Neck pain and headaches can really slow you down. They might come from infections, stress, or other health issues. If you’re feeling okay at home, that’s good. But watch out for a fever or if the pain gets worse. That could mean you need a doctor’s help.
Many people suffer from severe neck pain and headache base of skull, often without understanding why it happens or what truly helps. These pains can feel crippling especially when they interfere with your work, sleep, and daily life.
In this blog, we will break down the most effective treatments for severe neck pain and headache base of skull, explain what’s causing this pain, and show how to manage and prevent it for good. No fluff. Just real solutions, backed by medical science and explained in simple language you can actually understand.
Table of Contents
ToggleWhat’s Causing Your Neck and Skull Discomfort?
Your pain isn’t in your head. It often starts deep in the neck or at the base of the skull and radiates out. To treat it, you first need to know what parts of your body are involved and what’s triggering the discomfort.
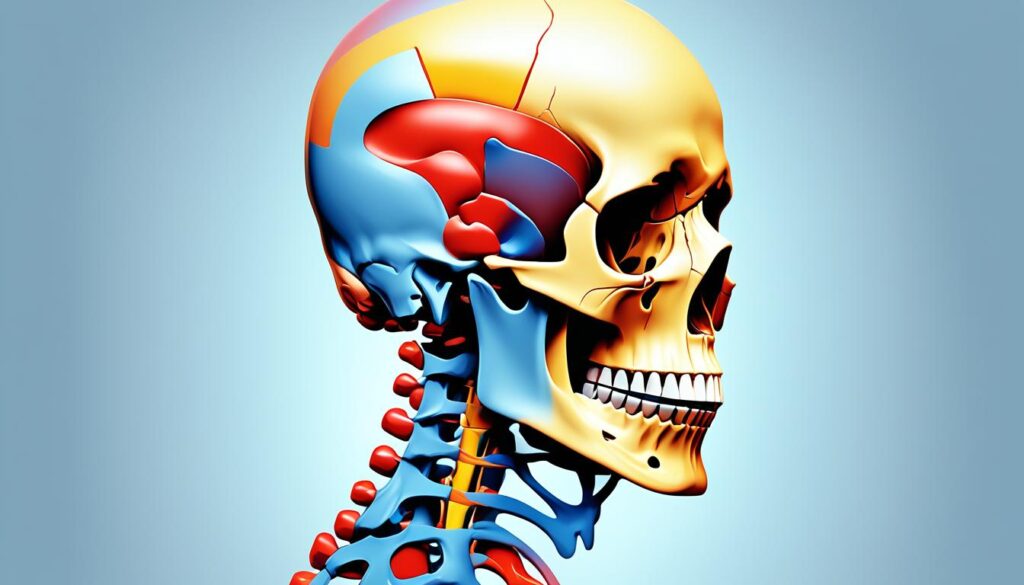
Anatomy of the Upper Neck and Skull Base
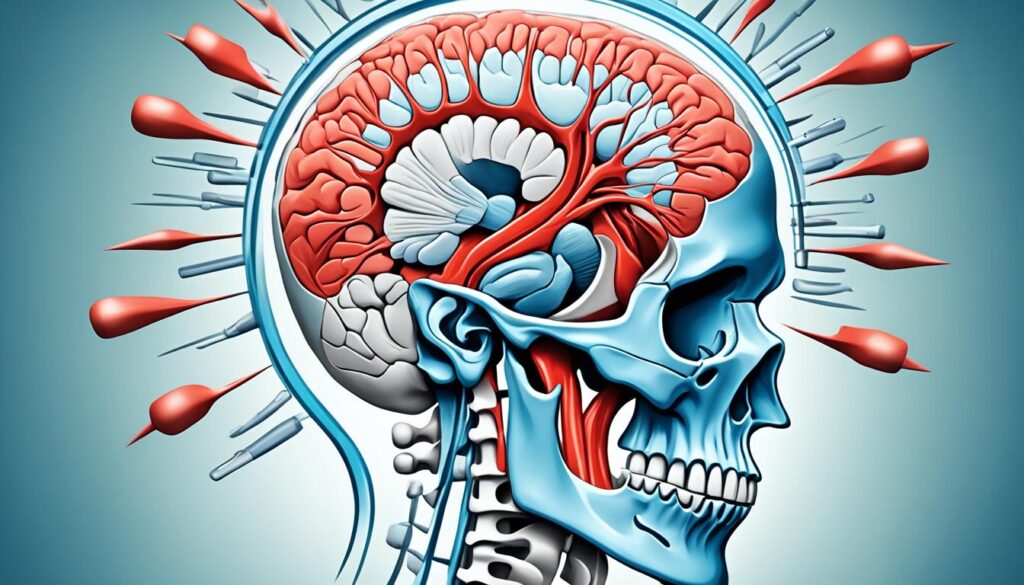
The base of the skull and upper neck is packed with sensitive structures that can all contribute to pain:
- Occipital nerves: These nerves run from the upper neck to the scalp. When irritated, they cause sharp or throbbing pain at the base of the skull.
- Cervical spine (C1–C3): The top vertebrae of your spine. Misalignment, disc issues, or arthritis here can lead to pressure and pain.
- Trapezius muscle: This large muscle stretches across your upper back and neck. Tension here can create headaches.
- Suboccipital triangle: A group of small muscles at the skull base, often tight or inflamed in people with chronic neck pain.
Understanding this setup helps pinpoint why the severe neck pain and headache base of skull feels the way it does.
Common Causes Behind the Pain
There isn’t just one cause. Your pain may be linked to multiple overlapping issues. Here are the most common ones:
- Occipital neuralgia: Irritation of the occipital nerves that causes stabbing or throbbing pain.
- Cervicogenic headache: Pain that starts in the neck but feels like a headache.
- Muscle strain or tension: Often from poor posture, stress, or long hours at a desk.
- Herniated disc: A slipped disc in the upper cervical spine can press on nerves.
- Poor posture/tech neck: Slouching over phones or computers strains neck muscles.
- Whiplash or trauma: Even minor accidents can throw off alignment and strain muscles.
- Arthritis or degenerative joint disease (DJD): Wear-and-tear in the cervical spine joints.
Stat: Nearly 20% of adults suffer from chronic neck pain, and up to 4% experience occipital headaches, according to the NIH.
Symptoms of Severe Neck Pain and Headache at the Base of Skull
Identifying your symptoms can help you understand whether you’re dealing with a deeper nerve issue or just muscle tension. Either way, the symptoms of severe neck pain and headache base of skull are hard to ignore.
How to Recognize a Suboccipital Headache
This type of headache has some signature signs:
- Throbbing or pulsing pain at the base of the skull
- Pain that radiates to the temples or behind the eyes
- Neck stiffness or difficulty turning the head
- Scalp sensitivity or tenderness when touched
- Visual problems or light sensitivity
- Nausea or dizziness during headache episodes
These headaches are often mistaken for migraines or sinus headaches, but their origin is actually neck-related.
Types of Headaches Caused by Neck Pain
Neck pain can lead to different types of headaches, like cervicogenic headaches and occipital neuralgia. It’s important to know how neck problems relate to these headaches for better treatment and relief.
Cervicogenic Headaches
Cervicogenic headaches start in the neck but move to the head. They are usually on one side and may make turning the neck uncomfortable. Studies show these headaches affect 0.4% to 4% of people, especially those aged 30 to 44.
These headaches can come from neck issues like arthritis, a slipped disc, or whiplash. Jobs that involve sitting a lot or sleeping in bad positions can also cause them.
Occipital Neuralgia
Occipital neuralgia is another headache type linked to neck pain. It happens when the occipital nerve in the neck gets pinched or irritated. People with this condition feel sharp, stabbing pain at the back of the head and scalp sensitivity.
Managing cervicogenic headaches and occipital neuralgia often means using medicine, physical therapy, and treatments like nerve blocks. Fixing the neck problems can help relieve these headaches.
Read → Cluster Headaches: How to treat
Types of Headaches That Lead to Neck Pain
Headaches and neck pain often go together. Certain headaches, like tension headaches and migraines, are common causes of neck pain.
Tension Headaches
Tension headaches are the most common type. They can make the neck hurt. These headaches feel like pressure or tightness around the forehead and neck.
The muscles at the base of the skull can get inflamed and sore. This adds to the pain.
Migraines
Migraines are a type of headache that can cause neck pain too. Often, people feel neck pain right when the migraine starts. Doctors aren’t sure if the neck pain causes the migraine or if it’s a symptom.
It’s important to understand how headaches and neck pain are linked. By finding the cause and getting the right treatment, people can feel better and live better lives.
Lifestyle Changes to Prevent Recurrence
Changing small habits can dramatically reduce the chance of future flare-ups.
Desk Ergonomics and Screen Time Limits
Adjusting your workstation setup can prevent strain:
- Keep screens at eye level to avoid forward head posture
- Use chairs with good lumbar support
- Take breaks every 30 minutes to move around
This is essential for neck pain caused by posture.
Sleep Position and Pillow Choice
The wrong pillow can worsen neck issues:
- Use a cervical pillow to support the natural curve of your neck
- Sleep on your back or side, not your stomach
- Avoid pillows that are too high or too firm
Hydration, Diet, and Magnesium
What you eat and drink affects how your muscles feel:
- Drink at least 2 liters of water daily
- Add magnesium-rich foods like spinach, almonds, and black beans
- Eat anti-inflammatory meals: fish, leafy greens, berries
Magnesium may help reduce chronic neck pain relief naturally.
Proven Medical Treatments for Severe Neck Pain and Headache Base of Skull
Once diagnosed, your treatment plan will likely include a combination of therapies. Let’s break down what works best for severe neck pain and headache base of skull.
Physical Therapy and Postural Training
Physical therapy is the cornerstone for long-term relief. It targets the root causes.
- Gentle neck stabilization exercises to strengthen deep muscles
- Myofascial release to loosen tight tissues
- Posture correction to fix slouching and forward head position
- Ergonomics training to adjust your workstation
Stat: A study in the Journal of Orthopaedic & Sports Physical Therapy found physical therapy reduced cervicogenic headache symptoms by over 70% in 6 weeks.
Medications
Short-term use of medication can help reduce inflammation and interrupt pain signals.
- NSAIDs like ibuprofen for swelling
- Muscle relaxants to ease tension
- Nerve pain medications like gabapentin
- Corticosteroid injections for occipital neuralgia treatment
These may not cure the condition but are very useful when pain flares.
Nerve Blocks & Injections
For cases that don’t respond to meds, injections can deliver targeted relief.
- Occipital nerve blocks: Inject anesthetic near the nerve to shut down pain.
- Trigger point injections: Calm overactive muscle fibers that generate referred pain
Stat: According to the American Migraine Foundation, occipital nerve blocks provide relief in 85% of patients with occipital neuralgia.
Advanced Interventions
In complex cases, these procedures may offer relief when others fail:
- Radiofrequency ablation (RFA) to deactivate pain-carrying nerves
- Spinal decompression therapy to reduce disc pressure
- Botox injections (off-label) to reduce muscle tension
These are usually done after imaging and evaluation by a specialist.

Seeking Professional Help
If you have ongoing or severe neck pain with headaches, you should get medical help. Look out for these red flags that mean you should see a doctor:
- Headache with fever, weight loss, confusion, or sudden start
- A change in your usual headache pattern
- Severe or ongoing neck pain and stiffness
- Pain that spreads down your arm
- Difficulty moving your head
It’s key to get professional help for [when to see a doctor for neck pain and headaches]. Your doctor will do a detailed check-up, order tests, and figure out what’s wrong. They can then make a plan to fix the main cause of your [red flags for seeking medical attention].
Cervicogenic Headaches: A Closer Look
Cervicogenic headaches come from a neck issue, not a head problem. They start at the back of the skull and move forward. You might feel stiff in the neck and find it hard to move it.
Symptoms of Cervicogenic Headaches
The main signs of cervicogenic headaches are:
- Pain on one side of the head, starting at the skull base and going to the forehead or eye
- Neck stiffness and less movement in the neck
- More pain when you move or change positions in your neck
- Sensitivity to light and sound
- Nausea or vomiting in some cases
Causes of Cervicogenic Headaches
Several neck issues can lead to cervicogenic headaches. These include:
- Whiplash: Quick, jerky neck movements, often from a car crash, can cause these headaches.
- Arthritis: Neck arthritis can irritate and inflame, leading to headaches.
- Neck Injuries: Neck muscle, tendon, or ligament injuries can also trigger headaches.
The pain comes from the neck and the trigeminal nerve working together. This mix sends pain signals to the head.
Diagnosing Cervicogenic Headaches
Diagnosing cervicogenic headaches can be tricky. They might seem like other headaches, like migraines or tension headaches. Your doctor will work hard to find the real cause by checking if your neck and head are connected to the pain.
Your doctor might do a detailed physical assessment. This means checking if moving your head and spine helps or changes your symptoms. They might also suggest nerve blocks to see if your neck really is the cause of your headaches.
Also, your doctor could order imaging tests, like an MRI. This scan looks at your neck’s bones, tissues, and nerves. It helps spot any problems, like disc issues or nerve damage, that might be causing your headaches.
With a full physical check-up, nerve blocks, and imaging tests, your doctor can pinpoint the cause of your cervicogenic headaches. Then, they can make a treatment plan to fix the problem.
Treatment Options for Cervicogenic Headaches
If you’re dealing with cervicogenic headaches, there are ways to find relief. The main goal is to fix the neck or spine issues causing the pain.
Physical Therapy
Physical therapy is often the first step for cervicogenic headaches. Experts in physical therapy can pinpoint the pain source. They’ll create a plan with exercises to help your posture, strengthen neck muscles, and improve flexibility.
Medications
Your doctor might suggest over-the-counter or prescription drugs for pain relief. Options include non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants. They can help ease the pain and discomfort from cervicogenic headaches.
Interventional Treatments
For severe or ongoing cervicogenic headaches, more advanced treatments might be needed. These include nerve blocks, radiofrequency ablation, and transcutaneous electrical nerve stimulation (TENS). In some cases, neuromodulation surgery to stimulate the occipital nerve could be an option.
The Pain Management NYC clinic in Midtown Manhattan offers advanced treatments for cervicogenic headaches. They work with each patient to find the best solution for neck pain and headaches.
Preventing and Managing Chronic Cervicogenic Headaches
If you have ongoing or frequent cervicogenic headaches, it’s key to work with your healthcare provider. Together, you can create a plan that might include physical therapy, medicine, and other treatments. This plan aims to fix the root causes and help you feel better over time.
Preventing these headaches can be done by keeping a good posture, making your workspace comfortable, and managing stress. By doing these things, you can lessen the number and intensity of cervicogenic headaches. This proactive approach helps you take charge of your health.
A study showed that up to 22% of people with ongoing headaches might have cervicogenic headaches. It’s important to know the signs like neck pain, limited neck movement, and shoulder pain. This knowledge helps doctors diagnose and treat the condition effectively.
Tests like X-rays, CT scans, and MRI scans can show what’s causing cervicogenic headaches. This info lets doctors make treatment plans just for you. These plans might include:
- Physical therapy to improve neck and shoulder movement, strengthen muscles, and help with posture
- Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), to help with pain and swelling
- Interventional treatments, like nerve blocks or radiofrequency ablation, to target specific nerve pain sources
Adding changes to your lifestyle, trying alternative therapies, and using home remedies like relaxation, yoga, and cognitive behavioral therapy can also help. These methods work alongside traditional treatments to manage cervicogenic headaches.
By working with your healthcare provider and using a variety of approaches, you can manage your chronic cervicogenic headaches. This can greatly improve your life quality.
When to See a Specialist for Severe Neck Pain and Headache Base of Skull
You’ve tried at-home care. You’ve taken meds. If pain still lingers, it’s time to see a professional.
Neurologist vs. Orthopedic vs. Pain Management Specialist
Each specialist has a unique role:
| Specialist | What They Do |
| Neurologist | Evaluates nerve-related pain and headaches |
| Orthopedic doctor | Handles bone and spine alignment issues |
| Pain specialist | Offers injections and long-term pain management |
Booking a visit with Dr. Chandril Chugh ensures you’re not left guessing.
Imaging Tests That May Be Needed
These tools help pinpoint the root cause of the problem:
- MRI to view nerves, discs, and soft tissues
- CT scan to examine bone structure and injury
- Nerve conduction tests to assess nerve function
Advanced imaging ensures your treatment is precise.
Conclusion
Severe neck pain and headache base of skull doesn’t have to rule your life. With the right approach, you can stop masking symptoms and actually solve the problem. Whether it’s nerve-related, posture-driven, or stress-induced, a neurologist like Dr. Chandril Chugh can guide you toward relief that lasts.
Dr. Chandril Chugh is a US-trained, board-certified neurologist known for helping patients overcome migraines, suboccipital headaches, tension-related pain, and complex nerve conditions.
If you’re tired of living with this pain, don’t wait. Book your consultation with Dr. Chugh today and get the expert care you need.
FAQ
What are some common causes of neck pain and headaches?
Neck pain and headaches can come from many things like infections, stress, and being sick. Poor posture, eye strain, and injuries can also cause these symptoms.
What are the different types of headaches that can be caused by neck pain?
Neck pain can lead to headaches like cervicogenic headaches, occipital neuralgia, tension headaches, and migraines.
How are cervicogenic headaches different from other types of headaches?
Cervicogenic headaches come from a neck problem. They cause pain on one side of the head, neck stiffness, and discomfort with certain neck movements.
What are some of the potential causes of cervicogenic headaches?
Cervicogenic headaches can come from things like whiplash, arthritis, neck sprains, or a neck fracture. These issues can affect the upper cervical vertebrae.
How can cervicogenic headaches be diagnosed?
Diagnosing cervicogenic headaches can be tough. Doctors might use a physical check-up, nerve blocks, and imaging tests to look at the neck’s bones, tissues, and nerves.
What are the treatment options for cervicogenic headaches?
Treatments for cervicogenic headaches aim to fix the root cause. Options include physical therapy, medicines, nerve blocks, radiofrequency ablation, TENS, and sometimes surgery.
When should someone seek medical attention for neck pain and headaches?
If you have a headache with fever, weight loss, confusion, sudden onset, or a change in your headaches, see a doctor. Look for signs like severe or ongoing neck pain, pain down the arm, or trouble moving your head.
How can home remedies and self-care measures help with neck pain and headaches?
Home remedies like better workplace setup, good posture, and quality sleep can ease headaches from neck pain. But, if these don’t work, you might need medical help.
What are some medical treatments for severe neck pain and headache at the base of the skull?
For severe neck pain and headaches, treatments might include nerve blocks, radiofrequency ablation, and TENS. In some cases, surgery might be an option.
How can chronic cervicogenic headaches be prevented and managed?
To prevent and manage chronic cervicogenic headaches, work with your doctor on a treatment plan. This might include physical therapy, medication, and other treatments. Keeping good posture and managing stress can also help reduce headaches.
Source Links
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.