Understanding Autism Spectrum Disorder (ASD )
Autism Spectrum Disorder (ASD) is a diverse condition that affects individuals in varying ways. It is not a single disorder but rather a spectrum of closely related disorders, each with its own unique insights. Autism spectrum disorder impacts individuals' social interaction, empathy, communication, and flexible behavior to different degrees.
With ASD, every person is unique and may exhibit a combination of symptoms that can vary greatly from one individual to another. Even individuals with the same diagnosis can have different behaviors and abilities. It's important to understand that autism spectrum disorder is a complex neurodevelopmental disorder that requires careful consideration and individualized support.
In this article, we'll provide you with in-depth understanding of autism spectrum disorder - what it is, how it is diagnosed, the challenges faced by individuals with ASD, treatment options, and the latest research insights. Whether you have a loved one with ASD or are interested in learning more about this condition, this article aims to provide valuable information and resources to help you navigate and understand autism spectrum disorder.
What is Autism Spectrum Disorder ASD?
Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder that affects how people interact with others, communicate, learn, and behave. It is described as a developmental disorder because symptoms generally appear in the first 2 years of life. People with ASD often have difficulty with communication and interaction with other people, as well as restricted interests and repetitive behaviors.
ASD is characterized by a shared core of symptoms that vary in severity among individuals. These symptoms primarily affect social interaction and communication, as well as flexibility in behavior. The shared core symptoms of ASD include:
- Challenges in social interaction and communication
- Restricted interests and repetitive behaviors
- Difficulties in understanding and expressing emotions
- Preference for routine and sameness
- Unusual sensory responses
Individuals with ASD may experience these symptoms to varying degrees. Some individuals may have mild symptoms and function well in certain areas of life, while others may require more support and assistance. It's important to recognize that every person with ASD is unique and may present differently.
The Different Terms and Labels of Autism Spectrum Disorder ASD
The terminology surrounding autism spectrum disorder (ASD) can be confusing, with various terms and labels used by different professionals. It's important to understand these different terms but remember that what truly matters is understanding your child's unique needs and finding the right treatment that address those needs.
Among the different labels used, high-functioning autism and atypical autism are two terms that are commonly used. High-functioning autism refers to individuals on the autism spectrum who have average or above-average intelligence and relatively mild symptoms. This label is often associated with individuals who have strong language and cognitive skills, but still face challenges in social interaction and communication.
On the other hand, atypical autism is a term used to describe individuals whose symptoms do not fit within the traditional diagnostic criteria for autism spectrum disorder. These individuals may exhibit some characteristics of ASD, but not enough to receive a formal ASD diagnosis. Atypical autism is sometimes used as a way to categorize individuals who have some autism-related traits but may not meet all the criteria for a specific ASD diagnosis.
It's worth noting that the diagnostic label itself is not as important as understanding and addressing your child's specific symptoms and needs. The focus should be on finding the right help and support for your child, regardless of the specific diagnostic label assigned.
The Importance of Understanding Your Child's Unique Needs
Each individual with ASD is unique, with their own strengths, challenges, and individual needs. Rather than getting caught up in diagnostic labels, it's crucial to focus on understanding your child's particular set of symptoms and finding the appropriate treatment and support that meets their needs.
By understanding your child's unique needs, you can tailor interventions and therapies to address their specific challenges. This individualized approach allows for a more effective and targeted treatment plan that can help your child thrive.
Remember, the key is not the label or diagnosis, but rather providing the right support and opportunities for your child to reach their full potential.
The Role of Diagnostic Labels in Autism Spectrum Disorder
While diagnostic labels can be helpful in understanding and categorizing the various presentations of autism spectrum disorder, it's important to recognize that they are not definitive or set in stone. The field of autism research and understanding is continuously evolving, and diagnostic labels may change as new insights emerge.
What's most important is to focus on your child's unique needs and work closely with healthcare professionals to develop an individualized treatment plan. This plan should address their specific challenges and provide the necessary support to help them thrive.
Remember, a diagnosis is just the starting point. It's the beginning of a journey towards better understanding and meeting your child's needs in the most effective way possible.
The Pre-2013 Classification of Autism Spectrum Disorder ASD
Before 2013, autism spectrum disorder (ASD) encompassed several distinct disorders that fell under the broader umbrella of ASD. These disorders included Autistic Disorder (classic autism), Asperger's Syndrome, Pervasive Developmental Disorder - Not Otherwise Specified (PDD-NOS), Childhood Disintegrative Disorder, and Rett Syndrome. Each of these disorders had its own diagnostic criteria and characteristics.
However, in an effort to streamline the classification and better reflect the diverse nature of ASD, the American Psychiatric Association made significant changes in the diagnostic criteria. In the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), these separate disorders were consolidated into a single diagnostic classification known as "Autism Spectrum Disorder" (ASD).
The consolidation of the pre-2013 classification into ASD acknowledges that individuals with ASD can present with a wide range of symptoms and abilities. It recognizes that there is considerable overlap among the different subtypes and that they share a common core set of characteristics.
The new classification system provides a more comprehensive and inclusive framework that allows for a better understanding, diagnosis, and treatment of individuals across the spectrum. It emphasizes the importance of addressing individual needs and tailoring interventions accordingly.
| Autism Spectrum Disorder Diagnosis | Pre-2013 Classification |
|---|---|
| Autism Spectrum Disorder (ASD) | Autistic Disorder (classic autism) |
| Asperger's Syndrome | |
| Pervasive Developmental Disorder - Not Otherwise Specified (PDD-NOS) | |
| Childhood Disintegrative Disorder | |
| Rett Syndrome |
This new classification system eliminates potential confusion and ensures that individuals with diverse presentations of autism spectrum disorder receive appropriate support and interventions.
Symptoms of Autism Spectrum Disorder ASD
The symptoms of autism spectrum disorder (ASD) can vary widely, but they generally involve difficulties with social interaction, communication, and repetitive behaviors. Individuals with ASD may exhibit a range of behaviors and characteristics that can impact their daily lives.
- Unusual or inappropriate body language
- Lack of interest in others
- Difficulty understanding other people's feelings
- Delays in speech development
- Repetitive body movements
- Strong need for sameness and routines
These symptoms can manifest differently in each individual, and the severity can also vary. Some individuals may have mild symptoms and can function relatively well, while others may have more significant challenges that require support and intervention.
Understanding these symptoms is crucial for early identification and intervention, as it allows for appropriate support and resources to be provided to individuals with ASD.

| Symptoms of Autism Spectrum Disorder ASD | Description |
|---|---|
| Social Interaction Difficulties | Individuals with ASD may struggle with understanding and engaging in social interactions. They may have trouble making eye contact, interpreting facial expressions, or developing relationships with others. |
| Communication Challenges | Many individuals with ASD experience difficulties in verbal and nonverbal communication. They may have delayed speech development, limited vocabulary, or struggle with understanding and using gestures, body language, and tone of voice. |
| Repetitive Behaviors | Repetitive behaviors and restricted interests are common in individuals with ASD. These behaviors can include repetitive movements, such as hand flapping or rocking, as well as intense interests in specific topics or objects. |
Challenges Faced by Individuals with Autism Spectrum Disorder ASD
Living with Autism Spectrum Disorder (ASD) can present various challenges for individuals. These challenges often manifest in different areas of life, impacting social interaction, communication, learning abilities, and sensory processing.
1. Social Interaction
People with ASD may struggle with social interaction, finding it difficult to understand social cues and engage in reciprocal communication. They may face challenges in forming and maintaining relationships, making it important to provide supportive environments that accommodate their unique needs.
2. Communication
Individuals with ASD may experience difficulties in verbal and non-verbal communication. They may struggle with understanding and using language effectively, which can hinder expressive skills and hinder their ability to express their thoughts and emotions.
3. Learning Difficulties
ASD can impact learning abilities. Some individuals may require additional support to achieve academic success due to challenges with attention, concentration, and processing information. Tailored educational strategies and interventions can help bridge these gaps and facilitate optimal learning experiences.
4. Sensory Problems
Sensory processing difficulties are common in individuals with ASD. They may exhibit heightened sensitivity or an underreacting response to sensory stimuli. This can involve being overwhelmed by certain sounds, textures, smells, or sights. Creating sensory-friendly environments and incorporating sensory integration techniques can help individuals with ASD better navigate their sensory experiences.
To gain a better understanding of these challenges, consider the following table:
| Challenges | Impact |
|---|---|
| Social Interaction | Difficulty understanding social cues; challenges in forming and maintaining relationships |
| Communication | Struggles with verbal and non-verbal communication, impacting expressive skills |
| Learning Difficulties | Challenges with attention, concentration, and processing information; may require additional support for academic success |
| Sensory Problems | Heightened sensitivity or underreacting response to sensory stimuli |
Understanding the challenges faced by individuals with Autism Spectrum Disorder is essential in providing them with the necessary support, accommodations, and inclusive environments. By addressing these challenges, we can foster a more inclusive and understanding society.
Diagnosis of Autism Spectrum Disorder ASD
Diagnosing autism spectrum disorder (ASD) involves a two-stage process that combines developmental screening and comprehensive evaluation by a specialized healthcare team. The purpose of this process is to assess the presence and severity of ASD symptoms, determine the need for further evaluation, and provide an accurate diagnosis.
The first stage of the diagnosis involves general developmental screening during routine well-child checkups. Pediatricians or primary care providers typically conduct this screening to identify any potential developmental delays or signs of ASD. Developmental screening tools, such as the M-CHAT-R/F or the Ages and Stages Questionnaires (ASQ), may be used to evaluate a child's communication skills, social functioning, and behavior.
If the developmental screening raises concerns or suggests a possible risk of ASD, further evaluation is recommended. The second stage involves a more in-depth diagnostic evaluation conducted by a multidisciplinary team of healthcare professionals who specialize in autism spectrum disorders. This team may include psychologists, pediatricians, speech therapists, and other specialists.
The diagnostic evaluation typically includes:
- Medical and neurological examinations to rule out any underlying medical conditions or genetic factors that may be contributing to the symptoms.
- Cognitive and language assessments to evaluate intellectual functioning, language skills, and cognitive abilities.
- Behavioral observations and assessments to analyze social interaction, communication abilities, and repetitive behaviors.
These evaluations help healthcare providers gather comprehensive information about the individual's developmental history, symptoms, and abilities. By considering multiple factors and conducting a thorough evaluation, an accurate diagnosis of autism spectrum disorder can be made.
Treatment Options for Autism Spectrum Disorder ASD
Treatment for autism spectrum disorder (ASD) is individualized and depends on the unique needs of each individual. It may involve a combination of interventions, therapies, and support services aimed at improving communication skills, social interaction, and overall quality of life.
Behavioral Therapy
Behavioral therapy is a widely used approach in treating ASD. Applied Behavior Analysis (ABA) is commonly employed to reinforce positive behaviors and teach new skills. It focuses on breaking tasks into smaller steps and providing consistent rewards to encourage desired behaviors. ABA therapy can be tailored to address specific challenges faced by individuals with ASD, such as social skills, communication, and self-help skills.
Speech and Language Therapy
Speech and language therapy can help individuals with ASD improve their communication skills. Therapists work with individuals to develop language abilities, improve nonverbal communication, and address speech challenges. Techniques may include using visual aids, social stories, and augmentative and alternative communication (AAC) devices to enhance communication and promote expressive language skills.
Occupational Therapy
Occupational therapy focuses on developing the necessary skills for everyday living, fine motor skills, sensory integration, and self-regulation. Therapists assist individuals with autism in learning and practicing tasks related to self-care, fine motor skills, and sensory processing. Occupational therapy can also address difficulties with sensory sensitivities and help individuals develop strategies to cope with environmental stimuli.
Educational Interventions
Education plays a vital role in the treatment of ASD. Individualized education plans (IEPs) are developed to tailor the educational experience to meet the specific needs of the individual. Special education instructors and support staff work together to provide a structured learning environment, accommodations, and strategies to help individuals with ASD succeed academically and socially.
| Treatment Option | Description |
|---|---|
| Behavioral Therapy | Applied Behavior Analysis (ABA) therapy focuses on reinforcing positive behaviors and teaching new skills. |
| Speech and Language Therapy | Speech and language therapy helps improve communication skills through various techniques and tools. |
| Occupational Therapy | Occupational therapy focuses on developing everyday living skills, fine motor skills, and sensory integration. |
| Educational Interventions | Individualized education plans (IEPs) provide tailored support and accommodations in educational settings. |
Early intervention is crucial in improving outcomes for individuals with ASD. The earlier treatment is initiated, the better the chances of positive progress and improved quality of life.
Remember, each individual with autism is unique, so it's important to consult with healthcare professionals and therapists to determine the most suitable treatment options for your loved one with ASD.
Research and Clinical Trials for Autism Spectrum Disorder ASD
Ongoing research and clinical trials play a crucial role in advancing our understanding of autism spectrum disorder (ASD) and developing more effective treatments and interventions. By participating in research studies and clinical trials, individuals with ASD and their families can gain access to cutting-edge treatments and contribute to the advancement of knowledge in the field.
The Importance of Research
Research is fundamental in enhancing our understanding of ASD's causes, diagnosis, and potential treatments. Scientists and clinicians worldwide are dedicated to unraveling the complexities of ASD, aiming to provide better support and tailored interventions for individuals on the spectrum.
Clinical Trials for ASD
Clinical trials are essential for evaluating the safety and effectiveness of new medications, therapies, and interventions for ASD. These trials involve carefully designed studies that follow ethical guidelines to protect the participants' rights and well-being.
By participating in clinical trials, individuals with ASD and their families have the opportunity to access novel treatments and interventions that might not be widely available yet. They also contribute to the generation of scientific evidence that informs future treatment options and guidelines.
How to Get Involved
If you're interested in participating in research studies or clinical trials for ASD, reach out to research institutions, universities, or specialized clinics in your area. These organizations often conduct studies and trials and are actively looking for participants.
Before participating, it's important to carefully review the study's details, requirements, and potential risks and benefits. Consult with healthcare professionals and consider discussing your involvement with trusted individuals in your support network.
Advancing Knowledge and Improving Lives
Research and clinical trials for ASD are critical for advancing knowledge, improving treatments, and enhancing the lives of individuals on the spectrum. By participating and contributing to the collective efforts in understanding and managing ASD, you play an active role in shaping the future of autism care and support.
Research and clinical trials hold the key to unlocking a brighter future for individuals with autism spectrum disorder.
Conclusion
Autism Spectrum Disorder (ASD) is a complex and diverse condition that affects individuals in unique ways. While there is no cure for ASD, early intervention and appropriate support can greatly improve outcomes and enhance the quality of life for individuals with autism spectrum disorder.
Understanding the specific needs and challenges faced by individuals with ASD is essential in providing them with the necessary support and opportunities to thrive. By recognizing and accommodating their individual differences, we can create an inclusive society that embraces and empowers individuals with ASD.
It is important to remember that autism spectrum disorder is not a one-size-fits-all condition. Each individual with ASD has their own strengths, abilities, and areas of growth. By promoting understanding and acceptance, we can create a supportive environment that celebrates the diversity within the autism community and ensures that every individual has the opportunity to reach their full potential.
FAQ
What is autism spectrum disorder (ASD)?
Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder that affects how people interact with others, communicate, learn, and behave. It is described as a "developmental disorder" because symptoms generally appear in the first 2 years of life.
What are the symptoms of autism spectrum disorder (ASD)?
The symptoms of autism spectrum disorder can vary widely, but they generally involve difficulties with social interaction, communication, and repetitive behaviors.
How is autism spectrum disorder (ASD) diagnosed?
Autism spectrum disorder is usually diagnosed through a two-stage process. The first stage involves general developmental screening during well-child checkups, which can help identify potential delays and determine if further evaluation is needed. The second stage involves additional diagnostic evaluation by a team of healthcare providers specializing in ASD.
How is autism spectrum disorder (ASD) treated?
Treatment for autism spectrum disorder is individualized and depends on the unique needs of each individual. It may involve a combination of interventions, therapies, and support services such as behavioral therapy, speech and language therapy, occupational therapy, and educational interventions.
What challenges do individuals with autism spectrum disorder (ASD) face?
Individuals with autism spectrum disorder often face challenges in various areas of life. They may struggle with social interaction, have difficulties in communication, experience learning difficulties, and may have sensory problems.
Are there any research and clinical trials for autism spectrum disorder (ASD)?
Ongoing research and clinical trials are essential for advancing our understanding of autism spectrum disorder and developing more effective treatments and interventions. Participating in research studies and clinical trials can provide individuals with ASD and their families with access to cutting-edge treatments and contribute to the advancement of knowledge in the field.
Can autism spectrum disorder (ASD) be cured?
While there is no cure for ASD, early intervention and appropriate support can significantly improve outcomes and quality of life for individuals with autism spectrum disorder.
Exploring the Causes of Autism: Insights & Research
Welcome to a comprehensive exploration of the causes of autism, where we delve into the latest insights and research surrounding this complex neurodevelopmental condition. Autism affects social interactions, communication skills, and behavior, posing unique challenges for individuals and their families. By understanding the underlying causes, we can enhance our ability to diagnose and treat autism effectively.
Research has shed light on various factors associated with autism, encompassing genetic variants, environmental influences, and neurological differences. These insights have paved the way for further investigation and have enabled us to develop more targeted approaches to diagnosis and intervention.
Throughout this article, we will explore the multifaceted aspects of autism, including the role of genetic factors, environmental influences, and neurological underpinnings. We will also examine the advances made in the diagnosis and treatment of autism, as well as the prevalence rates across different cultures. Additionally, we will discuss the importance of advocacy, public awareness, and the future of autism research and support.
Join us as we embark on this insightful journey, deepening our understanding of autism and paving the way for a more inclusive society for individuals with autism spectrum disorder.
Genetic Factors and Autism
Research has shown that genetic factors play a significant role in the development of autism spectrum disorder (ASD). Studies conducted by De Rubeis et al. (2014) have provided valuable insights into the genetic basis of autism. For example, research on twins has demonstrated a high heritability rate for ASD, indicating that genetic factors contribute to its occurrence. Concordance rates were found to be higher in identical twins compared to fraternal twins, further emphasizing the role of genetics in ASD.
In a study by Bernier et al. (2014), specific gene variants associated with autism were identified. These gene variants provide valuable clues about the biological mechanisms underlying autism and can also serve as potential targets for further research and personalized treatments.
To provide a better understanding of the genetic factors involved in autism, here is a table summarizing key findings from relevant studies:
| Study | Key Findings |
|---|---|
| De Rubeis et al. (2014) | High heritability rate for autism, concordance rates higher in identical twins. |
| Bernier et al. (2014) | Identification of specific gene variants associated with autism. |
Understanding the impact of genetic factors on autism is crucial for developing targeted interventions and personalized treatment strategies. Further research in this area will continue to deepen our understanding of the complex interplay between genetic variants and autism spectrum disorder.
Environmental Factors and Autism
Research has shown that environmental factors, in addition to genetic factors, can contribute to the development of autism spectrum disorder. Prenatal exposure to certain environmental influences has been associated with an increased risk of autism in children.
One significant environmental factor that has been studied is prenatal infections. Maternal infections during pregnancy, such as influenza, have been found to be linked to a higher likelihood of autism in the offspring. These infections can disrupt the delicate developmental processes in the brain, potentially leading to autism spectrum disorder.
Exposure to air pollutants is another environmental factor that has been identified as a potential risk factor for autism. Studies have found associations between exposure to substances like ozone and particulate matter and an increased risk of autism in children. It is believed that these pollutants can affect brain development and contribute to the manifestation of autism spectrum disorder.
Understanding the interaction between environmental factors and genetic vulnerabilities is essential for comprehending the complexity of autism. By recognizing and addressing these environmental influences, we can potentially reduce the risk and improve the lives of individuals with autism spectrum disorder.
To further illustrate the impact of environmental factors on autism, consider the following table:
| Environmental Factor | Associated Risk |
|---|---|
| Prenatal infections | Elevated likelihood of autism in offspring |
| Air pollutants | Higher risk of autism |
Gut Microbiome and Autism
Growing evidence suggests a potential link between imbalances in the gut microbiome and autism. The gut microbiome refers to the collection of microorganisms, including bacteria, fungi, and viruses, residing in the digestive tract.
Research studies have explored the role of the gut microbiome in autism spectrum disorder (ASD) and have found intriguing connections. Imbalances in the gut microbiota have been associated with gastrointestinal symptoms commonly experienced by individuals with autism, such as abdominal pain, constipation, and diarrhea. Furthermore, disturbances in the gut microbiome have been linked to the presence of autism-related behaviors, including social communication challenges and repetitive behaviors.
Microbiota transfer therapy (MTT), also known as fecal microbiota transplantation (FMT), has emerged as a potential treatment approach for individuals with autism. MTT involves transferring the gut microbiota from a healthy individual to a person with ASD, aiming to restore a healthy microbial balance. Preliminary studies have shown promising results, including improvements in gastrointestinal symptoms and behavioral outcomes.
The Gut-Brain Connection
One theory suggests that the communication between the gut and the brain, known as the gut-brain axis, plays a significant role in the development and manifestation of autism. The gut microbiome influences various aspects of brain function, including neurotransmitter production and inflammation regulation. Imbalances in the gut microbiota may disrupt this delicate balance and contribute to the neurological differences observed in individuals with autism.
Recent research has highlighted the potential interaction between genes and the gut microbiome in autism. Studies have identified specific gene variations that affect the composition and diversity of the gut microbiota. These findings highlight the complex interplay between genetic factors and the gut microbiome in autism development.
The Role of Diet and Probiotics
Investigations into the gut microbiome and autism have also explored the impact of diet on gut health and autism-related symptoms. Certain dietary interventions, such as eliminating gluten and casein or following a specific carbohydrate diet (SCD), have shown potential benefits in reducing gastrointestinal problems and improving behavior in some individuals with autism.
Probiotics, which are beneficial bacteria, have been studied for their potential to restore a healthy gut microbiome and alleviate autism-related symptoms. Research on the effectiveness of probiotics in autism is ongoing, with some studies suggesting positive outcomes in areas such as social interaction, communication, and repetitive behaviors.
| The Gut Microbiome and Autism | Key Findings |
|---|---|
| Imbalances in the gut microbiome | Associated with gastrointestinal symptoms and autism-related behaviors |
| Microbiota Transfer Therapy (MTT) | Shows potential in improving gastrointestinal symptoms and behavioral outcomes |
| Gut-brain axis | Contributes to the communication between the gut and the brain, influencing autism development |
| Diet and probiotics | Play a role in supporting a healthy gut microbiome and reducing autism-related symptoms |
Neurological Factors and Autism
Investigations into neurological factors associated with autism have revealed interesting findings. Neurological differences play a crucial role in the development of autism spectrum disorder (ASD), contributing to the characteristic symptoms and challenges faced by individuals on the autism spectrum.
One intriguing aspect is the potential impact of myelin integrity on autism. Myelin, a protective sheath surrounding nerve cells, is essential for efficient communication between neurons. Studies have shown that individuals with autism often exhibit a decrease in myelin integrity, which may disrupt brain development and impair neural connectivity.
Research is ongoing to understand the precise mechanisms underlying this malfunction in myelin production and its relationship to autism. By exploring neurological factors, scientists hope to uncover ways to enhance myelination and improve autism-associated behaviors.
Furthermore, other neurological factors such as atypical brain connectivity patterns and alterations in brain structure have also been observed in individuals with ASD. These factors contribute to the unique cognitive and behavioral characteristics of autism.
A better understanding of the neurological factors associated with autism holds promise for the development of targeted interventions and treatments. By addressing the root causes, researchers aim to enhance the overall well-being and quality of life for individuals with autism spectrum disorder.
Advances in Diagnosis and Biomarkers
Early diagnosis is crucial for effectively managing autism spectrum disorder (ASD). Researchers are making significant strides in developing innovative diagnostic methods and identifying biomarkers that can aid in early detection. These advancements have the potential to greatly improve outcomes for individuals with autism.
Diagnostic Methods
One promising diagnostic method being explored is the use of auditory brainstem response (ABR) hearing tests. These tests measure the brain's electrical activity in response to sound, allowing clinicians to assess auditory processing and identify potential signs of autism. ABR testing shows promise in detecting early indicators of ASD, enabling early intervention and targeted therapies.
Biomarkers and Metabotypes
Another area of research focuses on identifying biomarkers and metabotypes associated with autism. Biomarkers are measurable indicators in the body that can signify the presence or progression of a disorder. Metabotypes, on the other hand, are unique metabolic profiles observed in individuals with autism.
By identifying specific biomarkers and metabotypes, researchers aim to develop screening tests that can aid in early diagnosis and intervention. These tests could be non-invasive and easy to administer, enabling healthcare professionals and parents to identify potential signs of autism at an early stage. Early identification and intervention can lead to more effective treatment strategies and improved long-term outcomes for individuals with autism.
| Biomarker | Significance |
|---|---|
| Metabolic alterations | Associated with autism spectrum disorder |
| Neurotransmitter imbalances | Potential biomarkers for autism |
| Oxidative stress markers | Implicated in the pathogenesis of autism |
| Immune system dysregulation | Linked to autism spectrum disorder |
*Please note that the table above provides examples and is not an exhaustive list of biomarkers associated with autism.
These advancements in diagnosis and the identification of biomarkers offer hope for improved understanding, early intervention, and personalized treatment for individuals with autism. Continued research in this field will pave the way for a more comprehensive and accurate diagnostic process, providing individuals with autism the support they need to thrive.
Evolution of Understanding and Treatment Approaches
The understanding of autism has evolved significantly over time. From early misconceptions and the false "refrigerator mother" theory to current neurological and genetic perspectives, our understanding of autism has become more nuanced.
Treatment approaches for autism have also progressed, aiming to improve the quality of life for individuals with autism. One commonly used approach is Applied Behavioral Analysis (ABA), which focuses on reinforcing positive behaviors and reducing challenging ones. ABA interventions can be tailored to address specific goals, such as improving communication skills or reducing repetitive behaviors.
In addition to ABA, holistic therapies have gained recognition as complementary treatment options for autism. These therapies take into account the individual's overall well-being, including their physical, emotional, and social needs. Examples of holistic approaches include art therapy, music therapy, and sensory integration therapy.
The neurodiversity movement has played a significant role in changing societal perceptions of autism. This movement emphasizes the acceptance and inclusion of neurodiverse individuals, recognizing autism as a natural variation of human neurology rather than a disorder to be cured. By embracing the principles of neurodiversity, society can create a more inclusive environment that celebrates the unique strengths and perspectives of individuals with autism.
History of Autism
The history of autism dates back to the early 20th century when it was first recognized as a distinct condition. In 1943, psychiatrist Leo Kanner published a groundbreaking paper describing a group of children with unique social and communication difficulties. This marked the beginning of autism research and the identification of autism as a separate condition.
In the 1960s and 1970s, a controversial theory known as the "refrigerator mother" theory emerged, suggesting that autism was caused by emotional coldness and lack of maternal warmth. This theory has since been discredited, and it is now widely understood that autism has a complex interplay of genetic, environmental, and neurological factors.
Over the years, advancements in research have deepened our understanding of autism. Genetic studies have identified specific gene variants associated with autism, providing insights into the underlying biology of the condition. Neurological research has revealed differences in brain structure and connectivity in individuals with autism, further contributing to our understanding of the condition.
It is important to note that the history of autism is marked by changing diagnostic criteria and evolving terminology. The diagnostic criteria for autism have undergone revisions, leading to changes in how autism is diagnosed and classified. The most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes the diagnosis of Autism Spectrum Disorder (ASD) as a single category encompassing various levels of symptom severity.
Treatment Approaches
Over the years, various treatment approaches have been developed to support individuals with autism. These approaches aim to address the core symptoms of autism, such as social and communication challenges, and enhance overall functioning and quality of life.
Applied Behavioral Analysis (ABA) is one of the most widely used and researched treatment approaches for autism. ABA focuses on using positive reinforcement to teach and encourage desired behaviors while reducing challenging ones. This approach is often utilized in early intervention programs and can be highly individualized to meet the specific needs of each person with autism.
Holistic therapies have also gained popularity as complementary treatments for autism. These therapies take a comprehensive approach, considering the physical, emotional, and social well-being of individuals with autism. Examples of holistic therapies include art therapy, music therapy, animal-assisted therapy, and sensory integration therapy. These approaches often aim to improve sensory integration, emotional regulation, and social skills.
Table: Comparative Overview of Treatment Approaches
| Treatment Approach | Description | Benefits |
|---|---|---|
| Applied Behavioral Analysis (ABA) | Uses behavioral principles to teach and reinforce desired skills while reducing challenging behaviors. | Individualized interventions, measurable outcomes, evidence-based. |
| Speech-Language Therapy | Targets communication and language skills, including speech production, comprehension, and social communication. | Improves communication abilities, enhances social interactions. |
| Occupational Therapy | Helps individuals develop skills for daily living, fine motor coordination, sensory processing, and self-regulation. | Enhances independent living, sensory integration, self-care abilities. |
| Physical Therapy | Focuses on improving physical mobility, coordination, balance, and strength through therapeutic exercises. | Enhances motor skills, promotes physical fitness. |
While there is no cure for autism, early intervention and appropriate treatment can significantly improve outcomes for individuals with autism. The effectiveness of treatment approaches may vary depending on individual needs and preferences. It is important for caregivers and professionals to work together to develop personalized treatment plans that address the unique strengths and challenges of each individual with autism.
Prevalence and Cultural Perspectives of Autism
Autism prevalence rates vary globally, influenced by a combination of genetic and environmental factors, as well as cultural perspectives and diagnostic criteria. It is important to consider the impact of cultural differences on the diagnosis and perception of autism, as they can contribute to underdiagnosis or misdiagnosis in certain societies. A deeper understanding of cultural influences is crucial for ensuring accurate diagnosis and providing appropriate support for individuals with autism.
In some cultural contexts, the characteristics associated with autism may be perceived differently or interpreted as normal behavior, leading to challenges in recognizing and addressing the condition. Cultural beliefs, attitudes, and social norms surrounding developmental differences and disabilities can significantly impact the identification and acceptance of autism.
For example, in some societies where collective harmony and conformity are emphasized, individuals with autism may be expected to conform to social norms, leading to their differences being overlooked or misunderstood. Additionally, cultural stigmas and misconceptions surrounding autism can further contribute to underdiagnosis and hinder access to necessary resources and support.
To address the underdiagnosis of autism in different cultural contexts, it is essential to promote cross-cultural awareness, knowledge, and sensitivity among healthcare professionals, educators, and communities. By recognizing and valuing diverse cultural perspectives, we can improve early identification and interventions for individuals with autism, ensuring that their unique needs are met.
Challenges in Cultural Assessment and Diagnosis
Cultural perspectives play a significant role in shaping autism diagnosis, evaluation, and treatment, as they influence the interpretation and understanding of developmental differences. However, cultural biases and stereotypes can pose challenges in accurately assessing and diagnosing autism.
- Cultural variations in the expression of autism symptoms: The presentation and severity of autism symptoms may vary across cultures, making it crucial to account for cultural differences when evaluating individuals.
- Language barriers: Language differences can impact the assessment process, as communication difficulties associated with autism may be mistaken for language barriers. Culturally sensitive assessments should consider the use of interpreters or culturally relevant communication tools.
- Stigma and cultural beliefs: Cultural stigmas associated with disabilities, including autism, can hinder disclosure and awareness of developmental differences. Addressing these stigmas and fostering open dialogue is essential for accurate diagnosis and support.
Promoting Cultural Understanding and Inclusive Practices
Improving cultural competence and inclusivity in autism diagnosis and support requires collaboration and education at multiple levels. Here are some strategies to promote cultural understanding and ensure equitable access to services:
- Training healthcare professionals and educators: Providing training on cultural competence and autism in diverse cultural contexts equips professionals with the knowledge and skills necessary to recognize and address the unique needs of individuals with autism.
- Engaging with multicultural communities: Building partnerships with cultural and community organizations can help increase awareness, reduce stigma, and facilitate outreach efforts in underserved communities.
- Developing culturally sensitive assessment tools: The development of assessment tools that consider cultural variations in the presentation of autism symptoms can improve diagnostic accuracy and reduce underdiagnosis.
- Promoting inclusive practices in education: Creating inclusive learning environments that embrace diverse cultural perspectives fosters acceptance and understanding of individuals with autism.
Awareness and understanding of both the prevalence and cultural perspectives of autism are vital for ensuring accurate diagnosis, appropriate support, and inclusive practices. By acknowledging and addressing cultural influences, we can create a society that celebrates and supports the diverse experiences of individuals with autism.
Advocacy and Public Awareness
Advocacy groups play a vital role in promoting autism advocacy and raising public awareness about autism spectrum disorder. These organizations, such as Autism Speaks and the Autism Society, work tirelessly to advocate for the rights and needs of individuals with autism. By organizing events, launching campaigns, and providing resources, these groups ensure that the voices of the autism community are heard.
One powerful way of increasing public awareness about autism is through the medium of film. One notable example is the movie "Rain Man," which depicted the unique perspective and challenges faced by individuals with autism. This critically acclaimed film helped bring autism into the mainstream consciousness and fostered greater understanding among the general public.
Another symbol that has become synonymous with autism advocacy and awareness is the Autism Awareness Puzzle Ribbon. This iconic symbol represents the complexity and diversity of individuals with autism and serves as a powerful reminder to embrace neurodiversity. By wearing the Autism Awareness Puzzle Ribbon, individuals show their support and solidarity with the autism community.
Furthermore, the neurodiversity movement has emerged as a powerful force in autism advocacy. This movement, driven by self-advocacy, aims to shift the focus from seeing autism as a disorder that needs to be cured to recognizing and celebrating the unique strengths and perspectives of individuals on the autism spectrum. The neurodiversity movement advocates for acceptance, inclusion, and the right to be treated with respect and dignity.

| Advocacy Groups | Mission |
|---|---|
| Autism Speaks | To promote solutions, across the spectrum and throughout the life span, for the needs of individuals with autism and their families through advocacy and support, increasing understanding and acceptance of people with autism, and advancing research into causes and better interventions for autism spectrum disorder. |
| Autism Society | To promote lifelong access and opportunities for persons within the autism spectrum and their families to be fully included, participating members of their communities through advocacy, public awareness, education, and support. |
The Future of Autism Research and Support
Ongoing research in the field of autism aims to uncover new insights into the causes, diagnosis, and treatment of this complex condition. As our understanding of autism deepens, exciting advancements in genetic analysis, neurological studies, and biomarker identification pave the way for personalized treatment approaches.
With advancements in technology, researchers can now analyze genetic variations and identify specific markers associated with autism spectrum disorder (ASD). This research not only enables accurate diagnosis but also opens doors to targeted therapies tailored to the unique needs of individuals with autism.
Neurological studies have provided valuable insights into the intricacies of brain functions in individuals with autism. Through advanced imaging techniques, researchers have observed structural and functional differences that contribute to the challenges experienced by individuals with ASD. These findings aid in the development of innovative treatment strategies focused on enhancing brain connectivity and improving social and communication skills.
Personalized Treatment Approaches
The future of autism research is centered around personalized treatment approaches that take into account the unique characteristics of each individual with autism. By considering factors such as genetics, neurological profiles, and co-occurring conditions, researchers and healthcare professionals can develop tailored interventions that address specific challenges and promote optimal development and well-being.
Implementing personalized treatment approaches involves a multidisciplinary approach, with collaboration between healthcare providers, therapists, educators, and caregivers. This holistic approach aims to create a comprehensive support system that addresses the diverse needs of individuals with ASD and helps them reach their full potential.
Creating an Inclusive Society
Building an inclusive society is crucial for supporting individuals with autism and ensuring they have equal access to opportunities, resources, and acceptance. It requires the collective efforts of policymakers, communities, and individuals to create an environment that embraces neurodiversity and values the unique contributions of individuals with autism.
An inclusive society promotes understanding, empathy, and accommodates the diverse needs of individuals with autism. Through education, awareness campaigns, and advocacy, we can challenge stigmas, promote acceptance, and foster a sense of belonging for individuals with autism.
The Role of Future Research, Advocacy, and Policy Changes
The future of autism research and support lies in continued exploration, discovery, and implementation of evidence-based practices. Ongoing research efforts focusing on the genetic, environmental, and neurological aspects of autism will provide further insights, leading to advancements in early detection, intervention, and improved outcomes for individuals with ASD.
Advocacy plays a vital role in raising public awareness, generating research funding, and driving policy changes to ensure individuals with autism receive the support they need. By amplifying the voices of individuals with ASD and their families, we can drive societal change and create a more inclusive and supportive environment.
In conclusion, the future of autism research and support holds great promise. Through personalized treatment approaches, an inclusive society, and the continued dedication of researchers, advocates, and policymakers, we can enhance the lives of individuals with autism and create a more inclusive and compassionate world.
Conclusion
In conclusion, autism spectrum disorder (ASD) is a complex condition influenced by a combination of genetic, environmental, and neurological factors. The advancements in research have significantly deepened our understanding of autism, improving our ability to diagnose and treat individuals with ASD.
However, beyond diagnosis and treatment, it is crucial to foster societal acceptance, support, and inclusion for individuals with autism. Embracing the principles of neurodiversity, we must recognize the unique strengths and challenges of individuals with autism and create an inclusive society that celebrates their diversity.
Continued research, advocacy, and education are essential in further advancing our understanding of autism and developing effective support systems. By investing in resources and initiatives that promote awareness, acceptance, and accessibility, we can create a more inclusive world for individuals with autism and their families.
FAQ
What are the causes of autism?
Autism is influenced by a combination of genetic, environmental, and neurological factors. Genetic variants, environmental exposures, and differences in brain development all contribute to the development of autism.
Do genetics play a role in autism?
Yes, research has shown that genetic factors play a significant role in the development of autism. Studies on twins have revealed a high heritability rate for autism, and the identification of specific gene variants has further contributed to our understanding of the genetic basis of autism.
What environmental factors are associated with autism?
Environmental factors such as prenatal infections, exposure to toxins, and air pollution have been linked to an increased risk of autism. Maternal infections during pregnancy, like influenza, and exposure to air pollutants like ozone and particulate matter, have been found to be associated with a higher likelihood of autism in offspring.
How does the gut microbiome relate to autism?
Growing evidence suggests a potential link between imbalances in the gut microbiome and autism. Studies have shown that balancing the populations of gut microbes can lead to improvements in gastrointestinal symptoms and autism-related behaviors. There is also a connection between genes and the gut microbiome, highlighting the role of the microbiome in autism development.
What neurological factors are associated with autism?
Studies have shown a decrease in the integrity of myelin, a protective sheath surrounding nerve cells, in individuals with autism. This malfunction in myelin production may disrupt brain development and impair communication between nerve cells, contributing to the characteristic symptoms of autism.
Are there advancements in autism diagnosis?
Yes, researchers are exploring innovative diagnostic methods for autism, such as auditory brainstem response (ABR) hearing tests and the identification of metabotypes associated with autism. These advancements have the potential to provide earlier and more accurate diagnosis of autism.
How has the understanding and treatment of autism evolved?
Our understanding of autism has evolved significantly over time, from early misconceptions to current neurological and genetic perspectives. Treatment approaches, such as Applied Behavioral Analysis (ABA) and holistic therapies, aim to improve the quality of life for individuals with autism. The neurodiversity movement has also contributed to changing societal perceptions and promoting acceptance and inclusion of neurodiversity.
How prevalent is autism, and how is it perceived in different cultures?
Prevalence rates of autism vary globally, influenced by genetic and environmental factors, as well as cultural perspectives and diagnostic criteria. Cultural differences can impact the diagnosis and perception of autism, leading to underdiagnosis or misdiagnosis in certain societies. Awareness and understanding of cultural influences are essential for accurate diagnosis and appropriate support.
What role do advocacy groups play in supporting individuals with autism?
Advocacy groups such as Autism Speaks and the Autism Society play key roles in raising awareness, promoting research funding, and advocating for the rights and needs of individuals with autism. Films like "Rain Man" and symbols like the Autism Awareness Puzzle Ribbon have also contributed to increased public awareness.
What does the future hold for autism research and support?
Ongoing research aims to uncover further insights into the causes, diagnosis, and treatment of autism. Advances in genetic analysis, neurological studies, and biomarker identification hold promise for personalized treatment approaches. Creating an inclusive society that supports the unique needs and strengths of individuals with autism is a collective responsibility.
Spinocerebellar Ataxia Treatment Options
If you or a loved one are living with spinocerebellar ataxia, you may be wondering about the available treatment options to manage its symptoms. While there is no cure for this progressive neurological condition, there are strategies that can help improve your quality of life.
In this article, we will explore different treatment options for spinocerebellar ataxia and discuss how they can assist in managing symptoms. From medications to therapies and adaptive devices, there are various approaches that can be tailored to your specific needs.
Discover the possibilities for managing spinocerebellar ataxia and find the support you need to navigate this condition. Let's delve into the treatment options available for spinocerebellar ataxia and empower you to take control of your health.
Understanding Spinocerebellar Ataxia
Spinocerebellar ataxia is a group of genetic disorders characterized by the degeneration of the cerebellum and its connections. It can be caused by various genetic mutations and inheritance patterns. The symptoms of spinocerebellar ataxia include difficulties with balance and coordination, unsteady gait, speech difficulties, and involuntary eye movements.
Spinocerebellar ataxia is a complex condition that affects the central nervous system, specifically the cerebellum. The cerebellum plays a crucial role in coordinating movement and balance. When the cerebellum degenerates, it disrupts the communication between the brain and the muscles, leading to the symptoms of ataxia.
There are different types of spinocerebellar ataxia, each associated with a specific genetic mutation. The inheritance of spinocerebellar ataxia can be autosomal dominant, autosomal recessive, or X-linked. In autosomal dominant inheritance, a child has a 50% chance of inheriting the mutated gene if one of the parents carries it. Autosomal recessive inheritance requires both parents to be carriers of the mutated gene, resulting in a 25% chance of a child inheriting the condition. X-linked inheritance affects males more frequently, as the mutation occurs on the X chromosome.
Symptoms of Spinocerebellar Ataxia
The symptoms of spinocerebellar ataxia can vary depending on the type of genetic mutation and the progression of the disease. Common symptoms include:
- Difficulties with balance and coordination, leading to unsteady movements
- Speech difficulties, such as slurred or slow speech
- Involuntary eye movements, including jerking or difficulty focusing
- Muscle stiffness and rigidity
- Tremors or shaking
As spinocerebellar ataxia progresses, these symptoms may worsen and impact daily activities, making it difficult to perform tasks such as walking, writing, and speaking.
Causes of Spinocerebellar Ataxia
Spinocerebellar ataxia is primarily caused by genetic mutations that affect the structure and function of the cerebellum. These mutations can occur in different genes, resulting in different types of spinocerebellar ataxia.
The specific genes involved in spinocerebellar ataxia vary depending on the type of the condition. For example, spinocerebellar ataxia type 1 is caused by a mutation in the ATXN1 gene, while spinocerebellar ataxia type 3 is caused by a mutation in the ATXN3 gene.
Research is ongoing to better understand the molecular mechanisms underlying spinocerebellar ataxia and to identify potential targets for treatment and intervention.
| Type of Spinocerebellar Ataxia | Associated Gene Mutation | Inheritance Pattern |
|---|---|---|
| Spinocerebellar ataxia type 1 | ATXN1 | Autosomal dominant |
| Spinocerebellar ataxia type 2 | ATXN2 | Autosomal dominant |
| Spinocerebellar ataxia type 3 | ATXN3 | Autosomal dominant |
| Spinocerebellar ataxia type 6 | CACNA1A | Autosomal dominant |
| Spinocerebellar ataxia type 7 | ATXN7 | Autosomal dominant |
| Spinocerebellar ataxia type 10 | ATXN10 | Autosomal dominant |
This table provides an overview of some common types of spinocerebellar ataxia and their associated gene mutations and inheritance patterns.
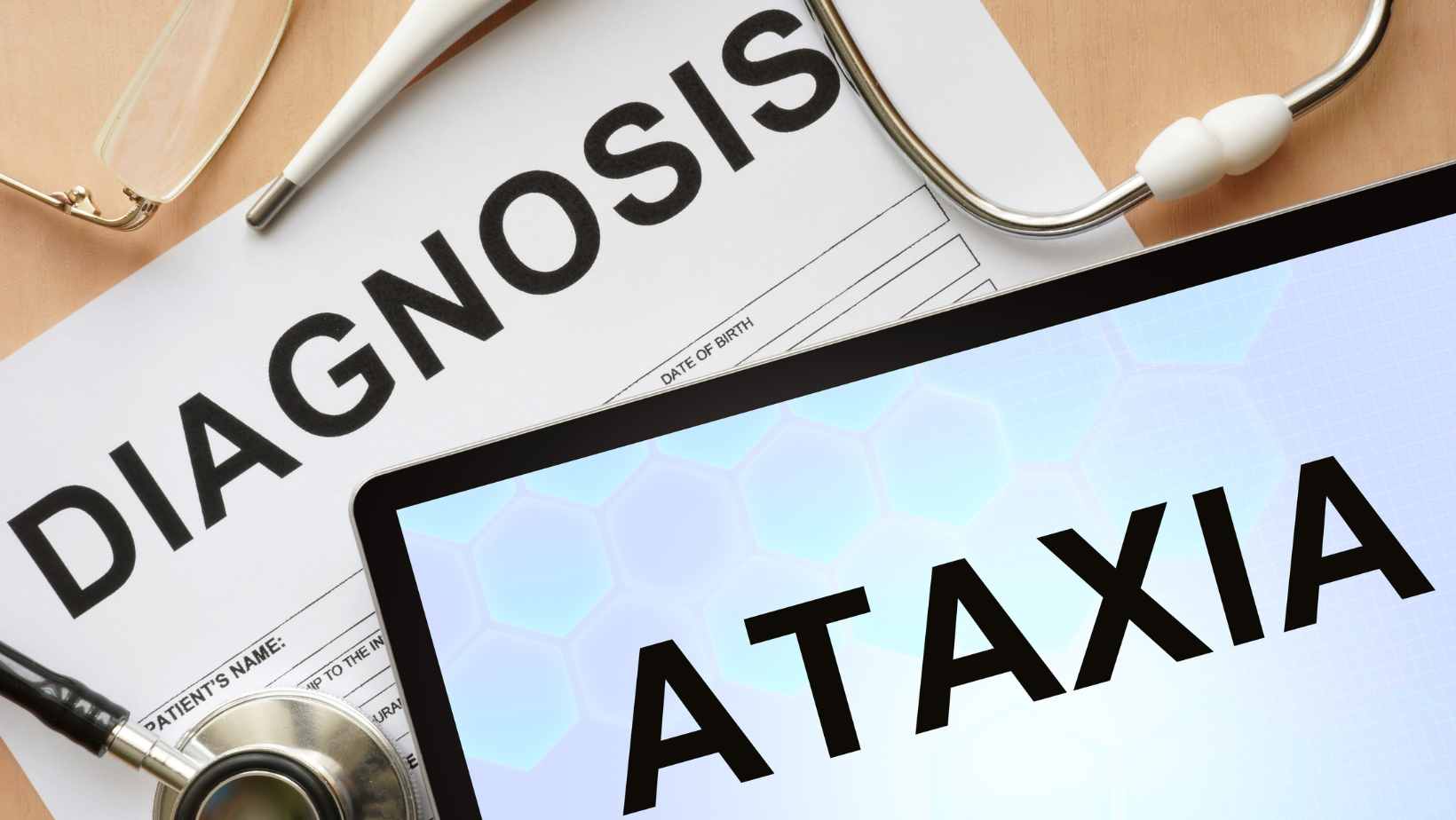
Diagnosing Spinocerebellar Ataxia
Diagnosing spinocerebellar ataxia involves a comprehensive evaluation conducted by healthcare professionals. The process typically begins with a thorough physical and neurological examination. During the examination, your doctor will assess your coordination, balance, reflexes, and muscle strength.
To further investigate the condition and rule out other potential causes, additional diagnostic tests may be conducted. These tests can help identify any underlying factors contributing to the development of spinocerebellar ataxia and provide a more accurate diagnosis. Some common diagnostic tests for spinocerebellar ataxia include:
- Blood tests: Blood tests can help determine if there are any abnormalities in your blood that may be associated with spinocerebellar ataxia. These tests can detect specific genetic mutations, assess the functioning of different organs, and evaluate nutrient levels.
- Imaging studies: Imaging studies, such as magnetic resonance imaging (MRI), may be conducted to examine the brain and spinal cord for any structural abnormalities or changes. This can help identify any areas of degeneration in the cerebellum and its connections.
- Genetic testing: Genetic testing is an essential component of diagnosing spinocerebellar ataxia. It involves analyzing your DNA to identify specific genetic mutations associated with spinocerebellar ataxia. This test can help determine the specific type of spinocerebellar ataxia you have and provide valuable information for personalized treatment decisions.
Genetic testing plays a crucial role in understanding the inheritance pattern of spinocerebellar ataxia as well. It helps determine if the condition is inherited and whether you may pass it on to your children.
It's important to note that diagnosing spinocerebellar ataxia can be complex due to the wide range of genetic mutations and the similar symptoms it shares with other neurological disorders. Therefore, a multidisciplinary approach involving specialized healthcare professionals, such as neurologists and geneticists, is often necessary.
| Diagnostic Tests for Spinocerebellar Ataxia | Purpose |
|---|---|
| Blood tests | To detect genetic mutations, assess organ functioning, and evaluate nutrient levels |
| Imaging studies (MRI) | To examine the brain and spinal cord for structural abnormalities or changes |
| Genetic testing | To analyze DNA and identify specific genetic mutations associated with spinocerebellar ataxia |
By utilizing these diagnostic tools, healthcare professionals can accurately diagnose spinocerebellar ataxia and provide personalized treatment plans based on your specific condition and needs.
Treatable Causes of Spinocerebellar Ataxia
In some cases, spinocerebellar ataxia may be caused by treatable underlying conditions. Identifying and addressing these causes can lead to improvements in symptoms and the overall management of ataxia. Some of the treatable causes of spinocerebellar ataxia include:
Vitamin Deficiencies
Vitamin deficiencies, such as deficiencies in vitamins E, B12, and thiamine, can contribute to the development or worsening of spinocerebellar ataxia. Ensuring an adequate intake of these vitamins or receiving supplements under medical supervision can help improve symptoms and promote overall neurological health.
Infections
Certain infections, such as Lyme disease or viral infections like human immunodeficiency virus (HIV) and Epstein-Barr virus (EBV), can also trigger or exacerbate spinocerebellar ataxia. Prompt and appropriate treatment of these infections can potentially reverse or slow down the progression of ataxia.
Medications
Some medications, known as ototoxic drugs, have been associated with secondary ataxia. These medications may include certain antibiotics, antiepileptic drugs, and some types of chemotherapy. If medication-induced ataxia is suspected, consultation with a healthcare professional is essential to assess the potential for changing or adjusting medications.
Metabolic Disorders
Metabolic disorders, such as Wilson's disease or thiamine-responsive megaloblastic anemia, can present with ataxia as a symptom. Prompt diagnosis and appropriate management of these underlying metabolic conditions are crucial in preventing further complications and optimizing outcomes for individuals with spinocerebellar ataxia.
Autoimmune Conditions
Some autoimmune conditions, including gluten ataxia and paraneoplastic cerebellar degeneration, can cause secondary ataxia. Identifying and effectively managing these autoimmune conditions through medication and lifestyle modifications can potentially improve ataxia symptoms.
It is important to note that the specific treatment approach will depend on the underlying cause identified through thorough diagnostic evaluations. Proper medical assessment by a healthcare professional is essential to determine the appropriate course of action for individuals with spinocerebellar ataxia.
| Treatable Causes of Spinocerebellar Ataxia | Description |
|---|---|
| Vitamin Deficiencies | Deficiencies in vitamins E, B12, and thiamine |
| Infections | Infections like Lyme disease, HIV, and EBV |
| Medications | Use of certain ototoxic drugs |
| Metabolic Disorders | Underlying metabolic conditions like Wilson's disease |
| Autoimmune Conditions | Autoimmune conditions such as gluten ataxia |
Medications for Spinocerebellar Ataxia
If you have been diagnosed with spinocerebellar ataxia, there are medications available that can help manage your symptoms and improve your quality of life. One such medication is riluzole. This drug has shown promising results in improving functional measures in SCA patients. It works by reducing the excitotoxicity caused by the excessive release of glutamate in the brain.
| Medication | Uses | Potential Benefits |
|---|---|---|
| Riluzole | Reduces glutamate toxicity | Improvement in functional measures |
| Varenicline | Nicotinic receptor agonist | Potential improvement in ataxic symptoms |
| Buspirone | Anxiolytic and anti-depressant | Potential improvement in ataxic symptoms |
It is important to note that the effectiveness of these medications may vary from person to person, and they may not be suitable for everyone. Your healthcare provider will consider your individual circumstances and medical history before recommending any specific medication. It is always recommended to consult with a healthcare professional for guidance on the most appropriate drug treatments for your spinocerebellar ataxia.

Therapies for Spinocerebellar Ataxia
In addition to medications, various therapies can help individuals with spinocerebellar ataxia manage their symptoms and improve their quality of life. Physical therapy, occupational therapy, and speech therapy are commonly used to address the specific needs of individuals with spinocerebellar ataxia.
Physical Therapy for Spinocerebellar Ataxia
Physical therapy plays a crucial role in the management of spinocerebellar ataxia. It focuses on improving balance, coordination, and muscle strength through tailored exercises and rehabilitation techniques. A physical therapist will work closely with you to design a personalized exercise program that targets your specific needs and helps optimize your physical function.
Occupational Therapy for Spinocerebellar Ataxia
Occupational therapy is aimed at helping individuals with spinocerebellar ataxia maintain their independence in daily living activities. An occupational therapist will assess your functional abilities and develop strategies to enhance your ability to perform self-care tasks, such as dressing, feeding, and bathing. They may also recommend adaptive equipment and modifications to your home environment to maximize safety and accessibility.
Speech Therapy for Spinocerebellar Ataxia
Speech and swallowing difficulties are common symptoms of spinocerebellar ataxia. Speech therapy can help improve communication skills, enhance speech clarity, and address swallowing difficulties. A speech therapist will provide specialized exercises and techniques to strengthen the muscles involved in speech production and swallowing, enabling you to communicate more effectively and reduce the risk of aspiration.
| Therapy Type | Goals | Benefits |
|---|---|---|
| Physical Therapy | Improve balance, coordination, and muscle strength | Enhanced physical function and reduced fall risk |
| Occupational Therapy | Enhance independence in daily living activities | Improved quality of life and increased self-reliance |
| Speech Therapy | Improve speech clarity and swallowing function | Effective communication and reduced risk of aspiration |
Adaptive Devices and Assistive Technology
Adaptive devices and assistive technology are invaluable tools for individuals with spinocerebellar ataxia, offering support and enhancing their ability to carry out daily activities. These devices are designed to compensate for the limitations caused by ataxia, promoting independence and improving overall quality of life.
Examples of Adaptive Devices
There are various adaptive devices available that cater to different needs specific to spinocerebellar ataxia. Here are some examples:
- Walking aids: Mobility aids such as canes, walkers, and rollators provide stability and support while walking, reducing the risk of falls and promoting safe movement.
- Modified utensils: Eating can be challenging for individuals with ataxia due to impaired hand control and coordination. Specialized utensils with ergonomic handles or custom grips can make self-feeding easier and more manageable.
- Communication aids: Ataxia can affect speech and communication. Augmentative and alternative communication (AAC) devices, such as speech-generating devices or communication apps, enable individuals to express themselves effectively and engage in conversations.
These adaptive devices are designed to accommodate the specific needs and challenges faced by individuals with spinocerebellar ataxia, enabling them to maintain their independence and participate actively in daily life.
Assistive Technology for Spinocerebellar Ataxia
Assistive technology offers a wide range of tools and devices that aid individuals with ataxia in performing specific tasks. These technologies are designed to compensate for motor and functional impairments, facilitating greater accessibility and inclusivity.
Some examples of assistive technology for spinocerebellar ataxia include:
- Voice-activated smart devices: Artificial intelligence-powered voice assistants, such as Amazon Echo or Google Home, can be programmed to control various home devices, make phone calls, set reminders, and perform other tasks with voice commands, reducing the reliance on manual interaction.
- Smart home automation systems: These systems integrate and automate various household functions, such as lighting, temperature control, and security, allowing individuals to control their environment more easily using voice commands or mobile applications.
- Computer accessibility software: Software programs like voice recognition software, screen reading software, and adaptive keyboards can enable individuals with ataxia to navigate computers, access the internet, and perform tasks efficiently.
Assistive technology empowers individuals with ataxia to overcome barriers and actively participate in various aspects of life. It enhances their ability to communicate, perform tasks, and access information, fostering independence and promoting a higher level of engagement.
| Benefits of Adaptive Devices and Assistive Technology | Benefits of Adaptive Devices and Assistive Technology |
|---|---|
| Enhanced mobility and independence | Improved communication and social interaction |
| Increased safety and reduced risk of falls | Greater access to information and resources |
| Facilitates participation in daily activities | Enhanced productivity and task performance |
| Promotes overall well-being and quality of life | Ensures inclusivity and equal opportunities |
Clinical Trials and Experimental Treatments
Researchers are constantly exploring new treatment options for spinocerebellar ataxia through clinical trials and experimental therapies. These trials investigate the safety and efficacy of novel medications, gene therapies, and other interventions. Participating in clinical trials can provide access to potentially groundbreaking treatments.
Clinical trials serve as a vital platform for evaluating the effectiveness of innovative approaches in managing spinocerebellar ataxia. These trials involve rigorous testing to ensure the safety of experimental treatments and gather data about their potential benefits. By participating in clinical trials, you have the opportunity to contribute to the advancement of research and gain access to cutting-edge therapies that may not yet be available to the general public.
Experimental treatments for spinocerebellar ataxia may include gene therapies aimed at targeting specific genetic mutations responsible for the condition. These therapies involve the delivery of modified genes to correct or compensate for the underlying genetic defect. While they are still in the investigational stage, gene therapies hold great promise in addressing the root cause of spinocerebellar ataxia.
In addition to gene therapies, other investigational therapies for spinocerebellar ataxia encompass a wide range of innovative approaches. These may involve targeting specific molecules or pathways in the brain to modulate or slow down the progression of the disease. Experimental medications, neuroprotective agents, and stem cell therapies are among the avenues being explored to develop more effective treatments.
It's important to note that participation in clinical trials is entirely voluntary, and each trial has specific eligibility criteria. Before considering participation, it's advisable to consult with your healthcare provider to understand the potential risks and benefits associated with a particular trial. Your healthcare provider can guide you in exploring the available clinical trial options and help you make an informed decision.
Coping with Spinocerebellar Ataxia
Living with spinocerebellar ataxia can be challenging, both for individuals with the condition and their loved ones. Fortunately, there are various ways to cope with the emotional and physical aspects of the disease. Seeking support through counseling or joining support groups can provide a valuable outlet for sharing experiences and receiving guidance from others who understand what you're going through.
Emotional support is crucial in managing the mental health impact of spinocerebellar ataxia. It's normal to experience a range of emotions, including frustration, sadness, and anxiety. Speaking with a therapist or counselor who specializes in neurological conditions can help you navigate these emotions and develop coping strategies.
Support groups can also offer a sense of community and connection. Interacting with individuals who share similar experiences can provide a space to share tips, insights, and encouragement. It can be empowering to learn from others who have successfully navigated the challenges of spinocerebellar ataxia.
Lifestyle Modifications for Spinocerebellar Ataxia
In addition to emotional support, making certain lifestyle modifications can enhance your overall well-being when living with spinocerebellar ataxia.
Maintaining a healthy diet: Eating a nutritious diet can help support your energy levels and overall health. A diet rich in fruits, vegetables, whole grains, and lean proteins can provide essential nutrients and promote optimal well-being. Consult a registered dietitian who can help tailor a diet plan specific to your needs.
Staying active: Engaging in regular physical activity, within the limits of your abilities, can have numerous benefits. Exercise can help improve balance, coordination, and muscle strength. Consult a physical therapist who can develop a personalized exercise plan that takes into consideration your individual needs and capabilities.
Adapting your environment: Making modifications to your home environment can help optimize your safety and mobility. Removing obstacles, installing handrails, and adding nonslip surfaces can help prevent falls and minimize accidents.
Assistive devices: Utilizing assistive devices can support your independence and make daily tasks easier. Walking aids, such as canes or walkers, can provide stability and improved mobility. Modified utensils and adaptive equipment can assist with tasks like eating, dressing, and bathing.
By incorporating these lifestyle modifications and seeking the right support, you can enhance your quality of life while coping with spinocerebellar ataxia.

Future Directions in Spinocerebellar Ataxia Treatment
Exciting advancements in genetic research and our understanding of the underlying mechanisms of spinocerebellar ataxia are paving the way for future treatments. Researchers and scientists are exploring various innovative approaches to develop more effective therapies and improve the lives of individuals with this condition.
Gene Editing Techniques
One promising avenue of research is the use of gene editing techniques to address the underlying genetic mutations that cause spinocerebellar ataxia. Technologies like CRISPR-Cas9 have shown potential in correcting the faulty genes responsible for the condition, offering hope for targeted and personalized treatments.
Stem Cell Therapy
Another area of exploration is stem cell therapy, which involves using stem cells to repair or replace damaged cells in the cerebellum. By harnessing the regenerative potential of stem cells, researchers aim to restore normal function and slow down the progression of spinocerebellar ataxia.
Neuroprotective Agents
Neuroprotective agents are being studied for their potential to prevent or minimize the degeneration of neurons in the cerebellum. These agents aim to protect the brain cells from further damage, potentially slowing down the progression of spinocerebellar ataxia and preserving neurological function.
The development of these and other emerging therapies offers hope for improved outcomes and a better quality of life for individuals living with spinocerebellar ataxia. While these treatments are still in the experimental stage, they hold great promise for the future.
Conclusion
Although there is no cure for spinocerebellar ataxia, there are treatment options available that can help manage symptoms and improve the quality of life for individuals with the condition. The multidisciplinary approach, involving medications, therapies, and assistive devices, plays a vital role in providing comprehensive care and support.
Medications such as riluzole have shown promising results in improving functional measures for spinocerebellar ataxia patients. Therapies like physical therapy, occupational therapy, and speech therapy can assist in managing symptoms and enhancing daily functioning. Additionally, adaptive devices and assistive technology enable individuals to maintain independence and improve their daily lives.
Looking to the future, ongoing research and clinical trials bring hope for new and more effective treatments. Advances in genetic research, including gene editing techniques and stem cell therapy, hold promise for the development of groundbreaking treatment options. It is an exciting time for the spinocerebellar ataxia community as advancements continue to be made.
FAQ
What is spinocerebellar ataxia?
Spinocerebellar ataxia is a neurological condition that affects coordination and balance. It is characterized by the degeneration of the cerebellum and its connections, caused by various genetic mutations and inheritance patterns.
What are the symptoms of spinocerebellar ataxia?
The symptoms of spinocerebellar ataxia include difficulties with balance and coordination, unsteady gait, speech difficulties, and involuntary eye movements.
How is spinocerebellar ataxia diagnosed?
Spinocerebellar ataxia is typically diagnosed through a thorough physical and neurological examination. Additional tests, such as blood tests and imaging studies, may be conducted to identify underlying causes or detect changes in the brain. Genetic testing is also recommended to determine the specific type of spinocerebellar ataxia.
Can spinocerebellar ataxia be caused by treatable underlying conditions?
Yes, in some cases, spinocerebellar ataxia may be caused by treatable underlying conditions such as vitamin deficiencies or infections. Treating these underlying causes can help improve symptoms.
Are there medications available for spinocerebellar ataxia?
Yes, there are medications available that can help manage the symptoms of spinocerebellar ataxia. Riluzole is one such medication that has shown promising results in improving functional measures in SCA patients. Other medications, such as varenicline and buspirone, have also been studied for their potential benefits in treating ataxia.
What therapies are available for spinocerebellar ataxia?
Various therapies can help individuals with spinocerebellar ataxia manage their symptoms and improve their quality of life. Physical therapy can assist with balance and coordination exercises, while occupational therapy focuses on daily living tasks. Speech therapy may also be beneficial for individuals with speech and swallowing difficulties.
How can adaptive devices and assistive technology help with spinocerebellar ataxia?
Adaptive devices and assistive technology can play a significant role in helping individuals with spinocerebellar ataxia maintain their independence and improve their daily functioning. Examples of adaptive devices include walking aids, modified utensils, and communication aids.
Are there any clinical trials or experimental treatments for spinocerebellar ataxia?
Yes, researchers are constantly exploring new treatment options for spinocerebellar ataxia through clinical trials and experimental therapies. These trials investigate the safety and efficacy of novel medications, gene therapies, and other interventions.
How can individuals cope with spinocerebellar ataxia?
It's important to seek support through counseling or support groups to cope with the emotional and physical aspects of the disease. Lifestyle modifications, such as maintaining a healthy diet and staying physically active, can also contribute to overall well-being.
What are the future directions in spinocerebellar ataxia treatment?
Advances in genetic research and understanding of the underlying mechanisms of spinocerebellar ataxia hold promise for future treatment options. Gene editing techniques, stem cell therapy, and neuroprotective agents are among the potential avenues being explored to develop more effective treatment options.
Can spinocerebellar ataxia be cured?
Currently, there is no cure for spinocerebellar ataxia. However, there are treatment options available that can help manage symptoms and improve the quality of life for individuals with the condition.
Understanding Spinocerebellar Ataxia - A Guide
Welcome to our comprehensive guide on Spinocerebellar Ataxia (SCA), a rare neurodegenerative inherited disease that primarily affects the cerebellum. In this guide, we will delve into the various aspects of SCA, including its genetic mutations, impact on health and life, and available treatment options. Whether you or a loved one are affected by SCA or you simply want to learn more about this condition, this guide will provide the information you need.
Etiology of Spinocerebellar Ataxia
Spinocerebellar Ataxia is a complex neurodegenerative disorder caused by various genetic mutations. One of the most common types of genetic mutations associated with Spinocerebellar Ataxia is trinucleotide repeat expansions. These expansions occur in specific genes, such as SCA1, SCA2, SCA3, and SCA6. The repeat expansions lead to the production of abnormal proteins, disrupting normal cellular processes in the cerebellum.
Spinocerebellar Ataxia can be inherited through autosomal dominant or autosomal recessive inheritance patterns. In cases of autosomal dominant inheritance, each newborn has a 50% chance of inheriting the mutated gene from an affected parent. Autosomal recessive inheritance occurs when both parents carry a single copy of a mutated gene, and the child inherits two copies, leading to the development of Spinocerebellar Ataxia.
It is important to note that while these genetic mutations account for many cases of Spinocerebellar Ataxia, the exact genetic cause remains unknown in a significant percentage of individuals.
Genes Associated with Spinocerebellar Ataxia and Inheritance Patterns
| Gene | Trinucleotide Repeat Expansion | Inheritance Pattern |
|---|---|---|
| SCA1 | CAG | Autosomal Dominant |
| SCA2 | CAG | Autosomal Dominant |
| SCA3 | CAG | Autosomal Dominant |
| SCA6 | CAG | Autosomal Dominant |
| Other Types | Varies | Autosomal Recessive |
Epidemiology of Spinocerebellar Ataxia
Spinocerebellar Ataxia (SCA) is a heterogeneous group of disorders with varying global prevalence. It is estimated that SCA affects 1 to 5 per 100,000 individuals worldwide. In Europe, the prevalence ranges from 0.9 to 3 per 100,000, with some geographical variation.
SCA encompasses different subtypes, with specific types being more prevalent than others. The most common types of SCA include:
- SCA3: This type accounts for 25-50% of all cases of SCA.
- SCA2: Approximately 13-18% of SCA cases are attributed to SCA2.
- SCA6: SCA6 is responsible for 13-15% of SCA cases.
- SCA7: While not as prevalent as SCA3, SCA7 remains a significant subtype.
It's important to note that the frequency of these types can vary in different regions. For example, SCA2 is more common in South Korea and India.
To provide a visual representation of the prevalence and distribution of SCA subtypes, here is a table summarizing the data:
| SCA Subtype | Global Prevalence | European Prevalence |
|---|---|---|
| SCA3 | 25-50% | Varies |
| SCA2 | 13-18% | Varies |
| SCA6 | 13-15% | Varies |
| SCA7 | Varies | Varies |
Understanding the epidemiology of Spinocerebellar Ataxia provides valuable insights into its global prevalence, variations within Europe, and the most prevalent subtypes. This knowledge contributes to enhanced awareness, accurate diagnosis, and improved care for individuals affected by this debilitating condition.
Pathophysiology of Spinocerebellar Ataxia
The exact pathogenesis of Spinocerebellar Ataxia (SCA) is not fully understood, but it primarily involves genetic mutations that lead to abnormal protein production and misfolding. These genetic mutations, particularly trinucleotide repeat expansions, result in the production of mutated proteins that are prone to misfolding.
One example of these misfolded proteins is ataxins, which are encoded by expanded CAG repeats. These misfolded proteins accumulate and form intranuclear inclusions within the Purkinje cells. Purkinje cells are the principal neurons in the cerebellum responsible for coordinating movement and maintaining balance.
As these misfolded proteins accumulate, they interfere with normal cellular functions and disrupt essential processes within the cells. This accumulation leads to the degeneration and eventual death of Purkinje cells, contributing to the progressive loss of coordination and movement observed in SCA.
In addition to protein misfolding and intranuclear inclusions, mitochondrial dysfunction plays a role in the pathophysiology of SCA. Mitochondria are responsible for producing energy within cells, and dysfunction in these crucial cellular powerhouses further contributes to the neurodegenerative process in SCA.
Overall, the pathophysiology of SCA involves a complex interplay of genetic mutations, protein misfolding, intranuclear inclusions, Purkinje cell degeneration, and mitochondrial dysfunction. Understanding the underlying mechanisms of SCA is vital for the development of effective treatments and therapies aimed at slowing down or halting the progression of this debilitating disease.
Histopathology of Spinocerebellar Ataxia
Spinocerebellar Ataxia (SCA) is characterized by various histopathological findings that help in understanding the disease's progression and underlying mechanisms. Gross examination of the brain in individuals with SCA often reveals cerebellar atrophy, where the cerebellum shows a noticeable reduction in size. This atrophy is accompanied by the enlargement of the lateral ventricles, indicating the presence of brain abnormalities.
On histopathological analysis, individuals with SCA exhibit significant loss of neurons, particularly in the cerebellum and other regions of the central nervous system. Notably, Purkinje cells, which are crucial for coordinating muscle movement, are prominently affected. The loss of these neurons contributes to the characteristic motor deficits observed in SCA.
Immunohistochemical studies have also revealed the presence of ubiquitin-positive intranuclear and cytoplasmic inclusions in certain types of SCA. These inclusions are aggregations of ubiquitin-tagged proteins and are indicative of protein misfolding and accumulation. The presence of these ubiquitin-positive inclusions further supports the role of abnormal protein handling and processing in the disease pathophysiology.
Overall, histopathological examination plays a crucial role in confirming the diagnosis of Spinocerebellar Ataxia and provides valuable insights into the underlying changes in the brain. By understanding the specific histopathological features associated with SCA, researchers can develop targeted therapeutic strategies aimed at preventing neuronal loss, promoting neuroprotection, and ultimately improving the quality of life for individuals living with this challenging condition.

Clinical Features and Diagnosis of Spinocerebellar Ataxia
Spinocerebellar Ataxia (SCA) is characterized by a range of clinical features that can vary from person to person. The onset of symptoms is typically gradual, often beginning with subtle coordination difficulties that progress over time. Symptoms may include:
- Gait instability: Individuals with SCA may experience unsteady and uncoordinated movements while walking.
- Tremors: Some individuals may develop involuntary shaking or trembling in their limbs.
- Balance problems: Maintaining balance and stability can be challenging for individuals with SCA.
- Speech difficulties: SCA can affect speech production, resulting in slurred or slow speech.
In evaluating possible cases of SCA, it is important to consider the patient's family history. SCA can be inherited, and individuals with a family history of the condition may have an increased risk of developing it themselves.
Diagnosing SCA typically involves genetic testing to identify specific gene mutations associated with the condition. Genetic testing can help confirm a diagnosis and provide information about the specific subtype of SCA. However, in some cases, the responsible gene mutation may not be identified.
In such instances, brain imaging techniques, such as a CT scan or MRI, may be used to detect brain abnormalities commonly observed in individuals with SCA. These imaging studies can help support the diagnosis by revealing cerebellar atrophy or other structural changes in the brain.
The image above illustrates the importance of brain imaging in the diagnosis of SCA. By visualizing the brain's structure, healthcare professionals can identify any abnormalities that may be indicative of the condition.
| Diagnostic Methods for Spinocerebellar Ataxia | Advantages | Limitations |
|---|---|---|
| Genetic Testing |
|
|
| Brain Imaging (CT scan or MRI) |
|
|
Treatment Options for Spinocerebellar Ataxia
Although there is no cure for Spinocerebellar Ataxia, various treatment options can help manage the symptoms and improve the quality of life for individuals with SCA. Spinocerebellar Ataxia treatment options include:
- Physical therapy: Physical therapy plays a crucial role in improving muscle strength, balance, and coordination in individuals with SCA. Therapists can design customized exercise programs to target specific motor impairments and help improve mobility.
- Occupational therapy: Occupational therapy focuses on enhancing daily functioning and independence. Therapists can teach individuals with SCA adaptive techniques, recommend assistive devices, and modify the environment to improve activities of daily living.
- Speech therapy: Speech therapy can help improve speech difficulties and swallowing problems commonly associated with SCA. Therapists work on speech exercises, swallowing techniques, and communication strategies to enhance overall communication skills.
- Stem cell therapy: Stem cell therapy is an innovative approach that holds promise in the treatment of Spinocerebellar Ataxia. It involves using stem cells to replace damaged cells and promote tissue repair in the cerebellum. While it is still an emerging field, ongoing research shows potential benefits for individuals with SCA.
- Neurorehabilitation: Neurorehabilitation programs focus on optimizing brain function and promoting neurological recovery. These programs combine various therapies, including physical therapy, occupational therapy, speech therapy, and cognitive training, to address multiple aspects of SCA and improve overall functioning.
By incorporating these treatment options into a comprehensive management plan, individuals with Spinocerebellar Ataxia can experience improved symptoms, enhanced quality of life, and better overall well-being.

Achieving Optimal Results with a Multidisciplinary Approach
The treatment of Spinocerebellar Ataxia often requires a multidisciplinary approach, involving collaboration between different healthcare professionals. By combining the expertise of physical therapists, occupational therapists, speech therapists, and other specialists, a comprehensive and individualized treatment plan can be developed to address the unique needs of each person with SCA.
Research studies and clinical trials continue to explore new therapeutic interventions and advancements in the field of Spinocerebellar Ataxia. As more is understood about the underlying mechanisms of the disease, additional treatment options may become available, offering hope for improved outcomes and eventual cures.
Impact on Daily Life and Prognosis of Spinocerebellar Ataxia
Spinocerebellar Ataxia can have a significant impact on daily life, leading to cognitive problems, functional limitations, and reduced quality of life. The progressive nature of the disease and its effects on coordination and balance can result in difficulties performing simple tasks, such as walking, eating, and speaking. These cognitive problems and functional limitations can greatly disrupt daily routines and hinder independence.
The rate of disease progression in Spinocerebellar Ataxia varies depending on the specific subtype and the age of disease onset. Some forms of SCA progress slowly, while others have a more rapid course. Individuals with early-onset SCA tend to experience a faster disease progression and may develop severe functional limitations at a younger age.
Unfortunately, there is currently no known cure for Spinocerebellar Ataxia. The disease progression and impact on daily life can be challenging for individuals and their families. However, with appropriate management, support, and rehabilitation measures, individuals with SCA can maintain a fulfilling life and adapt to their changing abilities.
It is crucial for individuals with SCA to receive comprehensive care that addresses their physical, emotional, and social needs. This may involve a multidisciplinary approach, including neurologists, physical therapists, occupational therapists, speech therapists, and mental health professionals.
By focusing on symptom management, functional improvements, and maintaining a positive mindset, individuals with Spinocerebellar Ataxia can enhance their quality of life and find ways to thrive despite the challenges they face.
Impact of Cognitive Problems
One of the significant challenges faced by individuals with Spinocerebellar Ataxia is cognitive dysfunction. Cognitive problems can range from mild difficulties with attention and concentration to more severe impairments in memory, executive functions, and information processing. These cognitive deficits can impact daily activities, work performance, and overall quality of life.
The underlying mechanisms of cognitive dysfunction in SCA are not yet fully understood. However, it is believed that the cerebellum, which is primarily affected in SCA, plays a crucial role in cognitive processes. The cerebellum has extensive connections with other brain regions involved in cognitive functioning, such as the prefrontal cortex.
Strategies for managing cognitive problems in Spinocerebellar Ataxia include cognitive rehabilitation techniques, compensatory strategies, and environmental modifications. Additionally, individuals with SCA and their families can benefit from education, counseling, and support groups to better understand and cope with the challenges posed by cognitive impairments.
Functional Limitations and Quality of Life
Functional limitations are a hallmark feature of Spinocerebellar Ataxia and can significantly impact an individual's ability to perform activities of daily living. Walking, balance, coordination, and fine motor skills are often affected, making routine tasks challenging or even impossible without assistance.
Functional limitations can lead to increased dependence, reduced mobility, and decreased participation in social and recreational activities. This can have a detrimental effect on an individual's quality of life, leading to feelings of frustration, isolation, and loss of independence.
Physical and occupational therapy play a crucial role in managing functional limitations caused by Spinocerebellar Ataxia. These therapies focus on improving mobility, balance, coordination, and strength. Assistive devices, such as walking aids, can also help enhance independence and functional ability.
| Functional Limitations | Impact on Quality of Life |
|---|---|
| Difficulty with walking and balance | Reduced mobility and increased risk of falls |
| Coordination problems | Challenges in performing fine motor tasks (e.g., writing, buttoning clothes) |
| Speech difficulties and swallowing problems | Impaired communication and reduced enjoyment of food and drink |
| Impaired eye movements | Difficulty reading, watching TV, or driving |
Despite the challenges posed by functional limitations, individuals with Spinocerebellar Ataxia can still lead meaningful and fulfilling lives. Adaptive strategies, support from healthcare professionals and caregivers, and assistive technologies can help individuals maximize their independence and maintain a good quality of life.
Disease Progression and Prognosis
The progression of Spinocerebellar Ataxia varies depending on the subtype and individual factors. Some forms of SCA progress slowly over many years, while others have a more rapid course with significant functional decline in a shorter period. The age of disease onset also plays a role in disease progression, with earlier onset generally associated with a worse prognosis.
SCA is a progressive condition, meaning that symptoms tend to worsen over time. The rate of disease progression can be unpredictable, even among individuals with the same subtype. Progressive loss of coordination, balance, and mobility can eventually lead to severe disability and the need for assistive devices or caregiving support.
It is important for individuals with SCA to have regular medical follow-ups to monitor disease progression, manage symptoms, and adjust treatment plans accordingly. A comprehensive approach to care that addresses physical, cognitive, and emotional well-being can help individuals maintain the best possible quality of life throughout the progression of Spinocerebellar Ataxia.
Research and Future Directions for Spinocerebellar Ataxia
Ongoing research in the field of Spinocerebellar Ataxia is dedicated to deepening our understanding of the underlying genetic mechanisms, identifying potential therapeutic targets, and developing new treatment approaches. Genetic studies play a crucial role in unraveling the complexities of SCA and uncovering novel genes associated with the disease.
Scientists and researchers are conducting clinical trials and research studies to explore promising therapeutic interventions for Spinocerebellar Ataxia. These investigations include gene therapies and targeted drug treatments, aiming to slow down the progression of the disease and alleviate its symptoms. By focusing on these cutting-edge therapeutic approaches, we hope to bring new hope and improved quality of life to individuals affected by SCA.
Current Research Focus Areas
- Genetic studies to identify novel genes associated with Spinocerebellar Ataxia
- Investigations into potential therapeutic interventions, such as gene therapies and targeted drugs
- Exploration of the underlying molecular mechanisms and pathways involved in SCA
- Development of neuroprotective strategies to prevent or slow down the neurodegeneration in SCA
- Identification of biomarkers for early detection and monitoring of disease progression
- Collaboration with international research teams to share knowledge and resources

Example Clinical Trial
To provide a glimpse into the ongoing clinical trials and research studies, here is an example:
| Study Title | Phase | Objective | Status |
|---|---|---|---|
| Gene Therapy for SCA3 | Phase 2 | To evaluate the safety and efficacy of gene therapy in slowing down disease progression | Ongoing |
This Phase 2 clinical trial aims to assess the potential of gene therapy as a therapeutic intervention for Spinocerebellar Ataxia Type 3 (SCA3). Researchers are investigating the safety and efficacy of introducing normal copies of the mutant gene into affected individuals using viral vectors. The trial is currently ongoing, and the results hold the promise of advancing our understanding and treatment options for SCA3.
Support and Resources for Individuals with Spinocerebellar Ataxia
Living with Spinocerebellar Ataxia can be challenging, both for individuals with the condition and their caregivers. Fortunately, there are various support and resources available to help navigate the journey. These include:
Patient Support Groups
Joining patient support groups can provide invaluable emotional support and a sense of belonging. These groups bring together individuals who understand the daily challenges of living with Spinocerebellar Ataxia, offering an opportunity to share experiences, exchange coping strategies, and offer encouragement. Many patient support groups also organize educational events and social activities to foster connections within the community.
Counseling Services
Seeking counseling services can be beneficial for individuals and their families affected by Spinocerebellar Ataxia. Counselors and therapists specializing in neurodegenerative conditions can provide professional guidance, coping strategies, and emotional support. Counseling sessions can help individuals navigate the psychological and emotional impact of the condition, manage stress and anxiety, and develop resilience.
Assistive Devices
Assistive devices play a significant role in enhancing independence and improving daily functioning for individuals with Spinocerebellar Ataxia. Walking aids, such as canes or walkers, provide stability and support while navigating uneven surfaces or walking longer distances. Communication devices, like speech-to-text software or communication boards, can assist individuals with speech difficulties in expressing their thoughts and needs effectively.
Caregiver Support
Caregivers of individuals with Spinocerebellar Ataxia also require support and resources to manage their responsibilities effectively. Caregiver support groups offer a safe space for caregivers to share their experiences, seek advice, and find emotional support from others who understand the unique challenges they face. Furthermore, respite care programs can provide temporary relief for caregivers, allowing them time to rest and recharge.
Conclusion
Having a comprehensive understanding of spinocerebellar ataxia (SCA) is crucial to grasp the full impact it can have on individuals' health and daily lives. This guide has provided a detailed overview of the etiology, epidemiology, pathophysiology, clinical features, diagnosis, treatment options, prognosis, research, and resources related to SCA.
By delving into the complexities of SCA, individuals and their caregivers can navigate the challenges associated with the disease more effectively. Armed with knowledge about the genetic mutations and trinucleotide repeat expansions that cause SCA, potential risk factors, and the prevalence of different types of the condition, individuals can better understand the nature of their condition and its implications.
Moreover, this guide has shed light on the various treatment options available to manage SCA symptoms, such as physical therapy, occupational therapy, speech therapy, and neurorehabilitation. Additionally, the importance of patient support groups, counseling services, and assistive devices in improving quality of life for individuals with SCA has been emphasized.
With ongoing research and advancements in the field of SCA, there is hope for future therapeutic interventions and targeted treatments. By staying informed about the latest research studies and opportunities for participation in clinical trials, individuals affected by SCA can actively contribute to the progress and development of innovative treatment approaches.
FAQ
What is Spinocerebellar Ataxia?
Spinocerebellar Ataxia is a progressive neurodegenerative inherited disease that mainly affects the cerebellum. It is a rare disease and is classified as a subset of hereditary cerebellar ataxia.
What causes Spinocerebellar Ataxia?
Spinocerebellar Ataxia is caused by genetic mutations, particularly trinucleotide repeat expansions, which lead to the gradual degeneration of the cerebellum. These mutations can occur in genes such as SCA1, SCA2, SCA3, and SCA6.
How common is Spinocerebellar Ataxia?
The global prevalence of Spinocerebellar Ataxia is estimated to be 1 to 5 per 100,000 individuals. In Europe, the prevalence ranges from 0.9 to 3 per 100,000, with some geographical variation.
What are the clinical features of Spinocerebellar Ataxia?
Spinocerebellar Ataxia can present with symptoms such as gait instability, tremors, balance problems, and speech difficulties.
How is Spinocerebellar Ataxia diagnosed?
Diagnosis typically involves genetic testing to identify specific gene mutations associated with Spinocerebellar Ataxia. In cases where the gene mutation cannot be identified, brain imaging may be used to detect brain abnormalities commonly observed in individuals with SCA.
Is there a cure for Spinocerebellar Ataxia?
Currently, there is no known cure for Spinocerebellar Ataxia. However, various treatment options, including physical therapy, occupational therapy, and speech therapy, can help manage the symptoms and improve the quality of life for individuals with SCA.
How does Spinocerebellar Ataxia impact daily life?
Spinocerebellar Ataxia can have a significant impact on daily life, leading to cognitive problems, functional limitations, and reduced quality of life. The rate of disease progression varies depending on the specific subtype of SCA and the age of disease onset.
What research is being done on Spinocerebellar Ataxia?
Ongoing research focuses on understanding the underlying genetic mechanisms of Spinocerebellar Ataxia, identifying potential therapeutic targets, and developing new treatment approaches. Clinical trials and research studies are investigating potential therapeutic interventions, including gene therapies and targeted drug treatments.
What support and resources are available for individuals with Spinocerebellar Ataxia?
Patient support groups and counseling services provide valuable emotional support and a platform for sharing experiences for individuals with Spinocerebellar Ataxia. Assistive devices, such as walking aids and communication devices, can enhance independence and improve daily functioning. Caregivers also require support and resources to manage their responsibilities effectively.
Where can I find more information about Spinocerebellar Ataxia?
This comprehensive guide provides an overview of Spinocerebellar Ataxia. For more detailed information and resources, you can consult medical professionals, patient support groups, and reputable websites specializing in neurological disorders.
Effective Dystonia Cervical Treatment Options
If you or a loved one is struggling with dystonia cervical treatment, finding effective options to manage symptoms and improve quality of life is essential. Cervical dystonia, also known as spasmodic torticollis, is a condition that affects the neck muscles, causing abnormal neck posturing, tremor, and pain. Without proper treatment, it can significantly impact your daily life and well-being.
In this article, we will explore the most effective treatment options for dystonia cervical treatment and how they can help you manage symptoms and improve your quality of life. From botulinum toxin injections to oral medications and deep brain stimulation, there are treatment options available that can provide relief and restore functionality.
By understanding these treatment options and working closely with your healthcare provider, you can find a plan that suits your individual needs and preferences. With the right treatment, the symptoms of dystonia cervical can be effectively managed, allowing for improved functionality and a better quality of life.
Botulinum Toxin Injections for Cervical Dystonia
Botulinum toxin injections, such as Botox, Dysport, Xeomin, and Myobloc, are the most effective and well-tolerated treatment for cervical dystonia. These injections provide targeted relief by selectively denervating and relaxing the affected neck muscles, leading to an improvement in the abnormal head posture and movements.
Patients with cervical dystonia often experience significant relief with botulinum toxin injections. The efficacy of these injections, along with their minimal side effects, makes them the preferred treatment option for cervical dystonia.
These injections are typically administered every three to four months and require repeat treatments to maintain their effectiveness. Regular follow-ups with a healthcare provider are necessary to monitor the progress and adjust the treatment plan as needed.
Botulinum toxin injections have revolutionized the management of cervical dystonia, offering patients a reliable method of achieving neck muscle relaxation and improving their overall quality of life. The targeted action of these injections provides significant relief, allowing individuals to regain control over their movements and reduce pain and discomfort.
In the next section, we will explore the role of oral medications as adjunct therapy for cervical dystonia, complementing the effects of botulinum toxin injections.
Oral Medications as Adjunct Therapy
While botulinum toxin injections are the primary treatment for dystonia cervical, oral medications can be used as adjunct therapy to enhance the effects or when injections are not practical or desired. These medications can complement the muscle-relaxing effects of botulinum toxin injections and provide additional relief for individuals with cervical dystonia.
Commonly used oral medications for dystonia cervical treatment include:
- Trihexyphenidyl
- Baclofen
- Tetrabenazine
Oral medications with a muscle-relaxing effect can help reduce muscle spasms and improve mobility in individuals with cervical dystonia. They are often prescribed as add-on therapy to enhance the effectiveness of botulinum toxin injections.
It is important to note that the effectiveness of oral medications may vary from person to person. Some individuals may experience significant relief from these medications, while others may have more modest improvements. Additionally, like any medication, oral medications may have potential side effects. It is important to discuss the potential risks and benefits with a healthcare provider before starting any oral medication regimen.
Overall, oral medications can be a valuable addition to the treatment plan for cervical dystonia, providing an extra layer of support and relief alongside botulinum toxin injections.

Adding a visual representation can help reinforce the message. The image above illustrates the different oral medications commonly used as adjunct therapy for dystonia cervical treatment.
Deep Brain Stimulation for Refractory Cases
In cases where botulinum toxin injections and oral medications fail to provide adequate relief, deep brain stimulation (DBS) can be considered as a surgical therapy option for cervical dystonia. DBS involves implanting a thin wire into the brain, connecting it to a neurostimulator device. Electrical pulses are then delivered through the wire, interrupting the nerve signals responsible for the abnormal head posture and movements. DBS is typically reserved for refractory cases that do not respond to other treatments. It is a complex and invasive procedure that requires careful evaluation and selection of appropriate candidates.
Deep brain stimulation is a promising treatment approach for individuals with cervical dystonia who have not achieved satisfactory results with other therapies. This surgical intervention targets the underlying neurological mechanisms contributing to the dystonic movements. By selectively modulating brain activity through electrical stimulation, DBS offers the potential for significant symptom improvement and enhanced quality of life.
Conclusion
Effective treatment options are available for managing cervical dystonia and improving the quality of life for those affected. If you are living with cervical dystonia, there are several strategies that can help alleviate your symptoms and allow you to regain control over your life.
Botulinum toxin injections, such as Botox, Dysport, Xeomin, and Myobloc, are the gold standard treatment for cervical dystonia. These injections selectively denervate and relax the affected neck muscles, providing significant relief from abnormal head posture and movements. Consult with your healthcare provider to determine if botulinum toxin injections are the right choice for you.
In addition to injections, oral medications can be used as adjunct therapy to enhance the effects of botulinum toxin injections. Medications with muscle-relaxing properties, like trihexyphenidyl, baclofen, and tetrabenazine, can complement the injections and further improve your symptoms. It is essential to work closely with your doctor to find the right combination and dosage of medications that suit your needs.
In rare cases where botulinum toxin injections and oral medications do not provide adequate relief, deep brain stimulation (DBS) may be considered as a surgical therapy option. This procedure involves implanting a wire into the brain and delivering electrical pulses to interrupt the nerve signals responsible for abnormal head movements. DBS should only be considered as a last resort for refractory cases, and careful evaluation is necessary to determine if you are a suitable candidate.
Remember, each person's journey with cervical dystonia is unique, and the most effective treatment plan will depend on your individual needs and preferences. Consult with your healthcare provider to discuss these effective treatment options and find the best approach to manage your cervical dystonia. With proper treatment, you can regain functionality, improve your quality of life, and live your life to the fullest.
FAQ
What is cervical dystonia?
Cervical dystonia, also known as spasmodic torticollis, is a common adult-onset focal dystonia that affects the neck muscles, causing abnormal neck posturing, tremor, and pain.
What is the most effective treatment for cervical dystonia?
The most effective treatment option for cervical dystonia is botulinum toxin (BoNT) injections, which selectively denervate and relax the affected neck muscles.
What are botulinum toxin injections?
Botulinum toxin injections, such as Botox, Dysport, Xeomin, and Myobloc, are administered directly into the affected neck muscles to selectively denervate and relax them, resulting in an improvement in the abnormal head posture and movements.
How often do botulinum toxin injections need to be repeated?
Botulinum toxin injections typically need to be repeated every three to four months.
Can oral medications be used for cervical dystonia?
Yes, oral medications with a muscle-relaxing effect, such as trihexyphenidyl, baclofen, and tetrabenazine, can be prescribed as adjunct therapy to enhance the effects of botulinum toxin injections or when injections are not practical or desired.
What is deep brain stimulation?
Deep brain stimulation (DBS) is a surgical therapy option for cervical dystonia that involves implanting a thin wire into the brain, connecting it to a neurostimulator device. Electrical pulses are then delivered through the wire, interrupting the nerve signals responsible for the abnormal head posture and movements.
When is deep brain stimulation considered?
Deep brain stimulation is typically considered for refractory cases of cervical dystonia that do not respond to other treatments.
What should I do to manage my cervical dystonia?
It is important to consult with a healthcare provider to determine the most suitable treatment plan based on individual needs and preferences, which can help manage the symptoms of cervical dystonia and improve overall functionality and well-being.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3495548/
- https://www.uptodate.com/contents/cervical-dystonia-treatment-and-prognosis
- https://www.mayoclinic.org/diseases-conditions/cervical-dystonia/diagnosis-treatment/drc-20354128
Alzheimer's disease diagnosis
Diagnosing Alzheimer's disease typically involves a comprehensive evaluation that includes medical history, physical examination, cognitive assessments, and sometimes imaging or laboratory tests. Here's a general overview of the diagnostic process:
- Medical History and Physical Examination: The healthcare provider will conduct a thorough review of the individual's medical history, including symptoms, family history of dementia, and any medications or medical conditions that could contribute to cognitive impairment. A physical examination may also be performed to assess overall health and rule out other potential causes of symptoms.
- MRI (Magnetic Resonance Imaging): It's like a big camera that takes detailed pictures of the brain. With MRI, we can see the structure of the brain, like its size and shape. In Alzheimer's, we might see shrinkage or atrophy in certain areas of the brain, which can help confirm the diagnosis.
- PET (Positron Emission Tomography) scans: These scans show us how the brain is working. We use a special dye that highlights certain things in the brain, like proteins associated with Alzheimer's. PET scans help us see changes in brain activity and metabolism, which can give us more clues about the disease.
- Functional MRI (fMRI): This is a type of MRI that shows us which parts of the brain are active when a person is doing different tasks. It helps us understand how the brain is functioning. For example, we might ask someone to remember things while in the fMRI machine to see which parts of their brain are working hard. In Alzheimer's disease, certain areas of the brain might not show as much activity as they should, which can indicate problems with memory or thinking.
- Cognitive Testing: This involves doing various tasks or answering questions to assess memory, thinking, and other brain functions.
- Mini-Mental State Examination (MMSE): It's like a quiz that helps us evaluate different aspects of cognitive function, such as memory, attention, and language. For example, we might ask someone to remember a list of words or draw a clock to see how well they can follow instructions and remember things.
- Montreal Cognitive Assessment (MoCA): This is another test that helps us assess cognitive abilities. It includes tasks like remembering words, drawing shapes, and following instructions. It gives us a broader picture of cognitive function beyond just memory.
- Neuropsychological Testing: In Alzheimer's disease, neuropsychological testing plays a crucial role in understanding the extent and pattern of cognitive impairment.
Here's how neuropsychological testing is used in Alzheimer's diagnosis and management:
- Assessment of Cognitive Function: Neuropsychological tests assess various cognitive functions that are typically affected in Alzheimer's disease, including memory, attention, language, executive function (such as planning and problem-solving), and visuospatial abilities. These tests help identify specific areas of cognitive decline and track changes over time.
- Differentiating Alzheimer's from Other Conditions: Neuropsychological testing helps distinguish Alzheimer's disease from other types of dementia or cognitive disorders. While Alzheimer's primarily affects memory and other cognitive functions, other conditions may have different patterns of cognitive impairment. Neuropsychological tests can help clinicians make a more accurate diagnosis.
- Monitoring Disease Progression: Neuropsychological testing is used to monitor the progression of Alzheimer's disease over time. By repeating tests at regular intervals, clinicians can track changes in cognitive function and assess the rate of decline. This information is valuable for adjusting treatment plans and providing appropriate support and interventions.
- Assessment of Functional Impairment: In addition to cognitive function, neuropsychological testing may also assess functional abilities related to daily living, such as managing finances, performing household tasks, and maintaining personal hygiene. Understanding the impact of cognitive decline on daily functioning is important for determining the level of support and assistance individuals with Alzheimer's may require.
- Evaluation of Treatment Efficacy: Neuropsychological testing can be used to evaluate the effectiveness of treatments and interventions aimed at managing symptoms of Alzheimer's disease. For example, if a person with Alzheimer's starts taking medication to improve cognition, neuropsychological testing can help assess whether there are any measurable improvements in cognitive function over time.
- Guiding Care Planning: Results from neuropsychological testing inform care planning and help caregivers and healthcare professionals develop personalized strategies to support individuals with Alzheimer's disease. These strategies may include cognitive rehabilitation techniques, environmental modifications, and caregiver education and support.
- Laboratory Tests: While there is currently no single blood test that can definitively diagnose Alzheimer's disease, certain blood tests can provide valuable information that may support the diagnostic process or help rule out other potential causes of cognitive impairment. Here are some blood tests that may be used in evaluating
Alzheimer's disease

- Complete Blood Count (CBC): A CBC measures various components of the blood, such as red blood cells, white blood cells, and platelets. Abnormalities in the CBC may indicate underlying medical conditions that could contribute to cognitive impairment, such as infections or anemia.
- Blood Chemistry Panel: A blood chemistry panel measures levels of glucose, electrolytes, liver enzymes, kidney function markers, and other substances in the blood. Abnormalities in these levels may indicate metabolic imbalances or organ dysfunction that could affect brain function.
- Thyroid Function Tests: Thyroid function tests measure levels of thyroid hormones (TSH, T3, and T4) in the blood. Thyroid disorders, such as hypothyroidism or hyperthyroidism, can cause symptoms similar to those of Alzheimer's disease, including cognitive impairment and memory problems.
- Vitamin B12 and Folate Levels: Deficiencies in vitamin B12 and folate (vitamin B9) can lead to neurological symptoms, including cognitive decline and memory loss. Blood tests can measure levels of these vitamins to identify deficiencies that may contribute to cognitive impairment.
- Inflammatory Markers: Chronic inflammation has been implicated in the development and progression of Alzheimer's disease. Blood tests may measure levels of inflammatory markers such as C-reactive protein (CRP) or interleukin-6 (IL-6) to assess inflammation levels in the body.
- Cerebrospinal Fluid Analysis: In some cases, a lumbar puncture (spinal tap) may be performed to analyze cerebrospinal fluid for biomarkers associated with Alzheimer's disease, such as amyloid-beta and tau proteins.
- Clinical Criteria: Diagnosis of Alzheimer's disease is often based on clinical criteria established by organizations such as the National Institute on Aging and the Alzheimer's Association. These criteria consider the pattern of cognitive impairment, progression of symptoms over time, and exclusion of other potential causes of dementia.
- Multidisciplinary Evaluation: Diagnosing Alzheimer's disease may involve a team of healthcare professionals, including neurologists, geriatricians, neuropsychologists, and other specialists, who collaborate to evaluate the individual's symptoms and determine the most likely diagnosis.
What is a Brain Aneurysm?
A Tiny Balloon in the Brain: Aneurysm is like a small balloon on the blood vessels in your brain. These vessels are like roads for blood to travel to different parts of your brain.
Where They Form: Aneurysms can pop up anywhere in the brain, but they mostly like to hang out at the junctions where blood vessels split or bend. It's like how a garden hose might bulge at a kink or a split.
Different Types of Aneurysms
- Saccular Aneurysms: These are the most common type. They are round and bulge out on one side of a blood vessel, looking like a berry hanging on a stem.
- Fusiform Aneurysms: These bulge out all around the blood vessel, making it look expanded in all directions.
- Dissecting Aneurysms: These are caused by a tear in the blood vessel wall. Blood can leak through this tear and cause the vessel to bulge out.
Hidden Threat of Aneurysms
- Sizes Matter: Aneurysms come in various sizes. Small ones might not cause any issues, while larger ones can be more risky.
- Silent Threat: What's tricky about aneurysms is that they often don't cause any symptoms until they're quite big or if they burst. It's like having a sneaky bubble that doesn't make a sound.
- The Brain's Neighborhoods: The location of an aneurysm in the brain can affect different functions. For example, an aneurysm near the part of the brain that controls vision might affect how you see.
Why Should We Learn About Brain Aneurysms?
It's super important to learn about brain aneurysms, even though they're rare. Here's why understanding them is a big deal.
- Knowledge is Power: By knowing what a brain aneurysm is, you can be smart about your health. If you know only then can you prepare.
- Early Detection: If we know what signs to look for, aneurysms can often be caught early. This means doctors can keep an eye on them or treat them before they cause serious issues.
- Understanding Symptoms: Sometimes, aneurysms give warning signs. If you or someone you know experiences symptoms like a sudden severe headache, it’s important to get it checked out quickly.
- Family History: In some families, aneurysms might be more common. If your family has a history of aneurysms, knowing about them can help you and your family members stay on top of your health.
- Health Choices: Learning about aneurysms can encourage us to make healthier life choices. Things like eating well, exercising, and not smoking can keep our blood vessels strong and reduce the risk of aneurysms.
How Does a Brain Aneurysm Happen?

Brain aneurysms can seem a bit mysterious, but there are several reasons why they might form. Let's dive into some of the causes:
- Genetic Factors: Just like you might inherit your eye color or hair type from your parents, some people might inherit the tendency to develop aneurysms. Its like there is weak point in the blood vessels right from birth.
- High Blood Pressure: This is a big one. High blood pressure is like having a strong, fast river flowing through weak banks. Over time, this pressure can cause a part of the blood vessel wall to bulge out. It’s important to keep our blood pressure in check through healthy habits.
- Arterial Wall Damage: Our blood vessels can get damaged over time, especially if we're not living healthily. Smoking, high cholesterol, and other factors can weaken the walls of our blood vessels, making them more prone to aneurysms.
- Aging: As we grow older, just like getting taller and wiser, the blood vessels in our brains can change too. They might weaken in some places as we age, increasing the risk of aneurysms.
- Head Injury: A strong hit to the head, like from a fall or a sports injury, can sometimes damage blood vessels in the brain. This damage might lead to an aneurysm.
- Lifestyle Choices: Smoking is a big no-no. It can seriously weaken blood vessel walls. Eating lots of unhealthy foods and not exercising can also contribute to the risk.
- Infections and Other Conditions: Rarely, infections or certain diseases can weaken blood vessels and lead to aneurysms.
What are the Signs of a Brain Aneurysm?
Spotting the signs of a brain aneurysm can be tricky because they often don't show any symptoms until they're quite large or if they burst. But there are some clues we can look out for Sudden,
- Severe Headache: This isn't your typical headache. It's often described as the worst headache ever experienced. It's like a sudden thunderstorm in your head, starting out of nowhere.
- Vision Changes: You might experience blurred or double vision. It's like trying to watch TV when the picture isn't clear.
- Feeling Dizzy or Sick: You could feel very dizzy, almost like you're on a merry-go-round that's spinning too fast. Or, you might feel like you're going to throw up, even if you haven't eaten anything weird.
- Confusion: It might become hard to think straight or to remember simple things. Imagine trying to do your homework but suddenly forgetting how to do simple math or spell easy words.
- Sensitivity to Light: Bright lights might suddenly seem too glaring, kind of like when you first step out into the sun from a dark room.
- Stiff Neck: Your neck might feel stiff or sore, making it hard to move your head around like you normally would.
- Seizure: In rare cases, an aneurysm might cause a seizure, which is like an electrical storm in your brain that causes uncontrollable body movements.
- Drooping Eyelid: One of your eyelids might start to droop, making it seem like you're winking but you're not trying to.
- Nausea and Vomiting: You might feel sick to your stomach and even throw up, which isn't fun.
What Happens if an Aneurysm Bursts?
When a brain aneurysm bursts, it's a serious emergency that needs immediate medical attention.
- A Sudden Burst: Imagine a water balloon bursting unexpectedly. That's similar to what happens when an aneurysm ruptures. It causes bleeding inside the brain, which is a very serious situation.
- Bleeding in the Brain: This bleeding can damage brain cells and cause swelling in the brain.This can lead to weakness in one part of the body and may cause unconsciousness.
- Symptoms of a Burst Aneurysm: The symptoms of a ruptured aneurysm are usually very sudden and severe. These can include
- A sudden and extremely painful headache – much worse than a normal headache.
- Stiff neck, almost like you can't move your head properly.
- Sensitivity to light, where even normal light feels too bright.
- Double vision, or seeing two of everything.
- Seizures, which are like electrical storms in your brain that you can't control.
- Losing consciousness – this means you might pass out and not wake up easily.
- Immediate Medical Help: If someone has a burst aneurysm, they need to go to the hospital right away. It's like calling firefighters for a fire; you need help fast.
- The Golden Hours: Doctors often talk about the "golden hour" in medical emergencies. This means the first few hours after something like a burst aneurysm is super important. Getting help quickly can make a big difference in recovery.
- Treatment: At the hospital, doctors will work quickly to stop the bleeding and reduce the pressure in the brain. They might use surgery or other special procedures to fix the broken blood vessel.
- Recovery: Recovery from a burst aneurysm can take time and depends on how severe the bleeding was and how quickly treatment started. Some people might need rehabilitation to relearn basic skills like talking or walking.
How Can Doctors Find an Aneurysm? How are aneurysms diagnosed
Detecting a brain aneurysm can be like a detective solving a mystery. Doctors use different tools and tests to find out if there's an aneurysm in the brain. Let's look at some of these cool methods:
- CT Scan (Computed Tomography): This is like a super-advanced camera that takes detailed pictures of your brain. It uses special X-ray technology to create images from different angles, which are then put together to show if there’s an aneurysm.
- MRI (Magnetic Resonance Imaging): An MRI uses powerful magnets and radio waves to create pictures of your brain. It's like a camera that can see inside your head without using X-rays. MRIs are great at looking at soft tissues and blood vessels.
- Cerebral Angiogram: This is a more detailed test. Doctors insert a thin tube into a blood vessel, usually in the leg, and guide it up to the brain. Then, they inject a special dye that shows up on X-rays. It's like drawing a map of all the blood vessels in your brain so doctors can spot any aneurysms.
- Lumbar Puncture: If doctors think an aneurysm has burst, they might do this test. It involves taking a small amount of fluid from around your spine (don’t worry, they use anesthetic to make it not hurt). They check this fluid to see if there’s any blood in it, which can be a sign of a burst aneurysm.
- MRA (Magnetic Resonance Angiography): This is a special type of MRI that focuses specifically on blood vessels. It’s like having a zoomed-in view of the highways in your brain to check for traffic jams or bulges.
Treatment for Brain Aneurysms
Treating a brain aneurysm is a bit like fixing a weak spot in a dam before it can burst. Doctors have several ways to treat aneurysms, depending on their size, location, and whether they've burst. Let's explore these fascinating treatments.
- Observation: Sometimes, if an aneurysm is small and not causing problems, doctors might just keep an eye on it. This is like watching a tiny crack in a vase to make sure it doesn't get bigger. They'll use regular check-ups and scans to watch the aneurysm closely.
Surgery
Clipping: This is a common Treatment Of A Ruptured Aneurysm. Surgeons open up the skull (this is called craniotomy) and place a tiny metal clip on the neck of the aneurysm. This clip stops blood from entering the aneurysm, like putting a clip on a balloon to stop it from inflating. This is falling out of favour because of the need for open surgery.
Endovascular Aneurysm Repair Coiling VS Clipping
- Coiling: This is less invasive than open surgery and preferred all over the world. Doctors thread a thin tube through the blood vessels to the aneurysm. They then push tiny coils through the tube into the aneurysm. These coils fill up the aneurysm, blocking blood flow into it and preventing it from bursting. It’s like filling the bubble with something that stops it from growing.
- Flow Diverters: These are like the coils but work differently. They are placed in the parent blood vessel to divert blood flow away from the aneurysm. Think of it as redirecting traffic away from a weak bridge. They help heal the vessel by redirecting blood flow and promoting tissue growth across the neck of the aneurysm.
- Medication: While medicines can't fix an aneurysm, they can help with related issues. For example, doctors might give medicine to control blood pressure, reduce headaches, or prevent seizures.
- Lifestyle Changes: Along with medical treatments, doctors will often advise lifestyle changes to help prevent new aneurysms. This includes quitting smoking, eating a healthy diet, and exercising regularly.
How Can We Prevent Brain Aneurysms?
While we can't control everything that might lead to a brain aneurysm, there are steps we can take to lower our risk. Let's explore some ways to keep our brain healthy and reduce the chances of an aneurysm.
- Healthy Eating: Just like putting good fuel in a car, eating healthy foods keeps our blood vessels strong. Fruits, vegetables, whole grains, and lean proteins are all great choices. Try to avoid too much salt, fat, and sugar.
- Regular Exercise: Staying active is like giving your blood vessels a good workout. It helps keep your blood pressure in check and your blood vessels in top shape. Activities like biking, swimming, or even just a brisk walk can make a big difference.
- Control Blood Pressure: High blood pressure can put extra stress on blood vessel walls. Keeping blood pressure under control is like avoiding heavy loads on a weak bridge. If you have high blood pressure, follow your doctor's advice and take any prescribed medication.
- Quit Smoking: Smoking is really bad for blood vessels. Quitting smoking can significantly reduce the risk of aneurysms.
- Limit Alcohol Consumption: Too much alcohol can weaken blood vessel walls and increase blood pressure. Moderation is key.
- Regular Check-Ups: If you have a family history of aneurysms or other risk factors, regular check-ups with your doctor can help catch any problems early.
- Manage Stress: High stress can also affect your blood pressure and overall health. Finding ways to relax and manage stress, like meditation, yoga, or just spending time doing things you enjoy, can be beneficial.
- Be Informed: Knowing the symptoms and risks of aneurysms can help you make better health choices.
FAQs
Hereditary and Genetic Factors
Are brain aneurysms hereditary?
There is a hereditary component to brain aneurysms, meaning that if a close family member has had one, your risk may be higher.
Are brain aneurysms genetic?
Certain genetic conditions can increase the risk of developing an aneurysm, but not all aneurysms are directly linked to genetic factors.
Prevalence and Risk
Are brain aneurysms fatal?
A ruptured brain aneurysm can be fatal, and prompt medical treatment is crucial.
Are brain aneurysms rare?
Brain aneurysms are not exceedingly rare; a significant number of adults may have small, unruptured aneurysms.
Are brain aneurysms common?
They are relatively common, but the majority do not rupture.
Can brain aneurysms happen to anyone?
Yes, they can occur in any individual, though certain factors may increase risk.
Who is at risk for brain aneurysm?
Risk factors include a family history of aneurysms, high blood pressure, smoking, and certain genetic conditions.
Symptoms and Detection
Are brain aneurysms painful?
Unruptured aneurysms often do not cause pain. A ruptured aneurysm can cause severe headache and other symptoms.
Where are most brain aneurysms located?
They commonly occur in the arteries at the base of the brain. Posterior communicating artery is commonest location.
Where is brain aneurysm pain located?
A sudden, severe headache (often described as the worst headache ever experienced) is a key symptom of a ruptured aneurysm.
Can brain aneurysms be detected?
Yes, through imaging tests like MRI or CT scans, especially if there are risk factors or symptoms.
Treatment and Management
Are brain aneurysms treatable?
Yes, there are several treatment options, including surgical clipping and endovascular coiling.
Can brain aneurysm be treated?
Treatment depends on the size, location, and risk of rupture.
Can brain aneurysms shrink?
Unruptured aneurysms typically do not shrink on their own.
Can you survive a brain aneurysm without surgery?
It depends on the aneurysm's size, location, and risk of rupture.
Why coil a brain aneurysm?
Coiling is a less invasive procedure than surgical clipping and is used to prevent blood flow into the aneurysm.
Prevention and Lifestyle
Can brain aneurysms be prevented?
While not all can be prevented, risk factors like high blood pressure and smoking can be managed.
What should you not do if you have a brain aneurysm?
Avoiding activities that could significantly raise blood pressure, such as heavy lifting or straining, is generally advised.
Comparisons and Related Conditions
Is brain aneurysm a stroke?
A ruptured aneurysm can lead to a type of stroke called a hemorrhagic stroke.
Brain aneurysm vs stroke, vs migraine, vs hemorrhage, vs blood clot, vs tumor, vs seizure:
These are all different medical conditions with distinct causes and symptoms, though they may share some similarities.
Additional Aspects
Brain aneurysm and stroke recovery:
Recovery depends on the severity of the aneurysm and the stroke.
Brain aneurysm and covid vaccine (Pfizer):
There's no established direct link between COVID-19 vaccines and an increased risk of brain aneurysms.
Brain aneurysm and alcohol:
Heavy alcohol use can increase blood pressure and potentially increase the risk of aneurysm rupture.
Brain aneurysm and dementia, pregnancy, cardiac arrest:
These are special conditions where managing an aneurysm may have different considerations.
Symptoms and Indicators
Brain aneurysm symptoms
Include severe headache, nausea, vision changes, and, if it ruptures, loss of consciousness.
Brain aneurysm coma
A severe rupture can lead to a coma.
Brain aneurysm uneven pupils:
This can be a sign of increased pressure in the brain due to a ruptured aneurysm.
Prognosis and Outcomes
Brain aneurysm surgery survival rate: Varies based on factors like the aneurysm's size and location, and the patient's overall health.
Do brain aneurysms kill you instantly?
Not always, but a rupture is a medical emergency requiring immediate attention.
Understanding Spastic Quadriplegia Cerebral Palsy
If you or someone you know has been diagnosed with cerebral palsy, it's essential to understand the different types and their impact. One severe form of cerebral palsy is spastic quadriplegia. This condition affects both the arms and legs, as well as the torso and face, making movements jerky and awkward. Children with spastic quadriplegia CP often have developmental disabilities and are unable to walk.
Spastic quadriplegia cerebral palsy is caused by brain damage or abnormal brain development. Factors like prematurity, fetal infections or stroke, maternal infections or medical conditions, exposure to toxins, or medical negligence can contribute to the development of this condition. Early interventions and treatments can benefit children with spastic quadriplegia, but they will require ongoing support throughout their lives.
What is Spastic Quadriplegic Cerebral Palsy?
Spastic quadriplegic cerebral palsy is the most severe form of spastic cerebral palsy, a condition that affects muscle tone and movement. Unlike other forms of cerebral palsy, spastic quadriplegia involves the impairment of all four limbs, including the legs, arms, trunk, and face in many cases. This extensive involvement of the body results in increased muscle tone and stiffness, making it challenging for individuals to perform daily activities.
One of the distinguishing characteristics of spastic quadriplegia is the presence of muscle stiffness and jerky movements, known as spasticity. The increased muscle tone and stiffness can significantly interfere with mobility and independence, affecting basic functions like walking, reaching, and grasping. Individuals with spastic quadriplegic cerebral palsy often require assistive devices and ongoing support to overcome the limitations caused by muscle stiffness.
Impact on Daily Life
Spastic quadriplegia cerebral palsy can have a profound impact on an individual's daily life. The muscle stiffness and limited range of motion make it difficult to perform tasks independently, such as getting dressed, eating, or even speaking. Additionally, the involvement of the face can lead to challenges in facial expressions and communication.
The severity of spastic quadriplegic cerebral palsy varies among individuals, with some being able to walk with assistance, while others may require a wheelchair for mobility. The level of functional impairment determines the support and interventions needed to improve quality of life.
Management and Treatment
Although there is no cure for spastic quadriplegia cerebral palsy, various interventions and treatments can help manage the condition and improve quality of life. The management approach typically involves a multidisciplinary team of healthcare professionals, tailored to address the individual's specific needs and challenges.
Treatment options for spastic quadriplegia cerebral palsy may include:
- Physical therapy to improve muscle strength, flexibility, and mobility.
- Occupational therapy to enhance daily living skills, such as self-care and fine motor control.
- Speech therapy to address communication difficulties and improve speech clarity.
- Medications to manage spasticity and alleviate associated symptoms.
- Assistive devices, such as braces or splints, to support mobility and improve posture.
A comprehensive treatment plan takes into account the individual's needs, goals, and overall health. Ongoing monitoring and adjustments may be necessary to ensure the best possible outcomes.
| Treatment Options | Description |
|---|---|
| Physical Therapy | Focuses on improving muscle strength, flexibility, and mobility through exercises and specialized techniques. |
| Occupational Therapy | Helps individuals develop independence in daily activities and enhances fine motor skills. |
| Speech Therapy | Targets communication difficulties and improves speech clarity through specialized exercises and techniques. |
| Medications | Prescribed to manage spasticity and alleviate associated symptoms. |
| Assistive Devices | Braces, splints, or mobility aids to support mobility and improve posture. |
How Severe is Spastic Quadriplegia Cerebral Palsy?
Spastic quadriplegia cerebral palsy is considered the most severe form of cerebral palsy due to its impact on multiple areas of the body. Children with this condition often experience significant motor impairments, making walking impossible. They may also have associated conditions such as speech difficulties or seizures. The severity of spastic quadriplegia CP requires lifelong support and care to manage developmental disabilities and associated complications.
The Impact of Spastic Quadriplegia Cerebral Palsy
Spastic quadriplegia cerebral palsy affects both arms, legs, and often the torso and face. The increased muscle tone and stiffness lead to jerky and awkward movements, making daily activities challenging for individuals with this condition. The severity of spastic quadriplegia CP can vary, but it significantly impacts mobility, independence, and overall quality of life.
Children with spastic quadriplegia CP are unable to walk and may require the use of assistive devices, such as wheelchairs or walkers, to move around. The limitations in mobility can affect their participation in various activities, hindering their social and emotional development.
| Severity of Spastic Quadriplegia Cerebral Palsy | Impact |
|---|---|
| Motor impairments | Movements are jerky, uncoordinated, and characterized by increased muscle tone and stiffness. |
| Speech difficulties | Communication can be challenging, with speech impediments or language disorders often present. |
| Seizures | Individuals with spastic quadriplegia CP may experience seizures, which can further complicate their condition. |
| Developmental disabilities | Children with spastic quadriplegia CP often have accompanying developmental disabilities, requiring ongoing support and management. |
Managing the severity of spastic quadriplegia CP involves a multidisciplinary approach. Physical therapy plays a crucial role in improving motor function, flexibility, and range of motion. Occupational therapy focuses on enhancing independence in daily activities, while speech therapy helps individuals communicate effectively. Medications may be prescribed to manage spasticity and associated conditions. In severe cases, surgical interventions may be necessary to address muscle tightness or joint deformities.
While there is no cure for spastic quadriplegia cerebral palsy, ongoing support and care can help individuals with this condition lead fulfilling lives. It is essential for individuals with spastic quadriplegia CP and their families to work closely with healthcare professionals to develop personalized treatment plans and ensure access to necessary resources and therapies.
What Causes Cerebral Palsy?
Cerebral palsy, including spastic quadriplegia cerebral palsy, is primarily caused by brain damage or abnormal brain development. Several factors contribute to the development of this condition, which affects individuals from different backgrounds, including:
- Prematurity: Babies born prematurely are at a higher risk of developing cerebral palsy due to their underdeveloped brains.
- Fetal Infections or Stroke: Infections during pregnancy or strokes that occur in utero can lead to brain damage, resulting in cerebral palsy.
- Maternal Infections or Medical Conditions: Maternal infections, such as rubella or cytomegalovirus, as well as medical conditions like thyroid disorders or epilepsy, can increase the risk of cerebral palsy in the baby.
- Exposure to Toxins: Certain toxins, such as lead or mercury, can interfere with the normal development of the brain, potentially causing cerebral palsy.
- Medical Negligence: In some cases, medical negligence during childbirth, such as oxygen deprivation or improper handling of a baby, can result in brain damage leading to cerebral palsy.
Brain damage during specific periods of development, such as between 26 and 34 weeks of gestation, can lead to white matter lesions or holes in the brain. These abnormalities affect the transmission of signals to the body, resulting in motor impairments seen in cerebral palsy.
Maternal high blood pressure during pregnancy can also increase the risk of fetal stroke and subsequent cerebral palsy.
Understanding the causes of cerebral palsy is crucial for prevention, early interventions, and providing support to individuals and families affected by this condition.
| Cause | Description |
|---|---|
| Prematurity | Babies born prematurely are at a higher risk of developing cerebral palsy due to their underdeveloped brains. |
| Fetal Infections or Stroke | Infections during pregnancy or strokes that occur in utero can lead to brain damage, resulting in cerebral palsy. |
| Maternal Infections or Medical Conditions | Maternal infections or medical conditions can increase the risk of cerebral palsy in the baby. |
| Exposure to Toxins | Certain toxins can interfere with the normal development of the brain, potentially causing cerebral palsy. |
| Medical Negligence | Medical negligence during childbirth can result in brain damage leading to cerebral palsy. |
Symptoms of Spastic Quadriplegia
The symptoms of spastic quadriplegia are more severe compared to other types of cerebral palsy. Individuals with this condition may experience:
- Rapid muscle contractions and muscle tightness
- Difficulty with limb movement and coordination
- Limb "scissoring" - when the legs cross, making walking difficult
- Speech impediments or language disorders
- Seizures
- Cognitive disabilities
- Other associated complications
The severity of symptoms can vary among individuals, and early identification is crucial for appropriate interventions and support.
Common Symptoms of Spastic Quadriplegia
| Symptoms | Description |
|---|---|
| Rapid muscle contractions | Uncontrolled and involuntary muscle movements |
| Muscle tightness | Increased muscle tone and stiffness |
| Difficulty with limb movement and coordination | Challenges with performing smooth and coordinated movements |
| Limb "scissoring" | Crossing of the legs, making walking difficult |
| Speech impediments or language disorders | Difficulties with speaking or understanding language |
| Seizures | Episodes of abnormal electrical activity in the brain |
| Cognitive disabilities | Challenges with learning, thinking, and problem-solving |
| Other associated complications | Additional medical conditions or impairments that may coexist |
Diagnosing and Treating Spastic Quadriplegia
Diagnosing spastic quadriplegia typically occurs during infancy when significant delays in development are observed. A comprehensive evaluation process is conducted to confirm the diagnosis and rule out other conditions. This includes a thorough physical examination, review of medical history, and brain imaging tests such as CT scans and MRIs.
Once the diagnosis is confirmed, a multidisciplinary approach is adopted for the treatment of spastic quadriplegia. This approach combines various therapies and interventions to address the individual needs and challenges faced by those with this condition.
Physical therapy plays a pivotal role in improving motor function, flexibility, and range of motion. Through tailored exercises and techniques, physical therapists help individuals with spastic quadriplegia strengthen their muscles, improve coordination, and enhance overall physical abilities. Regular physical therapy sessions can significantly enhance mobility and independence.
Occupational therapy focuses on developing independence in daily activities. Occupational therapists work with individuals to improve fine motor skills, adapt to daily challenges, and maximize functionality in areas such as self-care, school, work, and leisure activities. They may introduce tools and assistive devices to facilitate independent living and enhance overall quality of life.
Speech therapy is essential for individuals with spastic quadriplegia to improve communication skills. Speech-language pathologists assess speech and language abilities and develop personalized therapy plans to address specific challenges such as articulation, fluency, or language disorders. By enhancing communication skills, individuals can better express themselves and engage effectively with others in various social contexts.
In some cases, medications may be prescribed to manage spasticity, alleviate associated conditions, or control seizures. Assistive devices and technology, such as orthotics or mobility aids, can also be beneficial in enhancing mobility and independence.
In severe cases where muscle tightness or joint deformities persist despite therapy and medication, surgery may be considered. The goal of surgery is to correct physical abnormalities and improve function. Orthopedic procedures can help release tight muscles, correct bony deformities, or improve joint alignment, allowing for better movement and reduced discomfort.
Overall, the management of spastic quadriplegia involves a comprehensive and individualized treatment plan that addresses physical, functional, and communication needs. Through a collaborative effort among healthcare professionals, individuals with spastic quadriplegia can improve their abilities, achieve greater independence, and lead fulfilling lives.
| Treatment Options for Spastic Quadriplegia | Description |
|---|---|
| Physical Therapy | Improves motor function, flexibility, and range of motion through tailored exercises and techniques. |
| Occupational Therapy | Fosters independence in daily activities, enhances fine motor skills, and introduces assistive devices for better functionality. |
| Speech Therapy | Enhances communication skills, addresses speech or language disorders, and improves overall social interaction. |
| Medication | Manages spasticity, associated conditions, and controls seizures. |
| Surgery | Corrects physical abnormalities, improves function, and resolves persistent muscle tightness or joint deformities. |
Conclusion
Spastic quadriplegia cerebral palsy can have a profound impact on the lives of individuals, often necessitating lifelong support and care. While there is no cure for this condition, there are various treatment options and interventions available to help improve mobility, foster independence, and enhance overall quality of life.
It is crucial for individuals with spastic quadriplegia and their families to collaborate closely with healthcare professionals to develop personalized treatment plans. Through a multidisciplinary approach, including physical therapy, occupational therapy, speech therapy, and medication, individuals with spastic quadriplegia can make significant strides in managing symptoms and improving functionality.
Despite the challenges posed by spastic quadriplegia cerebral palsy, with the right support and treatment options, many individuals can lead fulfilling lives. It is important to remember that every person's journey is unique, and a comprehensive treatment approach tailored to individual needs is essential to maximize their potential and well-being.
FAQ
What is spastic quadriplegic cerebral palsy?
Spastic quadriplegic cerebral palsy is a severe form of cerebral palsy that affects both arms, legs, and often the torso and face. It is characterized by increased muscle tone and stiffness, making movements jerky and awkward. Children with this condition usually have developmental disabilities and are unable to walk.
How severe is spastic quadriplegia cerebral palsy?
Spastic quadriplegia cerebral palsy is considered the most severe form of cerebral palsy due to its impact on multiple areas of the body. Children with this condition experience significant motor impairments, making walking impossible. They may also have associated conditions such as speech difficulties or seizures.
What causes cerebral palsy, including spastic quadriplegia?
Cerebral palsy, including spastic quadriplegia, is caused by brain damage or abnormal brain development. Various factors can contribute to the development of this condition, including prematurity, fetal infections or stroke, maternal infections or medical conditions, exposure to toxins, or medical negligence.
What are the symptoms of spastic quadriplegia?
Symptoms of spastic quadriplegia include rapid muscle contractions, muscle tightness, difficulty with limb movement and coordination, limb "scissoring," speech impediments or language disorders, seizures, cognitive disabilities, and other associated complications. The severity of symptoms can vary among individuals.
How is spastic quadriplegia diagnosed and treated?
Spastic quadriplegia is generally diagnosed during infancy when significant delays in development are observed. A thorough physical examination, medical history review, and brain imaging tests can help confirm the diagnosis. Treatment for spastic quadriplegia includes a multidisciplinary approach, focusing on physical therapy, occupational therapy, speech therapy, medication, assistive devices and technology, and, in some cases, surgery.
Can spastic quadriplegia be cured?
There is no cure for spastic quadriplegia cerebral palsy. However, early interventions and comprehensive treatment approaches can help improve mobility, independence, and overall quality of life for individuals with this condition. Lifelong support and care are often necessary.
Source Links
- https://www.cerebralpalsyguidance.com/cerebral-palsy/types/spastic-quadriplegia/
- https://www.medicalnewstoday.com/articles/spastic-quadriplegic-cerebral-palsy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9868261/
Treatment Of A Ruptured Aneurysm Or Subarachnoid Hemorrhage (SAH): A Simplified Guide
What Is Subarachnoid Hemorrhage?
Subarachnoid hemorrhage (SAH) is a medical emergency that often results from a ruptured brain aneurysm. This critical condition involves bleeding into the space surrounding the brain, leading to severe complications, including death or long-term health issues. Understanding the treatment of a ruptured aneurysm is essential for improving outcomes and managing this life-threatening condition.
To learn more about what a brain aneurysm is, you can visit What is a Brain Aneurysm?.
Initial Steps in SAH Management
When a patient arrives at a healthcare facility with symptoms of SAH, the first priority is stabilizing their condition. This involves:
- Ensuring the patient can breathe: In severe cases, intubation and mechanical ventilation may be necessary.
- Stabilizing heart function: Maintaining stable heart function is crucial.
- Seizure management: Immediate treatment of seizures, if present, is essential.
Assessing the Severity of SAH
Healthcare professionals use specific grading systems to determine the severity of SAH. These systems assess the neurological impact and the extent of bleeding, guiding the approach to treatment.
Critical Care Management Strategies
The treatment of a ruptured aneurysm in a critical care setting involves several key strategies:
- Blood Pressure Control: Controlling blood pressure is vital to prevent further bleeding and ensure adequate blood flow to the brain.
- Aneurysm Repair: The primary goal is to secure the aneurysm through surgical clipping or endovascular coiling to prevent rebleeding. To understand these methods in detail, visit Endovascular Aneurysm Repair Coiling VS Clipping.
- Monitoring and Prevention of Complications: Continuous monitoring for neurological changes is essential, as is the prevention of complications like vasospasm, a condition where blood vessels constrict, reducing blood flow to the brain.
- Fluid Management: Maintaining proper fluid and electrolyte balance is crucial to prevent dehydration and other complications.
- Medication: Medications such as Nimodipine are used to improve outcomes, even though their exact mechanism in SAH treatment is not fully understood.
- Pain Control: Effective pain management is crucial for patient comfort and recovery.
Treating the Aneurysm
The risk of rebleeding after an aneurysmal SAH is significant, making the treatment of a ruptured aneurysm an urgent priority. Ideally, the aneurysm should be repaired within the first 24 hours after admission. Two main approaches are used:
- Surgical Clipping: A small clamp is placed at the base of the aneurysm to isolate it from normal blood flow.
- Endovascular Coiling: This less invasive method involves inserting coils into the aneurysm to induce clotting and seal it off.
For more information on the various methods, you can read about Endovascular Aneurysm Repair Coiling VS Clipping.
In cases where immediate surgery is not possible, medications like tranexamic acid or aminocaproic acid may be used temporarily, but typically not for more than 72 hours.

Early Complications of SAH
Rebleeding
One of the most severe early complications is rebleeding, which can occur within the first 24 hours after the initial hemorrhage. Factors that increase the risk of rebleeding include:
- Delay in treating the aneurysm
- Poor neurological status upon admission
- Large aneurysm size
- High blood pressure
- Presence of blood within the brain or ventricles
- Incomplete obliteration of the aneurysm during treatment
Rebleeding often leads to worse outcomes and can be fatal.
Vasospasm and Delayed Cerebral Ischemia
Another significant complication is delayed cerebral ischemia, often resulting from vasospasm. This typically occurs between 4 and 14 days after the SAH. Managing vasospasm involves several strategies:
- Nimodipine: Used to reduce the risk of poor outcomes.
- Euvolemia Maintenance: Ensuring the right balance of body fluids.
- Hemodynamic Augmentation: Increasing blood pressure to improve blood flow to the brain.
- Balloon Angioplasty and Vasodilators: Used in severe cases to open narrowed blood vessels.
Managing Elevated Intracranial Pressure (ICP)
When bleeding increases pressure inside the skull, known as elevated intracranial pressure (ICP), it can be dangerous and requires prompt management:
- Draining Excess Fluid (CSF): Doctors may use an external ventricular drain (EVD) to remove fluid buildup in the brain.
- Medication to Reduce Fluid: Certain medications help draw out fluid from the brain.
- Surgery: In severe cases, part of the skull may be temporarily removed to relieve pressure.
- Long-Term Solutions: If the problem persists, a permanent drainage solution like a shunt might be necessary.

What Is Hydrocephalus?
Hydrocephalus, where fluid becomes trapped in the brain, can affect about 1 in 5 SAH patients. Treatment options include using drains or closely monitoring the patient to determine if surgery is needed.
The Salt and Water Balance: Managing Hyponatremia
Hyponatremia, a condition characterized by low sodium levels in the blood, is a common complication after a brain hemorrhage. Managing this condition involves restoring the salt-water balance, often with the help of salt solutions.
When Seizures Strike
Types Of Seizures can occur after SAH, especially if the bleeding was significant or if the aneurysm was located in certain areas of the brain. Doctors use carefully selected medications to prevent further seizures without worsening the patient's condition.
Understanding the Impact of SAH: What Are the Long-Term Effects?
Early Challenges and Survival
- Immediate Risks: SAH can be life-threatening, with some patients not surviving long enough to receive hospital care.
- Early Hospital Mortality: The first few days in the hospital are critical, with complications like rebleeding, vasospasm, increased intracranial pressure, seizures, and heart issues posing significant risks.
Long-Term Outlook
Surviving SAH is just the first step. While survival rates have improved, SAH survivors often face a higher risk of health problems compared to the general population.
Dealing with Long-Term Effects
- Brain and Cognitive Challenges: Memory problems and difficulties with thinking and decision-making are common after SAH.
- Mood and Sleep: Depression, anxiety, and sleep problems can significantly affect the quality of life.
- Seizures and Epilepsy: A small number of survivors may develop epilepsy.
- Sense of Smell: Some patients may lose their sense of smell, especially after aneurysm surgery.
The Risk of Another Bleed
There’s a small chance of developing another aneurysm or experiencing a rebleed. Regular check-ups and monitoring are crucial. Learn more about Brain Aneurysms and related complications here.
Screening for Family Members
If you've had a SAH, your close family members might have a higher risk of experiencing it too. Doctors may suggest screening for them, especially if there’s a family history of brain aneurysms.
Final Thoughts
Dealing with SAH and its aftermath is a complex and challenging journey. However, with modern medical care, the chances of surviving and living a fulfilling life after SAH are better than ever. It's important to stay hopeful, remain connected with your medical team, and understand that each person's journey is unique. For more information on the treatment of a ruptured aneurysm, please visit What is a Brain Aneurysm?.
Amyotrophic Lateral Sclerosis (ALS): A Guide on Motor Neuron Disease.
What is Amyotrophic Lateral Sclerosis (ALS)?
Amyotrophic Lateral Sclerosis, or ALS, is a disease of spinal cord motor cells. Here's a closer look:
- A Nerve Disease: ALS is a condition that affects the nerves in our body, specifically the ones that control our muscles. Think of these nerves as tiny messengers that tell our muscles to move. It primarily affects the motor cells in the spinal cord.
- Muscle Weakness: People with ALS find it increasingly hard to move their arms legs, and even to talk or breathe. It's like the messages to the muscles get lost.
- Progressive Condition: ALS gets worse over time. This means Amyotrophic Lateral Sclerosis Symptoms start mild but gradually become more severe.
- Not Very Common: ALS is a rare disease. It only happens to a few people, but understanding it is still essential.
- Two Types: There are two main types of ALS - sporadic (the most common, and it can happen to anyone) and familial (which is inherited and happens in families).
Named After a Baseball Player, It's also known as Lou Gehrig's disease, named after a famous baseball player with ALS.
In ALS, the nerve cells (neurons) that control muscles weaken and die. This means the muscles don’t receive the signals they need to move, leading to muscle weakness. It's like having a remote control that slowly stops working.
Who Gets Amyotrophic Lateral Sclerosis ALS?
Understanding who can get Amyotrophic Lateral Sclerosis (ALS)
- Mainly Affects Adults: ALS is more common in adults, typically showing up between the ages of 40 and 70. The disease usually chooses to visit people in the middle or later part of their life journey.
- Slightly More Common in Men: While both men and women can get ALS, it's a bit more common in men. Think of it like flipping a coin where heads (men getting ALS) come up just a few times more often than tails.
- Familial and Sporadic Types: Most cases are sporadic, which means they happen randomly without an apparent reason. A smaller number, about 5-10%, are familial, meaning the disease runs in the family.
- Geographic and Occupational Factors: Some studies suggest that where you live and your job might play a role, but this is like having only a few pieces of a big puzzle.
- We Don’t Know Why for Sure: The exact cause of ALS is still a mystery. Scientists believe it's a mix of genetics and environmental factors.
What Happens in Amyotrophic Lateral Sclerosis ALS?
Let's dive into what happens in the body when someone has Amyotrophic Lateral Sclerosis (ALS).

- Nerve Cells Break Down: In ALS, the nerve cells (neurons) in the brain and spinal cord that tell muscles to move start to weaken and eventually die. It's as if the body's internal telephone lines are getting disconnected.
- Muscles Get Weaker: As these nerves stop working, the muscles don't receive the messages they need to move. Gradually, the muscles weaken, shrink, and become less able to do their job. Imagine a muscle is like a balloon slowly losing air.
- Different Symptoms for Everyone: Like everyone is unique, ALS affects people differently. One person might have trouble holding a pencil, while another might find speaking more challenging.
- Difficulty with Daily Tasks: As the muscles get weaker, simple things like walking, talking, eating, and even breathing can become challenging. The body's muscles slowly forget how to do their everyday jobs.
- Affects Voluntary Muscles: ALS mainly impacts the muscles we can control, like those in our arms, legs, and face. This is different from involuntary muscles, which do things like keep our heart beating without us thinking about it.
Amyotrophic Lateral Sclerosis Symptoms
- Nerve Damage: ALS mainly happens because the nerves that control muscles start to weaken.
- Muscle Weakness: A common early sign. People might find it hard to:
- Use their hands and fingers, Like having trouble buttoning a shirt or writing.
- Moving arms and legs easily: Difficulty climbing stairs or lifting things.
- Muscles Get Smaller: The muscles might look smaller because they're not used as much.
- Stiff Muscles and Overactive Reflexes: Muscles might feel tight, and reflexes, like the knee-jerk reaction, could be stronger.
- The trouble with Speaking and Swallowing: Speaking might become unclear, and swallowing food can be hard. Some people might drool more or find it hard to control their emotions.
- Muscle Twitching: Tiny, involuntary muscle movements, often in the arms or legs.
- Breathing Issues: It can become hard to breathe deeply, especially as ALS gets more advanced.
- Thinking and Behavior Changes: Some people might experience changes in thinking or acting.
- Feeling Tired: Tiredness can happen, even without much activity.
- Occasional Pain and Unusual Sensations: Some people might feel muscle cramps or a sort of pins-and-needles feeling, but it's not very common.
How Neurologists Diagnose Amyotrophic Lateral Sclerosis ALS
Diagnosing Amyotrophic Lateral Sclerosis (ALS) is a complex process. Doctors have to look at lots of clues because there isn't just a straightforward test for ALS. Here's how they do it:
- Check Symptoms: First, doctors listen to the person's symptoms - like muscle weakness, trouble speaking, or twitching.
- Physical Exam: They do a physical check to see how the muscles and reflexes work.
- Medical History: Doctors ask about the person's health history and if anyone in their family has had similar problems.
- Muscle and Nerve Tests: Special tests, like EMG (electromyography), check how well the nerves and muscles work.
- Imaging Tests: Sometimes, they do MRI scans or blood tests to ensure the symptoms aren't caused by something else.
- Rule Out Other Diseases: ALS can look like other diseases, so doctors check to ensure it’s not something else. It's like making sure they have the right puzzle piece.
- Repeat Tests: Sometimes, doctors need to do tests more than once over time to see how symptoms are changing.
Amyotrophic Lateral Sclerosis Diagnosis takes time and careful checking. No single test can tell for sure, so doctors look at all the different information they gather to make a diagnosis. Be patient and trust your neurologist.
Living with Amyotrophic Lateral Sclerosis ALS
Living with Amyotrophic Lateral Sclerosis (ALS) is a big challenge, both for the person who has it and their family. Since there's no cure for ALS right now, the focus is on making life as comfortable and fulfilling as possible. Here's how people manage life with ALS

- Medications: Doctors may prescribe medicines. These can't cure ALS, but they can slow it down a bit and help with some symptoms, like muscle cramps or stiffness.
- Physical Therapy: This is like a particular exercise with a therapist. It helps keep the muscles as strong as possible and makes moving around easier.
- Speech Therapy: If talking gets hard, speech therapists can help. They teach different communication methods, like using a computer or a particular board.
- Eating Changes: Dietitians can suggest softer foods or even special nutritional drinks if swallowing food becomes tough. It's all about ensuring the person gets enough to eat without trouble.
- Breathing Support: Sometimes, people with ALS need help with breathing. Doctors might give them a machine to help get more air into their lungs.
- Home Modifications: Making changes at home, like ramps for wheelchairs or grab bars in the bathroom, can make daily life safer and more accessible.
- Support Groups: Talking with others who understand what it's like can be helpful. Support groups offer a place to share tips and encouragement.
- Caregiver Support: Family members and caregivers also need support. It's a tough job, and getting help, taking breaks, and looking after their health is super important.
How Can We Help Someone with ALS?
Helping someone with Amyotrophic Lateral Sclerosis (ALS) is about understanding, patience, and kindness. Here are some ways we can support and help make their life easier and more comfortable:
- Understanding and Patience: Understand that things they used to do easily might now be difficult or take longer. Be patient when they need more time to speak or move.
- Lend a Hand: Offer help with everyday tasks and let them do what they can by themselves. It's about finding the right balance between helping and encouraging independence.
- Listening is Caring: Sometimes, being there to listen can mean a lot. Give them your full attention if they want to talk about their feelings or frustrations.
- Educate Yourself: Learn more about ALS. The more you know, the better you can understand what they're going through.
- Make Their Space Comfortable: Adjust their living space so it’s safe and easy to get around. Moving furniture to create clear paths and adding grab bars in the bathroom can make a big difference.
- Join in Activities: Share activities they enjoy and can still participate in. It could be watching their favourite movie together or listening to music.
- Support with Communication: If they have trouble speaking, learn their communication methods, like alphabet boards or speech-generating devices.
- Plan for the Future: Talk about what they want regarding care and support as ALS progresses. It’s important to respect their wishes and make plans together.
- Take Care of Yourself: Supporting someone with ALS can be challenging. Make sure you also take time to rest and do things you enjoy. It’s like putting on your oxygen mask first before helping others.
Helping someone with ALS is about providing support, love, and understanding. It’s not just about physical help; it’s also about emotional support. Remember, your care and presence can make a big difference in their life.
FAQs
Can ALS be cured?
Currently, there is no cure for ALS. But doctors and scientists are working hard to find one.
Can ALS kill you?
Yes, ALS is a severe disease that eventually leads to death, often due to breathing problems.
Can ALS be prevented?
Right now, we don't know how to prevent ALS because we don't fully understand what causes it.
Can ALS symptoms come and go?
Generally, ALS symptoms don’t come and go. Once they start, they usually continue and often get worse over time.
Can ALS be hereditary?
In some cases, yes. About 5-10% of ALS cases are familial, which means they can be inherited from parents.
Can ALS go into remission?
No, ALS does not go into remission. Symptoms usually get steadily worse.
Can ALS be reversed?
Currently, there's no way to reverse the damage caused by ALS.
How do ALS patients die?
Many people with ALS die from respiratory failure, which means their lungs stop working correctly.
How do ALS patients communicate?
They might use speech-generating devices, computer programs, or boards with letters or pictures to communicate.
How do ALS patients use the bathroom?
They might need help from others or use special equipment to help them use the bathroom as the disease progresses.
How is ALS diagnosed?
Doctors use a combination of physical exams, medical history, and tests like EMG (to check muscle activity) and MRI to diagnose ALS.
How does ALS affect the body?
ALS affects the nerves that control muscles, leading to muscle weakness, difficulty moving, speaking, swallowing, and eventually breathing.
Why does ALS happen?
We need to understand why fully. It might be a mix of genetic and environmental factors.
ALS and dementia:
Some people with ALS can also develop problems with thinking and memory, similar to dementia.
ALS and MS (Multiple Sclerosis):
Both affect the nervous system, but they are different diseases. MS affects the brain and spinal cord's protective covering, while ALS affects nerve cells that control muscles.
ALS and COVID:
People with ALS may be more vulnerable to complications if they get COVID due to their weakened respiratory systems.
ALS and exercise:
Exercise can help maintain muscle strength and mobility in ALS, but it should be gentle and supervised by a healthcare professional.
ALS and co (companionship or cohabitation):
Support and companionship are essential for people with ALS, as the disease can be isolating.
ALS and Lyme disease:
Lyme disease can sometimes mimic ALS symptoms, but they are different conditions.
ALS and constipation:
Constipation can be a problem for people with ALS, often due to reduced mobility and changes in diet.
ALS compared to MS:
ALS primarily causes muscle weakening and loss, while MS can cause a broader range of symptoms, including vision problems and numbness.
ALS compared to Parkinson's:
Parkinson's mainly affects movement, causing tremors and stiffness. ALS leads to muscle weakening and loss.
How is MS different from ALS?
MS can be managed and sometimes goes into remission, which doesn’t happen with ALS. MS symptoms vary more and include problems with vision and balance.
Is ALS similar to MS?
They have similarities in affecting the nervous system, but their causes and progression differ.
ALS-like diseases:
There are other motor neuron diseases similar to ALS, like progressive bulbar palsy and primary lateral sclerosis.
Is ALS like Parkinson's?
They both affect movement but in different ways. Parkinson's usually starts with tremors, while ALS begins with muscle weakness.
Is ALS like Huntington's disease?
Both are neurodegenerative, but Huntington's disease also affects mental abilities and behaviour, which is less common in ALS.
ALS specialist near me:
Contact Dr. Chandril Chugh, American Trained Adult Neurologist.
ALS with dementia:
Some people with ALS can develop symptoms like dementia, affecting their thinking and memory.
ALS without weakness:
ALS almost always causes muscle weakness. If there's no weakness, it might be a different condition.
ALS with normal EMG:
It's rare, but some early cases of ALS might have a normal EMG (a test that checks muscle activity) initially.
ALS with bulbar onset:
Bulbar onset ALS means the symptoms start with speech and swallowing difficulties.
ALS with sensory symptoms:
ALS usually doesn't cause sensory symptoms like numbness or tingling, which are more common in diseases like MS.
ALS with bulbar involvement:
This means ALS is affecting the muscles used for speaking and swallowing.
ALS with Parkinson's:
It's uncommon, but someone can have both ALS and Parkinson's disease.
ALS without muscle weakness:
ALS always involves muscle weakness; if there's no weakness, it's likely not ALS.
ALS without fasciculations:
Muscle twitching (fasciculations) is common in ALS but might not be present in every case.
ALS without feeding tube:
Some people with ALS might not need a feeding tube, especially in earlier stages or if swallowing isn't severely affected.
ALS without treatment:
Without treatment, ALS symptoms will progress. While there's no cure, treatments can help manage symptoms and improve quality of life.
ALS without bulbar symptoms:
ALS can occur without initially affecting speech and swallowing (bulbar muscles).
ALS without upper motor neuron signs:
ALS usually involves both upper and lower motor neurons, but in some cases, the signs might be more subtle.
ALS without spasticity:
Spasticity (muscle stiffness) is common in ALS but not always present.