How Pain and Spine Specialists Can Help Manage Chronic Pain
If you're one of the many adults dealing with ongoing back pain, there's hope. Pain and spine…
Benefits of Interventional Pain Treatments for Chronic Pain Sufferers
If you're one of the millions struggling with chronic pain, you know how tough it can be.…
Effective Strategies for Bulging Disc Pain Relief
Dealing with a bulging disc can be tough. But, there are ways to find relief and manage the pain.…
Comprehensive Guide to Slipped Disc Pain Relief
If you're feeling the pain of a slipped disc, you're not alone. Many people suffer from slipped…
7 Tips for Instant Back Pain Relief: Quick and Easy Solutions
Have you ever felt a sudden sharp ache in your back while getting out of bed or sitting at your…
Top Solutions for Managing Back Pain at Home
Back pain is a common issue in India, affecting many people. There are effective home remedies to…
Finding the Best Lower Back Pain Specialist Near You
Finding the right lower back pain specialist near you in India can greatly improve your health.…
How to Find Effective Back Pain Management in Your Area
Finding the right treatment for back pain is key to feeling better and living better. Whether…
How to Find the Best Pain Doctors Near You
Are you tired of waiting too long? Check out pain management clinics with options for male or…
Understanding ADHD Insomnia: Causes and Solutions
If you or someone close to you has ADHD, you might know how hard sleep issues can be. ADHD is a…
How Pain Management Clinics Can Help Alleviate Chronic Pain
If you're facing ongoing or chronic pain, you're not alone. Pain management clinics in India are…
Men's Mental Health: Why It’s Important to Seek Help | Dr. Chandril Chugh
Men's mental health is a big issue that often gets ignored. This is because of societal stigma and…
Causes of Depression in Men: Uncovering the Triggers | Dr. Chandril Chugh
Dr. Chandril Chugh is a top expert in men's mental health. He knows how depression affects men's…
Is Postpartum Depression Genetic? What You Should Know | Dr. Chandril Chugh
Dr. Chandril Chugh is a top expert in mental health. He has spent his career studying women's…
Depression in Young Men: Identifying the Red Flags | Dr. Chandril Chugh
Depression affects about 10% of men under 25. Dr. Chandril Chugh is a leading expert in mental…
Community Resources for Mental Health Support | Dr. Chandril Chugh
Your mental health is key to feeling good. It's about how you think, feel, and act. Many adults in…
Best Therapy for Depression: Effective Treatments Explained | Dr. Chandril Chugh
Finding the right therapy for depression is a big step. Dr. Chandril Chugh is here to help. He…
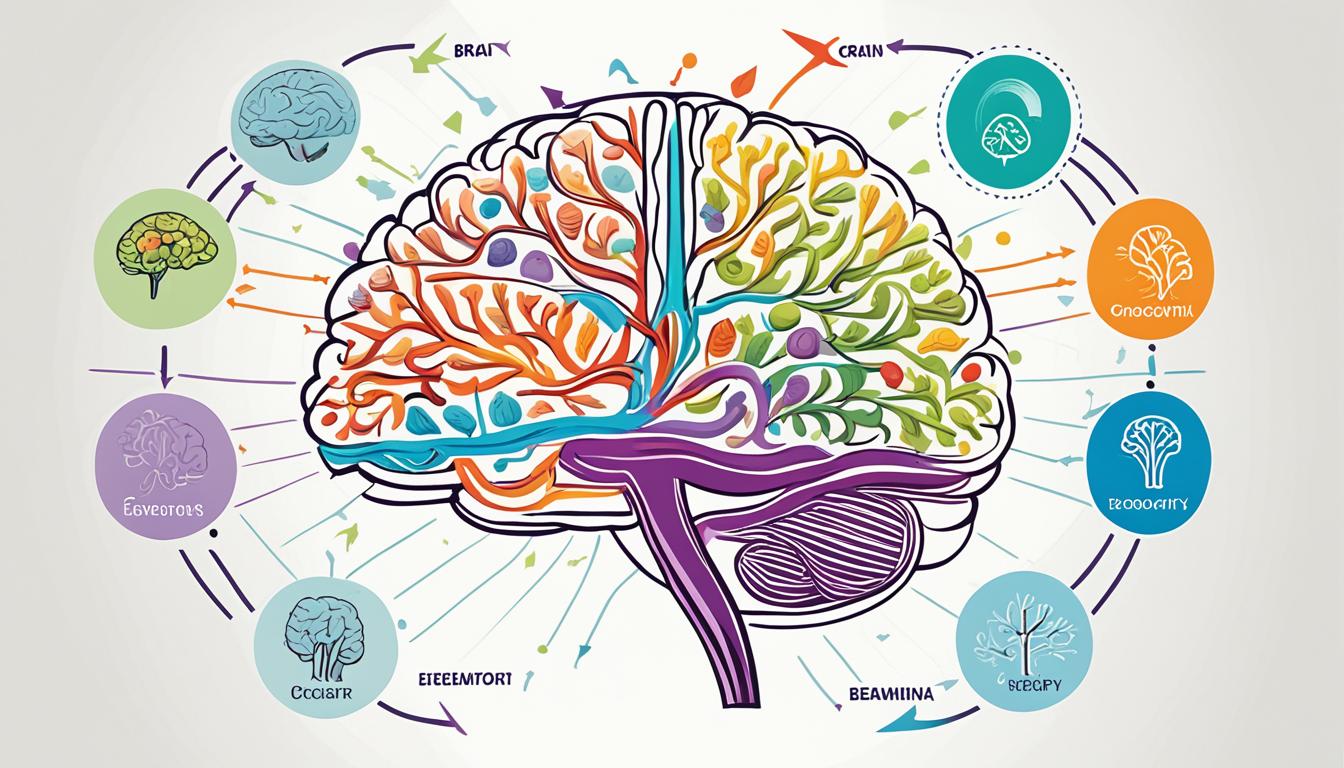
Electroconvulsive Therapy for Depression: What to Expect | Dr. Chandril Chugh
If you're dealing with severe or hard-to-treat depression, you might have heard of…
Depression Symptoms in Men: A Complete Overview | Dr. Chandril Chugh
Depression is a serious mental health issue that affects many people. It can change how someone…
Manic Depression in Men: Signs and Treatment Options | Dr. Chandril Chugh
Manic depression, also known as bipolar disorder, affects men deeply. It causes big mood swings.…
Best Therapy for Anxiety and Depression: A Comprehensive Guide | Dr. Chandril Chugh
Dealing with anxiety and depression can be tough. But, with the right help, you can feel better.…
Interpersonal Therapy for Depression: How It Works | Dr. Chandril Chugh
Depression is a silent battle that millions face every day. It affects their well-being and daily…
Breastfeeding and Postpartum Depression: What You Should Know | Dr. Chandril Chugh
Breastfeeding is known for its many benefits. But it can also affect your mental health. About…
An Introduction to Child Psychology: Understanding the Basics
Child psychology is at the core of human growth and development. It's about how children think,…
How to Heal After a Breakup: Tips for Moving On
Breakups can be tough, even if the relationship was ending. Losing your partner means losing shared…
Understanding Family Systems Therapy: A Comprehensive Guide
From the start, family plays a key role in your life. It shapes your emotional health and personal…
Postpartum Depression Bipolar Disorder: What’s the Connection? | Dr. Chandril Chugh
Being a new mom is both joyful and tough. The birth of a child is a big change. It can also lead to…
Postpartum Depression Relaxation Techniques: Finding Relief | Dr. Chandril Chugh
Postpartum depression affects up to 15% of new moms. It brings sadness, anxiety, and tiredness.…
Young Adult Mental Health: How to Identify & Treat Issues | Dr. Chandril Chugh
Young adulthood is a tough time for mental health. But, with the right help, you can get through…
Therapy Treatment for Depression: Exploring Your Options | Dr. Chandril Chugh
If you're fighting depression, you're not alone. Millions worldwide face this mental health battle.…
Signs of Depression in Men: How to Identify Them | Dr. Chandril Chugh
Depression is a serious mental health issue that affects both men and women. But it shows up…
Postpartum Depression Rage: Understanding & Managing It | Dr. Chandril Chugh
Being a new mom can bring both joy and challenges. One big issue many face is postpartum depression…
Low Testosterone and Depression in Men: Exploring the Link | Dr. Chandril Chugh
Have you ever felt unusually tired, irritable, or lost interest in things you once enjoyed? What if…
Postpartum Depression Herbal Treatment: Natural Remedies | Dr. Chandril Chugh
Welcoming a new life is a joy, but it can also bring big challenges for new moms. Postpartum…
Symptoms of Depression in Children: What Parents Need to Know | Dr. Chandril Chugh
Depression in children is a serious issue. It can really affect a child's happiness and health. The…
National Men’s Mental Health Month: Why It’s Important | Dr. Chandril Chugh
National Men's Mental Health Month is in June. It's a big push to help men feel better mentally.…
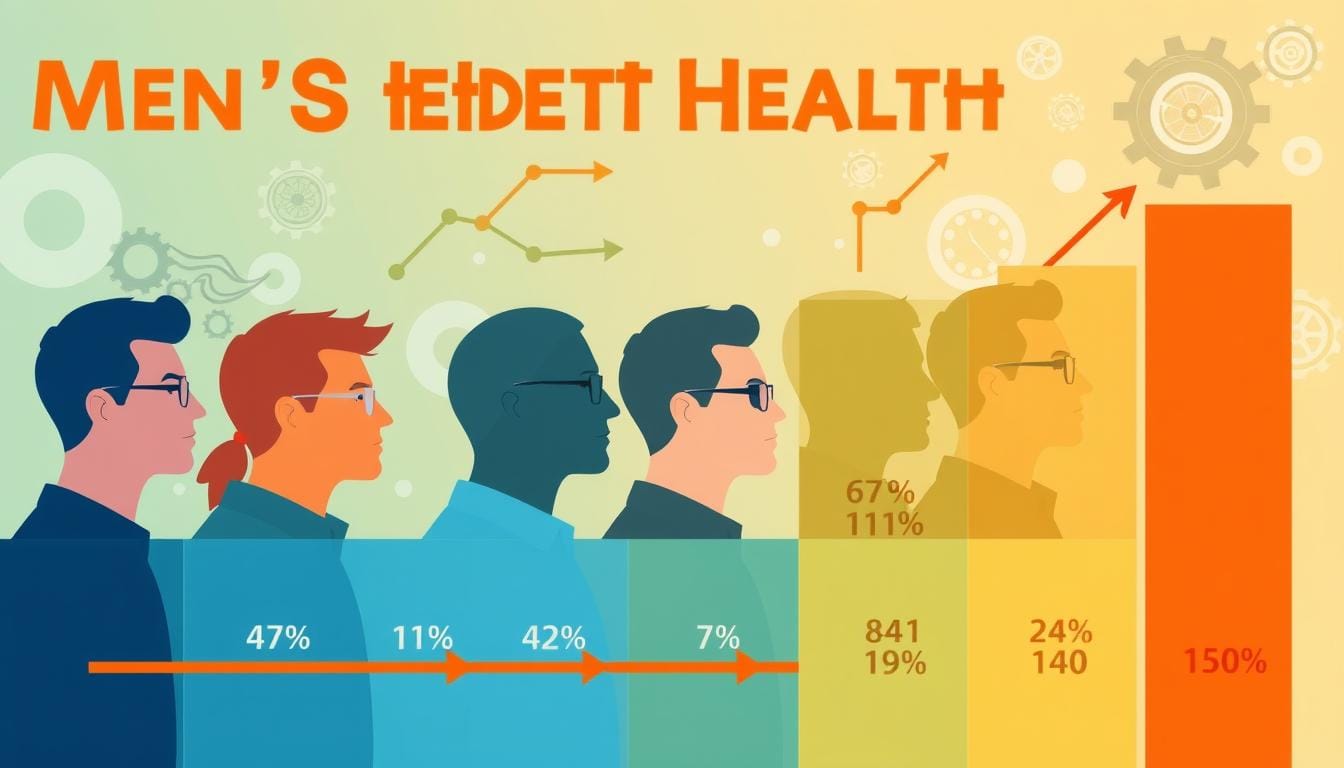
Men’s Mental Health Statistics: The Numbers You Should Know | Dr. Chandril Chugh
Have you ever noticed how men rarely talk about their feelings? It’s not because they don’t feel…
Therapy Goals for Depression: Setting Yourself Up for Success | Dr. Chandril Chugh
Depression affects millions worldwide. Getting help and setting goals is key to recovery. Dr.…
Symptoms of Depression in Men: Recognizing the Signs | Dr. Chandril Chugh
Dr. Chandril Chugh is a top mental health expert. He wants to help men understand depression…
Facts About Men’s Mental Health: Important Things to Know | Dr. Chandril Chugh
Men's mental health is very important but often ignored. It's key to know the mental health issues…
Magnetic Therapy for Depression: An Alternative Treatment | Dr. Chandril Chugh
Are you fighting depression and searching for a new way to feel better? Magnetic therapy might be…
Mental Health Rehab: When It’s Time to Consider Treatment | Dr. Chandril Chugh
Dr. Chandril Chugh is a top adult neurologist in Patna. He knows how important it is to deal with…
Men in Depression: How to Recognize and Help | Dr. Chandril Chugh
Depression is a complex mental health issue that can affect anyone. But men often find it hard to…
Managing Separation Anxiety in Babies: A Parent's Guide
Tearful, tantrum-filled goodbyes are common in a child's early years. Around the first birthday,…
Separation Anxiety Disorder in Adults
As an adult, you might feel scared and worried when you think about being away from someone you…
How to Deal with Separation Anxiety: Tips and Strategies
Separation anxiety can really affect your daily life and how you connect with others. But, you can…
Feeling Scared for No Reason? Understanding Anxiety Triggers
Anxiety is a common mental health issue that brings on worry, fear, and unease. It can make your…
Causes of Separation Anxiety: What You Need to Know
Have you ever felt nervous, panicky, or deeply sad when someone you love leaves the house? Maybe…
An Introduction to Internal Family Systems Therapy
Discover the power of Internal Family Systems (IFS) therapy. It's a way to see the "internal…
Understanding Anxiety Disorder in Children: Key Symptoms
Anxiety disorders are common in many children across the United States. They are marked by ongoing…
Therapy Interventions for Anxiety: What Works Best?
Anxiety affects nearly one in five people in the U.S. each year. While some anxiety is normal, too…
Exploring Types of Cognitive Behavioral Therapy for Mental Health
Cognitive behavioral therapy (CBT) is a key method used by mental health experts. It helps people…
Cognitive Behavioral Therapy for Anxiety: Techniques and Benefits
At our practice, we know how anxiety can really affect your daily life. Luckily, cognitive…
What is Child Psychology? An Overview for Parents and Educators
For parents and teachers, knowing about child psychology is key to helping kids grow well. It's the…
Top Child Psychology Courses: Start Your Journey Today
Start an exciting journey into child psychology with our top courses. You can learn more about…
Mental Health in Young Adults
We're all becoming more aware of how important mental health is, especially for young adults.…
ACEs Childhood Trauma: Understanding the Impact
Adverse childhood experiences, or ACEs, are a big issue in the U.S. They affect millions of people.…
Recognizing Anxiety Symptoms in Children: A Checklist for Parents
As parents, we face the challenge of helping our kids with their feelings. Anxiety is a big concern…
Importance of Mental Health Programs for Adults
Your mental health is key to your overall well-being. It includes how you think, feel, and act.…
Symptoms of Childhood Trauma in Adulthood: What to Watch For
Childhood trauma can deeply affect your life, even years later. It can come from abuse, neglect, or…
PTSD and Childhood Trauma: Understanding the Connection
Your experiences, both good and bad, deeply affect your mental health and well-being. The link…
Recognizing Signs of Childhood Trauma: A Guide for Adults
Trauma can deeply affect people, especially when it happens in childhood. As an adult, knowing the…
Anxiety from Childhood Trauma: Understanding the Link
Childhood trauma can deeply affect us, especially linking to anxiety disorders later. Trauma…
Common Women's Mental Health Issues: What to Know
It's key to understand women's mental health since women often face more mental health issues than…
Statistics on Women's Mental Health: Understanding the Data
Have you ever wondered why more women seem to struggle with sadness, anxiety, or stress? What’s…
Exploring Mental Health in Women: Key Issues and Insights
Your mental health is key to your overall well-being. Yet, it's often overlooked, especially for…
Effective Solutions for Extreme Sleep Apnea
If you're dealing with severe extreme sleep apnea, you're not alone. This condition means you stop…
How a Pain Doctor Can Help Manage Chronic Pain
If you're dealing with chronic pain, a pain doctor can be a big help. They have the skills and…
Effective Strategies for Comprehensive Pain Management
Chronic pain affects about 15% of people in the US, causing a lot of suffering and high healthcare…
Natural Pain Relief: Safe and Effective Home Remedies
If you're dealing with chronic pain, you're in good company. Millions worldwide face various types…
Effective Treatments for severe neck pain and headache base of skull
Neck pain and headaches can really slow you down. They might come from infections, stress, or other…
How to Cope with Central Pain Syndrome
Living with central pain syndrome is tough and can really slow you down. This condition happens…
How to Relieve Carpal Tunnel Pain Naturally
Are your fingers tingling? Do your wrists feel sore after a long day at work? If yes, you might be…
Natural and Easy Knee Pain Treatment At Home
Knee pain is a common issue that can often be managed at home. This article will show you natural…
5 Effective Strategies for Sleep Maintenance Insomnia Relief
Insomnia is a common sleep issue that makes it hard to fall asleep or stay asleep. If you're having…
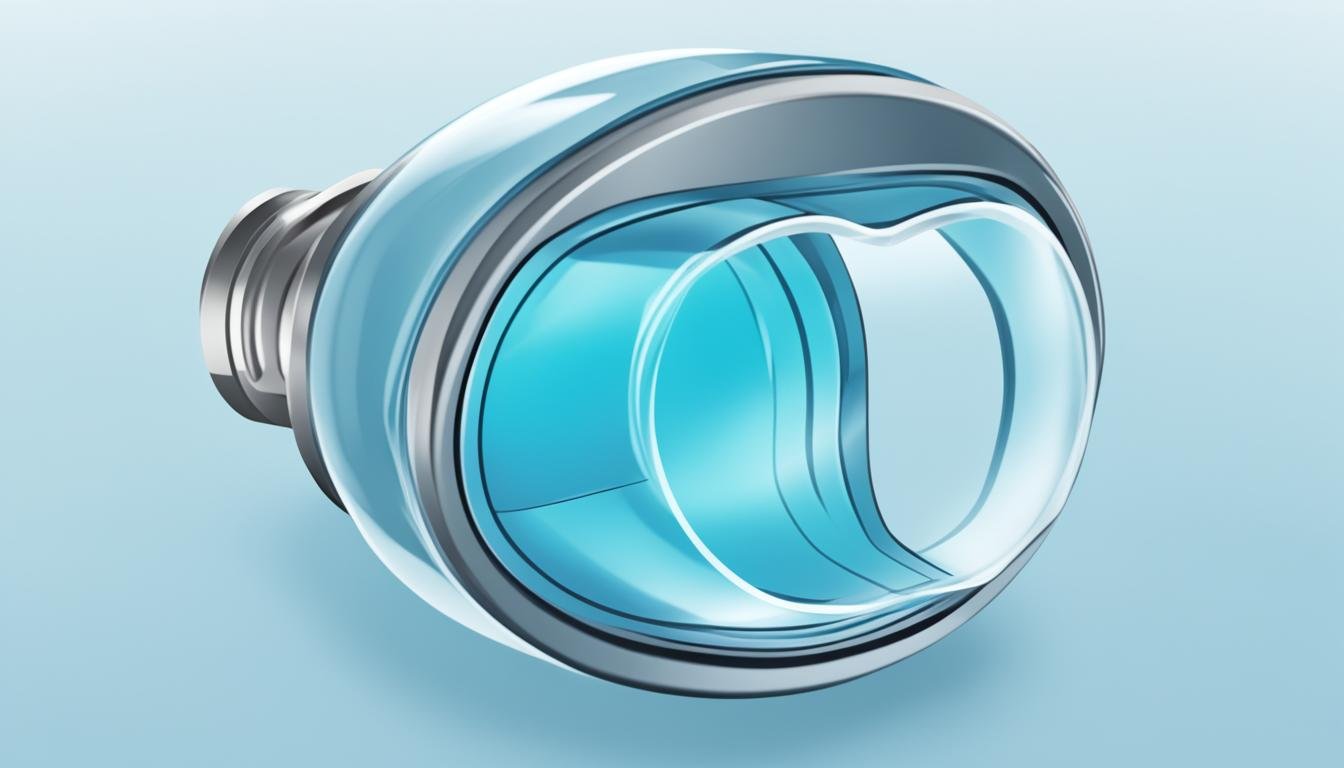
How an Apnea Mouthpiece Can Help You Sleep Better
If you have trouble sleeping because of obstructive sleep apnea (OSA), an apnea mouthpiece might be…
5 Top Strategies for Middle Back Pain Relief
Middle back pain, also known as thoracic spine discomfort, can really get in the way of your daily…
7 Tips to Manage Alzheimer’s and Parkinson’s
Dealing with Alzheimer's and Parkinson's can feel overwhelming. But, with the right strategies, you…
Radial Nerve Palsy Treatment: Modern Approaches for Recovery
Are you or a loved one dealing with radial nerve palsy (RNP)? This condition makes grip strength…
Lambert Eaton Myasthenic Syndrome: Symptoms, Causes, and Treatment
Lambert-Eaton myasthenic syndrome (LEMS) is a rare problem that affects how nerves and muscles…
Effective Treatment of Lambert Eaton Myasthenic Syndrome
Lambert-Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder. It impacts the connection…
What is Concussion Symptoms?
A concussion is a light traumatic brain injury that impacts the brain function. This leads to…
Effective Myasthenia Gravis Treatments: A Comprehensive Guide
Myasthenia gravis is a health issue where the body attacks itself by mistake. It leads to muscle…
Radial Nerve Palsy: Understanding This Nerve Condition
Feeling numb, weak, or uncoordinated in your arm, wrist, and hand? It might be radial nerve palsy.…
What Is Syringomyelia? An Overview of This Spinal Cord Disorder
Have you ever felt odd numbness in your arms, sudden weakness, or strange headaches with no clear…
Understanding Tarlov Cyst Disease: Symptoms and Treatments
If you've been diagnosed with tarlov cyst disease, you might feel lost about what to do next. If…
Creutzfeldt-Jakob disease (CJD) causes
Creutzfeldt-Jakob disease (CJD) is a rare brain disorder. It's caused by abnormal proteins called…
Creutzfeldt Jakob Disease Symptoms
Have you ever heard of a disease that can steal a person’s mind in a matter of months? Imagine…
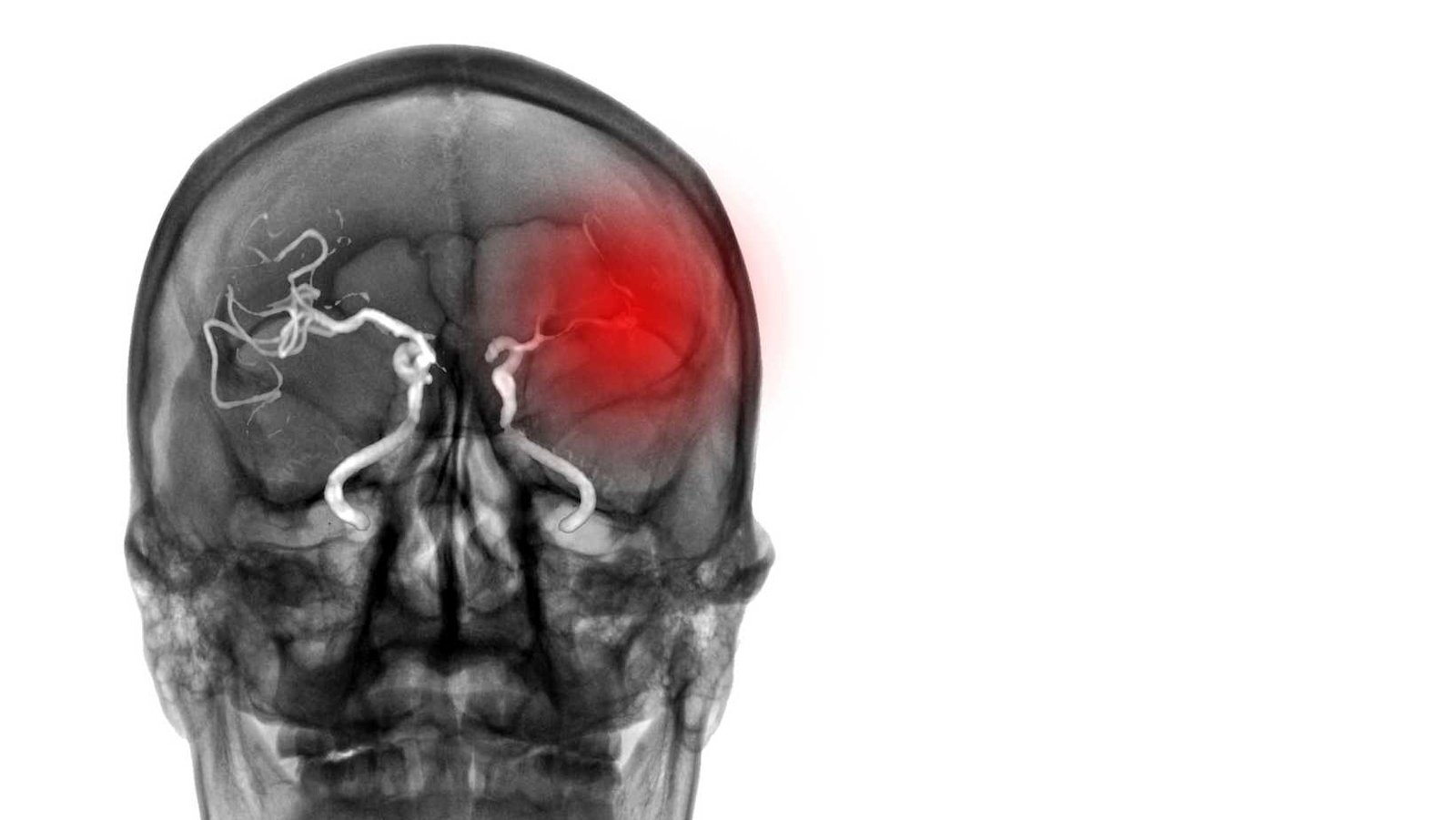
Ischemic Stroke Management Guidelines: Best Practices and Recommendations
Acute ischemic stroke (AIS) is a severe illness. It can cause serious disability and has a high…
Effective Treatments for Ischemic Stroke: Modern Approaches
Ischemic stroke is a major cause of disability and death globally, comprising most stroke cases. A…
Causes of Ischemic Stroke: Risk Factors and Prevention
Ischemic stroke is the top type of stroke, making up about 87% of all cases. It is caused by a…
Exploring the Pseudotumor Cerebri Causes: Why It Develops
Pseudotumor cerebri, or idiopathic intracranial hypertension, is when the skull's pressure rises.…
What Is Stiff Person Syndrome? A Rare Neurological Condition
Stiff person syndrome (SPS) is a rare, challenging to understand neurological disorder. It leads to…
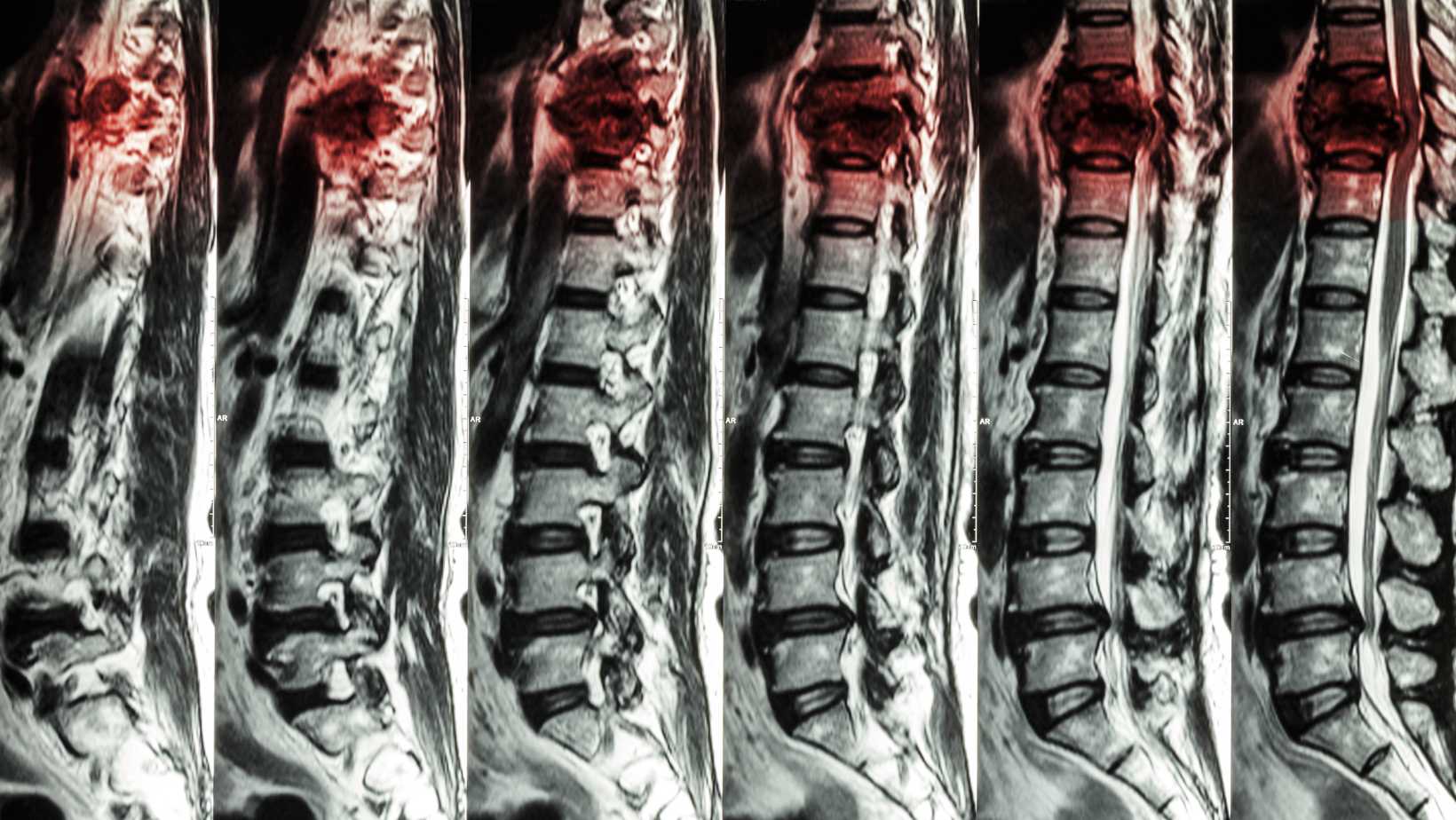
Understanding Compression of the Spinal Cord: Key Facts
Facing compression of the spinal cord can feel overwhelming. But learning the main points helps…
What Is Spinal Stenosis? A Comprehensive Overview
Spinal stenosis happens when nerve roots get pressed in the spine. This often causes pain,…
What Is Reye’s Syndrome? An Overview of This Rare Condition
If you have a child or teenager, knowing about Reye's syndrome is critical. Reye's syndrome mostly…
What Causes Sjogren’s Syndrome? Exploring the Underlying Mechanisms
Have you ever wondered why some people suddenly develop dry eyes, a dry mouth, and feel tired all…
Understand Disease Neurofibromatosis Types: Symptoms, Causes, and Treatment
Neurofibromatosis is a group of three genetic disorders leading to nerve tumors. These types…
Effective Lumbar Radiculopathy Treatment Options
Lumbar radiculopathy, or sciatica, affects around 5% of Americans. It is when a spinal nerve root…
Understand Lumbar Radiculopathy: An Overview
Lumbar radiculopathy brings pain, numbness, and weakness to the lower back and legs. It's a common…