Multiple system atrophy (MSA) is a rare disease that affects the brain and spinal cord. It leads to problems with balance, movement, and more. Catching multiple system atrophy (MSA) early is key to managing it well.
This condition’s signs often come on slowly. They can look like other brain conditions, like Parkinson’s. Knowing the initial symptoms of what is multiple system atrophy is vital. This knowledge can push you to get medical help. It can also help you start the right treatment, improving how you live.
Table of Contents
ToggleWhat is Multiple System Atrophy?
Definition and Overview
Multiple system atrophy (MSA) is a rare disease that acts fast, affecting how your body works without you controlling it. It messes up your balance and how you move, causes trouble with going to the bathroom, and messes with how your body reacts without you thinking about it. This happens because of some proteins in your brain that shouldn’t be there, destroying parts of the brain. MSA comes in different types, based on which problem is most noticeable, whether it’s with movement or balance.
Causes and Risk Factors
The exact reasons behind MSA are still a mystery, but doctors think it’s from both your genes and things in the environment. It’s not really something you get from your family, but certain gene changes might make it more likely to happen. Things like being around harmful chemicals or some viruses might also be linked to getting MSA. At the heart of it, though, is the wrong protein building up in your brain, causing brain cells to die and the disease’s symptoms to show up.
Early Symptoms of Multiple System Atrophy
Bladder and urinary problems are often the first signs of multiple system atrophy (MSA). This includes always feeling like you need to urinate, urinating a lot, and not being able to control your bladder. The issue also involves having trouble fully emptying your bladder. Autonomic nervous system dysfunction is the cause, which regulates these functions. As MSA progresses, these issues worsen and become hard to deal with.
Erectile Dysfunction in Men
Men with MSA might also face early erectile dysfunction. This means they can’t get or keep an erection. It’s caused by the autonomic nervous system not working right. This system is key for bodily functions, including sexual health. MSA’s damage on the nerve cells in the brain and spine can cause this. Early erectile problems in MSA men can greatly affect their quality of life and sex life.
Orthostatic Hypotension
A sudden drop in blood pressure when standing is orthostatic hypotension, and it’s common in MSA. This happens because the autonomic nervous system can’t control blood pressure well. So, when someone with MSA stands up, their blood vessels don’t tighten as they should. This leads to quick blood pressure drops and feelings of dizziness or even fainting. Early addressing of this issue is vital for managing MSA’s impact on daily life.
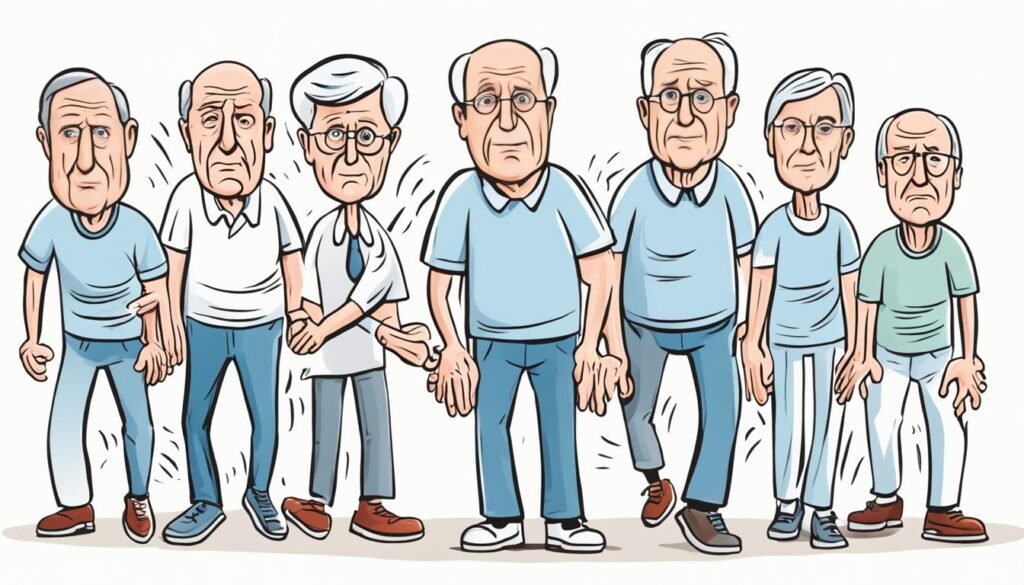
Motor Symptoms of Multiple System Atrophy
Cerebellar Ataxia
Cerebellar ataxia is a key motor symptom found in multiple system atrophy (MSA). It involves the loss of coordination and balance. This happens due to the cerebellum degenerating, which affects movement coordination.
People with MSA… difficulties with walking, standing, and doing small tasks. They might struggle with tasks like buttoning a shirt or using utensils. Additionally, they might have slurred speech, tremors, and uncoordinated movements.
These challenges can make everyday life hard and can affect independence.
Bradykinesia and Muscle Rigidity
MSA also brings bradykinesia and muscle rigidity, similar to Parkinson’s disease. Bradykinesia means moving slowly, making it hard to start or finish movements. They may walk slowly with very small steps.
Muscle rigidity, the muscles getting stiff, might lead to painful cramps. This makes moving even harder. Unfortunately, these symptoms don’t improve with Parkinson’s treatment, which makes MSA tough to deal with.
Other Common Symptoms
Multiple system atrophy (MSA) affects the autonomic nervous system. This system manages many of our body’s automatic functions. People with MSA can have trouble controlling their blood pressure, sweating, digesting food, and with sexual functions. A big issue is orthostatic hypotension, where blood pressure suddenly drops when standing up. This can also cause constipation, swallowing problems, and changes in how much you sweat. All these issues can greatly affect daily life.
Sleep Disturbances
Many with MSA face sleep problems. Issues like not sleeping well, being too sleepy during the day, or snoring can happen. There’s also restless legs or acting out dreams during REM sleep. These sleep issues come from the brain parts that control sleep and autonomic problems, both hit by MSA. Managing sleep is key for quality of life and daily activities.
Speech and Swallowing Difficulties
Over time, MSA might make speaking and swallowing harder. The disease can make your voice weak, soft, or hoarse. It might also cause problems with talking and swallowing. People could slur their speech, find it hard to swallow, and be at risk of choking. These issues affect how someone interacts with others and eats. They’re very important to manage when dealing with MSA.

multiple system atrophy symptoms
Multiple system atrophy (MSA) brings a wide mix of symptoms. These can change a lot from one person to the next. You might see the following signs most often:
- Bladder and urinary problems, like always feeling like you need to pee, peeing often, not being able to control your bladder, or having trouble emptying it.
- In men, not being able to perform sexually is often an early warning sign of MSA.
- When a person stands up, they might feel dizzy, light-headed, or even faint. This is called orthostatic hypotension.
- A condition called cerebellar ataxia causes issues with balance, coordination, and speaking. It’s from damage to the cerebellum.
- Slow movement and stiff muscles, making it hard to move, similar to what happens in Parkinson’s disease.
- Autonomic dysfunction affects how well people’s body functions work, changing how their blood pressure, sweat, digestion, and sex life work.
- Sleeping troubles, like not being able to fall asleep or to stay awake during the day, or doing things while you sleep that you shouldn’t, such as kicking or screaming.
- Speaking and swallowing can become hard, leading to a weak, quiet, or rough voice and issues with eating.
These symptoms can really hurt a person’s life and their daily activities. They often get worse fairly quickly over 5 to 10 years. It’s very important to spot these signs early and to manage them well. This is key in taking care of people with MSA.
Diagnostic Process for MSA
Diagnosing multiple system atrophy (MSA) is tough. Its symptoms look like other brain diseases, especially Parkinson’s. In the beginning, telling MSA apart from Parkinson’s is hard. But, there are differences doctors look for to get it right. People with MSA see their symptoms get worse quickly.
They don’t respond well to Parkinson’s drugs, like levodopa. And they have problems with their automatic body functions very early on. This includes low blood pressure when standing up. MSA also shows more issues with talking and eating than Parkinson’s. Checking for Parkinson’s is a big first step in finding MSA.
Neurological Exams and Brain Imaging
To find MSA, doctors do a deep neurological check and use brain scans. They ask about your health history and check your body. They look at how your symptoms have changed over time. Neurological tests see how well you move, keep balance, and if automatic functions are working right.
Scans like magnetic resonance imaging (MRI) look for brain changes linked to MSA. These tests help rule out other brain issues. This way, doctors can make a clear diagnosis.

Managing Multiple System Atrophy
There is currently no cure for multiple system atrophy (MSA). But, healthcare providers can help manage its symptoms to improve life quality. They use a team approach to handle each symptom as it shows.
Treating Specific Symptoms
Medications play a big part in managing symptoms like feeling dizzy when standing, trouble going to the bathroom, and not sleeping well. Physical therapy, work therapy, and speech therapy are also key. They help keep movement, independence, and the ability to talk.
Health providers might suggest changes in diet. They may also give devices to make life easier for people with swallowing issues and other challenges. By focusing on each person’s needs, the aim is to keep their life quality high even as MSA progresses.
Therapies and Support
Besides symptom management, healthcare providers might suggest therapies and support services. These can benefit both the person with MSA and their caregivers. Activities like physical and work therapy help keep movement and independence longer. Speech therapy improves communication and eating. It also teaches new ways to get your ideas across.
Talking to a counselor or joining support groups can be very helpful. They’re good for dealing with the feelings and changes that come with MSA. Caregivers can get a break with respite care or help with money. This is to lessen the stress of looking after someone with this nerve disorder.
Prognosis and Life Expectancy
Multiple system atrophy (MSA) is a quick moving nerve disease. Sadly, the outlook for people with MSA isn’t good. On average, those with MSA live between 6 to 9 years from when symptoms start. Yet, some might live longer, up to 10 years or more. This disease moves fast, making symptoms worse over time. This leads to big challenges and loss of independence.
How fast MSA gets worse can change from person to person. The kind of MSA, how strong the symptoms are, and how someone responds to treatments can all affect how long they live. The MSA type that looks like Parkinson’s disease is common. It brings problems like stiff muscles and moving slowly.
There is no known cure for MSA. But spotting the symptoms early and managing the disease well can make a big difference. A study pulling together many others found almost half of the people with MSA survived. Another study at the Mayo Clinic showed that when MSA starts with problems like blood pressure or sweating, it usually means a tough road ahead.
Learning about how MSA progresses and what it means for life comes from many different studies. For example, looking at lots of Japanese patients and in-depth studies on a smaller group helped a lot. The Mayo Clinic also used autopsies to learn more. They found that tests on how your body’s automatic functions are doing are crucial for diagnosing MSA.
Looking into the history of similar diseases in almost 500 patients also gave valuable insights. These findings help doctors understand what to expect in the long run for people with MSA. Lastly, looking at how Korean patients with MSA have done offered more global perspective. But in general, the future for someone with MSA isn’t bright. Still, getting an early start on managing their condition can bring comfort and a better quality of life.

Living with Multiple System Atrophy
Living with multiple system atrophy (MSA) is a big challenge for both the person and their family. This disease keeps getting harder as time goes on. People may find it tough to do everyday tasks and need more help moving around. Good coping strategies are important for handling the emotions, difficulties, and physical changes of MSA.
Coping Strategies
Here are some helpful ways to deal with MSA:
- Try to stay positive and focus on enjoying life.
- Get help from physical, occupational, and speech therapists to keep your body working well.
- Use tools like walkers or wheelchairs to move easier.
- Make adjustments to your lifestyle, such as changing your diet, to deal with problems like constipation.
- Talk to a counselor or join a support group to get emotional support.
- Always speak up for what you need and be involved in your healthcare decisions.
Caregiver Support
For those taking care of someone with MSA, the job is tough and can impact you physically, mentally, and money-wise. Caregivers need support too, including:
- Getting time off through respite care programs for much-needed breaks.
- Connecting with others in similar shoes by joining support groups.
- Seeing a counselor to handle the stress of caregiving.
- Looking into financial aid and local resources for care costs.
- Taking care of yourself and keeping a good balance between your personal life and your caregiver role.
By finding good ways to cope and getting support, those with MSA and their families can face the challenges ahead while aiming for the best life quality.
Conclusion
Multiple system atrophy (MSA) is rare and severely affects the brain and spinal cord. It brings on many symptoms that make life hard. Recognizing these symptoms early is important for diagnosis and care.
Unfortunately, there’s no cure for MSA. But, managing its symptoms through a team approach can enhance the life of those with MSA. Health teams and families can create plans to care for the specific needs of each patient.
Research is ongoing to learn more about MSA and find new treatments. It’s key for those with MSA and their families to stay informed and involved in their health. By closely working with doctors and using support services, they can manage through MSA and aim for the best life possible.
FAQ
What is multiple system atrophy?
Multiple system atrophy (MSA) is a rare disease that affects the brain and spinal cord. It slowly gets worse over time. People with MSA have trouble with balance, moving, and controlling their bladder.
What causes multiple system atrophy?
We don’t fully understand the causes of MSA. Both genes and the environment seem to play a part. The condition is linked to the buildup of certain abnormal proteins in the brain.
What are the early symptoms of multiple system atrophy?
Early signs of MSA can include problems with peeing, erectile dysfunction in men, and a drop in blood pressure when someone stands up.
What are the motor symptoms of multiple system atrophy?
Motor symptoms of MSA involve the loss of balance and coordination. They also include slow movement and stiff muscles.
What other common symptoms are associated with multiple system atrophy?
MSA can also cause issues with the autonomic system, sleep, and problems talking or swallowing.
How is multiple system atrophy diagnosed?
It’s hard to diagnose MSA because its symptoms are like those of other diseases, like Parkinson’s. Doctors do a full checkup, various tests, and rule out other conditions to be sure.
How is multiple system atrophy treated?
There’s no cure for MSA, but doctors can help with the symptoms to make life better. This care includes medicine, therapy, and support from various health professionals.
What is the prognosis and life expectancy for individuals with multiple system atrophy?
MSA gets worse quickly, and the outlook isn’t good. The average life span after symptoms start is 6 to 9 years. Some people may live more than 10 years despite this.
How can individuals with multiple system atrophy and their caregivers cope with the challenges of the condition?
Coping with MSA is tough for the person affected and their family. It’s crucial to find support and use every available resource to deal with the disease’s effects on both physical and emotional levels.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859695/
- https://www.nhs.uk/conditions/multiple-system-atrophy/
- https://www.ninds.nih.gov/health-information/disorders/multiple-system-atrophy
- https://www.mayoclinic.org/diseases-conditions/multiple-system-atrophy/symptoms-causes/syc-20356153
- https://www.mayoclinic.org/diseases-conditions/multiple-system-atrophy/diagnosis-treatment/drc-20356157
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139446/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10485100/
- https://en.wikipedia.org/wiki/Multiple_system_atrophy
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




