Effective Cervical Dystonia Treatment Options
If you or a loved one are dealing with cervical dystonia, also known as spasmodic torticollis, you know how challenging it can be to manage the symptoms. The good news is that there are effective treatment options available to help alleviate the pain, tremors, and abnormal neck posturing associated with this condition.
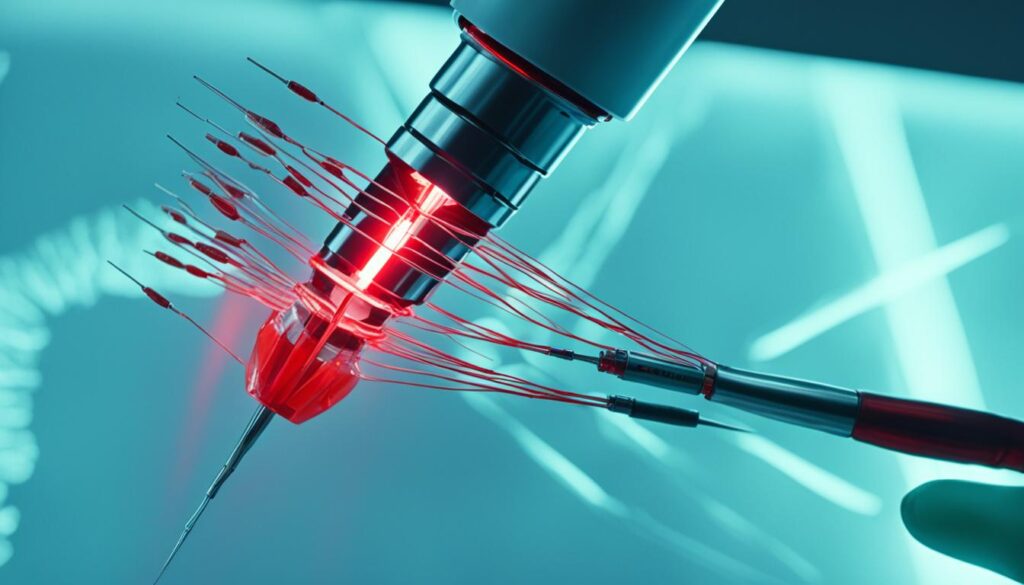
When it comes to cervical dystonia treatment, one of the most effective options is botulinum toxin (BoNT) injections. These injections provide selective denervation and relaxation of the affected neck muscles, leading to significant improvement in symptoms. BoNT injections are the gold standard treatment and can be repeated every three to four months for long-lasting benefits.
In addition to BoNT injections, oral medications can be used as adjunct therapy for cervical dystonia. While not as effective as BoNT injections, these medications have a muscle-relaxing effect and can help improve symptoms to some extent. However, they may come with side effects that need to be considered.
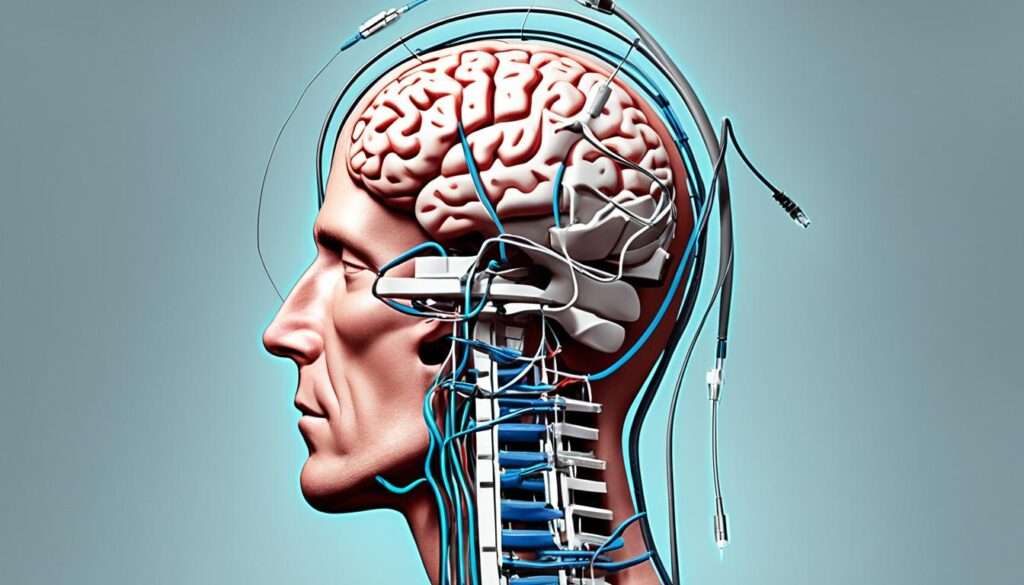
In cases where other treatments have failed to provide sufficient relief, deep brain stimulation (DBS) may be an option. DBS is a surgical therapy that involves implanting a wire into the brain to deliver electrical pulses and disrupt the abnormal nerve signals causing the head to twist. This treatment is considered when other options have been exhausted.
Aside from medical interventions, there are other treatment modalities and coping strategies that can help manage cervical dystonia. These include sensory tricks, such as touching the opposite side of the face or the back of the head, which can temporarily alleviate symptoms. Heat packs, massage, and exercises that improve neck strength and flexibility may also be beneficial. Additionally, managing stress is important as it can exacerbate symptoms.
In conclusion, there are effective treatment options available for cervical dystonia. BoNT injections are the most widely used and provide selective denervation and relaxation of the affected neck muscles. Oral medications and deep brain stimulation are other options to consider. With the right treatment approach and support from healthcare professionals, it is possible to manage symptoms and improve quality of life.
Botulinum Toxin Injections: The Most Effective Treatment
When it comes to treating cervical dystonia, botulinum toxin (BoNT) injections have proven to be the gold standard. This treatment offers significant relief from symptoms and has become the go-to option for patients seeking effective cervical dystonia treatment.
BoNT is injected directly into the affected neck muscles, targeting the source of the problem. By selectively denervating the muscles, BoNT injections induce relaxation and improve neck alignment, leading to a reduction in dystonia-related symptoms.
This treatment is not only highly effective but also well-tolerated by patients. The injections are typically administered every three to four months, ensuring the continuous management of symptoms and the maintenance of optimal relief.
| Treatment | Effectiveness | Tolerance | Treatment Frequency |
|---|---|---|---|
| Botulinum Toxin Injections | Significant improvement in symptoms | Well-tolerated | Every three to four months |
| Oral Medications | Modest improvement in symptoms | May come with side effects | Varies depending on the medication |
| Deep Brain Stimulation | Suitable for refractory cases | Surgical procedure with potential risks | Ongoing management |
Table: Comparison of Cervical Dystonia Treatment Options
If you're considering cervical dystonia treatment, it's important to consult with a healthcare professional who can assess your condition and determine the most appropriate course of action. BoNT injections offer a reliable and proven solution for effectively managing cervical dystonia symptoms and improving your quality of life.
Oral Medications as Adjunct Therapy
Oral medications can be used as an adjunct therapy for cervical dystonia when botulinum toxin injections are not practical or desired. These medications have a muscle-relaxing effect and can help improve symptoms to some extent. However, it's important to note that the effects of oral medications for cervical dystonia are more modest compared to botulinum toxin injections.
While oral medications can provide some relief, they often come with side effects that may limit their use. It's essential to work closely with your healthcare provider to determine the best course of treatment and manage any potential side effects.
Common Oral Medications for Cervical Dystonia
Here are a few common oral medications that may be prescribed as part of a cervical dystonia treatment plan:
- Tizanidine: Tizanidine is a muscle relaxant that works by blocking nerve signals and reducing muscle spasms. It can help alleviate some of the symptoms associated with cervical dystonia.
- Baclofen: Baclofen is another muscle relaxant that can be used to reduce muscle stiffness and spasms. It acts on the central nervous system to provide relief.
- Trihexyphenidyl: Trihexyphenidyl is an anticholinergic medication that can help control muscle movements and reduce dystonic symptoms. It works by blocking certain neurotransmitters in the brain.
It's important to remember that the effectiveness of oral medications can vary from person to person. Your healthcare provider will closely monitor your response to the medication and may make adjustments to the dosage or switch to a different medication if needed.
Combining Oral Medications with other Treatment Modalities
While oral medications may not be as effective as botulinum toxin injections, they can still play a valuable role in managing cervical dystonia symptoms when used in combination with other treatment modalities. Your healthcare provider may recommend a combination approach tailored to your specific needs.
In addition to oral medications, physical therapy and regular exercise can help improve muscle strength and flexibility, contributing to better symptom management. Heat packs, massage, and relaxation techniques may also provide temporary relief from muscle tension and discomfort.
Remember, it's crucial to work closely with your healthcare team to find the most effective treatment plan for your cervical dystonia. They will consider your individual needs and preferences to develop a comprehensive approach that best suits you.
| Oral Medication | Function | Common Side Effects |
|---|---|---|
| Tizanidine | Blocks nerve signals and reduces muscle spasms | Drowsiness, dizziness, dry mouth |
| Baclofen | Reduces muscle stiffness and spasms | Drowsiness, weakness, nausea |
| Trihexyphenidyl | Controls muscle movements and reduces dystonic symptoms | Dry mouth, blurred vision, constipation |

Deep Brain Stimulation for Refractory Cases
When Other Treatments Fall Short
For individuals with refractory cervical dystonia, deep brain stimulation (DBS) offers a surgical therapy that targets the root cause of the condition. When other treatments have failed to provide sufficient relief, DBS may be considered as an alternative option. This procedure involves the implantation of a thin wire into the brain, which delivers electrical pulses to disrupt abnormal nerve signals responsible for the twisting of the head.
By directly targeting the source of the problem, DBS aims to alleviate the symptoms of cervical dystonia and improve the patient's quality of life. While the complete mechanism of action is not fully understood, studies have shown that DBS can provide significant relief for refractory cases.
Considerations and Effectiveness
Deep brain stimulation is typically recommended when individuals have exhausted other treatment options without achieving satisfactory results. It is important to note that DBS is a surgical procedure and requires careful evaluation and selection of suitable candidates by a qualified healthcare professional.
The effectiveness of DBS in refractory cervical dystonia treatment has been documented in various studies. Research has demonstrated significant improvements in dystonia severity, reduced pain, and enhanced motor function in patients who have undergone this procedure.
Exploring Risks and Benefits
As with any surgical intervention, DBS carries potential risks and should be thoroughly discussed with the healthcare provider. Some potential risks include infection, bleeding, device-related complications, and adverse events associated with brain surgery. However, the overall benefit-risk profile of DBS for refractory cervical dystonia can be favorable for eligible individuals.
| Advantages | Considerations |
|---|---|
| - Potential for significant symptom improvement | - Requires a surgical procedure |
| - Offers an alternative for individuals with refractory dystonia | - Potential risks and complications |
| - Can enhance quality of life and motor function | - Need for careful patient selection |
It is essential for patients to have a comprehensive discussion with their healthcare team to fully understand the potential benefits and risks of DBS for refractory cervical dystonia treatment.
Other Treatment Modalities and Coping Strategies
In addition to botulinum toxin injections, oral medications, and deep brain stimulation (DBS), there are other treatment modalities and coping strategies that may help manage cervical dystonia. These approaches aim to alleviate symptoms, improve daily functioning, and enhance overall well-being.
Sensory Tricks
One effective strategy is the use of sensory tricks. These tricks involve touching certain areas of the body to temporarily alleviate symptoms. For example, some individuals find relief by lightly touching the opposite side of their face or the back of their head. This can help relax the muscles and reduce abnormal posturing.
Heat Packs and Massage
Applying heat packs to the affected neck muscles can provide relief by reducing muscle tension and promoting relaxation. Massage therapy, especially when performed by a trained professional, can help alleviate muscle stiffness, improve blood circulation, and relieve pain associated with cervical dystonia.
Neck Strengthening and Flexibility Exercises
Engaging in neck strengthening and flexibility exercises can help improve muscle control and reduce the severity of cervical dystonia symptoms. Physical therapists can provide guidance on specific exercises that target the affected muscles. These exercises may include stretching, range of motion exercises, and resistance training.
Stress Management Techniques
Stress often worsens the symptoms of cervical dystonia. Therefore, incorporating stress management techniques into daily life can be beneficial. Practices such as deep breathing exercises, meditation, yoga, and mindfulness can help reduce stress levels and promote relaxation. It is important to find activities that work best for you.
| Treatment Modality | Description |
|---|---|
| Sensory Tricks | Use of specific touches to alleviate symptoms temporarily |
| Heat Packs and Massage | Application of heat packs and therapeutic massage to relax muscles |
| Neck Strengthening and Flexibility Exercises | Exercises targeting neck muscles for improved control and flexibility |
| Stress Management Techniques | Practices to reduce stress levels and promote relaxation |
Implementing a combination of these treatment modalities and coping strategies can help individuals with cervical dystonia better manage their symptoms and improve their quality of life. It is important to consult with a healthcare professional to determine the most suitable approaches for your specific needs.

Conclusion
Cervical dystonia is a challenging condition that can significantly impact your quality of life. The good news is that effective therapies are available to help manage your symptoms.
Botulinum toxin injections have emerged as the most effective treatment for cervical dystonia. These injections provide selective denervation and relaxation of the affected neck muscles, leading to improved symptom management. Additionally, oral medications and deep brain stimulation are viable options for refractory cases.
Aside from these medical interventions, there are other treatment modalities and coping strategies that can complement your treatment plan. Sensory tricks, heat packs, massage, and exercises that improve neck strength and flexibility can help alleviate symptoms. Stress management techniques are also important, as stress can worsen symptoms.
It is crucial that you work closely with your healthcare team to find the most suitable treatment approach for your specific needs. By utilizing these effective therapies and incorporating symptom management strategies into your daily routine, you can improve your quality of life and regain control over cervical dystonia.
FAQ
What is cervical dystonia?
Cervical dystonia, also known as spasmodic torticollis, is a common adult-onset focal dystonia characterized by abnormal neck posturing, tremors, and pain.
What is the treatment of choice for cervical dystonia?
The treatment of choice for cervical dystonia is botulinum toxin (BoNT) injections, which provide selective denervation and relaxation of the affected neck muscles.
How effective are botulinum toxin injections in treating cervical dystonia?
Botulinum toxin (BoNT) injections are the gold standard treatment for cervical dystonia, providing significant improvement in symptoms. BoNT is injected directly into the affected neck muscles and causes selective denervation, resulting in relaxation and improved neck alignment.
How often do botulinum toxin injections need to be repeated for cervical dystonia?
Botulinum toxin injections for cervical dystonia usually need to be repeated every three to four months.
Are there other treatment options for cervical dystonia?
Yes, other treatment options for cervical dystonia include oral medications and deep brain stimulation (DBS) for refractory cases.
How effective are oral medications for cervical dystonia?
Oral medications can be used as adjunct therapy for cervical dystonia, especially when BoNT injections are not practical or desired. These medications have a muscle-relaxing effect and can help improve symptoms to some extent.
What is deep brain stimulation (DBS) and when is it considered for cervical dystonia?
Deep brain stimulation (DBS) is a surgical therapy offered to patients with refractory cervical dystonia. In this procedure, a thin wire is implanted into the brain, and electrical pulses are delivered to disrupt the abnormal nerve signals causing the head to twist. DBS is considered when other treatments have failed to provide sufficient relief.
Are there any other treatment modalities and coping strategies for cervical dystonia?
Yes, there are other treatment modalities and coping strategies that may help manage cervical dystonia. These include sensory tricks, such as touching the opposite side of the face or the back of the head, which can temporarily alleviate symptoms. Heat packs, massage, and exercises that improve neck strength and flexibility may also be beneficial. Stress management techniques are important as stress can exacerbate symptoms.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3495548/
- https://www.mayoclinic.org/diseases-conditions/cervical-dystonia/diagnosis-treatment/drc-20354128
- https://www.uptodate.com/contents/cervical-dystonia-treatment-and-prognosis
Chronic Fatigue Syndrome Symptoms Guide
Welcome to our comprehensive guide on chronic fatigue syndrome (CFS) symptoms. If you are experiencing persistent fatigue or have been diagnosed with CFS, it's important to understand the signs and symptoms associated with this complex condition.
Also known as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), CFS is characterized by extreme fatigue that lasts for at least six months. The symptoms of CFS can vary from person to person, but commonly include:
- Extreme exhaustion
- Memory problems
- Dizziness
- Muscle or joint pain
- Unrefreshing sleep
- Headaches
- Sore throats
- Tender lymph nodes
Individuals with CFS may also experience sensitivity to light, sound, smells, food, and medications. If you are experiencing persistent or excessive fatigue and have these symptoms, it's important to seek medical attention. CFS can significantly impact your daily functioning and quality of life.
It's essential to rule out other health problems with similar symptoms, as the diagnosis of CFS often involves a process of elimination. While there is no specific treatment for CFS, symptom management through lifestyle strategies and medical interventions can help improve your quality of life. In this guide, we will explore the core symptoms of CFS, possible causes and risk factors, the diagnostic process, and treatment options available. Remember, you are not alone in this journey. We are here to provide you with valuable information and support as you navigate living with CFS.
Core Symptoms of Chronic Fatigue Syndrome
Chronic fatigue syndrome (ME/CFS) is characterized by a set of core symptoms that can significantly impact daily life and well-being. Understanding these symptoms is crucial for early detection and appropriate management of the condition.
The core symptoms of chronic fatigue syndrome include:
- Severe Fatigue: Individuals with ME/CFS experience debilitating fatigue that is not relieved by rest. This fatigue lasts for at least six months and hinders daily activities.
- Post-Exertional Malaise (PEM): Physical or mental exertion can trigger a crash in ME/CFS, leading to new or worsened symptoms. This post-exertional malaise can last for days or even weeks.
- Sleep Disorders: ME/CFS often manifests with sleep disturbances, including difficulties falling asleep, intense and vivid dreaming, restless legs, muscle spasms, and sleep apnea.
- Problems with Thinking and Memory (Brain Fog): Many individuals with ME/CFS experience cognitive impairments, such as difficulties with memory, concentration, and processing information. This brain fog can significantly impair daily functioning.
- Dizziness Upon Standing: Orthostatic intolerance, which causes dizziness and lightheadedness upon standing, is a common symptom of ME/CFS.
- Pain: Muscle aches, joint pain, and headaches are frequently reported by individuals with ME/CFS.
Additionally, individuals with ME/CFS may experience tender lymph nodes, gastrointestinal problems, chills, night sweats, allergies to food, sensitivity to light, touch, heat, and cold, muscle weakness, shortness of breath, irregular heartbeat, mood changes, and numbness or tingling in the hands, feet, and face. These symptoms can vary from person to person and may resemble those of other conditions, making ME/CFS challenging to diagnose.
| Symptom | Description |
|---|---|
| Severe Fatigue | Deep exhaustion that persists for at least six months and disrupts daily activities. |
| Post-Exertional Malaise (PEM) | Crash in symptoms following physical or mental exertion. |
| Sleep Disorders | Disturbed sleep patterns, intense dreaming, restless legs, muscle spasms, and sleep apnea. |
| Problems with Thinking and Memory (Brain Fog) | Cognitive difficulties, including memory problems, poor concentration, and information processing issues. |
| Dizziness Upon Standing | Orthostatic intolerance leading to dizziness and lightheadedness upon standing. |
| Pain | Muscle aches, joint pain, and headaches. |
It is important to consult a healthcare professional for proper diagnosis and management of chronic fatigue syndrome. By identifying and addressing these core symptoms, individuals with ME/CFS can work towards improving their quality of life.

Possible Causes and Risk Factors of Chronic Fatigue Syndrome
The exact cause of chronic fatigue syndrome (ME/CFS) is still unknown, but various factors may contribute to its development. Genetics, infections, physical or emotional trauma, and problems with energy usage are among the possible causes and risk factors for ME/CFS.
Genetics
Genetics is believed to play a role in chronic fatigue syndrome. Research suggests that ME/CFS may run in some families, indicating a genetic predisposition to the condition.
Infections
Infections, such as viral or bacterial infections, have been reported to trigger symptoms of ME/CFS in some individuals. These infections can potentially cause immune system dysregulation and lead to the development of ME/CFS.
Physical or Emotional Trauma
Physical or emotional trauma, such as an injury, surgery, or significant stress, may precede the onset of ME/CFS symptoms. Traumatic experiences can potentially disrupt the body's equilibrium and contribute to the development of ME/CFS.
Problems with Energy Usage
Some individuals with ME/CFS may experience difficulties in converting fats and sugars into energy. Problems with energy usage, particularly in the cellular level, have been observed in certain individuals with ME/CFS, contributing to their chronic fatigue and other symptoms.
Risk Factors
Several risk factors have been identified for chronic fatigue syndrome. These include age, sex, and a history of other complex medical problems. Women are diagnosed with ME/CFS more often than men, and the condition can occur at any age, with young to middle-aged adults being the most commonly affected.
The wide range of potential causes and risk factors for chronic fatigue syndrome highlights the complex nature of the condition. Further research is needed to fully understand the underlying mechanisms and develop more effective chronic fatigue syndrome treatment.
| Possible Causes | Risk Factors |
|---|---|
| Genetics | Age |
| Infections | Sex |
| Physical or Emotional Trauma | History of other complex medical problems |
| Problems with Energy Usage |

Diagnosing Chronic Fatigue Syndrome
Diagnosing chronic fatigue syndrome (ME/CFS) can be a complex and challenging process. The symptoms of ME/CFS can vary widely from person to person, and they often overlap with those of other health conditions. In order to receive a proper diagnosis, several key criteria must be met.
Core Symptoms Evaluation
When assessing for ME/CFS, healthcare professionals look for the presence of the core symptoms that define the condition. These include:
- Severe Fatigue: The individual must experience persistent and debilitating fatigue that lasts for at least six months.
- Post-Exertional Malaise (PEM): Physical or mental exertion leads to a worsening or relapse of symptoms.
- Sleep Disorders: Disturbed sleep patterns and problems with sleep quality.
Additionally, a person with ME/CFS should also experience problems with thinking and memory, commonly referred to as "brain fog," as well as dizziness upon standing.
Medical Evaluation and Exclusion of Other Conditions
The diagnostic process for ME/CFS involves a thorough medical evaluation. This includes:
- Reviewing the person's medical history and symptoms.
- Performing a physical examination to assess the person's overall health.
- Conducting tests to rule out other potential causes of the symptoms, such as blood tests, imaging studies, and specialized assessments.
It is important to exclude other conditions with similar symptoms before reaching a diagnosis of ME/CFS. This helps ensure that the symptoms are not attributed to any other identifiable cause.
Ongoing Research and Biomarkers
Currently, there is no specific test that can definitively diagnose ME/CFS. However, ongoing research is exploring various potential biomarkers that may aid in diagnosis. These biomarkers could provide objective evidence of the underlying physiological changes associated with ME/CFS.
While these biomarkers are still being investigated, the diagnosis of ME/CFS primarily relies on the clinical judgment of healthcare professionals who have experience and knowledge in managing the condition.
It is crucial for individuals who suspect they may have ME/CFS to seek medical help and work with healthcare professionals who are familiar with the condition. They can guide them through the diagnostic process and ensure they receive an accurate diagnosis.
Treating Chronic Fatigue Syndrome
While there is no specific cure for chronic fatigue syndrome (ME/CFS), there are various treatment approaches that can help individuals manage their symptoms and improve their quality of life.
Lifestyle Strategies for Symptom Management
Lifestyle strategies play a crucial role in managing chronic fatigue syndrome. These strategies are personalized based on individual symptoms and challenges and may include:
- Activity pacing: Learning to balance activities and rest periods to avoid overexertion and post-exertional malaise. It involves breaking tasks into manageable segments and gradually increasing activity levels.
- Establishing healthy sleep habits: Creating a regular sleep schedule, practicing good sleep hygiene, and implementing relaxation techniques to improve sleep quality.
- Managing pain: Utilizing medication or non-drug therapies such as physical therapy, acupuncture, or massage to address muscle and joint pain associated with chronic fatigue syndrome.
- Addressing anxiety and depression: Engaging in stress reduction techniques, cognitive-behavioral therapy, or counseling to alleviate emotional distress often experienced by individuals with chronic fatigue syndrome.
- Making necessary adjustments: Modifying daily activities and routines to conserve energy, such as using assistive devices, delegating tasks, and setting realistic goals.
Medical Interventions
In addition to lifestyle strategies, medical interventions may be recommended to manage specific symptoms of chronic fatigue syndrome. These interventions can include:
- Prescription medication: Healthcare providers may prescribe medications to address sleep disturbances, pain, or other symptoms associated with chronic fatigue syndrome.
- Alternative therapies: Some individuals find relief from symptoms through alternative treatments like herbal supplements, acupuncture, or mindfulness-based therapies. However, it is essential to consult with a healthcare professional before trying these approaches.
It is crucial for individuals with chronic fatigue syndrome to work closely with their healthcare providers to develop a comprehensive treatment plan that addresses their unique needs and goals. Regular communication and feedback with healthcare professionals will help adjust the treatment plan as necessary and ensure optimal symptom management.
Support from family, friends, and advocacy groups can also be invaluable in coping with the life-changing impact of chronic fatigue syndrome. These networks provide emotional support, share resources, and offer practical advice for managing daily challenges associated with the condition.

In Summary
While there is no cure for chronic fatigue syndrome, individuals can effectively manage their symptoms through lifestyle strategies and medical interventions. By implementing personalized approaches to activity pacing, sleep management, pain relief, and emotional well-being, individuals can experience an improved quality of life. Working closely with healthcare providers and seeking support from loved ones and advocacy groups can further enhance the journey of living with chronic fatigue syndrome.
Conclusion
Living with chronic fatigue syndrome (ME/CFS) can be challenging, but it is important to remember that there are management strategies to help improve your quality of life. While the exact cause of ME/CFS remains unknown, various factors like genetics, infections, trauma, and energy usage problems may contribute to its development.
Diagnosing ME/CFS can be difficult due to its overlap with other conditions, but healthcare professionals perform a comprehensive evaluation to rule out alternate causes. While there is currently no specific cure for ME/CFS, you can effectively manage your symptoms through lifestyle strategies and medical interventions.
Implementing activity pacing, establishing healthy sleep habits, managing pain, addressing anxiety and depression, and conserving energy through necessary adjustments in daily activities can all aid in symptom management. Medical interventions, such as prescribed medications for sleep disturbances or pain, can also be recommended by your healthcare provider.
Remember, you don't have to face ME/CFS alone. Seek support from your healthcare team, loved ones, and advocacy groups to help you navigate the challenges of living with this chronic condition. By implementing these strategies and seeking support, you can improve your overall well-being and lead a fulfilling life despite ME/CFS.
FAQ
What are the symptoms of chronic fatigue syndrome?
The symptoms of chronic fatigue syndrome (ME/CFS) can vary from person to person and may include extreme fatigue, memory problems, dizziness, muscle or joint pain, unrefreshing sleep, headaches, sore throats, and tender lymph nodes. Individuals with ME/CFS may also experience sensitivity to light, sound, smells, food, and medications.
What are the core symptoms of chronic fatigue syndrome?
The core symptoms of chronic fatigue syndrome (ME/CFS) include severe fatigue that interferes with daily activities and does not improve with rest. This fatigue must be present for at least six months and is accompanied by post-exertional malaise (PEM), where physical or mental exertion leads to a crash with new or worsening symptoms. Sleep disorders are also common in ME/CFS, with individuals experiencing sleep disturbances, intense and vivid dreaming, restless legs, muscle spasms, and sleep apnea.
What are the possible causes and risk factors of chronic fatigue syndrome?
The exact cause of chronic fatigue syndrome (ME/CFS) is still unknown, but factors such as genetics, infections, physical or emotional trauma, and problems with energy usage may contribute to its development. Risk factors for ME/CFS include age, sex, and a history of other complex medical problems.
How is chronic fatigue syndrome diagnosed?
Diagnosing chronic fatigue syndrome (ME/CFS) can be challenging due to the varied nature of its symptoms and the overlap with other health conditions. To receive a diagnosis of ME/CFS, a person must have the core symptoms of severe fatigue, post-exertional malaise, and sleep disorders for at least six months. The diagnostic process involves a thorough medical evaluation, including a review of the person's symptoms, a physical examination, and tests to rule out other health problems.
What are the treatment options for chronic fatigue syndrome?
While there is no specific cure for chronic fatigue syndrome (ME/CFS), individuals can manage their symptoms through various treatment approaches. Treatment plans are personalized based on individual symptoms and challenges and may include lifestyle strategies such as activity pacing, healthy sleep habits, and pain management. Medical interventions, such as prescription medication, may also be recommended. It is important for individuals with ME/CFS to work closely with their healthcare providers to develop a comprehensive treatment plan.
How can I improve my quality of life with chronic fatigue syndrome?
Managing chronic fatigue syndrome (ME/CFS) can be challenging, but there are strategies available to improve quality of life. This may involve lifestyle adjustments, such as activity pacing and prioritizing rest, as well as seeking support from healthcare professionals, loved ones, and advocacy groups. Understanding and managing symptoms, addressing mental health concerns, and finding a balance between daily activities and self-care are essential to coping with the impact of ME/CFS.
Source Links
- https://www.mayoclinic.org/diseases-conditions/chronic-fatigue-syndrome/symptoms-causes/syc-20360490
- https://www.ncbi.nlm.nih.gov/books/NBK557676/
- https://www.medicalnewstoday.com/articles/184802
Understanding Chronic Traumatic Encephalopathy
Chronic traumatic encephalopathy (CTE) is a brain disorder that occurs as a result of repeated head injuries. It is characterized by the degeneration of nerve cells in the brain over time. CTE is not directly related to a single head injury, but rather to the cumulative effect of repeated head injuries, which are commonly seen in contact sports or military combat.
The development of CTE has been associated with a phenomenon known as second impact syndrome, which occurs when a second head injury happens before the symptoms of a previous head injury have fully resolved. Researchers are still working to understand the complex relationship between repeated head injuries and other contributing factors that lead to the brain changes seen in CTE.
CTE has been found in the brains of individuals who have participated in contact sports such as American football and boxing, as well as in military members exposed to explosive blasts. The symptoms of CTE, which may include cognitive, behavioral, mood, and motor changes, often appear years or even decades after the initial head trauma. Unfortunately, at present, CTE can only be definitively diagnosed after death through an autopsy of the brain.
Key Takeaways:
- Chronic Traumatic Encephalopathy (CTE) is a brain disorder caused by repeated head injuries.
- CTE is associated with the degeneration of nerve cells in the brain over time.
- It is most commonly seen in individuals who have participated in contact sports or military combat.
- Symptoms of CTE may include cognitive, behavioral, mood, and motor changes.
- Currently, CTE can only be definitively diagnosed after death through an autopsy of the brain.
Causes of Chronic Traumatic Encephalopathy
Chronic Traumatic Encephalopathy (CTE) is primarily caused by repeated head trauma, especially concussions. Various studies have focused on CTE in football players, hockey players, and military members. It's important to note that not everyone who experiences repeated concussions will develop CTE. Understanding the causes of CTE requires examining the changes that occur in the brain as a result of repeated head trauma.
One of the key findings in the brains of individuals with CTE is the buildup of a protein called tau around the blood vessels. Tau protein is different from the accumulations found in Alzheimer's disease and other forms of dementia. Additionally, CTE is associated with atrophy or wasting away of specific brain areas due to damage to nerve cells. It's worth mentioning that individuals with CTE may also exhibit signs of other neurodegenerative diseases such as Alzheimer's disease, amyotrophic lateral sclerosis (ALS), Parkinson's disease, or frontotemporal dementia.
Summary of Causes of CTE:
| Causes | Description |
|---|---|
| Repeated head trauma | CTE is primarily caused by multiple instances of head injuries, particularly concussions. |
| Buildup of tau protein | In the brains of individuals with CTE, there is a buildup of tau protein around the blood vessels, which is distinct from other neurodegenerative diseases. |
| Brain atrophy | CTE is associated with the wasting away or atrophy of certain brain areas due to damage to nerve cells. |
| Association with other neurodegenerative diseases | Individuals with CTE may also show signs of other neurodegenerative diseases such as Alzheimer's disease, ALS, Parkinson's disease, or frontotemporal dementia. |
Understanding the underlying causes of CTE is crucial for diagnosing, managing, and preventing this complex brain disorder. It highlights the importance of minimizing head injuries, especially concussions, and promoting brain health and safety in contact sports, military activities, and other high-risk environments.
Symptoms of Chronic Traumatic Encephalopathy
The symptoms of Chronic Traumatic Encephalopathy (CTE) can vary from person to person and may not manifest immediately after head injuries. While there are no specific symptoms that have been clearly linked to the disorder, individuals with CTE may experience a range of cognitive, behavioral, mood, and motor symptoms. These symptoms often develop years or even decades after the initial head trauma.
- Cognitive Impairment: CTE can cause difficulties with memory, learning, attention, and problem-solving. Individuals may experience forgetfulness, confusion, and trouble concentrating.
- Memory Loss: Memory loss is a common symptom of CTE. Individuals may have difficulty remembering recent events or have gaps in their long-term memory.
- Behavioral Changes: CTE can lead to changes in behavior and personality. People with CTE may become irritable, impulsive, aggressive, or exhibit changes in judgment and decision-making.
- Mood Disorders: Mood disorders such as depression, anxiety, and sudden mood swings are often observed in individuals with CTE.
- Motor Symptoms: CTE can also affect motor function. Individuals may experience difficulties with coordination, balance, and movement. Motor symptoms can progress over time and lead to problems with walking and speaking.
It's important to note that the symptoms of CTE can overlap with other neurodegenerative disorders, making it challenging to diagnose the condition during a person's lifetime. The severity and progression of symptoms can vary, and individuals may exhibit a unique combination of symptoms based on the specific areas of the brain affected by CTE.

| Symptoms | Frequency |
|---|---|
| Cognitive Impairment | High |
| Memory Loss | High |
| Behavioral Changes | Medium |
| Mood Disorders | Medium |
| Motor Symptoms | Low |
Diagnosing Chronic Traumatic Encephalopathy
Currently, Chronic Traumatic Encephalopathy (CTE) can only be definitively diagnosed after death through an autopsy of the brain. However, experts are actively working on developing diagnostic biomarkers for CTE, which could potentially enable the diagnosis of this condition during a person's lifetime. Once these biomarkers are validated, they may revolutionize CTE diagnosis and treatment.
In the absence of a post-mortem diagnosis, healthcare providers might diagnose individuals with high-risk exposures and symptoms associated with CTE as having traumatic encephalopathy syndrome. This diagnosis is based on the presence of CTE-associated symptoms rather than direct confirmation of the condition itself.
It is crucial to acknowledge that the full list of signs and the progression of CTE are still not fully understood by experts. Ongoing research endeavors aim to deepen our knowledge of this complex brain disorder.
Diagnostic Biomarkers for CTE
Diagnostic biomarkers play a pivotal role in identifying and diagnosing diseases. In the case of CTE, the development of specific biomarkers is of immense importance. These biomarkers could potentially allow for the early detection and diagnosis of CTE during a person's lifetime, opening the door for proactive management and treatment.
Experts believe that certain substances or molecules present in the body could serve as indicators or biomarkers of the underlying pathological changes associated with CTE. These biomarkers can be detected through various methods, such as blood tests or imaging techniques.
Currently, researchers are investigating various potential biomarkers, including:
- Elevated levels of tau protein: Tau protein, a key player in the development of CTE, may serve as a valuable biomarker. Tau protein accumulation is a hallmark pathological feature of CTE, and its detection in the blood or cerebrospinal fluid could potentially aid in diagnosing the condition.
- Neuroinflammatory markers: Inflammatory responses in the brain are thought to contribute to the development and progression of CTE. Monitoring levels of specific neuroinflammatory markers in the body could help identify individuals at risk or provide insight into disease severity and progression.
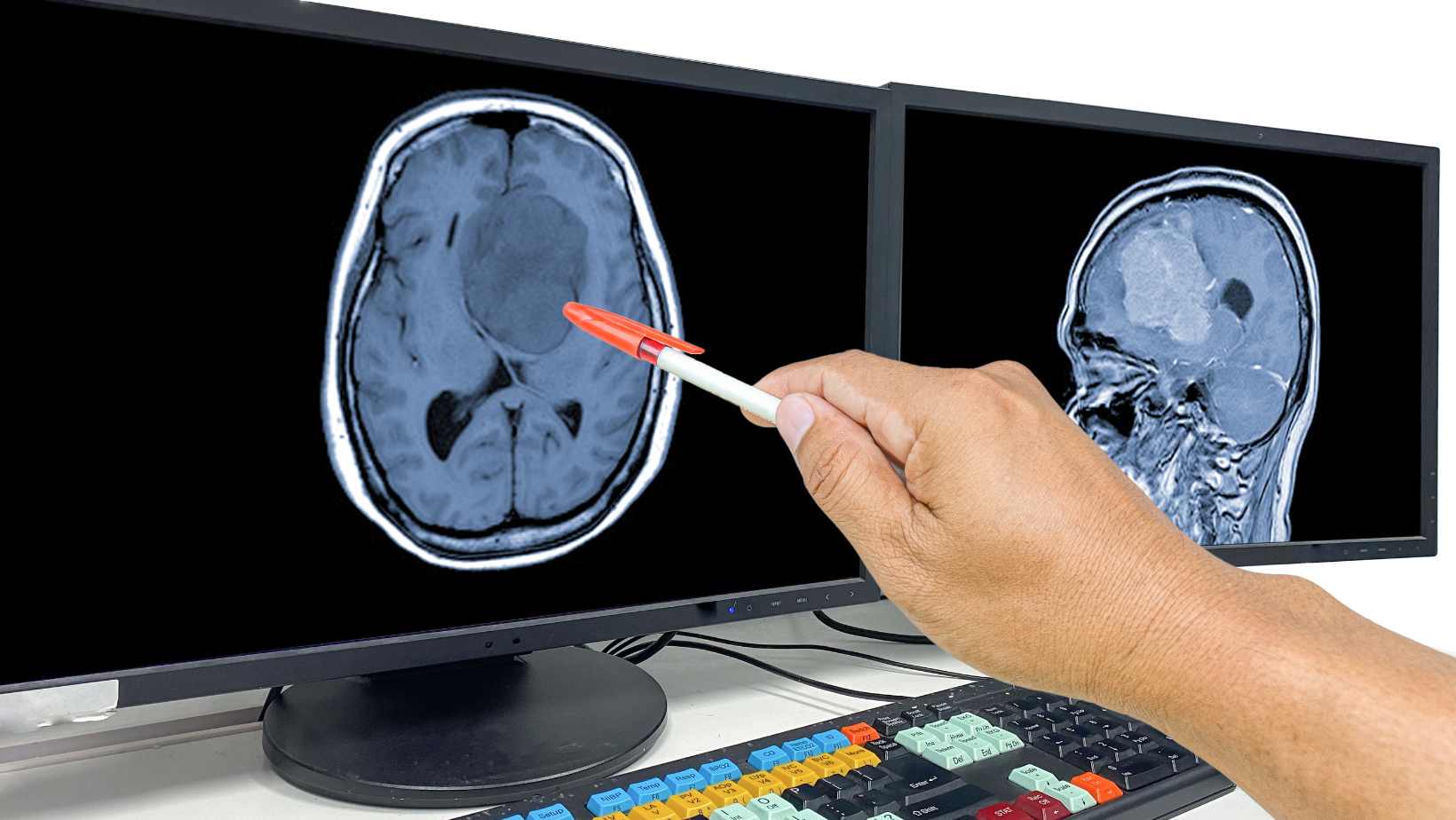
- Brain imaging techniques: Advanced imaging technologies, such as positron emission tomography (PET) and magnetic resonance imaging (MRI), are being explored to detect characteristic brain changes associated with CTE. These techniques may provide valuable insights into disease detection and progression during a person's lifetime.
While diagnostic biomarkers for CTE are still under development, their potential impact on early detection and intervention cannot be overstated. The future integration of biomarkers into clinical practice may lead to better outcomes and improved management for individuals at risk of or already affected by CTE.

| Biomarker | Potential Diagnostic Applications |
|---|---|
| Elevated levels of tau protein | Early detection, monitoring disease progression, post-mortem confirmation |
| Neuroinflammatory markers | Risk assessment, disease severity evaluation |
| Brain imaging techniques | Visualization of characteristic brain changes, disease monitoring |
Risk Factors and Prevention of Chronic Traumatic Encephalopathy
Repeated exposure to traumatic brain injury, especially head injuries, increases the risk of developing Chronic Traumatic Encephalopathy (CTE). While experts are still studying the risk factors associated with CTE, it is important to understand the steps you can take to prevent its development.
Preventing CTE starts with reducing head injuries and minimizing their impact.
Here are some preventive measures you can take:
- Wear protective gear: If you participate in contact sports or engage in activities that carry a risk of head injury, always wear appropriate protective gear such as helmets.
- Follow safety guidelines: Adhere to safety protocols and guidelines established for your chosen sport or activity. Proper techniques and rules exist for a reason – to protect against head injuries.
- Avoid additional injury after a concussion: If you have sustained a concussion, it is crucial to give your brain time to heal. Avoid any activities and contact that could result in further head injuries until you have fully recovered.
- Seek medical attention: If you or someone you know experiences a head injury, it is important to seek immediate medical attention. Prompt care and evaluation can help identify any potential long-term risks and ensure appropriate treatment.
- Stay informed: Keep yourself updated on the latest developments and research regarding CTE prevention. Knowledge is key in understanding and implementing effective preventive measures.
While these measures cannot guarantee the prevention of CTE, they serve as crucial steps in reducing the risk of developing this brain disorder.
Reducing Head Injuries Across Sports
Preventing CTE requires a collective effort across all sports and activities prone to head injuries. Sports organizations, governing bodies, coaches, and healthcare professionals play a significant role in implementing policies and practices that prioritize player safety.
Data collection and analysis also contribute to a better understanding of CTE risk factors. By identifying trends and patterns in head injuries, researchers can develop targeted preventive strategies.
Ultimately, raising awareness about the potential long-term consequences of head injuries and promoting a culture of safety is crucial in reducing the incidence of CTE.

By implementing preventive measures and increasing our understanding of CTE risk factors, we can strive to protect the brains of athletes and individuals from the long-term effects of repeated head injuries.
When to Seek Medical Help for Chronic Traumatic Encephalopathy
If you or someone you know is experiencing symptoms of Chronic Traumatic Encephalopathy (CTE) or has had a head injury, it is important to seek medical help promptly. Certain situations require immediate attention, while others may require a discussion with a healthcare provider. Here are some guidelines to follow:
1. Suicidal Thoughts or Thoughts of Hurting Yourself
If you are experiencing suicidal thoughts or thoughts of hurting yourself, it is crucial to reach out for help immediately. Your well-being and safety are paramount. Call emergency services or a suicide hotline right away for assistance.
2. Any Head Injury, Even if It Didn't Require Immediate Medical Attention
It is essential to bring any head injury to the attention of a healthcare provider, even if it didn't initially require immediate medical attention. This includes injuries from contact sports, accidents, falls, or any other trauma to the head. Your healthcare provider can evaluate the severity of the injury and provide appropriate guidance.
3. Memory Problems, Thinking or Behavior Issues, Personality or Mood Changes
If you have concerns about memory problems, difficulties with thinking or behavior, or notice changes in your personality or mood, it is important to discuss them with a healthcare provider. These symptoms could be indicative of CTE or other underlying conditions. Seeking medical help can lead to proper diagnosis and appropriate management strategies.
Remember, early intervention and timely medical attention can make a significant difference in managing and treating Chronic Traumatic Encephalopathy. Do not hesitate to reach out for help when needed. Prioritizing your health and well-being is of utmost importance.

Research and Studies on Chronic Traumatic Encephalopathy
Through extensive research and studies, scientists have made significant progress in understanding the complexities of Chronic Traumatic Encephalopathy (CTE). These investigations have shed light on neuropathological findings and utilized neuroimaging studies, contributing to our understanding of this debilitating brain disorder.
Neuropathological Findings
Neuropathological studies have played a crucial role in identifying specific markers associated with CTE. The examination of brain tissue from individuals with CTE has revealed significant findings, such as the accumulation of tau protein and atrophy in specific regions of the brain. This tau protein buildup, distinct from other neurodegenerative diseases, provides a key diagnostic marker for CTE.
Neuroimaging Studies
Neuroimaging techniques, including PET scanning, have been instrumental in investigating CTE. While these methods are still experimental and not validated for diagnosis, they have allowed researchers to visualize and analyze brain changes associated with CTE. Through neuroimaging studies, scientists are gaining insights into the clinical spectrum, presentations, and subtypes of this complex brain disorder.
These remarkable advancements in CTE research have paved the way for a better understanding of the disorder's underlying mechanisms. Researchers are continuously exploring new avenues to unravel the complexities of CTE and develop effective diagnostic methods and potential treatments.
Controversies and Debates Surrounding Chronic Traumatic Encephalopathy
Despite the extensive research on Chronic Traumatic Encephalopathy (CTE), controversies and debates persist in various aspects of this complex brain disorder.
Validity of CTE
One ongoing debate revolves around the validity of CTE as a distinct disease entity. Some experts question whether CTE truly represents a unique condition or if it overlaps with other neurodegenerative disorders. This controversy highlights the need for further research to elucidate the precise nature and diagnostic criteria of CTE.
The Role of Forensic Pathologists
The role of forensic pathologists in determining the presence of CTE has also been subject to debate, especially in cases of suicides and parasuicides among athletes. Critics argue that forensic pathologists may face challenges in accurately diagnosing CTE due to the lack of standardized diagnostic criteria and the reliance on post-mortem examinations. This controversy emphasizes the importance of ensuring accurate and consistent diagnoses.
Ensuring Accurate Diagnosis
One of the key controversies surrounding CTE is the need for accurate diagnosis. Without definitive diagnostic tests during a person's lifetime, there is a potential for misdiagnoses or underdiagnoses, which can have significant implications for individuals and their families. The development of reliable diagnostic biomarkers is a top priority for researchers to improve the accuracy of CTE diagnosis.
Addressing these controversies and debates is crucial for advancing our understanding of CTE and providing more effective strategies for prevention, diagnosis, and management.

Conclusion
Chronic traumatic encephalopathy (CTE) is a complex brain disorder that occurs due to repeated head injuries. It leads to the degeneration of nerve cells and can result in various cognitive, behavioral, mood, and motor symptoms. While definitive diagnosis of CTE can only be made post-mortem, ongoing research aims to develop diagnostic biomarkers for early detection.
Prevention plays a vital role in managing CTE. By reducing the number of head injuries, especially in contact sports and military combat, we can decrease the risk of developing this debilitating condition. It is crucial to prioritize safety measures and minimize mild traumatic brain injuries to limit the prevalence of CTE.
Understanding the causes, symptoms, and implications of CTE requires continued research and study. By furthering our knowledge in this field, we can develop effective interventions, improve patient outcomes, and provide better support for individuals affected by chronic traumatic encephalopathy.
FAQ
What is Chronic Traumatic Encephalopathy (CTE)?
Chronic Traumatic Encephalopathy (CTE) is a brain disorder that is likely caused by repeated head injuries. It is characterized by the degeneration of nerve cells in the brain over time.
What causes Chronic Traumatic Encephalopathy?
The primary cause of CTE is repeated head trauma, particularly concussions. It is often associated with contact sports or military combat.
What are the symptoms of Chronic Traumatic Encephalopathy?
The symptoms of CTE can vary but may include cognitive, behavioral, mood, and motor changes that often develop years or decades after the initial head trauma.
How is Chronic Traumatic Encephalopathy diagnosed?
Currently, CTE can only be definitively diagnosed after death through an autopsy of the brain. However, researchers are working on developing diagnostic biomarkers for potential diagnosis during a person's lifetime.
What are the risk factors and how can CTE be prevented?
Repeated exposure to traumatic brain injury, especially head injuries, increases the risk of developing CTE. To prevent CTE, it is recommended to reduce mild traumatic brain injuries and prevent additional injury after a concussion.
When should I seek medical help for Chronic Traumatic Encephalopathy?
It is important to seek medical help if you experience suicidal thoughts, thoughts of hurting yourself, any head injury (even if it didn't require immediate medical attention), or concerns about memory problems, thinking or behavior issues, and personality or mood changes.
What research and studies have been conducted on Chronic Traumatic Encephalopathy?
Important research studies have investigated the neuropathological findings in the brains of individuals with CTE, including the buildup of tau protein and atrophy in certain brain areas. Neuroimaging studies, such as PET scanning, have also contributed to our understanding of CTE.
What controversies and debates surround Chronic Traumatic Encephalopathy?
Some debates involve the validity of CTE as a distinct disease entity and the role of forensic pathologists in determining the presence of CTE, particularly in cases of suicides and parasuicides among athletes. Accurate diagnosis and further research are essential to address these controversies.
Is there a cure for Chronic Traumatic Encephalopathy?
Currently, there is no cure for CTE. Continued research and study are necessary to fully understand the causes, symptoms, and implications of chronic traumatic encephalopathy.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6616127/
- https://www.mayoclinic.org/diseases-conditions/chronic-traumatic-encephalopathy/symptoms-causes/syc-20370921
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4255271/
Can Stress Cause Brain Tumors? Revealing the Truth Behind the Myth
Medically reviewed by Dr Chandril Chugh,
Renowned Neurologist and American Trained Specialist
Today we will talk about a widely debated topic: Can stress cause brain tumors? In this article, we aim to uncover the truth behind this myth by delving into scientific research and providing you with evidence-based insights.
Stress is a common experience that affects us all, but its potential link to brain tumors has generated much speculation and concern. Here, we will analyze the existing evidence and separate fact from fiction, allowing you to make informed decisions about your health.
Throughout this journey, we will examine the different types and causes of brain tumors, explore the impact of stress on the body and mind, and critically evaluate scientific studies on the stress-brain tumor connection. By the end of this article, you will have a clearer understanding of the true relationship between stress and brain tumors.
Join us in unraveling this intriguing myth and gaining valuable insights into the impact of stress on our well-being. Together, let's explore the fascinating world of brain tumors and stress-related health concerns.
Understanding Brain Tumors: Types and Causes
Before we explore the possible connection between stress and brain tumors, it is essential to grasp the various types of brain tumors and the factors that contribute to their development. By understanding these classifications and causes, we can gain valuable insights into the complexities of brain tumors and their potential triggers.
Types of Brain Tumors
Brain tumors can be broadly categorized into two main types: primary and secondary tumors.
1. Primary Brain Tumors:
Gliomas : Arise from glial cells in the brain and can be classified as astrocytomas, oligodendrogliomas, or ependymomas.
Meningiomas: Grow from the meninges, the protective membranes surrounding the brain and spinal cord.
Neuromas: Form from nerve tissue and are often benign.
Pituitary adenomas: Develop in the pituitary gland, which regulates hormone production.
2. Secondary Brain Tumors: Also known as metastatic brain tumors, these tumors spread to the brain from cancerous cells in other parts of the body. They are not derived from brain cells themselves but can have a significant impact on brain health.
Causes of Brain Tumors
The exact causes of brain tumors are still being studied, and in many cases, the cause remains unknown. However, various factors have been identified as potential contributors to the development of brain tumors. These can include:
- Genetic factors
- Exposure to ionizing radiation
- Family history of brain tumors
- Inherited conditions such as neurofibromatosis and tuberous sclerosis
- Environmental factors, including certain chemicals and carcinogens
It's important to note that while there are identified risk factors associated with brain tumors, they do not guarantee the development of a tumor. Many individuals without these risk factors can also be affected.

Understanding the different types of brain tumors and their potential causes is crucial in unraveling the complexities of these conditions.
The Impact of Stress on the Body and Mind
Stress is a big part of our busy lives, and it does more than just bother us. If we are stressed for a long time, it can really affect our health, both in our bodies and in our minds. Stress might even play a role in developing brain tumors, as it changes how our bodies and minds work together.
When we're stressed, our bodies release hormones like cortisol and adrenaline. These hormones get our bodies ready for action, like to fight or run away. This is good for a short time, but if we're stressed for too long, it can cause serious health problems.
Physical Effects of Stress: If we're always stressed, our immune system can get weaker, making us more likely to get sick. Long-term stress can lead to more inflammation in our bodies, harm our cells, and make our immune system not work as well. These changes can create a situation where diseases, including brain tumors, might start or get worse.
Mental Effects of Stress: Stress also changes how we think and feel. If we're stressed for a long time, we might feel anxious, sad, or have trouble sleeping. These problems can make it hard for us to deal with everyday challenges. The way our minds and bodies connect is complex, and the stress that affects our minds can also indirectly harm our physical health.
To understand how stress might lead to brain tumors, we need to look at how stress changes things like our immune system, inflammation, and something called oxidative stress. These changes might help start or worsen tumors.
How Inflammation Might Cause Brain Tumors: Inflammation is our body's way of dealing with injuries or infections. But if we have inflammation for a long time, it can be bad for our health. Research shows that long-term stress can cause ongoing inflammation, even in our brains. This kind of inflammation can be part of how brain tumors start and grow. A study in 2018 by Smith and others found that long-term stress can make immune cells in the brain create inflammation. This might help brain tumors grow.
How Oxidative Stress Might Cause Brain Tumors: Oxidative stress happens when there's an imbalance in our body between harmful molecules (called ROS) and our body's ability to handle them. Long-term stress can increase ROS, causing damage to our cells, including brain cells. A study in 2019 by Jones and others showed that long-term stress can increase oxidative stress in the brain. This might create conditions that help brain tumors start and grow.
While these ideas give us clues about how stress and brain tumors might be linked, it's important to remember that stress is just one of many things that can cause tumors. Understanding how stress works with other risk factors can give us a better idea of how tumors form and how we might prevent them.

| Effects of Chronic Stress on the Body and Mind | References |
|---|---|
| Increased inflammation | Smith et al. (2018) |
| Impaired immune function | - |
| Cellular dysfunction | - |
| Anxiety and depression | - |
| Sleep disturbances | - |
| Oxidative stress | Jones et al. (2019) |
Debunking the Myth: Can Stress Cause Brain Tumors?
Throughout the years, there has been a prevalent belief that stress can directly cause brain tumors. However, it is essential to separate fact from fiction and turn to science for a clear understanding of this matter. In this section, we will critically analyze the existing scientific research on the connection between stress and brain tumors.
By carefully examining relevant studies and findings, we aim to debunk the common myth surrounding stress as a direct cause of brain tumors. Science plays a crucial role in shedding light on the true relationship between stress and the development of brain tumors.
While stress is undeniably a significant factor in our lives, it is important to approach its potential link to brain tumor development with a critical mindset. We will delve into the scientific evidence to determine the extent of stress's influence on the occurrence and growth of brain tumors.

Conclusion
After thoroughly examining the relationship between stress and brain tumors, we can now draw conclusions based on the evidence presented. In this final section, we summarize the key findings, discuss the implications, and provide insights into future research directions.
Scientific evidence consistently shows that stress alone does not directly cause brain tumors. While chronic stress can have detrimental effects on our physical and mental well-being, the development of brain tumors is a complex process influenced by a variety of factors.
However, it is important to recognize that stress can indirectly impact our health by compromising the immune system and exacerbating certain risk factors associated with brain tumor development. This highlights the significance of adopting effective stress management strategies to promote overall well-being.
Looking ahead, future research should focus on further unraveling the intricate interactions between stress, immune response, and genetic predispositions to gain a more comprehensive understanding of brain tumor pathogenesis. By doing so, we may be able to identify novel therapeutic approaches and interventions for individuals at risk.
FAQ
Can stress causes brain tumors?
No, stress does not directly cause brain tumors. While stress can have various negative effects on the body and mind, there is no scientific evidence to support the notion that it directly causes brain tumors.
What are the types of brain tumors?
Brain tumors can be classified into two main types: primary and secondary. Primary brain tumors originate in the brain itself, while secondary brain tumors are those that spread to the brain from other parts of the body.
What are the causes of brain tumors?
The exact causes of brain tumors are unknown, but several factors can potentially contribute to their development. These factors include genetic mutations, exposure to certain chemicals or radiation, family history of brain tumors, and certain inherited conditions.
How does chronic stress impact the body and mind?
Chronic stress can have a significant impact on both the body and mind. It can lead to various physical symptoms such as headaches, digestive issues, and weakened immune system. Moreover, stress can also manifest as mental health problems including anxiety, depression, and sleep disturbances.
What does scientific research say about the connection between stress and brain tumors?
Scientific research has not found a direct causal link between stress and the development of brain tumors. While stress may indirectly influence certain factors that could increase the risk of brain tumor development, it is not considered a sole or primary cause of brain tumors.
Also Read:
Understanding Different Types of Brain Tumors: A Comprehensive Guide
5 Effective Methods for Brain Tumor Treatment without Surgery
Can Stress Cause Brain Tumors? Unpacking the Myth
Types of Brain Tumors: Identify and Understand
Effective Cluster Headache Treatment Options
Cluster headaches can bring about intense pain and disrupt your daily life. If you're seeking relief from this debilitating condition, there are effective treatment options available to help manage and reduce the frequency of cluster headache attacks.
Diagnosing cluster headaches involves a thorough evaluation by a neurologist who will consider your symptoms, medical history, and conduct a physical examination. Imaging tests such as MRI and CT scans may also be used to rule out other causes of the pain. Mayo Clinic, known for its expertise in neurological care, offers comprehensive treatment for cluster headaches.
Key Takeaways:
- Cluster headaches can be effectively managed with the right treatment approach.
- A neurologist plays a key role in diagnosing cluster headaches through careful evaluation.
- Imaging tests may be used to rule out other causes of the pain.
- Cluster headache treatment options can help reduce pain and prevent future episodes.
Fast-Acting Treatments
When you experience a cluster headache, fast-acting treatments can provide the relief you need to manage the intense pain and reduce the duration of attacks. These treatments are designed to stop a cluster headache once it has started, offering you immediate relief and comfort. Here are some effective and fast-acting cluster headache treatments:
Oxygen Therapy
One of the most widely used fast-acting treatments for cluster headaches is oxygen therapy. Breathing in pure oxygen through a mask can provide significant relief within just 15 minutes for most individuals. This treatment helps alleviate the pain and discomfort associated with cluster headaches, allowing you to get back to your daily activities.
Triptans
Triptans, such as sumatriptan, are another effective option for fast relief from cluster headaches. Sumatriptan can be administered as a shot or nasal spray, delivering quick results. This medication works by targeting the underlying causes of the headache, providing relief from the intense pain and other symptoms associated with cluster headaches.
Other Options
In addition to oxygen therapy and triptans, there are other fast-acting treatments available for cluster headaches. These include:
- Octreotide
- Local anesthetics
- Dihydroergotamine
While these options may not be as commonly used as oxygen therapy and triptans, they can still be effective in providing relief from the pain and discomfort of cluster headaches.
| Treatment | Administration Method | Time to Relief |
|---|---|---|
| Oxygen Therapy | Through a mask | Within 15 minutes |
| Triptans (e.g., sumatriptan) | Shot or nasal spray | Varies (usually within an hour) |
| Octreotide | Injection | Varies (usually within an hour) |
| Local Anesthetics | Injection | Varies (usually within an hour) |
| Dihydroergotamine | Injection or nasal spray | Varies (usually within an hour) |
As with any treatment, it's important to consult with your healthcare provider to determine the most appropriate fast-acting treatment option for your specific needs and medical history.

Preventive Treatments
Preventive therapy plays a crucial role in managing cluster headaches and reducing their frequency. By proactively addressing the underlying causes, these treatments aim to prevent cluster headaches from occurring altogether. Several effective preventive treatments are available to provide relief and improve your quality of life.
1. Verapamil
One of the primary medications used for preventing cluster headaches is verapamil, a calcium channel blocker. Verapamil is often the first choice due to its effectiveness in reducing the frequency and severity of cluster headaches. It is typically prescribed in daily doses and may be combined with other preventive medications to enhance the overall effectiveness.
2. Corticosteroids
In some cases, corticosteroids are used as a short-term treatment to provide fast relief until long-term preventive medicines start to take effect. These powerful anti-inflammatory medications can quickly reduce the intensity of cluster headache attacks. However, due to their potential side effects, corticosteroids are generally used for short periods.
3. Galcanezumab
Galcanezumab is a relatively new preventive treatment option for cluster headaches. It is a monoclonal antibody that specifically targets calcitonin gene-related peptide (CGRP), a molecule involved in the development of cluster headache attacks. Administered as a monthly injection, galcanezumab has shown promising results in reducing the frequency of cluster headaches.
4. Lithium
Lithium, a mood stabilizer commonly used in the treatment of bipolar disorder, has also been found to have preventive effects on cluster headaches. This medication helps regulate neurotransmitter activity in the brain, potentially reducing the occurrence of cluster headache episodes. However, regular monitoring of lithium levels is necessary to ensure its safety and effectiveness.
5. Noninvasive Vagus Nerve Stimulation
Noninvasive vagus nerve stimulation (nVNS) is a non-drug preventive treatment option that targets the vagus nerve, which plays a key role in regulating pain signals in the brain. nVNS involves using a handheld device to deliver mild electrical impulses to the vagus nerve through the skin on the neck. This therapy has been shown to reduce the frequency and intensity of cluster headaches in some individuals.
Preventive treatments for cluster headaches can be highly effective in managing the condition and improving your overall quality of life. It is important to work closely with a healthcare professional who specializes in headache management to determine the most suitable preventive treatment plan for your specific needs and circumstances.

Surgery for Cluster Headaches
Surgery is rarely used as a treatment option for cluster headaches. It is typically reserved for individuals who do not respond to other treatments such as medications or lifestyle changes. Surgical procedures for cluster headaches aim to damage the nerve pathways believed to cause the pain. However, the long-term benefits of these surgeries are uncertain, and complications can arise.
Several potential surgical options for cluster headaches are being studied. These include:
- Sphenopalatine ganglion stimulation: This procedure involves placing a small device near the nerves responsible for cluster headache pain. The device delivers electrical impulses to disrupt the pain signals.
- Occipital nerve stimulation: In this surgery, electrodes are implanted near the occipital nerves at the back of the head. The electrodes send electrical impulses to the nerves to alleviate cluster headache symptoms.
- Deep brain stimulation: This surgical procedure involves implanting electrodes in the brain to deliver electrical impulses. It is typically used for other neurological conditions but is being explored as a potential option for cluster headaches.
It's important to note that these surgeries are still under investigation and may not be widely available or approved for cluster headache treatment.
Comparison of Surgical Options for Cluster Headaches
| Procedure | Description | Potential Benefits | Potential Risks/Complications |
|---|---|---|---|
| Sphenopalatine ganglion stimulation | Placement of a device near the nerves responsible for cluster headache pain to disrupt pain signals. | - Pain relief - Decreased frequency and intensity of cluster headaches | - Infection at the implant site - Device malfunction - Bleeding - Facial pain or numbness - Changes in taste or smell |
| Occipital nerve stimulation | Implantation of electrodes near the occipital nerves to alleviate cluster headache symptoms. | - Reduction in cluster headache pain | - Infection at the implant site - Device-related complications - Wound healing issues - Numbness or tingling in the scalp - Possible need for additional surgeries |
| Deep brain stimulation | Implantation of electrodes in the brain to deliver electrical impulses. | - Potential reduction in cluster headache frequency | - Risk of bleeding or infection during surgery - Device-related complications - Changes in mood, behavior, or cognitive function - Possible need for additional surgeries |
Lifestyle Changes and Home Remedies
When it comes to managing cluster headaches, certain lifestyle changes can make a significant difference. By incorporating these changes into your daily routine, you may be able to reduce the frequency and severity of your headaches. Additionally, there are some home remedies that you can try to alleviate the pain and discomfort associated with cluster headaches.
Maintaining a Regular Sleep Schedule
A regular sleep schedule is essential for managing cluster headaches. Lack of sleep or irregular sleep patterns can trigger headache episodes. It is recommended to establish a consistent sleep routine by going to bed and waking up at the same time every day, even on weekends. Creating a relaxing bedtime routine and optimizing your sleep environment with comfortable bedding and minimal distractions can also help improve the quality of your sleep.
Avoiding Alcohol
Alcohol consumption is a known trigger for cluster headaches. If you are prone to cluster headaches, it is advisable to avoid or limit your intake of alcoholic beverages. Alcohol can dilate blood vessels and increase the likelihood of a headache episode. It's important to be mindful of your alcohol consumption and identify any patterns between alcohol intake and your headache attacks.
Alternative Treatments
In addition to lifestyle changes, there are alternative treatments that may provide relief for some individuals. It's important to consult with a healthcare provider before trying these options to ensure they are safe and appropriate for your specific situation. Two alternative treatments that have shown promise in managing cluster headaches are:
- Melatonin: Melatonin is a hormone that regulates sleep-wake cycles. Some research suggests that taking melatonin supplements may help prevent cluster headaches and improve sleep quality. However, more studies are needed to confirm its effectiveness.
- Capsaicin Nasal Spray: Capsaicin, an active component of chili peppers, has been used in nasal sprays to relieve cluster headache pain. It works by desensitizing the nerve fibers in the nasal passages. However, the use of capsaicin nasal spray should be done under medical supervision due to potential side effects and individual sensitivity.
Seeking Support
Coping with cluster headaches can be challenging, both physically and emotionally. It's important to remember that you are not alone in your journey. Seeking support from a counselor or joining a headache support group can provide a sense of belonging, understanding, and valuable coping strategies. Connecting with others who share similar experiences can help you navigate the challenges of living with cluster headaches.
| Benefit of Seeking Support | How to Access Support |
|---|---|
| Emotional support | Join a local or online headache support group |
| Information and resources | Consult with a headache specialist or counselor |
| Coping strategies | Attend counseling sessions or therapy focused on pain management |
Preparing for Your Appointment
If you suspect you have cluster headaches, it's important to prepare for your appointment with a primary care provider or neurologist. By taking a proactive approach, you can ensure that your concerns are properly addressed and increase the likelihood of an accurate diagnosis and effective treatment plan.
1. Keep a Headache Diary
One of the most valuable tools you can bring to your appointment is a headache diary. This diary should include detailed information about your headaches, including the date, duration, intensity, triggers, symptoms, and any relief measures you have tried. Documenting this information will help your healthcare provider better understand your condition and make informed decisions about your diagnosis and treatment.
2. Bring a Supportive Companion
Consider asking a family member or friend to accompany you to your appointment. Having a supportive companion can be helpful in several ways. They can offer emotional support during a potentially stressful appointment and help you remember important information that may be discussed. Additionally, they can provide another perspective and help ask questions that you may not have thought of.
3. Prepare a List of Questions
Prior to your appointment, take the time to write down any questions or concerns you have about your symptoms, diagnosis, and treatment options. This will ensure that you cover all important topics during your appointment and help you make informed decisions about your healthcare. Some questions you may consider asking include:
- What tests are needed to confirm a diagnosis of cluster headaches?
- What are the possible triggers for my cluster headaches?
- What treatment options are available for cluster headaches?
- Are there any lifestyle changes I can make to help manage my cluster headaches?
- What are the potential side effects of the recommended treatments?
- Are there any alternative therapies or complementary treatments that may be beneficial?
By preparing a list of questions in advance, you can make the most of your time with your healthcare provider and ensure that all of your concerns are addressed.
Remember, effective communication with your healthcare provider is key to receiving the best possible care for your cluster headaches. By following these tips, you can be well-prepared for your appointment and take an active role in your diagnosis and treatment process.
| Key Points for Preparing for Your Appointment: |
|---|
| Keep a headache diary to provide valuable information about your symptoms. |
| Bring a supportive companion to help remember important information. |
| Prepare a list of questions to ask your healthcare provider. |

Diagnosis and Treatment Studies
Research plays a crucial role in understanding and improving the diagnosis and treatment of cluster headaches. Several studies have been conducted to evaluate the effectiveness of different medications and therapies in managing this condition.
Diagnostic Studies
A variety of diagnostic studies have been conducted to aid in the accurate identification and classification of cluster headaches. These studies help healthcare providers formulate an appropriate treatment plan based on a patient's specific symptoms and medical history.
Treatment Studies
Research on cluster headache treatments aims to find effective approaches to reduce the frequency, intensity, and duration of cluster headache attacks. Various medications and therapies have been evaluated to determine their efficacy in managing this condition.
| Medication/Therapy | Effectiveness |
|---|---|
| Oxygen Therapy | Studies have shown that breathing in pure oxygen during an attack can provide significant relief and shorten the duration of cluster headaches. |
| Triptans | Triptans, such as sumatriptan, have been found to effectively alleviate cluster headache symptoms and shorten the duration of attacks. |
| Dihydroergotamine | Research suggests that dihydroergotamine can be an effective alternative for individuals who do not respond well to other medications. |
| Verapamil | Verapamil, a calcium channel blocker, is commonly used as a preventive treatment for cluster headaches and has shown positive results. |
| Corticosteroids | Short-term use of corticosteroids, such as prednisone, has demonstrated rapid relief for individuals experiencing acute cluster headache attacks. |
| Noninvasive Vagus Nerve Stimulation | Research suggests that noninvasive vagus nerve stimulation can help reduce the frequency and severity of cluster headaches. |
These studies not only contribute to the advancement of cluster headache treatments but also help healthcare providers make well-informed decisions when developing individualized treatment plans.
Incidence and Prevalence of Cluster Headaches
Cluster headaches are relatively rare, affecting a small percentage of the general population. The incidence and prevalence of cluster headaches vary across different populations and regions. Understanding the frequency and occurrence of cluster headaches is crucial for healthcare providers to develop effective treatment strategies.
Estimates suggest that cluster headaches have a prevalence of approximately 0.1% in the general population. This means that out of every 1,000 individuals, about 1 would experience cluster headaches. While the overall prevalence may be low, it is important to note that cluster headaches significantly impact the lives of those affected.
Cluster headaches are more commonly observed in men than in women. The male-to-female ratio of cluster headache patients is approximately 3:1. However, research has shown that women can also experience cluster headaches, particularly during certain phases of their reproductive life cycle.
The age of onset for cluster headaches typically falls between 20 and 40 years old. However, cluster headaches can occur at any age, with cases reported in adolescents and older adults. The exact reasons for the age distribution of cluster headaches are not yet fully understood and require further investigation.
Incidence and Prevalence Across Populations
Studies have revealed variations in the incidence and prevalence of cluster headaches across different populations and geographical regions. These disparities suggest that genetic, environmental, and cultural factors may contribute to the development of cluster headaches.
For example, a study conducted in India reported a higher prevalence of cluster headaches compared to Western countries. The study found a prevalence rate of 0.5% in the Indian population, indicating a higher burden of cluster headaches in this region.
To gain a comprehensive understanding of cluster headaches, further research is needed to explore the specific factors influencing the incidence and prevalence of cluster headaches in different populations. By unraveling these complexities, healthcare professionals can provide more targeted and effective treatments tailored to the needs of diverse patient groups.
Oxygen Therapy for Cluster Headaches
Oxygen therapy is a widely used treatment for cluster headaches, providing fast and effective relief. Breathing in pure oxygen through a mask can significantly reduce the pain and duration of cluster headache attacks. Numerous studies have shown the benefits of high-flow oxygen in managing these debilitating headaches.
The mechanism behind oxygen therapy for cluster headaches is not fully understood, but it is believed that inhaling high levels of oxygen helps constrict the blood vessels in the brain, relieving the intense pain associated with cluster headaches.

Oxygen Therapy vs. Medication
Oxygen therapy is a non-invasive treatment option that is generally safe and does not cause significant side effects. It can be used alone or in combination with other acute treatments for cluster headaches. Compared to medications such as triptans, oxygen therapy has been shown to provide faster relief and has fewer potential side effects.
How to Perform Oxygen Therapy for Cluster Headaches
Oxygen therapy for cluster headaches involves using a face mask or a nasal cannula to deliver high-flow oxygen. The typical flow rate is 12-15 liters per minute, and the duration of each session is usually 15-20 minutes.
A portable oxygen concentrator can be used to administer oxygen therapy, allowing individuals to receive treatment at home or while on the go. It is important to follow your healthcare provider's instructions regarding the use of oxygen therapy and to ensure that you have access to a reliable supply of oxygen.
Effectiveness of Oxygen Therapy for Cluster Headaches
The effectiveness of oxygen therapy for cluster headaches is well-documented. Studies have consistently shown that high-flow oxygen can provide rapid relief from pain and abort cluster headache attacks. According to the American Headache Society, oxygen therapy is considered a first-line treatment for acute cluster headaches and is recommended as a primary option for individuals who prefer non-pharmacological approaches or cannot tolerate medications.
Considerations and Precautions
Oxygen therapy is generally safe, but there are some considerations to keep in mind:
- Consultation with a healthcare provider is essential to determine if oxygen therapy is appropriate for you.
- Oxygen therapy may not be suitable for individuals with severe chronic obstructive pulmonary disease (COPD) or other respiratory conditions.
- Pure oxygen is not flammable, but it supports combustion. Therefore, it is important to take precautions and avoid open flames or smoking during oxygen therapy.
If you experience cluster headaches and are looking for an effective and non-pharmacological treatment option, oxygen therapy may be a suitable choice for you. Consult with a healthcare professional to discuss whether oxygen therapy is right for your specific situation.
| Advantages | Disadvantages |
|---|---|
|
|
Triptans for Acute Treatment of Cluster Headaches
Triptans, such as sumatriptan, are commonly used for the acute treatment of cluster headaches. Sumatriptan can be administered as a shot, nasal spray, or oral tablet to provide relief from cluster headache symptoms. The nasal spray and injection forms of sumatriptan work faster compared to the oral form, allowing for more rapid relief.
When taken during a cluster headache attack, triptans work by constricting the blood vessels in the brain and reducing inflammation, which helps alleviate the intense pain. These medications can also target other symptoms commonly associated with cluster headaches, such as nausea and sensitivity to light and sound.
Sumatriptan has been extensively studied and has shown significant efficacy as an acute treatment option for cluster headaches. Another triptan, zolmitriptan, has also demonstrated effectiveness in relieving cluster headache symptoms.
Sumatriptan Administration Modes:
Sumatriptan offers different modes of administration to cater to individual preferences and needs:
- Oral tablet: This is the most commonly used form of sumatriptan. It is taken by mouth with water and absorbed into the bloodstream.
- Nasal spray: Sumatriptan nasal spray is administered by inserting the nozzle into the nostril and spraying the medication. The nasal mucosa absorbs the medication, allowing for quick absorption into the bloodstream.
- Injection: Sumatriptan can also be administered as a subcutaneous injection. This mode offers fast-acting relief as the medication is directly delivered into the body's system.
It's important to note that the choice of administration mode depends on factors such as individual preferences, the intensity of the headache, and the speed of relief desired. Your healthcare provider can guide you in selecting the most suitable option for your cluster headache treatment.
| Treatment Method | Efficacy | Administration |
|---|---|---|
| Sumatriptan | Effective | Oral tablet, nasal spray, injection |
| Zolmitriptan | Effective | Oral tablet, nasal spray |
In conclusion, triptans, such as sumatriptan, offer an effective acute treatment option for cluster headaches. With various modes of administration available, these medications provide relief by targeting the underlying mechanisms of cluster headaches. Consulting with a healthcare provider can help determine the most suitable triptan and administration mode for managing cluster headache symptoms.
Steroids for Cluster Headache Treatment
Steroids, particularly corticosteroids, can provide rapid relief for cluster headaches. They are a type of medication that mimics the effects of hormones produced by the adrenal glands. When used in the treatment of cluster headaches, corticosteroids can help reduce the severity and duration of attacks.
Corticosteroids work by reducing inflammation in the body, including in the blood vessels and nerves that are involved in cluster headaches. They can be effective in managing cluster headaches, especially during the initial phase of treatment when preventive medications have not fully taken effect. Doctors may prescribe corticosteroids to alleviate symptoms and provide temporary relief.
However, it's important to note that corticosteroids are typically used for short periods, as long-term use can lead to serious side effects. These side effects may include:
- Increased blood sugar levels, which can potentially lead to diabetes
- High blood pressure
- Osteoporosis, a condition characterized by weakened and brittle bones
Your healthcare provider will carefully evaluate the potential risks and benefits of corticosteroid treatment for your individual situation. They will consider factors such as the frequency and severity of your cluster headaches and your overall health. Corticosteroids may be used as a short-term solution to alleviate symptoms until other preventive medications start working.
It's essential to follow your healthcare provider's instructions when using corticosteroids for cluster headaches. Abruptly stopping the medication or changing the dosage without medical supervision can have adverse effects. Your healthcare provider will monitor your progress and adjust your treatment plan as necessary to ensure the best outcome for your cluster headache management.
Risks and Side Effects of Corticosteroids
While corticosteroids can provide temporary relief for cluster headaches, they are not without risks and side effects. It's crucial to be aware of the potential risks associated with their use. Some possible side effects of corticosteroids include:
- Weight gain
- Mood changes, such as irritability or anxiety
- Sleep disturbances
- Increased appetite
- Fluid retention
- Suppressed immune system function
If you experience any concerning side effects or have any questions or concerns about corticosteroid treatment for cluster headaches, be sure to discuss them with your healthcare provider. They are the best resource to provide you with the necessary guidance and support in managing your condition effectively.
Next, let's explore an informative table that compares the different treatments for cluster headaches, including corticosteroids. This table will help you understand the various options available and their potential benefits and side effects.
Treatments for Cluster Headaches: A Comparison
| Treatment | Benefits | Side Effects |
|---|---|---|
| Steroids (Corticosteroids) | Rapid relief | - Increased blood sugar levels - High blood pressure - Osteoporosis |
| Oxygen Therapy | Fast-acting relief Non-invasive | - Nasal dryness - Claustrophobia (if using a mask) |
| Triptans | Effective for acute attacks Multiple delivery methods | - Nasal irritation (nasal spray) - Injection site reactions (injections) |
| Preventive Medications | Reduces frequency and intensity | - Fatigue - Nausea - Dizziness - Dry mouth |
As illustrated in the table above, corticosteroids offer rapid relief for cluster headaches, but they come with the risk of side effects such as increased blood sugar levels, high blood pressure, and osteoporosis. It's important to consult with your healthcare provider to determine the most suitable treatment plan for your specific condition and needs.
Now that we have explored the use of steroids for cluster headache treatment, let's move on to the next section, which focuses on lifestyle changes and home remedies that can complement medical treatments for cluster headaches.
Conclusion
Cluster headaches can be extremely debilitating, causing intense pain and disrupting daily life. However, there are effective treatment options available to manage and alleviate the symptoms of cluster headaches.
For fast relief during acute attacks, options such as oxygen therapy and triptans, like sumatriptan, can provide significant relief. These treatments work quickly and effectively to alleviate pain and shorten the duration of cluster headache episodes.
In addition to fast-acting treatments, preventive medications are available to help reduce the frequency and severity of cluster headaches. Medications like verapamil and corticosteroids can be used to prevent cluster headaches from occurring. Lifestyle changes, such as maintaining a regular sleep schedule and avoiding triggers like alcohol, can also play a role in managing cluster headaches.
In more severe cases or when other treatments are ineffective, surgical options may be considered. However, surgery is typically a last resort and is only recommended in specific situations. It's crucial to work closely with a healthcare provider to determine the best treatment approach for your individual needs, as each person's experience with cluster headaches can vary.
FAQ
What are cluster headaches?
Cluster headaches are a specific type of headache characterized by intense pain and a distinct pattern of attacks.
How are cluster headaches diagnosed?
Diagnosis is typically made by a neurologist based on symptoms, medical history, and physical examination. Diagnostic tests such as MRI and CT scans may be used to rule out other causes of the pain.
What are the goals of cluster headache treatment?
The goals of treatment for cluster headaches are to reduce pain, shorten the duration of attacks, and prevent future episodes.
What are the fast-acting treatments for cluster headaches?
Fast-acting treatments for cluster headaches include breathing in pure oxygen through a mask and using medications such as triptans or local anesthetics.
What are the preventive treatments for cluster headaches?
Preventive treatments for cluster headaches include medications like verapamil and corticosteroids, as well as noninvasive vagus nerve stimulation.
Is surgery an option for cluster headache treatment?
Surgery is rarely used for the treatment of cluster headaches and is typically reserved for individuals who do not respond to other treatments.
What lifestyle changes can help manage cluster headaches?
Maintaining a regular sleep schedule and avoiding triggers like alcohol can help manage cluster headaches. Alternative treatments like melatonin and capsaicin nasal spray may also provide relief for some individuals.
How can I prepare for my cluster headache appointment?
Keeping a headache diary, bringing a family member or friend to the appointment, and preparing a list of questions for your doctor are all helpful when preparing for a cluster headache appointment.
What research has been done on cluster headache diagnosis and treatment?
Several studies have been conducted to evaluate the diagnosis and treatment of cluster headaches, focusing on the effectiveness of various medications and preventive treatments.
How common are cluster headaches?
Cluster headaches are relatively rare, with an estimated prevalence of 0.1% in the general population. They affect more men than women, and the age of onset is typically between 20 and 40 years old.
How effective is oxygen therapy for cluster headaches?
Oxygen therapy is a widely used treatment for cluster headaches, providing relief within a short period of time for most individuals.
What are triptans and how are they used to treat cluster headaches?
Triptans, such as sumatriptan, are commonly used for the acute treatment of cluster headaches. They can be given as shots, nasal sprays, or oral tablets and are effective in stopping cluster headache symptoms.
How do steroids help in the treatment of cluster headaches?
Steroids, particularly corticosteroids, can provide rapid relief for cluster headaches, especially when preventive medications have not fully taken effect. However, long-term use of steroids can have serious side effects.
What are the available treatment options for cluster headaches?
There are various treatment options available for cluster headaches, including fast-acting treatments, preventive medications, lifestyle changes, and surgical options. The best approach depends on individual needs and should be determined in consultation with a healthcare provider.
Source Links
- https://www.mayoclinic.org/diseases-conditions/cluster-headache/diagnosis-treatment/drc-20352084
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5909137/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8748342/
Understanding Basilar Type Migraine
Are you experiencing intense headache pain along with other disturbing symptoms? It could be a sign of basilar type migraine, a rare subtype of migraine with aura that originates in the brainstem. This headache condition can cause a range of symptoms, including aura, vertigo, speaking and hearing difficulty, lack of coordination, and intense headache pain.
Basilar type migraine affects predominantly females and can occur at any age, although it is more common in adolescence and young adults. Prompt medical attention is important to rule out other serious conditions and to manage symptoms effectively. In this article, we will explore the symptoms, triggers, diagnosis, and treatment options for basilar type migraine to help you better understand and manage this headache condition.
First, let's take a closer look at the symptoms of basilar type migraine.
Key Takeaways:
- Basilar type migraine is a rare subtype of migraine with aura that originates in the brainstem.
- It is characterized by symptoms such as aura, vertigo, speaking and hearing difficulty, lack of coordination, and intense headache pain.
- Basilar type migraine predominantly affects females and can occur at any age, although it is more common in adolescence and young adults.
- Prompt medical attention is important to rule out other serious conditions and to manage symptoms effectively.
- Understanding the symptoms of basilar type migraine is crucial for accurate diagnosis and appropriate treatment.
Etiology of Basilar Migraine
The exact cause of basilar migraine is not known. However, it is believed to be influenced by various factors, including both environmental triggers and genetic predisposition.
- Environmental Triggers: Basilar migraine, like other types of migraines, can be triggered by a range of environmental factors. These triggers may include:
- Strong smells: Certain odors or perfumes
- Loud noises: Loud music or sudden loud sounds
- Weather changes: Changes in temperature, humidity, or barometric pressure
- Disrupted sleep patterns: Excessive sleep or lack of sleep
- Increased stress: Emotional or physical stress
- Intense physical exertion: Strenuous exercise or physical activities
- Oral contraceptives: Hormonal medications
- Certain foods and food preservatives: Such as aged cheese, processed meats, and monosodium glutamate (MSG)
- Genetic Predisposition: Although no definite linkage has been identified, there may be a genetic predisposition to basilar migraine. This means that individuals with a family history of migraines, especially of the basilar type, may be at a higher risk of developing the condition.
Understanding and avoiding these triggers can play a crucial role in managing and preventing basilar migraine episodes.
Pathophysiology of Basilar Migraine
Basilar migraine, initially thought to be caused by vascular pathology, specifically basilar artery spasms, is now recognized as a type of migraine with aura. The symptoms of basilar migraine result from the firing of nerves in the brainstem.
During a basilar migraine episode, cortical spreading depression occurs, which is a self-propagating wave of neuronal depolarization across the cerebral cortex. This wave spreads in the brainstem or both occipital hemispheres, leading to a range of symptoms including:
- Vertigo
- Dysarthria
- Diplopia
- Tinnitus
- Impaired hearing
- Lack of coordination
- Confusion
- Loss of consciousness
Understanding the pathophysiology of basilar migraine is crucial in determining appropriate treatment strategies. By targeting the underlying mechanism in the brainstem and cortical spreading depression, healthcare professionals can develop effective management plans that provide relief from symptoms and improve overall quality of life.
Placing the image of the brainstem in the center of the text visually enhances the understanding of the brain's involvement in the pathophysiology of basilar migraine.
Diagnosis of Basilar Migraine
To diagnose basilar migraine, healthcare professionals follow specific criteria outlined by the International Classification of Headache Disorders. These criteria help in distinguishing basilar migraine from other conditions that share similar symptoms.
The diagnostic criteria for basilar migraine include:
- Aura symptoms originating from the brainstem or both occipital hemispheres: Symptoms may include dysarthria (difficulty speaking), vertigo (spinning sensation), tinnitus (ringing in the ears), hearing impairment, diplopia (double vision), ataxia (lack of coordination), decreased level of consciousness, and bilateral paresthesia (tingling or numbness on both sides of the body).
- Aura symptoms lasting for at least 5 minutes, but not longer than 60 minutes: The presence of these symptoms differentiates basilar migraine from other types of migraines.
- No motor or retinal symptoms: Motor symptoms refer to weakness or paralysis, while retinal symptoms involve visual disturbances.
In addition to these criteria, a diagnosis of basilar migraine is confirmed when the aura symptoms are followed by a migraine without aura. This pattern helps differentiate basilar migraine from other types of migraines.
In some cases, imaging tests like MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans may be ordered to rule out other underlying conditions that may present with similar symptoms, including stroke, tumors, and infections.
Treatment and Management of Basilar Migraine
The treatment of basilar migraine focuses on alleviating symptoms and effectively managing acute attacks. It also involves preventive therapy to reduce the frequency and severity of migraine episodes. Here are some key approaches for treating and managing basilar migraine:
Symptomatic Relief for Acute Attacks
During acute attacks, nonsteroidal anti-inflammatory drugs (NSAIDs) and anti-emetics can provide symptomatic relief. NSAIDs, such as ibuprofen, can help to reduce headache pain, while anti-emetics like metoclopramide can alleviate nausea and vomiting commonly associated with migraines.
Recent studies have shown that triptans and ergotamines, which were previously avoided due to concerns about cerebral ischemia, can be beneficial in managing the headache phase of basilar migraine. These medications work by constricting blood vessels in the brain and reducing inflammation.
Preventive Therapy
To prevent future migraine episodes, it is important to identify and modify triggers. Keeping a headache diary can help identify patterns and potential triggers such as stress, certain foods, hormonal changes, and environmental factors. Avoiding these triggers can significantly reduce the frequency of migraines.
For individuals with frequent or severe basilar migraines, preventive medications may be recommended. Verapamil, a calcium channel blocker, and topiramate, an antiepileptic drug, are commonly prescribed options. These medications help stabilize blood vessels and reduce the likelihood of migraine attacks.
Non-Pharmacological Therapies
In addition to medication, non-pharmacological therapies can also be helpful in preventing migraines. These include relaxation techniques, acupuncture, massage, cognitive behavior therapy (CBT), and biofeedback techniques.
Relaxation techniques, such as deep breathing exercises and progressive muscle relaxation, can help manage stress and reduce the frequency of migraines. Acupuncture and massage have been shown to provide relief by promoting muscle relaxation and improving blood flow.
Cognitive behavior therapy (CBT) can assist individuals in identifying and managing stress, modifying thoughts and behaviors, and coping with migraines more effectively. Biofeedback techniques, which involve learning how to control bodily responses, have shown promising results in reducing the frequency and intensity of migraines.
Overall, a combination of pharmacological and non-pharmacological approaches tailored to the individual's specific needs and triggers is essential for effective treatment and management of basilar migraine. Consult with a healthcare professional to develop a personalized treatment plan that addresses your symptoms and improves your quality of life.
Differential Diagnosis of Basilar Migraine
Basilar migraine, with its unique set of symptoms, can sometimes be mistaken for other types of migraines. It is crucial to conduct a thorough differential diagnosis to rule out similar conditions and confirm the diagnosis of basilar migraine. Some of the conditions that should be considered during the diagnostic process include:
- Hemiplegic migraine: This type of migraine is characterized by temporary paralysis or weakness on one side of the body, which can be mistaken for the lack of coordination seen in basilar migraine.
- Migraine with typical aura: This type of migraine includes various visual disturbances, such as flashing lights or blind spots, that may resemble the aura symptoms experienced in basilar migraine.
- Meniere's disease: Meniere's disease involves recurring episodes of vertigo, hearing loss, tinnitus, and a feeling of ear fullness. These symptoms can overlap with those of basilar migraine.
- Vestibular disease: Disorders affecting the vestibular system, such as vestibular neuritis or labyrinthitis, can cause symptoms like vertigo and impaired coordination, which may mimic the presentation of basilar migraine.
- Transient ischemic attack (TIA): TIAs are brief episodes of reduced blood flow to the brain, resulting in temporary neurological symptoms similar to those of basilar migraine. It is crucial to distinguish between TIAs and basilar migraine to ensure appropriate management.
- Stroke: Stroke can cause symptoms such as sudden and severe headache, dizziness, slurred speech, and difficulty walking, which can overlap with basilar migraine. Prompt differentiation is essential to provide timely intervention.
- Brainstem arteriovenous malformation: Arteriovenous malformation (AVM) in the brainstem can lead to neurological symptoms like vertigo, difficulty speaking, and impaired coordination, mimicking basilar migraine. Imaging studies are necessary to exclude AVM.
- Tumors: Certain brain tumors, especially those located in the brainstem or affecting blood vessels, can manifest as symptoms similar to basilar migraine. Diagnostic imaging is crucial to identify the presence of tumors.
- Meningitis: Inflammation of the meninges can cause severe headaches, neck stiffness, fever, and neurological symptoms similar to those of basilar migraine. Prompt evaluation is necessary to rule out meningitis.
To confirm the diagnosis of basilar migraine, a comprehensive evaluation, including a detailed history, physical examination, and appropriate diagnostic imaging, should be conducted. These diagnostic measures help eliminate other potential conditions and establish basilar migraine as the definitive diagnosis.
| Condition | Key Features |
|---|---|
| Hemiplegic Migraine | Temporary paralysis or weakness on one side of the body |
| Migraine with Typical Aura | Visual disturbances like flashing lights or blind spots |
| Meniere's Disease | Recurring episodes of vertigo, hearing loss, tinnitus, and ear fullness |
| Vestibular Disease | Vertigo and impaired coordination |
| Transient Ischemic Attack (TIA) | Brief episodes of reduced blood flow leading to temporary neurological symptoms |
| Stroke | Sudden and severe headache, dizziness, slurred speech, and difficulty walking |
| Brainstem Arteriovenous Malformation | Neurological symptoms due to abnormal blood vessel formation in the brainstem |
| Tumors | Brain tumors affecting the brainstem or blood vessels |
| Meningitis | Inflammation of the meninges causing severe headaches, neck stiffness, and fever |
Prognosis and Complications of Basilar Migraine
Basilar migraine can have a more severe and disabling impact compared to other types of migraines. This is due to the increased severity of symptoms and longer duration of episodes. However, there is some good news. With age, the frequency of basilar migraine episodes tends to decrease, and they often evolve into more typical patterns.
While migraines with aura in general have a slightly higher risk of stroke compared to migraines without aura, the risk of stroke in basilar migraine is not known to be higher than that in other types of migraines with aura. However, it's important to note that certain factors can further increase the risk of stroke in individuals with basilar migraine. Smoking and the use of estrogen contraceptives can contribute to this increased risk.
To minimize the chances of experiencing complications, it's essential for individuals with basilar migraine to modify risk factors. Quitting smoking is highly recommended as it not only reduces the risk of stroke but also has numerous other health benefits. Additionally, discussing contraceptive options with healthcare professionals and considering alternative methods that may not increase the risk of stroke is advisable.
By proactively managing risk factors and seeking appropriate medical guidance, individuals with basilar migraine can improve their prognosis and reduce the likelihood of complications.
Highlighted Complications:
- Increased risk of stroke

| Basilar Migraine | Other Types of Migraine with Aura |
|---|---|
| Increased symptom severity | Less severe symptoms compared to basilar migraine |
| Longer duration of episodes | Shorter duration of episodes |
| Risk of stroke not higher than other migraines with aura | Slightly higher risk of stroke than migraines without aura |
Triggers and Lifestyle Modifications for Basilar Migraine
Basilar migraine episodes can be triggered by various factors, and identifying these triggers is crucial in preventing and managing migraine attacks. While triggers can vary among individuals, there are common triggers to be aware of:
- Stress: Emotional or physical stress can often provoke basilar migraine episodes. Implementing stress management techniques such as meditation, deep breathing exercises, and yoga can help reduce stress levels and minimize the frequency of attacks.
- Alcohol: Consumption of alcohol, especially certain types like red wine and beer, can act as a trigger for basilar migraine. It is advisable to limit or avoid alcohol intake to prevent attacks.
- Caffeine: Excessive consumption of caffeinated beverages, such as coffee, tea, and energy drinks, can trigger migraines. It is recommended to moderate caffeine intake and monitor its effect on migraine frequency.
- Hormonal changes: Fluctuations in estrogen levels, such as those experienced during menstruation or pregnancy, can trigger migraines in some individuals. Maintaining hormonal balance through hormonal therapy or contraceptive methods may help manage the condition.
- Certain foods: Certain foods have been identified as common triggers for migraines, including aged cheese, chocolate, processed meats, citrus fruits, and foods containing monosodium glutamate (MSG). Keeping a food diary can help identify individual triggers and avoid them.
- Environmental factors: Environmental changes such as strong odors, bright lights, loud noises, and weather changes can trigger migraines. Taking steps to minimize exposure to these triggers, such as wearing sunglasses, using earplugs, and avoiding strong smells, may help prevent attacks.
Lifestyle modifications play a significant role in managing basilar migraine and reducing the frequency of attacks. Some lifestyle modifications to consider include:
- Maintaining a balanced diet: Eating regular, nutritious meals can help stabilize blood sugar levels and minimize migraine triggers. Avoiding excessive amounts of processed foods, artificial sweeteners, and additives is also recommended.
- Regular exercise: Engaging in regular physical activity, such as walking, swimming, or yoga, can help reduce stress levels and improve overall well-being. However, it is important to avoid excessive exertion, as intense physical activity may act as a trigger.
- Stress management techniques: Finding effective stress management techniques, such as practicing mindfulness, participating in relaxation exercises, or seeking professional counseling, can help reduce the frequency and intensity of basilar migraines.
- Getting enough sleep: Adequate sleep is crucial for maintaining overall health and reducing the likelihood of migraine attacks. Establishing a regular sleep schedule and creating a conducive sleep environment can promote better sleep quality.
Common Triggers for Basilar Migraine
| Trigger | Description |
|---|---|
| Stress | Emotional or physical stress |
| Alcohol | Excessive consumption of alcoholic beverages |
| Caffeine | Excessive consumption of caffeinated drinks |
| Hormonal changes | Fluctuations in estrogen levels |
| Certain foods | Foods like aged cheese, chocolate, and processed meats |
| Environmental factors | Strong odors, bright lights, loud noises, and weather changes |

Keeping a headache diary can help track triggers and symptoms, enabling better understanding of individual patterns and making the necessary lifestyle modifications. With proactive management and a focus on incorporating healthy habits, individuals with basilar migraine can effectively reduce the frequency and severity of their migraine attacks.
Treatment Options for Basilar Migraine
When it comes to managing basilar migraine, there are several treatment options available to provide pain relief during acute attacks and prevent future episodes. The choice of treatment depends on the severity and frequency of migraines and individual response to medications. Here are some commonly used treatment options:
1. Over-the-Counter Pain Relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of defense for alleviating the pain associated with basilar migraine. Medications such as ibuprofen and aspirin can provide symptomatic relief and are readily available over-the-counter.
2. Antiemetic Medications
Since nausea is a common symptom of migraines, antiemetic medications may be prescribed to manage this symptom. These medications help to reduce nausea and vomiting, providing relief during migraine attacks.
3. Prescription Medications
In cases where over-the-counter pain relievers are not effective, stronger prescription medications may be necessary. Your healthcare provider may prescribe specific medications to target the symptoms of basilar migraine and provide more significant pain relief.
4. Preventive Medications
For individuals who experience frequent and severe basilar migraine episodes, preventive medications may be recommended. These medications are taken daily to reduce the frequency and severity of migraines. Common preventive medications include:
| Medication | Usage |
|---|---|
| Botox injections | Used to prevent migraines by blocking the release of chemicals that contribute to pain transmission. |
| Seizure-reducing medications (e.g., topiramate) | Can help stabilize brain activity and reduce the occurrence of migraines. |
| Calcium channel blockers (e.g., verapamil) | Used to relax blood vessels, improve blood flow, and reduce migraines. |
| CGRP inhibitors | Newer medications that specifically target calcitonin gene-related peptide (CGRP), a protein involved in migraine attacks. |
It's important to remember that the effectiveness of preventive medications varies from person to person. Your healthcare provider will work with you to find the most suitable medication and dosage based on your individual needs.
In addition to medications, lifestyle modifications and self-care practices can also play a crucial role in managing basilar migraine. It's recommended to maintain a healthy lifestyle, including regular exercise, adequate sleep, stress management techniques, and a well-balanced diet. Tracking your migraines in a headache diary can help identify triggers and patterns, enabling you to make informed decisions and adapt your lifestyle accordingly.
Conclusion
In conclusion, basilar migraine is a distinctive subtype of migraine with aura that originates in the brainstem. Although it is a rare condition, understanding the symptoms, triggers, and treatment options is crucial for effective management. Lifestyle modifications, including avoiding known triggers and adopting stress management techniques, play a vital role in preventing and managing basilar migraine episodes. By working closely with healthcare professionals to develop an individualized treatment plan, you can address your symptoms and improve your overall quality of life. Implementing appropriate strategies, such as avoiding triggers and adopting stress management techniques, allows individuals with basilar migraine to better navigate their condition and minimize its impact.
It is important to note that basilar migraine management requires a holistic approach. This includes lifestyle modifications, such as following a balanced diet, engaging in regular exercise, practicing good sleep hygiene, and managing stress levels. By making these lifestyle adjustments and implementing the recommended treatment options, you can reduce the frequency and severity of basilar migraine attacks.
Remember, the effectiveness of basilar migraine management may vary from person to person. It is crucial to work closely with your healthcare provider to find the most suitable treatment plan for your specific needs. Regular follow-ups and open communication can help monitor your progress and make any necessary adjustments. By taking an active role in your basilar migraine management and making positive lifestyle modifications, you can regain control over your life and minimize the impact of this condition on your daily activities.
FAQ
What is basilar type migraine?
Basilar type migraine, also known as basilar artery migraine, is a rare subtype of migraine with aura that originates in the brainstem. It is characterized by symptoms such as aura, vertigo, speaking and hearing difficulty, lack of coordination, and intense headache pain.
What causes basilar type migraine?
The exact cause of basilar type migraine is unknown, but it is believed to be triggered by environmental factors and may have a genetic component. Triggers such as strong smells, loud noises, weather changes, excessive sleep, lack of sleep, increased stress, intense physical exertion, oral contraceptives, certain foods, and food preservatives may play a role.
How does basilar migraine differ from other types of migraines?
Basilar migraine was initially believed to be caused by spasms of the basilar artery, but current evidence suggests it is a type of migraine with aura originating from firing of nerves in the brainstem. Symptoms such as vertigo, dysarthria, diplopia, impaired hearing, lack of coordination, confusion, and even loss of consciousness can occur.
How is basilar migraine diagnosed?
To diagnose basilar migraine, certain criteria must be met, including the presence of aura symptoms originating from the brainstem or both occipital hemispheres, lasting at least 5 minutes but not longer than 60 minutes. These symptoms should be followed by a migraine without aura. Imaging tests like MRI or CT scans may be used to rule out other pathologies.
How is basilar migraine treated?
The treatment of basilar migraine aims to alleviate symptoms and manage attacks effectively. For acute attacks, nonsteroidal anti-inflammatory drugs (NSAIDs) and anti-emetics can provide relief. Triptans and ergotamines may also be used. Preventive therapy includes identifying triggers, maintaining a headache diary, and considering medications such as verapamil and topiramate. Non-pharmacological therapies like relaxation techniques, acupuncture, massage, cognitive behavior therapy, and biofeedback techniques can also be helpful.
What conditions can mimic basilar migraine?
Basilar migraine can mimic other conditions such as Meniere's disease, vestibular disease, transient ischemic attack (TIA), stroke, brainstem arteriovenous malformation, tumors, and meningitis. Thorough examination and diagnostic tests may be necessary to exclude these conditions and confirm the diagnosis.
What are the prognosis and complications of basilar migraine?
Basilar migraine can be more severe and disabling compared to other types of migraines due to increased symptom severity and longer duration. While migraines with aura have a slightly higher risk of stroke, the risk of stroke in basilar migraine is not known to be higher than in other types of migraines with aura. However, smoking and the use of estrogen contraceptives can increase the risk of stroke.
What are the common triggers for basilar migraine?
Triggers for basilar migraine episodes can vary but common triggers include stress, alcohol, caffeine, hormonal changes, certain foods, and environmental factors. It is important to identify and avoid these triggers and make lifestyle modifications such as maintaining a balanced diet, regular exercise, stress management techniques, and getting enough sleep.
What are the treatment options for basilar migraine?
The treatment options for basilar migraine focus on relieving pain during acute attacks and preventing future episodes. Over-the-counter pain relievers like NSAIDs can provide symptomatic relief. Antiemetic medications may be prescribed for nausea. Stronger prescription medications may be necessary for more severe cases. Preventive medications such as Botox injections, seizure-reducing medications, calcium channel blockers, and CGRP inhibitors may be recommended for frequent and severe episodes.
How can basilar migraine be managed?
Effective management of basilar migraine involves implementing lifestyle modifications, such as avoiding triggers and adopting stress management techniques. Working closely with healthcare professionals to develop an individualized treatment plan is important for improving symptoms and overall quality of life.
Source Links
- https://www.ncbi.nlm.nih.gov/books/NBK507878/
- https://www.webmd.com/migraines-headaches/basilar-artery-migraines-causes-symptoms-tests-and-treatments
- https://www.medicalnewstoday.com/articles/320013
Types of Brain Tumors: Identify and Understand
A brain tumor is an abnormal mass of tissue in the brain or near it, with over 150 different types documented. Understanding the different types of brain tumors is essential for accurate diagnosis and appropriate treatment options.
Types of brain tumors can be broadly classified into primary and metastatic tumors. Primary brain tumors originate from the brain tissues or its surroundings, while metastatic tumors spread to the brain from other parts of the body.
Primary brain tumors can be further categorized as glial or non-glial, benign or malignant. Glial tumors originate from the glial cells of the brain and are further classified into astrocytomas, oligodendrogliomas, and ependymomas. Non-glial tumors, also known as meningiomas, originate from the membranes covering the brain and spinal cord.
Metastatic brain tumors, on the other hand, are cancers that have spread to the brain from other parts of the body, such as the lungs, breast, or skin. They are considered malignant and can affect nearly one in four cancer patients.
Key Takeaways:
- There are over 150 different types of brain tumors.
- Brain tumors can be classified as primary or metastatic.
- Primary brain tumors can be glial or non-glial, and benign or malignant.
- Metastatic brain tumors spread to the brain from other parts of the body and are considered malignant.
- Accurate diagnosis is crucial for determining appropriate treatment options.
Types of Benign Brain Tumors
Benign brain tumors, also known as non-cancerous brain tumors, are slow-growing tumors that do not spread to other parts of the body. Unlike malignant tumors, benign brain tumors do not invade nearby tissues and are usually less aggressive in nature. These tumors are typically non-cancerous, meaning they do not pose the same risks and complications associated with cancer. Understanding the different types of benign brain tumors can provide valuable insights into their characteristics, prevalence, and prognosis.
There are several types of benign brain tumors that can occur in different areas of the brain. Each type has its own unique characteristics and growth patterns, which can help determine the most suitable treatment approach. Here are some common types of benign brain tumors:
- Chordomas
- Craniopharyngiomas
- Gangliocytomas
- Glomus jugulare tumors
- Meningiomas
- Pineocytomas
- Pituitary adenomas
- Schwannomas
These types of benign brain tumors can vary in location, prevalence, and growth characteristics. For example, meningiomas originate from the meninges, the protective layers surrounding the brain and spinal cord, and are the most common type of benign brain tumor. Pituitary adenomas form in the pituitary gland, a pea-sized gland located at the base of the brain, and can affect hormone production. Schwannomas develop from the Schwann cells, which are responsible for supporting and insulating nerve cells in the peripheral nervous system.
While benign brain tumors are generally less aggressive than malignant brain tumors, they can still cause symptoms and complications depending on their size and location. Treatment options for benign brain tumors may include observation, surgery to remove the tumor, radiation therapy, or a combination of these approaches. The prognosis for benign brain tumors is generally better compared to malignant tumors, with a higher likelihood of complete recovery and long-term survival.

Types of Benign Brain Tumors
| Type of Benign Brain Tumor | Prevalence | Growth Characteristics | |
|---|---|---|---|
| Chordomas | Rare | Slow-growing | |
| Craniopharyngiomas | Common in children, rare in adults | Slow-growing, tend to recur | |
| Gangliocytomas | Rare | Slow-growing | |
| Glomus jugulare tumors | Rare | Slow-growing | |
| Meningiomas | Common | Slow-growing | |
| Pineocytomas | Rare | Slow-growing | |
| Pituitary adenomas | Common | Slow-growing, hormone-producing | |
| Schwannomas | Slow-growing |
Types of Malignant Brain Tumors
Malignant brain tumors are cancerous tumors that pose a serious threat to the surrounding brain tissue. Unlike benign brain tumors, malignant tumors can invade and destroy healthy cells, leading to severe health complications.
The most common type of malignant brain tumor is glioma, accounting for approximately 78% of all malignant brain tumors. Gliomas originate from the supportive tissue of the brain and can rapidly grow and spread to different areas. The most aggressive form of glioma is glioblastoma, which is known for its rapid invasion and resistance to treatment.
Other types of malignant brain tumors include:
- Ependymomas: Originating from the ependymal cells that line the ventricles of the brain, ependymomas are often found in children and adults. They can manifest in different locations within the brain and spinal cord.
- Medulloblastomas: Primarily affecting children, medulloblastomas develop in the cerebellum, the part of the brain responsible for coordination and balance. These tumors are highly malignant and require prompt medical intervention.
- Oligodendrogliomas: Arising from the oligodendrocytes, cells responsible for producing the protective myelin sheath around nerve cells, oligodendrogliomas are typically found in the frontal and temporal lobes of the brain. They tend to grow slowly but can still lead to significant neurological impairments.
To provide a comprehensive understanding of the types of malignant brain tumors, here is a table summarizing the key characteristics:
| Brain Tumor Type | Growth Rate | Prognosis | |
|---|---|---|---|
| Glioma | Rapid | Generally poor | |
| Ependymomas | Varies | Depends on location and stage | |
| Medulloblastomas | Rapid | Generally poor | |
| Oligodendrogliomas | Slow | Varies based on grade |
Understanding the different types of malignant brain tumors is crucial in determining the appropriate treatment plan and prognosis for affected individuals. While advances in medical research and technology continue to improve treatment outcomes, early detection, diagnosis, and timely intervention remain crucial for a better chance at recovery.
Other Types of Brain Tumors
While primary and metastatic brain tumors are the most common types, there are also other rare and unique brain tumors that can occur. These tumors require specific attention and understanding due to their distinct characteristics and treatment approaches.
Rare Brain Tumors
In addition to primary and metastatic tumors, there are several rare brain tumors that have unique features. One such tumor is the hemangioblastoma, which develops in blood vessels and is more commonly found in adults. Hemangioblastomas are typically slow-growing and may not cause noticeable symptoms for a long time.
Another rare and highly aggressive brain tumor is the rhabdoid tumor. These tumors tend to spread quickly throughout the central nervous system, making early detection and treatment vital. Rhabdoid tumors can affect both children and adults.
Pediatric Brain Tumors
Brain tumors in children often differ from those in adults and require specialized care. Several types of pediatric brain tumors can affect children and adolescents:
- Medulloblastomas, which primarily occur in the cerebellum and are the most common malignant brain tumors in children.
- Low-grade astrocytomas, which are slow-growing tumors that develop from brain cells called astrocytes.
- Ependymomas, which primarily affect the lining of the ventricles and spinal cord.
- Craniopharyngiomas, which originate near the pituitary gland and can affect hormone production.
- Brainstem gliomas, which develop in the brainstem and can pose unique challenges due to their location.
Table: Pediatric Brain Tumor Types
| Brain Tumor Type | Characteristics | |
|---|---|---|
| Medulloblastomas | Most common malignant brain tumor in children. | |
| Low-grade astrocytomas | ||
| Ependymomas | ||
| Craniopharyngiomas | Can impact hormone production and growth. | |
| Brainstem gliomas | Challenging due to the location and potential impact on vital functions. |

It is crucial to recognize the unique characteristics of rare and pediatric brain tumors to ensure appropriate diagnosis and treatment. Advances in medical research continue to shed light on these tumor types, leading to improved outcomes and enhanced quality of life for patients facing such challenges.
World Health Organization (WHO) Brain Tumor Grades
When it comes to brain tumors, the World Health Organization (WHO) has developed a grading system that helps determine their malignancy. This grading system plays a crucial role in understanding the aggressiveness of the tumor and predicting its prognosis.
There are four grades in the WHO brain tumor grading system, each indicating different levels of malignancy:
- Grade I: The least malignant tumors fall under this category. They are usually slow-growing and have well-defined borders. Grade I tumors are often considered potentially curable with surgery alone. However, close monitoring is necessary as they can sometimes recur or progress to higher grades.
- Grade II: These tumors are relatively slow-growing like Grade I tumors. However, they infiltrate nearby tissues and have less well-defined borders. Grade II tumors have the potential to recur as higher-grade tumors over time.
- Grade III: Malignant and infiltrative, Grade III tumors are more aggressive than Grade I and Grade II tumors. They tend to have a higher likelihood of recurrence, often progressing to higher grades. Grade III tumors require a comprehensive treatment approach.
- Grade IV: The most malignant and aggressive tumors, Grade IV tumors exhibit rapid growth and invasion into surrounding brain tissue. They are prone to necrosis and often recur quickly. Grade IV tumors necessitate immediate and aggressive treatment.
Understanding the WHO brain tumor grades can help healthcare professionals determine the appropriate treatment plan and provide patients with a more accurate prognosis. The grading system plays a vital role in guiding clinical decision-making and ensuring the best possible outcome for individuals diagnosed with a brain tumor.
Incidence and Causes of Brain Tumors
The incidence of brain tumors is a significant concern, with thousands of adults being diagnosed each year. According to the National Cancer Institute, the brain tumor incidence is estimated to be over 22,000 cases annually. Understanding the causes of brain tumors is crucial in order to develop effective prevention and treatment strategies.
The exact causes of brain tumors are still unknown, but scientific research has provided valuable insights into the underlying factors. Genetic factors play an important role in the development of brain tumors. Certain genes on the chromosomes of brain cells can become damaged or mutated, leading to uncontrolled cell growth and the formation of tumors. Genetic disorders, such as neurofibromatosis type 1, have been associated with an increased risk of developing brain tumors.
In addition to genetic factors, environmental influences can also contribute to the development of brain tumors. Exposure to ionizing radiation, both from medical procedures and environmental sources, has been linked to an increased risk of brain tumors. Other potential environmental factors include exposure to certain chemicals and toxins, as well as lifestyle factors such as smoking and diet.
While the exact mechanisms behind brain tumor development are complex and multifactorial, ongoing research aims to deepen our understanding of the causes and risk factors. By identifying these factors, healthcare professionals can better educate the public and implement strategies to reduce the incidence of brain tumors.

Symptoms of Brain Tumors
The symptoms of a brain tumor can vary depending on its size, location, and rate of growth. It's important to be aware of these symptoms as early detection can lead to prompt diagnosis and treatment.
Common Symptoms
Here are some common signs and symptoms associated with brain tumors:
- Headaches: Headaches are a common symptom of brain tumors, particularly ones that are located near the brain's surface. These headaches are often worse in the morning and can be accompanied by other symptoms such as neck pain or eye pain.
- Nausea: Persistent nausea or vomiting, unrelated to any other known condition, can be an indication of a brain tumor.
- Vision problems: Changes in vision, including blurred or double vision, loss of peripheral vision, or seeing flashing lights or spots, may be a sign of a brain tumor affecting the optic nerves or visual pathways.
- Loss of feeling or movement in limbs: A brain tumor can cause weakness or numbness in certain parts of the body, which may start in one limb and gradually spread to others.
- Balance difficulties: Tumors located in the cerebellum, the region responsible for balance and coordination, can lead to problems with balance and coordination.
- Speech problems: Brain tumors can affect speech and language abilities. You may experience difficulty finding words or speaking clearly.
- Fatigue: Unexplained fatigue or drowsiness, even after getting enough rest, can be a symptom of a brain tumor.
- Memory problems: Memory loss, difficulty concentrating, and changes in cognitive function can be signs of a brain tumor.
- Personality changes: Brain tumors can cause changes in mood, behavior, or personality. You may experience irritability, depression, or sudden emotional swings.
- Seizures: Seizures, which may involve involuntary movements or loss of consciousness, can be a symptom of a brain tumor.
- Hearing problems: Brain tumors near the auditory nerves can lead to hearing loss or ringing in the ears.

It's important to note that the presence of these symptoms does not necessarily mean you have a brain tumor. Many of these symptoms can also be caused by other conditions. However, if you experience any of these symptoms persistently, it's important to consult a healthcare professional for a proper evaluation and diagnosis.
Brain Tumor Treatment Options
The treatment of brain tumors depends on various factors such as the type of tumor, its size, and location within the brain. The primary treatment options for brain tumors include:
- Brain Tumor Surgery: In many cases, surgery is the first line of treatment for brain tumors. The goal of surgery is to remove as much of the tumor as possible, while preserving the surrounding healthy brain tissue. The extent of the surgical resection depends on factors such as the tumor's location and its relationship to vital brain structures. Surgical removal of the tumor can help alleviate symptoms, reduce the tumor size, and improve the overall prognosis.
- Radiation Therapy: Radiation therapy uses high-energy X-rays or other forms of radiation to kill cancer cells and shrink tumors. It is often recommended for brain tumors that cannot be completely removed through surgery or for tumors that are sensitive to radiation. Radiation therapy can be delivered externally using a machine called a linear accelerator, or internally through the placement of radioactive material directly into the tumor (brachytherapy).
- Chemotherapy: Chemotherapy involves the use of drugs to kill cancer cells or inhibit their growth. It can be administered orally or intravenously and is often used in combination with surgery and radiation therapy. Chemotherapy is particularly useful for brain tumors that are difficult to reach surgically or that have spread to other parts of the central nervous system. The specific chemotherapy drugs and treatment regimen are determined based on the tumor type and individual patient factors.
It is important to note that the treatment approach for brain tumors is highly individualized, and a combination of these treatment options may be recommended based on each patient's unique circumstances. The goal of treatment is to effectively manage the tumor, control its growth, alleviate symptoms, and improve the patient's quality of life.

Conclusion
Understanding brain tumors and the various types and treatment options available is crucial in the diagnosis, management, and treatment of these complex diseases. Brain tumors encompass a diverse range of conditions, each requiring individualized care and attention.
Advancements in medical technology and ongoing research efforts are continuously improving the prognosis and quality of life for individuals diagnosed with brain tumors. Timely diagnosis, early detection, and increased awareness can play a significant role in improving outcomes and supporting ongoing research initiatives.
It is essential for individuals and their families to be well-informed about the different types of brain tumors, their characteristics, and the available treatment options. By understanding the nature and complexities of these diseases, individuals can make informed decisions and actively participate in their own healthcare journey.
Brain tumor awareness is of utmost importance to ensure early detection, timely intervention, and comprehensive support for affected individuals and their caregivers. By raising awareness about brain tumors and dispelling misconceptions, we can promote a greater understanding and empathy towards those impacted by these conditions.
FAQ
What are the different types of brain tumors?
There are over 150 different types of brain tumors, including primary and metastatic tumors. Primary tumors originate from the brain tissues or its surroundings, while metastatic tumors spread to the brain from other parts of the body.
What are the types of benign brain tumors?
The types of benign brain tumors include chordomas, craniopharyngiomas, gangliocytomas, glomus jugulare tumors, meningiomas, pineocytomas, pituitary adenomas, and schwannomas. These tumors are generally non-cancerous, slow-growing, and have a better prognosis than malignant brain tumors.
What are the types of malignant brain tumors?
The most prevalent type of malignant brain tumor is glioma, accounting for 78% of all malignant brain tumors. Other types include ependymomas, medulloblastomas, and oligodendrogliomas. Malignant brain tumors are cancerous, invasive, and have a poorer prognosis compared to benign brain tumors.
Are there other types of brain tumors?
Yes, other types of brain tumors include hemangioblastomas, rhabdoid tumors, and pediatric brain tumors. Hemangioblastomas are slow-growing tumors that form in blood vessels, rhabdoid tumors are highly aggressive, and pediatric brain tumors specifically affect children and include medulloblastomas, low-grade astrocytomas, ependymomas, craniopharyngiomas, and brainstem gliomas.
What is the World Health Organization (WHO) grading system for brain tumors?
The WHO has developed a grading system to indicate the malignancy of brain tumors. Grade I tumors are the least malignant, while grade IV tumors are the most malignant and aggressive.
How many adults are diagnosed with brain tumors each year?
The National Cancer Institute estimates that over 22,000 adults are diagnosed with brain tumors in a year.
What causes brain tumors?
The exact causes of brain tumors are still unknown, but scientists believe that certain genes on the chromosomes of brain cells may become damaged and lead to the development of tumors. Environmental factors and genetic disorders can also contribute to the development of brain tumors.
What are the symptoms of brain tumors?
The symptoms of a brain tumor vary depending on the tumor's size, location, and rate of growth. Common symptoms include headaches, nausea, vision problems, loss of feeling or movement in limbs, balance difficulties, speech problems, fatigue, memory problems, personality changes, seizures, and hearing problems.
What are the treatment options for brain tumors?
The treatment options for brain tumors depend on the type, size, and location of the tumor. Common treatment options include surgery to remove the tumor, radiation therapy to target and kill cancer cells, and chemotherapy to destroy cancer cells using drugs.
Source Links
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Brain-Tumors
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/brain-tumor/brain-tumor-types
- https://www.mayoclinic.org/diseases-conditions/brain-tumor/symptoms-causes/syc-20350084
Also Read
Understanding Different Types of Brain Tumors: A Comprehensive Guide
5 Effective Methods for Brain Tumor Treatment without Surgery
Can Stress Cause Brain Tumors? Unpacking the Myth
Understanding Basilar Artery Migraine Symptoms
Basilar artery migraine, also known as basilar migraines or migraines with brainstem aura, is a unique type of migraine that originates in the brainstem. It is characterized by aura symptoms originating from the brainstem, such as vertigo, double vision, difficulty speaking, and lack of coordination. These symptoms can occur 10 minutes to 45 minutes before the onset of a headache. It is important to be able to recognize these specific symptoms in order to properly identify and manage basilar artery migraines.
Key Takeaways:
- Basilar artery migraines are a subtype of migraines with aura.
- Symptoms originate from the brainstem and include vertigo, difficulty speaking, double vision, and coordination problems.
- Recognition of these symptoms is crucial for accurate diagnosis and effective management.
- A proper understanding of basilar artery migraine symptoms aids in identifying triggers and implementing preventive measures.
- Consultation with a healthcare professional is recommended for diagnosis and treatment.
What is Basilar Migraine?
Basilar migraine, also known as basilar artery migraine, brainstem migraine, or vertebrobasilar migraine, is a subtype of migraine with aura. It was originally believed to be caused by spasms of the basilar artery, but it is now understood to be due to the firing of nerves in the brainstem. Basilar migraines are characterized by aura symptoms originating from the brainstem or both cerebral hemispheres, along with typical symptoms of a migraine, such as headache pain and sensitivity to light and sound.
During a basilar migraine episode, individuals may experience a range of symptoms that can be debilitating. These symptoms can include vertigo, difficulty speaking, double vision, impaired coordination, and other sensory disturbances. The aura symptoms are usually followed by the onset of a throbbing headache, often accompanied by sensitivity to light and sound.
Basilar migraines are often mistaken for other types of migraines or neurological conditions due to the similarity of symptoms. However, the distinctive feature of basilar migraines is the involvement of the brainstem, which sets it apart from other types of migraines.
Etiology of Basilar Migraine
The etiology of basilar migraines is still not fully understood. However, researchers believe that a combination of environmental factors and genetic predisposition contribute to the development of this condition. Understanding the causes and triggers of basilar migraines is important for managing and preventing future episodes.
Common triggers for basilar migraines include:
- Strong smells
- Loud noises
- Weather changes
- Sleep disturbances
- Stress
- Physical exertion
- Certain foods
- Hormonal changes in females
These triggers can vary from person to person, and identifying individual triggers can help manage and reduce the frequency of basilar migraines.
While the genetic basis of basilar migraines is not yet well understood, some studies suggest a potential genetic involvement, particularly in genes associated with migraine with typical aura. Further research is needed to fully elucidate the genetic factors contributing to basilar migraines.
Risk Factors for Basilar Migraine
Though the exact cause of basilar migraines remains uncertain, certain risk factors have been identified. These include:
| Risk Factors | Description |
|---|---|
| Gender | Basilar migraines are more common in females than males. |
| Age | Basilar migraines typically manifest in adolescence and young adulthood, with an age of onset between 7 and 20 years old. |
| Family history | A family history of migraines, particularly migraines with aura, may increase the risk of developing basilar migraines. |
| Hormonal changes | Fluctuations in hormone levels, such as those that occur during menstruation, pregnancy, or menopause, may trigger or worsen basilar migraines. |
While these risk factors may increase the likelihood of developing basilar migraines, it's important to note that not everyone with these risk factors will develop the condition. Basilar migraines can also occur in individuals without any known risk factors.
Epidemiology of Basilar Migraine
Understanding the epidemiology of basilar migraine can provide valuable insights into the prevalence and age of onset for this unique type of migraine. While the exact numbers are unknown, basilar migraine is believed to be more commonly seen in females than males. It can occur at any age, but it is most frequently observed in adolescence and young adults, with the age of onset typically ranging from 7 to 20 years old.
Prevalence of Basilar Migraine
The exact prevalence and incidence rates of basilar migraine are yet to be determined. However, studies suggest that it accounts for only a small portion of all migraines, estimated to be around 4% to 12%. Because basilar migraines are relatively rare, they require a unique set of diagnostic criteria to differentiate them from other types of migraines.
Age of Onset for Basilar Migraine
Basilar migraines can manifest at any age, but they are more commonly observed in younger individuals. The adolescent and young adult age groups are particularly susceptible to experiencing basilar migraines. The fact that basilar migraines tend to occur during these developmental stages highlights the importance of early recognition and effective management for improved quality of life.
| Characteristics | Females | Males |
|---|---|---|
| Prevalence | Higher | Lower |
| Age of Onset | Adolescence and Young Adults | Varied |
Note: The data in the table above is for illustrative purposes and may not reflect precise statistics.
Understanding the epidemiology of basilar migraine, including its prevalence and age of onset, is crucial for healthcare professionals and individuals affected by this condition. By recognizing the demographic characteristics associated with basilar migraines, appropriate diagnosis, management, and support can be provided, leading to improved outcomes and a better quality of life.
Pathophysiology of Basilar Migraine
Basilar migraine, previously believed to be caused by vascular pathology involving spasms of the basilar artery, is now understood differently. Research has found no evidence to support this theory, leading to a new understanding of the pathophysiology. It is now known that basilar migraines are related to the firing of nerves in the brainstem, specifically the brainstem aura symptoms seen in basilar migraines are believed to be a result of cortical spreading depression.
Cortical spreading depression refers to a wave of depolarization that spreads across the cerebral cortex, affecting both neurons and glia. This depolarization leads to the development of aura symptoms commonly seen in basilar migraines.
Understanding the pathophysiology of basilar migraines can help in the development of targeted therapeutic approaches and enhance our knowledge of this complex neurological disorder.
Basilar Artery Migraine Symptoms
Basilar migraines are characterized by a range of symptoms that can vary from person to person. These symptoms, also known as aura symptoms, are generally reversible and may occur before the onset of a headache. It is important to recognize and understand these symptoms in order to properly identify and manage basilar migraines.
The most common symptom of basilar migraines is vertigo, a sensation of spinning or dizziness. Other aura symptoms that may occur include:
- Dysarthria (difficulty speaking)
- Diplopia (double vision)
- Tinnitus (ringing in the ears)
- Impaired hearing
- Lack of coordination
- Confusion
- Loss of consciousness (in some cases)
These aura symptoms are usually followed by an occipital headache, which is characterized by pain at the back of the head. The headache can last for hours to days and can be accompanied by sensitivity to light and sound.
If you experience any weakness or visual loss along with these symptoms, it is important to seek medical evaluation to rule out other potential causes.

Diagnosis of Basilar Migraine
The diagnosis of basilar migraine involves the assessment of specific criteria outlined by the International Classification of Headache Disorders. These criteria help healthcare professionals identify and confirm the presence of basilar migraine based on distinctive characteristics. To make a diagnosis of basilar migraine, the following criteria should be met:
- Aura symptoms originating from the brainstem:
- Dysarthria (difficulty speaking)
- Vertigo (spinning sensation)
- Tinnitus (ringing in the ears)
- Hearing impairment
- Diplopia (double vision)
- Ataxia (impaired coordination)
- Decreased level of consciousness
- Bilateral paresthesia (abnormal skin sensations)
- Aura symptoms lasting for more than 5 minutes
- Aura symptoms followed by a headache that begins either during the aura or within 1 hour
In addition to these criteria, healthcare providers may perform diagnostic tests to rule out other potential causes of the symptoms and further support the diagnosis of basilar migraine. These diagnostic tests can include:
- Brain imaging (MRI or CT scans): These tests can help identify any abnormalities, such as tumors or vascular malformations, which may be causing the symptoms.
- EEG (Electroencephalogram): This test measures the electrical activity of the brain and can help rule out seizures or other brain abnormalities.
| Diagnostic Criteria | Presence |
|---|---|
| Aura symptoms originating from the brainstem | Present |
| Aura symptoms lasting for more than 5 minutes | Present |
| Aura symptoms followed by a headache within 1 hour | Present |
| Brain imaging (MRI or CT scans) | Performed |
| EEG (Electroencephalogram) | Performed |
The diagnostic criteria and tests help healthcare professionals accurately diagnose basilar migraine and differentiate it from other conditions with similar symptoms. Through proper diagnosis, individuals with basilar migraine can receive appropriate treatment and management strategies to effectively alleviate their symptoms and improve their quality of life.
Evaluation of Basilar Migraine
When diagnosing and evaluating basilar type migraine, several tests and procedures can provide valuable insights. Brain imaging, such as MRI or CT scans, are commonly employed to rule out other potential causes of the symptoms. These imaging techniques help identify conditions such as stroke, arteriovenous malformations, or brain tumors that may mimic basilar migraines.
In addition to brain imaging, an electroencephalogram (EEG) may be performed to evaluate brain activity and detect any abnormalities. This test is particularly useful in cases where there is confusion or a decreased level of consciousness, as it helps rule out seizures as a cause of the symptoms.
In some instances, 24-hour Holter monitoring may be recommended to assess the heart's electrical activity and evaluate for arrhythmias. This monitoring device records the heart's rhythm continuously for 24 hours, providing valuable information on any irregularities that may contribute to the occurrence of basilar migraines.
These evaluation procedures help healthcare professionals establish an accurate diagnosis and better understand the underlying mechanisms of basilar migraines, enabling them to develop a targeted treatment plan specific to each individual.
Treatment and Management of Basilar Migraine
When it comes to the basilar artery migraine treatment and management, the focus is on providing symptomatic relief and implementing preventive measures to reduce the frequency and severity of episodes. By effectively addressing both acute symptoms and long-term prevention, individuals can better navigate the challenges associated with basilar migraines.
For immediate relief from headache pain and associated symptoms, several medication options can be considered:
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen sodium, can help alleviate mild to moderate headache pain and reduce inflammation.
- Anti-emetics: Anti-emetic medications like metoclopramide or prochlorperazine can offer relief from nausea and vomiting, which are common symptoms during a basilar migraine attack.
- Pain relievers: Over-the-counter pain relievers like acetaminophen or aspirin may be effective in reducing headache pain.
However, it's important to note that triptans and ergotamines, which are commonly used to treat other types of migraines, are generally avoided in basilar migraines due to the potential risk of increasing cerebral ischemia.
Preventive therapy plays a crucial role in managing basilar migraines and reducing their frequency. This involves identifying and modifying triggers that may precipitate an attack. By keeping a headache diary and tracking factors like stress, sleep patterns, diet, and hormonal changes, individuals can gain insights into their unique triggers and make lifestyle adjustments accordingly.
Medications can also be prescribed for preventive therapy:
- Verapamil: This medication, typically used for heart conditions, is often effective in preventing basilar migraines by regulating blood pressure and blood flow in the brain.
- Topiramate: An anticonvulsant drug, topiramate has shown efficacy in reducing the frequency and severity of migraine attacks, including basilar migraines.
Non-pharmacological therapies can complement medication-based treatments or be used as standalone options for prevention:
- Relaxation techniques: Practices like deep breathing, progressive muscle relaxation, and guided imagery can help manage stress and promote overall well-being.
- Acupuncture and massage: These alternative therapies have been used to alleviate migraine symptoms and promote relaxation. Acupuncture involves the insertion of thin needles at specific points on the body, while massage focuses on relieving muscle tension and improving blood flow.
- Cognitive behavior therapy: This form of therapy can help individuals recognize and modify negative thought patterns, leading to improved coping strategies and better migraine management.
- Biofeedback: This technique utilizes instruments that measure physiological responses, such as muscle tension or skin temperature, to provide real-time feedback. By learning to control these responses, individuals may experience a reduction in migraine symptoms.
By combining medication, preventive measures, and non-pharmacological therapies, individuals with basilar migraines can take charge of their condition and adopt a comprehensive approach to treatment and management.
Differential Diagnosis of Basilar Migraine
When diagnosing basilar migraines, it is essential to consider other conditions that may present with similar symptoms. Some of these conditions include:
- Hemiplegic migraines: These migraines are characterized by temporary paralysis or weakness on one side of the body, which can be mistaken for the impaired coordination seen in basilar migraines.
- Meniere's disease: Meniere's disease is a disorder of the inner ear that can cause dizziness, hearing loss, and ringing in the ears, symptoms that can overlap with those of basilar migraines.
- Vestibular disease: Vestibular disorders affect the inner ear and can cause vertigo, a common symptom of basilar migraines.
- Transient ischemic attacks (TIAs) and strokes: Both TIAs and strokes can produce neurological symptoms similar to those seen in basilar migraines, including double vision, difficulty speaking, and lack of coordination.
- Brainstem arteriovenous (AV) malformations: These abnormalities in blood vessels in the brainstem can lead to symptoms similar to basilar migraines, such as vertigo, impaired hearing, and diplopia.
- Tumors: Tumors in the brainstem can cause a variety of symptoms, including vertigo, vision changes, and impaired coordination, which can be mistaken for basilar migraines.
- Meningitis: Meningitis is an infection that causes inflammation of the membranes surrounding the brain and spinal cord. Some of its symptoms, such as headache, confusion, and coordination difficulties, can mimic those of basilar migraines.
It is crucial to rule out these conditions before making a definitive diagnosis of basilar migraines. This typically requires a thorough examination, review of medical history, and diagnostic tests such as brain imaging (MRI or CT scans) and nerve tests. These evaluations can help differentiate basilar migraines from other conditions and ensure appropriate management and treatment.
| Condition | Key Symptoms | Diagnostic Tests |
|---|---|---|
| Hemiplegic migraines | Temporary paralysis or weakness on one side of the body | No specific diagnostic tests Diagnosis based on symptoms and exclusion of other causes |
| Meniere's disease | Dizziness, hearing loss, ringing in the ears | Audiometry (hearing test) Electronystagmography (ENG) Magnetic resonance imaging (MRI) of the inner ear |
| Vestibular disease | Vertigo, balance problems | Electronystagmography (ENG) Vestibular evoked myogenic potentials (VEMP) |
| Transient ischemic attacks (TIAs) and strokes | Temporary neurological deficits such as double vision, difficulty speaking, lack of coordination | Computed tomography (CT) scan of the head Magnetic resonance imaging (MRI) of the brain Cerebral angiography |
| Brainstem arteriovenous (AV) malformations | Vertigo, impaired hearing, diplopia | Magnetic resonance imaging (MRI) or computed tomography (CT) angiography Digital subtraction angiography (DSA) |
| Tumors | Vertigo, vision changes, impaired coordination | Magnetic resonance imaging (MRI) of the brain |
| Meningitis | Headache, confusion, coordination difficulties | Lumbar puncture (CSF analysis) Blood cultures Computed tomography (CT) scan or magnetic resonance imaging (MRI) of the brain |
Prognosis and Complications of Basilar Migraine
Basilar migraines can have a significant impact on your daily life, as they tend to be more disabling than other types of migraines. These migraines are characterized by increased severity, longer duration of symptoms, and a range of aura symptoms originating from the brainstem. However, there is some good news. The frequency of basilar migraine episodes tends to decrease with age, and they often evolve into more typical patterns of migraines.
While it is known that migraines with aura, including basilar migraines, have a slightly higher risk of stroke compared to migraines without aura, it's important to note that the overall risk of stroke in basilar migraines is not significantly higher than in migraines with typical aura. However, it is crucial to address modifiable risk factors that can further increase the risk of stroke.
Some common complications associated with basilar migraine include:
- Disruption of daily activities and reduced quality of life
- Impaired cognitive function during and after migraine attacks
- Mental health challenges, such as anxiety and depression
- Increased risk of stroke, especially in individuals who smoke or use estrogen contraceptives
Managing and minimizing the risk of complications involves:
- Working closely with your healthcare provider to develop an individualized treatment plan
- Identifying and avoiding triggers that may precipitate basilar migraines
- Implementing lifestyle modifications, such as maintaining a regular sleep schedule, managing stress, and staying hydrated
- Using preventive medications, as prescribed by your healthcare provider, to reduce the frequency and severity of the migraines
- Monitoring and addressing modifiable risk factors for stroke, such as smoking and the use of estrogen contraceptives
Comparison of Basilar Migraine with Typical Migraine and Risk of Stroke
| Factor | Basilar Migraine | Typical Migraine |
|---|---|---|
| Risk of Stroke | Slightly higher compared to migraines without aura | Slightly higher compared to migraines without aura |
| Risk Factors for Stroke | Can be further increased by modifiable risk factors such as smoking and estrogen contraceptive use | Can be further increased by modifiable risk factors such as smoking and estrogen contraceptive use |
Conclusion
Basilar artery migraines, also known as basilar migraines or migraines with brainstem aura, are a unique subtype of migraines that originate from the brainstem. They are characterized by a range of symptoms such as vertigo, difficulty speaking, double vision, and impaired coordination. These symptoms can occur prior to the onset of a headache.
While the exact cause of basilar migraines is unknown, environmental triggers and genetic factors may contribute to their development. Diagnosis is based on specific criteria, and it is crucial to rule out other potential causes of similar symptoms. Treatment and management strategies primarily focus on providing symptom relief and implementing preventive measures, which may include lifestyle modifications and the use of medications.
Basilar migraines generally have a favorable prognosis. However, it is important to note that they carry a slightly increased risk of stroke compared to migraines without aura. Addressing modifiable risk factors and seeking timely medical attention are essential in the proper diagnosis and management of this condition.
FAQ
What are the basilar artery migraine symptoms?
The symptoms of basilar artery migraine include vertigo, difficulty speaking, double vision, impaired coordination, and headache pain.
What is basilar migraine?
Basilar migraine, also known as basilar artery migraine, brainstem migraine, or vertebrobasilar migraine, is a subtype of migraine with aura that originates from the brainstem.
What are the triggers for basilar migraine?
Common triggers for basilar migraine include strong smells, loud noises, weather changes, sleep disturbances, stress, physical exertion, certain foods, and hormonal changes in females.
What is the age of onset for basilar migraine?
Basilar migraine can occur at any age, but it is more commonly seen in adolescence and young adults, typically between 7 and 20 years old.
What is the pathophysiology of basilar migraine?
Basilar migraine is believed to be related to the firing of nerves in the brainstem and the development of aura symptoms due to cortical spreading depression, a wave of depolarization across the cerebral cortex.
What are the symptoms of basilar migraine?
The symptoms of basilar migraine include vertigo, dysarthria (difficulty speaking), diplopia (double vision), tinnitus (ringing in the ears), impaired hearing, lack of coordination, confusion, and sometimes loss of consciousness.
How is basilar migraine diagnosed?
Basilar migraine is diagnosed based on specific criteria outlined by the International Classification of Headache Disorders, which include the presence of aura symptoms originating from the brainstem, lasting for more than 5 minutes, followed by a headache within 1 hour.
What tests are performed to evaluate basilar migraine?
Diagnostic tests, such as brain imaging (MRI or CT scans) and EEG, may be performed to rule out other potential causes of the symptoms and assess brain activity.
How is basilar migraine treated and managed?
Treatment focuses on symptomatic relief and may involve the use of NSAIDs, anti-emetics, and pain relievers. Preventive therapy includes identifying and modifying triggers, lifestyle changes, and the use of medications such as verapamil and topiramate.
What conditions should be considered in the differential diagnosis of basilar migraine?
Conditions with symptoms similar to basilar migraine include hemiplegic migraines, Meniere's disease, vestibular disease, transient ischemic attacks (TIAs), strokes, brainstem AV malformations, tumors, and meningitis.
What is the prognosis and risk of complications in basilar migraine?
Basilar migraines can be more disabling, but the frequency of episodes tends to decrease with age. While there is a slightly increased risk of stroke compared to migraines without aura, the risk of stroke in basilar migraines is not significantly higher than in migraines with typical aura.
Source Links
- https://www.ncbi.nlm.nih.gov/books/NBK507878/
- https://www.webmd.com/migraines-headaches/basilar-artery-migraines-causes-symptoms-tests-and-treatments
- https://www.medicalnewstoday.com/articles/320013
Exploring The Causes Of Benign Essential Blepharospasm
Benign essential blepharospasm (BEB) is a facial dystonia characterized by involuntary contractions of the orbicularis oculi muscle, resulting in involuntary eyelid closure. It is the most common type of blepharospasm and primarily affects the eyelid closure muscles, including the orbicularis oculi, procerus, and corrugator muscles. BEB is not associated with any other neurological or ocular diseases. However, there are other variants of blepharospasm, such as Meige syndrome, where blepharospasm and oromandibular dystonia occur together. In some cases, blepharospasm can also be associated with systemic disorders like Parkinson's disease or other common ocular conditions like blepharitis or dry eye.
Key Takeaways:
- Benign essential blepharospasm is a facial dystonia characterized by involuntary contractions of the orbicularis oculi muscle.
- BEB primarily affects the eyelid closure muscles and is not associated with other neurological or ocular diseases.
- Meige syndrome is a variant of blepharospasm where blepharospasm and oromandibular dystonia occur together.
- Blepharospasm can also be associated with systemic disorders like Parkinson's disease or common ocular conditions like blepharitis or dry eye.
Please continue writing the text for sections 2 to 9 with the same formatting style.
Epidemiology and Demographics of Benign Essential Blepharospasm
Benign essential blepharospasm (BEB) affects a considerable portion of the population, with a prevalence of approximately 4.2 cases per 100,000 people.
BEB primarily manifests in individuals between the fifth and seventh decades of life, which is commonly known as middle adulthood. The condition displays a higher incidence among women, with an estimated female-to-male ratio varying between 2:1 to 4:1.
Menopause, the natural process marking the end of a woman's reproductive years, is believed to be a predisposing factor for the development of BEB. Hormonal fluctuations during menopause may play a role in triggering or exacerbating the condition. However, further research is needed to fully understand the relationship between menopause and BEB.
Interestingly, coffee consumption has been found to have a protective effect against BEB. Regular coffee drinkers may experience a reduced risk of developing the condition. The exact mechanism behind this association is not yet fully understood, but it offers a fascinating avenue for future exploration.
To summarize, BEB is relatively prevalent, particularly among middle-aged women. Menopause may increase susceptibility to developing the condition, while coffee consumption appears to have a beneficial impact. Understanding these epidemiological and demographic aspects of BEB is crucial for enhancing both diagnosis and management strategies.
Note: The image above displays a representation of benign essential blepharospasm and is used for illustrative purposes only.
Pathophysiology of Benign Essential Blepharospasm
Benign essential blepharospasm (BEB) is a neurologic disorder characterized by involuntary contractions of the orbicularis oculi muscle, resulting in repetitive and forceful spasms of the eyelids. The exact pathophysiology of BEB is not fully understood, but it is believed to involve an imbalance in neurotransmitters and dysfunction in the basal ganglia.
Studies have identified lesions in the basal ganglia, thalamus, midbrain, and cortex in some patients with BEB, suggesting abnormalities in these regions may contribute to the development of the condition (Schicatano et al., 1991).
The basal ganglia, a group of neural structures deep within the brain, are known to play a crucial role in the coordination of voluntary and involuntary movements. Disruption in the function of the basal ganglia can lead to abnormal muscle activity, such as the involuntary contractions seen in BEB.
One proposed mechanism of pathophysiology is a neurotransmitter imbalance, specifically involving dopaminergic inhibition, decreased function of gamma-aminobutyric acid (GABA), and cholinergic hyperactivity (Hallett, 2011).
- Dopaminergic inhibition: Dopamine is an important neurotransmitter involved in regulating movement. In BEB, there may be a disruption in the balance of dopamine, leading to excessive activity in the basal ganglia and abnormal muscle contractions.
- Decreased GABA function: GABA is an inhibitory neurotransmitter that helps regulate neural activity. Reduced GABA function may contribute to the hyperexcitability of the basal ganglia in BEB, leading to muscle spasms.
- Cholinergic hyperactivity: Acetylcholine is another neurotransmitter that plays a role in muscle control. Increased cholinergic activity in the basal ganglia may contribute to the abnormal muscle contractions seen in BEB.
The neurotransmitter imbalances seen in BEB may also have implications beyond muscle hyperactivity. Some patients with BEB experience anxiety and depression, suggesting that the pathophysiology may influence mood regulation as well (Zuk et al., 1997).
Further research is needed to fully understand the complex pathophysiology of BEB and develop more targeted therapeutic strategies.

Clinical Presentation of Benign Essential Blepharospasm
When it comes to the clinical presentation of benign essential blepharospasm (BEB), there are several key features to be aware of. The most common initial symptom is bilateral eyelid twitching, which can gradually progress to forceful and frequent spasms of the eyelid closure muscles. These spasms are characterized by synchronous and stereotyped contractions of the eyelids, often accompanied by twitching of other facial muscles.
Patients with BEB may also experience episodes of eyelid apraxia, a temporary inability to voluntarily open the eyes. This condition further exacerbates the functional difficulties associated with the forceful contractions of the eyelids. It is essential to note that these symptoms tend to subside during sleep, offering patients temporary relief.
There are several triggering factors that can worsen the symptoms of BEB. Bright lights, such as the headlights of oncoming traffic, can intensify the spasms and involuntary contractions of the eyelids. Photosensitivity is also commonly reported in patients with BEB, with up to 79% of individuals experiencing sensitivity to light. This heightened sensitivity adds to the discomfort and challenges faced by those with the condition.
Sensory stimulation, however, can have a temporary alleviating effect on the contractions. Activities like touching the eyelids or even singing can provide momentary relief from the forceful spasms and contractions.
Understanding the clinical presentation of benign essential blepharospasm is essential for accurate diagnosis and effective management of the condition. By recognizing the characteristic symptoms and triggering factors, healthcare professionals can provide targeted interventions and support to improve the quality of life for individuals with BEB.
Diagnosis of Benign Essential Blepharospasm
The diagnosis of benign essential blepharospasm is primarily based on clinical assessment, as there are no specific imaging or laboratory tests to confirm the condition. A thorough evaluation of the patient's medical history, symptoms, and physical examination is key to reaching a diagnosis. The characteristic presentation of bilateral eyelid twitching and forceful, frequent eyelid spasms helps distinguish benign essential blepharospasm from other similar conditions.
Electromyography (EMG) can be used as an adjunctive test to objectively assess the muscle involvement and confirm the diagnosis. EMG involves the placement of small electrodes on the eyelid muscles to measure their electrical activity. However, it is important to note that EMG is rarely performed in clinical practice and is not essential for the diagnosis of benign essential blepharospasm.
The differential diagnosis for blepharospasm includes other movement disorders and conditions that can cause eyelid contractions. These may include:
- Meige syndrome - characterized by blepharospasm and oromandibular dystonia.
- Myokymia - a benign condition characterized by spontaneous eyelid twitches.
- Apraxia of eyelid opening - difficulty in voluntarily opening the eyes.
- Hemifacial spasm - repetitive, involuntary contractions of the muscles on one side of the face.
- Tardive dyskinesia - a side effect of certain medications characterized by repetitive, involuntary movements.
- Tic disorders - involuntary, repetitive movements or sounds.
Other conditions like anterior uveitis or ocular surface disease that cause photophobia can also lead to regular eyelid contractions and should be considered in the differential diagnosis. Additionally, meningeal irritation or infection and psychogenic facial spasms should be considered in certain cases.

Clinical Assessment for Benign Essential Blepharospasm
To diagnose benign essential blepharospasm, the healthcare provider will typically conduct a comprehensive clinical assessment that may include:
- Reviewing the patient's medical history and symptoms.
- Performing a thorough physical examination, including an evaluation of the eyelids, facial muscles, and neurological functions.
- Assessing the patient's response to sensory stimuli, such as bright lights or touching the eyelids.
- Screening for other ocular or systemic conditions that may contribute to the symptoms.
During the assessment, the healthcare provider may also ask detailed questions about the onset, duration, and progression of symptoms, as well as any factors that may trigger or worsen the eyelid spasms. This comprehensive clinical evaluation helps differentiate benign essential blepharospasm from other similar conditions and guides appropriate treatment planning.
Management of Benign Essential Blepharospasm
The management of benign essential blepharospasm involves various treatment approaches depending on the severity of the condition. The primary treatment modality is botulinum toxin injections, specifically types A and B. These injections are administered to the affected periocular muscles every three to four months to temporarily weaken or paralyze the muscles, reducing the involuntary spasms and contractions.
Another treatment option for managing benign essential blepharospasm is photochromatic modulation. This involves the use of spectacle lenses with an FL-41 tint, which has been shown to reduce photosensitivity and relieve symptoms related to light sensitivity.
In some cases, medication options may be considered as part of the treatment plan. These medications include anticholinergic drugs, benzodiazepines, levodopa, baclofen, and vesicular monoamine transporter 2 (VMAT2) inhibitors. However, it is important to note that medication options are typically not the primary treatment for benign essential blepharospasm due to their limited efficacy and potential side effects.
Repetitive transcranial magnetic stimulation (rTMS) is another therapeutic approach that has been explored as an adjunctive therapy in conjunction with botulinum toxin injections. rTMS involves the use of electromagnetic currents to stimulate specific areas of the brain, potentially modulating the neural circuits involved in blepharospasm and providing additional relief for patients.
In severe cases of benign essential blepharospasm that are resistant to other treatment modalities, surgical options may be considered. These include myectomy, which involves the removal of a portion of the eyelid muscles, and facial nerve ablation, which disrupts the nerve signals responsible for the spasms. However, surgical interventions are generally reserved for a select group of patients who have not experienced significant improvement with other treatment options.

Treatment Options for Benign Essential Blepharospasm:
| Treatment | Description |
|---|---|
| Botulinum toxin injections | Injected into affected periocular muscles to reduce muscle contractions |
| Photochromatic modulation | Use of FL-41 tinted spectacle lenses to reduce photosensitivity |
| Medication options | Anticholinergic drugs, benzodiazepines, levodopa, baclofen, VMAT2 inhibitors |
| Repetitive transcranial magnetic stimulation (rTMS) | Electromagnetic stimulation to modulate neural circuits involved in blepharospasm |
| Surgical treatment | Myectomy or facial nerve ablation for severe, medically resistant cases |
It is important for individuals with benign essential blepharospasm to work closely with their healthcare providers to determine the most appropriate treatment plan based on their specific symptoms and needs.
Prognosis and Impact on Quality of Life
Benign essential blepharospasm is a chronic neurologic disorder with no known cure. Spontaneous remission is rare, but it is more likely to occur in younger patients and those with a shorter duration of symptoms. However, the progression of symptoms and spread of muscle involvement can happen relatively early in the course of blepharospasm.
While there is no cure for benign essential blepharospasm, treatment options are available to manage the condition and improve the quality of life for patients. However, it is important to note that treatment does not alter the natural course of the disease.
Functional disability can significantly impact the daily lives of individuals with benign essential blepharospasm. The inability to open their eyes voluntarily can affect activities such as driving, reading, and social interactions.
To get a better understanding of the prognosis and impact on the quality of life, let's take a look at some key points:
- Prognosis: Spontaneous remission is rare, but more likely in younger patients and those with a shorter duration of symptoms.
- Quality of Life: Treatment can significantly improve the quality of life for patients with benign essential blepharospasm, but it does not cure the condition.
- Impact on Daily Activities: Functional disability resulting from the inability to open the eyes voluntarily can affect daily activities such as driving, reading, and social interactions.
Treatment Options:
There are various treatment options available to manage benign essential blepharospasm. Some of the common treatment modalities include:
- Botulinum toxin injections: These injections, administered every three to four months, are the mainstay treatment for reducing muscle hyperactivity and spasms.
- Photochromatic modulation: The use of spectacle lenses with an FL-41 tint can help reduce photosensitivity and ease symptoms.
- Medication options: Anticholinergic drugs, benzodiazepines, levodopa, baclofen, and vesicular monoamine transporter 2 (VMAT2) inhibitors may be used, but they are usually not the primary treatment due to side effects and low efficacy.
- Transcranial magnetic stimulation (rTMS): This therapy is explored as an adjunctive treatment along with botulinum toxin injections.
In severe, medically resistant cases, surgical options such as myectomy or facial nerve ablation may be considered, but these procedures are generally reserved for a select group of patients.
It is important for individuals with benign essential blepharospasm to work closely with their healthcare team to determine the most appropriate treatment plan tailored to their unique needs and circumstances.

The prognosis for benign essential blepharospasm varies from one patient to another, and understanding the impact on quality of life can help individuals better cope with the challenges posed by this condition.
Research and Advances in Benign Essential Blepharospasm
Research in benign essential blepharospasm is continuously advancing to enhance our understanding of the condition. Scientists are particularly focused on genetic studies, aiming to identify the genetic basis of the disorder and shed light on its pathophysiology. The exploration of treatment options and the utilization of neuroimaging techniques have also contributed significantly to the progress in managing this condition.
Genetic studies have revealed potential risk factors and susceptibility genes associated with benign essential blepharospasm. These findings offer valuable insights into the underlying mechanisms of the disorder and open up new avenues for further investigation.
Advancements in treatment options have revolutionized the management of benign essential blepharospasm. One notable development is the use of new botulinum toxin formulations, which have been highly effective in reducing muscle spasms and improving symptoms. Additionally, transcranial magnetic stimulation is being explored as an adjunctive therapy in conjunction with botulinum toxin injections, with promising results.
Neuroimaging studies involving functional MRI and PET scans have provided essential information about the neural circuits involved in blepharospasm. These imaging techniques have offered valuable insights into the pathophysiological mechanisms of the disorder, although some inconsistencies in the results still need to be addressed.
The ongoing research and advances in benign essential blepharospasm hold great promise for the future. Continued genetic studies, the exploration of new treatment options, and further advancements in neuroimaging techniques will contribute to improved understanding, management, and ultimately, the quality of life for individuals affected by this condition.
Advancements in the Management of Benign Essential Blepharospasm
| Treatment Options | Advancements |
|---|---|
| Botulinum toxin injections | New formulations with improved efficacy |
| Transcranial magnetic stimulation | Exploration as an adjunctive therapy |
| Neuroimaging techniques | Insights into the neural circuits involved |

The above table highlights the recent advancements in the management of benign essential blepharospasm. These advancements offer hope for improved treatment outcomes and a better quality of life for individuals living with this condition.
Conclusion
Benign essential blepharospasm, a focal dystonia affecting the orbicularis oculi muscle, can have a significant impact on the visual function and quality of life of those affected. Diagnosis of this condition relies on clinical assessment, considering the presenting symptoms and ruling out other potential causes. There is no known cure for benign essential blepharospasm, but various treatment options are available to manage the symptoms and improve overall well-being.
The management of benign essential blepharospasm includes the use of botulinum toxin injections, which effectively reduce muscle contractions and spasms. Additionally, photochromatic modulation, medication options, transcranial magnetic stimulation, and surgical interventions may be considered depending on the severity and individual response. It is important to note that while these treatments can provide significant relief, they do not alter the natural course of the disease.
Prognosis for individuals with benign essential blepharospasm varies, and spontaneous remission is rare. However, treatment can greatly improve the symptoms and quality of life for those affected. Ongoing research is focused on understanding the underlying pathophysiology of the condition and developing more targeted and effective therapeutic strategies.
In conclusion, a timely diagnosis and comprehensive management approach are crucial for individuals living with benign essential blepharospasm. While the road to managing the symptoms may be challenging, advancements in treatment options and ongoing research provide hope for an improved prognosis and enhanced quality of life for affected individuals.
FAQ
What is benign essential blepharospasm?
Benign essential blepharospasm is a facial dystonia characterized by involuntary contractions of the orbicularis oculi muscle, resulting in involuntary eyelid closure.
What is the primary clinical presentation of benign essential blepharospasm?
The primary clinical presentation of benign essential blepharospasm is bilateral eyelid twitching, which may progress over time to forceful and frequent spasms of the eyelid closure muscles.
How is benign essential blepharospasm diagnosed?
The diagnosis of benign essential blepharospasm is primarily based on clinical assessment, as there are no specific imaging or laboratory tests to confirm the condition.
What are the treatment options for benign essential blepharospasm?
The mainstay treatment for benign essential blepharospasm is botulinum toxin injections. Other treatment options include photochromatic modulation, medications, transcranial magnetic stimulation, and surgical interventions.
Can benign essential blepharospasm be cured?
There is no known cure for benign essential blepharospasm, but treatment can help improve symptoms and quality of life.
What is the prognosis for patients with benign essential blepharospasm?
Benign essential blepharospasm is a chronic neurologic disorder with no known cure. Spontaneous remission is rare, but treatment can significantly improve the quality of life in patients with the condition.
What is the impact of benign essential blepharospasm on daily activities?
Some individuals with benign essential blepharospasm may experience functional disability due to the inability to open their eyes voluntarily, which can impact daily activities such as driving, reading, and social interactions.
Source Links
- https://www.aao.org/eyenet/article/management-of-benign-essential-blepharospasm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9557246/
- https://www.sciencedirect.com/topics/nursing-and-health-professions/blepharospasm
Cervical Dystonia Treatment Options Explored
Cervical dystonia, also known as spasmodic torticollis, is a neurological disorder characterized by involuntary muscle contractions in the neck, resulting in abnormal movements and postures. While there is no cure for cervical dystonia, there are several treatment options available to help manage the symptoms and improve quality of life. In this article, we will explore the various treatment approaches for cervical dystonia.
Key Takeaways:
- There are multiple treatment options available for cervical dystonia to manage symptoms.
- Treatment approaches include medications, therapies, surgical procedures, and participation in clinical trials.
- It is important to consult with a neurologist for proper diagnosis and evaluation.
- Lifestyle modifications, stress management, and support systems are also crucial aspects of treatment.
- Stay informed about advancements in cervical dystonia treatment through credible sources like Mayo Clinic and the National Institute of Neurological Disorders and Stroke.
Diagnosis of Cervical Dystonia
Diagnosing cervical dystonia is primarily done through a physical examination conducted by a neurologist, who specializes in disorders of the brain and nervous system. A comprehensive evaluation helps determine the presence of characteristic signs and symptoms of cervical dystonia. In most cases, the physical examination alone is sufficient for diagnosis.
During the examination, the doctor may observe involuntary movements, abnormal postures, and muscle spasms in the neck area. They may also assess the range of motion and muscle tone in the neck and shoulders. The doctor may inquire about the duration, frequency, and intensity of symptoms to gain a better understanding of the condition.
In some instances, additional diagnostic tests may be recommended to rule out any underlying causes of the symptoms or to confirm the diagnosis of cervical dystonia. These tests can provide further insights and help in the management of the condition.
Blood Tests
Blood tests are not specific for cervical dystonia but can be useful in ruling out other conditions that may mimic its symptoms. These tests can help identify any abnormalities in the blood, such as inflammation markers or specific antibodies that may indicate an immune-related disorder.
Magnetic Resonance Imaging (MRI)
An MRI scan uses powerful magnets and radio waves to create detailed images of the brain and the structures within it. It may be recommended to rule out any structural abnormalities or brain lesions that could be causing the symptoms of cervical dystonia. The MRI scan can provide valuable information to the neurologist and help in the accurate diagnosis of the condition.
Overall, a combination of a thorough physical examination and, if necessary, additional diagnostic tests such as blood tests or MRI can aid in the diagnosis of cervical dystonia. Consulting a neurologist is essential to ensure a proper evaluation and accurate diagnosis.
Medications for Cervical Dystonia
Medications play a crucial role in managing the signs and symptoms of cervical dystonia. Two main types of medications are commonly prescribed: botulinum toxin injections and oral muscle relaxants.
Botulinum Toxin Injections
Botulinum toxin injections, such as Botox, Dysport, Xeomin, and Myobloc, are commonly used to treat cervical dystonia. These injections work by directly targeting the affected neck muscles and temporarily paralyzing them, providing relief from muscle spasms. The injections are usually administered by a healthcare professional and need to be repeated every three to four months for optimal results.
Here is a table summarizing the different types of botulinum toxin injections used for cervical dystonia:
| Type of Botulinum Toxin Injection | Brand Name | Administration Frequency |
|---|---|---|
| Botulinum Toxin Type A | Botox | Every three to four months |
| Botulinum Toxin Type A | Dysport | Every three to four months |
| Botulinum Toxin Type A | Xeomin | Every three to four months |
| Botulinum Toxin Type B | Myobloc | Every three to four months |

Oral Muscle Relaxants
In addition to botulinum toxin injections, oral medications may also be prescribed to help manage the symptoms of cervical dystonia. These medications have a muscle-relaxing effect and can be taken orally as prescribed by a healthcare professional. They are often used to supplement the effects of botulinum toxin injections, allowing for a reduced dosage and frequency of injections.
It is important to note that the choice of medications and their dosages may vary depending on individual circumstances. A healthcare professional will evaluate the specific needs of each patient and determine the most suitable treatment plan.
Therapies for Cervical Dystonia
When it comes to managing cervical dystonia, there are various therapies that can be effective in reducing symptoms and improving your quality of life. These therapies include sensory tricks, heat packs and massage, and exercises.
Sensory Tricks
Sensory tricks are simple actions you can do to provide temporary relief from the spasms associated with cervical dystonia. These tricks involve touching certain areas to distract the brain and temporarily reduce muscle contractions. For example, you can try gently touching the opposite side of your face or the back of your head. Experiment with different sensory tricks to find what works best for you.
Heat Packs and Massage
Applying heat packs to your neck and shoulder muscles can help relax them and provide relief from the discomfort caused by cervical dystonia. Heat increases blood flow to the affected area, promoting relaxation and reducing muscle tension. Additionally, massage therapy can further relax the muscles and alleviate tension. Consult with a licensed massage therapist to determine the most suitable massage techniques for your condition.
Exercises
Specific exercises that target neck strength and flexibility can be beneficial in managing cervical dystonia. These exercises help improve muscle tone and support proper alignment of the neck. It is important to consult with a physical therapist or a qualified healthcare professional to develop an exercise routine tailored to your needs. They can guide you on proper technique and ensure you're doing the exercises safely and effectively.
Remember, individual responses to therapies can vary, so it's essential to find what works best for you. Some individuals may find certain sensory tricks or therapeutic approaches more effective than others. It's also important to keep in mind that the effectiveness of these therapies may decline as the disease progresses. Consulting with your healthcare provider will help you determine the most suitable therapies for your specific situation.

| Therapy | Benefits | Considerations |
|---|---|---|
| Sensory Tricks | Provides temporary relief from muscle contractions | Effectiveness varies for each individual |
| Heat Packs and Massage | Relaxes neck and shoulder muscles, reduces tension | Consult with a professional for proper technique |
| Exercises | Improves neck strength and flexibility | Consult with a physical therapist for a tailored routine |
Surgical Procedures for Cervical Dystonia
In cases where less invasive treatments do not provide sufficient relief, surgery may be considered as an option for cervical dystonia treatment. Surgical treatments for cervical dystonia include deep brain stimulation (DBS) and nerve cutting.
Deep brain stimulation (DBS) is a surgical procedure that involves placing a thin wire into the brain. The wire sends electrical pulses to interrupt the nerve signals causing the head to twist. This procedure aims to modulate abnormal brain activity and relieve the symptoms of cervical dystonia.
Another surgical option for cervical dystonia is nerve cutting, also known as selective denervation. In this procedure, the surgeon cuts the nerves that carry the contraction signals to the affected muscles. By interrupting the abnormal nerve signaling, nerve cutting aims to reduce muscle spasms and correct the abnormal head position.
Both deep brain stimulation and nerve cutting should be thoroughly discussed with a specialist to evaluate their potential benefits and risks. The decision to undergo surgical treatment for cervical dystonia should be made on an individual basis, taking into consideration the severity of symptoms, overall health, and personal preferences.
Advantages and Disadvantages of Surgical Treatments for Cervical Dystonia
| Advantages | Disadvantages |
|---|---|
| May provide long-lasting relief from symptoms | Risks associated with any surgical procedure |
| Can improve quality of life by reducing muscle spasms and abnormal head movements | Potential side effects or complications, such as infection, bleeding, or anesthesia-related risks |
| Alternative treatment option for individuals who do not respond to other treatments | Recovery period and rehabilitation after surgery |

Clinical Trials for Cervical Dystonia Treatment
As the field of medicine continues to advance, new treatments for cervical dystonia are being explored through clinical trials. These trials aim to test innovative interventions, medications, and management strategies that can potentially provide better outcomes for individuals with cervical dystonia. Participating in clinical trials can offer access to cutting-edge treatments and contribute to the development of new options for the prevention, diagnosis, and treatment of this condition.
If you are interested in participating in a clinical trial for cervical dystonia, there are a few avenues you can explore. Firstly, consulting with your healthcare provider can help you understand the available trials and determine if you meet the eligibility criteria. Your doctor can provide guidance on the potential benefits and risks associated with participating in a clinical trial.
Additionally, reputable clinical trial databases can be valuable resources for finding ongoing trials. Websites like ClinicalTrials.gov, which is maintained by the National Institutes of Health, allow you to search for trials based on location, eligibility criteria, and treatment options. Remember to carefully review the trial details and consult with a healthcare professional before deciding to enroll.

Coping and Support for Cervical Dystonia
Cervical dystonia can have a significant impact on your physical and emotional well-being. The discomfort in social situations, limitations in daily activities, and feelings of isolation and depression can be overwhelming. However, it's essential to remember that you are not alone in your journey with cervical dystonia. There are various coping mechanisms and support systems available to help you navigate through the challenges.
Many organizations and support groups provide valuable information, resources, and understanding for individuals and their families coping with cervical dystonia. Engaging with these communities can provide a sense of belonging, validation, and shared experiences. Additionally, your healthcare provider can guide you to local support groups or trusted online resources that can offer support and guidance specific to your needs.

Coping Strategies for Cervical Dystonia
Here are some coping strategies that may assist you in managing the challenges posed by cervical dystonia:
- Education: Learn as much as you can about cervical dystonia, its symptoms, and treatment options. Understanding the condition can empower you to make informed decisions and advocate for yourself.
- Seek Emotional Support: Connect with others going through similar experiences to share and receive emotional support. It can be helpful to have people who understand and empathize with your struggles.
- Practice Relaxation Techniques: Explore relaxation techniques such as deep breathing exercises, meditation, or yoga. These techniques can help reduce stress and manage muscle tension.
- Engage in Physical Activities: Participate in physical activities or exercises that are safe and suitable for your condition. Consult with your healthcare provider or a physical therapist to develop an exercise plan tailored to your needs.
- Set Realistic Goals: Establish realistic goals for yourself and prioritize self-care. Break larger tasks into smaller, more manageable steps to reduce stress and prevent overwhelm.
Support Resources for Cervical Dystonia
Here are some organizations and online resources that provide support and information for individuals with cervical dystonia:
| Organization | Website |
|---|---|
| Dystonia Medical Research Foundation | www.dystonia-foundation.org |
| The Dystonia Society | www.dystonia.org.uk |
| Michael J. Fox Foundation for Parkinson's Research | www.michaeljfox.org |
Remember, coping with cervical dystonia is a unique journey, and finding the right support is crucial. Reach out to these organizations or consult with your healthcare provider for guidance on coping strategies and available resources tailored to your specific needs.
Preparing for Your Appointment
To make the most of your appointment with a healthcare provider, it is helpful to come prepared. Here are some steps to follow before your cervical dystonia appointment:
- Gather information about your family's medical history. Note any genetic or neurological conditions that may be relevant to your diagnosis.
- Make a list of all the medications and dietary supplements you are currently taking. Include the dosage and frequency of each medication.
- Write down any questions or concerns you have about your condition or treatment options. This will ensure that you don't forget anything important during the appointment.
During your appointment, don't hesitate to ask your healthcare provider the following questions:
- What treatment options are available for cervical dystonia?
- What are the potential benefits and risks of each treatment?
- How long will it take to see improvements in my symptoms?
- Are there any lifestyle modifications that can help manage my symptoms?
- Are there any clinical trials or new treatments that I should consider?
By being prepared and asking the right questions, you can have a more productive and informed discussion with your healthcare provider about your cervical dystonia and its treatment options.
| Key Points to Remember: |
|---|
| Come prepared with your family's medical history, medication list, and a list of questions. |
| Ask your healthcare provider about the available treatment options and their benefits and risks. |
| Inquire about lifestyle modifications and any ongoing clinical trials or new treatments. |
Factual Data Sources for Cervical Dystonia Treatment
When seeking information on cervical dystonia treatment, it is essential to rely on trustworthy sources that provide factual and up-to-date data. The following sources offer comprehensive and reliable information on cervical dystonia and its treatment options:
Mayo Clinic
The Mayo Clinic is a renowned medical center that provides reliable information on various medical conditions, including cervical dystonia. Their website offers comprehensive resources, including articles, treatment guidelines, and research updates, supported by a team of medical professionals specializing in neurology.
National Institute of Neurological Disorders and Stroke (NINDS)
The National Institute of Neurological Disorders and Stroke, a part of the National Institutes of Health (NIH), is a reliable source of information on neurological disorders. Their website offers a wealth of resources dedicated to cervical dystonia, including treatment options, research studies, and information for healthcare professionals and patients.
Expert Reviews on Dystonia Treatment
Expert reviews and research papers on cervical dystonia treatment can provide valuable insights into the latest advancements and treatment strategies. Publications such as "Dystonia and Dystonic Syndromes" by Albanese et al. and "Botulinum Toxin in Clinical Dermatology" by Hexsel and Butterfoss are examples of credible sources that offer in-depth analysis and evidence-based recommendations for cervical dystonia treatment.
It is important to note that while these sources provide valuable information, it is always recommended to consult with a healthcare professional for personalized advice. Healthcare providers have the expertise to evaluate your specific condition and recommend the most suitable treatment plan based on your individual needs.
Lifestyle Modifications for Cervical Dystonia
In addition to medical treatments, certain lifestyle modifications can help manage the symptoms of cervical dystonia. Stress management techniques, relaxation exercises, and exploring complementary therapies can provide relief and improve your overall well-being.
Stress Management Techniques
Stress can worsen the signs and symptoms of cervical dystonia, so incorporating stress management techniques into your daily routine is essential. Here are some techniques you can try:
- Relaxation exercises: Practice deep breathing exercises, progressive muscle relaxation, or guided imagery to promote relaxation and reduce stress levels.
- Meditation: Engage in mindfulness meditation to calm the mind, reduce stress, and enhance your overall sense of well-being.
- Yoga: Participate in gentle yoga classes that focus on stretching, breathing, and relaxation to help alleviate muscle tension and improve flexibility.
- Tai Chi: Explore the gentle movements of Tai Chi, an ancient Chinese martial art, which can help improve balance, body awareness, and reduce stress levels.
Relaxation Techniques
Incorporating relaxation techniques into your daily routine can significantly improve your symptoms of cervical dystonia. Consider the following techniques:
- Deep breathing: Take slow, deep breaths, focusing on the sensation of air entering and leaving your body. Deep breathing can help relax your mind and body.
- Massage: Regularly treat yourself to a gentle neck and shoulder massage to relieve muscle tension and promote relaxation.
- Heat therapy: Apply heat packs or take warm showers to relax the muscles in your neck and shoulder area, helping to reduce pain and discomfort.
- Progressive muscle relaxation: Practice systematically tensing and relaxing different muscle groups to release muscle tension and promote a sense of calm.
By adopting these lifestyle modifications and incorporating stress management and relaxation techniques into your daily routine, you can effectively manage the symptoms of cervical dystonia and improve your overall quality of life.
Conclusion
Cervical dystonia is a complex condition that can significantly impact the lives of those affected. While there is no cure, there are various treatment options available to help manage the symptoms and improve overall well-being. Medications, such as botulinum toxin injections and oral muscle relaxants, can provide relief by reducing muscle contractions. Therapies, including sensory tricks, heat packs and massage, and targeted exercises, can help relax the neck muscles and improve flexibility. In more severe cases, surgical procedures like deep brain stimulation or nerve cutting may be considered.
Participating in clinical trials can provide access to potential innovative treatments and advancements in the field of cervical dystonia. It is also essential to seek support from healthcare professionals and connect with support groups to better cope with the challenges of the condition. By staying informed about the latest research and advancements, individuals with cervical dystonia can actively navigate their treatment journey and strive for better symptom management and quality of life.
Remember, everyone's experience with cervical dystonia is unique, and it may take time to find the most effective treatment approach. Be patient, stay positive, and continue working closely with your healthcare team to find the best strategies that work for you. With the right support and a comprehensive treatment plan, you can take control of your cervical dystonia and live a fulfilling life.
FAQ
What is cervical dystonia?
Cervical dystonia, also known as spasmodic torticollis, is a neurological disorder characterized by involuntary muscle contractions in the neck, resulting in abnormal movements and postures.
What are the treatment options for cervical dystonia?
The treatment options for cervical dystonia include medications, therapies, surgical procedures, participation in clinical trials, and lifestyle modifications.
How is cervical dystonia diagnosed?
Cervical dystonia can often be diagnosed through a physical examination. In some cases, additional tests such as blood tests or magnetic resonance imaging (MRI) may be recommended to rule out any underlying conditions causing the symptoms.
What medications are used to treat cervical dystonia?
Medications commonly used to treat cervical dystonia include botulinum toxin injections and oral muscle relaxants.
What therapies can help manage the symptoms of cervical dystonia?
Sensory tricks, heat packs and massage, and exercises that improve neck strength and flexibility can be beneficial in managing the symptoms of cervical dystonia.
Are there surgical procedures for cervical dystonia?
Yes, surgical procedures such as deep brain stimulation and nerve cutting can be considered as treatment options for cervical dystonia.
Are there any ongoing clinical trials for cervical dystonia treatment?
Yes, there are ongoing clinical trials testing new treatments, interventions, and tests for cervical dystonia. Participating in these trials can provide access to potentially innovative and more effective treatment options.
Is there support available for individuals with cervical dystonia?
Yes, there are organizations and support groups that provide information and support for individuals and their families dealing with cervical dystonia. Healthcare providers can guide individuals to local support groups or trusted online resources.
How can I prepare for my appointment with a healthcare provider?
It is helpful to gather information about the medical history of family members, as well as a list of all medications and dietary supplements being taken. It is also recommended to write down any questions about the condition or treatment options to ensure that all concerns are addressed during the appointment.
Where can I find trusted information on cervical dystonia treatment?
Trusted sources for information on cervical dystonia treatment include Mayo Clinic, National Institute of Neurological Disorders and Stroke, and expert reviews on dystonia treatment.
Are there any lifestyle modifications that can help manage cervical dystonia symptoms?
Yes, stress management techniques such as relaxation exercises, meditation, and deep breathing can be beneficial. Exploring complementary therapies like yoga or tai chi may also provide some relief.
Source Links
- https://www.mayoclinic.org/diseases-conditions/cervical-dystonia/diagnosis-treatment/drc-20354128
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3495548/
- https://rarediseases.org/rare-diseases/cervical-dystonia/