Understanding Brachial Plexus Injury - Causes and Care
Brachial plexus injury is a condition that affects the network of nerves in your shoulder, arm, and hand, known as the brachial plexus. This injury occurs when these nerves are damaged or torn, resulting in various symptoms and complications. It is essential to have a thorough understanding of the causes, symptoms, and proper care for managing this complex condition effectively.
There are several possible causes of brachial plexus injury, including trauma, birth complications, inflammation, tumors, and accidents. The severity of the injury can range from minor damage to complete paralysis of the arm. Seeking appropriate care and treatment is crucial for better management and improving outcomes.
Throughout this article, we will explore the anatomy and function of the brachial plexus, common symptoms, risk factors, diagnosis, treatment options, prevention methods, and rehabilitation for brachial plexus injury. We will also touch upon the specific challenges faced by infants with neonatal brachial plexus palsy (NBPP) and the latest advances in treatment options.
Key Takeaways:
- Brachial plexus injury occurs when the nerves in the network known as the brachial plexus are damaged or torn.
- The injury can be caused by trauma, birth complications, inflammation, tumors, and accidents.
- Common symptoms include weakness or inability to use certain muscles, complete lack of movement and feeling in the affected area, severe pain, and numbness.
- Early diagnosis, appropriate care, and rehabilitation are essential for managing brachial plexus injury effectively.
- Prevention methods include range-of-motion exercises, protective padding, and promoting healthy development in infants at risk.
Brachial Plexus Anatomy and Function
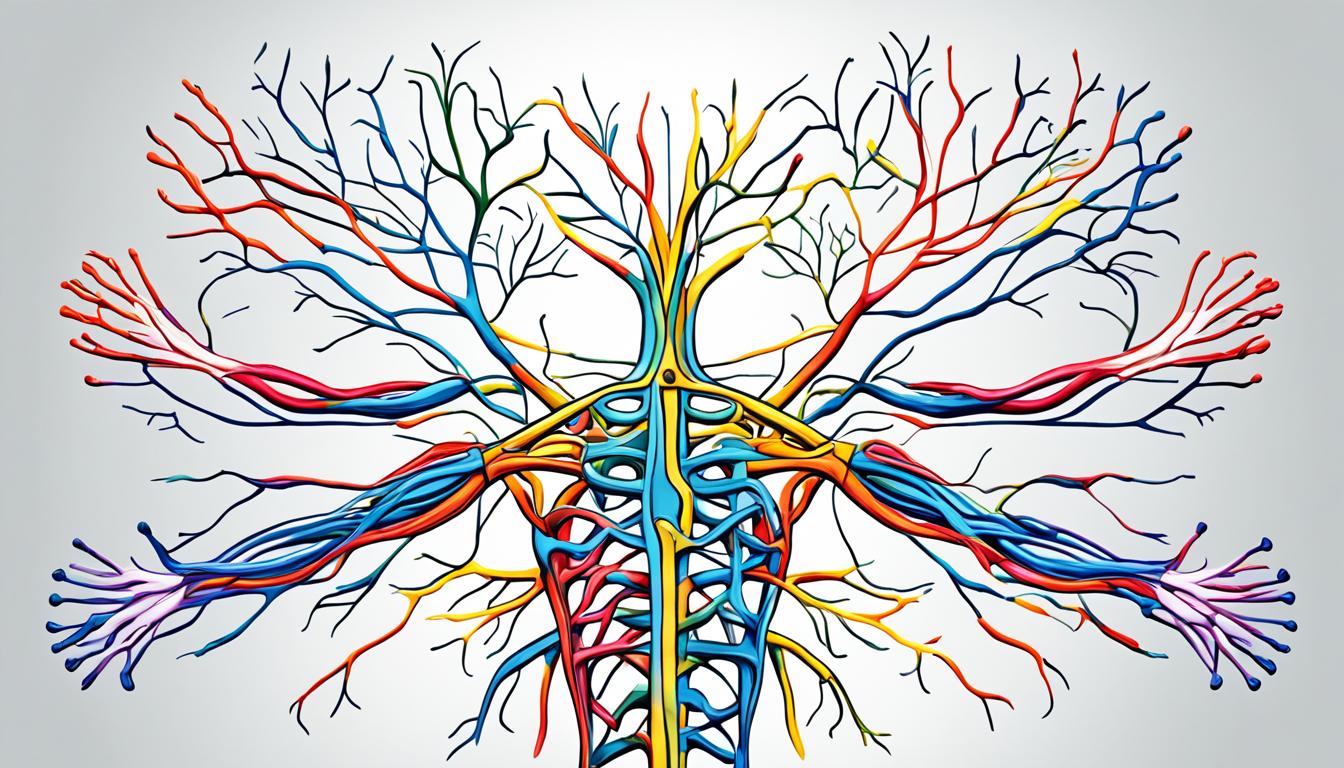
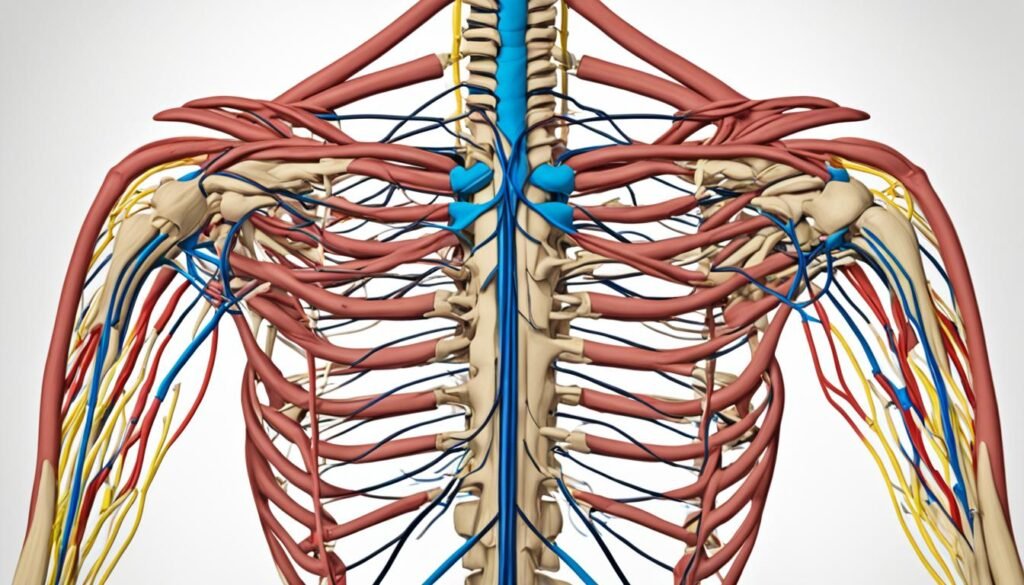
The brachial plexus is a complex network of nerves that originates in the neck and extends into the shoulder, arm, and hand. It plays a crucial role in controlling movement and sensation in the upper limb. Understanding the brachial plexus anatomy and its function is vital in comprehending the complexities of brachial plexus injury and its impact on daily life.
The brachial plexus consists of five major nerves:
- Musculocutaneous nerve
- Axillary nerve
- Median nerve
- Radial nerve
- Ulnar nerve
Each nerve has its own specific function:
| Nerve | Function |
|---|---|
| Musculocutaneous nerve | Controls the muscles involved in flexing the forearm and sensation in the lateral aspect of the forearm |
| Axillary nerve | Innervates the deltoid and teres minor muscles, which are important for shoulder movement and sensation in the shoulder joint |
| Median nerve | Responsible for controlling the muscles involved in finger flexion, as well as sensation in the thumb, index, middle, and half of the ring finger |
| Radial nerve | Controls the muscles responsible for extending the forearm, wrist, and fingers |
| Ulnar nerve | Innervates the muscles involved in finger adduction and controls sensation in the little finger and half of the ring finger |
These nerves work together to transmit signals from the spinal cord to the muscles, allowing us to perform intricate movements in the arm and hand. Additionally, they provide sensory information, enabling us to feel pain, temperature, and touch in these areas.
Common Symptoms of Brachial Plexus Injury
A brachial plexus injury can result in various symptoms, which can range in severity depending on the extent and location of the damage. Recognizing these symptoms is crucial in diagnosing and treating the injury effectively. Below are some common symptoms associated with brachial plexus injury:
- Weakness or inability to use certain muscles: Individuals may experience weakness or an inability to move specific muscles in the hand, arm, or shoulder due to nerve damage in the brachial plexus.
- Complete lack of movement and feeling: In some cases, a brachial plexus injury can lead to a complete loss of movement and sensation in the affected area.
- Severe pain: Pain is a prominent symptom of a brachial plexus injury and can range from mild discomfort to intense, debilitating pain.
- Numbness: Numbness or a tingling sensation in the affected arm or hand may indicate nerve damage in the brachial plexus.
- Recurrent burners or stingers: Some individuals may experience episodes of burning pain or electric shock-like sensations traveling down the arm, known as burners or stingers.
If you experience any of these symptoms, it is important to seek immediate medical attention. Brachial plexus injuries can potentially result in long-term complications such as arm paralysis and disability if left untreated.

Causes and Risk Factors of Brachial Plexus Injury
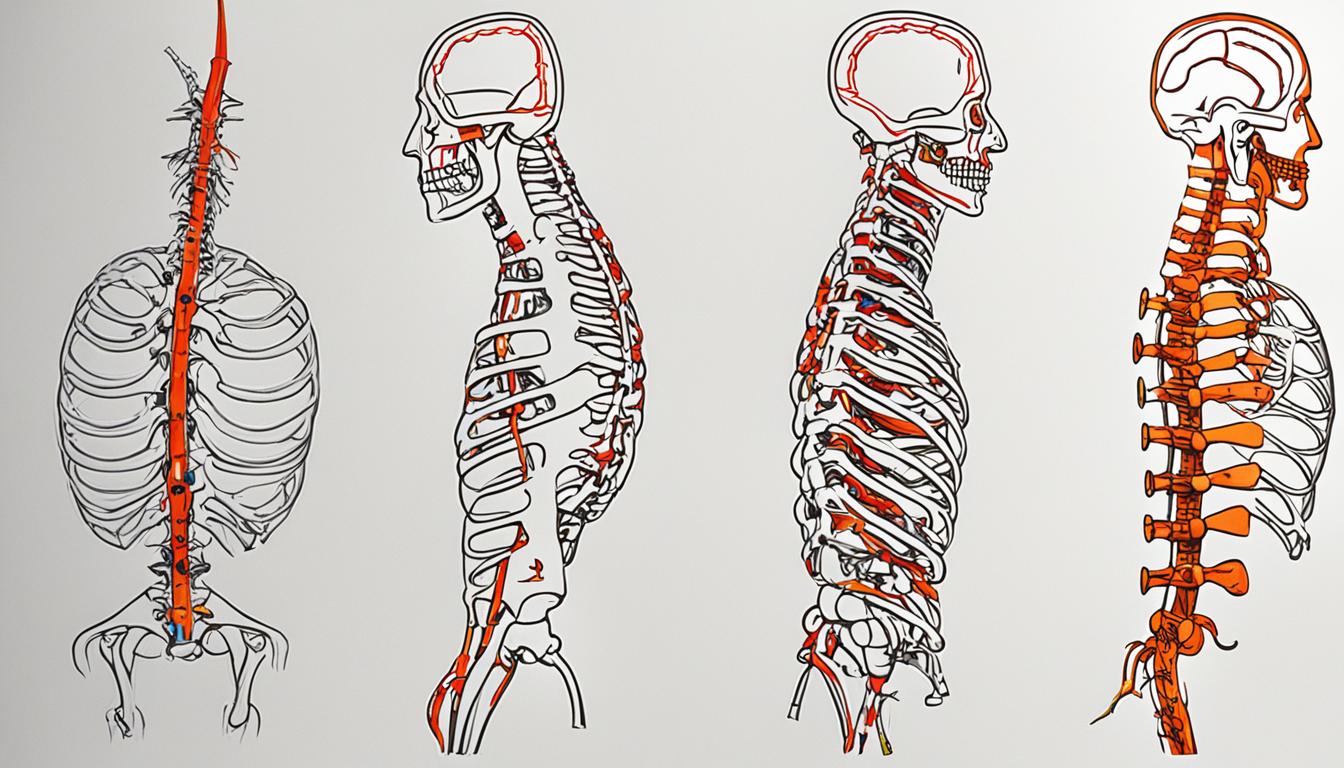
Brachial plexus injuries can occur due to various factors, including trauma, birth complications, tumors, and cancer treatments. The upper nerves of the brachial plexus are more likely to be injured when the shoulder is forced down while the neck stretches up, whereas the lower nerves are more likely to be injured when the arm is forced above the head.
Common causes of brachial plexus injury include:
- Participating in contact sports like football
- Being involved in high-speed motor-vehicle accidents
- Trauma from accidents or falls
- Tumors
- Cancer treatments
These activities and situations can increase the risk of brachial plexus injury as they put pressure or strain on the nerves.
Risk factors for brachial plexus injury:
- High birth weight: Babies with higher birth weights are more prone to brachial plexus injuries during delivery.
- Breech presentation during birth: When a baby is born feet-first or buttocks-first, it increases the likelihood of a brachial plexus injury.
- Prolonged labor: Long and difficult labors can increase the risk of brachial plexus injuries in newborns.
It is important to be aware of these causes and risk factors to take necessary precautions and seek appropriate medical care to prevent or manage brachial plexus injuries.
Diagnosis and Treatment of Brachial Plexus Injury
Diagnosing a brachial plexus injury involves a comprehensive evaluation to determine the extent of nerve damage. The diagnostic process typically includes:
- A physical examination: The doctor will assess your range of motion, muscle strength, and sensory function in the affected arm and hand. They may also test specific movements and reflexes.
- Sensation and function tests: These involve evaluating your ability to feel touch, temperature, and pain in the affected area. Additionally, the doctor may assess your grip strength and finger dexterity.
- Diagnostic imaging tests: X-rays, Magnetic Resonance Imaging (MRI), or Computerized Tomography (CT) scans may be conducted to obtain detailed images of the brachial plexus and identify any structural abnormalities or nerve damage.
The treatment of brachial plexus injuries varies depending on the severity and type of injury. Mild injuries may heal on their own with conservative methods, including:
- Physical therapy: Specific exercises and therapies aimed at improving range of motion, strength, and function in the affected arm and hand.
- Occupational therapy: Techniques to enhance your ability to perform daily activities and regain independence.
However, more severe brachial plexus injuries often require surgical intervention to repair or reconstruct the damaged nerves. Surgical treatments may include:
- Nerve grafting: A procedure in which a healthy nerve from another part of your body is used to bridge the gap and restore continuity in the damaged brachial plexus.
- Nerve transfers: The transfer of functional nerves from less important areas to restore function in the affected arm.
Early diagnosis and appropriate treatment are crucial for achieving the best possible outcomes and restoring function in the arm and hand. Seeking prompt medical attention and consulting with a specialist experienced in brachial plexus injuries can significantly improve your chances of a successful recovery.
| Treatment Options | Severity | Description |
|---|---|---|
| Physical Therapy | Mild to moderate | Involves exercises and techniques to improve range of motion, strength, and function in the affected arm and hand. |
| Occupational Therapy | Mild to moderate | Focuses on enhancing your ability to perform daily activities and regain independence. |
| Nerve Grafting | Severe | Transplanting a healthy nerve from another part of the body to reconstruct the damaged brachial plexus. |
| Nerve Transfers | Severe | Utilizing functional nerves from less critical areas to restore function in the affected arm. |
Early intervention and a comprehensive treatment plan tailored to your specific needs are essential in maximizing recovery and improving quality of life.

Complications of Brachial Plexus Injury
Brachial plexus injuries can lead to various complications, especially if left untreated or if the injury is severe. These complications can include stiffness in the joints, chronic pain, numbness, muscle atrophy, and permanent disability. Stiff joints can make movement difficult, and lack of feeling in the affected area can lead to accidental burns or injuries. Muscle atrophy can occur due to lack of use during the healing process, and severe injuries may result in permanent muscle weakness or paralysis. Managing these complications may require ongoing physical therapy, pain management strategies, and lifestyle adjustments.
Stiffness in the joints is a common complication of brachial plexus injury. When the nerves are damaged, the affected muscles may become tight and rigid, leading to limited range of motion in the joints. This stiffness can significantly impair daily activities and make it challenging to perform tasks that require precise movement. Physical therapy can help improve joint flexibility and restore functional mobility.
Chronic pain is another complication that individuals with brachial plexus injuries may experience. The damaged nerves can send continuous pain signals to the brain, resulting in persistent discomfort. This pain can significantly impact quality of life and hinder the ability to carry out daily activities. Pain management strategies, such as medication, physical therapy, and alternative therapies like acupuncture, can help alleviate chronic pain and improve overall well-being.
Numbness is a common sensation experienced in the affected area of a brachial plexus injury. The damaged nerves can disrupt the transmission of sensory signals, leading to a loss of feeling in the arm, shoulder, or hand. This lack of sensation can increase the risk of accidental burns, cuts, or injuries, as individuals may not be aware of potential dangers. Proper precautions, such as avoiding extreme temperatures and using protective measures, can help mitigate the risk of accidental injuries.
Muscle atrophy, or the wasting away of muscle tissue, is a potential complication of brachial plexus injury. When the affected arm is immobilized or not used during the healing process, the muscles can weaken and shrink in size. This can result in reduced muscle strength and functionality. Physical therapy and targeted exercises are essential in preventing or minimizing muscle atrophy and promoting muscle strength and endurance.
In severe cases, brachial plexus injuries can lead to permanent disability. If the nerves are severely damaged or torn, it may not be possible to fully restore function and sensation in the affected area. This can result in long-term muscle weakness or paralysis, significantly impacting an individual's ability to perform daily activities and participate in meaningful work or hobbies. Adaptive devices and assistive technologies, along with comprehensive rehabilitation programs, can help individuals with permanent disability regain independence and improve their overall quality of life.
Managing these complications requires a multidisciplinary approach that includes ongoing medical care, physical therapy, pain management strategies, and lifestyle modifications. It is crucial for individuals with brachial plexus injuries to work closely with healthcare professionals to develop personalized treatment plans and to stay vigilant in addressing any new or worsening symptoms. With proper care and management, individuals with brachial plexus injuries can minimize the impact of complications and optimize their recovery.

Prevention of Brachial Plexus Injury
While it may not always be possible to prevent brachial plexus injuries, there are measures that can be taken to reduce the risk and prevent complications. By incorporating a few simple strategies into your daily routine, you can help safeguard your brachial plexus and maintain optimal arm and hand function.
Range-of-Motion Exercises and Physical Therapy
Engaging in regular range-of-motion exercises and physical therapy can help prevent joint stiffness and maintain muscle strength, especially if you experience temporary loss of hand or arm function. These exercises aim to keep your joints flexible and improve circulation, promoting overall joint health and preventing the development of stiffness.
Range-of-motion exercises can include:
- Gentle stretching to improve flexibility
- Rotations and circular motions to maintain joint mobility
- Resistance exercises to strengthen muscles
Padding for Added Protection
If you participate in contact sports like football, wearing specific protective padding can provide an extra layer of safety for your brachial plexus. This padding is designed to cushion the area and reduce the risk of injury in case of impact or direct blows. By wearing appropriate padding, you can minimize the chances of sustaining a brachial plexus injury while actively participating in sports.
Preventing Brachial Plexus Injury in Infants
For infants who may be at risk of brachial plexus injury during birth, there are preventive measures that can be taken as well. Encouraging joint movement and maintaining muscle strength through exercises can be beneficial in preventing long-term stiffness and promoting healthy development. Consult with healthcare professionals or pediatric specialists for guidance on safe and effective exercises suitable for infants.

By implementing these preventive measures, you can minimize the risk of brachial plexus injury and protect the intricate network of nerves responsible for arm and hand function. Remember, prevention is always better than treatment when it comes to ensuring the health and well-being of your brachial plexus.
Care and Rehabilitation for Brachial Plexus Injury
Effective care and rehabilitation are essential for managing brachial plexus injuries. Treatment plans often involve a combination of surgical intervention, physical therapy, occupational therapy, pain management strategies, and the use of assistive devices.
Physical therapy is a critical component of the treatment plan. It aims to improve range of motion, strengthen muscles, and enhance functional abilities. Through targeted exercises and techniques, physical therapy helps individuals regain mobility and regain control over their affected arm and hand.
Occupational therapy focuses on improving daily activities and tasks such as dressing, eating, and personal care. Occupational therapists work with individuals to develop strategies and adaptive techniques that enable them to perform these activities with increased independence and efficiency.
Pain management strategies may be incorporated into the treatment plan to alleviate discomfort associated with brachial plexus injuries. This may include the use of medication, acupuncture, or other alternative therapies, depending on the individual's needs and preferences.
Assistive devices, such as braces or splints, may also be recommended to support the affected limb, promote proper alignment, and aid in functional recovery.
Rehabilitation for brachial plexus injury aims to restore function and promote independence in daily life. With the help of a comprehensive treatment plan and the guidance of healthcare professionals, individuals can achieve significant improvements and regain control over their lives.
Rehabilitation Goals for Brachial Plexus Injury
Rehabilitation programs for brachial plexus injury typically focus on achieving the following goals:
- Restoring range of motion and strength in the affected arm and hand
- Improving coordination and motor control
- Enhancing functional abilities for daily activities
- Promoting pain management and reducing discomfort
- Fostering independence and self-care
These goals are achieved through a combination of exercises, therapeutic interventions, and patient education. Physical therapists and occupational therapists work closely with individuals to develop customized treatment plans that address their unique needs and maximize their potential for recovery.
Rehabilitation for brachial plexus injury is a holistic process that requires dedication, patience, and active participation from the individual. It may take time, but with the guidance of healthcare professionals and a supportive environment, individuals can overcome the challenges of brachial plexus injury and regain their independence and functionality.
| Treatment Approaches | Benefits |
|---|---|
| Physical Therapy |
|
| Occupational Therapy |
|
| Pain Management |
|
| Assistive Devices |
|
Brachial Plexus Injury in Infants - Neonatal Brachial Plexus Palsy (NBPP)
Brachial plexus injuries can also affect infants during childbirth, resulting in Neonatal Brachial Plexus Palsy (NBPP). These injuries can occur due to complications such as shoulder dystocia or breech presentation. NBPP is often characterized by two specific conditions: Erb's palsy and Klumpke's palsy, which affect different areas of the brachial plexus.
Erb's palsy is the most common form of NBPP and typically affects the upper brachial plexus nerves. It can result in weakness or loss of motion in the affected arm. On the other hand, Klumpke's palsy affects the lower brachial plexus nerves and can cause weakness or paralysis in the hand and forearm.
Early diagnosis and intervention are crucial in managing NBPP effectively. Medical professionals will assess the severity of the injury and determine the appropriate treatment options. In many cases, physical therapy and occupational therapy may be recommended to improve muscle strength, range of motion, and overall function of the affected arm.
In some instances, surgical intervention may be necessary to repair or reconstruct the damaged nerves. The goal of treatment is to promote healing, restore function, and help the infant achieve full or near-full recovery.

Research and Advances in Brachial Plexus Injury Treatment
Ongoing research and advances in medical technology are paving the way for improved treatment options for brachial plexus injury. Scientists and healthcare professionals are constantly striving to develop innovative approaches that can restore function and enhance outcomes for individuals with this condition.
One significant area of advancement is in surgical techniques. Nerve grafting and nerve transfers have shown promising results in helping to restore function and improve overall outcomes for patients with brachial plexus injuries. These procedures involve transferring nerves from healthy areas of the body or using grafts to bridge the gap between damaged nerves, facilitating nerve regeneration and promoting recovery.
Another promising avenue of research is regenerative therapies, specifically stem cell therapy. Stem cells have the potential to differentiate and develop into various cell types, making them a viable candidate for repairing damaged nerve tissue in the brachial plexus. While still in the experimental stage, initial studies have shown encouraging results, and researchers continue to explore the potential of stem cell therapy in treating brachial plexus injuries.
In addition to surgical and regenerative advances, there have been significant strides in rehabilitation strategies, pain management techniques, and assistive devices. Physical therapy and occupational therapy play crucial roles in helping individuals with brachial plexus injuries regain independence and improve their quality of life. These therapies focus on strengthening muscles, improving range of motion, and developing compensatory strategies to maximize function in daily activities.
Pain management strategies have also evolved, offering individuals with brachial plexus injuries various options to manage their pain effectively. This can include medication, physical modalities, acupuncture, and other alternative therapies tailored to each individual's needs. The goal is to provide relief and improve overall well-being.
Assistive devices, such as splints and braces, can aid in supporting weakened or paralyzed muscles and help individuals maintain functionality. They are designed to promote independence and compensate for any limitations caused by the injury.
Overall, ongoing research and development in the field of brachial plexus injury continue to bring forth exciting advancements in treatment options. From surgical innovations to regenerative therapies, rehabilitation strategies, pain management techniques, and assistive devices, these advances provide hope for improved care and recovery for individuals affected by brachial plexus injury.
Conclusion
Brachial plexus injury is a complex condition that can have significant implications for your physical function and quality of life. Understanding the causes, symptoms, diagnosis, and treatment options is crucial in managing this condition effectively. Prompt medical attention, appropriate care, and rehabilitation are key factors in achieving optimal recovery and minimizing complications.
To improve your outcomes and live a fulfilling life with enhanced functionality and independence, it is important to follow these care tips:
- Seek immediate medical attention if you experience any symptoms or suspect a brachial plexus injury.
- Follow the recommended treatment plan, which may include physical therapy, occupational therapy, pain management strategies, and assistive devices.
- Stay informed about advancements in treatment options and discuss them with your healthcare provider to explore all available options.
- Be proactive in managing your condition by adhering to post-treatment care instructions and attending regular check-ups.
- Engage in range-of-motion exercises and other recommended therapies to maintain joint mobility and muscle strength.
- Take necessary precautions in activities or sports that pose a risk of injury to the brachial plexus.
By following these care tips, seeking necessary treatment, and staying informed about advancements in treatment options, you can improve your outcomes and live a fulfilling life despite the challenges posed by a brachial plexus injury.
FAQ
What is brachial plexus injury?
Brachial plexus injury is a condition that occurs when the nerves in the brachial plexus network are damaged or torn.
What are the causes of brachial plexus injury?
Brachial plexus injuries can be caused by trauma, birth complications, inflammation, tumors, and accidents.
What are the common symptoms of brachial plexus injury?
Common symptoms include weakness or inability to use certain muscles, arm paralysis, severe pain, and numbness.
What are the risk factors for brachial plexus injury?
Common risk factors include trauma from accidents or falls, difficult births, contact sports, and certain cancer treatments.
How is brachial plexus injury diagnosed and treated?
Diagnosis usually involves physical examination and imaging tests. Treatment options range from nonsurgical treatments to surgical intervention.
What are the complications of brachial plexus injury?
Complications can include stiffness, chronic pain, muscle atrophy, numbness, and permanent disability.
Can brachial plexus injury be prevented?
While not always preventable, measures such as range-of-motion exercises and wearing protective padding can help reduce the risk.
How is brachial plexus injury cared for and rehabilitated?
Treatment plans may include surgery, physical therapy, occupational therapy, pain management, and assistive devices.
What is Neonatal Brachial Plexus Palsy (NBPP)?
NBPP refers to brachial plexus injuries in infants, often caused by birth complications, and may require physical therapy or surgery for treatment.
What are the latest advancements in brachial plexus injury treatment?
New surgical techniques, regenerative therapies, and advancements in rehabilitation strategies offer hope for improved outcomes.
Source Links
- https://my.clevelandclinic.org/health/diseases/22822-brachial-plexus-injury
- https://www.mayoclinic.org/diseases-conditions/brachial-plexus-injury/symptoms-causes/syc-20350235
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/brachial-plexus-injuries
Effective Cerebral Palsy Treatment Options
If your child has been diagnosed with cerebral palsy, it's important to understand the available treatment options. Cerebral palsy is a condition that affects muscle control and movement due to brain damage, but with the right treatment approach, your child can lead a fulfilling and independent life.
Diagnosing cerebral palsy involves a series of tests, including brain scans, electroencephalogram (EEG), and laboratory tests. These tests help healthcare professionals determine the specific type of cerebral palsy and develop a tailored treatment plan based on your child's symptoms and needs.
Treatment options for cerebral palsy include medications, therapies, surgical procedures, and other interventions as necessary. Medications such as muscle relaxants can help manage symptoms like muscle stiffness, while therapies like physical, occupational, speech, and recreational therapy aim to improve muscle strength, balance, and mobility. In some cases, surgical procedures may be recommended to correct muscle tissue shortening or address bone and joint abnormalities.
Alternative therapies like acupuncture, aquatic therapy, hippotherapy, and music therapy may also be beneficial alongside traditional treatment methods. Additionally, finding a supportive network and seeking coping strategies for both you and your child can greatly enhance their well-being and quality of life.
Key Takeaways:
- Diagnosis of cerebral palsy involves tests such as brain scans, EEG, and laboratory tests.
- Treatment options for cerebral palsy include medications, therapies, and surgical procedures.
- Physical therapy plays a vital role in improving muscle strength, balance, and mobility.
- Medications like muscle relaxants and Botox injections can help manage symptoms.
- Surgical procedures can correct muscle tissue shortening and address severe symptoms.
Diagnosis of Cerebral Palsy
Diagnosing cerebral palsy involves a thorough evaluation of the child's symptoms, medical history, physical exams, and growth and development. Healthcare professionals use various tests to aid in the diagnosis.
Brain Imaging Tests
Brain scans such as Magnetic Resonance Imaging (MRI) and Cranial Ultrasound are commonly used to identify areas of brain damage or irregular development that may be contributing to cerebral palsy. These imaging tests provide valuable insights into the structural abnormalities of the brain.
Electroencephalogram (EEG)
An EEG is another important diagnostic tool that evaluates seizure activity in individuals with cerebral palsy. This non-invasive test measures the electrical activity of the brain and helps healthcare professionals understand the presence and severity of seizures.
Laboratory Tests
Laboratory tests are used to screen for genetic or metabolic conditions that could cause or contribute to cerebral palsy. These tests can provide valuable information regarding the underlying causes of the condition. Additionally, various other tests may be conducted to assess vision, hearing, speech, intellect, movement, and development, helping healthcare professionals gain a comprehensive understanding of the individual's condition.
By combining the information gathered from these diagnostic tests with the clinical evaluation, healthcare professionals can make an accurate cerebral palsy diagnosis and develop an appropriate treatment plan tailored to the individual's specific needs.

| Diagnostic Tests | Purpose |
|---|---|
| Brain Imaging Tests (MRI, Cranial Ultrasound) | Identify areas of brain damage or irregular development |
| Electroencephalogram (EEG) | Evaluate seizure activity |
| Laboratory Tests | Screen for genetic or metabolic conditions, and assess various aspects of the individual's health |
Types of Cerebral Palsy
Cerebral palsy encompasses different types based on the main movement condition that's present. Understanding these types can provide insight into the specific challenges individuals may face. The main types include:
- Spastic Cerebral Palsy: This is the most common type of cerebral palsy, accounting for approximately 70-80% of cases. It is characterized by stiff muscles and exaggerated reflexes. Individuals with spastic cerebral palsy may experience difficulties with movement and coordination.
- Dyskinetic Cerebral Palsy: Dyskinetic cerebral palsy, also known as athetoid cerebral palsy, affects approximately 10-20% of individuals with cerebral palsy. It is characterized by involuntary and uncontrolled movements, making it challenging to control voluntary muscles. People with dyskinetic cerebral palsy may have difficulty with tasks requiring precise movements, such as writing or eating.
- Ataxic Cerebral Palsy: Ataxic cerebral palsy is a less common form, accounting for around 5-10% of cases. It primarily affects balance and coordination. Individuals with ataxic cerebral palsy may exhibit shaky or unsteady movements and have difficulties with tasks that require precise control, such as buttoning clothes or tying shoes.
In some cases, individuals may have a combination of movement conditions, making it important to tailor treatment plans accordingly. Determining the type and severity of cerebral palsy can be assessed using rating scale tools like the Gross Motor Function Classification System, which evaluates function, mobility, posture, and balance.

| Type of Cerebral Palsy | Main Characteristics |
|---|---|
| Spastic Cerebral Palsy | Stiff muscles, exaggerated reflexes |
| Dyskinetic Cerebral Palsy | Involuntary and uncontrolled movements |
| Ataxic Cerebral Palsy | Trouble with balance and coordination |
Care for Cerebral Palsy
Children and adults with cerebral palsy may require lifelong care with a health care team comprised of various specialists. Treatment plans are tailored to address each individual's unique symptoms and needs. Early intervention plays a crucial role in improving outcomes for individuals with cerebral palsy. Treatment options can include a combination of:
- Medications to manage symptoms
- Therapies such as physical, occupational, speech, and recreational therapy
- Surgical procedures to address muscle tightness or bone changes
- Other treatments as needed based on the individual's condition
Collaboration with a health care team is essential for comprehensive and effective care. The team may include:
- A pediatrician for primary care
- A physical medicine and rehabilitation specialist to address mobility and function
- A pediatric neurologist to manage neurological aspects
- Therapists such as physical, occupational, and speech therapists for specialized rehabilitation
- Mental health specialists to support emotional well-being
Regular health screenings and ongoing care are important for adults with cerebral palsy to ensure their needs are being met and to address any potential health concerns proactively.
Early Intervention for Cerebral Palsy
Early intervention is crucial in providing the best possible outcomes for individuals with cerebral palsy. It involves identifying and addressing developmental delays or difficulties as early as possible. By initiating treatment and therapy during the early stages of a child's development, it can help minimize the impact of cerebral palsy on their overall functioning.
- Regular screenings to evaluate developmental milestones
- Physical therapy to promote gross motor skills and mobility
- Occupational therapy to develop fine motor skills and enhance independence in everyday activities
- Speech therapy to improve communication skills
These early interventions can significantly improve the child's quality of life and enhance their overall development.
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in the treatment of cerebral palsy, helping individuals improve their muscle strength, balance, and mobility. A physical therapist works closely with children who have cerebral palsy, guiding them through various exercises and activities tailored to their specific needs. These interventions aim to enhance overall function and independence in daily activities such as sitting, walking, and using assistive devices like wheelchairs.
Occupational therapy is another important aspect of rehabilitation for individuals with cerebral palsy. It focuses on improving their ability to perform everyday activities, including dressing, feeding, and school participation. Occupational therapists provide guidance and use specialized techniques and equipment to maximize independence and quality of life.
Speech and language therapy is particularly beneficial for children with cerebral palsy who experience challenges in communication. These sessions are designed to help improve speech clarity, language skills, and swallowing abilities, enabling better social interaction and overall oral health.
In addition to the vital physical, occupational, and speech therapies, recreational therapy offers unique benefits to individuals with cerebral palsy. Engaging in art programs, cultural activities, and sports helps promote physical fitness, social interaction, and emotional well-being. Recreational therapists use adaptive techniques and equipment to ensure everyone can participate and enjoy a wide range of activities.
Orthotic devices, assistive devices, and technologies are often incorporated into the rehabilitation process to improve function and mobility. Orthotics such as braces or splints can help support weak muscles and improve stability. Assistive devices like walkers, crutches, and wheelchairs are utilized to enhance mobility and independence. Advancements in technology, including robotic devices and virtual reality, are also being utilized in rehabilitation to facilitate motor learning and enhance overall outcomes.
Benefits of Physical Therapy and Rehabilitation for Cerebral Palsy:
- Improves muscle strength and control
- Enhances balance and coordination
- Increases mobility and range of motion
- Aids in the development of essential skills like sitting, standing, and walking
- Improves fine motor skills and dexterity
- Enhances speech and communication abilities
- Promotes social interaction and inclusion
- Boosts self-confidence and overall well-being
Rehabilitation is a comprehensive and personalized approach to managing cerebral palsy that aims to optimize functionality and improve an individual's quality of life.

Medications for Cerebral Palsy
When it comes to managing the symptoms of cerebral palsy, medications can play a crucial role. These medications are designed to address specific issues such as muscle stiffness, drooling, and spasticity. By working with a healthcare professional, you can develop a treatment plan that includes the appropriate medications to help improve your child's quality of life.
Muscle Relaxants:
One common type of medication used for cerebral palsy is muscle relaxants. These medications, such as baclofen and diazepam, help to relax stiff and spastic muscles, making movement and daily activities easier. They can be taken orally, injected into affected muscles, or even infused into the spinal cord using a pump.
Botox Injections:
In addition to muscle relaxants, Botox injections can also be used to manage symptoms of cerebral palsy. Botox helps to reduce muscle tightness and can be particularly effective in treating spasticity and drooling. By targeting specific muscles, Botox injections can provide targeted relief.
It's important to note that the use of medications for cerebral palsy should always be discussed with a healthcare professional. They will be able to assess your child's specific needs and determine the most appropriate medications and dosage. Additionally, they can provide guidance on potential benefits and risks associated with the use of these medications.
Surgical Procedures for Cerebral Palsy
In some cases, surgical procedures may be necessary to address severe symptoms of cerebral palsy. These procedures aim to improve mobility and correct muscle tissue abnormalities, bone deformities, and joint issues.
Orthopedic Surgery
Orthopedic surgery is commonly performed to correct muscle tissue shortening, bone or joint abnormalities, and improve overall mobility in individuals with cerebral palsy. This type of surgery may involve lengthening muscles, repositioning tendons, or modifying bone structures to improve alignment and function.
Selective Dorsal Rhizotomy
Selective dorsal rhizotomy is a surgical procedure that involves cutting specific nerves to reduce spastic movements in individuals with cerebral palsy. This procedure aims to selectively decrease muscle stiffness and improve motor function.
Common Surgical Procedures for Cerebral Palsy
| Procedure | Description |
|---|---|
| Orthopedic Surgery | Corrects muscle tissue shortening, bone or joint abnormalities, and improves mobility. |
| Selective Dorsal Rhizotomy | Cuts specific nerves to reduce spastic movements and improve motor function. |
| Muscle Lengthening | Lengthens muscles to increase mobility and improve range of motion. |
| Bone Correction | Corrects bone deformities to improve alignment and function. |
These surgical procedures, including orthopedic surgery and selective dorsal rhizotomy, can play a crucial role in improving the quality of life for individuals with cerebral palsy. However, it's important to carefully assess the benefits and risks of these procedures before proceeding with treatment.

Alternative Therapies for Cerebral Palsy
In addition to traditional treatment options, some children with cerebral palsy may benefit from alternative therapies. Alternative therapies, also known as complementary and alternative medicine, can provide additional support in improving fine motor skills, mobility, and overall well-being for children with cerebral palsy.
Acupuncture
Acupuncture is an alternative therapy that involves the insertion of thin needles into specific points on the body to stimulate natural healing processes. It is believed to help reduce muscle stiffness, promote relaxation, and alleviate pain. While research on the effectiveness of acupuncture for cerebral palsy is still limited, some individuals have reported positive results.
Aquatic Therapy
Aquatic therapy, also known as hydrotherapy, utilizes the properties of water to provide therapeutic benefits. Water buoyancy reduces the impact on joints and muscles, making movements easier and less painful. Aquatic therapy helps improve muscle strength, flexibility, balance, and coordination. It also provides a safe and enjoyable environment for children with cerebral palsy to engage in physical activities.
Hippotherapy
Hippotherapy involves horseback riding as a therapeutic tool. The rhythmic motion of the horse helps stimulate the muscles, improve postural control, balance, and coordination. It also enhances sensory integration and sensory processing, benefiting children with cerebral palsy. Trained therapists guide the child's movements and design specific activities to address individual therapy goals.
Music Therapy
Music therapy utilizes music-based interventions to address physical, emotional, cognitive, and social challenges. In the case of cerebral palsy, music therapy can help improve motor skills, enhance communication abilities, reduce muscle tension, and promote relaxation. The rhythmic elements of music can be utilized to facilitate movement and coordination.
When considering alternative therapies for cerebral palsy, it is important to discuss potential risks and benefits with a healthcare professional. While these therapies may provide additional support and benefits, they should not replace conventional medical treatments. A comprehensive treatment plan that combines traditional therapies and alternative approaches can help optimize the overall care and well-being of children with cerebral palsy.

Coping and Support for Cerebral Palsy
Caring for a child with cerebral palsy can be challenging, but there are various ways you can cope and find support. The first step is to seek help and guidance from professionals in the field, including doctors, therapists, and healthcare providers. They can offer valuable advice on managing your child's condition and provide resources to support their overall well-being.
Encouraging independence is another important aspect of coping with cerebral palsy. By fostering your child's autonomy and self-reliance, you can help them develop important life skills and boost their confidence. This can be achieved through activities tailored to their abilities and providing them with the necessary tools and support.
Joining support groups specifically designed for families of children with cerebral palsy can also be incredibly beneficial. These groups provide a safe space to share experiences, exchange information, and learn from others who are going through similar challenges. Connecting with other parents who understand the daily struggles and triumphs can provide emotional support and a sense of community.
Finally, it's crucial to ensure your child has the opportunity to participate in social, educational, and recreational activities. By fostering their inclusion in these activities, you not only enhance their quality of life but also promote their overall development and well-being. Encourage their involvement in school programs, extracurricular activities, and community events, as these experiences can help them build social skills and create lasting connections.
FAQ
What are the effective treatment options for cerebral palsy?
Treatment options for cerebral palsy include medications, therapies (such as physical, occupational, speech, and recreational therapy), surgical procedures, and other treatments as needed.
How is cerebral palsy diagnosed?
Cerebral palsy can be diagnosed through a series of tests such as brain scans, electroencephalogram (EEG), and laboratory tests. Healthcare professionals evaluate the child's symptoms, review medical history, conduct physical exams, and monitor growth and development to make a diagnosis.
What are the different types of cerebral palsy?
There are different types of cerebral palsy, including spastic, dyskinetic, and ataxic. Spastic cerebral palsy is characterized by stiff muscles and exaggerated reflexes, dyskinetic cerebral palsy makes it hard to control voluntary muscles, and ataxic cerebral palsy is characterized by trouble with balance and coordination.
What does lifelong care for cerebral palsy involve?
Children and adults with cerebral palsy may require lifelong care with a health care team that includes a pediatrician, physical medicine and rehabilitation specialist, pediatric neurologist, therapists, and mental health specialists. Treatment plans are customized based on the individual's symptoms and needs, with early intervention playing a crucial role in improving outcomes.
How does physical therapy and rehabilitation help with cerebral palsy?
Physical therapy is a key component of cerebral palsy treatment. It involves exercises and activities that improve muscle strength, balance, and movement. Occupational therapy focuses on everyday activities like dressing and school participation, while speech and language therapy helps improve communication skills. Recreational therapy involves art programs, cultural activities, and sports, and orthotic devices, assistive devices, and technologies can also be used to improve function and mobility.
What medications are used to manage cerebral palsy symptoms?
Medications such as muscle relaxants like baclofen and diazepam can help relax stiff muscles associated with cerebral palsy. Botox injections can be used to reduce muscle tightness and drooling. The choice of medication and delivery method depends on the individual's specific symptoms and needs, and it's important to discuss the benefits and risks with a healthcare professional.
Are surgical procedures necessary for cerebral palsy?
In some cases, surgical procedures may be necessary to address severe symptoms of cerebral palsy. Orthopedic surgery can correct muscle tissue shortening, bone or joint abnormalities, and improve mobility. Selective dorsal rhizotomy involves cutting specific nerves to reduce spastic movements. Surgery can also focus on lengthening muscles or repositioning tendons. It's crucial to carefully assess the benefits and risks of surgical procedures before proceeding.
Are there alternative therapies available for cerebral palsy?
Some children with cerebral palsy may benefit from alternative therapies in addition to traditional treatment options. Alternative therapies include acupuncture, aquatic therapy, hippotherapy, and music therapy. These therapies focus on improving fine motor skills, mobility, and overall well-being. It's important to discuss potential risks and benefits with a healthcare professional before considering alternative therapies.
How can families cope with cerebral palsy and find support?
Caring for a child with cerebral palsy can present challenges, and it's important for families to seek support. Encouraging independence and advocating for the child's needs are crucial. Finding support from support groups, healthcare professionals, therapists, and other parents can provide valuable guidance. Foster the child's participation in social, educational, and recreational activities to enhance their quality of life.
Source Links
- https://www.cerebralpalsyguide.com/treatment/
- https://www.mayoclinic.org/diseases-conditions/cerebral-palsy/diagnosis-treatment/drc-20354005
- https://www.nichd.nih.gov/health/topics/cerebral-palsy/conditioninfo/treatments
Understanding Bell's Palsy: Symptoms And Recovery
Welcome to our comprehensive guide on Bell's Palsy, a condition that can suddenly weaken the muscles on one side of your face. Also known as acute peripheral facial palsy of unknown cause, Bell's Palsy is characterized by facial paralysis, drooping of the mouth, difficulty closing the eye, drooling, and pain around the jaw or ear. While the exact cause remains unknown, experts believe that swelling and inflammation of the facial nerve play a role in its development.
If you or someone you know is experiencing these symptoms, it's important to seek medical help as soon as possible, as Bell's Palsy can present similar symptoms to a stroke. Understanding the symptoms and recovery process can help you navigate this condition with confidence.
Key Takeaways:
- Bell's Palsy causes sudden weakness in the muscles on one side of the face.
- Symptoms include facial paralysis, drooping of the mouth, difficulty closing the eye, drooling, and pain around the jaw or ear.
- Most people recover within a few weeks to six months, but some may experience long-term effects.
- It's important to seek medical help to rule out a stroke if paralysis is observed.
- Treatment options include corticosteroids, antiviral medicines, eye care, and physical therapy.
What is Bell's Palsy and Who Gets It?
Bell's palsy is an unexplained episode of facial muscle weakness or paralysis that typically affects only one side of the face. This condition can occur in anyone, but it is most commonly observed in individuals aged between 15 and 60 years. Interestingly, Bell's palsy affects both men and women equally, without any gender bias.
Several risk factors contribute to the development of Bell's palsy. These include pregnancy, upper respiratory infections like the flu or a cold, diabetes, high blood pressure, and obesity. Moreover, individuals with a family history of recurrent attacks are also susceptible, indicating a possible genetic link to the condition.
| Risk Factors | Prevalence |
|---|---|
| Pregnancy | Increased risk |
| Upper respiratory infections | Common trigger |
| Diabetes | Elevated risk |
| High blood pressure | Risk factor |
| Obesity | Potential trigger |
| Family history of recurrent attacks | Risk factor |
Understanding the risk factors associated with Bell's palsy is crucial for early identification and prompt medical intervention. By recognizing these factors, healthcare professionals can provide targeted support and management strategies tailored to an individual's unique circumstances.

Causes and Triggers of Bell's Palsy
Bell's Palsy is a condition characterized by sudden weakness or paralysis of the muscles on one side of the face. While the exact cause of Bell's Palsy is unknown, it is often associated with viral infections. Several viruses have been linked to the development of Bell's Palsy, including herpes simplex, herpes zoster, infectious mononucleosis, cytomegalovirus, adenovirus, and others.
In addition to viral infections, there are other triggers that can contribute to the development of Bell's Palsy. Trauma, such as an injury to the face or head, can lead to facial nerve damage and subsequent paralysis. Exposure to toxins, such as certain medications or chemicals, has also been identified as a potential trigger. Furthermore, individuals with underlying conditions like diabetes, high blood pressure, and certain autoimmune diseases may have a higher risk of developing Bell's Palsy.
It is important to note that Bell's Palsy itself is not contagious. It is not spread from person to person, even if they have direct contact with someone affected by the condition.

Symptoms and Diagnosis of Bell's Palsy
When it comes to bell's palsy symptoms and obtaining an accurate diagnosis is crucial for timely treatment and management. Understanding the signs can help you distinguish Bell's Palsy from other conditions and seek appropriate medical care.
Common Symptoms of Bell's Palsy
Bell's Palsy often manifests with the following symptoms:
- Sudden weakness or paralysis on one side of the face
- Drooping of the mouth
- Difficulty making facial expressions
- Drooling
- Pain around the jaw or ear
- Increased sensitivity to sound
- Headache
- Loss of taste
- Changes in tear and saliva production
If you experience any form of paralysis, especially on one side of the face, it is crucial to consult a healthcare professional. Although Bell's Palsy is not a life-threatening condition, it is essential to rule out a stroke or other underlying causes. Timely diagnosis and treatment can contribute to better outcomes.
Diagnosing Bell's Palsy
Diagnosing Bell's Palsy typically involves a comprehensive evaluation of symptoms and a thorough medical examination. Your doctor will carefully assess the facial paralysis, consider your medical history, and inquire about any associated pain or discomfort.
While physical examination and clinical observation are often enough to diagnose Bell's Palsy, additional tests may be recommended to rule out other conditions. These tests can include:
- Electromyography (EMG): This test measures the electrical activity of the facial muscles, helping to assess nerve functionality.
- Blood tests: Blood tests can help exclude other potential causes of facial paralysis, such as infections or autoimmune disorders.
- Imaging: In certain cases, imaging tests like an MRI or CT scan may be ordered to rule out other conditions that may mimic the symptoms of Bell's Palsy.
While these tests may supplement the diagnosis process, they are typically not necessary for every Bell's Palsy case. Your healthcare provider will determine the most appropriate diagnostic approach based on your specific situation.
Key Takeaways:
- Bell's Palsy is characterized by sudden weakness or paralysis on one side of the face, along with other associated symptoms.
- It is important to seek medical attention if you experience any form of paralysis to rule out more serious conditions like stroke.
- Diagnosis of Bell's Palsy is primarily based on symptoms, although additional tests may be conducted to confirm the diagnosis and rule out other potential causes.
Treatment Options for Bell's Palsy
When it comes to Bell's Palsy, the treatment options available vary depending on the severity of symptoms. In most cases, the condition resolves on its own without the need for medical intervention. However, certain treatments can help accelerate the recovery process and alleviate discomfort.
Corticosteroids are often prescribed to reduce inflammation and swelling of the facial nerve. These medications can effectively speed up the healing process and improve facial muscle function.
If a viral infection is suspected as the cause of Bell's Palsy, antiviral medicines may be used in conjunction with corticosteroids to help fight the underlying infection and prevent further damage.
To alleviate pain and discomfort associated with Bell's Palsy, analgesics can be used. Additionally, applying moist heat to the affected area can help reduce inflammation and promote healing.
Eye care is of utmost importance in managing Bell's Palsy. To protect the affected eye from drying out and potential complications, it is crucial to keep the eye lubricated with eye drops or ointment. Regular blinking exercises can also help maintain eye moisture.
Physical therapy plays a vital role in the recovery of Bell's Palsy. Facial exercises and stimulation techniques can help promote nerve regeneration and restore normal muscle function. Additionally, alternative therapies such as acupuncture and relaxation techniques may be considered to aid in the overall recovery process.
It is important to consult with a healthcare professional to determine the appropriate treatment options based on individual symptoms and needs.

| Treatment Options | Description |
|---|---|
| Corticosteroids | Reduce inflammation and swelling of the facial nerve |
| Antiviral Medicines | Used if a viral infection is suspected |
| Analgesics | Alleviate pain and discomfort |
| Moist Heat | Reduce inflammation and promote healing |
| Eye Care | Protect the affected eye from drying |
| Physical Therapy | Facial exercises and stimulation techniques |
| Alternative Therapies | Acupuncture and relaxation techniques |
Complications and Long-Term Effects of Bell's Palsy
While most cases of Bell's Palsy resolve within a month without complications, severe cases can lead to various complications and long-term effects. These can significantly impact the affected individual's quality of life and require additional medical attention.
Complications:
- Irreversible damage to the facial nerve: In some cases, Bell's Palsy can cause permanent damage to the facial nerve. This damage may result in persistent weakness or paralysis of the facial muscles.
- Irregular regrowth of nerve fibers: Sometimes, the regrowth of nerve fibers after Bell's Palsy can be irregular, leading to involuntary muscle contractions. These contractions can cause facial twitching or spasms.
- Partial or complete blindness of the eye: Excessive dryness of the eye due to the inability to close it properly can result in partial or complete blindness. Proper eye care is crucial to prevent this complication.
Long-Term Effects:
- Lopsided face: Bell's Palsy can result in facial asymmetry, causing one side of the face to appear droopy or lopsided.
- Crooked smile: The facial muscle weakness or paralysis can lead to a crooked smile, making it challenging to express emotions naturally.
- Involuntary facial movements: Some individuals may experience involuntary movements in the affected facial muscles.
- Tightness of facial or neck muscles: Long-term effects may include tightness or stiffness in the facial or neck muscles.
To manage these complications and long-term effects, a multidisciplinary approach involving physicians, physical therapists, and other healthcare professionals may be necessary. Treatments, such as physical therapy, facial exercises, medication, and surgical interventions, can help improve facial function and minimize the impact of these complications on daily life.

It is important for individuals with Bell's Palsy to seek ongoing medical care to monitor their progress and address any lingering symptoms or concerns. While the majority of cases resolve fully, understanding potential complications and long-term effects can help individuals make informed decisions about their treatment and recovery journey.
Bell's Palsy Recovery and Prognosis
When it comes to Bell's Palsy, the prognosis is generally positive, and most individuals can expect to experience a full recovery within a few weeks to months. Signs of recovery often become apparent through improved muscle tone and facial movements. However, it's important to note that some individuals may experience persistent symptoms or long-term effects.
To aid in the recovery process, following the recommended treatments and therapies is crucial. These may include:
- Corticosteroids: Medications that help reduce inflammation, allowing for faster healing.
- Physical therapy: Exercises and techniques to stimulate and strengthen the facial muscles.
- Eye care: Taking steps to protect the affected eye from dryness and potential damage.
Regular follow-up appointments with a healthcare provider are essential for monitoring progress and addressing any lingering symptoms. This ongoing care ensures that individuals receive the necessary support and guidance throughout their recovery journey.
Remember, each case of Bell's Palsy is unique, and the recovery timeline may vary. By staying proactive, adhering to the recommended treatments, and maintaining regular communication with a healthcare professional, you can maximize your chances of a successful recovery.
| Recovery Signs | Duration |
|---|---|
| Improved muscle tone | A few weeks |
| Facial movements | Months |
| Persistent symptoms | Varies |
| Long-term effects | Possible |
Living with Bell's Palsy
Bell's Palsy is a temporary condition that affects the muscles on one side of the face, causing weakness or paralysis. While the condition itself is not permanent, it is important to take proper care of the affected eye and support your overall well-being during the recovery process.
Eye Care
One of the key aspects of living with Bell's Palsy is ensuring proper eye care. The weakness or paralysis of the facial muscles can affect the eye's ability to blink and close properly, which can lead to complications such as corneal scratching and dryness.
To prevent these complications, your healthcare provider may recommend using eye drops or ointments to keep your eye moist during the day and protecting it at night. This can help alleviate discomfort and reduce the risk of further damage. Additionally, it's important to protect your eye from dust and debris by wearing sunglasses or using protective eyewear when necessary.
Managing Stress and Rest
Living with Bell’s Palsy can be challenging, both physically and emotionally. Managing stress and getting adequate rest are important aspects of supporting your overall well-being during the recovery process.
Additionally, getting enough rest is crucial for your body to heal and recover. Make sure to prioritize sleep and create a peaceful environment conducive to relaxation.
Supportive Measures
While there is no specific cure for Bell's Palsy, there are various supportive measures that can aid in your recovery. Physical therapy may be recommended to stimulate the facial nerve and improve muscle strength and control.
In addition, alternative therapies such as acupuncture and facial exercises have shown some benefits in promoting nerve regeneration and improving facial function. However, always consult with your healthcare provider before trying any alternative therapies.
It's important to remember that everyone's experience with Bell's Palsy is unique, and recovery timelines can vary. By taking proper care of your eye, managing stress, getting adequate rest, and exploring supportive measures, you can support your recovery and minimize the impact on your daily life.
Bell's Palsy vs. Stroke: Knowing the Difference
Bell's palsy and stroke share similar symptoms, including facial paralysis and difficulty closing the eye. However, there are significant differences between the two conditions that can help differentiate them.
In Bell's palsy, symptoms typically come on suddenly and only affect one side of the face. On the other hand, a stroke can cause numbness or weakness on one side of the body in addition to facial symptoms.
There are also other distinguishing factors that can help identify whether it is Bell's palsy or a stroke. Changes in taste, eye watering, and sensitivity to sound are more commonly associated with Bell's palsy.
To summarize, while Bell's palsy and stroke can present with similar facial symptoms, the sudden onset and exclusive involvement of one side of the face, along with other associated factors, can help differentiate Bell's palsy from a stroke.
Distinguishing Factors between Bell's Palsy and Stroke:
- Bell's Palsy:
- Sudden onset
- Facial paralysis on one side of the face
- Changes in taste
- Eye watering
- Sensitivity to sound
- Stroke:
- Numbness or weakness on one side of the body
- Facial symptoms in addition to other body symptoms
Bell's Palsy Recovery Signs and Duration
Recovering from Bell's Palsy can be a gradual process, and it's important to recognize the signs that indicate progress. The first signs of recovery often become evident within a few weeks.
- Improved muscle tone: As your facial muscles start to regain their strength, you may notice improved muscle tone. This can manifest as increased control over facial movements and a reduction in drooping or weakness.
- Facial movements: The ability to make facial expressions is a positive sign of recovery. You may observe improvements in your ability to smile, blink, and raise your eyebrows.
While some people experience a complete recovery within a few months, the duration of Bell's Palsy can vary from person to person. It is essential to be patient and not get discouraged if the recovery process takes longer for you.
On average, full recovery from Bell's Palsy can take anywhere from three to six months.
If your symptoms persist or worsen over time, it is crucial to seek further evaluation and treatment options from a healthcare provider. They can provide personalized guidance and recommend therapies that may accelerate your recovery.
Is Bell's Palsy Permanent?
While most people with Bell's Palsy make a full recovery, some may experience long-term effects or lingering symptoms. These can include a lopsided face, crooked smile, involuntary facial movements, and tightness of facial or neck muscles. In some cases, cosmetic procedures or surgery may be recommended to address these effects. Regular follow-up with a healthcare provider is important to monitor progress and address any ongoing concerns.
Potential Long-Term Effects of Bell's Palsy
Bell's Palsy can have lasting consequences that impact a person's facial appearance and muscle control. Some individuals may exhibit:
- A lopsided face
- A crooked smile
- Involuntary facial movements
- Tightness of facial or neck muscles
These long-term effects can significantly affect an individual's self-confidence and quality of life. Therefore, it is crucial to consult with a healthcare professional to explore potential treatment options and address any concerns.
Treatment Options for Long-Term Effects
Cosmetic procedures or surgery may be recommended to improve the appearance and function of the face for individuals experiencing long-term effects of Bell's Palsy. These interventions aim to restore symmetry, reduce involuntary movements, and alleviate muscle tightness.
It is important to note that the appropriateness of these treatment options varies based on individual circumstances. Consulting with a healthcare provider who specializes in facial nerve disorders can help determine the most suitable course of action.
Ongoing Monitoring and Support
Regular follow-up appointments with a healthcare provider are crucial for individuals with long-term effects of Bell's Palsy. These appointments allow for monitoring of progress, the evaluation of treatment effectiveness, and addressing any ongoing concerns or symptoms.
Additionally, healthcare providers can provide support and guidance, offer recommendations for managing symptoms, and ensure comprehensive care throughout the recovery process.
Conclusion
Bell's Palsy is a temporary condition that affects the muscles on one side of your face, causing weakness or paralysis. Although the exact cause is unknown, it is believed to be related to inflammation and swelling of the facial nerve, often triggered by viral infections. Most people recover fully within a few weeks to months with the help of treatment options such as corticosteroids and physical therapy.
However, it is important to note that complications and long-term effects can occur in some cases. These may include irreversible damage to the facial nerve, involuntary muscle contractions, and partial or complete blindness of the affected eye due to excessive dryness. Therefore, regular follow-up with a healthcare provider is crucial to monitor your progress and address any lingering symptoms or concerns.
If you are experiencing any symptoms of Bell's Palsy, it is vital to seek medical help to rule out other conditions such as stroke. Timely diagnosis and appropriate treatment can significantly improve your chances of full recovery. Remember to take care of your affected eye by using eye drops or ointments to keep it moist and protect it from scratching and dryness.
In conclusion, while Bell's Palsy can be a challenging condition to navigate, with proper care and treatment, most individuals can regain full facial function and lead a normal life. Stay informed, follow the recommended interventions, and consult with your healthcare provider for personalized guidance throughout your recovery journey.
FAQ
What is Bell's Palsy?
Bell's Palsy is a condition that causes sudden weakness or paralysis of the muscles on one side of the face.
What are the symptoms of Bell's Palsy?
Symptoms of Bell's Palsy include facial paralysis, drooping of the mouth, difficulty closing the eye, drooling, and pain around the jaw or ear.
What causes Bell's Palsy?
The exact cause of Bell's Palsy is unknown, but it is believed to be related to swelling and inflammation of the facial nerve. Viral infections and certain triggers such as trauma and toxins may also play a role.
How is Bell's Palsy diagnosed?
Diagnosis of Bell's Palsy is usually based on symptoms, but additional tests such as electromyography, blood tests, and imaging may be done to rule out other conditions.
What are the treatment options for Bell's Palsy?
Treatment for Bell's Palsy depends on the severity of symptoms. It may include corticosteroids to reduce inflammation, antiviral medicines, pain relief, eye care, and physical therapy.
Are there any complications or long-term effects of Bell's Palsy?
Complications of Bell's Palsy can include irreversible damage to the facial nerve, irregular regrowth of nerve fibers, and partial or complete blindness of the eye. Long-term effects may include a lopsided face, crooked smile, and involuntary facial movements.
What is the prognosis for Bell's Palsy?
Most people with Bell's Palsy experience full recovery within a few weeks to months. Regular follow-up with a healthcare provider is important to monitor progress and address any lingering symptoms.
How should I take care of my eye if I have Bell's Palsy?
It is important to protect the affected eye from drying and potential complications. Eye drops or ointments may be recommended to keep the eye moist, and protecting it from dust and debris is crucial.
How is Bell's Palsy different from a stroke?
While Bell's Palsy and stroke can have similar symptoms such as facial paralysis, Bell's Palsy affects only one side of the face and does not cause numbness or weakness on one side of the body.
How long does it take to recover from Bell's Palsy?
Most people start to see improvements in their symptoms within a few weeks, and full recovery can take anywhere from 3 to 6 months.
Is Bell's Palsy permanent?
Bell's Palsy itself is not a permanent condition, but some people may experience long-term effects or lingering symptoms.
Source Links
- https://www.mayoclinic.org/diseases-conditions/bells-palsy/symptoms-causes/syc-20370028
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/bells-palsy
- https://www.webmd.com/brain/understanding-bells-palsy-basics
Understanding Benign Essential Blepharospasm
Benign Essential Blepharospasm (BEB) is a neurological disorder that affects the muscles of the eyelids, causing involuntary contractions and spasms. It falls under the category of dystonia, which is a movement disorder. This condition primarily affects middle-aged and older women, and its symptoms can significantly impact daily life and quality of life. While the exact cause is unknown, researchers believe it may involve a combination of genetic and environmental factors. Diagnosis is made based on a clinical evaluation, history, and identification of characteristic symptoms.
Key Takeaways:
- Benign Essential Blepharospasm is a neurological disorder characterized by involuntary muscle contractions of the eyelids.
- This condition primarily affects middle-aged and older women.
- The exact cause of BEB is unknown, but it is believed to involve genetic and environmental factors.
- Diagnosis is made based on clinical evaluation, history, and identification of characteristic symptoms.
- Treatment options include botulinum toxin injections, medication, or surgery.
What is Benign Essential Blepharospasm?
Benign Essential Blepharospasm (BEB) is a neurological disorder that causes involuntary muscle contractions and spasms of the eyelid. It is considered a form of dystonia, a movement disorder characterized by abnormal muscle contractions. The exact cause of BEB is unknown, but it is believed to involve dysfunction in the basal ganglia, a region of the brain involved in motor control. BEB can affect anyone, but it is more commonly seen in middle-aged and older women.
The symptoms of BEB include:
- Frequent blinking
- Eye irritation
- Difficulty keeping the eyelids open
- Sensitivity to light
- Functional blindness

Managing the symptoms of BEB and understanding its impact on daily life is crucial for individuals affected by this condition.
Causes and Risk Factors of Benign Essential Blepharospasm
The exact cause of benign essential blepharospasm (BEB) is unknown, but researchers believe it may involve a combination of genetic and environmental factors. Dysfunction in the basal ganglia, a region of the brain involved in motor control, is thought to play a role. Some risk factors for BEB include:
- A family history of dystonia or tremors
- Head or facial trauma
- Ocular irritation or diseases
- Certain medications used to treat other conditions
However, in most cases, BEB develops spontaneously with no known precipitating factor.
| Causes of Benign Essential Blepharospasm | Risk Factors for Benign Essential Blepharospasm |
|---|---|
| Genetic factors | Family history of dystonia or tremors |
| Environmental factors | Head or facial trauma |
| Dysfunction in the basal ganglia | Ocular irritation or diseases |
| Certain medications used to treat other conditions |
Symptoms and Diagnosis of Benign Essential Blepharospasm
The early symptoms of benign essential blepharospasm often include frequent blinking, eye irritation, and sensitivity to light. As the condition progresses, the spasms and contractions of the eyelid muscles become more frequent and forceful, sometimes leading to prolonged closure of the eyelids. This can result in functional blindness, although vision itself remains unaffected.
The diagnosis of benign essential blepharospasm is made based on a thorough clinical evaluation, history, and identification of characteristic symptoms. There are no specific laboratory tests to diagnose benign essential blepharospasm, so it is a clinical diagnosis.
| Symptoms of Benign Essential Blepharospasm | Diagnosis |
|---|---|
|
|

Treatment Options for Benign Essential Blepharospasm
The primary treatment for benign essential blepharospasm is periodic injection of botulinum toxin into the eyelid muscles. This weakens the muscles and reduces the spasms and contractions. The injections need to be repeated every few months to maintain the effect.
Medications such as anticholinergic drugs and dopamine depleters may also be used, but their effectiveness is usually moderate or unsatisfactory.
Surgical procedures, such as myectomy (removal of eyelid muscles) or neurectomy (cutting off nerve branches), may be considered for patients who do not respond well to other treatments. However, these procedures are usually reserved for severe cases.
Treatment Options Overview
| Treatment Option | Description |
|---|---|
| Botulinum toxin injections | Periodic injections weaken the eyelid muscles and reduce spasms and contractions |
| Medications | Anticholinergic drugs and dopamine depleters may be used with varying effectiveness |
| Myectomy | Surgical removal of eyelid muscles |
| Neurectomy | Surgical cutting off of nerve branches |

It is important to consult with a healthcare professional to determine the most appropriate treatment option for your specific condition. They can provide personalized guidance and help minimize the impact of benign essential blepharospasm on your daily life.
Clinical Trials for Benign Essential Blepharospasm
Clinical trials play a crucial role in enhancing our understanding of disorders and developing improved methods for detection, treatment, and prevention. Participating in clinical trials can provide valuable insights into benign essential blepharospasm (BEB) and potentially lead to the development of new treatment options for individuals affected by the condition.
If you have been diagnosed with BEB, you might consider participating in ongoing clinical trials to contribute to the advancement of knowledge in this field. These trials are designed to test the efficacy and safety of new interventions or study the effectiveness of existing treatments. By actively engaging in clinical trials, you can help researchers gain a deeper understanding of BEB and potentially discover more effective strategies for its management.
Various clinical trials dedicated to studying and treating BEB are currently underway. These trials aim to explore innovative treatment methods, evaluate the impact of different medications, or assess potential surgical interventions. By participating, you can contribute to the development of improved therapies that can enhance the lives of individuals with BEB.
If you are interested in participating in a BEB clinical trial, it is essential to gather all the relevant information before making a decision. Websites such as NIH Clinical Research Trials and You and ClinicalTrials.gov provide comprehensive databases of ongoing trials, including those specifically focused on BEB. These platforms offer valuable resources to help you understand the trial requirements, eligibility criteria, and potential benefits or risks of participation.
It is important to consult with your healthcare professional and carefully assess the suitability of a clinical trial for your specific condition and needs. They can provide expert guidance, address any concerns or questions you may have, and help you make an informed decision about participating in a BEB clinical trial.
Benefits of participating in clinical trials
Participating in a clinical trial for BEB can offer several benefits:
- Access to innovative treatments: Clinical trials often provide access to new and promising therapies that may not be available through standard treatment options.
- Contributing to research: By participating, you become an active contributor to scientific research, potentially paving the way for better understanding and management of BEB.
- Comprehensive medical care: Clinical trials typically involve close monitoring and comprehensive medical care, ensuring you receive the most appropriate and up-to-date treatment for your condition.
- Potential personal benefits: In some cases, clinical trial participants may experience improvements in their condition or symptoms as a result of the treatment being investigated.
Considerations for participation
Before deciding to participate in a BEB clinical trial, consider the following:
- Eligibility criteria: Each clinical trial has specific eligibility criteria that determine who can participate. It is important to carefully review these criteria to determine if you meet the requirements.
- Potential risks and side effects: Clinical trials involve certain risks and side effects that vary depending on the treatment being studied. It is important to understand these potential risks and weigh them against the potential benefits.
- Financial considerations: Some clinical trials may offer compensation for participation, while others may not. It is essential to understand the financial implications before committing to a trial.
- Time commitment: Participating in a clinical trial may require regular visits to the study site, additional tests or procedures, and a significant commitment of time. Ensure that you can accommodate the necessary time commitment before enrolling.
By carefully evaluating the benefits, risks, and considerations associated with participating in a clinical trial, you can make an informed decision about your involvement in advancing the understanding and treatment of BEB.
| Benefits of Participating in Clinical Trials for BEB | Considerations for Participation |
|---|---|
| - Access to innovative treatments | - Eligibility criteria |
| - Contribution to research | - Potential risks and side effects |
| - Comprehensive medical care | - Financial considerations |
| - Potential personal benefits | - Time commitment |

Living with Benign Essential Blepharospasm
Living with Benign Essential Blepharospasm (BEB) can significantly impact your daily life and quality of life. The frequent spasms and contractions of the eyelids can make it challenging to perform everyday tasks, such as reading, driving, and even keeping your eyes open. This neurological disorder can also cause emotional distress and social challenges due to the visible symptoms.
Tackling Everyday Challenges
Managing BEB in your everyday life requires a multifaceted approach involving medical treatment, lifestyle adjustments, and support from healthcare professionals. Here are some strategies to help you navigate the challenges of living with BEB:
- Medical treatment: Work closely with your doctor to determine the most suitable treatment plan for you. This may include periodic botulinum toxin injections to weaken the eyelid muscles and reduce spasms and contractions.
- Lifestyle adjustments: Make modifications to your daily routines to accommodate the difficulties caused by BEB. For example, you can try using magnifying glasses for reading or adjusting lighting to minimize sensitivity to light.
- Support groups: Connecting with others who have BEB can provide valuable emotional support and practical advice. Consider joining support groups or online forums where you can share experiences and learn from others.
- Healthcare professionals: Seek regular check-ups with your healthcare professionals to monitor your condition and discuss any concerns or changes in symptoms. They can provide guidance on managing BEB in various aspects of your life.
Remember, living with BEB requires patience and resilience. By seeking appropriate treatment, making necessary adjustments, and accessing support, you can effectively manage the impact of the condition on your everyday life.
Real-life Insights: Coping Strategies
Many individuals living with BEB have developed coping strategies to navigate their everyday life. Here are some insights from people who have firsthand experience:
| Coping Strategy | Insight |
|---|---|
| Reducing Eye Strain | Take frequent breaks to rest your eyes, blink consciously, and use artificial tears to alleviate dryness and irritation. |
| Disclosure and Education | Inform your family, friends, and colleagues about BEB to increase their understanding and support. Educate them on your condition and how they can assist you in different situations. |
| Mindfulness and Relaxation | Practice relaxation techniques such as meditation, deep breathing, or yoga to reduce stress and manage the emotional impact. |
| Assistive Devices | Explore assistive devices such as specialized glasses or eye patches to help manage symptoms and improve daily functioning. |
Remember that coping strategies vary from person to person, and it may take time to find what works best for you. Don't hesitate to experiment, seek advice from healthcare professionals, and connect with others who share similar experiences.
Overall, living with Benign Essential Blepharospasm can be challenging, but with the right support and strategies in place, you can effectively manage the impact of this condition on your everyday life.
Resources for Benign Essential Blepharospasm
If you are seeking more information about benign essential blepharospasm, there are several reputable resources available to help you understand the condition and find support. Here are some recommended sources:
- Genetic and Rare Diseases Information Center (GARD): GARD provides comprehensive information about benign essential blepharospasm, including symptoms, causes, treatment options, and ongoing research. It serves as a valuable resource for individuals looking to learn more about the condition.
- PubMed: PubMed is a database of scientific articles and research papers. By searching for "benign essential blepharospasm" on PubMed, you can access a wealth of scholarly literature on the subject, which can deepen your understanding of the condition.
- NINDS Publication Catalog: The National Institute of Neurological Disorders and Stroke (NINDS) offers a publication catalog with printed materials on various neurological disorders, including benign essential blepharospasm. These materials are available free of charge and can be ordered online or downloaded as PDFs.
In addition to these resources, it may be beneficial to consult with healthcare professionals who specialize in movement disorders. They can provide personalized guidance and answer any specific questions you may have.
Connecting with others who have experienced similar challenges can also be helpful. Consider joining support groups or participating in online forums where you can share your experiences and learn from others in the community.
Comparison of Resources for Benign Essential Blepharospasm
| Resource | Key Features |
|---|---|
| Genetic and Rare Diseases Information Center (GARD) | Comprehensive information on symptoms, causes, treatment options, and ongoing research |
| PubMed | Access to scientific articles and research papers for in-depth knowledge |
| NINDS Publication Catalog | Free printed materials on neurological disorders, including benign essential blepharospasm |
By utilizing these resources, you can gain a better understanding of benign essential blepharospasm and find the information and support you need to manage the condition effectively.

Future Research and Developments for Benign Essential Blepharospasm
Future research in the field of benign essential blepharospasm aims to further our understanding of the condition's underlying mechanisms and develop more effective treatments. Ongoing studies are exploring potential genetic and environmental factors contributing to benign essential blepharospasm. Additionally, research is focused on improving the delivery of botulinum toxin injections, developing novel medications, and investigating alternative treatment approaches. It is hoped that continued research efforts will lead to advancements in the diagnosis, management, and overall care of individuals with benign essential blepharospasm.
In order to tackle the challenges associated with benign essential blepharospasm, researchers are investing significant efforts in understanding the underlying causes and risk factors. Some of the key areas of future research include:
- Identifying specific genetic markers associated with the development of benign essential blepharospasm.
- Investigating the role of environmental factors, such as exposure to toxins or trauma, in triggering the condition.
- Developing new techniques for the precise delivery of botulinum toxin injections to target the affected eyelid muscles more effectively.
- Exploring alternative treatment approaches, such as the use of non-invasive therapies or neurostimulation techniques.
By gaining a deeper understanding of the mechanisms behind benign essential blepharospasm and developing innovative treatment approaches, researchers hope to improve the quality of life for individuals living with this condition. Future research endeavors have the potential to revolutionize the diagnosis, management, and care of individuals with benign essential blepharospasm, offering new hope and possibilities for those affected by the disorder.
Conclusion
Benign Essential Blepharospasm is a neurological disorder characterized by involuntary muscle contractions and spasms of the eyelid. Although the exact cause of this condition is unknown, there are various treatment options available to manage the symptoms of BEB. These include botulinum toxin injections, medications, and surgical procedures.
For individuals living with BEB, it is essential to work closely with healthcare professionals to determine the most suitable treatment approach. By seeking support from available resources and exploring different treatment options, individuals can effectively manage the impact of BEB on their everyday life.
Ongoing research and clinical trials offer hope for further understanding and advancements in the field of BEB. Continued efforts in research aim to uncover the underlying mechanisms of the condition and develop more effective treatments. By participating in clinical trials, individuals with BEB can contribute to the advancement of knowledge and potentially benefit from new treatment options in the future.
FAQ
What is benign essential blepharospasm?
Benign essential blepharospasm is a neurological disorder characterized by involuntary muscle contractions and spasms of the eyelid. It is considered a form of dystonia, a movement disorder.
What are the causes and risk factors of benign essential blepharospasm?
The exact cause of benign essential blepharospasm is unknown, but it is believed to involve dysfunction in the basal ganglia, a region of the brain involved in motor control. Some risk factors include a family history of dystonia or tremors, head or facial trauma, ocular irritation or diseases, and certain medications.
What are the symptoms and how is benign essential blepharospasm diagnosed?
The symptoms of benign essential blepharospasm include frequent blinking, eye irritation, difficulty keeping the eyelids open, sensitivity to light, and functional blindness. The diagnosis is made based on a thorough clinical evaluation, history, and identification of characteristic symptoms. There are no specific laboratory tests to diagnose it.
What are the treatment options for benign essential blepharospasm?
The primary treatment for benign essential blepharospasm is periodic injection of botulinum toxin into the eyelid muscles. Medications and surgical procedures may also be considered for severe cases.
Are there any ongoing clinical trials for benign essential blepharospasm?
Yes, there are ongoing clinical trials that aim to improve our understanding of the disorder and develop new treatment options. Individuals with benign essential blepharospasm can consider participating in these trials to contribute to the advancement of knowledge in this field.
How does benign essential blepharospasm impact daily life?
Benign essential blepharospasm can significantly impact daily life and quality of life. It can make it challenging to perform everyday tasks and can cause emotional distress and social challenges due to the visible symptoms.
Where can I find additional resources for benign essential blepharospasm?
You can find additional resources from reputable sources such as the Genetic and Rare Diseases Information Center (GARD) and PubMed. The NINDS Publication Catalog also offers printed materials on neurological disorders, including benign essential blepharospasm, which are free of charge and can be ordered online or downloaded as PDFs.
What is the future research and development for benign essential blepharospasm?
Future research aims to further our understanding of the condition's underlying mechanisms and develop more effective treatments. Ongoing studies are exploring potential genetic and environmental factors contributing to benign essential blepharospasm.
Source Links
- https://eyewiki.aao.org/Blepharospasm
- https://www.ninds.nih.gov/health-information/disorders/benign-essential-blepharospasm
- https://rarediseases.org/rare-diseases/benign-essential-blepharospasm/
Brown Sequard Syndrome Symptoms
Brown Sequard syndrome (BSS) is a rare neurological condition that affects the spinal cord. It is characterized by muscle weakness or paralysis on one side of the body and a loss of sensation on the opposite side. This condition is named after Charles-Édouard Brown-Séquard, who first described it in 1849.
In Brown Sequard syndrome, the spinal cord is damaged, often due to trauma such as a gunshot or stab wound. It is considered an incomplete spinal cord injury, meaning that there is partial preservation of sensory and/or motor function below the level of the injury.
Understanding the brown sequard syndrome symptoms is crucial for early detection and appropriate management. In this article, we will explore the symptoms, causes, diagnosis, and treatment options for this condition.
Key Takeaways:
- Brown Sequard syndrome is a rare neurological condition that affects the spinal cord.
- It is characterized by muscle weakness or paralysis on one side of the body and a loss of sensation on the opposite side.
- This condition typically occurs as a result of trauma such as a gunshot or stab wound.
- Early diagnosis and appropriate management are important for improving the patient's quality of life.
- Treatment focuses on managing the underlying cause and providing supportive care to improve function and independence.
Understanding Brown Sequard Syndrome
The spinal cord is a cylindrical structure that runs through the center of the spine. It carries nerve bundles and cells that transmit messages between the brain and the rest of the body. Brown Sequard syndrome occurs when there is damage to only one side of the spinal cord in a specific area. This results in muscle weakness or paralysis on one side of the body and a loss of sensation on the opposite side. It is important to note that Brown Sequard spinal cord injury, meaning that some sensory or motor function is still preserved below the level of the injury.
Schematic representation of the spinal cord

In Brown Sequard syndrome, the damage to the spinal cord typically affects a specific segment, leading to a disruption in the transmission of signals along the affected side of the body. This can result in a range of symptoms depending on the location and severity of the injury. While muscle weakness or paralysis occurs on the same side as the damage, the loss of sensation is observed on the opposite side.
Brown Sequard syndrome is caused by various factors, most commonly trauma such as gunshot or stab wounds. However, inflammation or compression of the spinal cord can also lead to this condition in some cases. Understanding the underlying cause and the specific segment of the spinal cord affected is crucial in determining the appropriate treatment approach and managing the symptoms.
It is important to seek medical attention if you experience any unusual symptoms or suspect a spinal cord injury. A thorough evaluation, including imaging tests like magnetic resonance imaging (MRI), can help confirm the diagnosis of Brown Sequard syndrome and determine the appropriate course of treatment.
Causes of Brown Sequard Syndrome
Brown Sequard syndrome can be caused by various factors, with trauma being the most common cause. Penetrating injuries, such as gunshot or stab wounds, can result in damage to the spinal cord, leading to this syndrome. Additionally, inflammation or pinching of the spinal cord can also be responsible for causing Brown Sequard syndrome. Other possible causes include tumors, cysts, multiple sclerosis, and infectious diseases like tuberculosis or meningitis.
It is essential to note that Brown Sequard syndrome can occur in anyone, regardless of gender. However, it is considered to be a rare condition.

Possible Causes of Brown Sequard Syndrome:
| Cause | Description |
|---|---|
| Trauma | Penetrating injuries like gunshot or stab wounds |
| Inflammation | Inflammation of the spinal cord |
| Pinching | Compression or pinching of the spinal cord |
| Tumors | Abnormal growths in or near the spinal cord |
| Cysts | Fluid-filled sacs in the spinal cord or brain |
| Multiple sclerosis | An autoimmune disease affecting the central nervous system |
| Infectious diseases | Diseases like tuberculosis or meningitis |
Difference between Brown Sequard Syndrome and Central Cord Syndrome
While both Brown Sequard syndrome and central cord syndrome are forms of incomplete spinal cord injury, they are distinct conditions. Brown Sequard syndrome occurs when there is damage to only one side of the spinal cord, resulting in symptoms on that side of the body. On the other hand, central cord syndrome involves damage to the center of the spinal cord, usually in the neck.
In Brown Sequard syndrome, the symptoms are typically more pronounced on the side of the body opposite the injury. For example, if the injury occurs on the right side of the spinal cord, there will be muscle weakness or paralysis on the left side of the body and a loss of sensation on the right side.
In central cord syndrome, there is typically more pronounced weakness in the arms compared to the legs. This is because the nerves that control arm movements are located in the center of the spinal cord, while the nerves that control leg movements are located more towards the outer edges.
Here is a comparison between the two conditions:
| Brown Sequard Syndrome | Central Cord Syndrome |
|---|---|
| Damage to one side of the spinal cord | Damage to the center of the spinal cord |
| Symptoms on the opposite side of the body | Pronounced weakness in the arms |
| Loss of sensation on the same side of the body | Legs may be less affected |
In summary, while both Brown Sequard syndrome and central cord syndrome are forms of incomplete spinal cord injury, they present with different patterns of symptoms. Brown Sequard syndrome involves damage to one side of the spinal cord, resulting in symptoms on that side of the body, while central cord syndrome involves damage to the center of the spinal cord, usually with more pronounced weakness in the arms.
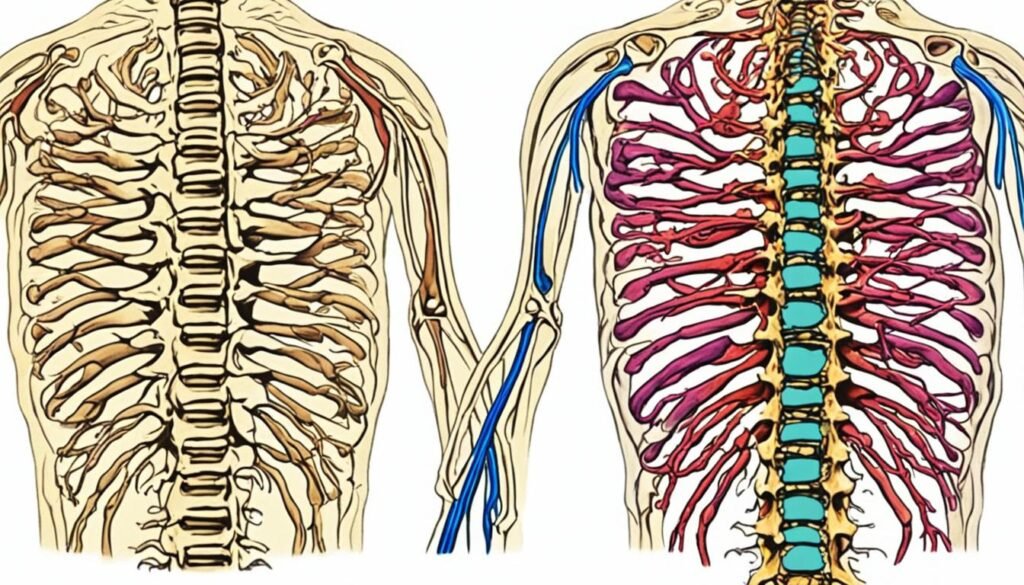
Who Does Brown Sequard Syndrome Affect?
Brown Sequard syndrome is a rare condition that can affect anyone, regardless of age or demographic factors.
It is known that this syndrome affects people assigned female at birth and people assigned male at birth in equal numbers. It does not discriminate based on gender or any other factor. Whether you are a man or a woman, you are at an equal risk of developing Brown Sequard syndrome.
This rare condition can occur in individuals of all ages, from infants to the elderly. However, it is important to note that Brown Sequard syndrome is a relatively uncommon neurological condition.

Having a better understanding of who may be affected by Brown Sequard syndrome can help raise awareness and promote early detection and treatment.
How Common is Brown Sequard Syndrome?
Brown Sequard syndrome, although rare, is a condition that can occur as a result of traumatic spinal cord injuries. Approximately 2% to 4% of traumatic spinal cord injuries are estimated to lead to Brown Sequard syndrome. In the United States alone, there are around 12,000 new cases of traumatic spinal cord injuries reported each year.
While Brown Sequard syndrome is considered to be a rare condition, its impact on individuals who experience traumatic spinal cord injuries should not be overlooked. Understanding the prevalence of this syndrome can help healthcare professionals, researchers, and patients gain insights into its nature and develop more effective treatment strategies.

Brown Sequard Syndrome Symptoms
When it comes to Brown Sequard syndrome, there are several common Brown Sequard Syndrome Symptoms that individuals may experience. These symptoms can vary depending on the location and severity of the spinal cord injury. Below are the key symptoms associated with Brown Sequard syndrome:
Sensory Loss:
One of the hallmark Brown Sequard Syndrome Symptoms is sensory loss on one side of the body. This means that individuals may have reduced or complete loss of sensation, such as touch or vibration, on the affected side.
Muscle Weakness or Paralysis:
Brown Sequard Syndrome Symptoms can also lead to muscle weakness or even paralysis on the same side of the body as the sensory loss. This happens because the damage to the spinal cord disrupts the signals that control muscle movement.
Loss of Pain and Temperature Sensation:
In addition to sensory loss, individuals with Brown Sequard Syndrome Symptoms may experience a loss of pain and temperature sensation on the opposite side of the body. This means that they may not be able to feel pain or changes in temperature on the affected side.
These symptoms can greatly impact an individual's daily life and require careful management and support. It is important for healthcare professionals to accurately diagnose and evaluate the extent of the spinal cord injury to develop an appropriate treatment plan.

| Symptom | Side of the Body |
|---|---|
| Sensory Loss (vibration and position sense) | On the same side as the spinal cord injury |
| Muscle Weakness or Paralysis | On the same side as the spinal cord injury |
| Loss of Pain and Temperature Sensation | On the opposite side of the spinal cord injury |
Diagnosis and Evaluation of Brown Sequard Syndrome
The diagnosis of BrownSequard syndrome is typically made based on your medical history and a thorough physical examination. During the medical history assessment, your healthcare provider will inquire about any recent trauma, symptoms, and any other relevant information related to your condition. This will help in determining the potential cause and underlying factors contributing to your symptoms.
The physical examination is a crucial part of diagnosing Brown Sequard syndrome. Your healthcare provider will evaluate your motor function, sensory responses, and reflexes to assess the extent of the spinal cord injury and the resulting neurological deficits. Specifically, they will examine the strength, range of motion, and sensation in different parts of your body.
Additional diagnostic tests may be recommended to confirm the diagnosis or evaluate the underlying cause of Brown Sequard syndrome. These tests can include:
- Magnetic resonance imaging (MRI): This imaging technique uses powerful magnets and radio waves to create detailed images of the spinal cord. It can provide valuable information about the location and extent of the spinal cord injury.
- X-rays: X-ray images may be taken to assess the bony structures of your spine and detect any fractures or abnormalities.
- Electromyography (EMG): This test measures the electrical activity of your muscles and the nerve signals that control them. It can help determine the extent of nerve damage.
- Computed tomography (CT) scan: A CT scan uses X-ray imaging to create cross-sectional images of the spinal cord. It can help identify fractures, tumors, or other abnormalities.
- Blood tests: Blood tests may be conducted to rule out any underlying medical conditions or infections that could be contributing to your symptoms.
These diagnostic tests, combined with your medical history and physical examination findings, will assist your healthcare provider in confirming the diagnosis of Brown Sequard syndrome and determining the appropriate course of treatment.
Treatment and Management of Brown Sequard Syndrome
When it comes to Brown Sequard syndrome treatment, there is no specific treatment available. However, the focus is on managing the underlying cause of the syndrome and providing supportive care to improve the patient's quality of life. This involves a combination of medications, devices, and therapies.
Medications
Medications may be prescribed to help control muscle symptoms and alleviate pain. These can include:
- Analgesics: to manage pain
- Spasticity medications: to reduce muscle stiffness and spasms
- Antidepressants: to address mood changes and promote emotional well-being
- Anticonvulsants: to manage seizures, if present
Devices and Assistive Technology
Devices and assistive technology play a crucial role in enhancing mobility and independence for individuals with Brown Sequard syndrome. Some commonly used devices include:
- Orthotic braces to support weakened muscles and improve stability
- Wheelchairs or mobility scooters for individuals with significant mobility impairments
- Limb supports and walking aids for balance and gait assistance
- Adaptive tools for daily activities such as dressing, eating, and personal care
Physical and Occupational Therapy
Physical and occupational therapy are essential components of the management plan for Brown Sequard syndrome. These therapies aim to improve muscle strength, flexibility, balance, and coordination, as well as enhance fine motor skills and functional abilities. Therapists employ various techniques, exercises, and modalities tailored to the individual's specific needs and goals.
Surgical Interventions
In severe cases of Brown Sequard syndrome where there is significant compression or damage to the spinal cord, surgical intervention may be considered. Decompression surgery aims to relieve pressure on the spinal cord and stabilize the spine. The specific surgical procedures will depend on the underlying cause and the location of the injury.
By addressing the underlying cause and providing supportive care, individuals with Brown Sequard syndrome can experience improvements in their quality of life and functional abilities. The treatment approach is multidisciplinary and may involve collaboration between neurologists, orthopedic surgeons, physical therapists, occupational therapists, and other healthcare professionals.
Conclusion
The prognosis for individuals with Brown Sequard syndrome can vary based on the cause and severity of the spinal cord injury. While recovery is possible, it is important to understand that the timeline and extent of recovery differ among patients. However, with dedicated rehabilitation and physical therapy, individuals with Brown Sequard syndrome can significantly improve their quality of life and regain some level of independence.
Rehabilitation and physical therapy are crucial components of the treatment plan for Brown Sequard syndrome. These therapies aim to help individuals regain function and enhance their overall well-being. Through personalized exercises and interventions, rehabilitation specialists assist patients in strengthening their muscles, improving coordination, and enhancing mobility.
It is important to note that rehabilitation and recovery for Brown Sequard syndrome require a multidisciplinary approach. In addition to physical therapy, individuals may also benefit from occupational therapy, which focuses on enhancing daily living skills, and psychological support to manage emotional challenges associated with the condition.
With appropriate care, support, and active participation in rehabilitation, many individuals with Brown Sequard syndrome can achieve significant recovery and improve their overall prognosis. While the journey may be challenging, it is important to remain optimistic and seek guidance from healthcare professionals who specialize in spinal cord injuries. Remember, every step towards recovery, no matter how small, is a milestone in your journey towards regaining functionality.
FAQ
What is Brown Sequard syndrome?
Brown Sequard syndrome is a rare neurological condition that occurs as a result of damage to the spinal cord. It is characterized by muscle weakness or paralysis on one side of the body and a loss of sensation on the opposite side.
What causes Brown Sequard syndrome?
The most common cause of Brown Sequard syndrome is trauma, particularly penetrating injuries like gunshot or stab wounds. However, inflammation or pinching of the spinal cord can also lead to this condition in some cases.
What is the difference between Brown Sequard syndrome and central cord syndrome?
Brown Sequard syndrome occurs when there is damage to only one side of the spinal cord, resulting in symptoms on that side of the body. Central cord syndrome involves damage to the center of the spinal cord, usually in the neck.
Who does Brown Sequard syndrome affect?
Brown Sequard syndrome can affect anyone, regardless of gender or other demographic factors.
How common is Brown Sequard syndrome?
Brown Sequard syndrome is a rare condition. Approximately 2% to 4% of traumatic spinal cord injuries are estimated to result in Brown Sequard syndrome.
What are the common symptoms of Brown Sequard syndrome?
The common symptoms of Brown Sequard syndrome include sensory loss on one side of the body, muscle weakness or paralysis on the same side, and a loss of pain and temperature sensation on the opposite side.
How is Brown Sequard syndrome diagnosed?
The diagnosis of Brown Sequard syndrome is typically made based on the patient's history and physical examination. Additional diagnostic tests such as magnetic resonance imaging (MRI) or X-rays may be ordered to confirm the diagnosis or evaluate the underlying cause of the syndrome.
Is there a specific treatment for Brown Sequard syndrome?
There is no specific treatment for Brown Sequard syndrome. The focus is on managing the underlying cause of the syndrome and providing supportive care to improve the patient's quality of life.
What is the prognosis for individuals with Brown Sequard syndrome?
The prognosis for individuals with Brown Sequard syndrome varies depending on the cause of the spinal cord injury and the extent of damage. While recovery is possible, the timeline and extent of recovery can vary greatly among patients. Rehabilitation and physical therapy play a crucial role in helping individuals with Brown Sequard syndrome regain function and improve their quality of life.
Source Links
- https://my.clevelandclinic.org/health/diseases/22749-brown-sequard-syndrome-bss
- https://www.ncbi.nlm.nih.gov/books/NBK538135/
- https://rarediseases.org/rare-diseases/brown-sequard-syndrome/
Basilar Type Migraine: Symptoms and Relief Options
If you experience migraines with aura symptoms originating from the brainstem, you may be suffering from basilar type migraines. This subtype of migraines is characterized by a range of symptoms, including vertigo, impaired coordination, confusion, and even loss of consciousness. Understanding the symptoms and available relief options is crucial in managing this condition effectively.
Key Takeaways:
- Basilar type migraines are a subtype of migraines with aura originating from the brainstem.
- Common symptoms include vertigo, impaired coordination, confusion, and loss of consciousness.
- Triggers for basilar migraines can include strong smells, loud noises, weather changes, lack of sleep, stress, certain foods, and hormonal changes.
- Treatment options for basilar type migraines include NSAIDs, anti-emetics, and lifestyle modifications such as stress management and trigger avoidance.
- Preventive therapies and medications may also be recommended for frequent and disabling migraines.
Understanding Basilar Migraine
Basilar artery migraine, also known as migraine with brainstem aura, is a rare type of migraine that originates in the brainstem. This condition is characterized by the occurrence of aura symptoms before or during a migraine episode.
Aura symptoms associated with basilar migraines can manifest as various sensory and motor changes. These can include alterations in speech, hearing, and vision. Individuals may also experience vertigo, tinnitus, double vision, impaired muscle control, and a reduced level of consciousness. It is important to note that while these symptoms can be frightening, they are completely reversible.
Basilar migraines can persist for a few hours to several days, significantly impacting the individual's daily life. The frequency and severity of episodes can be influenced by various factors, including stress, lack of sleep, certain foods, hormonal changes, and environmental stimuli.
It is crucial to understand the symptoms associated with basilar migraines to differentiate them from other types of migraines and seek appropriate treatment. Early recognition and management can significantly enhance the quality of life for individuals affected by this condition.
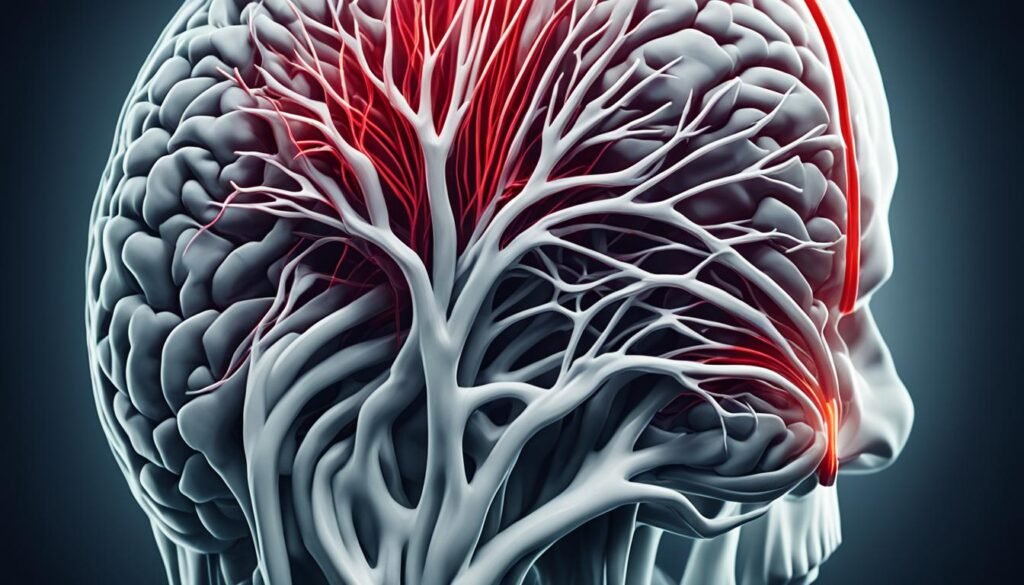
| Aura Symptoms | Key Features |
|---|---|
| Changes in speech | Altered speech patterns, difficulty finding words |
| Hearing changes | Impaired hearing, hypersensitivity to sound (phonophobia) |
| Vision changes | Visual disturbances such as blurred vision, seeing flashing lights or zigzag lines |
| Vertigo | Sensation of spinning or dizziness |
| Tinnitus | Ringing or buzzing sound in the ears |
| Double vision | Seeing two overlapping images |
| Impaired muscle control | Difficulty with coordination and fine motor skills |
| Reduced level of consciousness | Feeling disoriented, confused, or experiencing temporary loss of consciousness |
Etiology and Pathophysiology
The exact cause of basilar migraines is still unknown, but researchers believe that both genetic and environmental factors contribute to its development. Basilar migraines are now recognized as a subtype of migraines with aura and are commonly referred to as "migraines with brainstem aura."
The basilar artery migraine symptoms experienced during basilar migraines are believed to be caused by cortical spreading depression. This phenomenon refers to a self-propagating wave that spreads across the cerebral cortex due to the depolarization of neurons and glia. The firing of nerves in the brainstem is thought to play a significant role in triggering basilar migraines.
Contrary to previous beliefs, there is no proven evidence of vascular pathology involved in basilar migraines. Instead, it is the abnormal firing of nerves in the brainstem that leads to the characteristic aura symptoms.

Diagnosis and Evaluation
Diagnosing basilar migraine involves a thorough evaluation based on specific criteria outlined by the International Classification of Headache Disorders. These criteria are essential for distinguishing basilar migraine from other conditions with similar symptoms. The diagnosis relies on the presence of aura symptoms originating from the brainstem or both occipital hemispheres, the duration and characteristics of the aura symptoms, and the association of migraine without aura beginning during or within 1 hour of the aura.
While basilar migraine diagnosis is primarily based on clinical criteria, additional tests may be ordered to rule out other potential causes and ensure accurate evaluation. Imaging studies such as MRI or CT scans may be performed to exclude conditions like stroke, tumors, or infections that can present with similar symptoms. In some cases, an electroencephalogram (EEG) may be necessary to assess brain activity and rule out seizures, particularly in instances where confusion and decreased level of consciousness occur.
Evaluating basilar migraine requires a comprehensive approach that combines clinical assessment, patient history, and appropriate basilar type migraine diagnostic criteria tests. This ensures an accurate diagnosis and enables healthcare professionals to develop an effective treatment plan tailored to the individual's needs.
Treatment and Management
The basilar artery migraine treatment focuses on relieving symptoms and effectively managing the condition. Acute attacks are typically managed with medications such as NSAIDs (nonsteroidal anti-inflammatory drugs) and anti-emetics to alleviate pain and reduce nausea. Recent studies have shed light on the potential benefits of triptans and ergotamines in providing headache relief, despite their traditionally avoided status in basilar migraines due to concerns of increased cerebral ischemia.
Preventive therapy may be recommended for individuals experiencing frequent and disabling migraines. Medications like verapamil and topiramate are commonly prescribed for their ability to reduce the frequency and severity of migraines. However, it's essential to consult with a healthcare professional to determine the most suitable preventive treatment plan based on individual needs and medical history.
While medications play a critical role in managing basilar migraines, lifestyle modifications are equally important for long-term management and prevention. Making specific changes to your daily routine can help reduce the frequency of migraine attacks. It is recommended to:
- Avoid known triggers such as strong smells, loud noises, and certain foods.
- Practice stress management techniques, such as meditation and deep breathing exercises.
- Engage in regular exercise to promote overall well-being and reduce stress levels.
Incorporating these lifestyle modifications can significantly contribute to the prevention of migraine attacks and improve overall quality of life. Consulting with a healthcare professional is essential to develop an individualized treatment plan that addresses the specific needs and triggers of each person with basilar migraines.
Prognosis and Complications
Basilar migraines can have a significant impact on your daily life, as they tend to be more disabling than migraines without aura or migraines with typical aura. The severity and longer duration of symptoms can make it challenging to carry out your usual activities. However, there is some good news – the frequency of basilar migraines typically decreases with age, and they often evolve into more typical patterns.
While migraines with aura, including basilar migraines, have a slightly higher risk of stroke compared to migraines without aura, the specific risk remains unclear. It's important to note that the overall risk of stroke associated with migraines is still relatively low. However, certain factors such as smoking and the use of estrogen contraceptives can further increase this risk. Therefore, it's essential to address these risk factors and make necessary lifestyle changes to reduce the likelihood of complications.
Potential Complications of Basilar Migraines
Basilar migraines can have various complications or associated conditions. These may include:
- Increased risk of stroke
- Disruption of daily activities
- Interference with work or school
- Physical and emotional distress
- Decreased quality of life
These complications can be significant, underscoring the importance of effective migraine management and preventive strategies. By working closely with your healthcare provider and making the necessary lifestyle modifications, you can reduce the frequency and severity of basilar migraines, improving your overall well-being.
Managing Basilar Migraines for Better Prognosis
While basilar migraines can be challenging to deal with, a proactive approach to management can lead to a better prognosis. Here are some strategies that may help:
- Identify and manage triggers: Keep a headache diary to track potential triggers and avoid them as much as possible.
- Practice stress management: Engage in relaxation techniques, such as deep breathing, meditation, or yoga, to reduce stress levels.
- Consider preventive medications: Consult your healthcare provider about preventive medications to reduce the frequency of basilar migraines.
- Make lifestyle modifications: Maintain a balanced diet, exercise regularly, prioritize quality sleep, and limit alcohol and caffeine intake.
By taking these steps, you can actively participate in the management of basilar migraines and improve your overall prognosis. Remember, it's crucial to work closely with your healthcare provider to tailor a treatment plan that suits your specific needs and ensures the most effective management of your migraines.
Triggers and Prevention
Basilar migraines, like other types of migraines, can be triggered by various factors. Identifying these triggers and taking preventive measures can help reduce the frequency and severity of migraine attacks. Here are some common triggers to be aware of:
- Stress: Emotional and physical stress can trigger basilar migraines. Finding effective stress management techniques such as deep breathing exercises, meditation, or yoga can help prevent migraines.
- Alcohol and Caffeine: Excessive consumption of alcohol and caffeine can trigger migraines. Limiting or avoiding these substances may help prevent migraine attacks.
- Hormonal Changes: Fluctuations in hormone levels, particularly estrogen, can trigger migraines in some individuals. Understanding your hormonal patterns and discussing hormone-based treatments with your healthcare provider may be beneficial.
- Lack of Sleep: Irregular sleep patterns or lack of sufficient sleep can trigger migraines. Establishing a regular sleep schedule and practicing good sleep hygiene can contribute to preventing migraines.
- Strong Smells: Certain strong smells, such as perfumes, chemicals, or even strong cooking odors, can trigger migraines in some individuals. Minimizing exposure to these triggers or using scent-free products can help prevent migraines.
- Certain Foods: Some foods can act as triggers for migraines, including aged cheeses, processed meats, chocolate, and foods containing monosodium glutamate (MSG). Keeping a headache diary and avoiding known trigger foods can aid in preventing migraines.
In addition to identifying and avoiding triggers, preventive medications may be prescribed for individuals with frequent and disabling migraines. These medications are designed to reduce the frequency and severity of migraine attacks. Discussing preventive options with a healthcare professional can help determine the most suitable preventive medication for you.
Preventing Basilar Migraine Attacks
Preventing basilar migraines involves a combination of trigger management and lifestyle modifications. Here are some strategies to consider:
- Keep a Headache Diary: Tracking your migraines and potential triggers in a headache diary can help you identify patterns and avoid triggers in the future.
- Practice Stress Management: Finding effective stress management techniques, such as regular exercise, deep breathing exercises, or engaging in hobbies, can help reduce stress levels and prevent migraines.
- Maintain a Regular Sleep Schedule: Establishing a consistent sleep routine, including going to bed and waking up at the same time every day, can help regulate your body's internal clock and prevent migraines.
- Avoid Known Triggers: If certain triggers consistently lead to migraines, it's important to avoid or minimize exposure to them. This may include avoiding certain foods, limiting alcohol and caffeine intake, and managing environmental triggers.
By being proactive and making necessary lifestyle modifications, you can take control of your basilar migraines and reduce their impact on your daily life.

Lifestyle Modifications
In addition to trigger avoidance, making certain lifestyle modifications can help manage basilar migraines effectively. By incorporating the following habits into your everyday life, you can significantly reduce the frequency and severity of your migraines:
- Maintain a balanced diet, focusing on nutritious foods.
- Avoid the consumption of drugs and alcohol.
- Ensure you do not skip meals and maintain a regular eating schedule.
- Limit your caffeine intake, as it can act as a trigger for migraines.
- Avoid specific trigger foods such as dairy, wheat, chocolate, and citrus fruits.
- Engage in regular exercise to promote overall physical and mental well-being.
- Practice relaxation techniques, like deep breathing exercises and meditation, to reduce stress levels.
- Consider alternative therapies such as acupuncture and massage to alleviate migraine symptoms.
- Explore cognitive-behavioral therapy to develop effective coping strategies for dealing with migraines.
- Try biofeedback techniques to gain better control over your body's responses to stress and pain.
By embracing these lifestyle modifications, you can proactively manage your basilar migraines and improve your quality of life.
Conclusion
Basilar migraines, with their distinct brainstem aura symptoms, are a rare subtype of migraines. Although the exact cause is still unknown, various triggers such as stress, lack of sleep, certain foods, and hormonal changes can contribute to the occurrence of these migraines. Diagnosis is based on specific criteria and requires ruling out other potential causes to ensure accurate identification.
Treatment options for basilar migraines focus on relieving symptoms and may include medications, lifestyle modifications, and preventive therapies. By understanding their triggers and making appropriate lifestyle changes, individuals with basilar migraines can effectively manage their condition and reduce both the frequency and severity of their migraines.
It is crucial for people experiencing basilar migraines to work closely with their healthcare providers in order to develop a personalized treatment plan that suits their specific needs. By staying informed, seeking appropriate medical guidance, and adopting necessary lifestyle modifications, individuals can improve their quality of life and find relief from the symptoms of basilar migraines.
FAQ
What is a basilar migraine?
A basilar migraine, also known as migraine with brainstem aura, is a rare type of migraine that starts in the brainstem. It is characterized by aura symptoms that occur before or during the migraine episode.
What are the symptoms of a basilar migraine?
Symptoms of a basilar migraine can include changes in speech, hearing, and vision, as well as vertigo, tinnitus, double vision, impaired muscle control, and a reduced level of consciousness.
What causes basilar migraines?
The exact cause of basilar migraines is unknown, but it is believed to have a genetic and environmental component. Trigger factors such as stress, lack of sleep, certain foods, hormonal changes, and environmental stimuli can contribute to the occurrence of basilar migraines.
How are basilar migraines diagnosed?
The diagnosis of basilar migraine is based on specific criteria outlined by the International Classification of Headache Disorders. Imaging studies such as MRI or CT scans may be ordered to rule out other conditions, and an EEG may be necessary to rule out seizures.
What are the treatment options for basilar migraines?
Treatment options for basilar migraines include medications such as NSAIDs and anti-emetics to alleviate pain and nausea. Preventive therapy may be recommended for frequent and disabling migraines, and lifestyle modifications such as trigger avoidance and stress management can also help prevent migraine attacks.
How can basilar migraines be differentiated from other conditions?
Basilar migraines can mimic other conditions such as hemiplegic migraines, Meniere's disease, vestibular disorders, transient ischemic attacks (TIAs), strokes, brainstem AV malformations, tumors, and meningitis. A thorough evaluation, including a physical examination and appropriate imaging and testing, is necessary to differentiate basilar migraines from other potential causes of similar symptoms.
Are basilar migraines more severe than other types of migraines?
Basilar migraines can be more disabling than migraines without aura or migraines with typical aura due to the increased severity and longer duration of symptoms. However, the frequency of basilar migraines tends to decrease with age, and they often evolve into more typical patterns.
Can basilar migraines be prevented?
Basilar migraines can be triggered by various factors, including stress, alcohol, caffeine, hormonal changes, lack of sleep, strong smells, and certain foods. Identifying and avoiding these triggers, along with lifestyle modifications such as maintaining a balanced diet, regular exercise, and stress management, can help prevent migraine attacks.
What lifestyle modifications can help manage basilar migraines?
In addition to trigger avoidance, maintaining a balanced diet, avoiding drugs and alcohol, not skipping meals, limiting caffeine intake, and avoiding specific trigger foods like dairy, wheat, chocolate, and citrus fruits can all contribute to preventing migraine attacks. Regular exercise, relaxation techniques, acupuncture, massage, cognitive-behavioral therapy, and biofeedback techniques may also help reduce the frequency and severity of basilar migraines.
What is the prognosis for basilar migraines?
Basilar migraines can be disabling, but the frequency tends to decrease with age. While migraines with aura have a slightly higher risk of stroke compared to migraines without aura, the specific risk for basilar migraines is unclear. Risk factors like smoking and the use of estrogen contraceptives can further increase the risk of stroke, and risk factor modification should be reinforced.
Source Links
- https://www.webmd.com/migraines-headaches/basilar-artery-migraines-causes-symptoms-tests-and-treatments
- https://www.ncbi.nlm.nih.gov/books/NBK507878/
- https://www.medicalnewstoday.com/articles/320013
Effective Facial Nerve Paralysis Treatment Options
Facial nerve paralysis can be a challenging condition to treat. However, there are effective treatment options available that can help restore facial symmetry and improve facial function. In this article, we will explore the different treatment options for facial nerve paralysis and discuss their effectiveness in restoring facial movement and improving quality of life.
Key Takeaways:
- Facial nerve paralysis can be effectively treated with various treatment options.
- Treatment choice depends on the duration and severity of the paralysis.
- Surgical options include facial nerve decompression, nerve transfer procedures, and muscle transfers.
- Non-surgical options such as acupuncture and biofeedback training can also be beneficial.
- Collaborating closely with healthcare professionals is crucial for finding the most suitable treatment approach.
Diagnosing Facial Nerve Paralysis
Diagnosing facial nerve paralysis involves a comprehensive evaluation of your symptoms and a physical examination by a healthcare professional. This process allows doctors to determine the severity of the nerve damage and rule out other potential causes. In some cases, additional tests may be recommended to provide a more accurate diagnosis.
Physical Examination
During the physical examination, your doctor will assess your facial muscles, movement, and symmetry. They will carefully observe your ability to make facial expressions, close and open your eyes, and move your lips. Additionally, they may test your ability to taste, as the facial nerve also contributes to taste sensation in the front two-thirds of the tongue.
Specific Tests
To further evaluate facial nerve paralysis, your doctor may recommend specific tests to confirm the diagnosis and assess the extent of nerve damage. These tests include:
- Electromyography (EMG): This test measures the electrical activity of your facial muscles. It involves the insertion of small needles into the muscles to evaluate their function and response to nerve signals.
- Imaging Scans: Magnetic resonance imaging (MRI) and computerized tomography (CT) scans may be performed to visualize the facial nerve and rule out other possible causes of paralysis, such as tumors or structural abnormalities.
- Blood Tests: Blood tests can be used to rule out infections, autoimmune disorders, or other underlying medical conditions that could contribute to facial nerve paralysis.
These diagnostic tests help your healthcare team determine the most appropriate treatment plan for your specific condition.

| Diagnostic Tests | Purpose |
|---|---|
| Electromyography (EMG) | To measure the electrical activity of facial muscles and assess nerve function. |
| Imaging Scans (MRI/CT) | To visualize the facial nerve and rule out other potential causes of paralysis. |
| Blood Tests | To rule out infections and underlying medical conditions. |
Treating Acute Facial Paralysis
Acute facial paralysis refers to a temporary loss of facial muscle function that lasts for less than three weeks. When faced with this condition, surgical treatment options can be employed to help alleviate symptoms and restore facial movement. Two common surgical procedures used for the treatment of acute facial paralysis are facial nerve decompression and facial nerve repair.
Facial Nerve Decompression
Facial nerve decompression is a surgical procedure aimed at relieving pressure on the facial nerve. This pressure is often caused by viral infections such as Bell's palsy. By relieving the pressure, the surgical intervention can help restore facial function and hasten the recovery process.

Facial Nerve Repair
In cases where the facial paralysis is caused by direct nerve damage, facial nerve repair may be necessary. This surgery involves repairing or grafting the damaged facial nerve, allowing for the restoration of proper nerve function. Facial nerve repair can greatly improve facial movement and enhance overall recovery.
By opting for appropriate surgical interventions such as facial nerve decompression or facial nerve repair, individuals experiencing acute facial paralysis can benefit from improved facial function and a faster and more complete recovery process.
Managing Intermediate Duration Facial Paralysis
When faced with intermediate duration facial paralysis, lasting between three weeks and two years, nerve transfer procedures offer an effective treatment option. These procedures involve transferring nerves from unaffected areas of the body to the paralyzed facial muscles, such as the hypoglossal nerve, spinal accessory nerve, or branches of the trigeminal nerve. By restoring movement and function to the affected side of the face, nerve transfer procedures are instrumental in managing intermediate duration facial paralysis.
How Nerve Transfer Procedures Work
Nerve transfer procedures entail surgically connecting healthy nerves to the damaged facial nerves. This connection allows the healthy nerves to take over the function of the paralyzed facial muscles, facilitating improved facial movement and symmetry. By utilizing nerves from different areas of the body, nerve transfer procedures present a viable solution for managing intermediate duration facial paralysis.
During the surgery, the surgeon carefully selects the appropriate nerves to facilitate optimal facial function. The choice of nerve depends on factors such as the specific muscles affected and the severity of the paralysis. By strategically transferring nerves, the surgeon aims to restore movement and achieve the desired aesthetic outcome.
Post-surgery, patients undergo personalized rehabilitation to stimulate the newly transferred nerves and promote muscle reeducation. Through exercises and targeted therapies, individuals can enhance their facial control and regain natural movement.
The Benefits of Nerve Transfer Procedures
- Restoration of facial movement: By transferring nerves to the paralyzed facial muscles, nerve transfer procedures enable the restoration of facial movement, improving both functionality and expression.
- Enhanced facial symmetry: Nerve transfer procedures also contribute to improved facial symmetry, addressing the imbalances caused by the paralysis.
- Improved quality of life: The restoration of facial movement and symmetry can significantly enhance an individual's quality of life, boosting their confidence and self-esteem.
Nerve transfer procedures are a valuable treatment option for managing intermediate duration facial paralysis. These surgeries offer the potential for significant improvement in facial movement, symmetry, and overall well-being.

Image: Illustration depicting the management of intermediate duration facial paralysis.
Reconstructive Surgery for Chronic Facial Paralysis
In cases of chronic facial paralysis that lasts longer than two years, reconstructive surgery is often required. Reconstructive surgery aims to restore facial symmetry and improve facial function, allowing individuals to regain their confidence and quality of life.
The Techniques Used
There are two common techniques employed in reconstructive surgery for chronic facial paralysis: regional muscle transfer and free muscle transfer.
Regional muscle transfer involves moving a muscle from a nearby area to the paralyzed side of the face to restore movement. One example of regional muscle transfer is the temporalis muscle transfer, where the muscle from the temple area is used to replace the paralyzed facial muscles. This technique allows for the restoration of natural facial movements by utilizing the adjacent muscle's strength.
Free muscle transfer takes a different approach by using a muscle from another part of the body to replace the paralyzed facial muscles. The chosen muscle is detached at its origin and transferred to the face, providing new functionality and movement. Free muscle transfer is typically reserved for complex cases or when regional muscle transfer is not feasible.
Both regional muscle transfer and free muscle transfer have shown promising results in improving facial symmetry and function for individuals with chronic facial paralysis.
Benefits of Reconstructive Surgery
Reconstructive surgery for chronic facial paralysis offers several benefits, including:
- Improved facial symmetry
- Restoration of facial movement
- Enhanced quality of life
By addressing the root cause of the paralysis and utilizing muscle transfer techniques, reconstructive surgery can bring about remarkable improvements in facial aesthetics and functionality.
Static Techniques for Facial Reanimation
In addition to dynamic techniques, static techniques are another approach used for facial reanimation. While dynamic techniques focus on restoring active movement, static techniques aim to improve facial symmetry and aesthetics. These procedures can be particularly beneficial for individuals with limited to no active movement in their facial muscles.
Oculoplastic Surgery
Oculoplastic surgery is a type of procedure that focuses on the delicate structures around the eyes, including the eyelids and surrounding tissues. This technique can help improve eyelid function, reduce drooping, and enhance overall facial symmetry. Oculoplastic procedures may include eyelid lifts, eyelid suspension, or brow lifts to improve the appearance and balance of the eyes.
Eyelid Weights
Eyelid weights are commonly used in static facial reanimation to improve eyelid closure and symmetry. These weights are placed on the upper eyelid to help the affected eye close properly and reduce any noticeable drooping. By providing additional support to the eyelid, eyelid weights can enhance facial aesthetics and function.
Static Facial Suspension
Static facial suspension techniques involve the use of sutures or other materials to lift and suspend the affected side of the face. This helps to restore facial symmetry and counteract the drooping associated with facial muscle paralysis. Static facial suspension can be a valuable option for individuals seeking improvement in their facial appearance and overall facial balance.
These static techniques for facial reanimation offer individuals with facial paralysis alternative options for improving facial symmetry and aesthetics. While they may not restore active movement, they can significantly enhance self-confidence and quality of life. It's essential to consult with a qualified plastic or reconstructive surgeon to determine which static techniques are most appropriate for your specific condition.
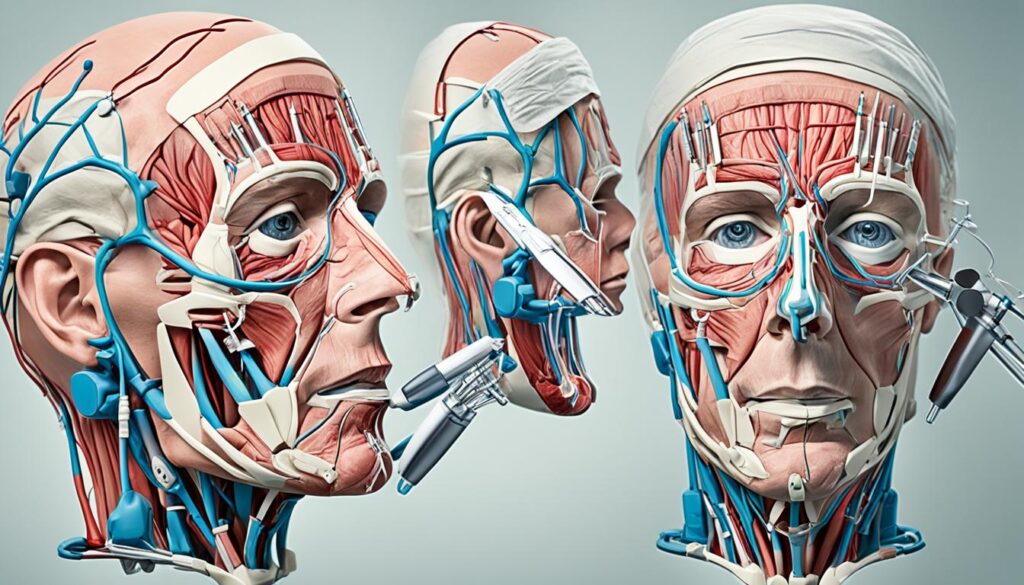
Non-surgical Options for Facial Paralysis Treatment
While surgery is often necessary for effective facial paralysis treatment, non-surgical options can also be beneficial. Acupuncture and biofeedback training are two non-invasive approaches that can complement surgical treatments and help improve facial function and well-being.
Acupuncture
Acupuncture is an ancient therapy originating from Traditional Chinese Medicine. It involves the insertion of thin needles into specific points of the body to stimulate nerves, muscles, and connective tissues. This practice has shown promising results in treating facial paralysis by promoting blood flow, reducing inflammation, and restoring balance to the facial muscles. Acupuncture can help relieve pain, enhance muscle tone, and improve facial symmetry.
Biofeedback Training
Biofeedback training is a technique that allows individuals to gain better control over their body's involuntary processes by providing real-time feedback on physiological responses. In the context of facial paralysis, biofeedback training focuses on enhancing the conscious control of facial muscles. It involves the use of sensors to monitor muscle activity, which is then displayed on a screen. By observing their muscle activity and receiving visual and auditory cues, individuals can learn to modify their facial muscle movements and improve their facial expressions and symmetry. Biofeedback training can be an effective tool in regaining control over facial muscles and improving overall facial function.
Both acupuncture and biofeedback training offer non-surgical alternatives for individuals with facial paralysis. These techniques can be used in conjunction with surgical treatments or as standalone therapies, depending on the severity and duration of the paralysis. It is important to consult with a qualified healthcare professional to determine the most suitable treatment approach for your specific case.
Let's take a look at the comparison table below for a clearer understanding of these non-surgical options:
Preparing for Facial Paralysis Treatment
Before undergoing any facial paralysis treatment, it's essential to be prepared. Proper preparation can help ensure a smooth and successful treatment process. Here are some important steps to take:
1. Document your Symptoms
Start by writing down any symptoms you have been experiencing related to your facial paralysis. This includes details about the onset, duration, and progression of the paralysis. Note any changes you have noticed in your facial movement, sensation, or muscle control. This information will help your doctor in the diagnosis and treatment planning process.
2. Provide Personal Information
During your consultation with the doctor, be prepared to provide key personal information. This includes details about your medical history, any previous surgeries, and any underlying health conditions you may have. Your doctor will also need information about any medications or supplements you are currently taking. Having this information readily available can help save time and facilitate effective communication with your doctor.
3. Make a Medication and Supplement List
Create a comprehensive list of all the medications and supplements you are currently taking. Include the names, dosages, and frequencies of each medication or supplement. This information is crucial for your doctor to evaluate any potential interactions or contraindications with the proposed treatment plan.
4. Bring a Support Person
Consider bringing along a family member or friend to your appointment. They can provide emotional support and help you remember important details discussed during the consultation. Having someone by your side can help alleviate any anxiety or stress associated with the treatment process.
5. Lifestyle and Home Remedies
In addition to medical treatment, there are lifestyle and home remedies that can complement your facial paralysis treatment plan. These remedies can help manage symptoms and enhance the effectiveness of the treatment. Here are some lifestyle and home remedies you can consider:
- Take pain relievers as recommended by your doctor to manage any facial pain or discomfort.
- Engage in physical therapy exercises to improve muscle strength and facial movement.
- Practice stress management techniques, such as deep breathing exercises or meditation, to reduce stress levels and promote overall well-being.
- Apply warm compresses to your face to relieve muscle tension and promote relaxation.
- Eat a balanced diet rich in nutrients to support overall health and healing.
Remember to consult your doctor before starting any new lifestyle or home remedy, as they can provide guidance specific to your condition and treatment plan.
By following these steps and being well-prepared, you can maximize the effectiveness of your facial paralysis treatment and optimize your chances of a successful outcome.

Conclusion
Facial nerve paralysis can be a challenging condition to live with, but there are effective treatment options available that can significantly improve your quality of life. The choice of treatment depends on the duration and severity of your paralysis, as well as your individual circumstances and preferences.
Surgical options, such as facial nerve decompression, nerve transfer procedures, and muscle transfers, offer the possibility of restoring facial movement and symmetry. These procedures involve relieving pressure on the facial nerve, transferring nerves from unaffected areas of the body to the paralyzed facial muscles, or using muscles from other parts of the body to replace the paralyzed ones.
Non-surgical options, including acupuncture and biofeedback training, can also be beneficial in conjunction with surgical treatments. Acupuncture can stimulate nerves and muscles, providing some relief and improving facial function. Biofeedback training helps you gain better control over your facial muscles through the use of your thoughts. It's important to work closely with healthcare professionals to determine the most suitable treatment approach for your unique situation.
FAQ
What are some effective treatment options for facial nerve paralysis?
Effective treatment options for facial nerve paralysis include facial nerve decompression, facial nerve repair, nerve transfer procedures, muscle transfers, oculoplastic procedures, static facial suspension, acupuncture, and biofeedback training.
How is facial nerve paralysis diagnosed?
Facial nerve paralysis is diagnosed through a thorough evaluation of symptoms and a physical examination. Specific tests like electromyography (EMG), magnetic resonance imaging (MRI), computerized tomography (CT), and blood tests may also be recommended.
What are the surgical treatment options for acute facial paralysis?
Surgical treatment options for acute facial paralysis include facial nerve decompression to relieve pressure on the nerve and facial nerve repair to directly repair or graft the damaged nerve.
How is intermediate duration facial paralysis managed?
Intermediate duration facial paralysis can be managed through nerve transfer procedures, in which nerves from unaffected areas of the body are transferred to the paralyzed facial muscles to restore movement and function.
What types of reconstructive surgery are used for chronic facial paralysis?
Reconstructive surgery for chronic facial paralysis may involve regional muscle transfer, such as the temporalis muscle transfer, or free muscle transfer, where a muscle from another part of the body is used to replace the paralyzed facial muscles.
What are static techniques for facial reanimation?
Static techniques for facial reanimation focus on improving facial symmetry and aesthetics. Procedures like oculoplastic surgery, eyelid weights, and static facial suspension can help improve eyelid function, reduce drooping, and enhance facial symmetry.
Are there non-surgical options for facial paralysis treatment?
Yes, non-surgical options for facial paralysis treatment include acupuncture, which stimulates nerves and muscles, and biofeedback training, which helps individuals gain better control over their facial muscles through the use of their thoughts.
How should I prepare for facial paralysis treatment?
Before undergoing any facial paralysis treatment, it's essential to be prepared by writing down symptoms, providing personal information, making a list of medications and supplements, and bringing along a support person. Lifestyle and home remedies like pain relievers and physical therapy exercises can also help manage symptoms.
What are the most important aspects to consider when choosing a treatment option for facial nerve paralysis?
The choice of treatment for facial nerve paralysis depends on the duration and severity of the paralysis, as well as individual circumstances and preferences. Consulting with healthcare professionals is crucial to find the most suitable treatment approach for each person's unique situation.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2440925/
- https://www.mayoclinic.org/diseases-conditions/bells-palsy/diagnosis-treatment/drc-20370034
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2671829/
Effective Bell's Palsy Physical Therapy Guide
Bell's palsy, a temporary form of facial paralysis, can be debilitating and significantly impact your daily life. Physical therapy is a crucial component of Bell's palsy treatment, helping to improve facial strength and promote recovery. If you experience facial weakness, seeking medical care immediately is important as it can also indicate more severe conditions like a stroke. Physical therapists, who are movement experts, can provide hands-on care, educate you about your condition, and prescribe specific exercises to regain facial strength and function.
Key Takeaways:
- Bell's palsy is a temporary form of facial paralysis that requires treatment.
- Physical therapy plays a crucial role in improving facial strength and promoting recovery.
- Seek immediate medical care for facial weakness to rule out more severe conditions.
- Physical therapists are movement experts who can provide hands-on care and prescribe exercises.
- Work closely with a licensed physical therapist for personalized treatment and optimal results.
What Is Bell's Palsy? Understanding the Condition
Bell's palsy is a sudden and temporary form of facial paralysis that occurs when the facial nerve becomes inflamed or damaged. It is characterized by the weakness or paralysis of the muscles on one side of the face.
The exact cause of Bell's palsy is often unclear, but it is thought to be related to viral infections, particularly the herpes simplex virus (HSV). This inflammation of the facial nerve can result in various symptoms such as facial asymmetry, difficulty closing the eye, drooping of the mouth, and loss of taste.
While the exact mechanism behind the development of Bell's palsy is not fully understood, it is believed that the herpes simplex virus causes an inflammatory response in the facial nerve, leading to the onset of facial paralysis.

In most cases, Bell's palsy improves naturally within six months, as the inflammation subsides and the facial nerve begins to heal. However, some individuals may experience long-term effects or may not fully recover their pre-palsy facial functionality.
Understanding the causes and symptoms of Bell's palsy is essential for timely diagnosis and appropriate treatment. The next section will explore the signs and symptoms of Bell's palsy in more detail.
Signs and Symptoms of Bell's Palsy
Bell's palsy is characterized by a range of noticeable bell's palsy symptoms that can significantly affect facial function and appearance. Recognizing these signs is crucial in seeking prompt medical attention and initiating appropriate treatment. The following are the common symptoms associated with Bell's palsy:
Facial Weakness and Paralysis
The most prominent symptom of Bell's palsy is the sudden onset of facial weakness or paralysis on one side of the face. This weakness can lead to difficulties in performing simple tasks such as smiling, blinking, and closing the affected eye. The severity of the weakness may vary from mild to complete facial paralysis.
Drooping of the Mouth and Eyelid
In addition to facial weakness, Bell's palsy often causes drooping of the mouth or eyelid on the affected side. This drooping may create an asymmetrical appearance and affect speech and eating patterns, impacting daily life activities.
Loss of Taste
Another common symptom of Bell's palsy is the loss of taste on the front two-thirds of the tongue. This can significantly affect a person's enjoyment of food and beverages. The sense of taste is closely linked to the sense of smell, so some individuals with Bell's palsy may also experience changes in their ability to detect and identify different smells.
Increased Sensitivity to Sound
Bell's palsy can also cause increased sensitivity to sound in one ear. Individuals may notice that certain sounds or noises are louder or more bothersome in the ear on the affected side.
Eye Closure and Corneal Protection
Due to facial weakness, individuals with Bell's palsy may experience difficulty fully closing the eye on the affected side. This can lead to eye dryness, irritation, and potentially damage to the cornea. It is essential to take appropriate measures, such as using eye drops and wearing protective eyewear, to prevent complications and ensure proper eye care.
Recognizing these signs and symptoms is crucial in differentiating Bell's palsy from other conditions that may cause similar facial weakness. If you experience any of these symptoms, it is recommended to seek medical attention promptly for a proper diagnosis and appropriate treatment.
| Symptoms | Description |
|---|---|
| Facial Weakness and Paralysis | Sudden weakness or paralysis on one side of the face, leading to difficulties in smiling, blinking, and closing the eye. |
| Drooping of the Mouth and Eyelid | Drooping of the mouth or eyelid on the affected side, causing asymmetry and impacting speech and eating patterns. |
| Loss of Taste | Loss of taste on the front two-thirds of the tongue, affecting the enjoyment of food and beverages. |
| Increased Sensitivity to Sound | Heightened sensitivity to sound in one ear, with certain noises or sounds appearing louder or more bothersome. |
| Eye Closure and Corneal Protection | Difficulty in fully closing the eye on the affected side, leading to dryness, irritation, and potential corneal damage. |
What Causes Bell's Palsy?
Bell's palsy is a condition characterized by the sudden paralysis or weakness of facial muscles on one side of the face. While the exact cause is not fully understood, it is believed to be associated with several factors, including viral infections, inflammation of the facial nerve, and the immune system's response. Let's take a closer look at these potential Bell's Palsy causes:
Viral Infections:
One of the main causes of Bell's palsy is viral infections, particularly the herpes simplex virus (HSV). These viral infections can lead to inflammation and swelling of the facial nerve, resulting in the characteristic facial paralysis.
Facial Nerve Inflammation:
Bell's palsy is often attributed to the inflammation or compression of the facial nerve, which controls the muscles responsible for facial expressions. This inflammation disrupts the normal functioning of the nerve, leading to the development of Bell's palsy.
Immune System Response:
The immune system plays a crucial role in the development of Bell's palsy. It is believed that an abnormal immune system response to viral infections or other stimuli can trigger inflammation and damage to the facial nerve, resulting in the onset of Bell's palsy symptoms.
Other Factors:
In addition to viral infections, facial nerve inflammation, and immune system response, other factors can contribute to the development of Bell's palsy. These include hereditary factors, environmental factors such as exposure to cold weather or wind, as well as autoimmune reactions.
While viral infections, especially the herpes simplex virus, are commonly associated with Bell's palsy, it's important to note that multiple factors may contribute to its development. Further research is needed to fully understand the complex causes of Bell's palsy.

Diagnosis of Bell's Palsy
The diagnosis of Bell's palsy is essential to determine the appropriate treatment and rule out other potential causes of facial paralysis. To diagnose Bell's palsy, a medical professional will conduct a thorough assessment that involves gathering a detailed medical history and performing a physical examination.
During the medical history interview, the doctor will ask about the onset and progression of symptoms, recent illnesses, exposure to viruses, and any other relevant factors. This information helps in identifying patterns and potential triggers that may be associated with Bell's palsy.
Following the medical history, a physical examination is conducted to evaluate facial muscle strength, symmetry, and the ability to perform various facial expressions. The doctor will assess the degree of weakness or paralysis on one side of the face and observe any changes in muscle tone and facial symmetry.
In some cases, additional tests may be ordered to rule out other causes of facial paralysis. These tests may include blood tests, imaging studies such as MRI or CT scans, and nerve conduction studies. These tests help in excluding conditions like stroke, tumors, trauma, and neurological disorders that may also present with facial paralysis.
Once other potential causes are ruled out, and a thorough assessment is completed, the medical professional can confidently diagnose Bell's palsy.
| Diagnosis Process | Key Steps |
|---|---|
| Medical History | - Gathering information about symptoms, illnesses, and exposure to viruses. - Establishing the timeline and progression of symptoms. - Identifying potential triggers. |
| Physical Examination | - Assessing facial muscle strength, symmetry, and mobility. - Evaluating the ability to perform various facial expressions. - Observing changes in muscle tone and facial symmetry. |
| Additional Tests | - Conducting blood tests to rule out other conditions. - Ordering imaging studies (MRI or CT scans) to assess the facial nerve and exclude structural abnormalities. - Nerve conduction studies to evaluate nerve function. |
Through a comprehensive evaluation process, a medical professional can make an accurate diagnosis of Bell's palsy, enabling timely and appropriate treatment to be initiated.

How Bell's Palsy Can Be Treated With Physical Therapy
Physical therapy plays a crucial role in the treatment of Bell's palsy. It helps manage and improve muscle weakness and facial asymmetry caused by the condition. With the guidance of a licensed and experienced physical therapist, a personalized treatment plan can be designed to address the specific needs of each individual.
Facial muscle strengthening exercises and facial exercises are key components of physical therapy for Bell's palsy. These exercises focus on improving muscle strength, coordination, and range of motion in the affected areas of the face. By regularly performing these exercises, the facial muscles can regain their strength and help restore facial symmetry.
In addition to muscle strengthening exercises, biofeedback techniques can be used to enhance muscle activation and coordination. Biofeedback provides real-time information on muscle activity, allowing individuals to learn how to control their facial muscles more effectively.
Furthermore, eye protection and care are important aspects of physical therapy for Bell's palsy. The inability to fully close the eye on the affected side can lead to eye damage and dryness. Protecting the eye with eye drops, ointments, or a patch can help prevent complications and promote healing.
Physical therapy for Bell's palsy should always be carried out under the guidance of a licensed physical therapist. They will assess the individual's condition and prescribe the appropriate exercises and techniques tailored to their needs. Regular sessions with the physical therapist, coupled with consistent at-home exercises, can significantly improve facial strength, function, and overall quality of life for individuals with Bell's palsy.
Physical Therapy Exercises for Bell's Palsy
Physical therapy exercises can be highly effective in improving facial muscle strength, coordination, and movement on the affected side of the face for individuals with Bell's palsy. These exercises, when performed under the guidance of a physical therapist, can help facilitate a faster and more comprehensive recovery. Consistency and gradual progression are key to achieving optimal results.
Eye Blinking Exercise
Bell's palsy exercises often include eye blinking exercises to strengthen the muscles involved in blinking and protect the eye from dryness and potential damage. Here's a simple eye blinking exercise you can try:
- Close your unaffected eye.
- Blink your affected eye gently and progressively increase the speed and intensity of the blinking.
- Repeat this exercise for a few minutes, taking short breaks if needed.
Smile Exercise
Smile exercises can help improve facial symmetry and strengthen the muscles responsible for smiling.
- Relax your facial muscles.
- Attempt to smile as wide as possible, lifting the corners of your mouth towards your ears.
- Hold the smile for a few seconds, then relax your facial muscles.
- Repeat this exercise several times, gradually increasing the duration of each smile.
Eye Closure Resistance Exercise
Eye closure resistance exercises aim to strengthen the muscles involved in fully closing the affected eye. This exercise can help prevent eye dryness and protect the eye from potential damage. Here's how to perform it:
- Sit upright and relax your facial muscles.
- Use your fingers to gently apply resistance against your affected eyelid while attempting to close it fully.
- Hold the resistance for a few seconds, then relax your facial muscles.
- Repeat this exercise for several repetitions, gradually increasing the intensity of the resistance.
Eyebrow Raise Exercise
The eyebrow raise exercise targets the muscles responsible for raising the eyebrows, helping to improve facial symmetry and expression.
- Relax your facial muscles.
- Attempt to raise your affected eyebrow as high as possible.
- Hold the raised position for a few seconds, then relax your facial muscles.
- Repeat this exercise multiple times, gradually increasing the duration of each eyebrow raise.
Cheek Puff Exercise
The cheek puff exercise targets the muscles used for puffing the cheeks, aiding in facial muscle coordination and symmetry.
- Relax your facial muscles.
- Puff out your affected cheek as much as possible, feeling the tension in the muscles.
- Hold the puff for a few seconds, then relax your facial muscles.
- Repeat this exercise for several repetitions, gradually increasing the duration of each cheek puff.
Tongue and Lip Mobility Exercise
Tongue and lip mobility exercises can improve facial muscle coordination and control. Here's one exercise you can try:
- Relax your facial muscles.
- Move your tongue from one side of your mouth to the other, touching the inside of each cheek.
- Purse your lips and move them from side to side, feeling the stretching and contraction of the muscles.
- Repeat this exercise for several repetitions, gradually increasing the speed and range of motion.
Remember, it is essential to perform these exercises gently and consistently under the guidance of a physical therapist. Over time, as the facial muscles regain strength and coordination, you can gradually increase the repetitions and intensity of the exercises. Stay dedicated and patient, as consistent practice can significantly contribute to your Bell's palsy recovery.
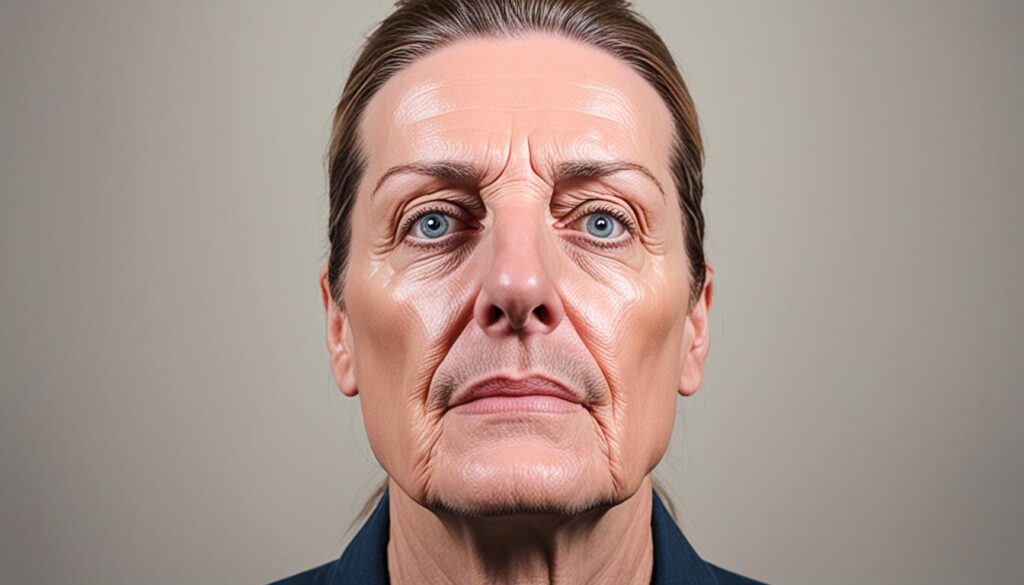
After Bell's Palsy Recovery
After recovering from Bell's palsy, you may experience various emotions and adjustments. While many individuals achieve near-complete recovery, some may still have residual effects or slight facial differences. It's important to remember that the recovery process for Bell's palsy can take time, and your facial muscles may continue to improve and adapt for several months.
The residual effects of Bell's palsy, such as mild weakness, muscle stiffness, or subtle facial asymmetry, are typically minimal and may not be noticeable to others. It's essential to practice patience and understanding during this recovery phase. Allow your body the time it needs to heal and adapt fully.
Engaging in activities that promote relaxation and stress reduction can support your recovery process. Consider incorporating techniques such as deep breathing exercises, meditation, and gentle facial massages into your daily routine. These practices can help relax your facial muscles, alleviate tension, and promote overall well-being.
Remember, everyone's recovery from Bell's palsy is unique, so be kind to yourself and celebrate each small improvement along the way. With time and patience, you can regain your facial strength and confidently embrace your renewed appearance.
Ways to Support Your Bell's Palsy Recovery:
- Practice patience and give yourself time for a complete recovery.
- Engage in stress-reducing activities such as deep breathing exercises and meditation.
- Incorporate gentle facial massages to relax and promote circulation in your facial muscles.
- Celebrate each small improvement in your facial strength and mobility.
Personalized Care and Support:
If you have any concerns or questions during your recovery journey, don't hesitate to consult with your healthcare provider or physical therapist. They can offer guidance, answer your queries, and provide further assistance specific to your unique situation.
Support from loved ones can also play a crucial role in your recovery. Openly communicate your needs and feelings to those around you, helping them understand and provide the support you require. Remember, you are not alone in your journey towards regaining complete facial strength and function.
| Key Aspects of Bell's Palsy Recovery | How It Impacts Recovery |
|---|---|
| Residual Effects | Minimal and may include mild weakness, muscle stiffness, or subtle facial asymmetry |
| Facial Differences | Varies among individuals and may not be noticeable to others |
| Time and Patience | Recovery can take several months as facial muscles continue to improve and adapt |
| Supportive Techniques | Relaxation exercises, facial massages, and stress reduction practices can aid recovery |
Seeking the Right Physical Therapist for Bell's Palsy Treatment
When it comes to Bell's palsy treatment, finding the right physical therapist is crucial for optimal results. It is important to seek a physical therapist with experience and expertise in treating neurological conditions, specifically Bell's palsy.
Physical therapists who have a neurological focus or are board-certified clinical specialists in neurologic physical therapy possess advanced knowledge and skills necessary for effectively addressing the unique challenges posed by Bell's palsy.
One way to find a physical therapist with the right expertise is by using the American Physical Therapy Association's Find a PT tool. This online resource allows you to search for physical therapists in your area who have specific clinical expertise, such as Bell's palsy treatment.
In addition, seeking recommendations from healthcare providers, friends, or family members who have undergone physical therapy for Bell's palsy can provide valuable insights and help you find a trusted and qualified physical therapist.
By selecting a physical therapist with a neurological focus and relevant expertise, you can ensure that you receive the specialized care and guidance needed to maximize your recovery and improve your quality of life.
The Efficacy of Physical Therapy for Bell's Palsy
Research studies have shown that physical therapy is highly effective in treating Bell's palsy and improving facial strength and function. Through a combination of targeted exercises and techniques, physical therapy helps promote facial muscle rehabilitation and enhance overall facial coordination.
Facial muscle strengthening exercises play a crucial role in restoring muscle tone and preventing muscle atrophy. These exercises, designed specifically for Bell's palsy patients, focus on gradually increasing muscle strength and improving facial symmetry. By regularly performing these exercises, individuals with Bell's palsy can regain control over their facial movements and experience significant improvements in their condition.
In addition to facial muscle strengthening exercises, facial expressions training and biofeedback techniques have also shown promising results in promoting recovery. Facial expressions training helps individuals regain control over their facial muscles, allowing them to effectively communicate emotions and expressions. Biofeedback techniques, on the other hand, use advanced technology to provide real-time information about muscle activity, helping patients develop greater control and coordination of their facial muscles.
Working with a licensed physical therapist is essential to ensure the effectiveness of the treatment. A physical therapist will conduct a thorough evaluation of the patient's condition, develop a personalized treatment plan, and provide guidance throughout the rehabilitation process. By closely following the prescribed treatment plan, patients can maximize the benefits of physical therapy and achieve optimal results.
Overall, physical therapy offers a comprehensive and evidence-based approach to Bell's palsy treatment. It not only aids in facial muscle rehabilitation but also improves muscle tone, enhances coordination, and restores facial symmetry. For individuals with Bell's palsy, physical therapy is a valuable intervention that plays a vital role in promoting recovery and improving quality of life.
Summary of Physical Therapy Techniques for Bell's Palsy Treatment
| Physical Therapy Technique | Description |
|---|---|
| Facial Muscle Strengthening Exercises | Targeted exercises that focus on improving muscle strength, tone, and coordination in the facial muscles. |
| Facial Expressions Training | Aims to retrain facial muscles to produce natural and expressive facial movements, enhancing communication and emotional expression. |
| Biofeedback Techniques | Uses advanced technology to provide real-time feedback on muscle activity, helping patients develop control and coordination of their facial muscles. |
Conclusion
In conclusion, physical therapy plays a crucial role in the recovery of Bell's palsy. By targeting facial weakness and promoting symmetrical movements, physical therapy can significantly improve facial strength and function. It is important to seek immediate medical care if you experience any facial weakness, as it may indicate more severe conditions. Working with a licensed physical therapist and following a personalized treatment plan can lead to enhanced facial strength, reduced asymmetry, and an improved quality of life for individuals with Bell's palsy.
Physical therapy offers numerous benefits for Bell's palsy recovery. It helps improve muscle strength, coordination, and range of motion in the face. Through facial muscle strengthening exercises and biofeedback techniques, physical therapy can enhance facial symmetry and promote optimal facial function. Alongside medical care, physical therapy can contribute to improved facial strength, reduced asymmetry, and an overall better quality of life.
In summary, physical therapy is a vital component of the treatment plan for Bell's palsy. By addressing facial weakness and incorporating targeted exercises, physical therapists can help patients regain facial strength and improve their quality of life. If you or someone you know is experiencing Bell's palsy, it is essential to consult with a licensed physical therapist to develop a tailored treatment plan that supports recovery and enhances facial function.
FAQ
What is Bell's Palsy?
Bell's palsy is a sudden and temporary form of facial paralysis that occurs when the facial nerve becomes inflamed or damaged.
What are the signs and symptoms of Bell's Palsy?
Common symptoms of Bell's palsy include facial asymmetry, difficulty closing the eye, drooping of the mouth, and loss of taste.
What causes Bell's Palsy?
The exact cause of Bell's palsy is not completely understood, but it is believed to be associated with viral infections, particularly the herpes simplex virus.
How is Bell's Palsy diagnosed?
The diagnosis of Bell's palsy is primarily based on a clinical evaluation of the symptoms and a physical examination conducted by a medical professional.
How can Bell's Palsy be treated with physical therapy?
Physical therapy plays a crucial role in the treatment of Bell's palsy by helping to manage and improve muscle weakness and facial asymmetry.
What are the physical therapy exercises for Bell's Palsy?
Physical therapy exercises for Bell's palsy are designed to improve facial muscle strength, coordination, and movement on the affected side of the face.
What can I expect after Bell's Palsy recovery?
After recovering from Bell's palsy, it is common to experience various feelings and adjustments. Residual effects such as mild weakness or muscle stiffness are usually minimal and may not be noticeable to others.
How do I find the right physical therapist for Bell's Palsy treatment?
When seeking a physical therapist for Bell's palsy treatment, it is important to consider their experience and expertise in treating neurological conditions.
Is physical therapy effective in treating Bell's Palsy?
Research studies have shown that physical therapy can be effective in improving facial strength and function in individuals with Bell's palsy.
What are the benefits of physical therapy for Bell's Palsy?
Physical therapy can enhance facial strength and function, reduce asymmetry, and improve the overall quality of life for individuals with Bell's palsy.
Source Links
- https://www.choosept.com/guide/physical-therapy-guide-bells-palsy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9510940/
- https://www.miraclerehabclinic.com/blog/physical-therapy-for-bells-palsy
Effective Brown-Sequard Treatment Options
Brown-Séquard syndrome is a rare neurological condition that can have a significant impact on your daily life. If you or someone you know has been diagnosed with this condition, it's important to understand that there are treatment options available to help manage symptoms and improve your quality of life.
Managing the symptoms of Brown-Séquard syndrome requires a comprehensive approach that may include physical therapy, occupational therapy, orthotics, Botox injections, speech therapy, and home exercises. These treatment options aim to promote neuroplasticity and enhance your functional recovery.
Key Takeaways:
- Brown-Séquard syndrome is a rare neurological condition that causes muscle weakness and loss of sensation on opposite sides of the body.
- Treatment options for Brown-Séquard syndrome focus on managing symptoms and improving quality of life.
- Physical therapy, occupational therapy, orthotics, Botox injections, speech therapy, and home exercises may be part of the treatment plan.
- Consistent practice and therapy can lead to improved mobility and functional independence.
- Working with healthcare professionals to create a personalized treatment plan is essential for optimal outcomes.
Understanding Brown-Séquard Syndrome
Brown-Séquard syndrome is a rare neurological condition that affects the spinal cord, resulting in muscle weakness or paralysis on one side of the body and a loss of sensation on the opposite side. This condition, often caused by spinal cord injury or inflammation, is characterized by the interruption of nerve signals between the brain and the body.
Individuals with Brown-Séquard syndrome experience specific neurological impairments due to the location of the spinal cord injury. The damage usually occurs on one side of the spinal cord, leading to a combination of motor deficits and sensory loss.
Neurological Impairments of Brown-Séquard Syndrome
The specific neurological impairments experienced by individuals with Brown-Séquard syndrome include:
- Muscle Weakness or Paralysis: The affected side of the body experiences a reduction in muscle strength or complete paralysis. This can significantly impact mobility and daily activities.
- Loss of Sensation: The opposite side of the body may experience a decreased or complete loss of sensation. This includes touch, temperature, and proprioception (awareness of body position).
- Sensory Deficits: Individuals may also experience sensory deficits, such as a partial preservation of deep sensation or loss of specific sensory modalities.
The neurological impairments of Brown-Séquard syndrome can vary depending on the level and extent of the spinal cord injury. It is essential for individuals with this condition to work closely with healthcare professionals to develop a comprehensive treatment plan that addresses their specific needs and goals.
Causes of Brown-Séquard Syndrome
Understanding the causes of Brown-Séquard syndrome Symptoms is crucial for diagnosing and treating this rare condition. The syndrome typically arises from damage to the spinal cord, which can occur due to various factors including:
- Trauma: Brown-Séquard syndrome often occurs as a result of traumatic spinalcord injury, such as gunshot or stab wounds, that disrupt the normal functioning of the spinal cord.
- Inflammation: Inflammation or pinching of the spinal cord can also lead to the development of Brown-Séquard syndrome, affecting the transmission of nerve signals.
- Spinal Cord Tumors: Tumors in the spinal cord can put pressure on the nerves, resulting in a range of neurological symptoms, including Brown-Séquard syndrome.
- Inadequate Blood Flow: Insufficient blood flow to the spinal cord, known as ischemia, can damage the nerve fibers and cause Brown-Séquard syndrome.
- Infectious Diseases: Certain infectious diseases like tuberculosis can affect the spinal cord and lead to the development of Brown-Séquard syndrome.
- Inflammatory Diseases: Inflammatory conditions, such as multiple sclerosis, can trigger inflammation in the spinal cord, potentially causing Brown-Séquard syndrome.
It is important to note that the exact cause of Brown-Séquard syndrome can vary from case to case. Comprehensive medical evaluation and diagnostic tests are necessary to determine the underlying cause and develop an appropriate treatment plan.
Symptoms of Brown-Séquard Syndrome
Brown-Séquard syndrome Symptoms is characterized by several distinct symptoms that can significantly impact an individual's daily life. Understanding these symptoms is crucial for timely diagnosis and effective management of the condition.
Muscle Weakness and Paralysis
One of the primary symptoms of Brown-Séquard syndrome is muscle weakness or paralysis on one side of the body. This asymmetric weakness affects the voluntary movement of the limbs and can vary in severity depending on the extent of spinal cord damage.
Loss of Sensation
In addition to muscle weakness, individuals with Brown-Séquard syndrome experience a loss of sensation on the opposite side of the body. This sensory deficit affects the perception of touch, temperature, and pain, making it challenging to detect stimuli and respond appropriately.
Sensory Deficits
Brown-Séquard syndrome can also lead to sensory deficits, particularly a loss of deep sensation. This includes proprioception, the ability to perceive the position and movement of body parts, and vibratory sensation. These deficits can further impair coordination, balance, and fine motor skills.
Individuals with Brown-Séquard syndrome may face various challenges in their daily lives due to these symptoms. Activities such as walking, self-care, and maintaining balance can become difficult or even impossible without assistance or appropriate therapeutic interventions.
Moreover, it is crucial to note that individuals with Brown-Séquard syndrome may be at risk of developing secondary effects. These may include spasticity, a condition characterized by muscle stiffness and involuntary contractions, as well as pressure ulcers and muscle atrophy due to immobility.

| Symptom | Description |
|---|---|
| Muscle Weakness and Paralysis | Asymmetric weakness or paralysis on one side of the body, affecting voluntary movement. |
| Loss of Sensation | Absence or reduced perception of touch, temperature, and pain on the opposite side of the body. |
| Sensory Deficits | Loss of deep sensation, including proprioception and vibratory perception, affecting coordination and balance. |
Prognosis and Recovery Outlook
The prognosis for individuals with Brown-Séquard syndrome is generally favorable. Studies have shown that 75-90% of individuals are able to recover their walking abilities by the time they are discharged from rehabilitation. This is due to the ability of the central nervous system to utilize neuroplasticity, allowing the spinal cord to make adaptive changes and rewire neural connections. With consistent practice and therapy, individuals with Brown-Séquard syndrome can improve their mobility and quality of life.
Walking Abilities and Neuroplasticity
The recovery of walking abilities in individuals with Brown-Séquard syndrome is attributed to the remarkable phenomenon of neuroplasticity. Neuroplasticity refers to the brain's ability to reorganize and rewire its neural connections, allowing alternate pathways to compensate for damaged areas. With focused rehabilitation and therapeutic interventions, the spinal cord can undergo adaptive changes, enabling individuals to regain control over their leg muscles and improve their walking abilities.
Neuroplasticity plays a crucial role in the recovery outlook for individuals with Brown-Séquard syndrome. The brain can form new neural connections and strengthen existing ones, facilitating motor function recovery and sensory improvements. Through targeted therapies and exercises that promote neuroplasticity, such as gait training and repetitive motion exercises, individuals can enhance their neural reorganization and regain functional abilities.
Rehabilitation programs that emphasize neuroplasticity can also help individuals with Brown-Séquard syndrome overcome specific challenges related to walking, such as gait abnormalities, muscle weakness, and coordination difficulties. By engaging in regular physical therapy sessions, individuals can gradually improve their balance, stability, and muscle control, leading to a significant enhancement in their walking abilities.
It is important to note that the recovery outlook may vary for each individual with Brown-Séquard syndrome, depending on factors such as the extent of spinal cord damage, the presence of underlying conditions, and the commitment to consistent therapy and exercise. While not everyone may achieve complete recovery, with a comprehensive rehabilitation approach that harnesses neuroplasticity, most individuals can experience notable improvements in their mobility and regain a level of independence.
Treatment Options for Brown-Séquard Syndrome
When it comes to managing Brown-Séquard syndrome, there are various treatment options available to promote neuroplasticity and improve functional recovery. These options focus on addressing specific symptoms and helping individuals regain mobility and independence.
Physical Therapy
Physical therapy plays a crucial role in the treatment of Brown-Séquard syndrome. It involves targeted exercises and techniques to improve motor control and strength on the affected side of the body. Physical therapists work closely with patients to develop personalized exercise programs designed to address their specific needs.
Occupational Therapy
Occupational therapy aims to maximize functional independence for individuals with Brown-Séquard syndrome. Therapists help patients learn compensatory strategies to overcome challenges and perform daily activities. Occupational therapy may involve training in adaptive techniques and the use of assistive devices.
Orthotics and Botox Injections
Orthotics, such as braces or splints, may be recommended to provide stability and support for weakened muscles. Botox injections can also be used to reduce spasticity and improve muscle function. These interventions are often employed in conjunction with physical and occupational therapy to enhance the effectiveness of treatment.
Speech Therapy
In some cases, individuals with Brown-Séquard syndrome may experience respiratory difficulties, affecting their ability to speak and swallow. Speech therapy can help address these issues by providing techniques to improve respiratory control, communication, and swallowing abilities.
Home Exercise
Continuing rehabilitation efforts at home is vital for the long-term management of Brown-Séquard syndrome. Home exercise programs, designed by therapists, help individuals maintain and further improve their mobility and strength. These exercises can be tailored to the specific needs and capabilities of each patient.
By combining these treatment options, individuals with Brown-Séquard syndrome can improve their overall well-being and quality of life. It is essential to consult with a healthcare professional to create a personalized treatment plan that considers individual goals and challenges.
Conclusion
Brown-Séquard syndrome, a rare neurological condition causing muscle weakness and loss of sensation on opposite sides of the body, presents significant challenges. However, there are effective treatment options available to manage symptoms and improve the quality of life for individuals with this condition.
By working closely with healthcare professionals, you can develop a personalized treatment plan tailored to your specific needs and goals. A combination of therapies, such as physical therapy, occupational therapy, and speech therapy, can help optimize your mobility and functional independence.
Furthermore, orthotics and Botox injections may be recommended to provide support and reduce spasticity, while home exercise programs can further augment your rehabilitation efforts. It's important to remain committed to your treatment program and actively engage in regular practice and therapy to achieve the best outcomes.
Remember, you are not alone in your journey with Brown-Séquard syndrome. There is ongoing research and support available to help you navigate the challenges and enhance your quality of life. With the right treatment options and a positive mindset, you can effectively manage your symptoms and achieve a better quality of life.
FAQ
What is Brown-Séquard syndrome?
Brown-Séquard syndrome is a rare neurological condition characterized by muscle weakness or paralysis on one side of the body and a loss of sensation on the opposite side. It is caused by damage to the spinal cord, often due to trauma or inflammation.
What are the causes of Brown-Séquard syndrome?
Brown-Séquard syndrome can be caused by various factors, including trauma to the spinal cord (such as gunshot or stab wounds), inflammation or pinching of the spinal cord, spinal cord tumors, inadequate blood flow, infectious diseases like tuberculosis, and inflammatory diseases like multiple sclerosis.
What are the symptoms of Brown-Séquard syndrome?
The symptoms of Brown-Séquard syndrome include muscle weakness or paralysis on one side of the body, a loss of sensation on the opposite side, and sensory deficits such as a loss of deep sensation. These symptoms can affect balance, walking ability, and everyday activities.
What is the prognosis for individuals with Brown-Séquard syndrome?
The prognosis for individuals with Brown-Séquard syndrome is generally favorable. Studies have shown that 75-90% of individuals are able to recover their walking abilities by the time they are discharged from rehabilitation. With consistent practice and therapy, individuals with Brown-Séquard syndrome can improve their mobility and quality of life.
What are the treatment options for Brown-Séquard syndrome?
Treatment options for Brown-Séquard syndrome focus on promoting neuroplasticity and improving functional recovery. Physical therapy can help individuals improve motor control and strength on their affected side. Occupational therapy assists in maximizing functional independence and teaching compensatory strategies. Orthotics and Botox injections may be recommended to provide support and reduce spasticity. Speech therapy can address respiratory difficulties. Home exercise is also important to continue rehabilitation efforts.
How can individuals with Brown-Séquard syndrome manage their symptoms?
Individuals with Brown-Séquard syndrome can manage their symptoms by working with healthcare professionals to create a personalized treatment plan that addresses their specific needs and goals. By following the recommended therapies and engaging in home exercise, individuals can improve their mobility and enhance their quality of life.
Source Links
- https://my.clevelandclinic.org/health/diseases/22749-brown-sequard-syndrome-bss
- https://www.ninds.nih.gov/health-information/disorders/brown-sequard-syndrome
- https://www.flintrehab.com/brown-sequard-syndrome/
Unveiling Bell's Palsy Causes – Know the Triggers
Bell's palsy is a condition that can cause sudden paralysis of the facial muscles, leading to facial drooping, difficulty in blinking, and an asymmetric smile. While the exact cause of Bell's palsy is not fully understood, there are several factors that are believed to contribute to its development.
Research suggests that inflammation of the facial nerve, viral infections such as the herpes simplex virus, autoimmune diseases, trauma, tumors, certain medications, and other underlying factors may trigger Bell's palsy. However, it's important to note that Bell's palsy is a diagnosis of exclusion, meaning that other conditions with similar symptoms should be ruled out before reaching a conclusion.
Key Takeaways:
- Bell's palsy is an idiopathic condition that results in sudden facial paralysis.
- Inflammation of the facial nerve, viral infections, autoimmune diseases, trauma, tumors, certain medications, and other factors may trigger Bell's palsy.
- It's important to exclude other conditions with similar symptoms before diagnosing Bell's palsy.
Epidemiology and Risk Factors of Bell's Palsy
Bell's palsy, although relatively rare, has an annual incidence of approximately 32 cases per 100,000 people. This condition is commonly diagnosed in individuals between the ages of 15 and 45, with younger patients generally having a better prognosis.
Several risk factors have been identified for Bell's palsy, including diabetes, hypertension, respiratory disease, obesity, pregnancy, and preeclampsia. These underlying conditions can increase the likelihood of developing Bell's palsy.
When it comes to gender differences, there are no significant variations in risk or outcomes between men and women. However, approximately 7% of patients experience recurrent Bell's palsy, usually within 1.5 years of the initial onset.
To summarize:
- Bell's palsy has an annual incidence of around 32 cases per 100,000 people.
- It is most commonly observed in individuals aged 15 to 45.
- Risk factors for Bell's palsy include diabetes, hypertension, respiratory disease, obesity, pregnancy, and preeclampsia.
- Recurrent Bell's palsy occurs in approximately 7% of patients, typically within 1.5 years of the initial onset.
Understanding the epidemiology and risk factors associated with Bell's palsy can help individuals and healthcare professionals identify potential triggers and take appropriate preventive measures.
Pathophysiology of Bell's Palsy
Bell's palsy is a condition that results from the inflammation of the facial nerve, specifically cranial nerve VII, as it exits the skull. This inflammation can cause various complications, including obstruction, ischemia, and demyelination of the nerve, ultimately leading to the weakness of the facial muscles.
The exact cause of inflammation in Bell's palsy is still uncertain. However, studies have explored the role of herpesviruses, such as the herpes simplex virus, in the development of the condition. These viruses have been investigated as potential causative agents due to their ability to trigger inflammatory responses and nerve damage.

Further research is needed to establish a definitive link between herpesviruses and the occurrence of Bell's palsy. Understanding the underlying mechanisms and triggers of inflammation can pave the way for targeted treatment strategies and improved patient outcomes.
Clinical Presentation of Bell's Palsy
In individuals with Bell's Palsy, the sudden weakness or paralysis of the facial muscles on one side of the face is the hallmark symptom. This can manifest as facial drooping, making it difficult to maintain a symmetrical appearance. An asymmetric smile is also common, with the affected side of the face showing limited movement. Moreover, closing the eyelid on the affected side can be challenging, resulting in eye closure difficulties. Facial pain may also be experienced in some cases.
Additional symptoms that may accompany Bell's Palsy include jaw pain, loss of taste, headache, and sensitivity to sound. These manifestations contribute to the overall impact of the condition on an individual's quality of life. To gauge the severity of facial nerve dysfunction, the House-Brackmann grading scale is often employed. This scale helps assess the degree of muscle weakness and paralysis, providing a standardized measure of the condition's impact.
Here is a table summarizing the common clinical presentations of Bell's Palsy:
| Clinical Presentations of Bell's Palsy | |
|---|---|
| Facial Drooping | An asymmetric appearance due to weakness or paralysis of the facial muscles. |
| Asymmetric Smile | Limited or affected movement on one side of the face while smiling. |
| Eye Closure Difficulties | Inability or challenges in closing the eyelid on the affected side. |
| Facial Pain | Pain experienced in the facial region, which may vary in intensity. |
It is important to recognize these symptoms and seek medical attention promptly for a proper diagnosis and appropriate management of Bell's Palsy.
Diagnosis of Bell's Palsy
The diagnosis of Bell's palsy is primarily based on clinical findings, as there is no specific test available to confirm the condition. To accurately diagnose Bell's palsy, healthcare professionals rely on a comprehensive approach that includes:
- Taking a detailed clinical history
- Conducting a thorough physical examination
- Performing imaging studies, if necessary
Clinical History for Bell's Palsy
A thorough clinical history is crucial in diagnosing Bell's palsy as it helps exclude other potential causes of facial paralysis. During this process, your healthcare provider will ask you questions about:
- Recent illnesses or infections
- Medications you are currently taking
- Prior herpes infections
By gathering this information, your healthcare provider can effectively rule out other underlying conditions that may mimic the symptoms of Bell's palsy.
Physical Examination for Bell's Palsy
Physical examination is a vital component of diagnosing Bell's palsy. Your healthcare provider will perform a comprehensive evaluation, which may include:
- A complete ophthalmologic exam to assess eye closure, tear production, and corneal sensitivity
- An assessment of your facial muscles, including facial symmetry, muscle strength, and mobility
Through this physical examination, your healthcare provider can further support the diagnosis of Bell's palsy.
Imaging for Bell's Palsy
In some cases, imaging studies may be necessary to rule out other underlying causes of facial paralysis. Magnetic resonance imaging (MRI) is commonly used to evaluate the facial nerve and exclude conditions such as tumors or other structural abnormalities. This imaging modality provides detailed images that aid in confirming the diagnosis of Bell's palsy.
It is important to note that imaging studies are not always required for every case of Bell's palsy and are typically reserved for individuals with atypical presentations or those who do not show signs of improvement over time.

Prognosis of Bell's Palsy
Recovery from Bell's Palsy is a common outcome, with the majority of individuals experiencing spontaneous improvement within three to five weeks of onset. The time for recovery in Bell's Palsy can vary from person to person, with some individuals recovering sooner and others taking a bit longer. Several factors can influence the recovery process in Bell's Palsy:
1. Severity of Palsy: The extent of recovery is closely associated with the initial severity of facial paralysis at presentation. Individuals with milder symptoms tend to have a better prognosis and a higher likelihood of full recovery.
2. Age: The age of the patient also plays a role in the recovery from Bell's Palsy. Younger patients generally have better outcomes and a higher chance of regaining complete facial function.
3. Comorbidities: The presence of underlying health conditions, such as diabetes or hypertension, can affect the recovery process. Managing these comorbidities effectively can contribute to a more favorable prognosis.
4. Prompt Treatment: Timely intervention and appropriate medical care can positively impact the recovery from Bell's Palsy. Initiating treatment early may help reduce inflammation, promote nerve regeneration, and enhance overall recovery.
While the majority of individuals recover fully, it is important to note that some may experience residual deficits, such as partial facial weakness or synkinesis (involuntary muscle movements). These residual symptoms may require additional treatment or management to optimize overall facial function.
Recovery Tips for Bell's Palsy:
- Follow your healthcare professional's advice and treatment plan consistently.
- Practice facial exercises recommended by your healthcare provider to help improve muscle strength and coordination.
- Take care of your overall health and well-being by eating a balanced diet, getting enough rest, and managing stress.
- Avoid exposure to extreme temperatures and excessive sunlight that can potentially irritate the affected facial nerves.
- Seek emotional support from friends, family, or support groups to cope with the challenges of facial paralysis.
By understanding the factors that influence recovery and adopting appropriate measures, you can improve your chances of a more complete recovery from Bell's Palsy.
Other Causes of Facial Paralysis
While Bell's palsy is the most common cause of sudden onset facial paralysis, there are several other potential causes that should be considered. Here are some other types of facial paralysis:
- Congenital Facial Paralysis:
Congenital facial paralysis refers to paralysis that is present at birth. It can be caused by various developmental abnormalities and may be associated with other congenital conditions.
- Acute Facial Paralysis:
Acute facial paralysis can occur suddenly over a short period of time. It can be caused by different factors such as stroke, infection, autoimmune diseases, tumors, surgery, and trauma.
- Chronic Facial Paralysis:
Chronic facial paralysis worsens over time. It can be associated with tumors or growths along the course of the facial nerve, leading to gradual loss of facial function and movement.
- Other Causes:
In addition to the above, there are various other causes of facial paralysis, including neurological disorders, Lyme disease, Ramsay Hunt syndrome, Guillain-Barre syndrome, and hereditary conditions.
It is important to identify the underlying cause of facial paralysis in order to determine the appropriate treatment and management strategies. Proper diagnosis and comprehensive evaluation by a healthcare professional are crucial.
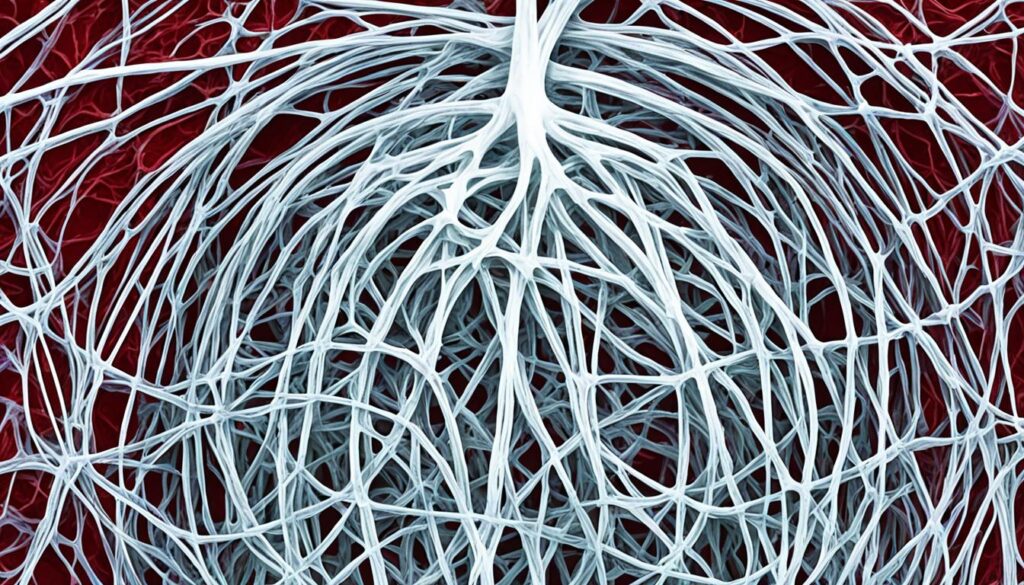
Treatment Options for Facial Paralysis
The treatment for facial paralysis depends on the underlying cause and the individual's specific condition. Medical, injectable, and surgical treatments are among the options available to address facial paralysis and restore facial function.
Medical Treatment for Facial Paralysis
Medical treatment for facial paralysis often includes the use of medications to manage symptoms, reduce inflammation, and promote nerve recovery. Antibiotics may be prescribed if an infection is suspected, while antiviral medications can help control viral infections that may contribute to facial paralysis. Steroids, such as prednisone, are commonly used to reduce inflammation and improve nerve function.
Injectable Treatment for Facial Paralysis
Injectable treatments offer a non-surgical approach to improving facial symmetry and function in individuals with facial paralysis. Botox®, a commonly used injectable, can help relax overactive muscles, reducing involuntary movements and improving facial appearance. Injectable fillers, such as hyaluronic acid fillers, can restore volume and improve facial contour, aiding in the restoration of facial balance and harmony.
Surgical Treatment for Facial Paralysis
In cases where the underlying cause of facial paralysis cannot be managed with medical or injectable treatments, surgical intervention may be necessary. Surgical treatment options for facial paralysis aim to address the underlying cause, restore facial balance, and optimize facial function. Procedures such as nerve decompression, nerve grafting, or muscle transfer may be performed to improve nerve function and restore facial movement.
It is important to note that the choice of treatment depends on the individual's specific condition, goals, and overall health. A personalized treatment plan should be developed in collaboration with a healthcare professional experienced in the management of facial paralysis.

| Treatment Option | Description |
|---|---|
| Medical Treatment | Includes the use of antibiotics, antivirals, and steroids to manage symptoms, reduce inflammation, and promote nerve recovery. |
| Injectable Treatment | Non-surgical options such as Botox® and injectable fillers can improve facial symmetry, reduce involuntary movements, restore volume, and improve facial contour. |
| Surgical Treatment | Procedures like nerve decompression, nerve grafting, or muscle transfer may be performed to address the underlying cause, restore facial balance, and optimize facial function. |
Conclusion
Facial paralysis, including Bell's palsy, can have a significant impact on your life, affecting facial movement, appearance, and essential functions. While the exact cause of Bell's palsy is unknown, several triggers have been identified, including inflammation of the facial nerve and viral infections. Early diagnosis and treatment are crucial for optimal recovery, and a range of treatment options, including medications, injectables, and surgery, are available.
By understanding the underlying causes of facial paralysis and exploring appropriate treatment options, you can improve your quality of life and regain facial function. It is important to work closely with healthcare professionals to develop a personalized treatment plan that addresses your specific needs and goals. Regular follow-up visits and ongoing management may be necessary to ensure the best possible outcome.
If you or a loved one are experiencing facial paralysis symptoms, seek medical attention promptly to determine the cause and explore available treatment options. Remember, while living with facial paralysis can present challenges, with the right care and support, you can enhance your well-being and regain control over your daily life.
FAQ
What are the causes of Bell's Palsy?
The exact cause of Bell's Palsy is not fully understood, but potential triggers include inflammation of the facial nerve, herpes simplex virus, other viral infections, autoimmune diseases, trauma, tumors, and certain medications.
What are the risk factors for Bell's Palsy?
Risk factors for Bell's Palsy include diabetes, hypertension, respiratory disease, obesity, pregnancy, and preeclampsia. Recurrent Bell's Palsy is seen in approximately 7% of patients, usually within 1.5 years of the initial onset.
How does Bell's Palsy occur?
Bell's Palsy occurs due to inflammation of the facial nerve as it exits the skull, leading to facial muscle weakness. The exact cause of inflammation is unclear, but herpesviruses, including herpes simplex virus, have been investigated as potential causative agents.
What are the symptoms of Bell's Palsy?
The onset of Bell's Palsy is characterized by sudden weakness or paralysis of the facial muscles on one side of the face. This can lead to facial drooping, an asymmetric smile, drooling, difficulty closing the eyelid on the affected side, jaw pain, loss of taste, headache, and sensitivity to sound.
How is Bell's Palsy diagnosed?
The diagnosis of Bell's Palsy is primarily based on clinical findings, as there is no specific test available to confirm the condition. A thorough clinical history and physical examination, including a complete ophthalmologic exam, can support the diagnosis. In some cases, imaging studies such as magnetic resonance imaging (MRI) may be necessary.
What is the prognosis for Bell's Palsy?
The majority of individuals with Bell's Palsy experience spontaneous recovery within three to five weeks. The extent of recovery is associated with the severity of palsy at presentation and the age of the patient. Younger patients and those with incomplete palsy tend to have a better prognosis.
What are the other causes of facial paralysis?
Aside from Bell's Palsy, facial paralysis can be caused by congenital factors, acute conditions such as stroke or infection, autoimmune diseases, tumors, surgery, trauma, or chronic conditions associated with tumors or growths along the course of the facial nerve.
What are the treatment options for facial paralysis?
The treatment for facial paralysis depends on the underlying cause and the individual's specific condition. Medical treatment options may include antibiotics, antivirals, and steroids. Injectable treatments such as Botox® and injectable fillers can improve facial symmetry and function. Surgical intervention may be necessary in some cases.
What impact does facial paralysis have on an individual's life?
Facial paralysis, including Bell's Palsy, can significantly impact an individual's life, affecting facial movement, appearance, and essential functions. Early diagnosis and appropriate treatment can help improve quality of life and regain facial function.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6169125/
- https://www.aao.org/eyenet/article/diagnosis-and-management-of-bell-palsy
- https://muschealth.org/medical-services/ent/fprs/facial-paralysis