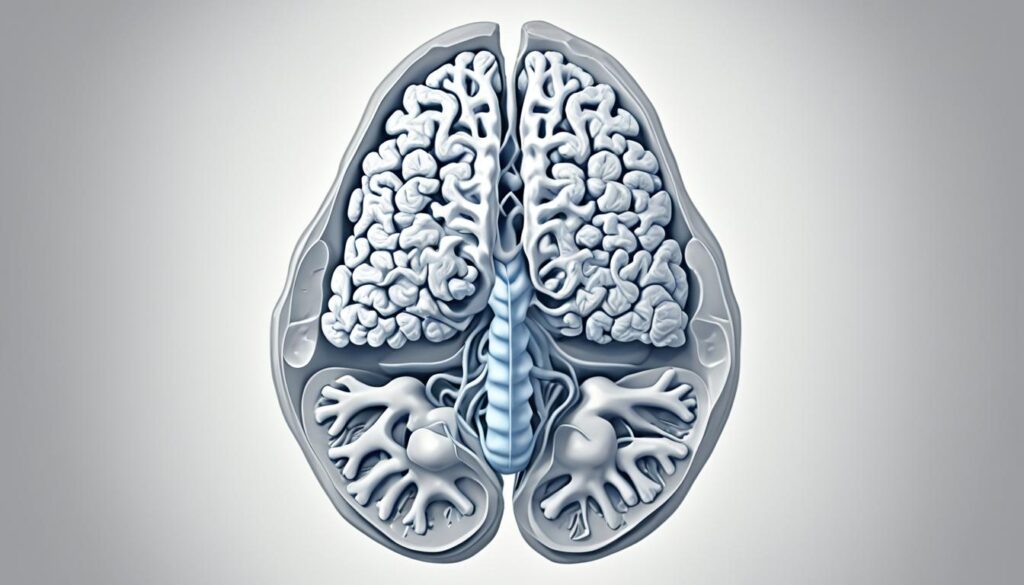
Arnold Chiari Malformation (CM) is a condition where brain tissue extends into the spinal canal, often due to a structural defect in the skull. It primarily affects the lower part of the brain called the cerebellum. Radiology plays a critical role in detecting and managing this condition. This guide explains what CM is, how radiologic techniques help in diagnosis and treatment, and what to expect during and after surgery.
Table of Contents
ToggleWhat is Arnold Chiari Malformation?
Chiari Malformations are grouped into several types based on severity:
- Type I (CM-1): The cerebellar tonsils extend into the spinal canal. Most common and typically diagnosed in teens or adults.
- Type 1.5: Includes the brainstem along with the cerebellar tonsils.
- Type 0: Involves syringomyelia without tonsillar herniation.
- Type II (CM-2): More severe; involves brainstem and cerebellum and is often detected at birth.
- Type III: Extremely rare and involves a portion of the brain protruding through an opening in the skull.
Each type has unique features that are best identified using radiological imaging, especially MRI.
How Radiology Helps
Radiologic imaging is essential to diagnosing and managing Arnold Chiari Malformation. It helps detect abnormal brain structures, track cerebrospinal fluid (CSF) flow, and identify related conditions like hydrocephalus and syringomyelia.
Imaging Techniques:
- MRI: Most common tool for identifying CM. Offers detailed images of brain and spinal tissues.
- Cine MRI: Shows real-time CSF flow. Useful for surgical planning.
- Phase-Contrast MRI: Measures CSF movement through the skull.
- Ultrasound: Used prenatally but limited in detail.
- CT Scan: Good for evaluating bone structure but uses radiation.
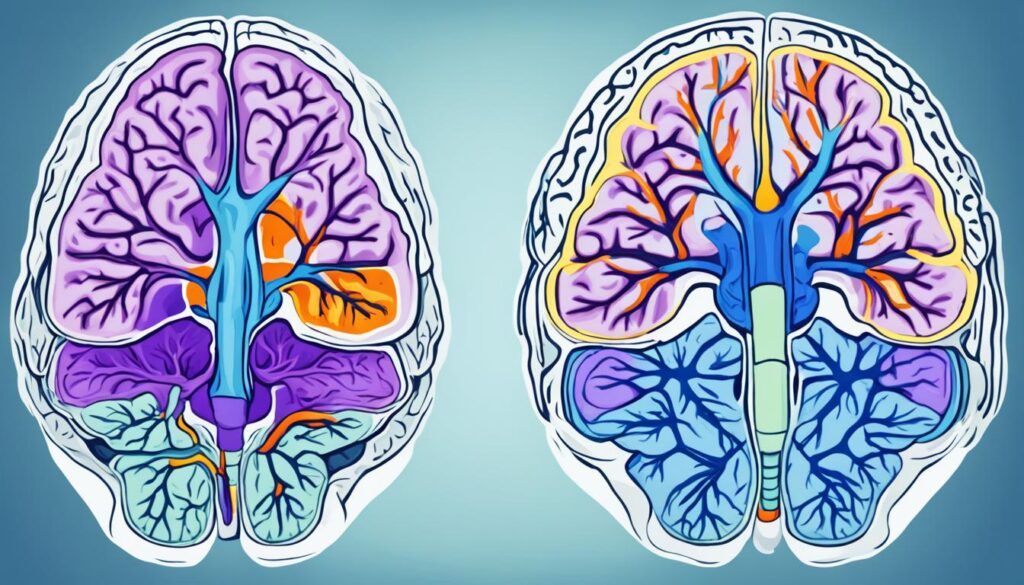
CM-1: Key Radiologic Features
CM-1 is the mildest and most common form. It is usually diagnosed when symptoms appear in late childhood or adulthood.
What to Look For:
- Cerebellar Tonsillar Herniation: More than 5 mm below the foramen magnum.
- Syringomyelia: Fluid-filled cavity in the spinal cord.
- Small Posterior Fossa: Less space for brain tissue at the skull base.
These signs are best detected with MRI, the gold standard in Arnold Chiari Malformation Radiology.
CM-2: What the Scans Show
More complex than CM-1, CM-2 typically appears with spina bifida. Radiology reveals:
- Downward displacement of brainstem and cerebellum
- Hydrocephalus (fluid build-up in the brain)
- Underdeveloped cerebellum (hypoplasia)
- Enlarged ventricles in the brain
MRI is essential for identifying these abnormalities, and fetal imaging can spot CM-2 before birth.
Advanced Radiologic Techniques
Arnold Chiari Malformation Radiology continues to evolve:
- Diffusion Tensor Imaging (DTI): Tracks white matter to assess brain function.
- Cine MRI: Helps plan surgery by showing CSF blockages.
- 3D MRI: Offers a complete view of skull and brain structure.
These methods improve accuracy and reduce the risk of misdiagnosis.
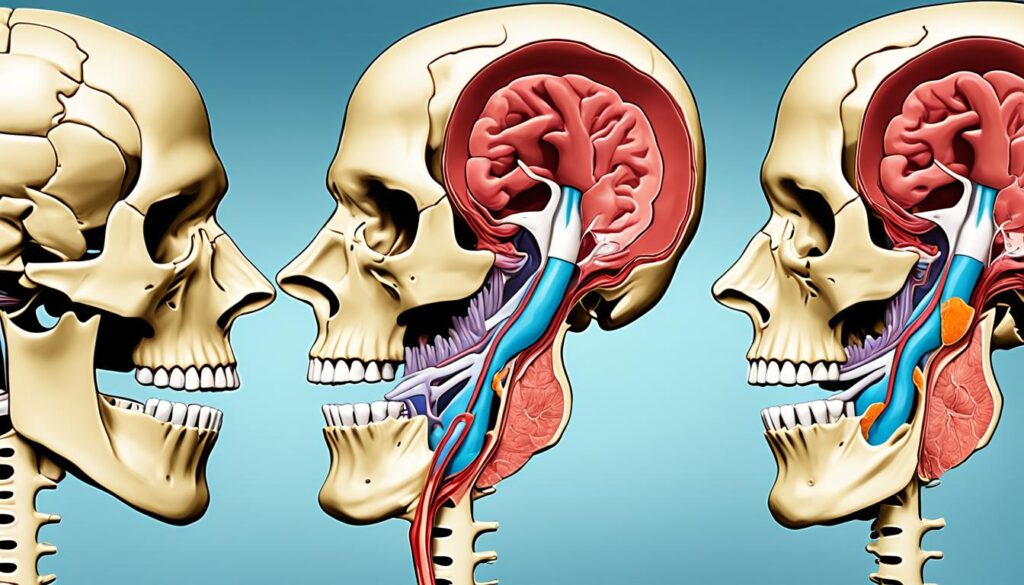
Radiology During Surgery
When symptoms become severe, surgery is needed. The most common procedure is posterior fossa decompression, where a small section of skull is removed.
Role of Radiology:
- Guides surgical planning
- Confirms that herniation is reduced
- Monitors healing after surgery
Post-Surgical Imaging
Even after surgery, radiology continues to play a role:
- MRI scans track recovery and ensure fluid flow is restored.
- Imaging can detect complications like CSF leaks or infections early.
Common Complications:
| Issue | How It’s Detected |
| CSF Leak | MRI shows fluid outside normal spaces |
| Infection | May show as swelling or fluid buildup |
| Re-herniation | MRI reveals tonsils dropping again |
Frequently Asked Questions
Q: Can Chiari Malformation be diagnosed before birth?
A: Yes. CM-2 can often be spotted using ultrasound or fetal MRI.
Q: What is the main test for diagnosing CM?
A: MRI is the most accurate tool, especially with advanced sequences.
Q: How is CM-1 treated?
A: Many cases don’t need surgery. When symptoms worsen, decompression surgery helps relieve pressure.
Q: What symptoms suggest CM?
A: Headache, balance issues, neck pain, numbness, or difficulty swallowing.
Q: Is it possible to live a normal life with CM?
A: Many people with CM-1 live symptom-free. Treatment improves outcomes.
Final Thoughts
Arnold Chiari Malformation Radiology offers life-changing insights. Whether it’s diagnosing a child before birth or guiding a life-saving surgery, imaging is the key to better outcomes. With advancements in MRI and related technologies, doctors can now see more clearly, act more precisely, and offer hope to patients and families.
If you or someone you know has symptoms of CM, talk to a neurologist and ask about imaging tests. Early detection can make all the difference.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




