What Is Duchenne Muscular Dystrophy?
Duchenne muscular dystrophy (DMD) is not common. It affects mostly young boys. They face issues with their muscles that get worse over time. This disease harms their heart and lung muscles too.
It is because of a changed dystrophin gene. This gene helps make a special protein for muscles. Missing this protein makes the muscles break down. Boys usually show signs when they are 2 or 3.
Normally, DMD is found in boys only. But, girls may also get it, though it’s rare. In Europe and North America, around 6 out of every 100,000 people have DMD.
Understanding Duchenne Muscular Dystrophy
Duchenne muscular dystrophy (DMD) is a genetic disorder that weakens muscles. It's one of four related conditions.
The others are Becker muscular dystrophy, an in-between form, and DMD-associated dilated cardiomyopathy.
Definition and Overview
Duchenne muscular dystrophy is a common hereditary disease. It affects about 2 in 10,000 people in the U.S.
This disease happens when a specific gene isn't working right. This gene makes a protein called dystrophin that our muscles need.
Without enough dystrophin, our muscles can't work well or fix themselves. This leads to muscle problems over time.
Prevalence and Affected Population
Worldwide, DMD affects about 6 in every 100,000 people. It mostly hits young boys. Around 1 in 3,600 baby boys are born with this each year.
Not long ago, boys with DMD didn't live very long. But, better medical treatments have changed that. Now, they can live up to 30 years or more.
| Statistic | Value |
|---|---|
| Prevalence of DMD in Europe and North America | Approximately 6 per 100,000 individuals |
| Estimated incidence of DMD | 1 in 3600 male live-born infants |
| Prevalence of DMD in the United States | Approximately 2 per 10,000 individuals |
| Percentage of DMD cases due to new mutations | 30% |
| Percentage of carrier females affected by muscular weakness | 2.5% to 20% |
A woman who carries the faulty gene might not feel weak herself. But, 2.5% to 20% may have some muscle issues.
Also, many cases of DMD come from new mutations. They are not always inherited from a parent.
Duchenne muscular dystrophy Symptoms
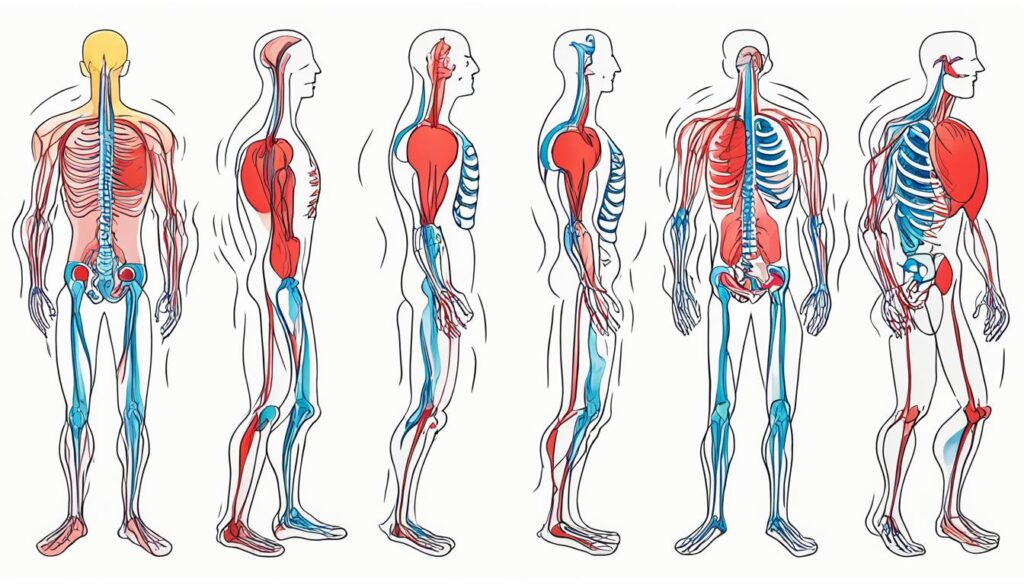
The main symptom of Duchenne muscular dystrophy is muscle weakness. It can start when a child is 2 or 3. This weakness usually begins in muscles near the core of the body.
Then, it moves to muscles closer to the hands and feet.
Early Signs and Indicators
Early signs of DMD include issues with jumping and running. Boys might have a hard time walking and have a waddling walk. You might also notice their calf muscles getting bigger.
These signs can show up when they're still toddlers.
Progression of Muscle Weakness
The muscle weakness in DMD keeps getting worse. It starts to affect more and more muscle groups. By school age, children with DMD may walk on their toes and have trouble using their arms.
Often, they end up using a wheelchair by age 12 as the disease progresses.
Impact on Respiratory and Cardiac Function
DMD also affects how the heart and lungs work. Those with DMD don't usually live past their 20s. They might die from breathing problems or a weak heart. If not managed well, the effect on breathing and heart health can be very serious.

Causes and Genetic Factors
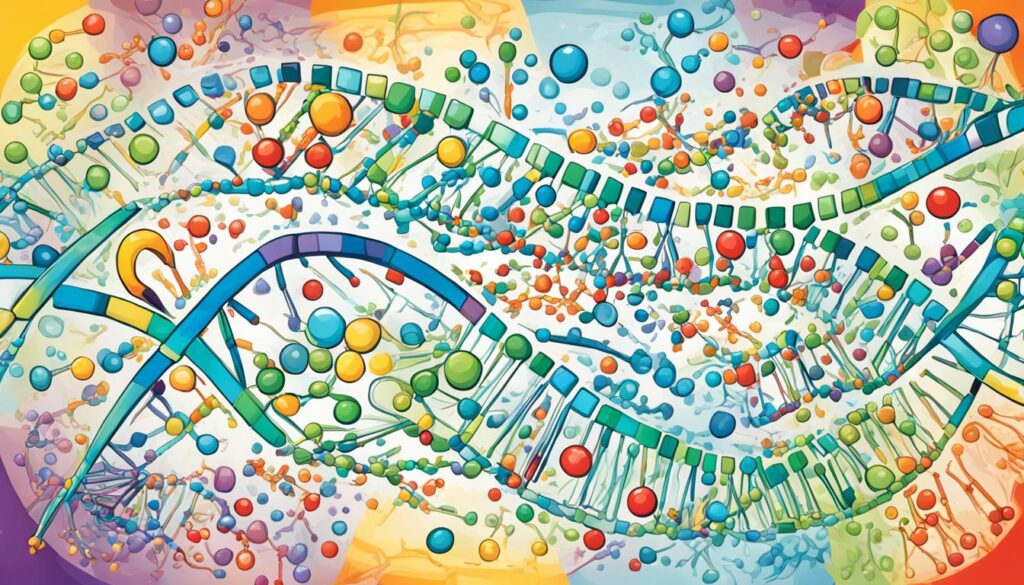
Duchenne muscular dystrophy (DMD) happens due to a gene mutation. This mutation affects the dystrophin protein, key for muscle function. Without it, muscles can't work or heal well, leading to their weakness in DMD.
Role of Dystrophin Protein
The dystrophin protein is vital for muscle cell structure. It links parts inside the cell to its outer layer. But, if the gene for dystrophin is mutated, this connection fails, and muscles start breaking down.
X-Linked Inheritance Pattern
DMD is inherited in an X-linked recessive way, so the faulty gene sits on the X chromosome. Thus, males with a mutation develop DMD because they have one X chromosome. Females, with two Xs, can be carriers if the mutation is on one X. The other X might usually have a healthy copy.
In some families, DMD appears without a past history because mutations can start anew. Women carrying the gene have a 50% chance of passing it to their children. This means a 50% chance of their sons having Duchenne.

| Genetic Factor | Explanation |
|---|---|
| Dystrophin Protein | The dystrophin protein is vital for muscle cells’ health. But if its gene has a mutation, a non-working or missing protein leads to muscle problems. |
| X-Linked Inheritance | DMD's inheritance pattern is X-linked recessive, placing the faulty gene on the X chromosome. Males with one mutation suffer from DMD. Females, having one healthy X, are often just carriers. |
| Spontaneous Mutations | One-third of DMD cases surprise families with no past record, due to new mutations. Carrier women have the same 50% risk of passing the mutation on to their children. |
Diagnosis and Testing
Diagnosing Duchenne muscular dystrophy (DMD) mixes physical checks with genetic tests. Doctors will look at the child's muscle strength, flexibility, and reflexes. They also search for muscle wasting and big calf muscles.
Physical Examination
A doctor measures the child's muscle use and growth. They watch how the child walks and stands from a sit. They also test other movement skills to spot early DMD signs. Doctors look for big calf muscles, a key DMD clue.
Genetic Testing and Analysis
Genetic tests pin down DMD and its specific gene issue. A muscle or blood sample is checked for mutations in the DMD gene. Around 70% to 80% of DMD cases have these mutations.
| Diagnostic Marker | DMD | BMD |
|---|---|---|
| Creatine Kinase (CK) Levels | They hit 10-20 times the limit by age 2, then drop 25% yearly | Elevated 5 times or more |
| Dystrophin Quantity | Less than 5% of normal | Usually more than DMD |
| Age of Onset | Starts in early years, usually age 2-3 | Can begin at 5-60 years, sometimes loss of walking later |
Exam and genetic test results combined give a DMD diagnosis. This diagnosis shows the exact genetic issues. Knowing this helps plan the best treatments.
Treatment and Disease Management
There's no cure for Duchenne muscular dystrophy (DMD) yet. But, its treatment helps manage symptoms and improve life quality. Supportive care and therapies are key for DMD management.
Supportive Care and Therapies
Steroids like prednisone and deflazacort can boost muscle strength for 6 months to 2 years in DMD patients. Physical and occupational therapy, with assistive devices, improve life quality and length for those with DMD.
For a few, creatine supplements help make muscles stronger. In later DMD stages, eating and swallowing trouble might happen. This is called dysphagia. It needs special care.
Sometimes, surgery is needed for issues like scoliosis, or tight tendons. This can make life better for DMD patients by fixing serious muscle problems.
Emerging Treatments and Clinical Trials
Today, researchers look for new ways to treat Duchenne muscular dystrophy. They are testing "exon skipping" for DMD in the UK and the Netherlands. This might be a new duchenne muscular dystrophy treatment approach.
There are now more medicines to fight DMD. Duvyzat helps slow down the disease and makes moving easier. Medicines like Eteplirsen (Exondys 51) and Ataluren (Translarna) target specific types of DMD. These increase dystrophin, an important protein for muscle health.
Gene therapies are also in development, aiming for future FDA approvals. Many clinical trials are ongoing. They look for new ways to help people with muscular dystrophy.

Living with Duchenne Muscular Dystrophy
Living with Duchenne muscular dystrophy (DMD) includes many challenges. But with support and strategies, both the person and their family can enjoy life. It's about managing the physical, emotional, and social parts of DMD well, to thrive.
Coping Strategies and Support
It's important to have good ways to cope with DMD. Talking to other families dealing with the same issues can be a big help. This includes joining support groups both online and in person to feel less alone and to share advice.
And don't forget about getting professional support like therapy. A counselor can help you and your family handle the tough feelings that may come up. They offer advice on dealing with stress and worry, and help you find ways to feel better.
Quality of Life Considerations
Focusing on a good life quality is crucial for those with DMD. You may need to adjust your living space, use tools that help, and maybe change how you learn or work. Adapting to new needs and limits over time is important.
Working with your healthcare team, teachers, and local groups is key. They can help you get the support and changes you need to live well. By standing up for what you require and being open to new ways of doing things, you can feel more independent and fulfilled.
| Coping Strategies | Quality of Life Considerations |
|---|---|
|
|
Conclusion
Even though Duchenne muscular dystrophy (DMD) is rare and hard to deal with, we've made great strides in its care. More is known about its causes. We have better ways to help. Plus, there are new treatments that give families hope for a better life. This isn't the end of the fight. But, with more research and teamwork, things are looking up for those with Duchenne muscular dystrophy.
It's important to keep learning about the latest treatments and getting support. This helps you face the challenges with strength. As we push forward, there is hope for better days. Together, we can make life better for those with Duchenne muscular dystrophy.
The search for a cure is ongoing. And the progress that's been made is uplifting. There's a strong drive to beat this disorder. Through awareness and working together, we aim for a future where this disease is less of a burden. There is hope for a better tomorrow for everyone touched by Duchenne muscular dystrophy.
FAQ
What is Duchenne muscular dystrophy (DMD)?
Duchenne muscular dystrophy (DMD) is a rare genetic disorder. It affects mainly young boys. They have weakening muscles because certain muscles are lost over time. This includes muscles in the skeleton, heart, and lungs.
What are the primary symptoms of Duchenne muscular dystrophy (DMD)?
The main symptom of DMD is muscle weakness. It often begins when the child is 2 or 3 years old. First, muscles close to the core weaken, then those near the hands and feet.
What causes Duchenne muscular dystrophy (DMD)?
DMD happens because of a missing protein. This protein, called dystrophin, is vital for muscles. Without it, muscles can't work or repair themselves right. That's why they become weaker over time.
How is Duchenne muscular dystrophy (DMD) diagnosed?
Doctors diagnose DMD with a physical check-up and genetic tests. They test muscle strength, flexibility, and reflexes. They also look for certain signs in the muscles, like how the calf muscles change.
How is Duchenne muscular dystrophy (DMD) treated?
There's no cure for DMD yet. But treatments aim to improve quality of life and manage symptoms. Supportive care and certain therapies are very important for people with DMD.
What is it like to live with Duchenne muscular dystrophy (DMD)?
It's not easy living with DMD. But having the right support and strategies helps. People with DMD and their families can still have a good life.
Source Links
- https://www.ncbi.nlm.nih.gov/books/NBK482346/
- https://www.parentprojectmd.org/about-duchenne/what-is-duchenne/
- https://www.mda.org/disease/duchenne-muscular-dystrophy
- https://www.mda.org/disease/duchenne-muscular-dystrophy/signs-and-symptoms
- https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/symptoms-causes/syc-20375388
- https://www.parentprojectmd.org/about-duchenne/what-is-duchenne/genetic-causes/
- https://www.genome.gov/Genetic-Disorders/Duchenne-Muscular-Dystrophy
- https://www.mda.org/disease/duchenne-muscular-dystrophy/diagnosis
- https://www.nhs.uk/conditions/muscular-dystrophy/treatment/
- https://www.webmd.com/children/duchenne-muscular-dystrophy
- https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/diagnosis-treatment/drc-20375394
- https://duchenneandyou.com/living-with-duchenne/
Hepatic Encephalopathy Treatments: Options and Approaches
This illness is a serious complication of chronic liver disease. It can cause changes in mental state and even coma. So, managing it well is key.
The first thing to do is find and treat the encephalopathy causes. This might mean dealing with infections, stopping bleeding, or fixing medication doses. It also involves fixing any imbalances in your body's salts. After that, doctors use medicine to stop the making and intake of toxins, like ammonia, in your gut.
Two main kinds of medicine help with encephalopathy. One is lactulose, a fake sugar. The other is a type of antibiotics called rifaximin. Using these two together is better than just one. But, sometimes, if the liver disease is too far along, a liver transplant may be the best choice.
It’s also key to keep watching how you do with lab tests, how well you think, and for signs that the HE is coming back. By working closely with your doctors, you can do a lot to handle your encephalopathy symptoms. This can make your daily life much better.
Understanding Hepatic Encephalopathy
Definition and Symptoms
Hepatic encephalopathy (HE) happens with chronic liver disease. The liver can't remove toxins, like ammonia, from our blood. These toxins then build up in the brain. This causes confusion, changes in how we act, and in bad cases, coma. HE can mean anything from minor memory issues to big problems like seizures.
Causes and Risk Factors
HE starts when the liver can't work right, letting too much ammonia and other toxins into the blood. This usually happens because of chronic liver disease or cirrhosis. Some things, like gut bleeding, infections, or some drugs, can make HE worse. People with serious liver issues, or a history of HE, are more at risk. Getting older, not eating right, and how serious the liver disease is, can also affect the chances of getting HE.
Prevalence and Burden
HE is a big problem, affecting between 30 to 45% of people with cirrhosis. It can cause a lot of harm and sometimes even lead to death. Every year, treating HE costs more than $10 billion in the U.S. It's very important to treat HE well to help patients and to lower these big costs.
Conventional Therapies for Encephalopathy
Changing what we eat is key in hepatic encephalopathy control. The focus is on lessening ammonia and toxin levels in the stomach. Eating a diet low in protein is a must. Foods that boost ammonia, like red meat and dairy, should be cut. Instead, try veggies for protein and branched-chain amino acids. It's also important to eat enough and stay hydrated to ward off malnutrition and liver harm.
Dietary Modifications
Eating right can cut down on the ammonia the body makes and absorbs. A diet low in protein, but rich in quality, easily digested proteins helps. It also means not eating foods that make more ammonia, like red meat. Instead, choose vegetable proteins and amino acids. This type of diet can really help with encephalopathy treatment.
Lactulose and Disaccharides
Lactulose, a type of sugar, is a big help with HE. It pulls water into the intestines, making stool softer and helping us go more often. This process gets rid of ammonia and toxins. Using lactulose can boost brain function and lower HE chances. Lactitol does a similar job and is another option.
Antibiotics (Rifaximin)
Antibiotics like rifaximin are a crucial part of fighting HE. Rifaximin is special because the body doesn't absorb it. It targets gut bacteria that make ammonia, cutting down on toxins. This leads to better brain function. Rifaximin helps with treating and stopping HE, especially when used with lactulose.

Emerging Treatments and Novel Approaches
Recent studies suggest that a bad gut balance might cause hepatic encephalopathy (HE). Fecal microbiota transplantation (FMT) is a new way to fix this. It puts healthy bacteria back in the gut, helping with HE symptoms. FMT has already made patients feel sharper, visit the hospital less, and avoid HE's comeback. It's a bright spot for those not helped by typical treatments.
Fecal Microbiota Transplantation
FMT aims to balance the gut's bacteria. It involves putting a healthy donor's stool into the patient's gut. This change may reduce harmful substances linked to HE, offering hope for fighting the disease. Early signs show cognitive boosts, fewer hospital trips, and less HE coming back for those with cirrhosis.
Zinc Supplementation
Low zinc levels are common in those with liver issues, increasing their HE risk. Zinc is key in liver cleanse processes. Adding zinc to the diet has benefited some patients, enhancing mental functions and cutting HE cases. Yet, clear guidelines on dosage and timing are still missing. Rectifying zinc levels in liver patients is a good step, though more study is vital to fine-tune the approach.
Branched-Chain Amino Acids
Liver illness often skews the body's amino acids, leaving out important ones like BCAAs. Without enough BCAAs, the body struggles with ammonia, a key HE player. A push in BCAA levels might help manage HE, with reports of better mental clarity and fewer hospital stays. Confirming BCAA's role in HE healing needs more work. This path, however, could offer new hope in treating HE.

Encephalopathy Treatment
Hepatic encephalopathy (HE) treatment is a complicated process. It aims to find and solve the main causes. This includes using medicines to stop the body from creating and taking in toxins. Lactulose and rifaximin are two key medicines for treating HE.
Lactulose pulls water into the bowels. This helps remove ammonia and other harmful substances. Rifaximin, an antibiotic, works against the bad gut bacteria that make these toxins.
Handling HE well is vital for patient health and saving money on healthcare. It requires finding and treating the root issues. Also, a mix of changes in diet, medicines, and care supports can help. They make it possible for patients to manage their condition and avoid serious episodes.
Combination Therapies and Individualized Management
Studies show treating HE with both lactulose and rifaximin works better than using just one. These drugs together fight HE's root causes. They cut down on ammonia, boost the movement in your gut, and balance the bugs in your stomach.
Lactulose and Rifaximin Combination
A 2010 study found a mix of lactulose and rifaximin helped people with HE a lot. It made complications and deaths less common. Another review in 2016 backed this up. It looked at studies using lactulose, lactitol, or no treatment for HE in people with liver cirrhosis.
Role of Supportive Care
Besides medicines, supportive care is key for HE management. It deals with issues like infections, gut bleeds, and odd electrolytes. These problems can start or make HE worse. Fixing them helps stop HE issues and make patients better.
Liver Transplantation for Advanced Cases
In really bad cases of end-stage liver disease, when people with hepatic encephalopathy (HE) don't get better with medicine, a liver transplant might be the only answer. This surgery swaps out a sick liver for a healthy one. This way, the body can again work like it should, keeping harmful toxins from building up.
After a liver transplant for hepatic encephalopathy, patients often get better at thinking, have to go to the hospital less, and see less HE happen again. This operation saves the lives of those with bad end-stage liver disease and hepatic encephalopathy who've tried everything else without luck.
The choice for getting a liver transplant for HE is very personal. Doctors look at how healthy the person is, how bad their liver is, and if there's a suitable liver available. A team of experts, like liver doctors, surgeons, and mental health doctors, work together to give the best care and results to these patients.
Monitoring and Follow-up
Watching closely and following up regularly create better care for hepatic encephalopathy (HE). Doctors do laboratory tests to check how well the liver works. They look at ammonia levels too, which are important for HE.
Laboratory Tests
Doctors use various lab tests to track HE and decide on treatments. These tests show how the liver is doing, like ammonia levels, liver enzymes, and more. By checking these things often, doctors can spot early signs of trouble. This means they can stop HE episodes before they happen.
Assessing Cognitive Function
Testing how well the brain works is key in HE care too. Doctors have many tests to check the mind, like the MMSE, the MoCA, and the PHES. These tests can find small changes in thinking, memory, and attention. Knowing these changes helps doctors treat patients better.
Keeping an eye on lab results and how the brain is working helps a lot. Doctors can make smart choices for HE care. This makes life better for patients.
Conclusion
Hepatic encephalopathy is a serious issue from chronic liver disease that can be life-threatening. It needs quick and good care. The treatment plan includes finding and treating the main causes. It also uses medicines to decrease toxins like ammonia in the gut.
Treatment includes changing what you eat, using lactulose, antibiotics like rifaximin, and new methods like fecal transplant and amino acid supplements. This can help a lot. Doctors need to keep checking the patient's tests and thinking ability. They should watch for signs of it coming back. This careful care is very important.
In short, treating hepatic encephalopathy needs a mix of different steps. It is key to lower the bad effects it can have on patients and the healthcare system.
FAQ
What is hepatic encephalopathy and what are its symptoms?
Hepatic encephalopathy is a serious result of liver disease. It can change how you think and feel, leading to coma if not treated. You might see things like changes in sleep, trouble focusing, or memory loss. Other signs include speaking slowly, shaking, and seizures.
What causes hepatic encephalopathy?
HE happens when the liver can't remove toxins from the blood. This can be from liver disease or cirrhosis. Things like bleeding in the gut, infections, and not enough water or salt can make it worse.
How common is hepatic encephalopathy and what is the impact on healthcare?
It's a common issue with liver disease, affecting 30-45% of those with cirrhosis. It can be very serious, with up to half of those with severe symptoms not surviving the next year. It also costs the healthcare system a lot, over billion a year in the U.S. from hospital stays.
How is hepatic encephalopathy treated?
Treating HE usually involves changing your diet, taking certain drugs, and getting extra care. Doctors often use lactulose, a sugar-like medicine, and rifaximin, an antibiotic. Using both together seems to work best.
What are some emerging treatments for hepatic encephalopathy?
New treatments include using poop from healthy donors, taking more zinc, and adding special amino acids to the diet. These ways are showing hope, but we need more studies to be sure they work for everyone.
How is the long-term management of hepatic encephalopathy achieved?
To look after HE for a long time, doctors use drugs, give extra support, and check on you often. They do blood tests and special brain tests. It's very important to watch for any signs it might be coming back, so the treatment can be changed in time.
When is liver transplantation considered for hepatic encephalopathy?
If HE is very bad and medicine doesn't help anymore, a new liver might be the only way to fix it. This operation can swap a sick liver for one that works right. It lets the body clear away the bad stuff and go back to normal.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8917954/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9099111/
- https://liverfoundation.org/liver-diseases/complications-of-liver-disease/hepatic-encephalopathy/treating-hepatic-encephalopathy/
- https://my.clevelandclinic.org/health/diseases/21220-hepatic-encephalopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8472037/
- https://www.uptodate.com/contents/whats-new-in-pediatrics
- https://my.clevelandclinic.org/health/diseases/8525-parkinsons-disease-an-overview
- https://www.webmd.com/brain/what-is-encephalopathy
- https://www.healthdirect.gov.au/encephalopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177461/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9205788/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4933409/
4 Types Of Guillain Barre syndrome A Classification Guide
Guillain-Barré syndrome or GBS is a rare disorder linked with infections. It happens when the immune system reacts too much and attacks its own self. There are types of GBS that need to be understood for its treatment. It can weaken or paralyze the body, making it hard to breathe.
GBS is usually caused after an infection, either bacterial or viral. It's important to know the 4 types of Guillain-Barre syndrome. This knowledge helps doctors give the right care. This leads to the best chances for a patient’s recovery.
Introduction to Guillain-Barré Syndrome (GBS)
Guillain-Barré Syndrome: An Overview
Guillain-Barré syndrome (GBS) is a rare disorder. It affects the peripheral nerves. These nerves help the brain, skin, and muscles talk to each other. The immune system mistakenly attacks these nerves. This causes inflammation and damage.
GBS and the Peripheral Nervous System
The peripheral nervous system is a network of nerves. It goes from the brain and spinal cord to the body. In GBS, the immune system damages these nerves. This disruption causes problems in sending signals. As a result, people may feel weak, tingle, or even become paralyzed.
Acute Inflammatory Demyelinating Polyneuropathy (AIDP)
AIDP is the main Guillain-Barré Syndrome (GBS) type in America. It damages the myelin sheaths on nerves. People with AIDP suddenly feel weak on both sides of their body. This weak feeling starts in the toes and moves up. They might also have trouble moving their face, speaking, or swallowing. Their reflexes can be low or not work at all.
Symptoms of AIDP
The main signs of AIDP are quick muscle weakness or not being able to move. This usually starts in the legs and goes up. The person might feel numb, tingly, or in pain in their arms or legs. They could find it hard to move their face, speak, or swallow. Their reflexes might be weak too.
Progression of AIDP
AIDP gets worse fast, with the strongest signs in the first two to four weeks. Someone might lose muscle strength very quickly. This might lead to not being able to move at all in severe cases. How fast it gets worse can change. Getting diagnosed and treated early is very important.
AIDP and Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
AIDP is a fast-moving GBS type. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is another kind but it gets worse over time. In CIDP, there's almost always some loss of myelin. It can take months to get very bad. Jumping on diagnosis and treatment is key to stop disability and get better in both AIDP and CIDP people.

Acute Motor and Sensory Axonal Neuropathy (AMSAN)
Acute Motor and Sensory Axonal Neuropathy (AMSAN) is a rare, severe type of Guillain-Barré syndrome (GBS). It affects the axons, or the nerves' message-carrying parts for both movement and sensation. Unlike other GBS forms, AMSAN targets both sensory and motor fibers' axonal degeneration.
Distinguishing Features of AMSAN
AMSAN shows in numbness and tingling in feet and hands, leading to limb weakness and walking difficulty within 10 days. Such a quick start and progression are typical for AMSAN. It can also affect automatic processes, like breathing, putting lives at risk.
Recovery from AMSAN
Healing from AMSAN is slow due to the needed axonal damage repair and regeneration. Patients might need a long time on mechanical ventilation and tracheostomy, along with extended care for nerve and muscle issues. With correct support and therapy, most regain some functionality. Yet, the path to recovery is long and tough, unlike other GBS types.
Acute Motor Axonal Neuropathy (AMAN)
Acute Motor Axonal Neuropathy (AMAN) is a rare type of Guillain-Barré syndrome (GBS). It mainly affects the motor nerves for movement. This form makes up 5-10% of GBS cases in the U.S.
Campylobacter jejuni and AMAN
Campylobacter jejuni bacteria plays a big role in AMAN's development. If someone gets infected with it, their body may react in a harmful way. This can cause problems and even harm the motor nerves. Studies have shown that Campylobacter jejuni is linked to some AMAN cases.
| GBS Variant | Percentage of Cases in the U.S. |
|---|---|
| Acute Inflammatory Demyelinating Polyneuropathy (AIDP) | 85-90% |
| Acute Motor Axonal Neuropathy (AMAN) | 5-10% |
| Acute Motor Sensory Axonal Neuropathy (AMSAN) | Rare |
Miller-Fisher Syndrome (MFS)
Miller-Fisher Syndrome (MFS) is very rare. It's a kind of Guillain-Barré Syndrome (GBS) that affects the nerves in your head. People with MFS have three main symptoms: weak eye muscles, no reflexes, and unsteady movements.
Cranial Nerve Involvement in MFS
MFS especially affects the cranial nerves. This can cause many problems. For example, eye muscle weakness can make you see double or cause your eyelids to droop. You might also have a weak face, find it hard to swallow, or move unsteadily.
Prognosis of Miller-Fisher Syndrome
Most people with MFS get better in 8 to 12 weeks, often without special treatment. Only a few may have symptoms come back. These symptoms usually go away in about six months. In some cases, doctors might use special treatments like IVIg or plasmapheresis.
| Characteristic | Statistic |
|---|---|
| Worldwide incidence of MFS | 1 to 2 per 1,000,000 people |
| Gender ratio (male to female) | 2:1 |
| Mean age at onset | 43.6 years |
| Incidence in Asians | 15% to 25% of GBS cases |
| Incidence in Western populations | 5% of GBS cases |
| Preceding viral infection | 72% of MFS cases |
| Positive for anti-GQ1b antibodies | 70% to 90% of MFS patients |
| Classic triad presentation | 90% of MFS patients |
| Albuminocytologic dissociation | 90% of MFS patients |
4 types of guillain barre syndrome
Guillain-Barré syndrome (GBS) is a rare disorder that affects the nerves. It shows up in four main types:
- Acute Inflammatory Demyelinating Polyneuropathy (AIDP): This is the most seen type in the U.S. It damages the myelin sheaths that cover nerves.
- Acute Motor and Sensory Axonal Neuropathy (AMSAN): A rare, severe form that mainly harms the axons. Axons are nerves that help us move and feel.
- Acute Motor Axonal Neuropathy (AMAN): This type only affects nerves that control movement. It makes up 5-10% of cases.
- Miller-Fisher Syndrome (MFS): A very rare kind that mostly affects facial nerves. It leads to issues with moving and eating, and weakens the face.
Each type of GBS has its own symptoms and ways of progressing. Knowing these differences helps healthcare providers treat GBS better.
| GBS Subtype | Prevalence | Key Features | Recovery Timeline |
|---|---|---|---|
| AIDP | Most seen in the U.S. | Hurts myelin sheaths of nerves | Most people walk again within 6 months |
| AMSAN | Rare, severe | Targets axons of nerves for movement and sensation | Recovery can be a year or more |
| AMAN | 5-10% of cases | Only affects nerves controlling movement | - |
| MFS | Very rare, affects 1-2 per million in the U.S. | Affects facial nerves, leading to problems with movement and coordination | - |
Diagnosis and Treatment Approaches
Doctors use your medical past, a checkup, and special tests to find out if you have Guillain-Barré syndrome. These tests show the kind of GBS and tell if it's something else.
Electrodiagnostic Testing for GBS
Tests like nerve conduction studies and electromyography are key in figuring out Guillain-Barré syndrome. They look at the nerves' electric activity to see the damage. This info helps doctors choose the right way to treat you.
Treatment Options for GBS
The main goals of treating Guillain-Barré syndrome are to ease symptoms and support recovery. Treatments include IVIG and plasma exchange to help your immune system and lower nerve inflammation. Sometimes, you might need help breathing with a machine. Fortunately, most people can walk on their own after six months. And around 60% get back full muscle strength a year later.
FAQ
What is Guillain-Barré syndrome (GBS)?
Guillain-Barré syndrome (GBS) is a rare nerve disorder. It can happen after someone gets sick. The body's immune system acts too much. This can make arms and legs weak. In bad cases, it can even make breathing hard.
What are the different types of Guillain-Barré syndrome?
There are four types of Guillain-Barré syndrome:
- Acute Inflammatory Demyelinating Polyneuropathy (AIDP)
- Acute Motor and Sensory Axonal Neuropathy (AMSAN)
- Acute Motor Axonal Neuropathy (AMAN)
- Miller-Fisher Syndrome (MFS)
What are the symptoms of Acute Inflammatory Demyelinating Polyneuropathy (AIDP)?
With AIDP, you might suddenly feel weak on both body sides. This weakness usually starts in the toes and moves up. You might also face weak facial muscles, have trouble speaking or swallowing, and show reduced reflexes.
How is Acute Motor and Sensory Axonal Neuropathy (AMSAN) different from other types of GBS?
AMSAN is rare and serious. It mainly affects the nerves' axons that control feeling and motion. Symptoms start with tingling in hands and feet. This can become limb weakness and trouble walking over 10 days. Breathing problems may also arise.
What causes Acute Motor Axonal Neuropathy (AMAN)?
Sometimes, AMAN happens because of Campylobacter jejuni. This bacteria causes a few AMAN cases. It's a rare GBS type that only affects nerves for movement.
How does Miller-Fisher Syndrome (MFS) differ from other GBS variants?
MFS is very rare and targets the head's nerves. It starts with eye muscle weakness. Symptoms may grow to include movement problems, weak face muscles, and trouble swallowing.
How is Guillain-Barré syndrome diagnosed?
Doctors find GBS through a person's health story, checkup, and special tests. Tests like nerve studies and muscle checks help to diagnose GBS. They also exclude other illnesses.
What are the treatment options for Guillain-Barré syndrome?
GBS can be treated with drugs that calm the immune system. Treatments like IVIG or plasma exchange help. In tough cases, a person might need help breathing.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939842/
- https://medlineplus.gov/genetics/condition/guillain-barre-syndrome/
- https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/symptoms-causes/syc-20362793
- https://www.ncbi.nlm.nih.gov/books/NBK532254/
- https://www.verywellhealth.com/introduction-to-guillain-barre-syndrome-2488658
- https://www.uofmhealth.org/conditions-treatments/brain-neurological-conditions/guillain-barre-syndrome-GBS-and-chronic-inflammatory-demyelinating-polyneuropathy-CIDP
- https://emedicine.medscape.com/article/1169959-overview
- https://www.medicalnewstoday.com/articles/types-of-guillain-barre-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7189311/
- https://www.ncbi.nlm.nih.gov/books/NBK507717/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7676442/
- https://rarediseases.org/rare-diseases/miller-fisher-syndrome/
- https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/diagnosis-treatment/drc-20363006
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6821638/
Guillain-Barré Syndrome Treatment Options
Guillain-Barré syndrome (GBS) is a immune mediated neurological disorder. The immune system wrongly attacks the nerves. It causes sudden numbness, weakness, and in some cases, paralysis. Luckily, there are effective treatments to manage the symptoms and aid recovery.
This article will look at the latest treatments for GBS. It will cover plasma exchange, IVIG therapy, supportive care, and new therapies. Knowing about these treatments can help you on your path to recovery from guillain-barré syndrome.
Understanding Guillain-Barré Syndrome
What is Guillain-Barré Syndrome?
Guillain-Barré syndrome, or GBS, is a rare condition that affects the nerves. It comes when the immune system attacks nerves by mistake. This attack damages the nerves, causing issues like muscle weakness, numbness, and sometimes paralysis.
Causes and Risk Factors
The exact reason for GBS is not fully known. However, it often starts after an infection or vaccination. People with certain infections, having had specific vaccinations, or existing health problems are more at risk. Knowing these facts can help you and your doctor spot the condition early.
Diagnosis and Early Detection
It's key to catch Guillain-Barré syndrome early for effective treatment. Signs usually show up as muscle weakness that gets worse, tingling or numbness, and trouble keeping balance. Sometimes, it can quickly lead to breathing problems from muscle weakness.
Symptoms to Watch Out For
The main signs of Guillain-Barré syndrome are:
- Starting weakness in the legs, then moving up
- Feeling of tingling or parts of the body going numb
- Finding it hard to keep balance and move well
- Severe breathing or swallowing problems in some cases
If you or someone you know shows these signs, get help as soon as possible. Quick diagnosis and treatment are very important for getting better.
Diagnostic Tests and Procedures
Doctors use specific tests to check for Guillain-Barré syndrome. These may include:
- Spinal tap to look for high protein in the spinal fluid
- Nerve tests to see how well they work
- A test called electromyography (EMG) to check muscle activity
These tests rule out other problems. They help doctors plan the best care for you if you have Guillain-Barré syndrome.
Quickly spotting and treating the disease is crucial for not getting worse and getting fully better. Knowing the early signs and getting medical help is the first step to deal with this tough condition.
Plasma Exchange (Plasmapheresis)
One top treatment for Guillain-Barré syndrome (GBS) is plasma exchange, or plasmapheresis. This method takes out the patient's blood. It then removes the plasma, the liquid part. Next, it puts the blood cells back. It replaces the plasma with a clean fluid. This removes any bad antibodies that harm the nerves.
How Plasma Exchange Works
Plasma exchange helps by taking away the damaging antibodies. This slows down GBS. A doctor draws the patient's blood. This is usually from the arm or neck. It goes through a machine. This machine takes out the plasma. Then, it adds a good fluid. After, the blood goes back to the patient.
Benefits and Risks
Most consider plasma exchange safe for [guillain barre syndrome treatment]. But, it does have some risks, like infections. Plasma exchange might also lower blood pressure or calcium levels. Yet, it has great benefits. It helps people with GBS. They recover the ability to walk sooner. They might not need a breathing machine. Their muscles might regain strength better in the long run.

Quick plasma exchange is key for those getting worse with GBS symptoms. It's useful for all GBS cases, even in severe ones. Proper care during therapy helps handle side effects. Thus, plasma exchange is a vital part of treating this nerve disorder.
Intravenous Immunoglobulin (IVIG) Therapy
IVIG therapy is a common treatment for Guillain-Barré syndrome (GBS). It's based on a blood product with lots of antibodies. These come from healthy donors. IVIG goes into the vein to stop harmful antibodies. This helps lessen how bad the symptoms are and how quickly people recover from GBS. The treatment lasts several days. It's known to be both effective and safe.
A review done by Cochrane in 2006 showed that IVIG works for GBS. Other studies, including ones from 1992 and 1997, found IVIG and plasma exchange to be equally good. Both help with treating Guillain-Barré syndrome.
In 2004, a study looked into adding methylprednisolone to IVIG for GBS. The results showed no added benefit. Also, in 2002, a study on milder cases of GBS offered information on their care and the risk of infections.
For GBS patients who can't walk, IVIG is given in a single dose over five days. Each session takes about three hours. People often need six to 12 months to fully recover. But for some, it may take up to three years. The recovery varies, with some getting completely better and others still having some weakness.
IVIG treatment can cause side effects like headaches and flu symptoms. Some might get bruises or feel sore. Others taste metal in their mouth. It’s critical for patients and doctors to watch for these signs during the treatment.
Supportive Care and Symptom Management
Primary treatments like plasma exchange are key in [guillain barre syndrome treatment]. Additional care is needed for full recovery. For Guillain-Barré syndrome, support and symptom management are critical.
Pain Relief Medications
The nerve damage from [guillain barre syndrome treatment] can be very painful. Your doctors might give you pain meds to help. This can make you feel more comfortable as you heal.
Breathing and Swallowing Assistance
Some people with [guillain barre syndrome treatment] have weak muscles for breathing or swallowing. It might be hard for them to breathe or swallow right. Doctors can help with breathing using special machines. They also suggest ways to make swallowing easier.
Physical Therapy and Rehabilitation
For those with [guillain barre syndrome treatment], rebuilding strength is important. Doctors and therapists will create a plan just for you. It focuses on exercises and using tools to help you get back to daily life.
Support and symptom management aid in [guillain barre syndrome treatment] recovery. They work alongside main treatments. This holistic approach improves patients' lives on all fronts.
Guillain-Barré Syndrome Treatment
Plasma exchange and IVIG therapy are common treatments for Guillain-Barré syndrome (GBS). Sometimes, doctors mix these treatments or try new ones to better help patients. Using both plasma exchange and IVIG together might work better than using just one. This approach deals with symptoms and helps recovery more fully.
Combination Therapies
Doctors might suggest both plasma exchange and IVIG for GBS patients. Using both can take out bad antibodies in the blood and boost the immune system. This could make recovery quicker and complete. It’s especially helpful for severe GBS cases or when one treatment doesn’t work alone.
Experimental and Emerging Treatments
Experts are always looking for new GBS treatments. They’re trying out different ways to make things better and reduce long-lasting effects. Some new treatments in research include corticosteroids, monoclonal antibodies, and stem cells. These methods aim to stop the immune system from hurting the nerves and help them heal.
The fight against Guillain-Barré is getting stronger with new treatments and hope. Patients working closely with their doctors can keep up with the latest treatment news. This way, they can find the best options for their recovery.
Conclusion
Guillain-Barré syndrome (GBS) is a serious nerve condition. It can be life-threatening but can get better with quick and right treatment. Most people recover fully or they get a lot better. Treatments like plasma exchange and IVIG help a lot, along with supportive care. New treatments are always coming out, making things look good for the future.
If you know the treatment options for GBS, you can work with your doctors better. This way, you can improve and get the best results during your recovery. It's important to keep informed and proactive if you or someone you love has GBS. This can really help in getting better and becoming independent again.
GBS may be tough, but there are many ways to treat it now. Those who fight this illness are really strong and give others hope. With good care and support, life can get back to normal for people with GBS. Being well-informed and pushing for good treatments is key to getting better. It helps you take charge of your health and look forward to a better life.
FAQ
What is Guillain-Barré syndrome?
Guillain-Barré syndrome (GBS) is a rare disorder. The immune system attacks nerves. This causes sudden numbness, weakness, and maybe paralysis.
What are the causes and risk factors for Guillain-Barré syndrome?
The cause of GBS is not fully known. It can start after getting sick or a vaccine. Risks include certain illnesses, vaccines, and medical conditions.
What are the typical symptoms of Guillain-Barré syndrome?
GBS shows as muscle weakness, numbness, and balance issues. It can quickly lead to breathing problems. Let's move on to the next question.
How is Guillain-Barré syndrome diagnosed?
Doctors use tests like a spinal tap and nerve tests. They do this to be sure of the diagnosis. Quick treatment is key for a better recovery.
What is plasma exchange (plasmapheresis) and how does it treat Guillain-Barré syndrome?
Plasma exchange removes blood, takes out harmful plasma, and puts back the blood. It can remove the bad antibodies. This may help slow the disease.
What is intravenous immunoglobulin (IVIG) therapy and how does it treat Guillain-Barré syndrome?
IVIG is a blood product with many antibodies. Given through a vein, it can stop the bad antibodies. This makes symptoms less severe and helps recovery.
What other types of supportive care and symptom management are provided for individuals with Guillain-Barré syndrome?
Those with GBS need pain relief, help breathing and swallowing, and therapy. The healthcare team creates a plan for each patient. This helps them recover.
What are some of the emerging treatments for Guillain-Barré syndrome?
New treatments like corticosteroids and stem cells are being studied. These may make GBS easier to treat. Now, let's go to the next topic.
Source Links
- https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/diagnosis-treatment/drc-20363006
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/guillainbarr-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3152164/
- https://www.who.int/news-room/fact-sheets/detail/guillain-barré-syndrome
- https://www.webmd.com/brain/what-is-guillain-barre
- https://www.dukehealth.org/blog/plasma-exchange-therapy-guillain-barre-helps-woman-make-drastic-recovery
- https://pubmed.ncbi.nlm.nih.gov/12076424/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464100/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2883091/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10242495/
- https://infusionassociates.com/infusion-therapy/guillain-barre-syndrome/
- https://emedicine.medscape.com/article/315632-treatment
- https://www.ncbi.nlm.nih.gov/books/NBK532254/
- https://www.nature.com/articles/s41582-019-0250-9
Treatment For Diabetic Neuropathy
Diabetic neuropathy is a severe problem of diabetes. It can lead to nerve damage. This causes pain, numbness, and loss of feeling, especially in the feet and legs. Treating it well involves keeping blood sugar normal, managing pain, and avoiding more problems. This guide will look at ways to treat diabetic nerve damage. It aims to help those with diabetic neuropathy feel better and improve life quality.
Living with diabetic nerve pain is hard, but we are here to help. We provide the information and support you need to handle this problem. Working closely with your healthcare team and finding the best treatment for diabetic peripheral neuropathy is crucial. This way, you can manage your health and work towards a more comfortable life.
Understanding Diabetic Neuropathy
Diabetic neuropathy is a common problem for those with type 1 or type 2 diabetes. Up to 26% of people with type 2 diabetes might have it when they find out. It usually starts with symptoms like pain, tingling, and numbness in the toes and feet.
Symptoms and Diagnosis
Doctors can spot diabetic neuropathy with a checkup and some tests. They look at the patient's symptoms, which might be pain, tingling, or loss of feeling in the feet and toes.
Risk Factors and Complications
Bad blood sugar control, high blood pressure, and being overweight can up the chances of getting neuropathy. If not treated, it can cause foot ulcers, infections, and maybe even the loss of a limb.
Managing Blood Sugar Levels
Maintaining tight control of blood sugar levels is key in managing diabetic neuropathy. This helps prevent further nerve damage. The ADA suggests aiming for blood glucose levels between 80-130 mg/dL before meals and under 180 mg/dL after meals.
Your A1C should be 7% or lower. This is important for most people with diabetes to prevent nerve damage.
Importance of Glycemic Control
It's crucial to reach and keep optimal blood sugar levels. This is shown by A1C tests. For those with diabetes and neuropathy, high A1C levels mean more risk of nerve damage.
Focusing on blood sugar control can help slow down nerve damage. It might also make current symptoms better.
Dietary and Lifestyle Modifications
Besides medicine, what you eat and how active you are matters. A healthy diet and exercise can really help. Try to eat foods that are good for you and do not raise your blood sugar quickly.
Do activities like walking or swimming. This can help your body use insulin better. It's good for your health in many ways.
Working hard to manage blood sugar well is key for people with diabetes. Doing this lowers the impact of neuropathy. It also leads to better health in the long run.
what is the best treatment for diabetic neuropathy
Diabetic neuropathy has no cure. But, there are ways to manage its symptoms and prevent more nerve damage. Medications like pregabalin and gabapentin can reduce nerve pain. Antidepressants and even opioids help too.
Prescription Medications
Prescription drugs are key in managing diabetic neuropathy. Medicines like pregabalin and gabapentin help lessen nerve pain. Antidepressants, including duloxetine, are also effective in treating the pain.
Alternative Therapies
Many people get relief from alternative treatments. These can be topical creams with capsaicin or supplements like alpha-lipoic acid. Other methods include TENS, acupuncture, and acetyl-L-carnitine. Although more research is needed, users often say these methods help.
So, treating diabetic neuropathy often combines medicines, lifestyle changes, and alternative therapies. It's important to work with your doctor to find the best solution. They can guide you on effective drugs and see if alternative treatments help.

Pain Management Strategies
Dealing with severe pain from diabetic neuropathy is crucial. We look into many ways to manage this pain better. We aim to boost our life's quality and how well we function each day.
Over-the-Counter Remedies
Mild to moderate nerve pain can sometimes lessen with basic medications. These include acetaminophen, ibuprofen, and creams with lidocaine. They might be a good option when starting to deal with diabetic nerve pain.
Prescription Pain Relievers
If the pain is severe or constantly there, you might need stronger help. Doctors might recommend drugs like antidepressants or anticonvulsants. Sometimes, opioids can also be an option. These stronger medications can target the pain from diabetic peripheral neuropathy.
Interventional Treatments
For more challenging cases, interventional options might be on the table. These include nerve blocks, spinal cord stimulation, or surgery to release nerve pressure. These advanced methods offer specific help for those facing hard-to-treat pain.

Conclusion
Diabetic neuropathy is a complex condition. It needs a lot of different treatments. By keeping blood sugar levels under control, managing pain, and stopping complications, people can feel better. They can improve how they live.
This guide talks about many treatment choices. These include medicine, alternative therapies, and treatments like surgeries. While diabetic neuropathy can't be cured, the right treatments can help a lot.
Working with your healthcare team is key. Together, you can make a plan that fits you. This can include many treatments to help your specific needs.
Using the advice in this guide can make a big difference. It can help people with diabetic neuropathy better manage their health. They can lessen their symptoms. And they can enjoy a better quality of life.
This guide is key for anyone dealing with diabetic nerve damage. It gives a good overview of treatment options. And it's a great help for managing diabetic neuropathy well.
FAQ
What is diabetic neuropathy and how is it treated?
Diabetic neuropathy is a serious issue with diabetes. It causes nerve damage. This leads to pain, numbness, and sometimes not feeling your feet or legs. To treat it, you must control your blood sugar. You also need to manage pain and stop further problems.
What are the symptoms and risk factors of diabetic neuropathy?
The main type affects many nerves, leading to different symptoms in the toes and feet. These include pain, tingling, and sometimes not feeling anything. The risks are due to bad control of sugar, high blood pressure, and obesity. Smoking is also a big risk.
How important is maintaining blood sugar control for managing diabetic neuropathy?
It's very important to keep your blood sugar in check. This is key to slowing down or preventing more nerve damage. Good sugar control can even make symptoms better for some people.
What are the treatment options for diabetic neuropathy?
Several options are available. These include drugs like anticonvulsants and antidepressants. There are also alternatives like capsaicin cream and acupuncture. The best treatment combines drugs, lifestyle changes, and what suits the person best.
How can the pain associated with diabetic neuropathy be managed?
Dealing with the severe pain is crucial. You can use over-the-counter drugs, prescriptions, or methods that target the nerves. These include nerve blocks or spinal cord treatments. They aim to make life better and improve daily tasks.
Source Links
- https://www.uptodate.com/contents/diabetic-neuropathy-beyond-the-basics/print
- https://www.webmd.com/diabetes/peripheral-neuropathy-treating-nerve-pain
- https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/diagnosis-treatment/drc-20371587
Understanding the Causes of Hereditary Spastic Paraplegia
Have you or someone you love been diagnosed with hereditary spastic paraplegia (HSP)? If so, you're probably looking for answers. This condition is rare and passed down from family. It affects the legs, making them weak and stiff. It is known as familial spastic paraparesis. The cause is genetic, leading to damage in the spinal cord.
The effects of HSP can be very different from one person to another. Some feel only a little weak or stiff. Others get more disabled as time goes by. Doctors use exams and genetic tests to diagnose it. Right now, there's no cure. But, treatments can help you live better.
Physical therapy, medicine, and devices can all help. Doctors will work with you to lessen the muscle problems. By knowing how to treat hereditary spastic paraplegia, you can play a big part in staying healthy and happy.
What is Hereditary Spastic Paraplegia?
Hereditary Spastic Paraplegia (HSP) is a group of disorders you get from your parents. It mostly affects your legs, making them weak and stiff over time. It's also called familial spastic paraparesis. This condition is about motor neurons in the spinal cord. They break down, making your leg muscles not work well.
Signs and Symptoms of Pure HSP
Most people with HSP, about 90%, have a less complex kind. Their main symptoms show up in their legs. They start with weak legs and muscles that are tight. It makes their muscles spasm. They might also have a hard time controlling their bladder. And they could miss feelings in their feet.
Signs and Symptoms of Complicated HSP
But about 10% of those with HSP face more symptoms. They might have nerve problems, epilepsy, or issues with their balance. Sometimes their eyesight, thinking, or skin might be different than usual. This more complex form is a bit harder to handle.
Progression of HSP Symptoms
HSP can act very differently from one person to another. For some, it doesn't change much as they grow up. But for others, it gets a bit worse slowly over many years. The type of gene change you have can affect how bad the symptoms are and how fast they get worse.
What Causes Hereditary Spastic Paraplegia?
Hereditary spastic paraplegia (HSP) comes from genetic mutations. These mutations affect long motor neurons in the spine. These neurons help our leg muscles move and stay toned. There are over 80 types of HSP, each with its own gene mutation. This is why symptoms and how HSP changes over time can vary a lot.
Genetic Mutations Linked to HSP
The genetic kinds of HSP have different gene mutations. This leads to various health issues. HSP symptoms include leg weakness and spasticity, which gets worse over time.
Inheritance Patterns of HSP
HSP can be inherited in different ways. This includes dominant, recessive, X-linked, or from a maternal pattern. For dominant HSP, one bad gene from a parent can cause it. Recessive HSP needs a bad gene from each parent to show symptoms. The X-linked and maternal types are rarer but add to HSP's complexity.
Knowing about the genetic causes of hereditary spastic paraplegia and the inheritance patterns of HSP is key. It helps with diagnosis, genetic counseling, and developing treatments. This knowledge benefits both those with HSP and their families.
Diagnosis of Hereditary Spastic Paraplegia
Diagnosing hereditary spastic paraplegia (HSP) starts with a detailed clinical exam. A neurologist looks at your symptoms, medical, and family history. This is the first step to find out if you have HSP.
Clinical Examination
The neurologist will watch how you walk and check your muscle tone. They'll test your reflexes, feeling, and how well you coordinate. They'll ask about leg weakness, stiffness, and if you have trouble controlling your bladder. They also check your medical and family history for clues about the cause of your HSP.
Specialized Tests
The doctor may do some extra tests to confirm your HSP. These could include MRI scans of your brain and spine, tests on your cerebrospinal fluid, and nerve checks. These tests show if there are any changes or problems in your brain or nerves.
Genetic Testing
Genetic testing is key in diagnosing HSP. It pinpoints the genetic change that causes your condition. Knowing the genetic cause helps in planning your treatment and understanding how serious your HSP might get. The doctor combines your checkup with special tests to make a clear diagnosis.

Treatment Options for Hereditary Spastic Paraplegia
Hereditary spastic paraplegia (HSP) has no cure, but treatments can make life better. Muscle relaxants like baclofen or Botox can ease tight muscles and stiffness. These drugs help you move more easily.
Symptom Management
Physical therapy is key for keeping your muscles strong and flexible. It also helps you walk better. Occupational therapy makes your home and daily life more manageable as HSP gets worse.
Physical Therapy
Physical therapy is vital for HSP. Therapists create exercises just for you. These exercises keep your muscles strong, flexible, and mobile. They can slow down disability and keep you active longer.
Assistive Devices
Moving on, you might need things like braces, canes, or wheelchairs. These aids help you get around better. They boost your independence and keep you doing daily tasks.
HSP is lifelong, but treatments can improve your life. By teaming up with your healthcare providers, you can make a plan to cope with HSP symptoms. This plan can keep you enjoying life as much as possible.

Complications and Outlook of Hereditary Spastic Paraplegia
Hereditary spastic paraplegia (HSP) can bring many problems. People with HSP often have tight and hard calf muscles, causing pain. This makes it hard for them to move. Some may also face nerve damage, resulting in cold feet and other feelings.
Feeling tired, back and knee pain, as well as stress and feeling sad, are also common. The effects can change a lot from one person to another. They depend on the kind of HSP and how well treatment works.
Potential Complications
- Muscle contractures and stiffness
- Nerve deterioration leading to cold feet
- Chronic pain, fatigue, and depression
- Varying levels of disability, from mild to severe
Life Expectancy
The future for people with HSP varies. While some need wheelchairs, others don't need help to move. Normally, HSP alone doesn't make life shorter. But if HSP is more complex, the future is less certain. It depends on the symptoms each person has.
Quality of Life
Living with HSP can be tough, but many find ways to be active. Still, it affects their life greatly. Doing exercises, using tools to help, and taking steps to feel better are key. These can improve how they live.

Clinical Trials and Research Opportunities
Ongoing research and trials help us learn more about treating hereditary spastic paraplegia (HSP). If you or someone you know has this genetic condition, consider joining a clinical trial. Doing so can help you access new treatments and help others by adding to our knowledge about HSP.
Groups like the Spastic Paraplegia Foundation and the NIH's Clinical Research Trials and You program can help. They offer information about HSP research efforts. By getting involved in these studies, you can really make a difference in HSP care. This might help improve future outcomes for those with HSP.
Don't miss the chance to help. Look into clinical trials and studies now. You can take part in making progress in understanding and treating hereditary spastic paraplegia.
Conclusion
Hereditary spastic paraplegia is a mix of genetic problems. It mostly affects the legs. This leads to leg weakness and tightening over time. There is no known cure. But people can use different treatments to make life better.
It's important to learn about this condition’s causes and symptoms. Knowing your care options is also key. This knowledge helps in dealing with hereditary spastic paraplegia for life.
By keeping yourself up-to-date and taking part in research, you can be healthier. You'll feel better emotionally and socially, too. Groups like the Spastic Paraplegia Foundation and NIH can help you join research and trials.
Your involvement in studies can improve future care for HSP patients. This might lead to better outcomes for everyone with this rare disease.
Handling hereditary spastic paraplegia means being active in your care. With enough support and the newest treatments, things can get better. Everyone affected, including families, can aim for a better life. Hope and hard work are important steps in this journey.
FAQ
What is hereditary spastic paraplegia?
Hereditary spastic paraplegia (HSP) is a rare group of inherited disorders. They cause your legs to get weak and stiff over time. It's because of changes in your genes that affect your spinal cord's motor neurons.
What are the main symptoms of hereditary spastic paraplegia?
People with HSP see their legs get weaker slowly. They might have tight muscles and find it hard to control their bladder. Sometimes, they don't feel their feet as well. They could have other issues like nerve damage, epilepsy, trouble balancing, vision problems, and they might find it hard to think clearly.
What causes hereditary spastic paraplegia?
HSP comes from changes in your genes. These changes affect the long motor neurons in your spinal cord. These neurons help control how your leg muscles move.
How is hereditary spastic paraplegia diagnosed?
Doctors usually check for HSP with a detailed exam and some special tests. They look at your symptoms, your health history, and your family's history. Tests like MRI, spinal fluid checks, and nerve tests help rule out other problems.
What treatments are available for hereditary spastic paraplegia?
There's no cure for HSP, but treatments can help make life better. These include medicines to relax muscles, physical and occupational therapy, and using tools like braces or walkers.
What are the potential complications and outlook for individuals with hereditary spastic paraplegia?
People with HSP might face some issues like tight muscles that won't relax, lasting pain, being tired all the time, or feeling sad. How much these problems affect someone can be different. It depends on the HSP type and how they respond to care. Most times, HSP doesn't make life shorter. But if it's a more complex form, things can be less clear.
How can individuals with hereditary spastic paraplegia get involved in clinical research?
Joining research can help find better ways to understand and treat HSP. Families and patients are welcome to check out these studies. They offer a chance to try new treatments and help others learn more about HSP.
Source Links
- https://rarediseases.org/rare-diseases/hereditary-spastic-paraplegia/
- https://www.ninds.nih.gov/health-information/disorders/hereditary-spastic-paraplegia
- https://www.nhs.uk/conditions/hereditary-spastic-paraplegia/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6349696/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6309810/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8835766/
What is Huntington's Disease? An In-Depth Look
Huntington's disease (HD) is a hereditary disease which means its passed down in families. It makes nerve cells in your brain slowly break and die. This attack affects how you move and can lead to uncontrollable dance-like actions.
These movements can happen in your fingers, feet, face, or body. They are called chorea. Over time, these actions can become very obvious. People with HD may also have issues with how they think, feel, and act.
HD usually shows up when you're older (adult HD), but can start in childhood (juvenile HD) - though that's rare. The disease only gets worse as time goes by.
Early HD signs might be mild clumsiness or trouble with balance. Or, you might see changes in thinking, emotion, or behavior. Figuring out and learning about HD is key to coping with it.
Understanding Huntington's Disease
Huntington's disease (HD) is a family-related sickness. It comes from one generation to another. There's a tiny error in the body's building instructions.
This mistake happens in the huntingtin gene. People with HD have this error. It slowly hurts the brain and shows HD signs.
Defining Huntington's Disease
The main problem in HD is in the huntingtin gene. In 1993, researchers found this gene. Anyone can have this gene, but only some get the HD gene.
This disease can affect children, too. They might inherit it from their parents.
Inherited Nature of Huntington's Disease
If a parent has HD, their child has a 50% chance of getting it. The huntingtin gene makes a protein. But in HD, this protein becomes too long and hard to work with.
The problem starts with extra CAG repeats. These make the huntingtin protein faulty.
Causes and Genetic Factors
Over time, this faulty protein gathers in the brain. It harms and kills brain cells. HD comes from a DNA problem called CAG repeats.
What is Huntington's disease?
Physical Symptoms
Huntington's disease (HD) starts slowly. It may be hard to hold a pen or keep your balance. As time goes on, these signs get worse and can make daily life hard. People with HD often fidget and have sudden movements in their face and limbs.
These movements can cause big weight loss and trouble walking. They might find it hard to keep their balance and move well. Later, they may not be able to work, drive, or take care of things at home. They might need help and could get disability benefits.
Cognitive and Behavioral Symptoms
HD can also change how you think and act. At first, you might have trouble planning, remembering, or focusing. You might also feel sad, anxious, or get angry easily. Over 10 to 25 years, these issues can get worse. They may affect your ability to think and talk and make it hard to walk.
Huntington's Disease Progression
The way HD progresses is different for everyone, but it generally gets worse over time. Most people show signs in their 30s or 40s. But sometimes, it shows up before someone turns 20. When this happens, it leads to different signs and a faster progress of the disease.
The time it takes from the first sign to death is usually 10 to 30 years. With early signs appearing before someone is 20, death could happen in 10 to 15 years. Pneumonia, falls, and swallowing issues are common causes of death in HD.
Diagnosis and Treatment
Diagnosing huntington's disease usually involves different steps. A doctor will look at your medical history and do a physical exam. They will also talk to you and maybe do some tests like an MRI. These tests aim to check your brain and see if there's huntington's disease.
Diagnostic Tests for Huntington's Disease
Genetic testing is key in finding out if you have this disease. It checks the huntingtin gene for certain changes. This test is very accurate and can tell for sure if you have huntington's disease.
Managing Symptoms and Care
Unfortunately, huntington's disease doesn't have a cure. But there are ways to help with its effects. There are medicines to manage the jerky movements (chorea) and other symptoms. They can make the condition a bit easier to live with.
Therapies and support are also available. Speech and physical therapy can help you keep up your daily activities. These therapies can improve your quality of life. Overall, a good care plan includes both medical and emotional support.

Latest Research and Developments
Scientists are learning more about Huntington's disease (HD) daily. Their work helps us understand the disease better. They find ways to spot the disease early and look for new treatments. Stem cell research is a hot topic in this field right now.
Understanding Disease Mechanisms
Specialists funded by NINDS look closely at what happens in HD at a tiny level. They check how the huntingtin protein signals cells. They also study its shape and its role in making the disease worse. They want to know if the Huntington gene changes much later can cause or worsen the disease. How healthy DNA in the brain tries to fight off the disease also interests them. This might help find new ways to treat HD by finding new drug targets.
Biomarkers and Genetic Factors
The PREDICT-HD team and others are searching for signs and markers of HD. These markers could help predict and check the disease, showing how treatments are working. They also look at how genes can speed up when HD starts, which affects when the disease shows up. This matters for planning care and coming up with new ways to treat HD.
Stem Cell Research
A dedicated group of scientists is looking into how stem cells can help with HD. They use special HD cell lines to do their research. This work is key to finding new treatments. They aim to fix or replace brain cells harmed by HD.

Conclusion
Huntington's disease is an inherited disorder that affects the brain. It causes many problems, like physical issues, memory loss, and strange behaviors. Right now, there is no cure for it. But, scientists are learning more about it and working on new treatments. They are looking at things like biomarkers and stem cell research.
It's very important to know about Huntington's disease. Supporting research can help us find better ways to care for people with it. We must keep trying to bring hope to those facing this disease.
We are making progress in understanding Huntington's disease. With new knowledge and ongoing support, we can make a difference. Together, we can lessen the harm caused by this illness.
FAQ
What is Huntington's Disease?
Huntington's disease is a health problem that you can get from your parents. It makes nerve cells in your brain stop working and die. This illness affects how you move on purpose and other parts of your brain.
What are the symptoms of Huntington's Disease?
People with Huntington's disease can show many different signs. They might act differently, change moods often, and feel very sad. They could have problems remembering things and not make good choices. Their walk might be unsteady, or they might make movements they can't control. They could also talk in a way that's hard to understand, find it tough to swallow, and lose a lot of weight.
How is Huntington's Disease diagnosed?
To see if someone has Huntington's disease, doctors use different tests and check their medical past. They do neurological and lab tests, look at the brain with imaging, and do genetic testing. The best way to know for sure is by checking the HD gene for a certain mistake.
What treatments are available for Huntington's Disease?
Right now, there is no cure for Huntington's disease. But there are many ways to help with its symptoms. These include using certain drugs, getting therapy to keep moving well, learning how to eat and speak better, and getting the right foods.
What causes Huntington's Disease?
Huntington's disease comes from a mistake in how our DNA works. This error happens in a gene called huntingtin. It makes a bad protein that harms the brain.
How does Huntington's Disease progress?
Huntington's disease gets worse over time, affecting movement, thinking, and talking. At first, people might have trouble planning or remembering things. They might also feel different. Slowly, talking and eating can get hard, and moving can become stiff and slow.
What is the latest research on Huntington's Disease?
Scientists are always studying Huntington's disease. They look at how cells and molecules are involved, find ways to measure the sickness, and explore using stem cells to help.
Source Links
- https://www.ninds.nih.gov/health-information/disorders/huntingtons-disease
- https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/symptoms-causes/syc-20356117
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/huntingtons-disease
- https://hdsa.org/what-is-hd/overview-of-huntingtons-disease/
- https://my.clevelandclinic.org/health/diseases/14369-huntingtons-disease
- https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/diagnosis-treatment/drc-20356122
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10674993/
Physical Therapy for Hereditary Spastic Paraplegia: Benefits and Techniques
Hereditary spastic paraplegia (HSP) is a group of disorders that cause a lot of spasticity and weakness in the legs. HSP can be either pure or complicated, with the complicated type affecting more than just your legs. It can cause problems in different parts of the nervous system, leading to many symptoms.
Physical therapy is very important for people with HSP. It helps manage symptoms and makes life better. The main goals of physical therapy for HSP are to help with moving and flexibility, make muscles stronger, and improve how you live every day.
Understanding Hereditary Spastic Paraplegia
Hereditary spastic paraplegia, or HSP, is a rare group of inherited disorders. They cause increased muscle tightness and weakness in the lower limbs over time. Genetics mutations harm the upper motor neurons. These neurons control leg movement and muscle tone.
What is Hereditary Spastic Paraplegia?
HSP affects the upper motor neurons, leading to difficulties walking and doing tasks. It's also known as familial spastic paraplegia. This disorder makes movement and muscle control hard to manage.
Types of Hereditary Spastic Paraplegia
Hereditary spastic paraplegia has several subtypes, each with different genetic mutations. The pure form mainly affects the lower limbs. The complicated form may impact the whole nervous system, leading to more symptoms. These include difficulties with vision, balance, speech, and intellect. Every person with HSP may experience it differently.
Symptoms and Complications
The key symptoms of HSP are increasing muscle tightness and weakness in the legs. This makes walking and normal activities hard. Some people may have sensory issues, trouble thinking, and other nervous system symptoms, based on their subtype and mutation.
Benefits of Physical Therapy
Physical therapy helps a lot with hereditary spastic paraplegia (HSP). It makes life better for those with HSP. Some benefits are:
Improving Mobility and Range of Motion
Exercises in physical therapy help you move better. They also help you use your legs more. This makes daily life easier and helps you be more independent.
Increasing Strength and Coordination
You can work on making your muscles stronger and improving how you move. This helps you do more and be less at risk of falling. It improves your strength, balance, and coordination.
Enhancing Quality of Life
Physical therapy addresses the problems of HSP. It improves how you move and feel. This lets you do more on your own, feel better, and have fun doing what you like.

Physical Therapy Techniques for Hereditary Spastic Paraplegia
Physical therapists use many methods to help those with hereditary spastic paraplegia (HSP). They aim to boost movement, power, and coordination. This helps improve the way of life of these individuals.
Stretching and Flexibility Exercises
Stretching is key in physical therapy for HSP patients. They need to stretch their leg, hip, and back muscles once or twice daily. This is because HSP can limit movement over time.
Aerobic and Strengthening Exercises
Walking, biking, and water exercises are great for those with HSP. They should aim for three to four sessions weekly. Each should last 15 to 60 minutes. Strength training for various muscles is also critical for mobility and health.
Gait Training and Assistive Devices
Improving how they walk is important for HSP patients. Therapists help with this and teach balance skills. They might use walkers or canes to aid walking. This supports keeping mobility and independence.
A mix of these physical therapy exercises can make HSP easier to live with. It helps manage symptoms and boost overall life quality.
Hereditary Spastic Paraplegia Physical Therapy
Physical therapy is key for those with hereditary spastic paraplegia (HSP). It helps them keep or better their movement, strength, and life quality. Therapists make special plans for each person. These plans might have stretching, strength-building, and walking exercises. They also include using devices to help.
Therapists use many ways to help those with HSP. This includes stretching to stay flexible, and exercises to get stronger. They work on walking using things like walkers. This makes it easier for people to move and do things on their own.
Working together, therapists and patients make plans that fit individual needs and goals. They might add swimming or other gentle exercises to help without hurting the body. The main goal is to keep or make the body work better. This allows patients to enjoy daily life.

There's new hope from ongoing therapy methods and studies. Things like magnetic and electrical activities, plus virtual reality, are making a difference. They are improving movement skills and how patients experience life.
To look after HSP well, a group effort is needed. Physical therapists, neurologists, and others work together. They aim to care for every aspect of the patients' lives. Working in a team, they create plans that support the independence and happiness of those with HSP.
Tailoring a Personalized Therapy Plan
Creating a therapy plan for hereditary spastic paraplegia starts by looking at what each person needs. Physical therapists closely examine every patient. They look at challenges related to moving, strength, staying upright, and daily tasks.
Assessing Individual Needs and Limitations
After this check-up, they design a plan just for that person. This plan is all about addressing the patient's specific issues. It helps overcome the problems caused by hereditary spastic paraplegia.
Incorporating Low-Impact and Aquatic Exercises
As part of this plan, therapists often suggest gentle or water exercises. Things like walking, cycling, and sitting exercises offer a softer way to build up moves and power. Warm water activities, on the other hand, give a big hand to those with tight or painful joints. The water lessens the bother on joints and upgrades how the body works.
Emerging Therapies and Research
Researchers and healthcare workers are looking into new ways to help those with hereditary spastic paraplegia (HSP). They're finding that some treatments show real hope. For example, they are testing out things like transcranial magnetic stimulation and using virtual reality.
Transcranial Magnetic Stimulation
Transcranial magnetic stimulation (TMS) is an exciting method. It doesn't need surgery and uses magnetic fields. It tries to make certain brain areas work better. This can help with moving and control for people with hereditary spastic paraplegia.
Transspinal Direct Current Stimulation
One more possible treatment is transspinal direct current stimulation (tsDCS). It uses a weak electric current on the spine. This might also improve moving and reduce tight muscles in people with hereditary spastic paraplegia.
Virtual Reality and Exergaming
Virtual reality (VR) and games might help, too. They make physical therapy more fun. Those with HSP can try out games that challenge moving and balance. This can help them get stronger and make life more enjoyable. therapies.
Managing Hereditary Spastic Paraplegia: A Multidisciplinary Approach
Helping people with hereditary spastic paraplegia (HSP) works best when many healthcare workers join forces. These experts team up to make a care plan covering physical, emotional, and mental needs.
Collaborating with Healthcare Professionals
A care team for HSP often includes physical therapists, occupational therapists, neurologists, and family doctors. They all work together to understand the patient's challenges and plan a special approach to help them. This teamwork makes sure the patient gets care for everything from moving better and getting stronger to feeling better emotionally and mentally.
Addressing Emotional and Psychological Needs
Having a condition like HSP can be tough emotionally and mentally for both patients and their families. The care team is there to help with emotional and mental health, such as talking to a counselor or joining support groups. Dealing with these needs helps the patients and their families handle HSP better and enjoy life more.
Conclusion
Physical therapy is important for managing hereditary spastic paraplegia. It offers many benefits to keep or improve your mobility, strength, and life quality. Therapists use stretching, exercises, and other methods to create a personalized treatment plan for you.
Many studies have looked at how physical therapy can help with this condition. They have tested different therapies like transcranial magnetic stimulation and virtual reality rehab. These studies show that physical therapy can make a big difference in how you live with this disease.
When dealing with hereditary spastic paraplegia, working with a team of experts is crucial. This team includes physical therapists, neurologists, and occupational therapists. They help you create a plan that meets your physical and emotional needs. With the right care and support, you can lead a full life despite the challenges.
FAQ
What is hereditary spastic paraplegia?
Hereditary spastic paraplegia (HSP) is a rare group of inherited nerve disorders. These cause tight muscles and weakness in the legs. They come from gene changes that affect how the brain sends signals to the legs.
What causes hereditary spastic paraplegia?
It's caused by changes in genes. These affect how our brains send signals to the legs' muscles. This is why the legs become tight and weak over time.
How does physical therapy help with hereditary spastic paraplegia?
It's a big help in making life better for those with HSP. This therapy increases how easily one can move and their muscle strength. It also makes day-to-day activities easier.
What techniques do physical therapists use to treat hereditary spastic paraplegia?
Physical therapists use many methods to help with HSP. They do stretching and strengthening exercises for the legs. Walking practice and special tools to help move may also be part of the plan.
How do physical therapists tailor a treatment plan for someone with hereditary spastic paraplegia?
In creating a plan, they look at each person's specific issues. They check the patient's muscles, strength, and balance. Then, they make up activities and exercises specially designed for that person.
What emerging therapies are being explored for hereditary spastic paraplegia?
New treatments are always being looked into. Some include using magnets or currents to stimulate the brain and spinal cord. Also, virtual reality games that can help with movement are being studied.
How does a multidisciplinary approach help manage hereditary spastic paraplegia?
Handling HSP well means many experts working together. This includes physical therapists, doctors, and more. Together, they make plans for the best care that fits each person's needs.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10716443/
- https://sp-foundation.org/understanding-pls-hsp/treatments-therapies-pages/physical-therapy-and-exercise.html
- https://emedicine.medscape.com/article/306713-treatment
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6642887/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8835766/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8009193/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6349696/
- https://link.springer.com/article/10.1007/s10072-023-07200-1
- https://touchneurology.com/movement-disorders/journal-articles/how-can-we-improve-current-practice-in-spastic-paresis/
- https://www.medicaljournals.se/jrm/content/html/10.2340/16501977-2227
What is Hydrocephalus? Understanding the Condition
Hydrocephalus is a brain disorder. It happens when too much fluid builds up in the brain. This fluid, called cerebrospinal fluid, makes the brain's spaces expand. This puts pressure on the brain and can damage it. This issue can be there from birth or develop later due to injuries. It can happen to people of any age, but it's more common in babies and adults over 60.
Knowing about hydrocephalus and its causes is very important. If it's not treated, it can cause serious symptoms and problems. But, with the right care, many people can live well with hydrocephalus. Later on, we'll talk more about this condition and its different aspects.
What is Hydrocephalus?
Hydrocephalus is the buildup of fluid in the brain's ventricles. It makes the ventricles bigger, putting pressure on the brain. This happens when cerebrospinal fluid doesn't flow right, damaging brain tissues.
It can happen at any age, but it's more common in infants and adults over 60.
Definition and Causes
Your brain floats in a bath of cerebrospinal fluid. This fluid also fills large structures deep in your brain called ventricles. It helps the brain stay buoyant and protected. When there's too much fluid, hydrocephalus occurs. This happens when there's an issue with fluid production and absorption.
Brain Ventricles and Cerebrospinal Fluid
Your brain sits in cerebrospinal fluid. It's in ventricles deep within the brain. These ventricles keep the brain afloat and protected. Hydrocephalus arises when there's a hiccup with fluid production and absorption.
Types of Hydrocephalus
There are different types of hydrocephalus. These include communicating and non-communicating hydrocephalus. There's also normal pressure hydrocephalus, more common in the elderly. Another type is hydrocephalus ex-vacuo, which happens when brain tissue shrinks from damage or disease.

Symptoms of Hydrocephalus
Infants
Infants with Hydrocephalus Symptoms. These include a bigger head size than usual and a quickly growing head. A bulge or tense soft spot on the head could be present.
They might also seem sleepy, be irritable, or not eat well. Other signs can be vomiting, seizures, and eyes looking downward. Babies might have issues with their muscle strength and tone.
Children and Adolescents
Hydrocephalus signs in older kids or teens can vary. Headaches, vision problems, and odd eye movements might happen. The head could also enlarge; they could feel tired or get sick.
They might have issues balancing or coordinating. Appetite might be low, and they could lose control of their bladder. This could lead to crankiness, personality changes, or in school.
Adults
For young to middle-aged adults, symptoms might include headaches or feeling sluggish. They could also lose their balance or speak, have vision issues, or notice memory decline.
Older adults might experience worse memory loss or find it hard to think. Walking, coordination, and balancing could also become difficult. Bladder control problems, particularly for both age groups, can be signs too.
Risk Factors and Complications
Newborns
Hydrocephalus might be there when a baby is born, called congenital hydrocephalus. It's from the brain growing in a way that stops fluid from flowing right. Also, bleeding or an infection when in the womb can cause it.
Other Contributing Factors
Tumors in the brain or spine, infections in the central nervous system, and brain bleeding from events like strokes can lead to hydrocephalus. So can serious head injuries.
Potential Complications
Untreated hydrocephalus can get worse and cause problems like learning and physical issues. It might even lead to death. But, with early treatment, serious problems can be less.
What is Hydrocephalus? Understanding the Condition
Hydrocephalus is a brain condition. It's when too much fluid builds up in the head's ventricles. This pressurizes the brain's tissues. The excess fluid makes the ventricles widen.
It can affect anyone, but it's most common in infants and those 60 or older. The added pressure on the brain can be serious. If not treated, it causes problems with how the brain works.
This issue can happen for different reasons. It might be there when a baby is born. Or it could develop later due to things like tumors, infections, or injuries. People of all ages can get it, but certain groups are at higher risk.
It's vital to know the warning signs of hydrocephalus for fast help. Babies might have a bigger head, be sick a lot, or seem tired and weak. Older kids and teens could get headaches or have trouble seeing or moving. They might also act differently than before.
Adults can struggle with their memory, walking, or handling their bladder. Quick treatment is key to dealing with hydrocephalus. It can stop serious problems from happening. Many with hydrocephalus live fulfilling lives with the right care.
Diagnosis and Testing
Finding out if you have hydrocephalus is the first step in treating it. Your doctor will start by talking with you and checking your health history. Then, they will do a full exam to look at your brain's health.
Imaging Tests
Your doctor might also want images of your brain to diagnose hydrocephalus. They could order an ultrasound, CT scan, or an MRI scan. These tests show if you have too much fluid in the ventricles of your brain. They can check for anything blocking the fluid too.
Other Diagnostic Procedures
If needed, there are more tests. You might have a spinal tap to check liquid pressure. Or, they could use a tiny pressure sensor in your head to monitor the pressure. These tests give your team more information to plan the best care for you.
Treatment Options
Have you or a loved one been diagnosed with hydrocephalus? There are several treatment options. These are to help manage the condition and its symptoms. Shunt surgery is the most common. Another option is endoscopic third ventriculostomy (ETV). After any surgery, it's vital to have ongoing monitoring and possibly rehabilitation for your health and wellbeing.
Shunt Surgery
Shunt surgery is the top choice for hydrocephalus treatment. A flexible tube called a shunt drains extra cerebrospinal fluid (CSF) from the brain. It moves it to another part of the body where it’s absorbed. The shunt has a valve to manage the CSF flow, which eases brain pressure. This surgery takes 1-2 hours and might need a few days in the hospital to recover.
Endoscopic Third Ventriculostomy
Another choice is endoscopic third ventriculostomy (ETV). ETV uses a tiny camera to make a new path for CSF to flow. This action lowers the pressure. It's done under general anesthesia in about an hour. ETV usually has less infection risk than shunt surgery. However, there could be blockage risks over time.
Follow-up and Monitoring
Regular check-ups and monitoring are crucial after hydrocephalus surgery. Your healthcare team will test your brain function. They will also see if you need more rehab or support. It's key to report any troubling symptoms quickly. Shunts may need fixing or can block, needing more surgery to fix.
Conclusion
Hydrocephalus is a serious condition that affects the brain. It needs quick diagnosis and treatment. This stops big problems from happening. It happens when fluid builds up in the brain, mostly in babies and older people.
Doctors often use shunt surgery to treat it. This surgery helps manage the problem. It is important to keep an eye on the condition over time.
Visiting your doctor regularly is key. They can help you know how to live well with hydrocephalus. By learning about it, you can be a big part of your care.
For more on hydrocephalus, check out this guide from the University of New Mexico. With the right help, many people with hydrocephalus lead full lives.
FAQ
What is hydrocephalus?
Hydrocephalus is a disorder from too much fluid in the brain. This fluid buildup can squash the brain's tissues by widening spaces that hold it.
What causes hydrocephalus?
An overflow of cerebrospinal fluid causes hydrocephalus. This happens when the body makes too much fluid or can't clear it well. It's seen from infancy through old age, but most often in babies and seniors.
What are the symptoms of hydrocephalus?
The signs change with age. Babies may show a fast head growth, be sick a lot, and seem fussy. They might also have weak muscles. Older folks might get headaches, trouble with their eyes, or it's harder to think straight. They could also have a hard time walking and controlling when they pee.
How is hydrocephalus diagnosed?
Doctors start with a close look at symptoms, your past health, and how you look and move. Tests, like CT scans and MRIs, show the problem. Things like spinal taps or watching brain pressure might also happen.
How is hydrocephalus treated?
Shunt surgery is the go-to fix for hydrocephalus. A tiny tube lets fluid leave the brain to be soaked up elsewhere. Another choice is a surgery that makes an opening to let fluid out. After either, patients face rehab and regular check-ups.
Source Links
- https://www.mayoclinic.org/diseases-conditions/hydrocephalus/symptoms-causes/syc-20373604
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Hydrocephalus
- https://www.ninds.nih.gov/health-information/disorders/hydrocephalus
- https://www.mayoclinic.org/diseases-conditions/hydrocephalus/diagnosis-treatment/drc-20373609
- https://www.nhs.uk/conditions/hydrocephalus/treatment/
- https://coc.unm.edu/common/manual/hydrocephalus.pdf
Recognizing Ischemic Stroke Symptoms: What to Look For
Ischemic strokes are a major health issue, making up 85% of all strokes and it happens when a blood clot blocks a vital brain blood vessel. This blocks blood supply to the brain.
Ischemic stroke symptoms can start suddenly. They may include trouble speaking, a hard time understanding others, and feeling numb or unable to move one side of your face, arm, or leg. You might have issues seeing with one or both eyes, walking, or keeping your balance. If these signs come and go, it's vital to get medical help right away. Fast action is key in ischemic stroke treatment because every minute matters.
Getting help fast can lower the risk of severe brain damage, death, or disability from an ischemic stroke. Knowing the signs and acting promptly can lead to life-saving care. This can significantly improve your health. In dealing with ischemic stroke management, time is of the essence.
Understanding Ischemic Stroke: A Life-Threatening Emergency
An ischemic stroke happens when a blood clot or plaque piece blocks a brain's vital blood vessel. It stops the blood flow, leading to an ischemic stroke definition. This kind of stroke is more frequent than hemorrhagic strokes, making up more than 85% of cases. Dr. Chandril Chugh says this affects about 800,000 Americans yearly. And these strokes are a main cause of death and disability. Getting quick treatment is key to reducing brain damage and serious outcomes.
What is an Ischemic Stroke?
An ischemic stroke comes from a clot or plaque block in the brain's crucial blood vessel. This stops blood flow, which can cause lasting brain damage if not treated fast.
Prevalence and Impact of Ischemic Strokes
Ischemic strokes are the most common, making up about 87% of all strokes in the U.S. Each year, nearly 800,000 individuals suffer from them. So, the prevalence of ischemic stroke is a big health issue. These strokes often lead to death or severe disability in those impacted.

Knowing the signs of an ischemic stroke and seeking urgent care is critical. Time is brain, and acting fast can reduce damage. It also boosts the chances of surviving and recovering.
Ischemic Stroke Symptoms: Act F.A.S.T.
It's vital to know the signs of an ischemic stroke. Fast medical help could save a life. Look for facial drooping, arm weakness, and speech difficulty.
Face Drooping: A Telltale Sign
One clear sign is a sudden drooping face, often on just one side. It might show as a crooked smile or not being able to shut an eye.
Arm Weakness: Inability to Raise Arms
Suddenly feeling weak or numb in an arm is a sign. Asking them to lift both arms could reveal one arm falling down or not moving.
Speech Difficulty: Slurred or Incomprehensible Speech
Stroke victims may not speak clearly. Their words might be hard to make out. They might struggle to talk or seem lost.
Other signs, like vision problems, walking difficulty, and balance loss, might occur. Act F.A.S.T. and get help at once. Every minute is important in stroke care. Call 911 immediately to improve their chance of recovery.
Risk Factors for Ischemic Stroke
Dr. Chugh says many things can up your chance of a stroke. If you're 55 or older, male, or of African-American or Hispanic descent, you're at risk. Family history, being overweight or inactive, and heavy alcohol or drug use also matter. So does smoking, high blood pressure or high cholesterol, and poorly managed diabetes. Certain heart diseases are a risk too. Knowing and handling these risk factors can lower your chance of a stroke.
Age and Gender
Those 55 and older face a higher risk of ischemic stroke. Men are more likely to have a stroke than women. It's key to be aware of these risk factors. They can help you stay alert about health and get quick medical help if needed.
Race and Ethnicity
Stroke risk can change based on your race and ethnicity. African Americans and Hispanics are more at risk. They also face worse outcomes. This includes a higher death and disability risk. Knowing about these risks is important. It ensures everyone gets the care and treatment they need.
Lifestyle Factors
Your lifestyle choices really matter. Being too heavy or not active, and using a lot of alcohol, drugs, or smoking, increase your stroke risk. A good diet, regular exercise, and dropping bad habits are key. They can lower your risk of a stroke.
Medical Conditions
Health conditions play a big role in stroke risk too. High blood pressure, high cholesterol, and unmanaged diabetes are major risks. So are heart problems like atrial fibrillation. They can make blood clots more likely, which can cause a stroke. It's critical to handle these conditions. This helps prevent strokes.

Diagnostic Tests for Ischemic Stroke
If you or someone shows signs of an ischemic stroke, doctors will do tests. These tests will show the type of stroke and the best treatment for ischemic stroke plan. Dr. Chandril Chugh tells us they use a CT scan or MRI to see the brain and blood vessels. They also do a carotid ultrasound to check the carotid arteries and blood tests for more details.
CT Scan and MRI
Doctors use CT and MRI scans to look at the brain for an ischemic stroke. A CT scan comes first. It quickly shows brain images to identify the stroke type. An MRI is used for tricky cases or after a TIA.
Carotid Ultrasound
Carotid ultrasound checks the neck arteries for blockages within 48 hours. It helps doctors find the causes of ischemic stroke. Then they decide on treatments like surgery or stents.
Blood Tests
Blood tests give more info about the patient's health. They help spot issues like clotting disorders or high cholesterol.
The team needs all this data to diagnose well and plan the right treatment fast. Their goal is to improve blood flow to the brain. This lowers the risk of disability or death.
Ischemic Stroke Treatment: Time is Brain
In treating ischemic stroke, remember: time is brain. With every minute, 1.9 million brain cells may die. Quick treatment is key to reduce brain damage and help the patient recover.
Intravenous Clot-Busting Medication
One main treatment is giving clot-busting meds like tPA through a vein. This drug dissolves the blockage and lets blood flow back to the brain. Studies, like the one in the New England Journal of Medicine in 1995, show how tPA can greatly help stroke patients.
Endovascular Procedures
For some, doctors use endovascular procedures. These are less invasive and use a tiny tube to remove the clot. Endovascular therapy has revolutionized the treatment of ischemic stroke and is big life saver.
Ischemic Stroke Symptoms: What to Look For.
It's vital to know the signs of an ischemic stroke. Quick medical help saves lives. Dr. Chugh says look out for ischemic stroke symptoms like sudden facial drooping, arm weakness, and speech problems. Remember the F.A.S.T. acronym. Vision problems, trouble walking, and balance issues may also happen.
If you see these signs in yourself or others, call 911 right away. Don't wait, even if the symptoms seem to go away.
Knowing and acting fast on ischemic stroke signs can save a life. By getting quick medical help, you boost the chance of recovery. Let’s make sure people get the care they need, without delay.
Conclusion
Ischemic strokes are serious and need quick treatment. Signs include face drooping, weak arms, and trouble speaking. Call 911 fast to boost your chances of help and recovery.
Reducing risk is important too. This means watching your age, lifestyle, and other health factors. Thanks to new medical advancements, doctors can now help more.
Learn about ischemic stroke overview and ischemic stroke management guidelines. This knowledge can help you and your family stay healthy. Remember, acting fast is key to surviving a stroke.
FAQ
What is an ischemic stroke?
An ischemic stroke happens when a blood clot blocks a brain blood vessel. This stops blood from reaching the brain.
How common are ischemic strokes?
Ischemic strokes are common, making up more than 85% of all strokes. They affect about 800,000 Americans every year.
What are the symptoms of an ischemic stroke?
Key signs of an ischemic stroke are sudden face drooping, arm weakness, and speech problems. Remember, F.A.S.T. stands for Face, Arms, Speech, Time - act quickly if these signs show up. You might also have trouble seeing, walking, or staying balanced.
What are the risk factors for an ischemic stroke?
Stroke risk factors include age (55+), being male, and having certain backgrounds like African-American or Hispanic. Other risks are family history of heart issues, obesity, not being active, heavy drinking or drug use, smoking, and high blood pressure. High cholesterol and diabetes also raise your risk.
What diagnostic tests are used to diagnose an ischemic stroke?
Doctors may do a CT scan or MRI to look at the brain and vessels. A carotid ultrasound checks your neck arteries. Blood tests offer more info on your health condition.
What are the treatment options for an ischemic stroke?
Treatments can include meds to break up the clot, like tPA, which helps get blood flowing again. Doctors might also remove the clot with a thin tube called a catheter. Surgery could be needed in some cases too.
Why is prompt treatment for an ischemic stroke so important?
Quick treatment is key because each minute without blood, 1.9 million brain cells can die. The faster someone gets help, the more brain function they can save.
Source Links
- https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
- https://www.ssmhealth.com/services/neurosciences/stroke/ischemic-stroke
- https://medlineplus.gov/ischemicstroke.html
- https://my.clevelandclinic.org/health/diseases/24208-ischemic-stroke-clots
- https://my.clevelandclinic.org/health/diseases/5601-stroke
- https://www.stroke.org/en/about-stroke/stroke-symptoms
- https://www.webmd.com/stroke/understanding-stroke-symptoms
- https://health.ucdavis.edu/blog/cultivating-health/learn-the-5-stroke-symptoms-and-why-you-need-to-act-fast-to-help/2023/05
- https://www.medicalnewstoday.com/articles/318098
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke
- https://www.mayoclinic.org/diseases-conditions/stroke/diagnosis-treatment/drc-20350119
- https://www.nhs.uk/conditions/stroke/diagnosis/
- https://www.aafp.org/pubs/afp/issues/2015/0415/p528.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6188407/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6707502/
- https://www.ncbi.nlm.nih.gov/books/NBK499997/