Guillain-Barré syndrome is a rare autoimmune condition in which your immune system mistakenly attacks the nerves that control movement and sensation. This sudden nerve damage can lead to tingling, weakness, and in some cases, temporary paralysis that spreads upward through the body.
Symptoms can worsen quickly, and most people survive and recover with proper treatment. The life expectancy of Guillain-Barré syndrome today is far better than in the past.
Table of Contents
ToggleWhat Is Guillain-Barré Syndrome?
Guillain-Barré syndrome (GBS) is a rare autoimmune disorder. “Autoimmune” means your own immune system (the body’s defense against germs) accidentally attacks healthy tissue. In GBS, it attacks peripheral nerves, which are the nerves that link your brain and spinal cord to your muscles and skin. When these nerves swell or lose their myelin coating (the protective layer around the nerve), signals slow down or stop. You then feel tingling, weakness, and in some cases, paralysis.
Most cases appear one to four weeks after a gut or breathing infection. GBS is rare, with only a few thousand cases each year in a large country like the United States. The trigger itself does not decide the life expectancy of Guillain-Barré syndrome . What matters more is how fast you reach the hospital, how early treatment starts, and how well doctors prevent complications.
How GBS Affects The Nervous System (Immune Attack On Nerves)
In many people, immune cells target the myelin sheath, the fatty coating that helps nerve signals move quickly. When myelin peels away, messages between brain and muscles slow down. This leads to loss of reflexes, tingling, and rising weakness. Reviews from NIH show that this “active” phase usually peaks within about four weeks.
In other people, the attack hits the axon, the core part of the nerve fiber. Axon damage heals more slowly and can leave lasting weakness. This often means a longer ICU stay and more rehab. In older adults, this pattern can slightly reduce the life expectancy of Guillain-Barré syndrome , because it raises the risk of issues like infections and blood clots in the early months, not because the nerves themselves shorten life.
Variants Of Guillain-Barré Syndrome (AIDP, AMAN, Miller Fisher)
Doctors group GBS into variants based on how the nerves are damaged. The most common in North America and Europe is acute inflammatory demyelinating polyneuropathy (AIDP). Weakness usually starts in the legs and climbs upward, and reflexes fade. AIDP often responds well to treatment with IVIG or plasma exchange, and most survivors have a life expectancy of Guillain-Barré syndrome similar to people their age who never had GBS.
Acute motor axonal neuropathy (AMAN) and other axonal forms are more common in parts of Asia and Latin America. They tend to cause more sudden and severe weakness and more frequent need for ventilation. Yet many people with AMAN still regain walking over time.
Miller Fisher syndrome, another variant, mainly affects eye muscles, balance, and reflexes. Long-term follow-up suggests that the life expectancy of Guillain-Barré syndrome in Miller Fisher cases is close to normal when early treatment and rehab are available.
Who Is Most At Risk For Developing GBS?
You can develop GBS at any age, but it is more common after age 50, and men are affected slightly more often than women. Many cases follow infections such as Campylobacter jejuni gut infection or viral illnesses like flu or certain respiratory viruses. Vaccine-linked GBS is rare. CDC vaccine safety reviews show that the overall risk of GBS after vaccines is very small compared with the benefit of preventing serious infections.
Having these risk factors does not guarantee you will get GBS. Most people with these infections never do. If you do develop GBS, age and other illnesses like heart disease or diabetes can increase the chance of ICU care and may slightly reduce the life expectancy of Guillain-Barré syndrome , but good monitoring and evidence-based treatment still give a strong chance of a long life.
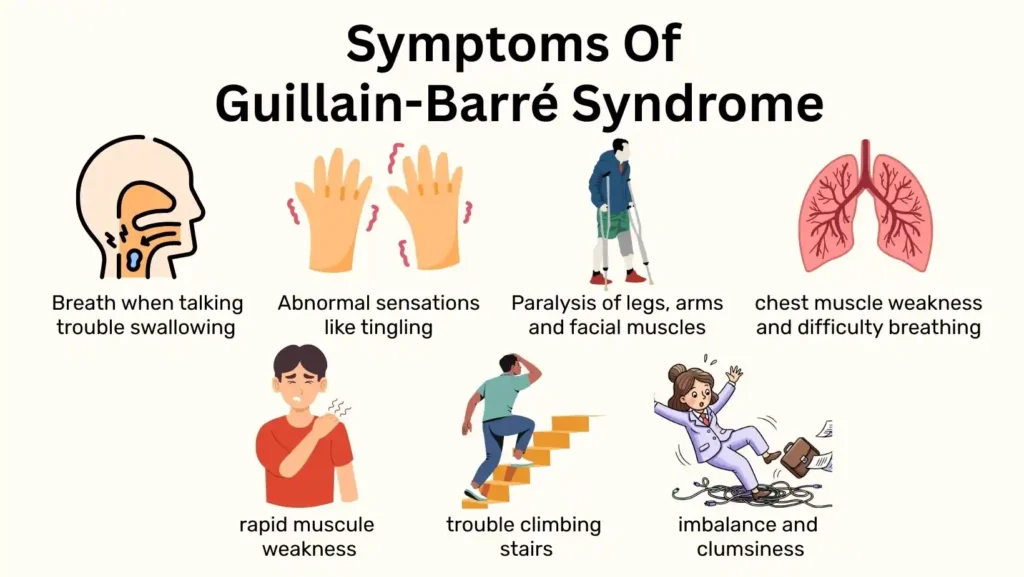
Symptoms Of Guillain-Barré Syndrome
The Symptoms of Guillain-Barré syndrome often start in your feet and legs and then spread upward. You may feel tingling in your toes, burning pain in calves, or a heavy feeling when you try to walk. These early Symptoms of Guillain-Barré syndrome reflect failing peripheral nerves.
Early Symptoms (Weakness, Tingling, Difficulty Walking)
In the early stage, you may notice pins and needles in your feet, trouble climbing stairs, or difficulty rising from a chair. Some people think they are just tired but rising weakness is a classic GBS pattern. Getting urgent medical review at this point matters, because early IVIG or plasma exchange can shorten the illness and support a better life expectancy of Guillain-Barré syndrome in the years that follow.
Progression Of Symptoms And When To Seek Emergency Care
Over hours or days, weakness can climb from legs to arms, face, and chest. You may drop objects, find it hard to smile, speak clearly, or keep your balance. Short breath when talking, trouble swallowing, or choking on water are red flags.
At this stage, you need emergency care, often in a hospital that can move you to ICU if needed. Studies show that early admission and close breathing checks reduce complications, which increases the life expectancy of Guillain-Barré syndrome .
Severe Symptoms (Paralysis, Breathing Difficulty)
In severe GBS, you may lose almost all movement in arms and legs. Breathing muscles can fail, so about one in five patients need a ventilator for a period of time. Even then, many ventilated patients later leave ICU, walk again, and live for many years.
For these survivors, the life expectancy of Guillain-Barré syndrome is shaped more by age, smoking, blood pressure, and other long-term risks than by the past episode of paralysis.
Symptoms That Affect Long-Term Life Expectancy
Some patterns during the illness link to higher early death risk. These include very fast onset to full paralysis, long need for mechanical ventilation, severe swings in blood pressure or heart rhythm, and repeated infections like ventilator-associated pneumonia. These problems can shorten the life expectancy of Guillain-Barré syndrome in the first few years, although many people with such complications still recover and live long lives.
Guillain-Barré Survival Rate
Across many countries, in-hospital death is often between 2-5%, which means the large majority survive the acute phase. Ventilated patients have a higher risk in the short term, but many of them regain walking and independence. These results explain why the long-term life expectancy of Guillain-Barré syndrome is often far better than families fear at diagnosis.
Current GBS Survival Statistics And Outcome Trends
Modern ICU care and early IVIG or plasma exchange have steadily improved the survival rate of Guillain-Barré over the last decades. Overall mortality is around 3-7%, with older age, severe weakness at entry, and lung or heart complications as the main risk factors. Long-term, Danish registry data show that after the first four years, the life expectancy of Guillain-Barré syndrome has increased.
Factors That Improve Survival (Early Treatment, Supportive Care)
Survival improves when you reach hospital early, get IVIG or plasma exchange within about two weeks of symptom onset, and receive strict monitoring of breathing and heart rhythm.
Simple steps such as preventing pneumonia, using blood thinners when safe, turning you in bed, and starting gentle physiotherapy reduce complications. Supportive care improves both the survival rate of Guillain-Barré and the life expectancy of Guillain-Barré syndrome , especially in older adults or those with other illnesses.
Factors That Increase Mortality Risk (Age, Respiratory Failure, Complications)
Older age, very severe initial weakness, the need for a ventilator, and complications such as sepsis or dangerous heart rhythm changes increase early death risk. These factors can shorten the life expectancy of Guillain-Barré syndrome in the first years after onset. Even so, they are risk markers, not fixed outcomes.
How ICU Care Impacts Survival For Severe GBS Cases
For the sickest patients, ICU care is central. Studies report that more than half of ICU patients have at least one major complication, most often pneumonia, yet careful breathing support, infection control, and early rehab help many survive and regain independent walking.
For these survivors, the life expectancy of Guillain-Barré syndrome often depends more on long-term habits and other diseases than on GBS itself, which is why neurologists stress follow-up and heart-healthy living after discharge.
GBS Recovery Timeline
When doctors describe the recovery timeline of GBS , they divide it into three phases. First is the worsening phase, usually up to four weeks. Second is the plateau phase, when symptoms stop getting worse. Third is the slow recovery phase, when nerves heal and strength returns over months or sometimes years.
Most people reach their weakest point within four weeks, then begin to improve. Studies show that more than 80% of people regain independent walking within about six months.
The nerve attack is brief, but healing is slow, which is why the recovery timeline of GBS can feel long while the life expectancy of Guillain-Barré syndrome remains good.
How Long Weakness And Paralysis Last
In GBS, weakness usually worsens for up to four weeks, then stops getting worse. Doctors call this the peak. After that, strength returns slowly. Mild cases may see clear gains in a few weeks.
More severe cases, especially those that needed a ventilator, may take many months before you notice great daily improvement. Most people who survive the acute stage walk again, even if early paralysis lasted several weeks.
What Percentage Of Patients Fully Recover
Research that compares many countries finds that about seven or eight out of ten people recover to normal or near normal strength. They may feel a bit more tired at the end of the day, yet they live active lives. Another group keeps some weakness or numbness but still walks on their own.
Only a small group remains dependent on a wheelchair or full-time help. This pattern fits with the recovery timeline of GBS , where function keeps improving for one to three years after the first attack in some patients.
Why Some Patients Recover Slower Than Others
Recovery depends on how much of the nerve axon was damaged, not just the myelin coating. Axon injury heals slowly and sometimes not completely. Older age, delayed treatment, and long stays in intensive care also slow recovery.
Some people develop joint stiffness, muscle wasting, or deep tiredness from months in bed. These problems then feed into the long-term effects of Guillain-Barré , which means you may feel weaker than your nerve tests suggest.
Long-Term Effects Of Guillain-Barré Syndrome
Even after the main symptoms of Guillain-Barré syndrome fade, some people have lasting problems. These long-term effects of Guillain-Barré vary a lot from person to person. They may be mild, such as slightly reduced ankle strength, or more serious, such as constant nerve pain or breathlessness on stairs. One in five people report some daily limits several years after GBS, even when they walk on their own.
Chronic Pain, Numbness, And Fatigue
Nerve pain can feel burning, stabbing, or electric. It often affects feet and hands. Numbness or tingling may stay even when strength returns. Fatigue is common and does not always match test results.
You might walk fine in clinic yet feel drained after a short trip to the shop. These long-term effects of Guillain-Barré may reflect lingering nerve damage and changes in how your brain handles pain and effort.
Persistent Weakness Or Mobility Difficulty
Some people notice that they cannot run as before, or they need to pull on a rail to climb stairs. Ankles and hips are common weak spots. If you were on a ventilator or in bed for weeks, muscles shrink and joints stiffen, which adds to nerve damage.
Even when full strength does not return, the right aids, such as braces or walking sticks, can help you stay independent. These problems rarely change the overall life expectancy of Guillain-Barré syndrome , yet they can affect work, driving, or sports choices.
Psychological And Emotional Effects After GBS
GBS arrives suddenly, often in someone who felt healthy a few days before. Many people later describe fear of being left alone, flashbacks to intensive care, or worry that every tingle means a new attack.
Anxiety and depression are more common in GBS survivors than in the general population. Counseling, peer support groups, and honest talks with your care team help you make sense of what happened and set real expectations for recovery. Addressing these hidden long-term effects of Guillain-Barré is as important as building muscle strength.
Long-Term Breathing Or Autonomic Issues
A smaller group has ongoing shortness of breath, especially when walking uphill, or sleep related breathing problems. Some keep trouble with blood pressure swings, fast heart rate, or stomach and bladder function. These issues link more to the severity of the original illness than to age alone.
Guillain-Barré Outcomes After Treatment
Guillain-Barré outcomes after treatment are how well you walk, breathe, work, and enjoy life months and years after IVIG or plasma exchange.
How IVIG And Plasma Exchange Improve Outcomes
IVIG supplies pooled antibodies from healthy donors that block harmful immune activity. Plasma exchange removes some harmful antibodies from your blood. Both methods shorten the time to peak weakness and speed early recovery.
They also reduce the chance that you will need a ventilator. These benefits lead to better Guillain-Barré outcomes after treatment , especially when started within about two weeks from the first symptoms.
Outcome Differences Between Treatment Types
Several trials show that IVIG and plasma exchange work about as well overall. Some newer research hints that plasma exchange may give slightly better results in certain very severe cases, but this depends on local skills and equipment, and evidence is still limited.
Doctors usually choose based on how fast they can start therapy, your medical background, and what your hospital can deliver safely. Both choices can support a good recovery timeline of GBS with strong chances for walking and self care.
Reducing Complications To Protect Life Expectancy
Good nursing care, early physical therapy, and strict infection control are just as important as IVIG or plasma exchange. Turning you often in bed, protecting your skin, and giving blood thinners when safe reduce clots and bed sores. Breathing exercises and early sitting help prevent pneumonia.
Rehabilitation Strategies And Long-Term Therapy
Rehab begins even in ICU. Therapists move your joints, sit you up in bed, and later help you stand and walk with support. After discharge, you may continue outpatient physiotherapy and occupational therapy. Treatment focuses on small, regular steps rather than sudden intense workouts. Pacing, where you balance effort and rest, helps manage fatigue.
Life Expectancy After Guillain-Barré Syndrome
After the early high-risk period, most survivors have a lifespan close to people of the same age without GBS, especially if they control blood pressure, sugar, and smoking.
What Research Shows About Long-Term Survival
Some studies report slightly higher death rates in the first few years, mainly due to heart and lung problems or other serious illnesses rather than direct nerve damage. By about four to six years after onset, the curve for survivors nearly matches the general population. This means that your long-term future often depends more on everyday health choices than on the old GBS episode itself.
How Age And Symptom Severity Influence Life Expectancy
Age over 60, very rapid onset, and need for ventilation link to higher risk of death in hospital and within the first few years. Younger adults with milder weakness and fast treatment tend to have excellent survival. In both groups, careful follow-up and heart-healthy habits give the best chance that the life expectancy of Guillain-Barré syndrome will match your peers.
Reasons Some Patients Experience Relapse Or Chronic GBS
True repeat episodes of classic GBS are rare. A small number of people develop a related condition called chronic inflammatory demyelinating polyneuropathy, known as CIDP. CIDP causes ongoing or repeated weakness and often needs long-term treatment with IVIG, steroids, or other immune drugs. Evidence about long-term survival in CIDP is still limited, but many patients manage a good quality of life with regular care.
Life Expectancy Differences Between Mild And Severe GBS
People who had mild GBS, did not need ventilation, and recovered walking early usually have long lives with little added risk. Those who had very severe paralysis, long ICU stays, or repeated infections face a higher risk in the early years.
Even so, many in this group live far beyond the first decade after GBS, especially when they stay active, treat blood pressure and cholesterol, and keep close contact with their medical team.
Improving Quality Of Life After GBS
Lifestyle Adjustments That Support Recovery
Simple steps such as regular light exercise, balanced meals, and good sleep patterns support nerve healing. Breaking tasks into shorter parts with rests in between helps you stay independent without crashing from fatigue. Staying in touch with your neurologist and therapist lets you adjust activity as your strength grows.
Preventing Long-Term Complications
You can lower future risk by keeping a healthy weight, stopping smoking if you smoke, and treating conditions such as diabetes and high blood pressure. Watching for mood changes and asking for help early prevents emotional strain from turning into major depression. These actions reduce the impact of long-term effects of Guillain-Barré on daily life.
Support Options For Patients And Caregivers
Support groups, whether local or online, connect you with others who understand what ICU and rehab feel like. Caregivers also need rest and time for their own health checks. When both you and your caregiver feel supported, it is easier to keep up with rehab and medical appointments and to protect health over the long term.
FAQs
Can People Fully Recover From Guillain-Barré Syndrome?
Many people make a full recovery, especially with early treatment and rehab, and later enjoy normal work, family life, and hobbies, even though some remember fatigue or minor weakness after hard activity.
How Long Does GBS Recovery Usually Take?
Recovery varies a lot. Many people improve within weeks, walk again within months, and continue to gain strength and stamina for one to three years, depending on age, severity, and other health conditions.
What Affects The Survival Rate Of Guillain-Barré Syndrome?
The survival rate of Guillain-Barré depends on age, speed of diagnosis, need for a ventilator, and complications such as pneumonia or sepsis, along with access to IVIG, plasma exchange, and intensive care.
Can Guillain-Barré Syndrome Come Back After Recovery?
True relapse is uncommon, yet a few people have a second episode years later or develop CIDP, a related chronic disease, so any new weakness or tingling needs fast medical review and nerve testing.
Do Most Patients Recover The Ability To Walk?
Yes, most people who survive the acute phase and complete rehab walk independently again, although some walk more slowly, tire faster, or need an aid such as a cane for longer distances outdoors.
When Should Someone With GBS Go To The ICU?
A person with GBS should go to ICU if breathing becomes hard, speech or swallowing changes, weakness spreads quickly, or heart rhythm and blood pressure change, since these signs can signal serious risk.
What Complications Increase The Risk Of Severe Outcomes?
The biggest risks come from pneumonia, sepsis, blood clots, severe swings in heart rhythm or blood pressure, and very long ventilation, which is why hospitals focus on early prevention and quick treatment.
Does Age Affect Guillain-Barré Syndrome Prognosis?
Yes, older adults have a higher chance of severe weakness, slower recovery, and complications, although many still survive and improve when they receive guideline-based care, careful monitoring, and structured rehabilitation.
What Percentage Of Patients Experience Long-Term Nerve Damage?
Studies suggest that about twenty to thirty percent of people keep some numbness, weakness, or pain years later, though the intensity varies, and many still manage work and family roles with adjustments.
Can GBS Be Fatal If Not Treated Quickly?
Without fast medical care, GBS can cause breathing failure, serious infections, or heart rhythm problems that may be fatal, which is why new, rapidly rising weakness always needs urgent hospital evaluation.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.