A migraine is a neurological disorder that affects how your brain processes pain and sensory signals. A headache is a broad symptom with many causes, often linked to muscle tension, dehydration, or illness. Knowing the difference helps you choose the right care and avoid delays that can worsen attacks.
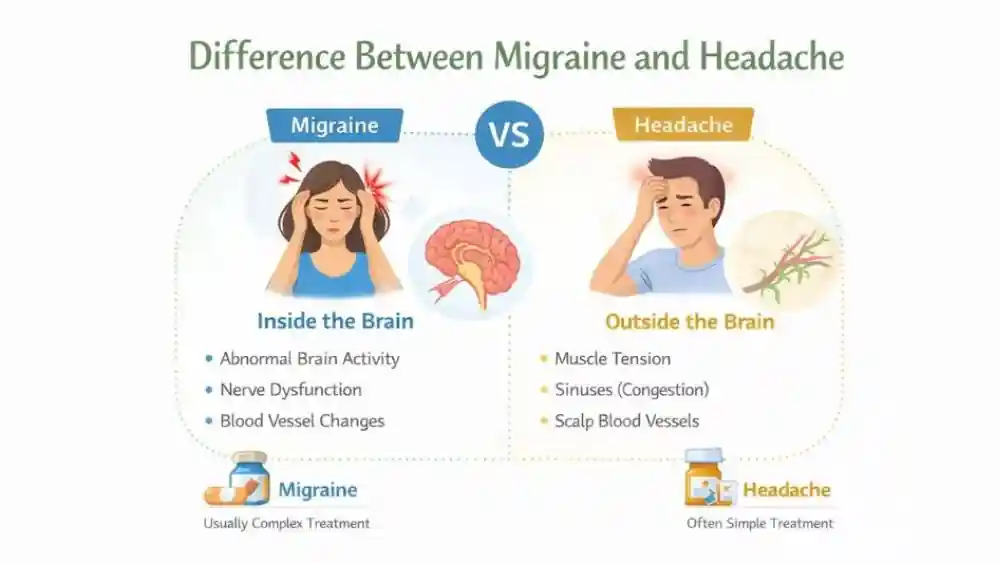
Difference Between Migraine and Headache
The difference between migraine and headache begins with what is happening inside your body. A headache usually starts outside the brain, often in muscles, sinuses, or blood vessels near the scalp. A migraine starts inside the brain and nervous system, where pain pathways become overly sensitive.
Why Migraine Is Not “Just a Headache”
A migraine involves abnormal brain activity. Nerve cells release chemicals that increase pain and inflammation. This is why a migraine can bring nausea, vomiting, and sensitivity to light or sound. A headache rarely affects these systems. This clear difference between migraine and headache explains why simple painkillers may help a headache but fail during a migraine attack.
People with migraine have changes in brainstem activity and altered pain control even between attacks. That pattern does not appear in people who only get a headache .
How The Nervous System Is Involved Differently
During a migraine , the trigeminal nerve, a major facial nerve, sends repeated pain signals to the brain. Blood vessels around the brain also react abnormally. This causes throbbing pain and sensory overload.
In a headache , nerve signaling stays normal. Muscles tighten and restrict blood flow, creating pressure pain. This nervous system gap is a core difference between migraine and headache .
Why Correct Diagnosis Matters
When a migraine is mistaken for a headache , treatment often fails. Delayed care can increase attack frequency and severity, whereas early, correct treatment for migraine lowers long-term disability. Correct diagnosis also reduces medication overuse, a known cause of chronic pain.
Headache vs Migraine Symptoms
The symptoms of migraine are broader and more disruptive than the symptoms of headache . Pain alone does not tell the full story.
Pain Intensity And Quality Comparison
A headache usually feels like steady pressure or tightness. Pain stays mild to moderate. A migraine often causes moderate to severe pain that throbs or pulses. Movement can worsen it. These differences in pain quality help separate symptoms of headache from symptoms of migraine in daily life.
Associated Symptoms (Nausea, Light Sensitivity)
Nausea is common in a migraine . Some people vomit or lose their appetite. Light and sound may feel unbearable. These are classic symptoms of migraine caused by sensory processing changes in the brain. A headache may cause mild discomfort but rarely triggers these reactions. Light sensitivity during a migraine activates visual areas of the brain even when eyes are closed. This does not happen with a typical headache .
Duration And Recurrence Patterns
A headache often ends within hours and responds to rest. A migraine can last from four hours to several days. Attacks often return in patterns. Hormonal cycles, sleep loss, or stress can predict timing. This recurrence pattern is another major divide between symptoms of headache and symptoms of migraine .
Migraine vs Headache Pain Location
Migraine pain often follows nerve pathways linked to the eye, temple, or one side of the head. Headache pain usually spreads evenly across the scalp or neck due to muscle involvement.
Typical Pain Areas In Headaches
A headache often affects both sides of the head. Pain may wrap around the forehead or press at the temples. Neck and shoulder muscles may ache. This bilateral pattern defines the pain location of headache in tension-related cases.
One-Sided vs Bilateral Pain In Migraine
A migraine often starts on one side of the head. It may shift sides between attacks, but usually stays unilateral during one episode. This one-sided pattern is a hallmark pain location of migraine and helps guide diagnosis.
Neck, Eye, And Temple Involvement
A migraine frequently causes pain behind one eye or deep in the temple. Neck stiffness may appear due to shared nerve pathways. A headache usually stays superficial. These distinctions between the pain location of a headache and the pain location of a migraine help you describe symptoms clearly to a doctor.
Migraine vs Headache Causes
The causes of migraine include genetic sensitivity, neurotransmitter imbalance, and brain hyperexcitability. The causes of headache are more mechanical or situational, such as dehydration, posture strain, or infection. This cause gap shapes prevention strategies.
Common Headache Triggers
Stress is the most common trigger. Poor posture strains neck muscles. Dehydration reduces blood volume. Eye strain from screens also contributes. These causes of headache are usually short-term and reversible.
Neurological And Genetic Migraine Triggers
A migraine often runs in families. Inherited changes in ion channels control nerve signaling. Brain chemicals like serotonin fluctuate during attacks. These internal changes define the causes of migraine and explain why attacks can start without obvious external triggers. Hormonal shifts, especially estrogen changes, strongly influence migraine risk. This link is weaker in people with a simple headache .
Role Of Stress, Sleep, And Hormones
Stress affects both conditions, but its impact differs. Stress tightens muscles and leads to a headache . In a migraine , stress alters brain signaling and lowers pain thresholds. Poor sleep disrupts brain recovery and raises migraine risk. Hormonal changes strongly affect the causes of migraine , especially around puberty, pregnancy, and menopause.
Migraine vs Headache Treatment
Migraine care and headache care work on different levels. Using the wrong approach often leads to poor relief or repeated attacks. Treatment choices depend on attack pattern, severity, and how your body responds.
Over-The-Counter Options And Limits
For a headache , over-the-counter pain relievers often work. These drugs reduce muscle tension and mild inflammation. They support short-term treatment for headache when the pain stays mild or moderate. Problems start when these drugs are used too often. Repeated use can cause rebound pain, also called medication-overuse headache.
In a migraine , these same drugs may only dull pain or fail. Frequent use of simple painkillers can worsen migraine frequency over time. This limit shows why treatment for headache cannot replace proper treatment for migraine .
Migraine-Specific Medications
Doctors use targeted drugs for migraine attacks. These medicines act on serotonin pathways in the brain, which regulate pain and blood vessel activity. They work best when taken early in an attack. They do not cure migraine , but they shorten attacks and reduce their intensity.
Preventive medicines may also be prescribed when attacks are frequent. These drugs aim to stabilize nerve signaling. Dosage varies by age, health status, and attack pattern. Doctors usually adjust treatment slowly to avoid side effects. Preventive therapy reduces attack days in many people with chronic migraine .
Lifestyle And Preventive Strategies
Lifestyle changes support both conditions. Regular sleep helps the brain reset. Hydration prevents blood volume changes linked to pain. Balanced meals stabilize energy levels. These habits strengthen treatment for migraine plans and improve long-term treatment for headache success. Avoiding known triggers remains one of the most effective preventive tools.
When To See A Doctor For Migraine Or Headache
Sudden onset, neurological changes, or pain with fever may indicate conditions beyond migraine or headache . Early evaluation prevents missed diagnoses and complications.
Red-Flag Symptoms You Should Not Ignore
Sudden severe head pain needs urgent care. Pain with fever and stiff neck may signal infection. Vision loss, confusion, or fainting requires evaluation. These signs go beyond common symptoms of headache or symptoms of migraine and demand medical review.
Headaches That Need Urgent Evaluation
A new headache after age fifty should be checked. Pain following a head injury matters even if it seems mild. Headaches that wake you from sleep may point to pressure changes in the brain. Doctors may order imaging to rule out bleeding or tumors.
Migraine Symptoms That Mimic Stroke
Some symptoms of migraine look alarming. Temporary weakness, numbness, or speech trouble can occur during certain migraine types. Because these signs overlap with stroke symptoms, doctors must rule out emergencies
Can A Headache Turn Into A Migraine?
Yes. A headache can trigger a migraine in people with sensitive nervous systems. Ongoing stress, sleep loss, or delayed treatment increases this risk. Early intervention helps stop this escalation.
Transition From Tension Headache To Migraine
Stress often starts as muscle tension. This causes a headache . In people with sensitive nervous systems, ongoing stress lowers pain thresholds. This can trigger a migraine attack. Early rest and hydration may stop the progression.
Medication Overuse Headaches
Frequent painkiller use changes how the brain processes pain. This leads to daily or near-daily pain that mimics migraine . This condition often improves only after medication reduction under medical guidance.
Importance Of Early Intervention
Treating pain early reduces nerve sensitization. Early care shortens attacks and lowers recurrence risk. This approach is central to long-term migraine management and prevents chronic patterns.
How Doctors Diagnose Migraine vs Headache
Diagnosis relies on symptom patterns, frequency, and triggers rather than scans. Migraine diagnosis follows strict criteria based on attack features. Headache diagnosis often depends on identifying reversible causes.
Clinical History And Symptom Patterns
Doctors ask detailed questions about pain type, timing, and triggers. They compare symptoms of migraine with symptoms of headache over time. Family history also matters, especially for migraine , which often runs in families.
When Imaging Or Tests Are Needed
Scans are used to rule out serious causes. They do not confirm a migraine . Most people with migraine have normal imaging results. Tests are reserved for red-flag signs or unusual patterns.
Diagnostic Criteria For Migraine
Formal criteria include attack duration, pain features, and associated symptoms. Meeting these criteria separates migraine from other headache disorders. This structured approach improves treatment accuracy.
Living With Migraines or Chronic Headaches
Chronic pain reshapes daily routines, focus, and energy levels. Migraine often causes post-attack fatigue and brain fog, while chronic headache leads to ongoing discomfort. Structured management improves function and consistency.
Daily Life Impact And Productivity
A migraine can stop work, school, and social plans. Recovery time after attacks may include fatigue and poor focus. A headache may slow productivity but rarely causes prolonged aftereffects.
Trigger Tracking And Headache Diaries
Keeping a diary helps identify the causes of migraine and causes of headache . Recording sleep, meals, stress, and weather patterns reveals trends. Many doctors rely on diaries to adjust treatment plans.
Long-Term Management Strategies
Long-term care focuses on consistency. Regular routines calm the nervous system. Stress management reduces attack frequency. Education empowers you to respond early and effectively.
Prevention Tips For Migraine And Headache
Prevention reduces total pain days more than rescue treatment alone. Regular sleep, hydration, and stress control stabilize pain thresholds. Avoiding personal triggers remains one of the strongest protective strategies.
Sleep, Hydration, And Diet
Irregular sleep raises migraine risk. Dehydration triggers both conditions. Skipped meals destabilize blood sugar. These basics matter more than many people expect.
Stress Management Techniques
Relaxation techniques lower muscle tension and nerve excitability. Deep breathing and structured breaks reduce both headache and migraine frequency over time.
Avoiding Common Triggers
Bright lights, strong smells, and prolonged screen time often trigger migraine attacks. Poor posture contributes to headache development. Avoiding triggers requires awareness, not perfection.
FAQs
How Do I Know If It’s A Migraine Or a Headache?
You can tell by pain type and symptoms. A migraine often includes nausea, light sensitivity, and one-sided throbbing pain. A headache usually causes steady pressure without sensory overload.
Are Migraines More Serious Than Headaches?
A migraine is a neurological disorder with genetic and brain-based causes. A headache is a symptom with many triggers. Migraines often need long-term medical management.
Can Headaches Cause Nausea Like Migraines?
Most symptoms of headache do not include nausea. When nausea or vomiting occurs, doctors consider symptoms of migraine more likely.
What Is The Fastest Way To Relieve Migraine Pain?
Early treatment works best. Doctors usually recommend taking prescribed medication at the first sign of an attack. Resting in a dark, quiet space supports migraine treatment .
Do Migraines Show Up On Brain Scans?
No. Brain scans usually look normal in people with migraine . Imaging is used to rule out other conditions, not to confirm migraine itself.
Can Children Have Migraines?
Yes. Children can develop migraine , often with shorter attacks and more stomach symptoms. Early diagnosis helps prevent school and learning issues.
Is Migraine a Lifelong Condition?
For many people, migraine persists for years. Frequency and severity may change with age, hormones, and lifestyle adjustments.
Can Dehydration Cause Migraines or headaches?
Yes. Dehydration is a well-known trigger. It contributes to common causes of headache and can also trigger migraine attacks in sensitive individuals.
Are Migraines Linked To Sleep Problems?
Yes. Poor sleep quality increases attack risk. Regular sleep schedules reduce migraine frequency, according to sleep medicine research.
When Should I Worry About Frequent Headaches?
If a headache becomes frequent, severe, or changes pattern, you should seek medical advice. Chronic pain needs evaluation to prevent long-term complications.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.