Bell’s palsy is a condition that can cause sudden paralysis of the facial muscles, leading to facial drooping, difficulty in blinking, and an asymmetric smile. While the exact cause of Bell’s palsy is not fully understood, there are several factors that are believed to contribute to its development.
Research suggests that inflammation of the facial nerve, viral infections such as the herpes simplex virus, autoimmune diseases, trauma, tumors, certain medications, and other underlying factors may trigger Bell’s palsy. However, it’s important to note that Bell’s palsy is a diagnosis of exclusion, meaning that other conditions with similar symptoms should be ruled out before reaching a conclusion.
Key Takeaways:
- Bell’s palsy is an idiopathic condition that results in sudden facial paralysis.
- Inflammation of the facial nerve, viral infections, autoimmune diseases, trauma, tumors, certain medications, and other factors may trigger Bell’s palsy.
- It’s important to exclude other conditions with similar symptoms before diagnosing Bell’s palsy.
Table of Contents
ToggleEpidemiology and Risk Factors of Bell’s Palsy
Bell’s palsy, although relatively rare, has an annual incidence of approximately 32 cases per 100,000 people. This condition is commonly diagnosed in individuals between the ages of 15 and 45, with younger patients generally having a better prognosis.
Several risk factors have been identified for Bell’s palsy, including diabetes, hypertension, respiratory disease, obesity, pregnancy, and preeclampsia. These underlying conditions can increase the likelihood of developing Bell’s palsy.
When it comes to gender differences, there are no significant variations in risk or outcomes between men and women. However, approximately 7% of patients experience recurrent Bell’s palsy, usually within 1.5 years of the initial onset.
To summarize:
- Bell’s palsy has an annual incidence of around 32 cases per 100,000 people.
- It is most commonly observed in individuals aged 15 to 45.
- Risk factors for Bell’s palsy include diabetes, hypertension, respiratory disease, obesity, pregnancy, and preeclampsia.
- Recurrent Bell’s palsy occurs in approximately 7% of patients, typically within 1.5 years of the initial onset.
Understanding the epidemiology and risk factors associated with Bell’s palsy can help individuals and healthcare professionals identify potential triggers and take appropriate preventive measures.
Pathophysiology of Bell’s Palsy
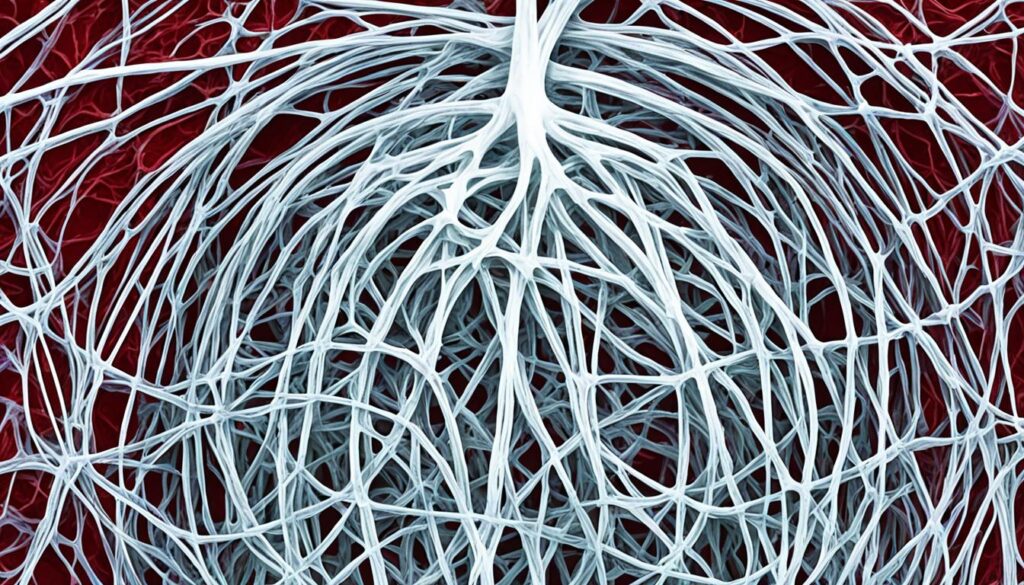
Bell’s palsy is a condition that results from the inflammation of the facial nerve, specifically cranial nerve VII, as it exits the skull. This inflammation can cause various complications, including obstruction, ischemia, and demyelination of the nerve, ultimately leading to the weakness of the facial muscles.
The exact cause of inflammation in Bell’s palsy is still uncertain. However, studies have explored the role of herpesviruses, such as the herpes simplex virus, in the development of the condition. These viruses have been investigated as potential causative agents due to their ability to trigger inflammatory responses and nerve damage.

Further research is needed to establish a definitive link between herpesviruses and the occurrence of Bell’s palsy. Understanding the underlying mechanisms and triggers of inflammation can pave the way for targeted treatment strategies and improved patient outcomes.
Clinical Presentation of Bell’s Palsy
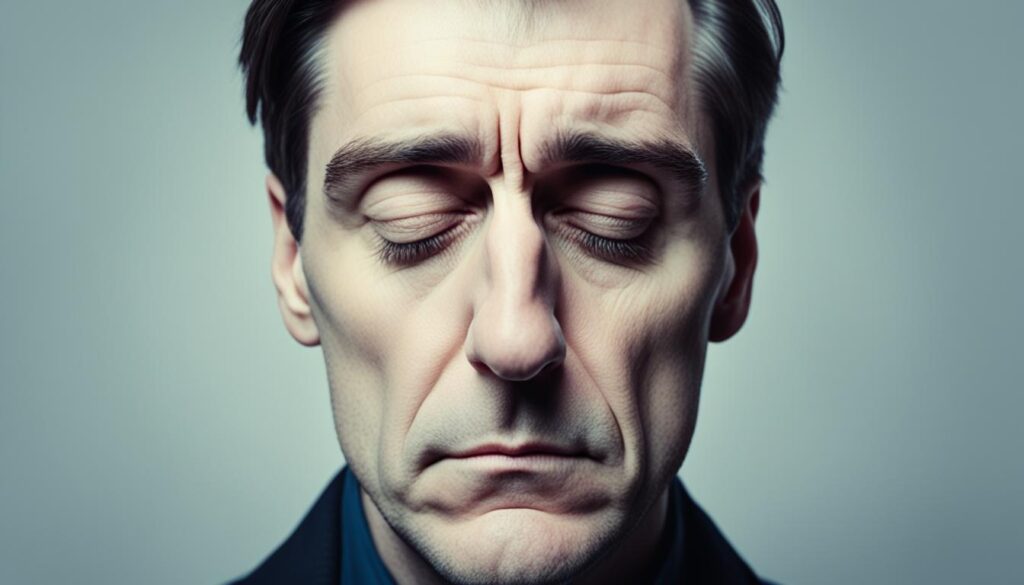
In individuals with Bell’s Palsy, the sudden weakness or paralysis of the facial muscles on one side of the face is the hallmark symptom. This can manifest as facial drooping, making it difficult to maintain a symmetrical appearance. An asymmetric smile is also common, with the affected side of the face showing limited movement. Moreover, closing the eyelid on the affected side can be challenging, resulting in eye closure difficulties. Facial pain may also be experienced in some cases.
Additional symptoms that may accompany Bell’s Palsy include jaw pain, loss of taste, headache, and sensitivity to sound. These manifestations contribute to the overall impact of the condition on an individual’s quality of life. To gauge the severity of facial nerve dysfunction, the House-Brackmann grading scale is often employed. This scale helps assess the degree of muscle weakness and paralysis, providing a standardized measure of the condition’s impact.
Here is a table summarizing the common clinical presentations of Bell’s Palsy:
| Clinical Presentations of Bell’s Palsy | |
|---|---|
| Facial Drooping | An asymmetric appearance due to weakness or paralysis of the facial muscles. |
| Asymmetric Smile | Limited or affected movement on one side of the face while smiling. |
| Eye Closure Difficulties | Inability or challenges in closing the eyelid on the affected side. |
| Facial Pain | Pain experienced in the facial region, which may vary in intensity. |
It is important to recognize these symptoms and seek medical attention promptly for a proper diagnosis and appropriate management of Bell’s Palsy.
Diagnosis of Bell’s Palsy
The diagnosis of Bell’s palsy is primarily based on clinical findings, as there is no specific test available to confirm the condition. To accurately diagnose Bell’s palsy, healthcare professionals rely on a comprehensive approach that includes:
- Taking a detailed clinical history
- Conducting a thorough physical examination
- Performing imaging studies, if necessary
Clinical History for Bell’s Palsy
A thorough clinical history is crucial in diagnosing Bell’s palsy as it helps exclude other potential causes of facial paralysis. During this process, your healthcare provider will ask you questions about:
- Recent illnesses or infections
- Medications you are currently taking
- Prior herpes infections
By gathering this information, your healthcare provider can effectively rule out other underlying conditions that may mimic the symptoms of Bell’s palsy.
Physical Examination for Bell’s Palsy
Physical examination is a vital component of diagnosing Bell’s palsy. Your healthcare provider will perform a comprehensive evaluation, which may include:
- A complete ophthalmologic exam to assess eye closure, tear production, and corneal sensitivity
- An assessment of your facial muscles, including facial symmetry, muscle strength, and mobility
Through this physical examination, your healthcare provider can further support the diagnosis of Bell’s palsy.
Imaging for Bell’s Palsy
In some cases, imaging studies may be necessary to rule out other underlying causes of facial paralysis. Magnetic resonance imaging (MRI) is commonly used to evaluate the facial nerve and exclude conditions such as tumors or other structural abnormalities. This imaging modality provides detailed images that aid in confirming the diagnosis of Bell’s palsy.
It is important to note that imaging studies are not always required for every case of Bell’s palsy and are typically reserved for individuals with atypical presentations or those who do not show signs of improvement over time.

Prognosis of Bell’s Palsy
Recovery from Bell’s Palsy is a common outcome, with the majority of individuals experiencing spontaneous improvement within three to five weeks of onset. The time for recovery in Bell’s Palsy can vary from person to person, with some individuals recovering sooner and others taking a bit longer. Several factors can influence the recovery process in Bell’s Palsy:
1. Severity of Palsy: The extent of recovery is closely associated with the initial severity of facial paralysis at presentation. Individuals with milder symptoms tend to have a better prognosis and a higher likelihood of full recovery.
2. Age: The age of the patient also plays a role in the recovery from Bell’s Palsy. Younger patients generally have better outcomes and a higher chance of regaining complete facial function.
3. Comorbidities: The presence of underlying health conditions, such as diabetes or hypertension, can affect the recovery process. Managing these comorbidities effectively can contribute to a more favorable prognosis.
4. Prompt Treatment: Timely intervention and appropriate medical care can positively impact the recovery from Bell’s Palsy. Initiating treatment early may help reduce inflammation, promote nerve regeneration, and enhance overall recovery.
While the majority of individuals recover fully, it is important to note that some may experience residual deficits, such as partial facial weakness or synkinesis (involuntary muscle movements). These residual symptoms may require additional treatment or management to optimize overall facial function.
Recovery Tips for Bell’s Palsy:
- Follow your healthcare professional’s advice and treatment plan consistently.
- Practice facial exercises recommended by your healthcare provider to help improve muscle strength and coordination.
- Take care of your overall health and well-being by eating a balanced diet, getting enough rest, and managing stress.
- Avoid exposure to extreme temperatures and excessive sunlight that can potentially irritate the affected facial nerves.
- Seek emotional support from friends, family, or support groups to cope with the challenges of facial paralysis.
By understanding the factors that influence recovery and adopting appropriate measures, you can improve your chances of a more complete recovery from Bell’s Palsy.
Other Causes of Facial Paralysis
While Bell’s palsy is the most common cause of sudden onset facial paralysis, there are several other potential causes that should be considered. Here are some other types of facial paralysis:
- Congenital Facial Paralysis:
Congenital facial paralysis refers to paralysis that is present at birth. It can be caused by various developmental abnormalities and may be associated with other congenital conditions.
- Acute Facial Paralysis:
Acute facial paralysis can occur suddenly over a short period of time. It can be caused by different factors such as stroke, infection, autoimmune diseases, tumors, surgery, and trauma.
- Chronic Facial Paralysis:
Chronic facial paralysis worsens over time. It can be associated with tumors or growths along the course of the facial nerve, leading to gradual loss of facial function and movement.
- Other Causes:
In addition to the above, there are various other causes of facial paralysis, including neurological disorders, Lyme disease, Ramsay Hunt syndrome, Guillain-Barre syndrome, and hereditary conditions.
It is important to identify the underlying cause of facial paralysis in order to determine the appropriate treatment and management strategies. Proper diagnosis and comprehensive evaluation by a healthcare professional are crucial.
Treatment Options for Facial Paralysis
The treatment for facial paralysis depends on the underlying cause and the individual’s specific condition. Medical, injectable, and surgical treatments are among the options available to address facial paralysis and restore facial function.
Medical Treatment for Facial Paralysis
Medical treatment for facial paralysis often includes the use of medications to manage symptoms, reduce inflammation, and promote nerve recovery. Antibiotics may be prescribed if an infection is suspected, while antiviral medications can help control viral infections that may contribute to facial paralysis. Steroids, such as prednisone, are commonly used to reduce inflammation and improve nerve function.
Injectable Treatment for Facial Paralysis
Injectable treatments offer a non-surgical approach to improving facial symmetry and function in individuals with facial paralysis. Botox®, a commonly used injectable, can help relax overactive muscles, reducing involuntary movements and improving facial appearance. Injectable fillers, such as hyaluronic acid fillers, can restore volume and improve facial contour, aiding in the restoration of facial balance and harmony.
Surgical Treatment for Facial Paralysis
In cases where the underlying cause of facial paralysis cannot be managed with medical or injectable treatments, surgical intervention may be necessary. Surgical treatment options for facial paralysis aim to address the underlying cause, restore facial balance, and optimize facial function. Procedures such as nerve decompression, nerve grafting, or muscle transfer may be performed to improve nerve function and restore facial movement.
It is important to note that the choice of treatment depends on the individual’s specific condition, goals, and overall health. A personalized treatment plan should be developed in collaboration with a healthcare professional experienced in the management of facial paralysis.

| Treatment Option | Description |
|---|---|
| Medical Treatment | Includes the use of antibiotics, antivirals, and steroids to manage symptoms, reduce inflammation, and promote nerve recovery. |
| Injectable Treatment | Non-surgical options such as Botox® and injectable fillers can improve facial symmetry, reduce involuntary movements, restore volume, and improve facial contour. |
| Surgical Treatment | Procedures like nerve decompression, nerve grafting, or muscle transfer may be performed to address the underlying cause, restore facial balance, and optimize facial function. |
Conclusion
Facial paralysis, including Bell’s palsy, can have a significant impact on your life, affecting facial movement, appearance, and essential functions. While the exact cause of Bell’s palsy is unknown, several triggers have been identified, including inflammation of the facial nerve and viral infections. Early diagnosis and treatment are crucial for optimal recovery, and a range of treatment options, including medications, injectables, and surgery, are available.
By understanding the underlying causes of facial paralysis and exploring appropriate treatment options, you can improve your quality of life and regain facial function. It is important to work closely with healthcare professionals to develop a personalized treatment plan that addresses your specific needs and goals. Regular follow-up visits and ongoing management may be necessary to ensure the best possible outcome.
If you or a loved one are experiencing facial paralysis symptoms, seek medical attention promptly to determine the cause and explore available treatment options. Remember, while living with facial paralysis can present challenges, with the right care and support, you can enhance your well-being and regain control over your daily life.
FAQ
What are the causes of Bell’s Palsy?
The exact cause of Bell’s Palsy is not fully understood, but potential triggers include inflammation of the facial nerve, herpes simplex virus, other viral infections, autoimmune diseases, trauma, tumors, and certain medications.
What are the risk factors for Bell’s Palsy?
Risk factors for Bell’s Palsy include diabetes, hypertension, respiratory disease, obesity, pregnancy, and preeclampsia. Recurrent Bell’s Palsy is seen in approximately 7% of patients, usually within 1.5 years of the initial onset.
How does Bell’s Palsy occur?
Bell’s Palsy occurs due to inflammation of the facial nerve as it exits the skull, leading to facial muscle weakness. The exact cause of inflammation is unclear, but herpesviruses, including herpes simplex virus, have been investigated as potential causative agents.
What are the symptoms of Bell’s Palsy?
The onset of Bell’s Palsy is characterized by sudden weakness or paralysis of the facial muscles on one side of the face. This can lead to facial drooping, an asymmetric smile, drooling, difficulty closing the eyelid on the affected side, jaw pain, loss of taste, headache, and sensitivity to sound.
How is Bell’s Palsy diagnosed?
The diagnosis of Bell’s Palsy is primarily based on clinical findings, as there is no specific test available to confirm the condition. A thorough clinical history and physical examination, including a complete ophthalmologic exam, can support the diagnosis. In some cases, imaging studies such as magnetic resonance imaging (MRI) may be necessary.
What is the prognosis for Bell’s Palsy?
The majority of individuals with Bell’s Palsy experience spontaneous recovery within three to five weeks. The extent of recovery is associated with the severity of palsy at presentation and the age of the patient. Younger patients and those with incomplete palsy tend to have a better prognosis.
What are the other causes of facial paralysis?
Aside from Bell’s Palsy, facial paralysis can be caused by congenital factors, acute conditions such as stroke or infection, autoimmune diseases, tumors, surgery, trauma, or chronic conditions associated with tumors or growths along the course of the facial nerve.
What are the treatment options for facial paralysis?
The treatment for facial paralysis depends on the underlying cause and the individual’s specific condition. Medical treatment options may include antibiotics, antivirals, and steroids. Injectable treatments such as Botox® and injectable fillers can improve facial symmetry and function. Surgical intervention may be necessary in some cases.
What impact does facial paralysis have on an individual’s life?
Facial paralysis, including Bell’s Palsy, can significantly impact an individual’s life, affecting facial movement, appearance, and essential functions. Early diagnosis and appropriate treatment can help improve quality of life and regain facial function.
Source Links
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




