Understand Lumbar Radiculopathy: An Overview
Lumbar radiculopathy brings pain, numbness, and weakness to the lower back and legs. It's a common…
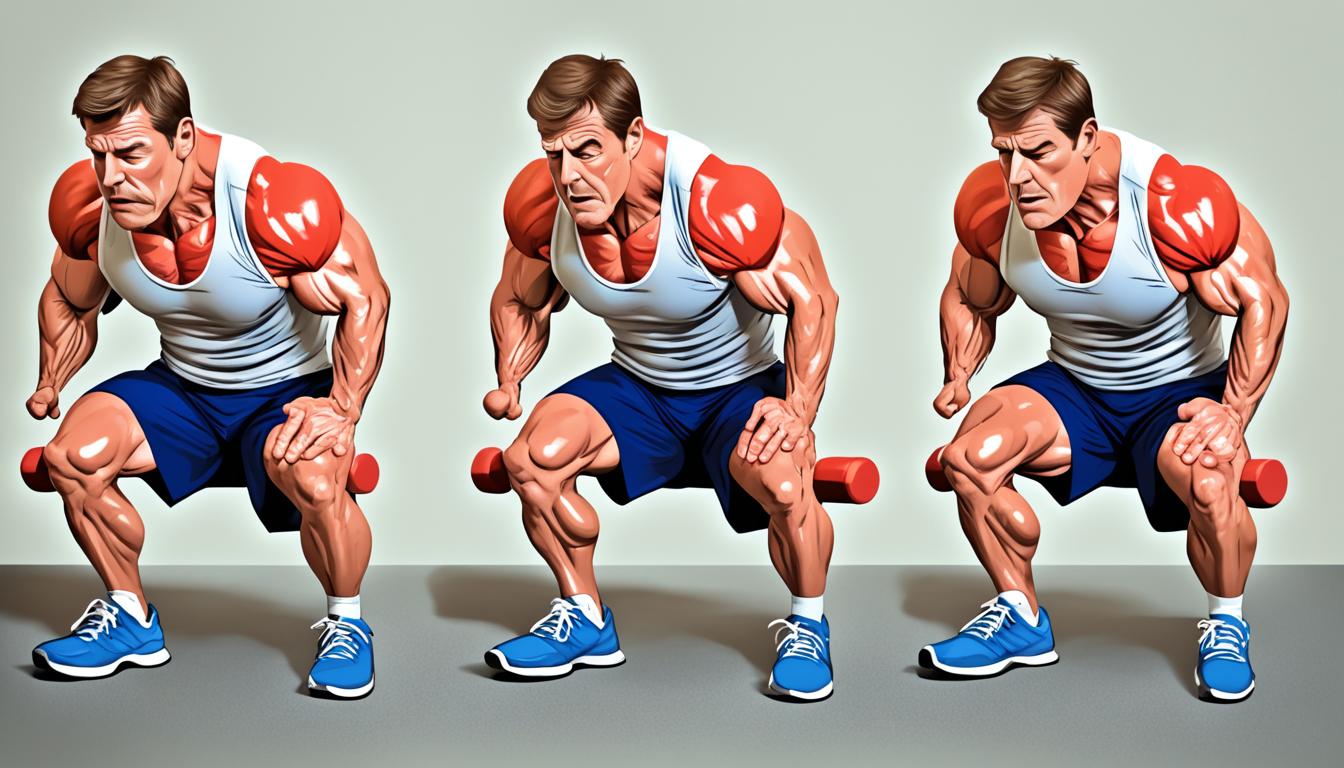
Top Lumbar Radiculopathy Exercises for Pain Relieve
Lumbar radiculopathy exercises are one of the most effective ways to reduce lower back pain caused…
Drugs That Cause Myoclonus: What You Need to Know
Understanding Myoclonus What is Myoclonus? Myoclonus is sudden jerks in your body. Myoclonus is…
What is Myoclonus? A Comprehensive Guide
Myoclonus is a unique and puzzling movement issue. It's marked by quick, sudden muscle movements…
What is Hereditary Spastic Paraplegia? An Overview
Hereditary spastic paraplegia (HSP), or familial spastic paraparesis, is a group of inherited…
What is Neuropathy? An Overview
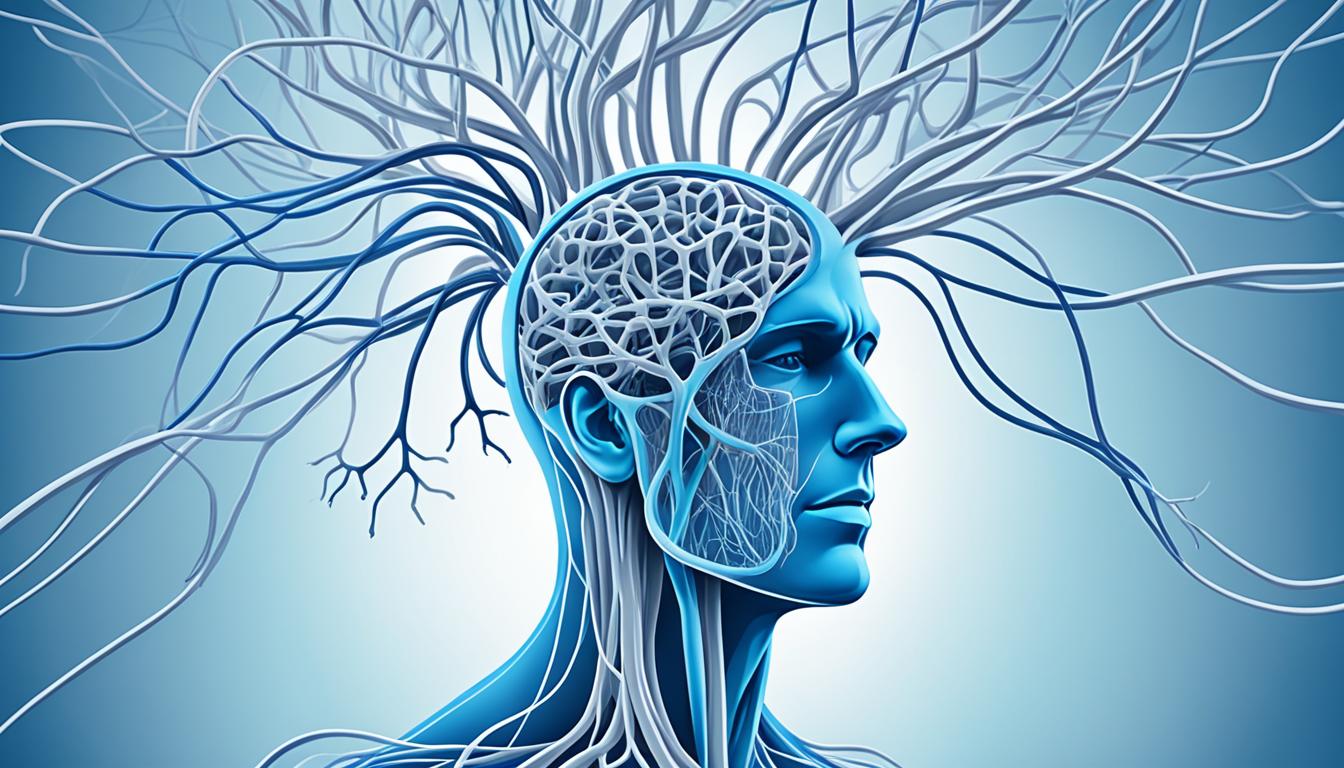
Neuropathy is when your nerves are damaged or not working right. It often affects the peripheral…
Understand Landau Kleffner Syndrome: Overview and Key Facts
Have you ever seen a child suddenly stop talking or act like they don’t understand you anymore? For…
Understand Muscular Dystrophy Symptoms
Muscular dystrophy is a set of genetic diseases that make your skeletal muscles weaker over time.…
Multiple System Atrophy Symptoms: Recognizing Early Signs
Multiple system atrophy (MSA) is a rare disease that affects the brain and spinal cord. It leads to…
Multiple Sclerosis Medication: Types and Benefits
Multiple sclerosis (MS) is a long-lasting disease that affects the body's immune system. It…
Multiple Sclerosis Treatments: Therapeutic Approaches
Multiple sclerosis, or MS, is a long-term autoimmune disease. It affects the brain and spinal cord,…
What is Multiple Sclerosis? Exploring the Condition
Multiple sclerosis (MS) is a common disease that affects young adults. Its symptoms usually start…
Multiple Sclerosis Symptoms: Understanding the Signs
Multiple sclerosis (MS) is a complex disorder that affects the nervous system. It can change your…
Mitochondrial Inheritance Diseases: Overview and Key Aspects
Mitochondrial inheritance diseases are a type of genetic issue. They affect the energy production…
Moyamoya Disease Treatment: Options and Advances
Moyamoya disease is a rare but serious disorder of the brain's arteries. It causes them to narrow…
Exploring Miller Fisher Syndrome: Symptoms and Treatment options
Miller Fisher syndrome is a rare disease where nerves are attacked. It's like a type of…
What is Myasthenia Gravis? An Overview
Myasthenia gravis is a long-lasting neuromuscular disease. It makes voluntary muscles weaker. This…
What is Encephalitis? An In-Depth Overview
If you're worried about encephalitis, you're not alone. It's a serious brain condition that needs…
What is Paraneoplastic Syndrome? Understanding This Rare Condition
If you've faced cancer, the term "paraneoplastic syndrome" might have come up. It's a rare group of…
What is Polymyositis? Understanding This Inflammatory Muscle Disease
Do you have mysterious muscle weakness and feel tired all the time? You might be curious about…
Effective Polymyositis Treatment: Medical and Therapeutic Approaches
Polymyositis is a rare condition that weakens muscles due to inflammation. This article focuses on…
Effective Benign Peripheral Nerve Sheath Tumor Treatment: Medical and Surgical Approaches
These tumors form around your peripheral nerves and can lead to pain, numbness, tingling, and…
Effective Opsoclonus Myoclonus Syndrome Treatment
Opsoclonus myoclonus syndrome (OMS) is a rare condition that often affects children and can make…
Understanding Progressive Supranuclear Palsy: Causes, Symptoms, and Treatment
Progressive supranuclear palsy (PSP) is a rare and complex brain disorder. It causes problems with…
Effective Progressive Supranuclear Palsy Treatment: Medical and Supportive Approaches
If you've just been diagnosed or are already dealing with PSP's challenges, this article is for…
Best Energy Drinks for Studying – Backed by Science & Neurology
The best energy drinks for studying are more than a caffeine kick. They affect your brain…
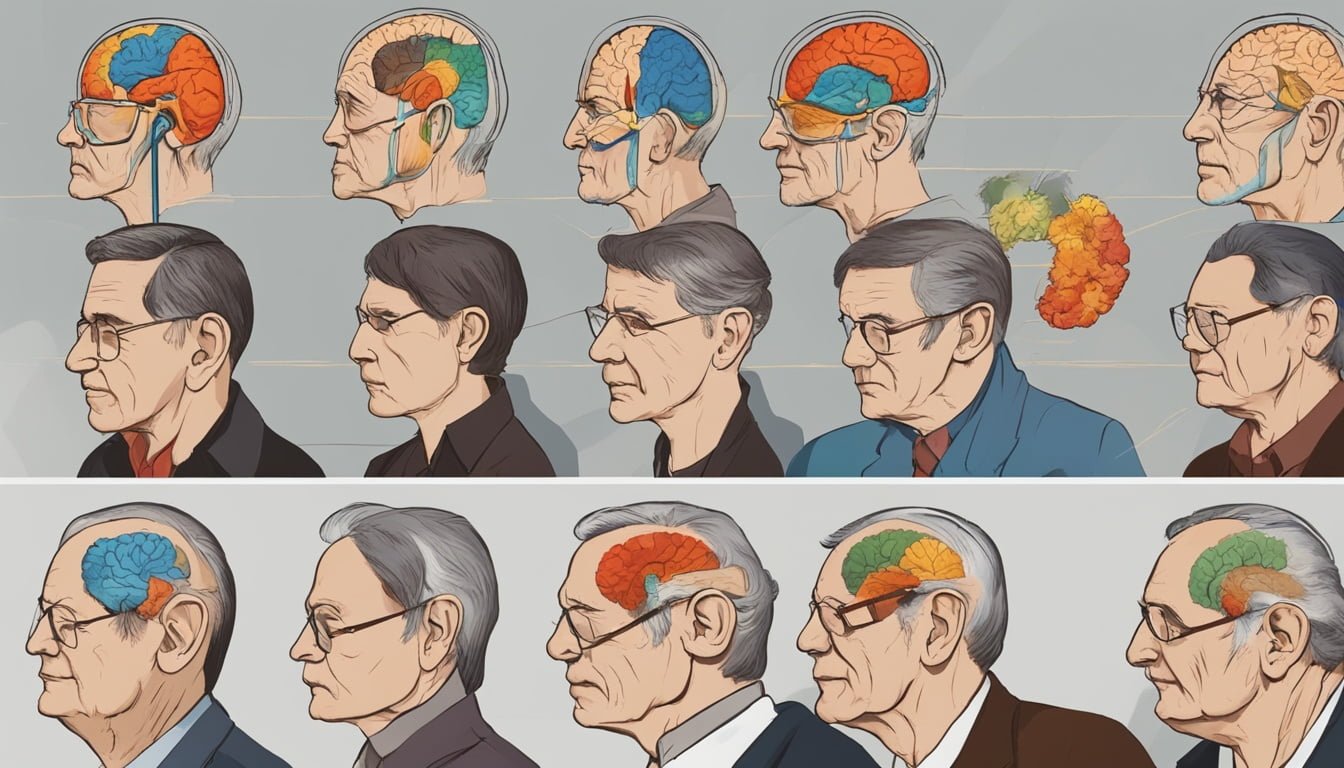
The 7 Stages of Frontotemporal Dementia: A Progression Overview
7 stages of frontotemporal dementia explain how this condition usually moves from small, odd…
What is Frontotemporal Dementia? A Detailed Explanation
Frontotemporal dementia (FTD) is a group of disorders. They happen when nerve cells in the brain's…
Essential Tremor Symptoms: Recognizing the Signs
Essential Tremor Symptoms: Recognizing the Signs Essential tremor is a type of movement disorder.…
Giant Cell Arteritis Treatment: What to Expect
If you've been diagnosed with giant cell arteritis (GCA), it's normal to feel worried. This type of…
What is Giant Cell Arteritis? An In-Depth Look
Giant cell arteritis (GCA) is the most common vasculitis in adults. It causes inflammation of…
Identifying Epilepsy Symptoms: What You Need to Know
Epilepsy is a disorder that causes seizures. Seizures are bursts of electrical activity in the…
What is Epilepsy? Understanding This Neurological Disorder
Epilepsy is the fourth most common neurological disorder in the world. It affects around 3 million…
Effective Treatments for Gait Disorders: Approaches and Therapies
Have you ever felt unsteady while walking or seen an older adult struggle to move confidently? That…
Gait Disorder Causes: An Informative Guide
Gait is how you walk, and it's key to moving smoothly and staying balanced. But some injuries or…
What is a Gait Disorder? A Comprehensive Overview
Have you seen someone walk oddly, like dragging their toes or taking big steps? This shows they…
Define Encephalopathy Symptoms: Early Signs and Indicators
Encephalopathy is a change in how the brain works. It can cause various mental and physical…
Exploring Encephalopathy Causes: A Comprehensive Guide
Encephalopathy is a neurological disorder that affects brain function. It can greatly impact health…
Understanding Encephalitis Symptoms: What to Look For
Encephalitis is a serious illness that causes the brain to swell. This swelling can happen because…
Duchenne Muscular Dystrophy Treatment Options
Duchenne muscular dystrophy (DMD) is a rare and serious genetic condition. It causes progressive…
What Is Duchenne Muscular Dystrophy?
Duchenne muscular dystrophy (DMD) is not common. It affects mostly young boys. They face issues…
Hepatic Encephalopathy Treatments: Options and Approaches
This illness is a serious complication of chronic liver disease. It can cause changes in mental…
4 Types Of Guillain Barre syndrome A Classification Guide
Guillain-Barré syndrome or GBS is a rare disorder linked with infections. It happens when the…
Treatment For Diabetic Neuropathy
Diabetic neuropathy is a severe problem of diabetes. It can lead to nerve damage. This causes pain,…
Understanding the Causes of Hereditary Spastic Paraplegia
Have you or someone you love been diagnosed with hereditary spastic paraplegia (HSP)? If so, you're…
Recognizing Ischemic Stroke Symptoms: What to Look For
Ischemic strokes are a major health issue, making up 85% of all strokes and it happens when a blood…
Aneurysmal Subarachnoid Hemorrhage (SAH)
A Aneurysmal Subarachnoid Hemorrhage is a medical emergency. It happens when a weak area in a brain…
Mysteries of Alzheimer's and Dementia
If you have ever walked into a room and forgotten why or watched a loved one slowly forget the…
Dandy Walker Syndrome Symptoms
Welcome to the first section of our article on Dandy Walker Syndrome. In this section, I will…
Treatments For Dementia
As someone who has witnessed the impact of dementia on my loved ones, I understand the importance…
CRPS Treatment: Physical Therapy Solutions
Hello! I'm glad you've found your way to this article on CRPS treatment and physical therapy's role…
Understanding Complex Regional Pain Syndrome Type 1
CRPS type 1 is a chronic pain condition that often occurs after an injury or medical event like…
Understanding Spastic Quadriplegic Cerebral Palsy
Spastic quadriplegic cerebral palsy affects both the arms and legs, as well as the trunk and face,…
What Causes Dementia?
Welcome to our article where we will explore the causes of dementia and the underlying factors…
Diabetic Neuropathy Symptoms
Welcome to our blog post where we will discuss the symptoms associated with diabetic neuropathy, a…
Symptoms Of Dementia
Understanding the symptoms of dementia early on can make a big difference in managing the condition…
Brachial Plexus Injury Newborn Treatment Options
Welcome to our article on brachial plexus injury newborn treatment. If your baby has been diagnosed…
Brachial Plexus Birth Injury Recovery Insights
What if your newborn couldn’t move their arm right after birth? For any parent, that’s a terrifying…
Effective Brachial Plexus Injury Treatment Options
In this article, we'll explore the comprehensive treatment approaches, both surgical and…
Recognizing Early Signs of Cervical Dystonia
Cervical dystonia, also known as spasmodic torticollis, is a rare neurological disorder that is…
Cerebral Palsy Diagnosis - Key Facts
Are you familiar with cerebral palsy? Do you know the key facts about its diagnosis? If not, don't…
4 Tips For Diabetic Neuropathy Self-care
Are you feeling a constant burning or tingling in your feet? Do your toes feel numb at night or…
What Is Dandy Walker Syndrome ?
Lets discuss a rare condition called Dandy Walker Syndrome. It is a brain malformation that affects…
Relax your mind in Summer | Mindful Practices For Summer Relaxation
Unwind and Embrace Summer Serenity: Your Guide to Mindful Relaxation. As the sun beckons and the…
How To Balance Productivity And Rest | Work Life Balance
Rest and productivity are deeply linked. When you chase work alone and skip rest, both quality and…
How To Relax When You Are Feeling Stressed | Stress Management
Feeling stressed can take a toll on your physical, mental, and emotional well-being. However, there…
Understanding CRPS: Key Stages Explained
Complex regional pain syndrome (CRPS) is a neuropathic pain disorder that affects individuals…
Trigeminal Nerve Cluster Headache: Causes and Relief
Did you know that cluster headaches are so painful they’re often called “suicide headaches”? This…
Understanding Traumatic Encephalopathy Syndrome
Welcome to our article on Traumatic Encephalopathy Syndrome, a rare brain disorder that is caused…
Cerebral Traumatic Encephalopathy: A Guide
Cerebral traumatic encephalopathy (CTE) is characterized by the progressive buildup of a protein…
Chronic Fatigue Syndrome Cure: New Insights
Welcome to our article on chronic fatigue syndrome (CFS) and the latest advancements in its…
Complex Regional Pain Syndrome Diagnosis Guide
Diagnosing CRPS is a complex process that relies on a thorough physical examination and evaluation…
Understanding Ataxic Cerebral Palsy - Key Facts
In this article, we will provide you with key facts about ataxic cerebral palsy which affects…
Charcot Marie Tooth Disease Diagnosis Guide
Welcome to our comprehensive guide on the diagnosis of Charcot Marie Tooth disease (CMT). If you or…
Innovative Brain Cancer Treatment Options
As someone who has witnessed the impact of brain cancer on individuals and families, I am thrilled…
Understanding Different Types of Brain Tumors: A Comprehensive Guide
Welcome to our comprehensive guide on types of brain tumors! In this article, I will provide…
Relief for CRPS: Sympathetic Nerve Block Info
Lets provide you with information on an effective treatment option for chronic regional pain…
CRPS Alternative Treatments: Hopeful Options
Does your pain feel like a fire that won’t go out? Wondering what if the pain never stops? If you…
Understanding Types of Brain Cancer Explained
Hello, India! Today, I want to talk to you about an important topic that affects many people: brain…
5 Effective Methods for Brain Tumor Treatment without Surgery
Brain tumor treatment without surgery is no longer a distant hope. Medical science has evolved to…
Understanding Chronic Traumatic Encephalopathy Symptoms
In the first section, we will explore the symptoms of this brain disorder that is caused by…
Cervical Dystonia Symptoms: Early Signs and Relief
If you're experiencing abnormal neck movements or pain, you may be dealing with cervical dystonia,…
Understanding the Cause of Cerebral Palsy
There are various factors that can contribute to the development of cerebral palsy. These include…
Charcot Marie Tooth Life Expectancy Insights
Welcome to our article on Charcot Marie Tooth (CMT) disease and its impact on life expectancy. CMT…
Understanding Autism Spectrum Disorder Essentials
Autism spectrum disorder is a complex condition that encompasses a wide range of disorders with a…
Ataxia Symptoms in Adults: Spot the Signs
Are you experiencing difficulties with coordination, balance, or muscle control? It's essential to…
What Is Arnold Chiari Malformation?
Welcome to our article series on Arnold Chiari Malformation, a group of deformities affecting the…
Cerebellar Ataxia Treatment Options Explored
Welcome to our article on cerebellar ataxia treatment options. If you or someone you know is living…
Understanding Chronic Fatigue Syndrome
Chronic fatigue syndrome, also known as myalgic encephalomyelitis (ME) or systemic exertion…
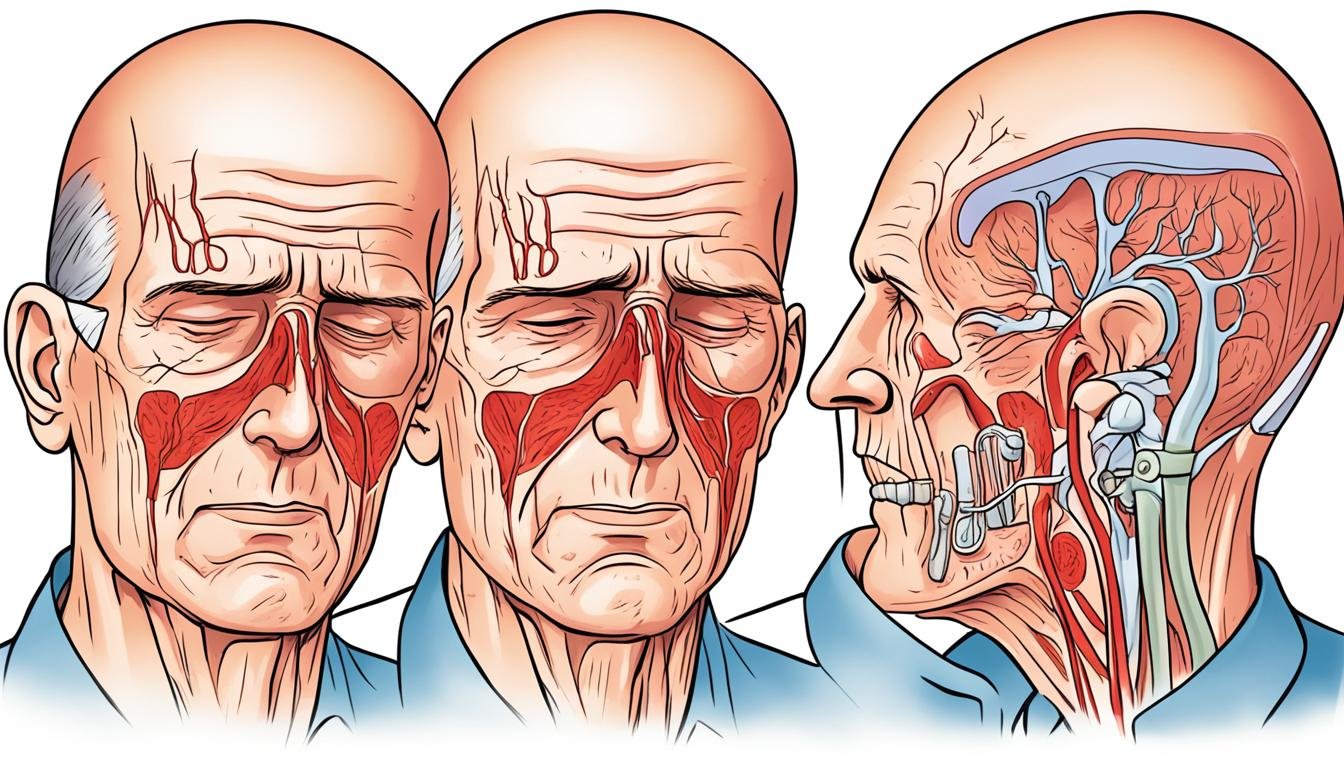
Effective Bell's Palsy Treatment Options
Bell's palsy is a condition that can cause sudden paralysis of the facial muscles, resulting in…
How to deal with dementia patients
Caring for Loved Ones with Dementia: A simple guide for people with Alzheimer's Understanding…
Understanding Ataxia Telangiectasia Fundamentals
Welcome to our comprehensive guide on Ataxia Telangiectasia, a rare genetic disorder that affects…
Effective Ataxia Management: Physical Therapy for Ataxia
If you or a loved one is living with ataxia, a neurological disorder that affects coordination and…
Ataxia New Treatment: Groundbreaking Advances
Are you or someone you know struggling with ataxia, a neurological condition that affects…
Exploring Friedreich's Ataxia Treatment Options
If you or a loved one is living with Friedreich's ataxia, understanding the available treatment…
Understanding Cerebellar Ataxia Symptoms
Do you experience balance and coordination issues? Are you struggling with muscle control and…
Charcot Marie Tooth Disorder: Symptoms & Treatment
Welcome to our article on Charcot Marie Tooth disorder. If you or a loved one have been diagnosed…
CTE Treatment Options Explored - Stay Informed
Have you or someone you love been affected by repeated head injuries? Have memory problems, mood…
Unveiling Chronic Traumatic Encephalopathy Causes
Have you ever wondered why some athletes or soldiers suddenly start behaving differently years…
Friedreich's Ataxia Life Expectancy Insights
What if one diagnosis could change the course of a child’s life forever? That's the case for…