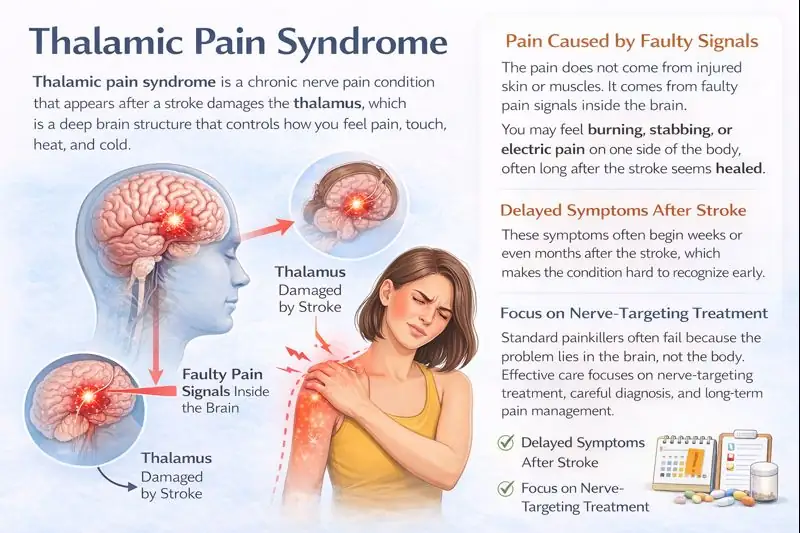
Thalamic pain syndrome is a chronic nerve pain condition that appears after a stroke damages the thalamus, which is a deep brain structure that controls how you feel pain, touch, heat, and cold.
The pain does not come from injured skin or muscles. It comes from faulty pain signals inside the brain. You may feel burning, stabbing, or electric pain on one side of the body, often long after the stroke seems healed. These symptoms often begin weeks or even months after the stroke, which makes the condition hard to recognize early.
Standard painkillers often fail because the problem lies in the brain, not the body. Effective care focuses on nerve-targeting treatment, careful diagnosis, and long-term pain management.
Thalamic Pain Syndrome Symptoms
The symptoms of thalamic pain syndrome (also known as central post-stroke pain) usually affect the side of the body opposite the damaged thalamus. The pain feels abnormal and intense. It often appears weeks or months after a stroke, which confuses many people.
Burning, Stabbing, Or Electric Shock–Like Pain
The most common symptom is burning pain. Many people describe it as fire under the skin. Others feel stabbing or sudden electric shock sensations. The pain can stay constant or come in waves. This happens because the thalamus no longer filters pain signals correctly. In thalamic pain syndrome , the brain sends pain messages even when there is no injury.
Pain Triggered By Light Touch, Temperature, Or Movement
Normal touch can hurt. Clothes brushing the skin may feel painful. Cold air can cause sharp pain. Warm water may feel scalding. This problem is called allodynia, which means pain from non-painful stimuli. It is a key part of the symptoms of thalamic pain syndrome and confirms that the pain is coming from the brain, not the skin.
Sensory Disturbances And Numbness
You may feel numbness mixed with pain. One area may feel dead, while another feels overly sensitive. This combination seems strange, but it is common. The thalamus processes sensation, so damage causes mixed signals. These changes are classic symptoms of thalamic pain syndrome .
Delayed Onset Of Symptoms After Stroke
Pain does not always start right away. It may begin months after the stroke. Brain rewiring after injury can slowly turn normal signals into pain signals. Delayed pain does not mean the condition is psychological. Delayed onset strongly supports thalamic pain syndrome .
Emotional And Sleep Disturbances Linked To Chronic Pain
Chronic pain affects sleep quality. Poor sleep increases pain sensitivity. Anxiety and depression may follow. These emotional effects do not cause the pain, but they worsen it. Managing mood and sleep is important when living with thalamic pain syndrome .
Causes Of Thalamic Pain Syndrome
The causes of thalamic pain syndrome always involve damage to pain-processing areas in the brain. The thalamus acts as a relay station. When it fails, pain perception becomes distorted.
Damage To The Thalamus After Ischemic Stroke
An ischemic stroke happens when a blood vessel is blocked. Brain cells lose oxygen and die. If the stroke damages the thalamus, pain control breaks down. Studies using MRI imaging show a strong link between thalamic injury and thalamic pain syndrome .
Hemorrhagic Stroke Affecting Sensory Pathways
A hemorrhagic stroke causes bleeding in the brain. Blood irritates and compresses nerve tissue. If bleeding affects the thalamus or nearby sensory pathways, abnormal pain signaling can develop. This is a known cause among the causes of thalamic pain syndrome .
Disruption Of Pain-Processing Neural Circuits
Pain travels through specific brain circuits. Stroke damage breaks these circuits. The brain tries to adapt by forming new connections. Sometimes these new pathways send constant pain signals. This process explains why thalamic pain syndrome can worsen over time.
Why Pain Persists Despite Tissue Healing
Skin heals, muscles recover, but brain pathways heal differently. Once central pain circuits become active, they may stay active. Research from neuroscience journals shows that central pain can continue even after the stroke area stabilizes. This explains long-lasting thalamic pain syndrome .
Risk Factors Increasing Likelihood Of Thalamic Pain
Large strokes raise the risk. Severe sensory loss increases risk. Poor blood pressure control increases risk. Diabetes also raises stroke damage severity. These factors increase the chance of developing thalamic pain syndrome .
Thalamic Stroke Pain Syndrome
Thalamic stroke pain syndrome describes pain caused by thalamic damage. It helps separate this condition from muscle or joint pain after a stroke.
How Thalamic Strokes Alter Pain Perception
The thalamus sorts sensory input before you feel it. Damage removes this filter. Normal sensations reach the brain in a distorted way. This explains why thalamic stroke pain syndrome feels intense and strange.
Difference Between Peripheral Pain And Central Pain
Peripheral pain comes from injured nerves outside the brain. Central pain comes from damaged brain tissue. This difference matters because common painkillers work poorly for thalamic stroke pain syndrome . Treatment must target nerve signaling, not inflammation.
Timeline Of Pain Development After Thalamic Stroke
Pain may start within weeks or months. Some people develop pain within six months. Others feel it later. Medical reviews from stroke rehabilitation research confirm that delayed pain is common in thalamic stroke pain syndrome .
Why Pain May Worsen Over Time
Repeated pain signals strengthen nerve pathways. Stress and poor sleep increase sensitivity. Without early treatment, pain intensity may increase. This explains why thalamic stroke pain syndrome can become more severe if untreated.
Burning Pain After Stroke Thalamus
Burning pain after a stroke is one of the most distressing experiences you may face after a thalamic injury. This pain feels intense, deep, and constant. Many people say it feels like heat trapped inside the body.
Why Burning Pain Is A Hallmark Symptom
Burning pain appears because the brain mislabels normal sensory signals as danger. The thalamus normally sorts pain, temperature, and touch. When damaged, it sends false alarms. This makes thalamic pain syndrome feel like ongoing burning even without injury.
Temperature Sensitivity And Allodynia
Cold water may feel icy and sharp. Warm water may feel too hot and a light touch may hurt. This reaction happens because pain pathways become overactive. In burning pain after a stroke thalamus , the brain reacts too strongly to harmless signals.
Pain Severity Fluctuations During The Day
Pain often worsens at night. Fatigue lowers pain tolerance. Poor sleep increases nerve sensitivity. Stress during the day can also increase symptoms. These patterns are common in thalamic pain syndrome .
Triggers That Intensify Burning Sensations
Cold weather increases pain. Emotional stress worsens symptoms. Lack of sleep raises pain levels. Avoiding triggers helps control burning pain after a thalamic stroke , even if pain never fully disappears.
Thalamic Pain Syndrome Treatment
There is no single cure, but treatment for thalamic pain syndrome focuses on reducing pain signals and improving daily function.
First-Line Medications For Central Post-Stroke Pain
Doctors usually start with medications that calm nerve activity. These drugs reduce abnormal firing in pain circuits. They do not repair brain damage, but they help control pain intensity in thalamic pain syndrome .
Role Of Antidepressants And Anticonvulsants
Some antidepressants affect pain pathways, not mood alone. Anticonvulsants stabilize nerve signals. Studies show these drugs help with central pain more than standard painkillers. They form the backbone of treatment for thalamic pain syndrome .
Limitations Of Traditional Painkillers
Drugs like acetaminophen or anti-inflammatory medicines target tissue pain. Central pain comes from the brain. This is why these drugs often fail in thalamic pain syndrome . Opioids may reduce pain in the short-term, but rarely help in the long-term.
Neuromodulation And Advanced Pain Therapies
Some patients try nerve stimulation therapies. These include spinal cord stimulation or deep-brain stimulation. These methods aim to interrupt pain circuits. Evidence is limited, but selected patients with severe thalamic pain syndrome may benefit.
Physical Therapy And Sensory Retraining
Gentle exposure to touch and temperature may help retrain the brain. Physical therapy also prevents stiffness and weakness. Therapy does not cure pain but supports overall treatment for thalamic pain syndrome .
Living With Thalamic Pain Syndrome
Daily life changes when pain becomes constant. Thalamic pain syndrome affects more than nerves. It affects routines, sleep, and mental health.
Impact On Quality Of Life And Daily Functioning
Pain limits movement, and simple tasks become tiring. Sleep problems increase fatigue. Many people reduce social activities. These changes are common with thalamic pain syndrome .
Psychological Coping Strategies For Chronic Pain
Pain affects the brain and emotions. Cognitive therapy helps you manage stress responses. Relaxation techniques reduce pain flares. Coping strategies do not mean the pain is imagined. They support people living with thalamic pain syndrome .
Importance Of Multidisciplinary Pain Management
Neurologists manage brain injury. Pain specialists adjust medication. Therapists support movement and coping. Team care improves outcomes for thalamic pain syndrome .
Long-Term Expectations And Prognosis
Some people improve over time. Others reach stable pain levels. Complete pain relief is rare. Early treatment improves long-term control of thalamic pain syndrome .
Diagnosis Of Thalamic Pain Syndrome
Diagnosis relies on careful symptom review and brain imaging rather than a single test. Many cases are missed early because pain starts late and mimics other post-stroke problems.
Clinical History And Neurological Examination
Doctors ask about pain type, timing, and triggers. Sensory testing checks touch and temperature response. These steps help confirm thalamic pain syndrome .
MRI And Imaging Findings Of Thalamic Injury
MRI scans show the stroke location. Damage to the thalamus supports diagnosis. Imaging helps rule out other causes of pain in thalamic pain syndrome .
Differentiating From Other Post-Stroke Pain Disorders
Joint pain comes from stiffness. Muscle pain comes from spasm. Central pain feels burning or electric. Correct diagnosis prevents wrong treatment in thalamic pain syndrome .
Challenges In Early Diagnosis
Pain may start late. Symptoms vary. Many doctors miss early signs. Awareness improves early diagnosis of thalamic pain syndrome .
Preventing Worsening Of Thalamic Pain Syndrome
While the brain injury cannot be reversed, steps can reduce pain progression. Early rehabilitation, trigger control, and stroke risk management help limit worsening symptoms.
Early Stroke Rehabilitation And Pain Control
Early therapy supports healthy brain adaptation. Early pain treatment prevents pain circuits from strengthening in thalamic pain syndrome .
Managing Blood Pressure And Stroke Risk Factors
High blood pressure increases stroke damage. Controlling risk factors protects remaining brain tissue. This matters for people with thalamic pain syndrome .
Avoiding Triggers That Exacerbate Symptoms
Cold exposure worsens pain. Stress raises pain levels. Trigger control reduces flare-ups in thalamic pain syndrome .
Importance Of Early Specialist Referral
Pain specialists recognize central pain faster. Early referral improves treatment success in thalamic pain syndrome .
When To See A Doctor For Thalamic Pain Syndrome
Certain pain changes signal the need for medical review. Ignoring worsening symptoms can delay treatment and reduce long-term pain control.
Pain Not Responding To Standard Treatment
Persistent pain needs specialist care. Do not accept uncontrolled pain with thalamic pain syndrome .
Rapid Worsening Of Burning Or Sensory Pain
Sudden changes need evaluation. New damage must be ruled out in thalamic pain syndrome .
New Neurological Symptoms
Weakness, vision loss, or speech changes require urgent care. Stroke risk remains in the thalamic pain syndrome .
FAQs
Is Thalamic Pain Syndrome Permanent?
Thalamic pain syndrome can last long-term. Some people improve with treatment. Others reach stable pain levels. Early care improves long-term pain control.
Can Thalamic Pain Syndrome Improve Over Time?
Yes. Brain adaptation may reduce pain. Medication, therapy, and coping strategies support improvement in thalamic pain syndrome over months or years.
Why Does Pain Appear Months After A Stroke?
Brain circuits reorganize slowly. This delayed rewiring can turn normal signals into pain in thalamic pain syndrome.
Is Thalamic Pain Syndrome The Same As Neuropathic Pain?
It is a type of central neuropathic pain. It differs from nerve damage outside the brain.
What Type Of Doctor Treats Thalamic Pain Syndrome?
Neurologists diagnose thalamic pain syndrome. Pain specialists manage long-term treatment and symptom control.
Why Does Pain Severity Fluctuate During The Day?
Fatigue, stress, and sleep quality affect nerve sensitivity. These factors influence daily pain levels in thalamic pain syndrome.
What Triggers Can Intensify Burning Pain Sensations?
Cold temperatures, emotional stress, and poor sleep often trigger burning pain after a thalamic stroke.
What Treatment Options Are Available For Thalamic Pain Syndrome?
Treatment for thalamic pain syndrome includes nerve-stabilizing medication, therapy, coping strategies, and advanced pain procedures for selected cases.
What Are First-Line Medications For Central Post-Stroke Pain?
Doctors usually prescribe nerve-targeting medications. Dosage varies by age, health, and pain severity in thalamic pain syndrome.
Why Are Traditional Painkillers Often Ineffective?
Traditional painkillers target tissue pain. Thalamic pain syndrome comes from abnormal brain signaling, so these drugs rarely provide relief.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




