Cluster headaches are sudden, severe, one-sided headaches that strike in repeating cycles, often around the same time each day, and are one of the most painful headache conditions known.
The attacks bring sharp pain behind one eye along with redness, tearing, and a blocked nose on the same side. Because the pain builds fast, you need approaches that work fast, which is why treatment focuses on oxygen therapy, rapid-acting triptans, and steady routines that protect the body’s internal clock.
To deal with cluster headaches in a more controlled way, you must spot attack patterns early, avoid major triggers like alcohol and disrupted sleep, and use rescue treatments as soon as symptoms start.
Keeping a daily log, supporting good sleep habits, and working with a headache specialist strengthen your long-term plan.
Table of Contents
ToggleWhat Are Cluster Headaches?
Cluster headache is a brain disorder where you get very strong, one-sided head pain that comes in groups called clusters. A cluster period can last from a few weeks to several months, and then you may have a long break with no pain at all. Every single attack usually lasts 15 to 180 minutes. That timing range is confirmed in studies reviewed by NIH and other expert groups.
During a cluster period, you may have up to eight attacks in a day. You might feel fine between attacks, which makes life feel like a constant waiting game. When doctors treat cluster headaches , they pay attention to both the pain during attacks and the pattern over months.
What Makes Cluster Headaches Different From Migraines & Other Headaches
In a cluster headache, pain is usually sharp, burning, or drilling on one side of the head, centered around the eye. It builds to full strength within minutes. Many people feel so restless that they pace or rock instead of lying still.
Migraine pain is often throbbing and can affect one or both sides of the head, and you may prefer to lie down in a dark, quiet room. Tension headaches feel more like a tight band around your head and do not usually cause eye redness or a blocked nose.
These clear differences matter because they change how doctors treat cluster headaches and what medicines they choose. Treatments that help migraine may be too slow for cluster attacks.
Why Cluster Headaches Are Called “Suicide Headaches”
The pain from cluster headaches is so intense that some people have reported thoughts of self-harm. Surveys in peer-reviewed articles show a higher rate of suicidal thoughts in this group compared with the general population.
Doctors do not use this nickname to scare you. They use it to stress how serious the pain can feel and why fast ways to treat cluster headaches are important. If you ever feel like you might hurt yourself, you should see this as a medical emergency and seek help right away.
How Common Are Cluster Headaches & Who Is At Risk
Cluster headaches are rare compared with migraine. WHO and large reviews say that about 0.1 percent of people are affected, which means around 1 in 1,000.
They usually start between the ages of 20 and 40. Men are diagnosed more often than women, although women may be misdiagnosed with migraine at first. Smoking is a strong risk factor. Having a family member with cluster headaches also raises your risk.
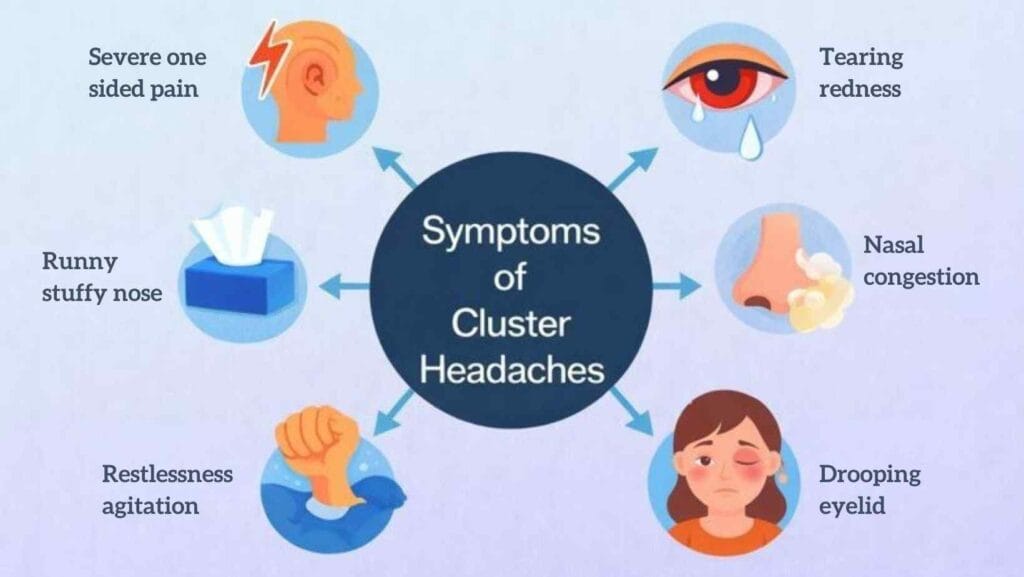
Cluster Headache Symptoms
Classic Symptoms: Severe One Sided Pain, Tearing, Nasal Congestion
The classic cluster attack has a sudden start. You feel severe pain on one side of your head, often behind or around one eye. That eye may turn red, water, or swell. The eyelid might droop, and the pupil can look smaller.
On the same side, your nose may block or run, and your forehead may sweat. These are called autonomic symptoms (automatic body responses) and show that nerves around the eye are deeply involved
Attack Patterns (Cyclic, Episodic Vs Chronic Cluster Headaches)
Most people have episodic cluster headache. You have clusters that last weeks or months, with daily attacks, followed by breaks of at least three months. Around 80 to 90 percent of people fall into this group.
Chronic cluster headache is less common. Attacks continue for more than a year without a long break or with only short pain-free gaps. Doctors may use different cluster headache treatment options for chronic cases, such as stronger preventive plans, since the burden on daily life is higher.
Warning Signs Before An Attack
Some people feel mild warning signs before a full attack. You may notice a dull ache around the eye, slight tearing, or a strange sense of pressure. Restlessness can show up even before the real pain starts. Many attacks wake you 1 to 2 hours after you fall asleep, which matches your natural sleep cycle.
Fast action gives you a better chance to stop cluster headaches before they peak, especially when your doctor later adds oxygen or other acute treatments.
Cluster Headache Triggers
Alcohol, Strong Smells, Heat, Bright Lights
Alcohol is a well-known trigger during an active cluster period. Even a small drink can quickly start an attack.
Strong smells, such as petrol, paint, or heavy perfume, and exposure to bright sunlight or flashing lights can also spark attacks in many people. When doctors help you treat cluster headaches , they usually advise strict alcohol avoidance during cluster periods and careful handling of these triggers.
Sleep Disruptions & Circadian Rhythm Changes
Cluster headaches have a close link with your internal clock, also called the circadian rhythm. The hypothalamus (a deep brain area that controls sleep and hormones) shows abnormal activity in brain scans of people with cluster headache.
Irregular bedtimes, night shifts, and jet lag can all increase attacks. Good sleep habits are an important part of managing cluster headache attacks , even before any medicine is used. This also explains why some natural remedies for cluster headaches focus on sleep support, such as melatonin in later treatment plans.
Tobacco, Stress, Altitude, Other Common Triggers
Cigarette smoking is both a risk factor and a trigger. Many studies note that a high number of people with cluster headaches smoke or used to smoke, although not every smoker develops this condition. Stress, intense exercise, hot baths, and high altitude travel can also raise the chance of an attack.
What Causes Cluster Headaches?
Role Of The Hypothalamus (Biological Clock)
Brain imaging from multiple research groups shows that a small area called the posterior hypothalamus (part of the body’s “clock”) lights up during cluster attacks. This region controls daily rhythms such as sleep, appetite, and some hormones. When you treat cluster headaches , keeping your sleep and daily schedule steady helps support this brain area.
Nerve Pathway Dysfunction & Vascular Changes
Cluster headache belongs to a group called trigeminal autonomic cephalalgias. In simple terms, the trigeminal nerve (the main facial nerve) and nearby autonomic nerves fire abnormally and send pain signals. Blood vessels around the eye widen, and chemicals that cause inflammation are released.
The pain starts from nerve network changes rather than from blocked blood flow. This is why modern plans to treat cluster headaches focus on nerve pathways, not general painkillers alone.
Genetic & Environmental Factors
Family studies show that cluster headaches can be more common in close relatives, which means genes play some role. At the same time, smoking, sleep habits, and hormone changes are important outside factors.
So far, no single “cluster gene” explains everything. Medical groups such as WHO and NIH stress that research is still growing, and findings may change as new studies appear. For now, doctors treat cluster headaches by balancing what they know about biology with your personal triggers and lifestyle, not by relying on one genetic test.
Diagnosis: How Doctors Confirm Cluster Headaches
Doctors confirm cluster headache mainly by listening to your symptom pattern. They ask when the pain starts, how long attacks last, where the pain sits, and what happens to your eye and nose.
A full nerve exam checks strength, balance, reflexes, and vision. This helps rule out other problems that might look similar. These steps guide how they treat cluster headaches most safely.
CT or MRI Scans to Rule Out Other Conditions
A CT or MRI scan does not show cluster headache directly, but it helps rule out issues like tumors, bleeding, or infections. Since cluster pain sits near the eye, doctors want to be sure that nothing behind the eye or in nearby blood vessels is causing the attacks. These scans help build a safe plan to treat cluster headaches without missing anything important.
When to See a Neurologist or Headache Specialist
You should see a neurologist if your attacks are frequent, last longer than expected, or do not respond to early treatments. Specialists are trained to spot rare headache types and can guide you through both standard and advanced cluster headache treatment options . They also help if you have other health conditions that may limit medicine choices.
How to Stop Cluster Headaches During an Attack
High Flow Oxygen Therapy
High-flow oxygen is one of the fastest tools to stop cluster headaches during an attack. You breathe pure oxygen through a tight mask at a flow your doctor recommends. Many people feel relief in around 15 minutes when they start early.
Oxygen is safe for most patients and does not cause sedation, which makes it a top option when doctors treat cluster headaches at home or in urgent care.
Fast-Acting Triptans
Triptans used as injections or nasal sprays act much faster than pills. They target nerves that send pain signals during an attack. Doctors often use them when oxygen alone is not enough.
These medicines work best when taken at the first sign of pain. Because they affect blood vessels, doctors check your heart history before adding them to your cluster headache treatment options .
Cold Compresses, Relaxation, and Deep Breathing
Cold packs placed over the eye or temple can dull pain for some people. Simple breathing exercises help ease panic and give you some control while other treatments start to work. These steps are support tools, not stand-alone treatments, but they still play a part when you treat cluster headaches at home.
Safe Ways to Cope During Intense Pain
The pain can make you feel restless or panicked. Choose a safe space where you can sit upright, breathe slowly, and start your rescue plan. Keep sharp objects away. If fear rises, call a trusted person. Sudden mood drops are common and deserve care just like physical pain. Good coping skills support long-term management of cluster headache attacks .
Natural Remedies for Cluster Headaches
Melatonin, Magnesium, Kudzu Extract
Some people try natural remedies for cluster headaches to support medical treatment. Melatonin helps balance the sleep cycle, which may reduce night attacks. Magnesium supports nerve activity, and low levels can raise headache risk.
Kudzu extract is a plant-based option with early reports of benefit, though expert groups say research is still limited. None of these replace medical care, but they can be added with your doctor’s guidance when you treat cluster headaches .
Capsaicin Cream, Essential Oils, Cold Therapy
Capsaicin cream used inside the nose can reduce how strongly the face nerve reacts. Essential oils like peppermint may relax muscle tension, though support for cluster headache is limited.
Cold therapy, such as ice packs or cool air, remains simple and helpful. These ideas may stack with your other cluster headache treatment options but should never replace proven medical steps.
Evidence-Based vs Unsupported Natural Treatments
Reliable sources warn that some herbs sold online have no proof and may interact with medicines. When choosing natural remedies for cluster headaches , focus on options with at least some clinical data, always tell your doctor, and avoid products that promise a cure. Cluster headache is complex, and experts agree that no single natural plan works for everyone.
Cluster Headache Treatment Options
Preventive Medications
Preventive medicines help shorten cluster periods and reduce daily attacks. Verapamil is often the first choice and needs heart checks while you take it. Lithium is used when other options fail, especially in chronic cases. Short steroid courses may stop a fresh cluster cycle. These medicines help you treat cluster headaches before they even start and work alongside attack-time treatments.
Nerve Blocks and CGRP Treatments
A nerve block places numbing medicine near a nerve at the back of your head. Many people feel fewer attacks for weeks. CGRP medicines block pain signals and can be helpful for some patients. Both methods expand your cluster headache treatment options when standard medicines are not enough.
Neuromodulation Therapy
Neuromodulation uses small electrical pulses to calm overactive nerves. Some devices are placed on the skin, while others require surgery. These steps are for people with very severe, chronic symptoms who did not respond to other ways to treat cluster headaches .
Managing Cluster Headache Attacks Daily
Tracking Triggers and Patterns
A simple diary helps you spot cluster headache triggers such as alcohol, poor sleep, bright light, or strong smells. Tracking also helps you show your doctor what works and what does not. It is one of the most useful ways of managing cluster headache attacks long-term.
Sleep Hygiene and Circadian Rhythm Control
Sticking to a steady sleep schedule supports your body clock. Cluster attack timing is closely linked to this clock, so stable sleep can lower attack risk. Avoid screens before bed, keep your room dark, and follow the same wake time every day. Better sleep also boosts your ability to treat cluster headaches effectively.
Lifestyle Changes That Reduce Attack Frequency
Avoid alcohol during a cluster period. Try to quit smoking. Stay hydrated and eat steady meals. Reduce long gaps between meals to prevent drops in energy that may trigger pain. Gentle movement, fresh air, and stress control all support managing cluster headache attacks .
Support Groups and Mental Health Strategies
Cluster headaches affect mood, work, and family life. Support groups help you connect with others who understand this condition. Therapy helps you build skills to handle fear of the next attack. Caring for mental health is part of how you treat cluster headaches , not something separate.
FAQs
What instantly helps a cluster headache?
High-flow oxygen and fast-acting triptans give the quickest relief for many people and form the core of how doctors treat cluster headaches during attacks.
What is the fastest way to stop a cluster headache attack?
Starting oxygen or your rescue triptan at the earliest warning sign is the fastest method to stop cluster headaches before they peak.
Can cluster headaches be prevented?
Preventive medicines, steady sleep, and avoiding key cluster headache triggers can lower attack frequency even though they may not stop every cycle.
What natural remedies actually work for cluster headaches?
Melatonin, magnesium, and capsaicin cream are the natural remedies for cluster headaches with the most supportive evidence, though results differ by person.
How long do cluster headache attacks last?
Most attacks last 15 to 180 minutes, and knowing this range helps guide how you treat cluster headaches with fast acting tools.
What triggers cluster headaches the most?
Alcohol, sleep changes, strong smells, and tobacco are common cluster headache triggers and often appear repeatedly in headache diaries.
Why do cluster headaches happen at the same time every day?
The body clock inside the brain shapes attack timing, which is why sleep routines matter when you treat cluster headaches .
Do cluster headaches get worse with age?
Some people see fewer attacks with age, but others stay the same, so doctors adjust cluster headache treatment options as your pattern changes.
Can lack of sleep cause cluster headaches?
Poor or unstable sleep raises attack risk for many people, making sleep care a key part of managing cluster headache attacks every day.
Do cluster headaches cause brain damage?
Cluster headaches do not appear to cause brain damage, but they impact quality of life, so early steps to treat cluster headaches remain important.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.