A Aneurysmal Subarachnoid Hemorrhage is a medical emergency. It happens when a weak area in a brain blood vessel, called an aneurysm, bursts and causes bleeding in the space around the brain. This isn’t just any headache. It can be life-threatening within minutes.
Many people don’t know the signs or risks. That’s why early information is powerful. In this blog, we will explore what an aneurysmal subarachnoid hemorrhage is, how it feels, how it’s treated, and how it can be prevented.
What Happens During an Aneurysmal Subarachnoid Hemorrhage?
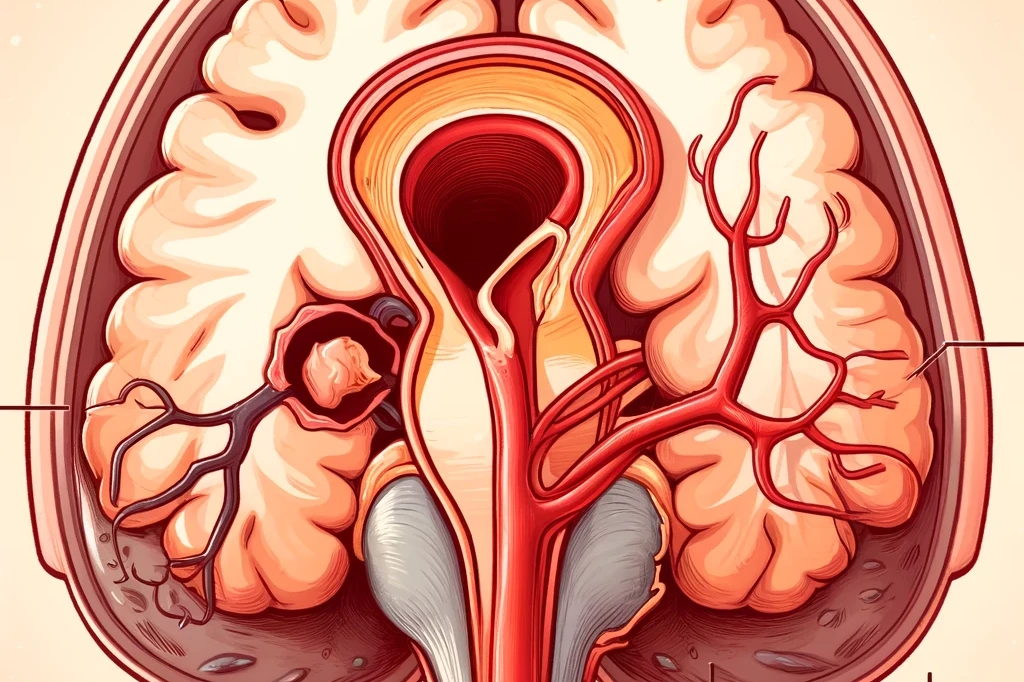
When an aneurysm bursts in the brain, blood leaks into the subarachnoid space, the area between the brain and the thin tissues covering it. This bleeding puts dangerous pressure on the brain.
How Does Bleeding Occur in the Brain During SAH?
Bleeding happens when a weak blood vessel wall breaks. This weak spot is known as an aneurysm.
- The blood spills into the space surrounding the brain.
- This space is filled with fluid that cushions the brain. Blood here causes swelling.
- Pressure builds up fast, squeezing the brain.
This type of bleeding in the brain can stop oxygen and nutrients from reaching brain tissue.
What is the Difference Between Aneurysmal and Non-Aneurysmal SAH?
There are two main types:
- Aneurysmal SAH: Caused by a burst aneurysm.
- Non-Aneurysmal SAH: Bleeding without an aneurysm. Often less dangerous.
Aneurysmal subarachnoid hemorrhage is the most severe and requires immediate treatment.
Read: 8 Foods That Naturally Boost Brain Health
Why is a Brain Aneurysm Rupture Life-Threatening?
A brain aneurysm rupture is like a bomb going off inside the head.
- Blood floods the brain space.
- Swelling leads to high intracranial pressure.
- Brain cells die quickly without oxygen.
Half of all people with aneurysmal subarachnoid hemorrhage die within 30 days. 10–15% never make it to the hospital.
Stat:
- SAH accounts for 5% of all strokes.
- Up to 85% of SAH cases are due to aneurysm rupture.
- Median age of onset: 50–60 years.
- 10–15% of SAH patients die before reaching the hospital.
What Are the Common Symptoms of Aneurysmal Subarachnoid Hemorrhage?
The symptoms often come suddenly and feel extreme. Early action can save a life.
Thunderclap Headache
This is the most classic sign of an aneurysmal subarachnoid hemorrhage.
- Sudden, sharp, worst-ever headache
- Feels like getting hit in the head
- Reaches full strength in seconds
It is often described as a sudden, severe headache that feels “like a lightning strike.”
Are Nausea, Neck Stiffness, and Seizures Also Warning Signs?
Yes, and they can come quickly after the headache.
- Nausea or vomiting
- Stiff neck or light sensitivity
- Confusion or seizures
These symptoms mean the brain is reacting to irritation and swelling from blood. Symptoms like brief fainting, vomiting, and neck pain are also common in SAH.
How Quickly Do Symptoms Develop?
- Symptoms appear within seconds to minutes
- They worsen quickly
- Delay in treatment can lead to death or lasting neurological deficits
The faster you recognize these signs, the better the chances of survival.
Headache Location and Type
- No Specific Location: The pain can be anywhere on the head, making it hard to pinpoint based on location alone.
- Different From Other Headaches: Those with a history of migraines or tension headaches often find the SAH headache to be uniquely severe.
How Is Aneurysmal Subarachnoid Hemorrhage Diagnosed?
Doctors use tests to look for blood in the brain. Time is critical.
🧪 Diagnosis Table:
| Diagnostic Test | Purpose | Time Sensitivity | Notes |
|---|---|---|---|
| CT scan for brain bleeding | Detects fresh blood in subarachnoid space | Immediate | First-line test; quick and non-invasive |
| Lumbar Puncture | Confirms blood if CT is negative | Within hours | Detects xanthochromia in cerebrospinal fluid |
| Angiogram (DSA/CTA/MRA) | Visualizes aneurysm and location of rupture | After confirmation | Guides surgery or endovascular coiling |
How Quickly Should a Diagnosis Be Made?
- Within the first hour of symptoms
- Early diagnosis reduces risk of re-bleeding
- Helps doctors follow SAH treatment guidelines
Table of Contents
ToggleWhat Are the Causes and Risk Factors of Aneurysmal Subarachnoid Hemorrhage?
Several things increase the chances of a rupture. Some you can control, some you can’t.
What Conditions Increase Your Risk of a Brain Aneurysm Rupture?
- High blood pressure
- Smoking
- Alcohol abuse
- Older age
These conditions weaken blood vessel walls.
How Do Genetics, Lifestyle, and Hypertension Contribute?
- Family history means higher risk
- Poor lifestyle choices increase blood pressure
- Genetics may lead to fragile vessels
People with these factors must be more careful.
Are There Gender and Age Differences in SAH Risk?
- Women over 50 are at higher risk
- Risk rises with age
- Hormonal changes may affect vessel strength
Risk Factors and Their Contribution
| Risk Factor | Risk Contribution |
| Smoking | 2–3x increased risk |
| High Blood Pressure | Major contributor |
| Family History | Increases SAH risk by 3–4x |
| Alcohol Abuse | Associated with poor outcomes |
| Female Sex (Age >50) | Higher prevalence |
Why SAH Diagnosis is Often Mistaken?
- Varied Symptoms: A key mistake in SAH diagnosis is missing the wide array of symptoms it can present. Not every case of SAH looks the same, which can lead to oversight.
- Reliance on Head CT Scans: Another pitfall is either not conducting a head CT scan or not fully understanding its limits in identifying SAH.
- Lumbar Puncture Oversights: This procedure, crucial in SAH diagnosis, can be either not performed or misinterpreted, adding to the diagnostic challenges.
A Common Misconception
A major misconception in SAH diagnosis is the belief that patients will always appear visibly ill or show obvious neurological symptoms. In reality, nearly 40% of SAH patients can be awake, alert, and showing no neurological impairments, leading to potential underestimation of their condition.
Our Approach to SAH Diagnosis
- Head CT Scan: A noncontrast head CT scan is essential. Its effectiveness is highest within the first six hours after the onset of symptoms, capturing even small amounts of blood that indicate SAH.
- Lumbar Puncture: If the CT scan doesn’t reveal SAH, a lumbar puncture is typically the next step. This procedure involves collecting and analyzing spinal fluid for signs of bleeding.
- Further Imaging: In cases where CT and lumbar puncture results are inconclusive, additional imaging like CT angiography or MR angiography is considered, especially if symptoms began more than two weeks ago.
The Specifics of Lumbar Puncture in SAH Diagnosis
- What We Look For: During a lumbar puncture, doctors look for high opening pressure, an elevated red blood cell count, and xanthochromia (a pink or yellow discoloration in the spinal fluid), which are tell-tale signs of SAH.
- Differentiating Factors: It’s crucial to distinguish between blood from SAH and blood introduced during the lumbar puncture itself. This distinction is often made by comparing the red blood cell count in different samples of spinal fluid.
Reducing the Chances of Misdiagnosis
Studies suggest that if every patient experiencing a sudden, severe headache (known as thunderclap headache) underwent a head CT scan and, if necessary, a lumbar puncture, the majority of SAH cases would be correctly diagnosed. There remains a small risk of missing cases, particularly those with non-ruptured aneurysms, but this approach significantly reduces the likelihood of misdiagnosis.
How Doctors Identify the Cause of Bleeding in Subarachnoid Hemorrhage?
- Finding the Source of a Brain Bleed: A Key Step in SAH Treatment
Once a Subarachnoid Hemorrhage (SAH) is diagnosed, the next crucial step is to find out where the bleeding is coming from. This is typically done using special imaging techniques, and understanding these can help demystify the process.
Choosing the Right Imaging Technique
Digital Subtraction Angiography (DSA):
- Considered the most detailed test for finding brain aneurysms.
- Can also be used to treat the aneurysm at the same time.
- However, it’s more complex than other methods.
Computed Tomography Angiography (CTA):
- Faster and easier to do than DSA.
- Often the first choice in emergency situations.
- Can miss small aneurysms but is getting better with technological advances.
Magnetic Resonance Angiography (MRA):
- Another non-invasive option like CTA.
- Useful for planning surgery but not as detailed as DSA.
What Are the Treatment Options for Aneurysmal Subarachnoid Hemorrhage?
Once diagnosed, fast and focused treatment starts. Surgery is often needed.
| Treatment Method | Purpose | Timing | Key Benefit |
| Neurosurgical clipping | Clamps the aneurysm shut to stop bleeding | Early (within 72h) | Reduces risk of rebleeding |
| Endovascular coiling | Fills aneurysm with coils via catheter | Early (within 72h) | Less invasive, safer for deep vessels |
| Blood pressure management | Prevents rebleed and maintains stability | Continuous | Lowers risk of complications |
| ICU monitoring for SAH | Tracks vital signs, detects vasospasm | Ongoing in ICU | Improves survival and brain protection |
| Intracranial pressure control | Prevents further brain injury | ICU stay | Keeps pressure in safe range |
What Are the Possible Complications After an SAH?
Complications can happen right away or weeks later.
| Complication | Description | Frequency | Impact on Recovery |
| Cerebral vasospasm | Brain arteries shrink days after bleeding | 30–70% of cases | Can lead to stroke and more damage |
| Hydrocephalus | Blood blocks brain fluid flow, causing pressure buildup | Up to 20% | May need surgical drain/shunt |
| Delayed ischemic neurological deficits | Reduced blood flow causes stroke-like problems | Common in severe SAH | Causes weakness, vision loss, confusion |
What Is the Recovery Time for Aneurysmal Subarachnoid Hemorrhage?
Healing takes time. Every patient recovers at a different speed.
- Short-term: ICU care for 1–2 weeks
- Long-term: physical therapy, medication
- Most recover in 3–6 months
Is Full Recovery Possible After SAH?
Yes, but not always.
- 30% have permanent problems
- Recovery depends on age, bleed size, and time to treatment
- Most return to daily life with support
What Role Does Neurorehabilitation Play?
It helps regain lost skills.
- Movement training
- Speech therapy
- Memory exercises
Subarachnoid hemorrhage recovery time depends a lot on rehab.
Stats:
- 30% survivors have permanent disability
- Recovery ranges from weeks to months
See a Neurologist if You Suspect a Brain Aneurysm
A Aneurysmal Subarachnoid Hemorrhage is serious, fast, and deadly without proper care. Know the signs. Reduce your risks. If you or someone you love has symptoms, act fast. The brain doesn’t wait.
Don’t ignore your body’s warning signs. Book a consultation with Dr. Chandril Chugh today to protect your brain health.
FAQs
Can stress cause a brain aneurysm to burst?
Stress alone is unlikely to cause an aneurysm to rupture. However, it can raise blood pressure, which may increase the risk of rupture in someone with a pre-existing brain aneurysm.
What are the chances of surviving an aneurysmal SAH?
Survival rates are around 50%, and outcomes depend heavily on early detection and treatment. People who receive care within the first 24 hours have better recovery rates.
Can a brain aneurysm go unnoticed?
Yes, many brain aneurysms remain silent with no symptoms. They are often found by accident during scans for other problems or during screenings in high-risk individuals.
Is aneurysmal SAH hereditary?
There is a known genetic link. If you have a close relative who had an aneurysmal SAH, your own risk may be three to four times higher than average.
What are the first warning signs of a brain hemorrhage?
The most common sign is a thunderclap headache—sudden and severe. Other signs include nausea, vomiting, neck stiffness, and brief loss of consciousness.
Can aneurysms be detected before they rupture?
Yes, non-invasive imaging like CT angiography or MR angiography can detect aneurysms before they burst, especially in people with family history or risk factors.
What not to do after a subarachnoid hemorrhage?
Avoid smoking, alcohol, intense physical exertion, and activities that raise blood pressure. Regular follow-ups and lifestyle changes are crucial to avoid complications.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.