CTE Treatment Options Explored - Stay Informed
Welcome to our informative guide on chronic traumatic encephalopathy (CTE) treatment options. If you or someone you know is impacted by repetitive head trauma and concussions, this article will provide valuable insights into managing this degenerative neurological disorder.
Currently, there is no definitive way to diagnose CTE during a person's lifetime. However, there are clinical criteria for diagnosing traumatic encephalopathy syndrome (TES), which is associated with CTE. Diagnosis of CTE requires evidence of brain tissue degeneration and the presence of tau and other protein deposits in the brain, which can only be seen during an autopsy.
Research is ongoing to develop tests for diagnosing CTE while a person is alive, such as neuropsychological tests and specialized MRIs. Seeking medical care from experts, such as those at Mayo Clinic, can help address CTE-related health concerns and provide guidance on detection and management of traumatic brain injury.
While there is currently no specific treatment for CTE, the focus is on preventing head injuries and managing traumatic brain injury. In this article, we will explore the various treatment options available and discuss the importance of seeking professional care and staying informed about the latest advancements in CTE research.
Understanding Chronic Traumatic Encephalopathy (CTE)
Chronic traumatic encephalopathy (CTE) is a degenerative neurological disorder that primarily affects individuals who have experienced repetitive head trauma, particularly in sports or military settings.
The symptoms of CTE can vary from person to person, but they generally resemble those of other neurodegenerative diseases like Alzheimer's. CTE typically develops slowly over time after multiple head impacts or concussions and can lead to cognitive impairment and eventual dementia.
Common symptoms of CTE include:
- Cognitive problems: difficulties with memory, attention, and thinking processes
- Emotional changes: mood swings, depression, and irritability
- Confusion: difficulty understanding and organizing thoughts
- Difficulty with comprehension: trouble understanding and processing information
As the disease progresses, individuals may experience more severe cognitive issues, motor symptoms like tremors and rigidity, and even swallowing difficulties.
The exact causes of CTE are still being studied, but repetitive hits to the brain and repeated bouts of trauma are known to increase the risk. Athletes involved in contact sports like boxing, football, and soccer, as well as military personnel exposed to blast injuries, are particularly vulnerable to developing CTE.

Image: Chronic Traumatic Encephalopathy (CTE) - Understanding the Impact
Seeking Professional Care for CTE
Currently, there is no definitive diagnostic test for chronic traumatic encephalopathy (CTE). Diagnosing CTE is typically based on a person's history of participating in high-risk activities and the presence of symptoms and examination findings consistent with CTE. If you or someone you know is experiencing symptoms related to memory and cognition, seeking medical care is crucial for proper evaluation and management.
To start, reach out to your primary care provider who can guide you through the next steps. They may refer you to specialists such as neurologists, psychiatrists, or neuropsychologists who have expertise in diagnosing and treating CTE. These specialists will conduct a thorough evaluation and may use various tests and assessments to gather information about your symptoms and overall condition.
To make the most of your appointment, it's helpful to come prepared. Write down your symptoms, including any specific details such as when they started and how they have progressed. Provide a detailed medical history, noting any head injuries or concussions you've experienced. It's also important to bring a list of medications and supplements you are currently taking.
In some cases, additional testing may be recommended to rule out other conditions or gain further insights into the brain. Neuroimaging scans, such as MRI or CT scans, can provide detailed images of the brain and help detect any abnormalities. These tests may be helpful in confirming a diagnosis of CTE or ruling out other potential causes of your symptoms.
Remember, seeking professional care from experts who specialize in CTE is crucial for accurate diagnosis and appropriate management. They can provide personalized guidance based on your unique situation and help you navigate the complexities of living with CTE.

| Benefits of Seeking Professional Care for CTE | Drawbacks of Delaying Care |
|---|---|
|
|
Current Treatment Options for CTE
At present, there is no specific treatment or cure for chronic traumatic encephalopathy (CTE). The condition is progressive, meaning it worsens over time. The focus of current management strategies is on preventing further head injuries and minimizing the impact of traumatic brain injury.
Preventive measures include:
- Practicing safe sports techniques
- Using appropriate protective gear
- Raising awareness about the risks of repetitive head trauma
While there are no approved medications or therapies specifically designed for CTE, complementary treatments like cognitive rehabilitation and behavioral therapies may help manage some of the symptoms associated with the disease. Working closely with a healthcare team that specializes in CTE and traumatic brain injury is crucial to developing an individualized treatment plan.
Staying informed about the latest research and developments in CTE treatment is essential.
Treatment Measures for CTE
Although there is currently no cure for CTE, individuals can take certain steps to manage the condition and improve their quality of life:
- Engage in cognitive rehabilitation programs to enhance memory, attention, and executive functioning skills.
- Participate in behavioral therapies, such as counseling or psychotherapy, to address emotional changes associated with CTE.
- Follow a healthy lifestyle, including regular exercise, a balanced diet, and sufficient sleep, to support overall brain health.
- Seek support from support groups or mental health professionals to cope with the challenges posed by CTE.
It is crucial to consult with a healthcare professional experienced in managing CTE to develop a personalized treatment plan that addresses individual needs and goals.
| Treatment Strategies | Benefits |
|---|---|
| Cognitive Rehabilitation Programs | - Improve memory, attention, and executive functioning skills - Enhance overall cognitive abilities |
| Behavioral Therapies | - Address emotional changes and challenges - Provide coping strategies |
| Healthy Lifestyle | - Support brain health and function - Improve overall well-being |
| Support Groups/Mental Health Professionals | - Provide emotional support and understanding - Offer guidance on managing the impact of CTE |
While current treatment options for CTE focus on symptom management and improving quality of life, ongoing research aims to uncover new therapies and interventions that can target the underlying mechanisms of the disease. Staying informed and actively engaging in conversations with healthcare professionals can help individuals make informed decisions and access the most up-to-date treatment options available.

The Future of CTE Diagnosis and Treatment
As research in the field of chronic traumatic encephalopathy (CTE) continues to progress, there is hope for advancing the diagnosis and treatment of this degenerative neurological disorder. Scientists and clinicians are focusing on developing new diagnostic tools and treatment options to improve our understanding of the disease and provide better care for individuals affected by CTE.
One area of research involves the exploration of potential biomarkers to aid in the early detection of CTE during a person's lifetime. These biomarkers may include neuropsychological tests and specialized imaging techniques that can reveal early signs of brain tissue degeneration and the presence of tau and other protein deposits, which are characteristic of CTE. By identifying CTE at earlier stages, interventions and treatment strategies can be implemented to potentially slow down the progression of the disease and mitigate its impact.
Ongoing clinical trials are also exploring experimental treatments for CTE. These trials aim to uncover new insights into the disease and evaluate the efficacy of different therapeutic approaches. By participating in these trials, eligible individuals can contribute to the advancement of CTE research and potentially benefit from emerging treatment options.
Staying informed about the latest advancements in CTE research is crucial for individuals and their families. By keeping up to date with scientific discoveries and breakthroughs, you can better understand the disease and make informed decisions about your health and well-being. Consultation with healthcare professionals who specialize in CTE and traumatic brain injuries can provide guidance on the latest diagnostic techniques and treatment strategies.
The future holds promise for improved diagnostics and treatments for CTE. Ongoing research efforts and clinical trials are paving the way for advancements in our understanding of the disease and offering hope to individuals affected by CTE and their loved ones.
Conclusion
Chronic traumatic encephalopathy (CTE) is a degenerative neurological disorder associated with repetitive head trauma and concussions. Although there is currently no definitive way to diagnose CTE during a person's lifetime, clinical criteria exist for diagnosing traumatic encephalopathy syndrome (TES), which is associated with CTE. The focus of current management strategies for CTE is on preventing head injuries and effectively managing traumatic brain injury.
While specific treatment options for CTE are still unavailable, complementary therapies like cognitive rehabilitation and behavioral interventions can help manage symptoms. Ongoing research is dedicated to developing new diagnostic tools and treatment options for CTE, with a particular emphasis on biomarkers and clinical trials. Staying informed about the latest advancements is crucial for individuals managing CTE and working closely with healthcare professionals to make informed decisions regarding their health and well-being.
By being proactive in preventing head injuries and seeking appropriate medical care, individuals can take control of their CTE-related health concerns. While challenges remain, the scientific community's dedication to understanding and managing CTE provides hope for improved diagnostics and treatments in the future. Stay informed, stay proactive, and work closely with healthcare professionals for the best possible outcomes in your CTE journey.
FAQ
What is chronic traumatic encephalopathy (CTE)?
Chronic traumatic encephalopathy (CTE) is a degenerative neurological disorder caused by repetitive head trauma and concussions. It primarily affects individuals who have experienced repetitive head trauma, particularly in sports or military settings.
What are the symptoms of CTE?
The symptoms of CTE can vary from person to person, but they generally resemble those of other neurodegenerative diseases like Alzheimer's. Common symptoms include cognitive problems, emotional changes, confusion, and difficulty with comprehension. As the disease progresses, individuals may experience more severe cognitive issues, motor symptoms like tremors and rigidity, and even swallowing difficulties.
How is CTE diagnosed?
Currently, there is no definitive diagnostic test for CTE. A diagnosis is typically made based on a person's history of participating in high-risk activities, the presence of symptoms, and examination findings consistent with CTE. Medical professionals, such as neurologists and neuropsychologists, may be involved in the diagnostic process.
Is there a specific treatment for CTE?
At present, there is no specific treatment or cure for CTE. The focus of current management strategies is on preventing further head injuries and minimizing the impact of traumatic brain injury. Complementary treatments like cognitive rehabilitation and behavioral therapies may help manage some of the symptoms associated with the disease.
What is the future of CTE diagnosis and treatment?
Ongoing research is focused on advancing our understanding of CTE and developing new diagnostic tools and treatment options. Scientists and clinicians are exploring potential biomarkers and specialized imaging techniques to aid in the early detection of CTE during a person's lifetime. Clinical trials investigating experimental treatments for CTE are also underway.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8069746/
- https://www.mayoclinic.org/diseases-conditions/chronic-traumatic-encephalopathy/diagnosis-treatment/drc-20370925
- https://www.vedantu.com/biology/chronic-traumatic-encephalopathy
Unveiling Chronic Traumatic Encephalopathy Causes
Welcome to our informative article that delves into the causes of chronic traumatic encephalopathy (CTE). If you or someone you know participates in contact sports or has a history of traumatic brain injuries, understanding the underlying factors behind this progressive brain disease is crucial. In this section, we will explore the primary causes of CTE and shed light on the risk factors associated with this debilitating condition.
Chronic traumatic encephalopathy is often linked to repeated traumatic brain injuries, including concussions and repeated blows to the head. Athletes engaged in contact sports, such as boxers and football players, as well as military veterans, face the greatest risk due to the higher chances of sustaining frequent head trauma.
While the exact causes of CTE are still being researched, the accumulation of abnormal tau protein in the brain appears to be a significant contributing factor. Studies have shown that individuals who experience traumatic brain injuries in early to midlife have an increased risk of developing dementia later in life.
Furthermore, the risk of developing CTE is further heightened in individuals who have experienced multiple traumatic brain injuries throughout their lives. The long-term effects of enduring such injuries can manifest in the form of cognitive decline, memory problems, and behavioral changes.
In the subsequent sections, we will delve into a comprehensive examination of the symptoms, diagnostic methods, ongoing research, and potential treatments for chronic traumatic encephalopathy. Stay tuned to gain a better understanding of this complex condition and the steps you can take to prioritize brain health.
Symptoms of Chronic Traumatic Encephalopathy
Chronic traumatic encephalopathy (CTE) can manifest with a range of symptoms that may vary from person to person. While researchers do not unanimously agree on the specific signs of the disease, there are common symptoms associated with CTE that individuals should be aware of.
- Memory and thinking problems: CTE can lead to difficulties with memory, concentration, and cognitive function. This may manifest as forgetfulness, difficulty making decisions, and impaired problem-solving skills.
- Confusion: Individuals with CTE may experience a sense of confusion or disorientation, particularly in unfamiliar or complex situations.
- Personality changes: CTE can cause significant changes in personality, leading to alterations in mood, behavior, and overall temperament.
- Erratic behavior: Aggression, impulsivity, anger, and irritability are often observed in individuals with CTE. These behavioral changes can impact personal and professional relationships.
- Depression and suicidal thoughts: CTE has been linked to an increased risk of depression and suicidal ideation. These symptoms should always be taken seriously and addressed with professional help.
- Attention and organization problems: Difficulty concentrating, staying focused, and organizing thoughts and tasks are common challenges faced by individuals with CTE.
- Balance and motor skill issues: CTE can affect motor coordination and balance, leading to problems with movements and coordination.
It is important to note that the onset of these symptoms may not occur immediately after the brain injuries but may present years or even decades later. This delayed manifestation can make it challenging for individuals to connect their current symptoms with past traumatic brain injuries.
To provide a visual representation of the symptoms associated with CTE, refer to the table below:
| Symptoms of Chronic Traumatic Encephalopathy |
|---|
| Memory and thinking problems |
| Confusion |
| Personality changes |
| Erratic behavior |
| Depression and suicidal thoughts |
| Attention and organization problems |
| Balance and motor skill issues |
Note: The table above provides a concise visual summary of the common symptoms associated with chronic traumatic encephalopathy.
It is crucial for individuals who have experienced multiple traumatic brain injuries or have been involved in contact sports or military service to be vigilant about their brain health and seek medical attention if they experience any of these symptoms. Early detection and management are key to maximizing quality of life and providing appropriate support.
Diagnosis of Chronic Traumatic Encephalopathy
Diagnosing chronic traumatic encephalopathy (CTE) can be challenging, as a definitive diagnosis can only be made after death through a brain examination. However, there are methods available to help identify potential cases and rule out other causes of symptoms while the individual is still alive.
A comprehensive approach is typically adopted, which includes:
- Medical history: Your medical history, including any instances of traumatic brain injuries (TBIs), will be assessed. This information helps the healthcare provider evaluate the potential risk of CTE.
- Mental status testing: Cognitive and psychological tests may be conducted to assess memory, thinking, and behavioral changes. These tests help in identifying the possible symptoms of CTE.
- Neurological exams: Physical evaluations, including neurological exams, can provide valuable insights into motor skills, balance, reflexes, and sensory perception.
- Brain imaging: Advanced imaging techniques, such as MRI or PET scans, may be utilized to detect any abnormalities in the brain structure or function. These scans can help differentiate CTE from other brain disorders.
While these approaches can assist in diagnosing CTE, they cannot provide a definitive confirmation. Currently, researchers are focusing on identifying biomarkers or specific imaging patterns that can aid in the early diagnosis of CTE.
| Diagnosis Methods | Pros | Cons |
|---|---|---|
| Autopsy | - Definitive confirmation of CTE presence | - Requires postmortem examination |
| Medical history | - Helpful in assessing risk factors | - Relies on accurate recollection of past events |
| Mental status testing | - Identifies cognitive and behavioral changes | - Results may vary and are subjective |
| Neurological exams | - Evaluates motor skills and sensory perception | - Findings may be non-specific |
| Brain imaging | - Provides visual insights into brain structure | - Cannot definitively diagnose CTE |
Treatment and Research on Chronic Traumatic Encephalopathy
Currently, there is no cure or specific treatment for chronic traumatic encephalopathy (CTE). However, certain medications may be used to temporarily manage the cognitive and behavioral symptoms associated with the disease. Ongoing research is being conducted by various organizations, such as the National Institute of Neurological Disorders and Stroke (NINDS) and the Brain Injury Research Institute (BIRI), to better understand the causes, risk factors, and progression of CTE. The Alzheimer's Association has also invested significant funds in research grants to further explore the connection between CTE and dementia.
Medications for Symptom Management
Although there is no cure for CTE, some medications can help alleviate certain symptoms in individuals with the disease. These medications are primarily aimed at managing cognitive impairments, mood disorders, and behavioral changes. Commonly prescribed medications for CTE may include:
- Antidepressants: These medications can be used to address symptoms of depression and anxiety often associated with CTE.
- Mood stabilizers: Mood stabilizing drugs can help regulate mood swings and reduce impulsive behaviors in individuals with CTE.
- Memory enhancers: Some medications may be prescribed to improve memory and cognitive function in individuals with CTE.
It is important to note that while these medications may help manage symptoms, they do not alter the progression of the disease or provide a long-term solution.
Ongoing Research Efforts
Researchers are actively investigating various aspects of CTE to advance our understanding and develop more effective treatments. The NINDS and BIRI, among other institutions, are conducting studies to identify biomarkers, imaging techniques, and other diagnostic tools that can aid in the early detection and monitoring of CTE. They are also investigating potential neuroprotective therapies that could slow down or prevent the progression of the disease.
In recent years, there has been a growing focus on developing interventions that target the accumulation of abnormal tau protein in the brain, a hallmark of CTE. Researchers are exploring different approaches, including immunotherapies and gene therapies, to inhibit tau aggregation and promote its clearance from the brain.
Additionally, efforts are being made to improve safety protocols in contact sports and military operations to reduce the incidence of TBIs and minimize the risk of developing CTE. Enhanced protective gear, rule changes, and education initiatives are being implemented to prioritize player safety and concussion prevention.

Current Challenges and Future Directions
Chronic traumatic encephalopathy remains a complex condition that poses significant challenges in terms of diagnosis, treatment, and prevention. As research continues, it is hoped that advancements in understanding CTE's underlying mechanisms will lead to the development of targeted therapies and preventive strategies.
By collaborating across disciplines and investing in innovative research, scientists aim to unravel the mysteries surrounding CTE and provide much-needed support for affected individuals and their families.
Conclusion
Chronic traumatic encephalopathy (CTE) is a serious and devastating brain disease that is strongly associated with repeated traumatic brain injuries. Athletes participating in contact sports and military veterans, who are more prone to head trauma, face a higher risk of developing CTE. Although the exact causes and progression of the disease are still being researched, there is currently no known cure.
Ongoing research efforts are aimed at deepening our understanding of CTE, enhancing diagnostic methods, and exploring potential treatments to support individuals affected by the disease. It is of utmost importance to prioritize brain health and take preventive measures to minimize the risk of traumatic brain injuries. Such measures can include using appropriate protective gear, adopting safe playing techniques, and promoting concussion awareness and management protocols.
By staying informed and vigilant, we can work together to create a safer environment for athletes and individuals at risk of traumatic brain injuries. Continued research and advancements in the field of CTE not only provide hope for improved diagnosis and treatment options in the future but also contribute to the overall well-being and long-term brain health of individuals worldwide.
FAQ
What is chronic traumatic encephalopathy (CTE)?
Chronic traumatic encephalopathy (CTE) is a progressive and fatal brain disease that is associated with repeated traumatic brain injuries (TBIs), including concussions and repeated blows to the head.
Who is at the greatest risk of developing CTE?
Athletes who play contact sports, such as boxers and football players, as well as military veterans, are at the greatest risk of developing CTE due to the increased chances of enduring repeated head trauma.
What are the symptoms of chronic traumatic encephalopathy?
Symptoms of chronic traumatic encephalopathy can vary from person to person and may include memory and thinking problems, confusion, personality changes, aggression, depression, and even suicidal thoughts. Other potential symptoms include problems with attention, organization, balance, and motor skills.
How is chronic traumatic encephalopathy diagnosed?
Currently, a definitive diagnosis of chronic traumatic encephalopathy can only be made after death through an autopsy that examines the brain for the presence of the characteristic changes associated with CTE. However, while the individual is still alive, a medical history, mental status testing, neurological exams, and brain imaging may be used to help identify potential cases of CTE and rule out other causes of symptoms.
Is there a cure or treatment for chronic traumatic encephalopathy?
Currently, there is no cure or specific treatment for chronic traumatic encephalopathy. However, certain medications may be used to temporarily manage the cognitive and behavioral symptoms associated with the disease. Ongoing research is being conducted to better understand the causes and progression of CTE and to explore potential treatments.
Source Links
- https://www.alz.org/alzheimers-dementia/what-is-dementia/related_conditions/chronic-traumatic-encephalopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8069746/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6532781/
Friedreich's Ataxia Life Expectancy Insights
Welcome to our insightful exploration of Friedreich's Ataxia (FA) life expectancy in India. If you or a loved one are impacted by this progressive degenerative condition, it's crucial to understand the factors that influence life expectancy and gain valuable insights. In this article, we will delve into important aspects such as the age of disease onset, severity of symptoms, and complications that can affect the lifespan of individuals with Friedreich's Ataxia. By shedding light on these factors, we aim to empower you with knowledge and provide a better understanding of the challenges faced by those living with FA in India.
Understanding Friedreich's Ataxia Diagnosis
Diagnosing Friedreich's ataxia involves a combination of clinical symptoms, genetic testing, and neurological examinations. Common symptoms of Friedreich's ataxia include progressive ataxia, muscle weakness, loss of sensation, and impaired speech.
Genetic testing plays a crucial role in the diagnosis of Friedreich's ataxia. It helps to identify the presence of GAA trinucleotide expansions in the frataxin gene, which is responsible for the condition. By analyzing the genetic makeup, healthcare professionals can confirm the diagnosis and understand the underlying causes of the disease.
Neurological examinations are another important component of the diagnostic process. These assessments help evaluate the extent of neurological impairments caused by Friedreich's ataxia. They provide valuable insights into the specific areas of the nervous system affected by the condition, aiding in treatment planning and management.
Early and accurate diagnosis is crucial in managing Friedreich's ataxia effectively. It allows healthcare providers to develop personalized treatment plans, provide appropriate interventions, and offer support tailored to the individual's needs.
Diagnosis Algorithm:
Here is a step-by-step overview of the diagnosis process for Friedreich's ataxia:
- Consultation with a healthcare professional specializing in neurology or genetics.
- Evaluation of symptoms, medical history, and family history.
- Physical examination to assess motor skills, coordination, and reflexes.
- Genetic testing to detect GAA trinucleotide expansions in the frataxin gene.
- Neurological examinations, including imaging tests such as magnetic resonance imaging (MRI), to evaluate nervous system involvement.
- Confirmation of diagnosis and discussion of treatment options with the healthcare provider.
By following this diagnostic algorithm, healthcare professionals can accurately identify Friedreich's ataxia and initiate appropriate management strategies to improve the quality of life for individuals with the condition.
| Diagnostic Methods | Advantages | Limitations |
|---|---|---|
| Genetic testing | - Provides definitive confirmation of the diagnosis - Identifies carriers and determines the risk for future generations - Can be performed at any age | - May not detect rare mutations - Costly and not readily available in all healthcare settings |
| Neurological examinations | - Assesses the extent and progression of neurological impairments - Guides treatment planning and management | - Results may vary depending on individual interpretation - Requires specialized expertise |
| Physical examination | - Evaluates motor function, coordination, and reflexes - Provides a comprehensive overview of the individual's physical capabilities | - Relies on subjective assessments - Does not provide genetic confirmation |
Complications of Friedreich's Ataxia
Friedreich's ataxia is a complex condition that can give rise to various complications, impacting different aspects of the body. These complications include:
- Cardiomyopathy: The most common cause of death in patients with Friedreich's ataxia, cardiomyopathy refers to the weakening and enlargement of the heart muscle, leading to poor cardiac function.
- Diabetes Mellitus: Some individuals with Friedreich's ataxia may develop diabetes mellitus, a chronic condition characterized by high blood sugar levels.
- Scoliosis: Scoliosis is a lateral curvature of the spine that can occur in individuals with Friedreich's ataxia, leading to postural issues and discomfort.
- Foot Deformities: Friedreich's ataxia can cause abnormalities in the structure and alignment of the feet, resulting in difficulties with walking and balance.
- Retained Tendon Reflexes: Friedreich's ataxia affects the signaling between the nerves and muscles, leading to retained tendon reflexes, which can contribute to muscle stiffness and impaired coordination.
While cardiomyopathy is the primary cause of death in Friedreich's physical therapy for ataxia patients, other complications can also contribute to mortality. These include stroke, diabetic coma, ischemic heart disease, trauma sequelae, and bronchopneumonia. It is important to manage these complications effectively to improve the overall quality of life and extend life expectancy in individuals with Friedreich's ataxia.
Prognosis of Friedreich's Ataxia
The prognosis of Friedreich's ataxia can vary depending on the age of onset, severity of symptoms, and presence of complications. A study from the early 1980s reported the mean age of death in patients with Friedreich's ataxia to be 37.5 years. Another study found a median age of death of 34.5 years and a median estimated survival from disease onset of 36 years. More recent studies have reported a mean age of death of 36.5 years and a majority of deaths occurring between the ages of 16 and 45 years.
However, advancements in medical care and interventions have improved the life expectancy of patients with Friedreich's ataxia in recent years.
Medical advancements and interventions have offered hope for individuals with Friedreich's ataxia, increasing their life expectancy and improving quality of life. It is essential for patients with FA to receive early diagnosis, appropriate medical care, and access to supportive therapies to enhance their prognosis.
| Study | Mean Age of Death | Median Age of Death | Median Estimated Survival from Disease Onset |
|---|---|---|---|
| Early 1980s Study | 37.5 years | - | - |
| Recent Studies | 36.5 years | 34.5 years | 36 years |
While the prognosis of Friedreich's ataxia still presents challenges, ongoing research and advancements in medical management offer hope for improved outcomes and extended survival rates for individuals with the condition.
Genetic Factors and Friedreich's Ataxia
Friedreich's ataxia is an autosomal recessive disease that is primarily caused by mutations in the frataxin gene. This gene is responsible for producing a protein called frataxin, which plays a crucial role in mitochondrial function and iron regulation. When there are GAA trinucleotide expansions in the frataxin gene, it leads to a reduction in the production of frataxin. This reduction results in mitochondrial dysfunction and the accumulation of iron in the body.
The number of GAA repeats in the frataxin gene is linked to the age at which the disease manifests and the severity of its symptoms. Patients with a higher number of GAA repeats tend to experience an earlier onset of the disease and more severe symptoms. This genetic factor plays a significant role in determining the progression and prognosis of Friedreich's ataxia.
Understanding the genetic factors involved in Friedreich's ataxia is crucial for both diagnosis and potential future treatments. By identifying these genetic markers, healthcare professionals can develop targeted interventions that aim to mitigate the effects of the disease and improve the quality of life for individuals living with Friedreich's ataxia.
Genetic Factors and Friedreich's Ataxia
| Genetic Factor | Impact on Friedreich's Ataxia |
|---|---|
| Frataxin gene mutations | Causes reduced production of frataxin, leading to mitochondrial dysfunction and iron accumulation |
| GAA trinucleotide expansions | Associated with earlier disease onset and more severe symptoms |
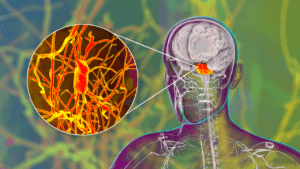
Neurological Pathology of Friedreich's Ataxia
Friedreich's ataxia, a progressive neurodegenerative disorder, primarily affects the central and peripheral nervous systems. The disease leads to degeneration and loss of neurons in various regions, including:
- The dorsal columns
- The corticospinal tracts
- The dentate nucleus
- The spinal ganglia
This degeneration results in significant neurological impairments and manifests as ataxic symptoms. The loss of myelinated fibers in the spinal cord and sensory ganglia leads to sensory ataxia and the loss of tendon reflexes. Particularly, the dentate nucleus exhibits severe neuronal loss and modification of corticonuclear terminals.
The neurological pathology of Friedreich's ataxia plays a crucial role in the progression and expression of symptoms associated with the condition.
| Region | Neuronal Loss |
|---|---|
| Dorsal columns | Degeneration and loss of neurons |
| Corticospinal tracts | Degeneration and loss of neurons |
| Dentate nucleus | Severe neuronal loss and modification of corticonuclear terminals |
| Spinal ganglia | Degeneration and loss of neurons |
Factors Affecting Friedreich's Ataxia Life Expectancy and Survival Rates
Several factors can influence the life expectancy and survival rates of individuals with Friedreich's ataxia. These factors include:
Age of Disease Onset
The age at which Friedreich's ataxia symptoms manifest can impact life expectancy. Generally, an earlier onset is associated with a shorter life expectancy.
Severity of Symptoms
The severity of symptoms experienced by individuals with Friedreich's ataxia can also affect life expectancy. Those with more severe symptoms may have a reduced life expectancy compared to individuals with milder symptoms.
Presence of Complications
Complications such as cardiomyopathy and diabetes can further shorten the life expectancy of individuals with Friedreich's ataxia. These complications require careful management to improve overall outcomes.
Access to Medical Care and Interventions
Access to proper medical care, including cardiac management and supportive therapies, can significantly impact life expectancy and survival rates for individuals with Friedreich's ataxia.
While early onset, severe symptoms, and complications can be associated with a shorter life expectancy in Friedreich's ataxia, advancements in medical care have contributed to improved life expectancy and survival rates in recent years.
Promising Advances in Friedreich's Ataxia Management and Treatment
Research and advancements in the management and treatment of Friedreich's ataxia offer hope for individuals living with the condition. Current approaches aim to address the underlying genetic defects, manage complications, and provide supportive care.
Potential treatments being explored include:
- Gene therapy
- Frataxin replacement therapy
- Pharmacological approaches to enhance mitochondrial function and reduce oxidative stress
Clinical trials are ongoing to evaluate the safety and efficacy of these treatments. These innovative therapies have the potential to significantly improve the quality of life for individuals with Friedreich's ataxia.
Multidisciplinary Care Teams
Managing Friedreich's ataxia requires a multidisciplinary approach. Care teams comprising neurologists, cardiologists, physical therapists, and genetic counselors play a crucial role in providing comprehensive care and support. They work collaboratively to address the unique challenges posed by FA, tailor treatment plans, and optimize outcomes.
Supportive Care and Symptom Management
In addition to targeted therapies, supportive care is crucial in improving the overall quality of life for individuals with Friedreich's ataxia. Symptom management strategies include:
- Physical therapy to address muscle weakness and promote mobility
- Cardiac management to monitor and treat cardiomyopathy
- Pain management techniques to alleviate discomfort
Proactive management of complications such as scoliosis, foot deformities, and diabetes mellitus further contribute to symptom relief and improved functioning.
The combination of advanced treatments, multidisciplinary care, and supportive strategies offers considerable promise in the management and treatment of Friedreich's ataxia. Ongoing research and clinical trials continue to push the boundaries of medical understanding, instilling hope in the FA community and advancing towards a brighter future.
Conclusion
Friedreich's ataxia is a progressive degenerative condition that affects the central and peripheral nervous systems, leading to various symptoms and complications. Individuals with FA often face a shorter life expectancy compared to the general population, primarily due to cardiac dysfunction, the most common cause of death in FA patients. However, there is hope on the horizon.
Advancements in medical care and treatments for Friedreich's ataxia have shown promise in recent years, resulting in improvements in life expectancy and survival rates. These advancements include targeted therapies, such as gene therapy and frataxin replacement therapy, along with pharmacological approaches to enhance mitochondrial function and reduce oxidative stress.
To continue fostering progress in managing Friedreich's ataxia, it is crucial to raise awareness, support ongoing research efforts, and provide comprehensive care to enhance the quality of life for individuals living with FA, not only in India but also worldwide. The pursuit of further research and development of innovative therapies holds the potential to transform the prognosis and outcomes for those affected by Friedreich's ataxia.
By coming together as a global community, we can make a difference in the lives of individuals with Friedreich's ataxia and pave the way for a brighter future. Let us stand together, supporting and advocating for those living with FA, as we strive for a world where this debilitating condition no longer limits their potential.
FAQ
What is Friedreich's ataxia?
Friedreich's ataxia is a progressive degenerative condition that affects the central and peripheral nervous systems, leading to various symptoms and complications.
What is the life expectancy for individuals with Friedreich's ataxia?
The life expectancy of individuals with Friedreich's ataxia is generally shorter than that of the general population, with cardiac dysfunction being the most common cause of death.
Are there any advancements in medical care and treatments for Friedreich's ataxia?
Yes, advancements in medical care and treatments are offering hope for those diagnosed with Friedreich's ataxia, with improvements in life expectancy and survival rates observed in recent years.
How is Friedreich's ataxia diagnosed?
Friedreich's ataxia is diagnosed through a combination of clinical symptoms, genetic testing, and neurological examinations.
What are the complications associated with Friedreich's ataxia?
Friedreich's ataxia can lead to various complications, including cardiomyopathy, diabetes mellitus, scoliosis, foot deformities, and retained tendon reflexes.
What factors can affect the life expectancy and survival rates of individuals with Friedreich's ataxia?
Factors such as age of disease onset, severity of symptoms, presence of complications, and access to medical care and interventions can influence the life expectancy and survival rates of individuals with Friedreich's ataxia.
What are the genetic factors associated with Friedreich's ataxia?
Friedreich's ataxia is an autosomal recessive disease caused by mutations in the frataxin gene, which leads to reduced production of frataxin and mitochondrial dysfunction.
What is the role of neurological pathology in Friedreich's ataxia?
Neurological pathology plays a key role in the manifestation of ataxic symptoms in Friedreich's ataxia, leading to degeneration and loss of neurons in various regions of the nervous system.
What promising advances are being made in the management and treatment of Friedreich's ataxia?
Current research is exploring potential treatments such as gene therapy, frataxin replacement therapy, and pharmacological approaches to enhance mitochondrial function and reduce oxidative stress in individuals with Friedreich's ataxia.
Understanding End Stage Cerebellar Ataxia
Welcome to our comprehensive guide on understanding end stage cerebellar ataxia. If you or a loved one are dealing with this challenging condition, we are here to provide you with valuable insights into its impact on daily life and effective coping strategies. With a deeper understanding of end stage cerebellar ataxia, you can navigate through this journey with confidence and support
Cerebellar ataxia is a complex neurological disorder characterized by poor muscle control and coordination due to damage to the cerebellum or its connections. In this article, we will explore the definition, causes, and symptoms of cerebellar ataxia, as well as delve into the anatomy and physiology of the cerebellum. By understanding the underlying mechanisms and impact of this condition, you can better navigate its challenges.
We will also discuss the different classifications of cerebellar ataxias, including acquired, genetic, and sporadic ataxias, to provide you with a comprehensive overview. Furthermore, our guide will cover the diagnostic approaches used by healthcare professionals to identify ataxias accurately, including clinical evaluations, neuroimaging, and genetic testing.
Managing and treating ataxia is a crucial aspect of the journey. Throughout this article, we will outline various treatment and management strategies aimed at enhancing daily functionality and quality of life. From physical therapy to adaptive devices, we will explore the range of options available. Additionally, we will discuss the importance of emotional well-being and support systems for coping with end stage cerebellar ataxia.
Stay tuned as we delve deeper into each aspect of end stage cerebellar ataxia, providing you with valuable insights and guidance. By equipping yourself with knowledge and understanding, you can navigate this challenging journey with resilience and optimism.
What is Cerebellar Ataxia?
Cerebellar ataxia is a neurological disorder characterized by poor muscle control and coordination, resulting from damage to the cerebellum or its connections.
Definition
Cerebellar ataxia refers to the impairment of voluntary muscle movement and coordination due to cerebellar dysfunction or damage. It affects the body's ability to maintain balance, perform smooth and coordinated movements, and control speech and eye movements.
Causes
The causes of cerebellar ataxia can be classified into three broad categories:
- Acquired: Cerebellar ataxia can be acquired as a result of factors such as brain injury, stroke, tumors, infection, or exposure to toxins.
- Degenerative: Certain degenerative conditions, such as Spinocerebellar Ataxia (SCAs) and Friedreich's Ataxia, can cause progressive damage to the cerebellum.
- Hereditary: Cerebellar ataxias can also be inherited genetically, with several different gene mutations associated with the condition.
Symptoms
The symptoms of cerebellar ataxia can vary depending on the underlying cause and the extent of damage to the cerebellum. Common symptoms include:
- Poor coordination and unsteady movements
- Difficulty with balance and walking
- Speech difficulties, such as slurred or dysarthric speech
- Abnormal eye movements, including nystagmus (involuntary eye movement)
- Tremors or involuntary muscle contractions
Anatomy and Physiology of the Cerebellum
The cerebellum, a vital component of the brain, plays a crucial role in motor coordination, balance, and executing precise movements. Despite its modest size compared to the rest of the brain, the cerebellum houses a significant number of neurons, illustrating its importance in various functions.
The complex microanatomy of the cerebellum enables its intricate interconnectedness with other brain regions, facilitating sensory integration and accurate motor planning. This intricate network ensures seamless communication between the cerebellum and other parts of the brain, allowing for smooth coordination of motor functions.
Moreover, the cerebellum's influence extends beyond motor control. It also plays a vital role in cognitive function and emotions. Recent research suggests that the cerebellum contributes to cognitive processes such as attention, language, and working memory. Its involvement in emotional regulation and affective processing further emphasizes its significance in overall brain function.
Cerebellum Anatomy and Physiology at a Glance:
- Responsible for motor coordination, balance, and precise movements.
- Accounts for a small percentage of brain volume but houses a significant number of neurons.
- Complex microanatomy enables sensory integration and accurate motor planning.
- Interconnected with other brain regions for seamless communication.
- Influences cognitive function, including attention, language, and working memory.
- Plays a role in emotional regulation and affective processing.
To better understand the cerebellum's significance in guiding motor function, cognitive processes, and emotional regulation, let's explore the specific structures and physiological mechanisms that contribute to its overall functioning.
| Structure | Function |
|---|---|
| Cerebellar hemispheres | Control motor coordination and movement precision on the same side of the body. |
| Vermis | Regulates posture, balance, and coordination of the trunk and axial muscles. |
| Deep cerebellar nuclei | Receive input from the cerebellar cortex and send output signals to various brain regions to coordinate motor activities. |
| Cerebellar cortex | Consists of three layers: molecular, Purkinje, and granular. The molecular layer contains dendrites, the Purkinje layer connects the cerebellar cortex to deep nuclei, and the granular layer contains granule cells that integrate sensory and motor information. |
| Cerebellar peduncles | Connect the cerebellum with other parts of the brain, including the brainstem and cerebral cortex, facilitating communication and coordination. |
Understanding Ataxia Symptoms

Ataxia is a condition that manifests in various ways, impacting an individual's mobility, coordination, and speech. The symptoms of ataxia can differ from person to person, but there are common signs to be aware of. These symptoms include:
- Difficulties with walking and balance
- Impaired coordination and motor skills
- Speech difficulties, including slurred or unclear speech
- Balance problems and a tendency to stumble or fall
- Tremors or shaky movements
- Poor handwriting and difficulty with fine motor tasks
- Problems with eye movements, such as involuntary eye jerking
The severity of these symptoms can range from mild to severe, and they may progress over time. It's important to note that each individual may experience a unique combination of symptoms. These symptoms can significantly impact daily life, making it essential for individuals with ataxia to seek proper medical care and support.
Understanding the symptoms of ataxia is crucial for early detection and intervention. If you or someone you know is experiencing any of these symptoms, it's important to consult a healthcare professional for a proper diagnosis and appropriate management.
Classification of Cerebellar Ataxias
Cerebellar ataxias can be classified into three broad categories: acquired, genetic, and sporadic. Understanding the classification of ataxias is essential for diagnosing and managing these conditions effectively.
Acquired Ataxias
Acquired ataxias are caused by external factors that result in damage to the cerebellum or its connections. These factors can include:
- Alcohol misuse
- Medication side effects
- Toxins
- Nutritional deficiencies
Genetic Ataxias
Genetic ataxias are inherited conditions caused by gene mutations. They can be further classified into dominant or recessive forms:
- Dominant genetic ataxias: These ataxias are caused by mutations in a single gene copy. They have a 50% chance of being passed on to offspring if one parent carries the mutated gene. Examples include Spinocerebellar Ataxia.
- Recessive genetic ataxias: These ataxias occur when both copies of a gene contain mutations. They are typically inherited when both parents carry a single mutated gene. Examples include Friedreich's Ataxia and ataxia telangiectasia.
Sporadic Ataxias
Sporadic ataxias refer to a group of ataxias that have no discernible cause, despite thorough evaluation. These ataxias can present without a clear genetic or acquired component. Examples of sporadic ataxias include multiple system atrophy and idiopathic late-onset cerebellar ataxia.
Understanding the classification of cerebellar ataxias helps in guiding the diagnostic process and determining appropriate management strategies for individuals with ataxia.
| Category | Causes | Examples |
|---|---|---|
| Acquired Ataxias | Alcohol misuse, medication side effects, toxins, nutritional deficiencies | Alcohol-related cerebellar degeneration, drug-induced ataxia |
| Genetic Ataxias | Inherited gene mutations | Spinocerebellar ataxia, Friedreich's ataxia |
| Sporadic Ataxias | No discernible cause | Multiple system atrophy, idiopathic late-onset cerebellar ataxia |
Diagnostic Approach for Ataxias
Diagnosing ataxias can be challenging due to the overlapping symptoms and diverse etiologies. To determine the underlying cause and provide appropriate Ataxia New Treatment, a comprehensive diagnostic approach is essential.
A detailed medical history is the first step in the diagnostic process. This involves gathering information about the patient's symptoms, medical conditions, and family history. A thorough neurological examination is then conducted to assess motor function, balance, coordination, and reflexes.
Clinical evaluation plays a crucial role in diagnosing ataxias. Neurologists use clinical rating scales to quantify the severity of symptoms and track disease progression. These scales provide valuable insights into motor impairment, speech difficulties, and balance problems.
Neuroimaging and Genetic Testing
Neuroimaging, such as brain MRI, is recommended for all ataxia cases. It helps identify specific lesions in the cerebellum or other regions of the brain. MRI scans can reveal structural abnormalities, tumors, or signs of degeneration that may be causing the ataxia.
Genetic testing may also be necessary, especially when hereditary ataxias are suspected. This involves analyzing the patient's DNA for specific genetic mutations associated with ataxias. Genetic testing can confirm or rule out a genetic cause and provide important information for prognosis and family planning.
By combining clinical evaluation, neuroimaging, and genetic testing, healthcare professionals can accurately diagnose ataxias and develop an individualized Cerebellar Ataxia Treatment plan.
Treatment and Management Strategies for Ataxia
The treatment and management of ataxia depend on the underlying cause and specific symptoms. While there is no cure for most forms of ataxia, there are various strategies that can help manage the condition and improve quality of life. For example, individuals diagnosed with Spinocerebellar Ataxia can explore supportive therapies and adaptive devices to enhance daily functioning and mobility.
1. Physical Therapy
Physical therapy plays a crucial role in the treatment of ataxia. It focuses on improving coordination, balance, and muscle control. The aim is to enhance overall mobility and independence. A qualified physical therapist will develop a personalized exercise program that may include balance training, strength exercises, and coordination drills.
2. Occupational Therapy
Occupational therapy can assist individuals with ataxia in performing activities of daily living. An occupational therapist will provide strategies and adaptive techniques to overcome challenges related to self-care, work, and leisure activities. They may recommend modified tools or assistive devices to enhance independence.
3. Speech Therapy
Speech difficulties are common in ataxia, affecting both articulation and vocal control. Speech therapy can help individuals improve their speech clarity, volume, and swallowing abilities. A speech-language pathologist will design exercises and techniques tailored to the individual's specific needs.
4. Adaptive Devices
The use of adaptive devices can provide support and enhance independence for individuals with ataxia. Walkers, canes, and orthotic devices can assist in maintaining balance and stability while walking. Additionally, devices such as hand splints and utensil grips can help compensate for fine motor difficulties. For those seeking relief from foot and leg discomfort, which is common in ataxia, the Creliver EMS & TENS Foot Circulation Stimulator or Creliver EMS Foot Stimulator Pro can be a beneficial tool. This device enhances circulation, reduces pain, and improves muscle function, making it a valuable addition to your ataxia management plan.
5. Regular Exercise and Balanced Diet
Regular exercise is crucial for overall health and well-being. Engaging in low-impact aerobic exercises, such as swimming or cycling, can help improve cardiovascular fitness without putting excess strain on the joints. A balanced diet, rich in vitamins and minerals, can support overall health and provide essential nutrients for optimal functioning of the body.
It is important to consult with a healthcare professional for an individualized treatment plan based on the specific needs and challenges associated with ataxia.
Coping with End Stage Cerebellar Ataxia
Coping with end stage cerebellar ataxia can be a challenging journey, both physically and emotionally. However, with the right strategies and support systems, you can enhance your well-being and maintain a positive outlook on life.
One of the most crucial aspects of coping with end stage ataxia is having a strong support system. Surrounding yourself with understanding family members, friends, and compassionate healthcare professionals can make a world of difference. They can provide the necessary emotional support, assist with daily activities, and offer a listening ear when you need it the most.
Joining support groups specific to cerebellar ataxia can also be immensely beneficial. These groups provide a safe space for individuals with similar experiences to share their challenges, achievements, and coping strategies. Connecting with others who understand what you are going through can provide a sense of unity and validation.
Support Systems for Coping with End Stage Cerebellar Ataxia
To help you navigate the emotional rollercoaster that can accompany end stage ataxia, consider seeking counseling or therapy. Talking to a trained professional who specializes in neurodegenerative conditions can assist you in processing your feelings, managing stress, and building resilience.
Education about your condition is key to understanding it better and finding effective coping mechanisms. Stay informed by reading credible sources, attending webinars or workshops, and seeking guidance from reliable medical professionals. The more you know about your condition, the better equipped you will be to manage it.
| Coping Strategies for End Stage Cerebellar Ataxia |
|---|
| Practice mindfulness techniques to stay present, reduce anxiety, and improve overall well-being. |
| Engage in stress management activities such as deep breathing exercises, yoga, or meditation to help alleviate tension. |
| Maintain a positive outlook by focusing on the things you can still enjoy and accomplish despite the challenges. |
| Seek out hobbies and activities that bring you joy and provide a sense of purpose. |
| Reach out for assistance when needed, whether it's physical support, financial aid, or emotional guidance. |
| Stay connected with loved ones through regular communication and social interactions. |
Remember, your emotional well-being is just as important as your physical well-being. By implementing coping strategies and building a strong support system, you can find moments of joy, peace, and fulfillment in your life, even in the face of end stage cerebellar ataxia.
Conclusion
End stage cerebellar ataxia has a significant impact on individuals' daily lives, affecting their mobility, communication, and overall well-being. However, there is hope and ways to cope with the challenges it presents. With a comprehensive understanding of the condition and access to appropriate medical care, individuals with end stage cerebellar ataxia can effectively manage their symptoms and maintain a better quality of life.
Prioritizing both physical and emotional well-being is crucial when dealing with end stage cerebellar ataxia. Physical therapy and adaptive devices can help improve coordination and mobility, allowing individuals to maintain independence for as long as possible. It is equally important to address the emotional aspect, seeking support from family, friends, and healthcare professionals. Support groups, counseling, and education about the condition can provide valuable resources and assistance.
Despite the challenges, those facing end stage cerebellar ataxia can find ways to adapt and overcome. By staying proactive, seeking help when needed, and remaining positive, individuals with ataxia can embrace coping strategies that enhance their overall well-being. With the right support systems in place, individuals and their families can navigate this journey together, finding strength and resilience along the way.
FAQ
What is end stage cerebellar ataxia?
End stage cerebellar ataxia refers to the advanced stage of the neurological disorder characterized by poor muscle control and coordination due to damage to the cerebellum or its connections. It is the final and most severe stage of cerebellar ataxia.
What are the symptoms of cerebellar ataxia?
The symptoms of cerebellar ataxia include poor coordination, unsteady walking, balance problems, speech difficulties, and abnormalities in eye movement. Individuals may also experience tremors, poor handwriting, clumsiness, and problems with fine motor skills.
What causes cerebellar ataxia?
Cerebellar ataxia can have various causes, including acquired factors such as alcohol misuse, medication side effects, toxins, and nutritional deficiencies. It can also be hereditary, with dominant or recessive genetic mutations being responsible. In some cases, the cause is unknown.
How is cerebellar ataxia diagnosed?
Diagnosing cerebellar ataxia involves a comprehensive approach, including a detailed medical history, neurological examination, and the use of clinical rating scales. Neuroimaging, such as brain MRI, is recommended to identify specific lesions, and genetic testing may be necessary to confirm or rule out hereditary ataxias.
Is there a cure for cerebellar ataxia?
Currently, there is no cure for most forms of cerebellar ataxia. However, management strategies can help alleviate symptoms and improve quality of life. These may include physical therapy, occupational therapy, speech therapy, and the use of adaptive devices like walkers and canes.
How can individuals cope with end stage cerebellar ataxia?
Coping with end stage cerebellar ataxia can be physically and emotionally challenging. It is important to have a strong support system, including family, friends, and healthcare professionals. Support groups, counseling, and education about the condition can be beneficial. Strategies such as mindfulness, stress management, and maintaining a positive outlook can also improve quality of life.
Understanding Adult Ataxia Symptoms
If you or a loved one are experiencing difficulty walking, balance problems, or changes in speech, you may be dealing with adult ataxia. Ataxia is a condition that affects muscle control and coordination, leading to various neurological challenges. It can significantly impact your daily life and overall health management.
Early recognition and understanding of ataxia symptoms in adults are crucial for prompt medical intervention and appropriate care. This article will provide insights into the common signs and symptoms of ataxia, its underlying causes, and the importance of seeking medical attention. We will also explore the diagnosis, evaluation, treatment, and management strategies that can help improve your quality of life.
Whether you are personally affected by ataxia or seeking information for a loved one, this article will provide valuable insights into managing the challenges posed by this condition. By understanding the symptoms and exploring effective management strategies, you can take proactive steps towards maintaining your neurological health and overall well-being.
Causes of Ataxia
Ataxia primarily occurs due to damage to the cerebellum or its connections in the brain. The causes of ataxia can be categorized into three major groups: acquired, degenerative, and hereditary.
Acquired causes:
- Long-term excess alcohol use
- Certain medications (such as sedatives and anti-seizure drugs)
- Heavy metal poisoning
- Vitamin deficiencies
- Thyroid conditions
- Stroke
- Multiple sclerosis
- Autoimmune diseases
- Infections (such as chickenpox and COVID-19)
- Paraneoplastic syndromes triggered by cancerous tumors
- Changes in the brain (abscess or tumor)
- Head trauma
- Cerebral palsy
Degenerative causes:
- Multiple system atrophy
Hereditary causes:
Hereditary ataxia results from genetic conditions that are passed down in families. Various gene changes can cause different types of ataxia, and most types tend to worsen over time.
Symptoms of Ataxia
Ataxia symptoms can vary depending on the individual and the underlying cause, but they generally involve poor coordination and motor control. Common symptoms of ataxia include:
- Difficulties with balance
- Unsteady or wide-based walking
- Poor coordination of hand movements
- Slurred speech
- Uncontrollable eye movements
- Trouble swallowing
These symptoms can impact daily activities, such as eating, writing, and buttoning a shirt.
It is important to note that the symptoms of ataxia may resemble those of other conditions, so it is crucial to consult a healthcare professional for a proper diagnosis.
| Symptom | Description |
|---|---|
| Poor coordination | Difficulty in controlling movements |
| Balance problems | Unsteadiness while standing or walking |
| Changes in speech | Slurred or slow speech patterns |
When to Seek Medical Attention
If you experience symptoms such as loss of balance, muscle coordination issues in the hands, arms, or legs, difficulty walking, slurred speech, or trouble swallowing, it is important to see a healthcare professional for a proper evaluation. Seeking early medical attention is crucial to determine the cause of your symptoms and develop an appropriate treatment plan. Prompt intervention can significantly impact the progression and management of ataxia, improving your quality of life.
Common symptoms of ataxia include:
- Loss of balance
- Muscle coordination issues in the hands, arms, or legs
- Difficulty walking
- Slurred speech
- Trouble swallowing
If you experience any of these symptoms without a pre-existing condition that causes ataxia, it is recommended to consult with a doctor. They will conduct a thorough assessment and may refer you to a specialist, such as a neurologist, for further evaluation.
Ataxia can be caused by various factors, including genetic conditions, acquired causes, or other underlying health issues. Identifying the underlying cause is vital to determine the most appropriate management strategies and provide necessary support.
Remember, early medical intervention is key to effectively managing ataxia. Don't hesitate to make an appointment with a healthcare professional if you experience any concerning symptoms.
Diagnosis and Evaluation of Ataxia
The diagnosis of ataxia involves a thorough evaluation of your medical history, family history, and a comprehensive neurological and physical examination. Your healthcare professional will gather information about your symptoms, their progression, and any potential triggers or underlying conditions. This medical history assessment provides valuable insights into the possible causes of ataxia.

Following the medical history review, a neurological examination will be conducted to assess your coordination, muscle strength, reflexes, and sensory function. This examination helps identify specific neurological abnormalities associated with ataxia and determine the areas of your brain or nervous system that may be affected.
In addition to the examination, your healthcare professional may order diagnostic tests to aid in the diagnosis of ataxia. These tests can help rule out other conditions that may cause similar symptoms or identify potential underlying causes. Some common diagnostic tests include:
- Blood and urine studies: These tests can provide information about your overall health, check for specific genetic markers or infections, and assess for any metabolic or hormonal imbalances that may contribute to your symptoms.
- Genetic testing: Genetic tests can help identify specific gene mutations associated with hereditary ataxias. They can also assist in determining if you have a genetic predisposition to develop ataxia.
- Brain imaging scans: Magnetic resonance imaging (MRI) scans may be performed to visualize your brain and identify any structural abnormalities, such as cerebellar atrophy or lesions, which may be causing your ataxia symptoms.
| Diagnostic Tests for Ataxia | Purpose |
|---|---|
| Blood and urine studies | To assess overall health, check for genetic markers, infections, and metabolic imbalances. |
| Genetic testing | To identify specific gene mutations associated with hereditary ataxias or genetic predisposition. |
| Brain imaging scans (MRI) | To visualize the brain and identify structural abnormalities, such as cerebellar atrophy or lesions. |
The combination of the medical history, neurological examination, and diagnostic tests plays a crucial role in accurately diagnosing ataxia. These evaluations help healthcare professionals understand the underlying cause of your symptoms and determine the most appropriate treatment and management strategies for your specific condition.
Treatment and Management of Ataxia
The treatment and management of ataxia depend on the underlying cause, as there is currently no cure for hereditary ataxias. However, various strategies can help manage the symptoms and improve the quality of life for individuals with ataxia.
Adaptive devices such as walkers or canes can assist with mobility and provide support for individuals with balance difficulties.
Physical therapy plays a crucial role in improving muscle strength and coordination. It involves exercises and techniques that aim to enhance motor control and minimize the impact of ataxia on daily activities.
Speech therapy is essential for addressing speech and swallowing difficulties that may arise from ataxia. Therapists work with individuals to improve speech clarity, swallowing function, and overall communication skills.
- Adaptive devices like walkers or canes
- Physical therapy to improve muscle strength and coordination
- Speech therapy to address speech and swallowing difficulties
- Regular exercise to maintain overall health
Additionally, regular exercise is essential for individuals with ataxia, as it aids in maintaining overall health and well-being. Engaging in physical activities that are suitable for each individual's capabilities can promote strength, balance, and coordination.
In certain cases, medications may be prescribed to alleviate specific symptoms associated with ataxia, such as tremors or stiffness. However, these medications are typically symptom-specific and may vary depending on individual needs. It's important to consult with healthcare professionals for proper evaluation and medication management.
Overall, a personalized treatment plan that incorporates adaptive devices, physical therapy, speech therapy, regular exercise, and potentially medication can help individuals with ataxia manage their symptoms effectively and maintain an active and fulfilling lifestyle.
Complications of Ataxia
Ataxia can lead to various complications, particularly if not properly managed or treated. It's important to be aware of these complications and take appropriate measures to reduce their impact on your daily life. Some common complications of ataxia include:
- Falls and injuries: Impaired balance and coordination can increase the risk of falls, which can result in fractures, head injuries, or other serious injuries. It's important to take precautions to prevent falls, such as using assistive devices and making your home environment safer.
- Respiratory difficulties: Ataxia can affect the muscles involved in breathing, leading to respiratory issues. This can include shortness of breath, difficulty in clearing secretions, or even respiratory failure in severe cases. If you experience any respiratory symptoms, it's crucial to seek medical attention promptly.
- Pressure sores: Prolonged immobility and difficulty in changing positions can increase the risk of developing pressure sores, also known as bedsores. These are areas of damaged skin and underlying tissue caused by constant pressure. Proper positioning, regular movement, and good skincare can help prevent pressure sores.
- Infections: Immobility and respiratory difficulties can also increase the risk of infections, such as pneumonia or urinary tract infections. It's important to practice good hygiene and maintain a healthy lifestyle to minimize the risk of infections.
- Blood clots: Reduced mobility and muscle function can increase the risk of blood clots, especially deep vein thrombosis (DVT). Blood clots can be life-threatening if they travel to vital organs, such as the lungs (pulmonary embolism). Staying active, maintaining good circulation, and following your healthcare professional's advice can help prevent blood clots.
- Cognitive or behavioral changes: In some cases, ataxia can result in cognitive or behavioral changes, such as difficulties with memory, concentration, or mood disturbances. These changes can significantly impact your daily life and overall well-being. Seeking appropriate support and care from healthcare professionals can help manage these challenges.
It's important to remember that everyone's experience with ataxia is unique, and the complications may vary. Regular medical follow-ups and adherence to management strategies are essential in reducing the risk of these complications and maintaining optimal health. By actively addressing these complications and working closely with your healthcare team, you can enhance your quality of life and minimize the impact of ataxia on your day-to-day activities.

Variability in Ataxia Progression
The progression of ataxia can vary significantly depending on the underlying cause. Understanding the different patterns of progression is crucial in accurately diagnosing and managing this condition.
Acute Onset
Ataxia can have an acute onset, meaning it occurs suddenly and progresses rapidly. Acute onset ataxia can be triggered by factors such as stroke, infectious or parainfectious cerebellitis, or acute toxin exposure. In these cases, individuals may experience a sudden onset of symptoms and notice a rapid decline in their motor function.
Rapid Progression
In some cases, ataxia may progress rapidly over a short period of time, typically spanning hours to days. This type of progression can be associated with certain immune-mediated disorders or metabolic derangements. The rapid decline in motor control and coordination can significantly impact an individual's daily life.
Chronic Progression
On the other hand, ataxia can exhibit a chronic and indolent progression over a longer duration, ranging from months to years. This type of progression is commonly observed in genetic ataxias, sporadic neurodegenerative disorders like multiple system atrophy, or idiopathic late-onset cerebellar ataxia. The symptoms gradually worsen over time, affecting motor function and overall quality of life.
Having an understanding of the rate and tempo of progression is essential in guiding the diagnosis and management of ataxia. It allows healthcare professionals to develop a personalized treatment plan tailored to the individual's specific needs and prognosis.
| Progression Type | Characteristics | Underlying Causes |
|---|---|---|
| Acute Onset | Sudden and rapid progression | Stroke, infectious or parainfectious cerebellitis, acute toxin exposure |
| Rapid Progression | Fast decline over hours to days | Immune-mediated disorders, metabolic derangements |
| Chronic Progression | Slow and gradual worsening over months to years | Genetic ataxias, sporadic neurodegenerative disorders, idiopathic late-onset cerebellar ataxia |
Evaluation and Diagnostic Tests for Ataxia
The evaluation of ataxia involves a combination of clinical assessment and diagnostic tests. Alongside a thorough history and physical examination, healthcare professionals may order brain magnetic resonance imaging (MRI) to assess for structural lesions and atrophy in the cerebellum and brainstem. Serum tests, including blood chemistries, genetic testing, and specific lab markers, may help identify underlying causes or rule out other conditions. Cerebrospinal fluid studies can provide valuable information in cases of paraneoplastic, immune-mediated, infectious, or inflammatory disorders affecting the nervous system. Additional testing, such as CT scans or PET scans to investigate occult malignancy, may be recommended based on the individual presentation.
Evaluation and Diagnostic Tests for Ataxia
To diagnose ataxia, healthcare professionals employ various evaluation and diagnostic tests to gather comprehensive information. These tests aid in identifying potential underlying causes, ruling out other conditions, and assessing the extent of damage in the brain.
The evaluation process begins with a thorough clinical assessment, including a detailed medical history and physical examination. This provides important insights into the onset, progression, and severity of symptoms.
Brain Magnetic Resonance Imaging (MRI): MRI scans are commonly used to assess the structural integrity of the cerebellum and brainstem. By detecting any lesions, atrophy, or abnormalities in these regions, MRI helps in diagnosing ataxia and identifying the specific areas of neurological damage.
| Diagnostic Tests | Purpose |
|---|---|
| Serum Testing | Includes blood chemistries, genetic testing, and specific lab markers to identify underlying causes or rule out other conditions. |
| Cerebrospinal Fluid Studies | Used to examine cerebrospinal fluid for signs of paraneoplastic, immune-mediated, infectious, or inflammatory disorders affecting the nervous system. |
| Additional Testing | In certain cases, CT scans or PET scans may be recommended to investigate the presence of hidden malignancies that may be contributing to ataxia. |
These diagnostic tests play a crucial role in confirming the diagnosis of ataxia and determining its underlying cause. They provide valuable information that helps healthcare professionals develop an effective treatment plan and identify any relevant associated conditions or complications.

By utilizing a combination of evaluation techniques and diagnostic tests, medical professionals can accurately diagnose ataxia and provide appropriate treatment and management strategies tailored to each individual's specific needs.
Genetic Ataxias
A significant subset of ataxias is attributed to genetic factors. Genetic ataxias occur due to inherited defects in specific genes. These can be passed down through families in various inheritance patterns, including autosomal dominant (AD), autosomal recessive (AR), or X-linked. Depending on the specific mutation, genetic ataxias can manifest in different forms and have varying rates of progression.
Spinocerebellar ataxias (SCAs) are the most common autosomal dominant genetic ataxias, while Friedreich ataxia and ataxia-telangiectasia are examples of autosomal recessive genetic ataxias. Genetic testing can aid in confirming a diagnosis and provide insights into prognosis and potential treatment options.
Management and Prognosis of Ataxia
While there is no cure for many forms of ataxia, effective management strategies can greatly improve symptoms and enhance overall quality of life. The primary goal of managing ataxia is to optimize functional abilities and maintain independence. A multidisciplinary approach is often employed, involving various healthcare professionals who specialize in different aspects of rehabilitation.
One key aspect of managing ataxia is physical therapy, which focuses on improving muscle strength, coordination, and balance. Physical therapists design personalized exercise programs that target specific areas of weakness and work towards enhancing mobility. Occupational therapy is also beneficial, as it focuses on improving fine motor skills and helping individuals adapt to their daily activities.
Speech therapy plays a crucial role in managing ataxia-related speech and swallowing difficulties. Speech therapists help individuals improve their articulation, voice control, and swallowing function through targeted exercises and techniques.
In addition to therapy, the use of adaptive devices can significantly enhance mobility and independence for individuals with ataxia. Walkers, canes, and assistive devices for daily activities, such as buttoning shirts or eating utensils, can make a substantial difference in daily life.
A comprehensive management plan for ataxia requires regular follow-up appointments to monitor the progression of the condition and make necessary adjustments to the treatment strategies. It is essential to work closely with healthcare professionals to ensure that the management plan remains effective and aligned with the individual's evolving needs.
The prognosis and outcomes of ataxia can vary depending on the underlying cause. Some forms of ataxia progress slowly over many years, allowing individuals to maintain a relatively high level of functional ability. However, other forms may lead to more rapid functional decline and greater disability.
It is important to note that while the progression of ataxia cannot be halted, supportive care can greatly improve the overall quality of life. Regular monitoring, comprehensive symptom management, and emotional support are essential components of long-term management.
Treatment strategies for ataxia
| Treatment | Description |
|---|---|
| Physical Therapy | Focuses on improving muscle strength, coordination, and balance through tailored exercise programs. |
| Occupational Therapy | Helps individuals adapt to daily activities and improve fine motor skills. |
| Speech Therapy | Aims to improve speech articulation, voice control, and swallowing function. |
| Use of Adaptive Devices | Assistive devices such as walkers, canes, and adaptive tools for daily tasks can enhance mobility and independence. |
Although ataxia can present challenges, with proper management and support, individuals can live fulfilling lives and maintain their independence for as long as possible.
Conclusion
Understanding the symptoms of ataxia is essential for effective management and improving the quality of life for individuals facing this condition. Ataxia can manifest differently based on various underlying causes, which can include genetic conditions, acquired factors, and degenerative disorders. Early recognition and intervention are crucial in providing timely support and maximizing overall well-being.
While there is currently no cure for ataxia, there are strategies available to help alleviate symptoms and enhance independence. Physical therapy and the use of adaptive devices can assist in improving muscle control and mobility. Additionally, a comprehensive evaluation, accurate diagnosis, and personalized treatment plan are fundamental in managing ataxia effectively.
Regular follow-up appointments and consistent communication with healthcare professionals are vital for ongoing support and monitoring the progression of the condition. By establishing a collaborative relationship with your healthcare team, you can navigate the challenges of ataxia more confidently and optimize your well-being.
FAQ
What is ataxia?
Ataxia is a condition characterized by poor muscle control that affects various aspects of daily life, such as walking, balance, hand coordination, speech, and swallowing.
What are the causes of ataxia?
Ataxia can be caused by a variety of factors, including genetic conditions, stroke, tumors, multiple sclerosis, degenerative diseases, alcohol misuse, certain medicines, and even COVID-19.
What are the symptoms of ataxia?
Symptoms of ataxia can include poor coordination, unsteady walking, balance problems, difficulty with fine motor tasks, changes in speech, uncontrollable eye movements, and trouble swallowing.
When should I seek medical attention for ataxia?
If you experience symptoms such as loss of balance, muscle coordination problems in the hands, arms, or legs, difficulty walking, slurred speech, or trouble swallowing, it is important to see a healthcare professional as soon as possible.
How is ataxia diagnosed and evaluated?
The diagnosis of ataxia involves a thorough medical history, family history, and a comprehensive neurological and physical examination. Diagnostic tests, such as blood and urine studies, genetic testing, and brain imaging scans, may also be ordered.
What treatments are available for ataxia?
The treatment and management of ataxia depend on the underlying cause and may include the use of adaptive devices, physical therapy, speech therapy, and medications to alleviate specific symptoms.
What are the complications of ataxia?
Complications of ataxia can include falls and injuries, respiratory difficulties, pressure sores, infections, blood clots, and cognitive or behavioral changes.
How does ataxia progress?
The progression of ataxia can vary depending on the underlying cause, with some types progressing rapidly and others progressing slowly over time.
What evaluation and diagnostic tests are used for ataxia?
The evaluation of ataxia involves a combination of clinical assessment and diagnostic tests, such as brain imaging scans, serum tests, and cerebrospinal fluid studies.
What are genetic ataxias?
Genetic ataxias occur due to inherited defects in specific genes and can be passed down through families in various inheritance patterns.
How is ataxia managed, and what is the prognosis?
While there is no cure for many forms of ataxia, management strategies can help improve symptoms and overall quality of life. Prognosis and outcomes can vary depending on the underlying cause of ataxia.
Friedreich's Ataxia Symptoms – Know the Signs
If you or someone you know has been experiencing unsteadiness, difficulty walking, and other motor impairments, it's crucial to be aware of the potential signs of Friedreich's ataxia. This genetic disorder, also known as FRDA, is a progressive neurodegenerative condition that typically develops during adolescence.
Friedreich's ataxia symptoms may manifest as an unsteady posture, frequent falling, and progressive difficulty in walking due to impaired coordination of voluntary movements. Other common symptoms include slurred speech, foot deformities, an irregular curvature of the spine, and the presence of cardiomyopathy and diabetes in some cases.
Monitoring your health and recognizing the early signs of Friedreich's ataxia can lead to timely intervention and improved management of the condition. Understanding the symptoms is crucial for individuals who may be at risk or have a family history of this genetic disorder.
Primary Symptoms of Friedreich's Ataxia
Friedreich's ataxia is characterized by several primary symptoms that affect motor function and coordination. These symptoms progressively worsen over time and can significantly impact an individual's quality of life.
The main symptom of Friedreich's ataxia is progressive ataxia, which refers to the loss of muscle coordination. This primarily affects the limbs, especially during walking. People with Friedreich's ataxia experience an unsteady gait and have difficulty maintaining balance. The impairment in muscle coordination also leads to poor control of fine movements in the limbs, making tasks such as writing or handling objects challenging.
Another symptom commonly associated with Friedreich's ataxia is impaired swallowing. This can result in difficulties in eating and drinking, requiring careful monitoring and modifications to the diet. Additionally, individuals may develop slurred speech (dysarthria) as the disease progresses, affecting their ability to communicate clearly.
Loss of reflexes is also observed in individuals with Friedreich's ataxia. This means that certain automatic responses that normally occur in response to stimuli, such as the knee-jerk reflex, may be absent or reduced. Though this symptom can vary among individuals, it is essential to note that intellect is usually unaffected in individuals with Friedreich's ataxia, as it primarily affects physical coordination and motor function.

Atypical Presentations of Friedreich's Ataxia
If you think Friedreich's ataxia only affects individuals in their teenage years, think again. While most people are diagnosed before the age of 25, there are instances where the disease presents later in life. Late-onset Friedreich's ataxia (LOFA) and very late-onset Friedreich's ataxia (VLOFA) are two atypical forms of the condition that affect approximately 15% of individuals with Friedreich's ataxia.
LOFA is characterized by an age of onset between 26 and 39 years, while VLOFA typically presents after the age of 40 years. Compared to typical Friedreich's ataxia cases, individuals with LOFA and VLOFA experience a slower disease progression.
Understanding Late-onset Friedreich's Ataxia (LOFA)
LOFA is a form of Friedreich's ataxia that manifests between the ages of 26 and 39. Despite the later onset, individuals with LOFA still experience similar symptoms to those with the typical form of the condition. However, the progression of the disease tends to be slower, allowing individuals to retain certain motor functions for a longer period of time.
Exploring Very Late-onset Friedreich's Ataxia (VLOFA)
VLOFA is a rare variant of Friedreich's ataxia that occurs after the age of 40. Individuals with VLOFA may experience milder symptoms compared to those with typical Friedreich's ataxia. Similar to LOFA, the disease progression in VLOFA is slower, giving individuals more time before significant motor impairments occur.
While late-onset and very late-onset Friedreich's ataxia are rare, it is important to be aware of their existence. If you or a loved one are experiencing symptoms of Friedreich's ataxia later in life, consult a healthcare professional for proper evaluation and diagnosis.
Causes of Friedreich's Ataxia
Friedreich's ataxia is a genetic condition that is caused by pathogenic variants in the FXN gene. The FXN gene plays a crucial role in the production of frataxin, a protein that is necessary for proper mitochondrial functioning. In individuals with Friedreich's ataxia, both copies of the FXN gene are abnormal, leading to a reduced production of frataxin.
This deficiency in frataxin production has a detrimental effect on various tissues, particularly on nerve and heart cells. The lack of frataxin causes degeneration in these cells, contributing to the development of symptoms associated with Friedreich's ataxia.
The majority of individuals with Friedreich's ataxia have an expanded GAA trinucleotide repeat in both copies of the FXN gene. This expansion leads to gene silencing and a significant reduction in frataxin production.
Friedreich's Ataxia Genetics
Friedreich's ataxia follows an autosomal recessive pattern of inheritance, which means that an individual must inherit two copies of the abnormal FXN gene, one from each parent, to develop the condition. If only one copy of the FXN gene is abnormal, the individual is considered a carrier and does not typically experience symptoms.
| Genotype | Phenotype |
|---|---|
| Normal FXN gene | No symptoms, not a carrier |
| One normal FXN gene and one abnormal FXN gene | Carrier, no symptoms |
| Two abnormal FXN genes | Develops Friedreich's ataxia |
It is important to note that the severity of Friedreich's ataxia symptoms can vary among individuals, even those who carry the same genetic mutations. Other genetic and environmental factors may contribute to this variability, and ongoing research aims to better understand these influences.
Understanding the underlying genetic cause of Friedreich's ataxia is key to developing targeted therapies and interventions. Research efforts continue to focus on unraveling the complex mechanisms of this genetic condition, with the aim of improving the quality of life for individuals affected by Friedreich's ataxia.
Affected Populations of Friedreich's Ataxia
Friedreich's ataxia is a relatively rare disorder, affecting approximately 1 in 40,000 people. While it may be considered a rare condition, it can have a significant impact on the lives of those affected. Friedreich's ataxia is most commonly observed in populations of European, Middle Eastern, South Asian (Indian subcontinent), and North African descent, although it can occur in other populations as well.
Prevalence of Friedreich's Ataxia
To better understand the prevalence of Friedreich's ataxia, let's take a closer look at various regions:
| Region | Prevalence |
|---|---|
| Europe | Higher prevalence compared to other regions |
| Middle East | Significant presence in the population |
| South Asia (Indian subcontinent) | Relatively common occurrence |
| North Africa | Notable prevalence in the population |
These regions have a higher incidence of Friedreich's ataxia due to genetic factors and shared ancestry. However, it is important to note that the disorder can still occur in individuals from other backgrounds.
Diagnosis of Friedreich's Ataxia
The diagnosis of Friedreich's ataxia involves a comprehensive evaluation that encompasses medical history, physical examination, and genetic testing. By considering these factors together, healthcare providers can accurately diagnose the condition and formulate an appropriate treatment plan.
Medical History
When assessing a patient suspected of having Friedreich's ataxia, the healthcare provider will obtain a detailed medical history. This includes collecting information about the patient's symptoms, their progression over time, and any associated medical conditions or family history of the disease. A thorough understanding of the patient's medical background helps to provide valuable insights into the diagnosis process.
Physical Examination
During the physical examination, the healthcare provider will carefully assess various aspects of the patient's neurological function. This may involve evaluating reflexes, balance, muscle strength, and coordination. Additionally, the provider may perform tests to assess sensory function, such as nerve sensation. By conducting a comprehensive physical examination, the healthcare provider can gather essential clinical information that can aid in the diagnosis of Friedreich's ataxia.
Genetic Testing
Genetic testing is a crucial component of the diagnostic process for Friedreich's ataxia. It involves analyzing the patient's DNA to identify any pathogenic variants in the FXN gene, which is associated with this condition. By detecting the presence of these variants, genetic testing confirms the diagnosis of Friedreich's ataxia. It also helps to distinguish the condition from other disorders that may present with similar symptoms.
Additional Diagnostic Tests
In some cases, healthcare providers may utilize additional diagnostic tests to further support the diagnosis of Friedreich's ataxia. These tests may include blood tests to assess specific biomarkers, imaging scans such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to evaluate the structure of the brain, nerve conduction studies to assess nerve function, and heart tests to evaluate any associated cardiac abnormalities.

Genetic testing is crucial for identifying the pathogenic variants in the FXN gene and confirming the diagnosis of Friedreich's ataxia.
Treatment of Friedreich's Ataxia
While there is no cure for Friedreich's ataxia, there are several treatment options available to help manage symptoms and improve quality of life. A multidisciplinary approach that involves continuous medical supervision is recommended to address the complex nature of this condition and its impact on various organ systems.
One of the key components of treatment for Friedreich's ataxia is symptomatic management. This involves addressing specific symptoms and providing supportive care. Some common symptomatic treatments include:
- Braces: Braces and assistive devices can help improve mobility, stability, and reduce the risk of falls.
- Physical therapy: Physical therapy exercises and interventions can help improve coordination, strength, and flexibility.
- Speech therapy: Speech therapy can assist individuals with Friedreich's ataxia in improving their speech and swallowing abilities.
- Orthopedic surgery: In more severe cases, orthopedic surgery may be necessary to correct foot deformities or address scoliosis.
In recent years, there has been an exciting development in the treatment of Friedreich's ataxia. In 2023, the FDA approved omaveloxolone, a drug specifically designed to treat this condition. Omaveloxolone has shown promising results in reducing disease progression and improving certain symptoms associated with Friedreich's ataxia.
Living with Friedreich's Ataxia
Friedreich's ataxia is a progressive disorder, and the rate of disease progression can vary among individuals. As the disease advances, it can give rise to several complications that significantly impact daily life. It is important for individuals living with Friedreich's ataxia to understand and address these challenges effectively, promoting their overall well-being.
One of the common complications is scoliosis, which leads to an abnormal curvature of the spine. This can cause discomfort, pain, and difficulty maintaining proper posture. Regular monitoring and interventions such as bracing or corrective surgery may be necessary to manage scoliosis and maintain spinal alignment.
Another area of concern is heart problems, specifically cardiomyopathy, which affects the heart muscle and can lead to heart failure. Close monitoring of heart function and regular visits to a cardiologist are essential for individuals with Friedreich's ataxia. Medications, lifestyle modifications, and other interventions may be recommended to manage and treat cardiomyopathy.
Foot deformities, including pes cavus (high arches) and hammer toes, are also common in Friedreich's ataxia. These deformities can lead to difficulties with walking and balance. Orthopedic interventions such as orthotics or corrective surgeries may be necessary to alleviate discomfort and improve mobility.
As Friedreich's ataxia progresses, individuals may experience challenges in mobility. Many individuals with advanced stages of the condition rely on mobility aids such as wheelchairs or walkers to maintain independence and move around safely. These aids can help improve mobility, reduce falls, and enhance overall quality of life.
In addition to physical complications, Friedreich's ataxia may also impact speech, hearing, and vision. Speech therapy, hearing aids, and other assistive devices may be recommended to address communication and sensory impairments.
Living with Friedreich's ataxia requires regular follow-up with healthcare providers, including neurologists, orthopedic specialists, cardiologists, and other relevant specialists. It is important to follow their recommendations, seek appropriate interventions, and actively participate in managing the disease to optimize overall health and well-being.
Common Complications of Friedreich's Ataxia
| Complication | Description |
|---|---|
| Scoliosis | An abnormal curvature of the spine, leading to postural problems and discomfort. |
| Cardiomyopathy | A condition characterized by weakened heart muscle, increasing the risk of heart failure. |
| Foot Deformities | Abnormalities in foot structure, such as high arches or hammer toes, affecting walking and balance. |
| Mobility Challenges | Difficulties with walking and physical movement, often necessitating the use of mobility aids. |
| Communication and Sensory Impairments | Speech, hearing, and visual difficulties that may require interventions and assistive devices. |
Clinical Trials and Research
The Friedreich's Ataxia Research Alliance (FARA) is dedicated to advancing knowledge and finding new treatments for Friedreich's ataxia. FARA provides valuable information on ongoing clinical trials and current therapies in development for Friedreich's ataxia.
Clinical trials and research studies are vital in expanding our understanding of the disease and exploring potential treatment options. By participating in clinical trials, individuals with Friedreich's ataxia can contribute to the development of new therapies and help shape the future of Friedreich's ataxia research.
To stay informed about the latest research advancements and ongoing clinical trials, you can visit the following websites:
- ClinicalTrials.gov
- NIH Clinical Center
- ClinicalTrialsRegister.eu
Participating in clinical trials not only provides a potential opportunity for accessing innovative treatments but also plays a crucial role in advancing the understanding and management of Friedreich's ataxia.
Current Clinical Trials for Friedreich's Ataxia
Below is a table summarizing some of the ongoing clinical trials for Friedreich's ataxia:
| Trial Name | Phase | Intervention | Study Design | Location |
|---|---|---|---|---|
| Trial 1 | Phase 2 | Drug A | Randomized, Double-blind | United States |
| Trial 2 | Phase 3 | Drug B | Open-label | Europe |
| Trial 3 | Phase 1 | Gene Therapy | Single-arm | Canada |
These trials are designed to evaluate the safety and efficacy of different interventions in individuals with Friedreich's ataxia. If you are interested in participating in a clinical trial, consult with your healthcare provider and visit the respective trial websites for more information.
Conclusion
Friedreich's ataxia is a genetic disorder that affects the coordination and movement of the limbs. It is characterized by symptoms such as ataxia, impaired coordination, and sensory loss. While there is currently no cure for Friedreich's ataxia, treatment focuses on managing symptoms and improving quality of life.
The primary goal of treatment is to alleviate symptoms, such as difficulties in walking and speaking, through a multidisciplinary approach. Physical therapy, speech therapy, and the use of mobility aids can help individuals with Friedreich's ataxia maintain their independence and functionality.
Ongoing research and clinical trials provide hope for the future of Friedreich's ataxia treatment. By participating in research studies and clinical trials, individuals with Friedreich's ataxia can contribute to the advancement of knowledge and the development of new therapies. It is important to stay informed about the latest research and work closely with healthcare providers to explore all available options.
In conclusion, while living with Friedreich's ataxia can be challenging, ongoing research and treatment advancements offer hope for a better future. By staying informed, seeking appropriate treatment, and contributing to research efforts, individuals with Friedreich's ataxia can actively participate in their own care and contribute to the overall understanding and treatment of the condition.
FAQ
What are the primary symptoms of Friedreich's Ataxia?
The primary symptoms of Friedreich's Ataxia include progressive ataxia of the limbs during walking, impaired muscle coordination, an unsteady gait, and impaired swallowing.
Are there atypical presentations of Friedreich's Ataxia?
Yes, there are atypical presentations of Friedreich's Ataxia known as Late-onset Friedreich's Ataxia (LOFA) and very late-onset Friedreich's Ataxia (VLOFA). LOFA presents between the ages of 26 and 39 years, while VLOFA presents after the age of 40. The disease progression tends to be slower in these cases compared to typical Friedreich's Ataxia.
What causes Friedreich's Ataxia?
Friedreich's Ataxia is caused by abnormalities in the FXN gene, which leads to reduced production of the frataxin protein. This gene abnormality is typically inherited from both parents, leading to autosomal recessive inheritance.
Who is affected by Friedreich's Ataxia?
Friedreich's Ataxia is a relatively rare disorder with a prevalence of approximately 1 in 40,000 people. It is most commonly observed in populations of European, Middle Eastern, South Asian (Indian subcontinent), and North African descent.
How is Friedreich's Ataxia diagnosed?
The diagnosis of Friedreich's Ataxia is typically based on a combination of medical history, physical examination, and genetic testing. Healthcare providers may assess reflexes, balance, and nerve sensation during the physical examination. Genetic testing is essential for confirming the diagnosis by identifying pathogenic variants in the FXN gene.
Is there a cure for Friedreich's Ataxia?
Currently, there is no cure for Friedreich's Ataxia. However, treatment aims to manage symptoms and maintain quality of life. This may involve a multidisciplinary approach that includes symptomatic treatments and continuous medical supervision. In 2023, the FDA approved omaveloxolone as a therapy for Friedreich's Ataxia, which has shown to reduce disease progression.
How does Friedreich's Ataxia progress?
Friedreich's Ataxia is a progressive disorder, and the rate of disease progression can vary among individuals. As the disease progresses, it can lead to complications such as scoliosis, foot deformities, heart problems (such as cardiomyopathy), and mobility challenges. Many individuals with Friedreich's Ataxia eventually require the use of a wheelchair to maintain mobility.
Are there clinical trials and research studies for Friedreich's Ataxia?
Yes, there are ongoing clinical trials and research studies for Friedreich's Ataxia. The Friedreich's Ataxia Research Alliance (FARA) provides up-to-date information on current therapies in development and ongoing clinical trials. Individuals with Friedreich's Ataxia can stay informed about research advancements and consider participating in clinical trials to contribute to the development of new treatments.
Friedreich's Ataxia Prognosis Insights and Facts
If you or someone you know has been diagnosed with Friedreich's ataxia, understanding the prognosis and outlook of this genetic condition is crucial. Friedreich's ataxia is a progressive disease that affects the nervous system, leading to mobility impairments and other physical challenges. In this article, we will explore the key insights and facts about Friedreich's ataxia prognosis, shedding light on what to expect and how to navigate this condition.
Etiology of Friedreich Ataxia
Friedreich ataxia, a progressive genetic condition, is primarily caused by a loss of function mutation in the frataxin gene. Specifically, the mutation occurs in the centromeric region of chromosome 9q. The frataxin gene plays a crucial role in regulating iron homeostasis and ATP production within mitochondria.
This inherited disease is associated with an expansion of the GAA trinucleotide repeat in the gene's first intron. This repetitive expansion leads to reduced transcription of the frataxin gene and a consequent decrease in frataxin production.
Frataxin Gene Mutation and Friedreich Ataxia
The frataxin gene mutation hinders the production of frataxin, an essential protein involved in mitochondrial function. A deficiency in frataxin disrupts the regulation of iron levels and impairs ATP production, which are critical for the normal functioning of cells, particularly in neurons and cardiomyocytes.
The progressive nature of Friedreich ataxia can be attributed to the harmful effects of frataxin deficiency on cellular health and viability. The accumulation of iron within mitochondria leads to increased production of free radicals, causing oxidative stress and ultimately resulting in cell death.
Further research into the underlying mechanisms of the frataxin gene mutation and GAA trinucleotide repeat expansion may provide valuable insights for potential therapeutic interventions.
| Etiology of Friedreich Ataxia | |
|---|---|
| Genetic Mutation | Loss of function mutation in the frataxin gene |
| Location of Mutation | Centromeric region of chromosome 9q |
| Effect on Frataxin Gene | Expansion of GAA trinucleotide repeat in the gene's first intron, leading to reduced transcription and frataxin production |
| Consequences | Disruption of iron homeostasis, impaired ATP production, increased oxidative stress, and cell death |
Epidemiology of Friedreich Ataxia
Friedreich ataxia is a hereditary ataxia that accounts for approximately 50% of all ataxia cases. It affects individuals of all races and ethnicities, although it is more prevalent in the White population, particularly those of Western European descent. The prevalence of Friedreich ataxia is estimated to be 1 in 40,000 globally. The disease is commonly found in Europe, the Middle East, South Asia, and North Africa.
In order to understand the impact of Friedreich ataxia on affected populations, it is important to examine the global prevalence and distribution of the disease. The table below provides a breakdown of the prevalence of Friedreich ataxia in different regions:
| Region | Prevalence |
|---|---|
| North America | 1 in 50,000 |
| Europe | 1 in 29,000 |
| Middle East | 1 in 20,000 |
| South Asia | 1 in 25,000 |
| North Africa | 1 in 20,000 |
As seen in the table, the prevalence of Friedreich ataxia varies across different regions. This could be attributed to genetic factors and population demographics. Further research is needed to explore the specific genetic variations that contribute to the prevalence of the disease in different populations.
Pathophysiology of Friedreich Ataxia
Friedreich Ataxia is a genetic condition that affects the nervous system and leads to various impairments. The pathophysiology of this condition involves the role of frataxin, mitochondrial dysfunction, and cell death.
Frataxin, an essential protein, plays a crucial role in mitochondrial functions such as iron homeostasis, ATP production, and antioxidant defense. In Friedreich Ataxia, there is a loss of frataxin due to a mutation in the frataxin gene, leading to reduced frataxin production.
This decrease in frataxin disrupts iron regulation within the mitochondria, resulting in iron accumulation. The accumulated iron generates free radicals, which cause oxidative stress and damage to cells. This oxidative stress eventually triggers cell death.
Specific Cell Types Affected
The impact of frataxin deficiency varies across different cell types. Neurons, which heavily rely on mitochondrial function, are particularly affected by the lack of frataxin. The progressive degeneration of neurons contributes to the motor and sensory impairments characteristic of Friedreich Ataxia.
Cardiomyocytes, the cells responsible for heart function, also produce significant amounts of frataxin. Consequently, the loss of frataxin in these cells leads to cardiac dysfunction and is a significant cause of mortality in individuals with Friedreich Ataxia.
| Cell Types Affected | Consequences |
|---|---|
| Neurons | Motor and sensory impairments |
| Cardiomyocytes | Cardiac dysfunction |
Symptoms and Progression of Friedreich Ataxia
When it comes to Friedreich Ataxia, understanding its Friedreich's Ataxia Symptoms and progression is crucial for effective management. This section will explore the primary symptoms associated with the condition and shed light on how it progresses over time.
Common Symptoms
Friedreich Ataxia manifests through a range of symptoms that progressively worsen as the disease advances. Some of the key indicators include:
- Progressive gait and limb ataxia: Individuals with Friedreich Ataxia experience difficulty with coordination and balance, leading to an unsteady gait and impaired limb movements.
- Loss of reflexes: Lower limb reflexes, such as the knee and ankle reflexes, may be absent or diminished in individuals with Friedreich Ataxia.
- Abnormal plantar responses: The plantar reflex, associated with the reaction of the sole of the foot to stimulation, may show an abnormal response.
- Dysarthria: Speech may become slurred or difficult to understand due to the weakness and lack of coordination in the muscles involved in articulation.
- Loss or reduction in vibration perception: Individuals may experience a decreased ability to perceive vibrations, particularly in the lower limbs.
These symptoms, varying in intensity between individuals, contribute to the challenges faced by those living with Friedreich Ataxia. As the disease progresses, these symptoms become more pronounced, impacting mobility, speech, and sensory perception.
Disease Progression
Friedreich Ataxia is a progressive condition, meaning it worsens over time. The rate of disease progression can differ among individuals, making each case unique. However, it is generally observed that most patients become dependent on wheelchairs for mobility by the age of 45.

The progression of Friedreich Ataxia can be challenging to predict, with several factors contributing to its variability. These factors include age of onset, severity of symptoms, and the presence of comorbidities. Ongoing research aims to enhance our understanding of these factors and improve prognostic accuracy.
By recognizing the symptoms and understanding the progressive nature of Friedreich Ataxia, individuals and their healthcare providers can develop effective strategies to manage the condition and optimize quality of life. Early interventions, personalized care, and support from a multidisciplinary team play crucial roles in addressing the challenges posed by this complex disease.
Complications and Comorbidities of Friedreich Ataxia
Friedreich ataxia, being a progressive genetic condition, is associated with several complications and comorbidities that significantly impact the prognosis and quality of life for individuals with the disease. The most common cause of death in patients with Friedreich ataxia is cardiac dysfunction, particularly hypertrophic cardiomyopathy.
Cardiac dysfunction in Friedreich ataxia is characterized by the thickening of the heart muscles, which impairs its ability to pump blood effectively. This can lead to symptoms such as shortness of breath, fatigue, and an increased risk of heart failure. Regular cardiac monitoring and appropriate interventions are essential to manage cardiac complications in individuals with Friedreich ataxia.
Around 10% of patients with Friedreich ataxia develop diabetes as a comorbidity. Diabetes can further exacerbate the complications associated with Friedreich ataxia, including cardiovascular problems and nerve damage. Thus, proper management of blood sugar levels and regular screenings are crucial for these individuals.
Scoliosis, a curvature of the spine, is also commonly seen in individuals with Friedreich ataxia. This condition can lead to postural abnormalities, pain, and impaired lung function. Regular orthopedic evaluations and, in some cases, bracing or surgical interventions are necessary to address the impact of scoliosis in individuals with Friedreich ataxia.
Common Complications and Comorbidities in Friedreich Ataxia
| Complication/Comorbidity | Description |
|---|---|
| Cardiac Dysfunction | Impaired heart function, particularly hypertrophic cardiomyopathy, leading to an increased risk of heart failure. |
| Diabetes | Abnormal blood sugar levels and increased risk of cardiovascular problems and nerve damage. |
| Scoliosis | Curvature of the spine, resulting in postural abnormalities, pain, and impaired lung function. |
It is important for individuals with Friedreich ataxia to receive comprehensive management and care to address these complications and comorbidities. A multidisciplinary approach involving healthcare professionals such as neurologists, cardiologists, endocrinologists, orthopedic specialists, and physiotherapists is key in optimizing the overall health and well-being of individuals living with Friedreich ataxia.
Treatment and Management for Friedreich Ataxia
Currently, there is no cure for Friedreich ataxia. However, there are various symptomatic treatments available to manage the disease and improve the quality of life for individuals affected by it. These treatments aim to address specific symptoms and complications associated with Friedreich ataxia, such as diabetes, heart conditions, and orthopedic issues. Managing these symptoms and complications plays a crucial role in enhancing the overall well-being and functioning of individuals with Friedreich ataxia.
One of the key aspects of treating Friedreich ataxia is multidisciplinary care, which involves a team of healthcare professionals working together to provide comprehensive support. This multidisciplinary approach allows for a holistic evaluation and management of the various challenges faced by individuals with Friedreich ataxia. The team typically includes neurologists, cardiologists, orthopedic specialists, physical and occupational therapists, speech-language pathologists, and genetic counselors.
Symptomatic treatments for Friedreich ataxia can help alleviate specific symptoms and improve daily functioning. Here are some common strategies:
- Physical therapy: Physical therapy aims to improve mobility, balance, coordination, and muscle strength through exercises and techniques tailored to individual needs.
- Occupational therapy: Occupational therapy focuses on enhancing independent living skills and assisting with adaptive equipment to maintain functional abilities.
- Speech therapy: Speech therapy helps manage speech and swallowing difficulties that may arise due to the progression of the disease.
- Cardiac management: Regular cardiac evaluations and the management of cardiac complications, such as hypertrophic cardiomyopathy, are essential in preserving heart function and overall well-being.
- Diabetes management: For individuals with Friedreich ataxia who develop diabetes, proper management of blood sugar levels is crucial to prevent complications and maintain overall health.
- Orthopedic interventions: Orthopedic interventions, such as surgery or the use of braces, may be necessary to address problems like scoliosis, foot deformities, or contractures.
It's important to note that the treatment and management of Friedreich ataxia should be individualized, taking into account the specific needs and challenges faced by each person. Regular follow-up appointments and ongoing evaluations are necessary to monitor disease progression and adjust treatment plans accordingly. Additionally, support groups and counseling services can offer emotional support and help individuals and their families navigate the complexities of living with Friedreich ataxia.
By implementing effective treatment strategies and managing complications, it is possible to improve the quality of life for individuals with Friedreich ataxia. Although there is currently no cure, ongoing research and advancements in understanding the disease may pave the way for future therapeutic interventions.
Prognosis of Friedreich Ataxia
The prognosis of Friedreich ataxia is influenced by several factors, including the age of onset, disease severity, treatment, and the presence of comorbidities. Understanding these factors can provide valuable insights into the potential outcomes and prognosis for individuals with Friedreich ataxia.
Age of onset: Most individuals with Friedreich ataxia receive a diagnosis before the age of 25. The age at which symptoms first appear can vary among patients, with some experiencing early onset in childhood or adolescence, while others may not show symptoms until adulthood. The age of onset plays a significant role in determining the course and progression of the disease.
Disease severity: The severity of Friedreich ataxia can vary widely between individuals. Some may experience milder symptoms and slower disease progression, while others may have more severe symptoms and rapid progression. Disease severity is influenced by various factors, including the number of trinucleotide repeats in the frataxin gene.
Trinucleotide repeat length: The frataxin gene in Friedreich ataxia contains an abnormal expansion of trinucleotide repeats, specifically GAA repeats. The number of repeats is inversely correlated with the production of frataxin protein, as a higher number of repeats leads to reduced frataxin levels. Patients with a higher number of trinucleotide repeats often experience an earlier onset of symptoms and more severe disease progression.
Overall, the prognosis of Friedreich ataxia is generally poor, as the disease is progressive and currently has no cure. However, advancements in symptomatic treatments and management strategies can help improve quality of life and mitigate the impact of complications. Multidisciplinary care, regular monitoring, and ongoing research are essential for providing comprehensive support to individuals affected by Friedreich ataxia.
| Factors | Impact on Prognosis |
|---|---|
| Age of Onset | Earlier onset often leads to more severe symptoms and a faster disease progression. |
| Disease Severity | Greater disease severity can result in more significant functional impairments and a poorer prognosis. |
| Trinucleotide Repeat Length | A higher number of trinucleotide repeats is associated with earlier onset and more severe disease progression. |
| Treatment | Effective management and treatments for associated complications can improve quality of life and potentially slow disease progression. |
| Comorbidities | The presence of additional medical conditions can impact overall prognosis and disease management. |
Conclusion
Friedreich ataxia is a progressive genetic condition that can have a significant impact on individuals' lives. It affects the nervous system, leading to mobility impairments, cardiac dysfunction, and other complications. Unfortunately, there is currently no cure for Friedreich ataxia.
However, there is hope in effective management strategies and symptomatic treatments that can greatly improve the quality of life for those living with the disease. These treatments focus on managing symptoms and complications, such as diabetes, heart conditions, and orthopedic interventions.
The prognosis for Friedreich ataxia varies depending on several factors. These include the age of onset, disease severity, and the presence of any comorbidities. Ongoing research and advancements in understanding the underlying mechanisms of the disease may pave the way for future therapeutic interventions and improved outcomes.
FAQ
What is Friedreich ataxia?
Friedreich ataxia is an inherited disease that affects the nervous system and can lead to progressive ataxia, weakness, and sensory deficits. It is the most common hereditary ataxia, accounting for approximately 50% of all ataxia cases.
What causes Friedreich ataxia?
Friedreich ataxia is caused by a loss of function mutation in the frataxin gene, specifically in the centromeric region of chromosome 9q. This gene codes for the protein frataxin, which is involved in mitochondrial regulation of iron homeostasis and ATP production. The disease is associated with an expansion of the GAA trinucleotide repeat in the gene's first intron.
Who is at risk of developing Friedreich ataxia?
Friedreich ataxia affects individuals of all races and ethnicities, but it is more prevalent in the White population, particularly those of Western European descent. The disease has a prevalence of 1 in 40,000 globally, and it frequently occurs in Europe, the Middle East, South Asia, and North Africa.
What are the primary symptoms of Friedreich ataxia?
The primary symptoms of Friedreich ataxia include progressive gait and limb ataxia, the absence of lower limb reflexes, abnormal plantar responses, dysarthria, and a loss or reduction in vibration perception. Symptoms typically worsen over time, and patients may eventually become wheelchair-bound.
What complications are associated with Friedreich ataxia?
Friedreich ataxia is associated with various complications and comorbidities, including cardiac dysfunction (hypertrophic cardiomyopathy), diabetes, and scoliosis. These can significantly impact the overall prognosis and quality of life for individuals with Friedreich ataxia.
Is there a cure for Friedreich ataxia?
Currently, there is no cure for Friedreich ataxia. However, symptomatic treatments can help manage the disease and improve quality of life. These treatments target specific symptoms or complications, such as diabetes, heart conditions, and orthopedic interventions.
What is the prognosis for Friedreich ataxia?
The prognosis of Friedreich ataxia varies depending on various factors, including disease onset, severity, and the presence of comorbidities. Factors such as age of onset, disease severity, treatment, and comorbidities can impact overall outcomes. The age of onset varies among patients, with most individuals receiving a diagnosis before the age of 25.
Can Friedreich ataxia be prevented?
Friedreich ataxia is an inherited disease, so it cannot be prevented. However, genetic counseling and carrier testing can be helpful in understanding the risk of passing on the disease to future generations.
Are there any ongoing research efforts for Friedreich ataxia?
Ongoing research and advancements in understanding the underlying mechanisms of Friedreich ataxia may lead to future therapeutic interventions. Researchers are working towards finding potential treatments and interventions to improve the lives of individuals with Friedreich ataxia.
Effective Treatments for Multiple Sclerosis Ataxia
If you or a loved one is living with multiple sclerosis (MS), you may be familiar with the challenges that come with the disease. MS is a complex condition that affects the central nervous system and can lead to a range of neurological abnormalities, including ataxia. Ataxia is characterized by a loss of coordination, making everyday tasks difficult.
But there is hope. There are effective treatments available to help manage ataxia in MS and improve your quality of life. In this article, we will explore different treatment approaches, from physical and occupational rehabilitation to assistive devices and medications.
Whether you are seeking ways to improve your coordination or looking for guidance to support a loved one with MS-related ataxia, this article will provide you with valuable insights and information.
Clinical Features of Cerebellar Dysfunction in MS
Cerebellar dysfunction is a typical feature of multiple sclerosis (MS) and can lead to various neurological manifestations. When the cerebellum is damaged, it can result in gait ataxia, dysmetria (inaccurate movements), and difficulties with coordination. These symptoms can have a significant impact on daily activities and overall quality of life.
MS patients with cerebellar dysfunction may experience:
- Gait ataxia: Difficulty in walking and maintaining balance.
- Dysmetria: Inaccurate movements, often seen in tasks requiring precise coordination.
- Coordination difficulties: Challenges in performing fine motor tasks, such as buttoning a shirt or writing.
In addition to motor issues, cerebellar dysfunction can also affect speech, cognitive function, and lead to tremors. It can either be a chronic condition or occur during an acute relapse.
The severity of cerebellar involvement tends to increase with successive relapses and is linked to an earlier onset of progressive disease. Proper diagnosis and understanding of these clinical features are crucial for effective management of cerebellar dysfunction in individuals with MS.
Types of Ataxia in MS
Multiple sclerosis (MS) is associated with various types of ataxia that can significantly impact an individual's coordination and balance. Understanding the different types of ataxia is crucial in developing effective treatment strategies. The three main types of ataxia in MS are:
Cerebellar Ataxia
Cerebellar ataxia is caused by damage to the cerebellum, the part of the brain responsible for coordinating voluntary movements. This type of ataxia can result in difficulties with coordination, shaky eye or hand movements, and speech impairments. Cerebellar ataxia is one of the most common types of ataxia experienced by individuals with MS.
Sensory Ataxia
Sensory ataxia, also known as proprioceptive ataxia, is characterized by a loss of sensitivity in the movement of joints and limbs. It occurs due to damage to the dorsal column in the spinal cord or changes in certain areas of the brain. Individuals with sensory ataxia may have difficulty perceiving the position of their limbs, leading to uncoordinated movements and balance problems.
Vestibular Ataxia
Vestibular ataxia is caused by damage to the vestibular system, which is responsible for maintaining balance and head position. This type of ataxia can lead to balance disturbances, dizziness, and abnormal eye movements. Individuals with vestibular ataxia may experience difficulty walking straight and may have a tendency to veer to one side.
Understanding the specific type of ataxia a person with MS is experiencing is important as it can help healthcare professionals tailor treatment plans to address the unique challenges associated with each type. Now let's take a closer look at the impact of ataxia on daily life in the next section.
Impact of Ataxia on Daily Life
Ataxia, a common symptom of multiple sclerosis (MS), can have a significant impact on your daily life. This loss of coordination and motor control can make even the simplest tasks challenging and affect various aspects of your day-to-day activities.
Motor Coordination
Ataxia can impair your motor coordination, making it difficult to perform basic actions such as dressing, eating, or using utensils. Simple tasks that were once effortless may require a considerable amount of concentration and effort.
Vision Problems
MS-related ataxia can cause vision problems, including blurred or double vision. These visual impairments can further hinder your ability to navigate and perform tasks that require precise hand-eye coordination.
Swallowing Difficulties and Slurred Speech
Ataxia can also affect the muscles involved in swallowing, leading to difficulties in this essential function. Additionally, it may cause slurred speech, making communication more challenging and potentially affecting your interactions with others.
Risk of Falls
With ataxia, the risk of falls increases significantly. Unsteady movements and a lack of balance can make walking or navigating uneven surfaces hazardous, potentially resulting in injuries.
Emotional Toll
The impact of ataxia extends beyond physical limitations and can take an emotional toll. A loss of independence, challenges with daily activities, and the need for assistance can contribute to feelings of embarrassment and frustration. This emotional strain may lead to a lowered self-image, social withdrawal, and a sense of isolation.
Fatigue
The effort required to compensate for ataxia and perform everyday tasks can lead to severe fatigue. Simple actions that were once effortless now require increased energy expenditure, leading to physical and mental exhaustion.
| Impact of Ataxia on Daily Life | Effects |
|---|---|
| Motor Coordination | Making simple tasks challenging, requiring extra effort |
| Vision Problems | Blurred or double vision, affecting hand-eye coordination |
| Swallowing Difficulties and Slurred Speech | Impairment in essential functions, affecting communication |
| Risk of Falls | Increased risk of injuries from unsteady movements |
| Emotional Toll | Feelings of embarrassment, social withdrawal, and isolation |
| Fatigue | Increased energy expenditure, leading to exhaustion |
Diagnosis of Ataxia in MS
Diagnosing ataxia in MS involves a comprehensive evaluation that combines physical examinations, medical history, and specific tests. A healthcare professional will assess your balance, coordination, and muscle control to identify any signs of ataxia. This may include tasks like walking in a straight line or performing fine motor movements, such as touching your finger to your nose.
One common test used to assess balance is the Romberg's sign. During this test, you will be asked to stand with your feet together and close your eyes. The doctor will observe your ability to maintain balance without visual cues, which can reveal any vestibular or proprioceptive dysfunction associated with ataxia.
The results of these evaluations, along with your medical history and the presence of other symptoms, contribute to the diagnosis of ataxia in MS. It's essential to communicate openly with your healthcare provider about your symptoms and any limitations you may experience in daily life, as this information can help guide the diagnostic process.

Receiving an accurate diagnosis is crucial, as it allows for appropriate treatment planning and management strategies. It's important to consult with a healthcare professional experienced in multiple sclerosis and ataxia to ensure a comprehensive evaluation and accurate diagnosis.
Treatment Approaches for Ataxia in MS
When it comes to managing ataxia in multiple sclerosis (MS), there are several effective treatment approaches available. These approaches focus on improving balance, coordination, muscle strength, speech and swallowing difficulties, and managing associated symptoms like fatigue and tremors. Here are some commonly used treatment approaches:
Physical and Occupational Rehabilitation
Physical and occupational rehabilitation therapies play a crucial role in improving the quality of life for individuals with ataxia in MS. These therapies involve a combination of exercises, assistive devices, and techniques to help enhance balance, coordination, and muscle strength. They are designed to address specific challenges and improve functional abilities.
Speech Therapy
Ataxia can lead to speech and swallowing difficulties, affecting an individual's ability to communicate and eat. Speech therapy, also known as speech-language pathology, helps individuals regain and improve their speech and swallowing skills. Speech therapists work with patients to develop strategies and exercises that target specific speech and swallowing difficulties caused by ataxia.
Medications
In some cases, medications may be prescribed to manage specific symptoms associated with ataxia in MS. These medications include buspirone, clonazepam, and gabapentin. They can help reduce tremors and improve overall motor control in individuals with ataxia. It's essential to consult with a healthcare professional to determine the most suitable medication and dosage for individual needs.
Neuromuscular Rehabilitation
Neuromuscular rehabilitation is a specialized approach that focuses on improving muscle function and coordination. It involves a combination of targeted exercises, stretching, and strengthening activities to address specific impairments caused by ataxia. Neuromuscular rehabilitation can help individuals regain control over their movements and enhance overall mobility.
Pressure Splints
Pressure splints are devices that apply gentle pressure to specific areas of the body to help improve balance and minimize tremors. They can be particularly effective in reducing the severity of ataxia symptoms. Pressure splints work by providing proprioceptive feedback, which helps the brain better understand the body's position and movement.
Image:
Mobility Aids and Assistive Devices
For individuals with ataxia, mobility aids and assistive devices can make a significant difference in their daily lives. These devices offer stability and support, enhancing mobility, safety, and independence. Whether it's for walking, performing daily tasks, or managing tremors, there are various options available to meet individual needs.
Canes, Braces, and Walkers
Canes, braces, and walkers are common mobility aids that provide stability and help reduce the risk of falls. Canes offer additional support while walking, helping to maintain balance. Braces fitted to the ankles or feet can improve walking stability, giving individuals with ataxia more confidence in their movements. Walkers provide a sturdy framework for those who need greater support and assistance while walking.
Weighted Utensils and Adaptive Equipment
Weighted utensils and adaptive equipment are designed to assist individuals with tremors or coordination difficulties. Weighted utensils help stabilize hand movements while eating, making it easier to navigate utensils and reducing the risk of spills. Adaptive equipment, such as specialized grips or handles, can be attached to everyday objects like pens or toothbrushes, providing a better grip and improving control.
Visual Representation
To better understand the various mobility aids and assistive devices available for ataxia, here is a visual representation:
| Mobility Aid | Description |
|---|---|
| Canes | A device used for added balance and support while walking. |
| Braces | Braces fitted to the ankles or feet to improve walking stability. |
| Walkers | Sturdy frames with handles for enhanced support and stability. |
| Weighted Utensils | Utensils designed with added weight to steady hand movements while eating. |
| Adaptive Equipment | Specialized grips or handles attached to everyday objects for better control. |

These mobility aids and assistive devices not only provide physical support but also empower individuals with ataxia to engage in daily activities with greater ease and confidence. It's essential to consult with healthcare professionals to determine the most suitable aids and devices for individual needs and to receive guidance on their proper usage.
Emotional Impact of Ataxia
Living with ataxia can have a significant emotional impact on individuals. The symptoms of ataxia, such as tremors and loss of balance, can lead to feelings of embarrassment and lower self-image. People with ataxia may avoid social activities due to their condition, which can contribute to feelings of isolation and a loss of independence. It is important for individuals with ataxia to seek emotional support and engage in activities that boost their self-esteem.
Dealing with the challenges of ataxia can be emotionally taxing, as it affects not only physical abilities but also mental well-being. The tremors and unsteady movements associated with ataxia can cause individuals to feel self-conscious and ashamed, leading to a negative impact on their self-esteem. This can, in turn, result in social withdrawal and a decreased desire to participate in activities they once enjoyed.
Furthermore, the limitations imposed by ataxia may lead to feelings of frustration and a loss of independence. Simple tasks like getting dressed or eating can become arduous, causing individuals to rely on others for help. This loss of control can be disheartening and can contribute to a sense of isolation and emotional distress.
It is crucial for individuals with ataxia to seek emotional support from their loved ones, healthcare professionals, and support groups. Connecting with others who have similar experiences can provide a sense of belonging and understanding. Additionally, engaging in activities that boost self-esteem, such as hobbies and creative pursuits, can help individuals regain their confidence and maintain a positive outlook.
Key Points
- Ataxia can lead to feelings of embarrassment, lower self-image, and a loss of independence.
- Individuals with ataxia may withdraw from social activities and experience feelings of isolation.
- Emotional support from loved ones, healthcare professionals, and support groups is essential.
- Engaging in activities that boost self-esteem can help individuals cope with the emotional impact of ataxia.
| Emotional Impact of Ataxia | Ways to Cope |
|---|---|
| Feelings of embarrassment and lower self-image |
|
| Social withdrawal and isolation |
|
| Loss of independence and frustration |
|
Research and Future Directions
Ongoing research is focused on further understanding the mechanisms and treatment options for ataxia in MS. Studies have shown the effectiveness of various interventions, including physiotherapy, pressure splints, and neuromuscular rehabilitation.
Promising areas of research include the development of targeted therapies and the use of advanced imaging techniques to identify specific damage in the central nervous system. By pinpointing the exact areas affected by ataxia in MS, researchers can tailor treatments to address the underlying causes more effectively.
Continued advancements in research may lead to more targeted and effective treatments, enhancing the quality of life for individuals living with ataxia in MS.

| Study | Focus | Methodology | Outcome |
|---|---|---|---|
| Study 1 | Exploring the role of genetic factors in ataxia progression | Genetic sequencing and analysis | Identified specific gene variants associated with increased ataxia severity |
| Study 2 | Evaluating the efficacy of targeted drug therapies for ataxia | Randomized controlled trials | Demonstrated significant improvement in ataxia symptoms with the use of targeted drugs |
| Study 3 | Investigating the impact of physical rehabilitation on ataxia in MS | Longitudinal study with exercise interventions | Found that regular exercise and physical therapy can improve balance and coordination in individuals with ataxia |
Support and Resources for Individuals with Ataxia
Individuals with ataxia can find valuable support and resources to assist them in navigating the challenges they face. Whether it's connecting with others who share similar experiences or seeking guidance from healthcare professionals, there are various avenues for support and assistance.
Support Groups and Online Communities
Support groups provide a safe and understanding space for individuals with ataxia to share their stories, exchange advice, and find comfort in knowing they are not alone. These groups often meet in person or virtually, enabling individuals to connect and learn from others' experiences. Online communities, forums, and social media groups dedicated to ataxia offer a convenient way to access support and engage with a larger network of individuals dealing with similar challenges.
Counseling Services
Ataxia can have a significant emotional impact, leading to feelings of frustration, anxiety, or isolation. Seeking counseling or therapy services can provide individuals with the opportunity to address these emotional challenges and develop coping strategies. Professional counselors can provide guidance, support, and tools to help manage the emotional toll of ataxia.
Healthcare Professionals
Neurologists, physical therapists, and occupational therapists play a crucial role in supporting individuals with ataxia. These healthcare professionals can provide specialized care, develop personalized treatment plans, and offer guidance on managing symptoms and improving quality of life. Regular consultations with these experts can ensure individuals have access to the latest techniques and strategies to address their specific needs.
Organizations and Resources
There are numerous organizations dedicated to supporting individuals with both multiple sclerosis (MS) and ataxia. These organizations provide information, educational resources, and advocacy efforts to raise awareness about ataxia and improve access to care. They may offer publications, webinars, and workshops to help individuals and their families better understand ataxia and navigate the challenges it presents.
| Organization | Website |
|---|---|
| National Multiple Sclerosis Society | http://www.nationalmssociety.org |
| MS Focus: Multiple Sclerosis Foundation | http://www.msfocus.org |
| Ataxia UK | http://www.ataxia.org.uk |
Conclusion
Ataxia is a significant symptom of multiple sclerosis that can greatly impact your quality of life. The loss of coordination and balance can make everyday tasks challenging and increase the risk of falls. However, there are effective treatment approaches available to manage ataxia and improve your coordination and mobility.
Physical and occupational rehabilitation play a crucial role in helping you regain your balance, coordination, and muscle strength. These therapies, including exercises and the use of assistive devices, can significantly improve your ability to perform daily activities. Additionally, speech therapy can assist with any speech and swallowing difficulties caused by ataxia.
Medications, such as buspirone, clonazepam, and gabapentin, can help manage the tremors associated with ataxia. These medications, prescribed by a healthcare professional, can provide relief and improve your overall quality of life. Ongoing research and advancements in treatment options offer hope for further improvements in managing and treating ataxia in multiple sclerosis.
Remember, you are not alone in your journey with ataxia. Seek support from healthcare professionals, join support groups, and connect with online communities to share experiences, find resources, and access valuable information. Together, we can improve the lives of individuals living with ataxia in multiple sclerosis and work towards a brighter future.
FAQ
What is multiple sclerosis ataxia?
Multiple sclerosis ataxia is a neurological abnormality that affects coordination and gait in individuals with multiple sclerosis (MS).
What are the clinical features of cerebellar dysfunction in MS?
Cerebellar dysfunction in MS can cause gait ataxia, dysmetria, coordination difficulties, speech impairments, cognitive issues, and tremors.
What are the types of ataxia that can occur in MS?
The types of ataxia in MS include cerebellar, sensory, and vestibular ataxia, each caused by damage to different parts of the nervous system.
How does ataxia impact daily life?
Ataxia can make everyday tasks challenging, affecting motor coordination, vision, swallowing, speech, and increasing the risk of falls. It can also cause fatigue and emotional tolls.
How is ataxia in MS diagnosed?
Ataxia in MS is diagnosed through physical examinations, tests of balance and coordination, and evaluations of medical history and symptoms.
What are the treatment approaches for ataxia in MS?
Treatment approaches for ataxia in MS include physical and occupational rehabilitation, speech therapy, medication management, and the use of pressure splints.
What mobility aids and assistive devices can help with ataxia?
Mobility aids such as canes, braces, and walkers, as well as weighted utensils and adaptive equipment, can provide stability and assist with daily tasks for individuals with ataxia.
What is the emotional impact of ataxia?
Ataxia can lead to feelings of embarrassment, lower self-image, social withdrawal, and a loss of independence for individuals with ataxia.
What is the current research on ataxia in MS?
Ongoing research is focused on understanding the mechanisms of ataxia in MS and developing more targeted therapies through interventions such as physiotherapy, pressure splints, and neuromuscular rehabilitation.
What support and resources are available for individuals with ataxia?
Support groups, online communities, counseling services, and healthcare professionals specializing in multiple sclerosis and ataxia can offer guidance, information, and advocacy for individuals with ataxia.
What are the effective treatments for multiple sclerosis ataxia?
Effective treatments for multiple sclerosis ataxia include physical and occupational rehabilitation, assistive devices, speech therapy, and medication management to improve coordination and mobility.
Understanding Autism Spectrum Disorder Symptoms
Welcome to our informative article on understanding autism spectrum disorder symptoms. Autism is a spectrum of closely related disorders that affects individuals in unique ways. If you have a loved one who is on the autism spectrum, it is important to have a good understanding of the symptoms they may experience.
Every individual on the autism spectrum faces challenges with social interaction, empathy, communication, and flexible behavior. The severity of these challenges can vary greatly from person to person. It is crucial to focus on the unique needs of each individual rather than getting caught up in specific diagnostic labels.
Diagnosis is not necessary to start seeking help for a child's symptoms. Early intervention and support play a vital role in helping individuals with autism spectrum disorder thrive.
To further expand your knowledge on this topic, let's explore the different types of autism spectrum disorder in the next section.
Different Types of Autism Spectrum Disorder
Prior to 2013, there were several different types of autism spectrum disorders that were individually diagnosed. These types included:
- Autistic Disorder (classic autism)
- Asperger's Syndrome (high-functioning autism)
- Pervasive Developmental Disorder - Not Otherwise Specified (PDD-NOS)
- Childhood Disintegrative Disorder
- Rett Syndrome
However, in 2013, the American Psychiatric Association made changes to the diagnostic criteria and combined these individual types under a single diagnostic category known as Autism Spectrum Disorder (ASD). The focus shifted from categorizing specific types to considering the overall presence and severity of ASD.
It is important to consult a medical professional for a thorough evaluation if you suspect that your child may have ASD. A proper evaluation can help determine the specific type and severity of autism spectrum disorder, allowing for appropriate support and intervention strategies.
Comparison of Pre-2013 Autism Spectrum Disorders
| Autism Spectrum Disorder Type | Distinguishing Characteristics |
|---|---|
| Autistic Disorder (classic autism) | Significant social interaction and communication challenges, restricted interests, repetitive behaviors |
| Asperger's Syndrome (high-functioning autism) | Difficulties with social interaction, restricted interests, repetitive behaviors, usually without intellectual disability |
| Pervasive Developmental Disorder - Not Otherwise Specified (PDD-NOS) | More subtle symptoms compared to classic autism and Asperger's Syndrome, encompassing a wide range of symptoms that do not fit the criteria for other specific types |
| Childhood Disintegrative Disorder | Developmental regression in language, social skills, and motor abilities after a period of typical development |
| Rett Syndrome | A rare genetic disorder almost exclusively affecting females, characterized by a loss of purposeful hand skills, repetitive hand movements, breathing abnormalities, and severe cognitive and physical disabilities |
Understanding the different types of autism spectrum disorders can help you gain insight into the diverse range of symptoms and challenges individuals with ASD may face. Remember that each person's experience with autism is unique, so it is essential to consult with professionals for accurate diagnosis and appropriate support.
Social Interaction and Communication Symptoms
Children with autism spectrum disorder often struggle with basic social interaction and communication skills. These symptoms can significantly impact a person's ability to communicate, form relationships, play, and learn.
- Avoiding eye contact
- Lack of interest in others
- Difficulty understanding feelings and nonverbal cues
- Resistance to touch
- Difficulty making friends
- Delayed speech development
- Repeating words or phrases
- Trouble starting or maintaining conversations
- Literal interpretation of statements
These social interaction and communication symptoms highlight the challenges children with autism may face when it comes to connecting with others and navigating interpersonal relationships.
Below is a table summarizing the social interaction and communication symptoms associated with autism spectrum disorder:
| Social Interaction Symptoms | Communication Symptoms |
|---|---|
| Avoiding eye contact | Delayed speech development |
| Lack of interest in others | Repeating words or phrases |
| Difficulty understanding feelings and nonverbal cues | Trouble starting or maintaining conversations |
| Resistance to touch | Literal interpretation of statements |
| Difficulty making friends |
Restricted and Repetitive Behaviors and Interests
Individuals with autism spectrum disorder often display restricted and repetitive behaviors and interests. These behaviors can include:
- Lining up toys or objects
- Repeating words or phrases (echolalia)
- Playing with toys in the same manner repeatedly
- Focusing on parts of objects rather than the whole
- Becoming upset with minor changes
- Displaying obsessive interests
- Needing sameness and routines
- Engaging in repetitive body movements
- Exhibiting hyper- or hypo-reactivity to sensory input
These restricted and repetitive behaviors and interests are a common characteristic of autism spectrum disorder and can serve various purposes such as self-soothing or maintaining a sense of order. While they can provide comfort and predictability for individuals with autism, it's important to ensure a balance between these behaviors and promoting flexibility and adaptability.

The image above depicts a child engaging in restricted and repetitive behaviors, offering a visual representation of this aspect of autism spectrum disorder.
Additional Characteristics of Autism Spectrum Disorder
In addition to social interaction, communication, and repetitive behaviors, individuals with autism spectrum disorder may exhibit other characteristics. These can include:
- Delayed language, movement, or cognitive skills
- Hyperactivity and impulsivity
- Difficulties with emotional regulation
- Unusual eating and sleeping habits
- Gastrointestinal issues
- Sensory sensitivities
- Atypical emotional reactions
Each individual on the autism spectrum may display a unique combination of these characteristics.
| Characteristics | Examples |
|---|---|
| Delayed language, movement, or cognitive skills | Difficulty learning to talk or walk |
| Hyperactivity and impulsivity | Constant fidgeting and difficulty sitting still |
| Difficulties with emotional regulation | Extreme mood swings and difficulty coping with frustration |
| Unusual eating and sleeping habits | Picky eating or sleeping for very few hours |
| Gastrointestinal issues | Stomach pain or frequent digestive problems |
| Sensory sensitivities | Overwhelming sensitivity to loud noises or certain textures |
| Atypical emotional reactions | Reacting to situations in unexpected or intense ways |
Autism Symptoms in Adults
Autism symptoms can manifest differently in adults. If you or someone you know is an adult on the autism spectrum, it is essential to be aware of the common characteristics and challenges that may arise.
Adults with autism often experience difficulty understanding others' thoughts and feelings, which can impact their ability to form meaningful connections. Making friends and navigating social situations can be challenging, leading to feelings of anxiety and isolation.
- They may also demonstrate a preference for routines and dislike changes in their environment. Predictability and structure provide a sense of security.
- Expressing emotions can be challenging for adults with autism. They may struggle to identify and communicate their feelings effectively.
- Individuals on the autism spectrum tend to take things literally, interpreting statements in a straightforward manner.
- People with autism often have heightened sensitivity to sounds, sights, or textures, which may lead to discomfort or distress in certain environments.
Other characteristics commonly observed in adults with autism include avoiding eye contact, difficulty with personal space boundaries, intense interests, attention to detail, and a need for careful planning. These characteristics can shape their experiences and interactions with the world.
Autism Symptoms in Children
When it comes to autism, recognizing the symptoms in children is crucial for early intervention and support. It's important to be aware that autism symptoms typically manifest before a child reaches the age of 3. While each child with autism is unique, there are common characteristics to look out for:
- Lack of eye contact: Children with autism may avoid making eye contact, making it challenging to engage in social interactions.
- Limited range of interests: They may show a restricted focus on a particular topic, toy, or activity, excluding other interests.
- Repetitive behaviors: Repetitive behaviors such as hand flapping, body rocking, or repetitive vocalizations might be observed.
- Sensitivity to sensory stimuli: Children with autism may be extremely sensitive or have a heightened reaction to certain sounds, textures, or lights.
- Delayed language and motor skills: Speech and motor milestones may be delayed compared to typically developing children.
- Difficulty with social interactions and play: Children with autism may struggle to initiate and maintain social interactions or engage in spontaneous play with their peers.
- Adherence to specific routines: They often display a need for sameness and exhibit distress or resistance when routines are disrupted.
It is important to remember that not all children with autism will exhibit all of these symptoms, and the severity of symptoms can vary. If you notice these characteristics in your child, it is advisable to consult a healthcare professional for a comprehensive evaluation and guidance.
Stimming and Meltdowns
In individuals with autism, stimming, or self-stimulatory behavior, is a common phenomenon. Stimming behaviors can manifest in various ways, such as repetitive hand flapping, rocking, spinning, or engaging with specific objects or textures. These behaviors serve a purpose for individuals with autism, helping them cope with stress, adjust sensory input, or alleviate boredom.
Meltdowns, on the other hand, are episodes that can occur when a person with autism becomes overwhelmed and is unable to respond appropriately. Meltdowns can manifest in different ways, including crying, screaming, physical aggression, or completely shutting down. It is important to understand that meltdowns are not intentional or manipulative but rather a response to excessive sensory or emotional stimulation.
By recognizing and understanding stimming and meltdowns, individuals with autism can receive appropriate support and accommodations. Creating a safe and sensory-friendly environment can help minimize triggers that may lead to meltdowns, while providing alternative outlets for stimming can offer individuals with autism a means of self-regulation.
Benefits of Stimming
- Helps individuals cope with stress
- Allows adjustment of sensory input
- Alleviates boredom
Strategies for Managing Meltdowns
- Create a calm and safe environment
- Identify triggers and minimize them
- Teach alternative coping mechanisms
- Encourage self-expression through communication tools
It is important to remember that stimming and meltdowns are natural responses for individuals with autism and should not be suppressed or punished. Instead, the focus should be on understanding and supporting individuals with autism in managing their unique sensory and emotional needs.
| Stimming | Meltdowns |
|---|---|
| Self-stimulatory behavior | Response to overwhelming stimuli |
| Repetitive hand flapping, rocking, spinning, or engaging with specific objects or textures | Crying, screaming, physical aggression, or shutting down completely |
| A means of coping with stress, adjusting sensory input, or alleviating boredom | Result from excessive sensory or emotional stimulation |
Causes and Risk Factors for Autism Spectrum Disorder
The exact causes of autism spectrum disorder are not yet fully understood. It is likely a combination of genetic and environmental factors. Genetic mutations and certain chromosomal issues have been linked to autism. Advancing parental age, exposure to certain drugs or chemicals during pregnancy, metabolic conditions, and other medical factors may also increase the risk. Vaccines have been extensively studied and do not cause autism.
Genetic Factors
Genetic factors play a significant role in the development of autism spectrum disorder. Studies have shown that certain genetic mutations and chromosomal abnormalities can increase the risk of autism. Additionally, having a family history of autism can also contribute to an individual's susceptibility to the disorder.
Environmental Factors
Environmental factors during pregnancy and early infancy may also influence the development of autism. Exposure to certain drugs, such as valproic acid and thalidomide, or chemicals, like pesticides and air pollutants, has been associated with an increased risk of autism. Maternal metabolic conditions, such as diabetes and obesity, have also been linked to a higher likelihood of having a child with autism.
Advancing Parental Age
Research suggests that parental age at the time of conception may be a contributing factor to autism spectrum disorder. Advanced paternal age, especially in fathers over 40, has been associated with a higher risk of autism in children. Maternal age may also play a role, although the effect is less pronounced compared to paternal age.
Medical Factors
Certain medical conditions and events can increase the likelihood of autism spectrum disorder. These include prenatal complications, such as maternal infections during pregnancy, fetal distress, and premature birth. Additionally, children born with certain genetic conditions, such as fragile X syndrome and tuberous sclerosis, are at a higher risk of developing autism.
Vaccines and Autism
Vaccines have been extensively studied, and there is clear scientific evidence that they do not cause autism. Multiple large-scale studies involving hundreds of thousands of children have consistently shown no link between vaccines and autism spectrum disorder. It is essential to rely on credible scientific research and expert consensus when addressing concerns about vaccines and their association with autism.
Conclusion
Understanding the symptoms and characteristics of autism spectrum disorder (ASD) is crucial in providing the necessary support and intervention for individuals with ASD. It is important to remember that ASD is a complex condition that affects each person in unique ways. While early diagnosis and intervention can be beneficial, it is essential to focus on the individual's needs rather than solely relying on a specific diagnostic label.
Autism spectrum disorder is not a one-size-fits-all diagnosis. Each person with ASD has their own strengths, challenges, and abilities that should be considered. By recognizing and respecting these individual differences, we can create a more inclusive society that supports and empowers individuals with autism.
As we continue to learn more about autism spectrum disorder, it is important to approach it with empathy, understanding, and acceptance. By promoting awareness and education about ASD, we can foster a more inclusive and supportive environment for individuals on the autism spectrum. Together, we can make a positive difference in the lives of those with autism and their families.
FAQ
What are the symptoms of autism spectrum disorder?
Symptoms of autism spectrum disorder can include problems with social interaction, communication difficulties, restricted and repetitive behaviors, delayed language and cognitive skills, sensory sensitivities, and atypical emotional reactions.
What were the different types of autism spectrum disorders before 2013?
Before 2013, the different types of autism spectrum disorders included Autistic Disorder (classic autism), Asperger's Syndrome (high-functioning autism), Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), Childhood Disintegrative Disorder, and Rett Syndrome.
What are the social interaction and communication symptoms of autism spectrum disorder?
Social interaction and communication symptoms can include avoidance of eye contact, difficulty understanding nonverbal cues, delayed speech development, repetitive speech patterns, trouble making friends, and difficulties starting or maintaining conversations.
What are the restricted and repetitive behaviors and interests associated with autism spectrum disorder?
Restricted and repetitive behaviors and interests can include lining up objects, repeating words or phrases, playing with toys in the same manner repeatedly, becoming upset with minor changes, engaging in repetitive body movements, and exhibiting hyper- or hypo-reactivity to sensory input.
What are some additional characteristics of autism spectrum disorder?
Additional characteristics of autism spectrum disorder can include delayed language, movement, or cognitive skills, hyperactivity, impulsivity, difficulties with emotional regulation, unusual eating and sleeping habits, gastrointestinal issues, and sensory sensitivities.
What are the symptoms of autism spectrum disorder in adults?
Symptoms of autism spectrum disorder in adults can include difficulty understanding others' thoughts and feelings, trouble making friends, anxiety in social situations, preference for routines and dislike of changes, challenges in expressing emotions, and heightened sensitivity to sounds, sights, or textures.
What are the symptoms of autism spectrum disorder in children?
Symptoms of autism spectrum disorder in children can include lack of eye contact, limited range of interests, repetitive behaviors, delayed language and motor skills, difficulty with social interactions and play, and adherence to specific routines.
What are stimming and meltdowns in relation to autism spectrum disorder?
Stimming, or self-stimulatory behavior, is common in individuals with autism and may involve repetitive hand flapping, rocking, spinning, or engaging with specific objects or textures. Meltdowns can occur when a person with autism becomes overwhelmed and may involve crying, screaming, physical aggression, or shutting down.
What are the causes and risk factors for autism spectrum disorder?
The causes of autism spectrum disorder are not fully understood, but it is likely a combination of genetic and environmental factors. Genetic mutations, advancing parental age, certain drugs or chemicals during pregnancy, metabolic conditions, and other medical factors may increase the risk.
How can understanding autism spectrum disorder symptoms help?
Understanding the symptoms of autism spectrum disorder can help in providing appropriate support and intervention for individuals with ASD. It is important to focus on the individual's needs rather than the specific label, as autism spectrum disorder is not a one-size-fits-all diagnosis.
Understanding Mild Autism Symptoms in Depth
Welcome to our comprehensive guide on mild autism symptoms, also known as autism spectrum disorder level 1. If you or someone you know has been diagnosed with mild autism, it's important to gain a thorough understanding of this condition. Mild autism is characterized by subtle traits and lower support needs, but it still presents challenges in social interactions, understanding social cues, and sensory experiences.
Diagnosing mild autism can often occur at an older age, sometimes even in adulthood, as the symptoms may not be immediately noticeable during early intervention screenings in childhood. However, early identification and support are crucial for individuals with mild autism to navigate their daily lives successfully.
In this guide, we will delve into the definition of mild autism, explore the characteristics of mild autism in both children and adults, discuss the diagnosis process, and examine the prevalence and possible causes of mild autism. We will also touch on common comorbidities associated with mild autism and provide insights into treatment and support options available for individuals with this condition.
By gaining a deeper understanding of mild autism, we can contribute to creating a supportive environment and promoting inclusivity for individuals with this condition. Stay with us as we shed light on the unique experiences of those with mild autism and how we can all play a role in their journey towards a fulfilling and successful life.
What is Mild Autism?
Mild autism, also referred to as autism spectrum disorder level 1, is a form of autism with lower support needs. Individuals with mild autism may excel academically but can face challenges in various areas of daily life.
People with mild autism often experience difficulties in social skills, sensory challenges, and organization. Social communication may be a struggle, and they may resist changes in routine. Additionally, individuals with mild autism may be hypersensitive to noise, smell, touch, and other sensations.
The level of support needed for individuals with mild autism varies from person to person. While some may require minimal assistance, others may benefit from structured support systems that help them navigate daily challenges.
Mild Autism Characteristics at a Glance
- Excelling academically
- Challenges with social skills and communication
- Difficulties adapting to changes in routine
- Hypersensitivity to sensory stimuli
Understanding the unique characteristics and support needs of individuals with mild autism is crucial in providing them with the necessary assistance to thrive.
| Characteristics | Impact |
|---|---|
| Challenges in social skills | Difficulty forming and maintaining relationships |
| Sensory sensitivities | Overwhelmed by certain sensory stimuli |
| Rigid adherence to routines | Anxiety and distress when routines are disrupted |
It is important to recognize and support individuals with mild autism in order to promote their well-being and ensure they have the tools to succeed in their daily lives.
Characteristics of Mild Autism in Children
Children with mild autism may exhibit a range of traits that can provide early signs of their condition. It's important to recognize these characteristics to facilitate timely intervention and support. Here are some common traits associated with mild autism in children:
Social Interaction and Communication
- Difficulty with eye contact
- Appearing distant or "in their own world"
- Challenges in understanding others' perspectives
- Struggles with social situations and forming relationships
Routines and Flexibility
- Rigid adherence to routines
- Difficulty adapting to changes
Behavior and Interests
- Repetitive behaviors
- Limited range of interests
Sensory Sensitivities
- Sensory sensitivities, such as being hypersensitive or hypo-sensitive to noises, smells, touch, or other sensations
It's essential to note that the intensity and expression of these traits may vary among children with mild autism. Early recognition of these characteristics can expedite appropriate support and effective strategies to help children with mild autism thrive.
| Characteristics | Description |
|---|---|
| Social Interaction and Communication | Difficulty with eye contact, appearing distant or "in their own world," challenges in understanding others' perspectives, struggles with social situations and forming relationships |
| Routines and Flexibility | Rigid adherence to routines, difficulty adapting to changes |
| Behavior and Interests | Repetitive behaviors, limited range of interests |
| Sensory Sensitivities | Hypersensitivity or hypo-sensitivity to noises, smells, touch, or other sensations |

Characteristics of Mild Autism in Adults
Adults with mild autism often exhibit similar traits to children, although their coping mechanisms and masking strategies may make their condition less noticeable. Here are some common characteristics of mild autism in adults:
Social Challenges:
- Difficulty relating to others
- Challenges in maintaining friendships
- Difficulties with back-and-forth communication
Expressive Difficulties:
- Trouble expressing oneself verbally
Sensory Sensitivities:
- Strong need for routine and dislike of change
- Anxiety in social situations
Intense Interests:
- Intense interests in specific subjects
Average to Above-Average Intelligence:
- Intellectual capabilities ranging from average to above-average intelligence
| Characteristic | Description |
|---|---|
| Social Challenges | Difficulty relating to others and maintaining friendships |
| Expressive Difficulties | Trouble expressing oneself verbally |
| Sensory Sensitivities | Strong need for routine and dislike of change, anxiety in social situations |
| Intense Interests | Intense interests in specific subjects |
| Average to Above-Average Intelligence | Intellectual capabilities ranging from average to above-average intelligence |
Diagnosis of Mild Autism
Diagnosing mild autism can be challenging, both in adults and children. Adults with mild autism may have developed masking strategies or may have been missed during childhood screenings, making it harder to identify their condition. For adults, evaluations conducted by professionals specializing in adult autism are often necessary to determine the presence of autism traits.
In children, the diagnosis of mild autism typically involves assessments conducted by child psychologists, child psychiatrists, or developmental pediatricians. These assessments comprehensively evaluate the child's behavioral, social, and communication patterns to determine if they align with the characteristics of mild autism.
It is crucial to conduct a thorough evaluation when diagnosing mild autism, as it helps individuals receive appropriate support and interventions tailored to their needs. By understanding the behavioral, social, and communication patterns, professionals can provide targeted strategies and therapies to help individuals with mild autism thrive.
| Diagnosing Autism in Adults | Diagnosing Autism in Children | |
|---|---|---|
| Evaluations | Conducted by professionals specializing in adult autism | Assessments by child psychologists, child psychiatrists, or developmental pediatricians |
| Focus | Evaluating presence of autism traits | Comprehensive evaluation of behavioral, social, and communication patterns |
| Significance | Helps individuals receive appropriate support and interventions | Provides a foundation for targeted strategies and therapies |
Missed Autism Diagnoses
Undiagnosed autism in adults is not uncommon, and there are several reasons why mild autism may go unnoticed or missed. Understanding these reasons can help shed light on the challenges faced by individuals with undiagnosed autism.
1. Traits overlooked in assigned females: Assigned females with mild autism may have their traits overlooked or misinterpreted. Autism symptoms can present differently in girls and women, leading to missed diagnoses. The focus on male-dominated diagnostic criteria and studies has contributed to this oversight.
2. Masking and coping strategies: Individuals with mild autism often develop masking and coping strategies to camouflage their autistic traits. They may mimic neurotypical behavior to fit into social norms, making their autism less noticeable. These strategies can make it challenging for professionals and even the individuals themselves to recognize the underlying autistic traits.
3. Misdiagnosis as mental health conditions: Mental health diagnoses such as anxiety and depression may be mistaken for autism or be results of autistic burnout, a state of exhaustion experienced by autistic individuals due to the demands of navigating a neurotypical world. The similarities between these conditions can complicate the diagnostic process.
It is important to improve awareness and understanding of the unique presentations of autism in different individuals, especially in adults. By addressing these barriers to diagnosis, we can create a more inclusive and supportive environment for individuals with undiagnosed autism.
| Reasons for Missed Autism Diagnoses |
|---|
| Traits overlooked in assigned females |
| Masking and coping strategies |
| Misdiagnosis as mental health conditions |
Prevalence of Adult Autism
Understanding the prevalence of adult autism is essential for raising awareness and ensuring appropriate support for individuals on the autism spectrum. While the prevalence of autism is commonly associated with children, it is important to recognize that adults can also be affected by this developmental disorder.
Research suggests that the prevalence of autism among adults is similar to that among children, with an estimated 1-3% of the adult population being on the autism spectrum. This means that there are millions of adults worldwide who may have autism but may be undiagnosed or unaware of their condition.
The reasons for undiagnosed autism in adults can vary. Autism traits may present differently in adults, making recognition and diagnosis more challenging than in children. Additionally, many adults with autism have developed masking strategies or coping mechanisms to hide their symptoms, further contributing to underdiagnosis.
Prevalence of Adult Autism in India
In India, the prevalence of adult autism remains a topic of ongoing research. Limited studies have been conducted on the prevalence of autism in this specific population, but it is believed to be consistent with the global estimates of 1-3%. The lack of awareness and understanding surrounding adult autism in India may contribute to a significant number of undiagnosed individuals.
Efforts are being made to improve the recognition and diagnosis of autism in adults in India. Increased awareness among healthcare professionals, educators, and the general public is crucial for identifying and supporting adults with autism and ensuring their access to appropriate resources and services.
| Country | Prevalence of Adult Autism |
|---|---|
| United States | 1-3% |
| United Kingdom | 1-3% |
| India | Research ongoing |
As awareness and understanding of adult autism continue to grow, it is hoped that more individuals will be accurately diagnosed and receive the support they need to thrive.

Possible Causes of Mild Autism
Mild autism, also known as autism spectrum disorder level 1, is thought to have various contributing factors. Research suggests that genetic factors, environmental influences, and brain changes play a role in the development of mild autism.
Genetic studies have identified specific gene mutations associated with autism. These mutations can affect the development and functioning of the brain, leading to the manifestation of autistic traits. Although there isn't one single gene responsible for autism, the presence of certain genetic variations increases the likelihood of developing the condition.
Differences in brain structure and function have also been observed in individuals with autism. Brain imaging studies have shown that there are distinct changes in the structure and connectivity of the brain in people with autism. These changes can affect how the brain processes and interprets information, leading to difficulties in social interaction, communication, and sensory experiences.
Furthermore, researchers are exploring the role of neuroinflammation and neurotransmission anomalies in the development of mild autism. Neuroinflammation refers to inflammation in the brain, which can disrupt normal brain development and functioning. Similarly, abnormalities in neurotransmission, the process by which nerve cells communicate, can impact the way information is transmitted and processed in the brain.
Understanding the causes of mild autism is essential for developing effective interventions and support strategies for individuals with the condition. By identifying the underlying factors contributing to autism, researchers can pave the way for targeted treatments and therapies that address the specific needs of individuals with mild autism.
Common Comorbidities in Mild Autism
Individuals with mild autism may experience various comorbidities that can impact their mental and physical health. It is important to recognize and address these comorbidities to provide comprehensive support for individuals with mild autism.
Mental Health Issues
Mental health issues are commonly associated with mild autism. Individuals with mild autism may be more prone to:
- Anxiety disorders
- Mood disorders
- Obsessive-compulsive disorder
Mental health challenges can significantly affect the overall well-being and quality of life for individuals with mild autism.
Physical Health Issues
Physical health problems can also be prevalent in individuals with mild autism. Some common physical health issues include:
- Sleep disturbances
- Gastrointestinal issues
- Epilepsy
- ADHD
It's essential to address these physical health concerns alongside the management of mild autism symptoms to ensure optimal health and functioning.
Treatment and Support for Mild Autism
While there is no cure for mild autism, there are various treatment options and support available to help individuals manage their symptoms and improve their quality of life. Treatment strategies for mild autism focus on addressing the specific challenges and needs of the individual.
Behavioral Therapies
Behavioral therapies, such as Applied Behavior Analysis (ABA), can be highly effective in helping individuals with mild autism develop essential life skills and improve their social interactions. ABA involves breaking down complex tasks into smaller, more manageable steps and using positive reinforcement to encourage desired behaviors.
Social Skills Training
Social skills training programs provide structured learning opportunities for individuals with mild autism to develop and enhance their social communication skills. These programs may involve role-playing, group activities, and real-life scenarios to help individuals navigate social interactions and improve their relationships.
Sensory Integration Therapy
Sensory integration therapy focuses on helping individuals with mild autism better process and respond to sensory information. It involves engaging in activities that stimulate the senses, such as swinging, jumping, or playing with textured materials, to help individuals regulate their sensory experiences and improve their sensitivity to sensory inputs.
Coping Strategies and Support
Support from professionals, family members, and a supportive environment plays a crucial role in managing mild autism symptoms. Professionals can provide guidance and teach individuals effective coping strategies to handle stress, anxiety, and sensory challenges. Family members and peers can offer understanding, patience, and encouragement, creating a positive and inclusive support system.
Managing mild autism symptoms requires a holistic approach that takes into account the unique needs and strengths of each individual. With the right treatment and support, individuals with mild autism can lead fulfilling lives and reach their full potential.
Conclusion
Understanding mild autism, also known as autism spectrum disorder level 1, is crucial in providing the necessary support for individuals with this condition. Although mild autism may have subtle traits that can go unnoticed, early identification is key to helping individuals navigate their social interactions, sensory challenges, and daily activities.
Each person's experience with mild autism is unique, and it is essential to recognize and respect their individual needs. By understanding the characteristics of mild autism and providing appropriate support, we can make a positive impact on the lives of individuals with this condition.
Early identification and intervention play a significant role in ensuring that individuals with mild autism receive the support they require. By identifying and addressing their needs at an early stage, we can help them develop essential skills, improve their overall well-being, and facilitate a fulfilling and successful life. Through empathy, understanding, and early support, we can create a more inclusive society where individuals with mild autism can thrive.
FAQ
What is mild autism?
Mild autism, also known as autism spectrum disorder level 1, is a form of autism with lower support needs. People with mild autism may excel academically but struggle with social skills, sensory challenges, and organization.
What are the characteristics of mild autism in children?
Children with mild autism may display traits such as difficulty with eye contact, rigid adherence to routines, challenges in understanding others' perspectives, struggles with social situations and relationships, repetitive behaviors, limited range of interests, and sensory sensitivities.
What are the characteristics of mild autism in adults?
Adults with mild autism may exhibit traits such as difficulty relating to others, challenges in maintaining friendships, difficulties with communication, a strong need for routine, anxiety in social situations, intense interests in specific subjects, and average to above-average intelligence.
How is mild autism diagnosed?
Diagnosing mild autism requires a comprehensive evaluation of behavioral, social, and communication patterns. Professionals specializing in adult autism may conduct evaluations in adults, while assessments by child psychologists, child psychiatrists, or developmental pediatricians are common in children.
Why are missed autism diagnoses common?
Mild autism may go undiagnosed or missed for several reasons, including differences in how autistic traits present in females, masking strategies adopted by individuals with mild autism, and mistaken mental health diagnoses.
What is the prevalence of autism in adults?
The prevalence of autism among adults is estimated to be 1-3% of the adult population, with many adults being undiagnosed or unaware of their condition due to differences in the presentation of autism traits.
What are the possible causes of mild autism?
Mild autism is believed to have multifactorial causes, including genetic factors, environmental influences, brain changes, neuroinflammation, and neurotransmission anomalies.
What are common comorbidities in mild autism?
Individuals with mild autism may be more likely to experience comorbidities such as anxiety disorders, mood disorders, obsessive-compulsive disorder, sleep disturbances, gastrointestinal issues, epilepsy, and ADHD.
What treatments and support are available for mild autism?
While there is no cure for mild autism, appropriate support and interventions such as behavioral therapies, social skills training, sensory integration therapy, and coping strategies can help individuals manage their symptoms and improve their quality of life.
How does early identification and support impact mild autism?
Early identification and support are crucial in helping individuals with mild autism navigate social interactions, sensory challenges, and daily life activities, contributing to a fulfilling and successful life.