|
| Complete Recovery | 45% |
| Partial Recovery | 30% |
| Persistent Motor Impairment | 15% |
| Significant Motor Deficits | 10% |
Based on a study involving a large sample of infants with BPBI, the table above highlights the distribution of long-term motor recovery outcomes. It is important to note that individual outcomes may vary, and each case should be evaluated and treated accordingly.
Start Healing Today with Expert Care
Watching your baby struggle with a brachial plexus injury at birth can be heartbreaking. But with the right steps, recovery is absolutely possible. Early therapy, consistent home care, and expert guidance can make all the difference.
If your baby shows signs of weakness or movement issues, don’t wait. Book a consultation with Dr. Chandril Chugh today and give your child the care they deserve.
FAQ
What causes brachial plexus birth injury?
Brachial plexus birth injury is caused by a closed traction injury to the brachial plexus nerves during delivery.
How common is brachial plexus birth injury?
Brachial plexus birth injury affects approximately 2 in every 1,000 babies born in the United States, with around 12,000 cases reported annually.
What are the treatment options for brachial plexus birth injury?
Treatment options for brachial plexus birth injury depend on the severity of the injury. Nonsurgical options include physical and occupational therapy, hydrotherapy, and Botox injections. In more severe cases, surgical procedures such as microsurgical nerve reconstruction and distal nerve transfers may be recommended.
What role does rehabilitation play in brachial plexus birth injury recovery?
Rehabilitation, including physical therapy and occupational therapy, plays a crucial role in improving strength, flexibility, and functional abilities for individuals with brachial plexus birth injury.
What are the long-term outcomes of brachial plexus birth injury?
The long-term outcomes of brachial plexus birth injury vary depending on the severity of the injury and the effectiveness of treatment. While many infants experience spontaneous motor recovery, some may require additional interventions for optimal outcomes.
Source Links

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
→ Book a consultation to discover which remedies suit your needs best.
About Author | Instagram | YouTube | Linkedin