Moyamoya disease is a rare but serious disorder of the brain’s arteries. It causes them to narrow or close, leading to the growth of new blood vessels. Patients can experience symptoms like strokes or bleeding in the brain. In this article, we will explore the latest in understanding, treatments, and breakthroughs for moyamoya disease.
Table of Contents
ToggleUnderstanding Moyamoya Disease
Moyamoya disease is a rare condition that affects the brain’s blood vessels. It’s known for the narrowing or blocking of important arteries. This narrowing forces the body to create new, smaller blood vessels.
These new vessels are called “moyamoya” vessels and are very fragile. While their exact cause is still unknown, both genes and immune issues might play a part.
What is Moyamoya Disease?
Moyamoya disease slowly blocks or narrows the blood vessels to the brain. This forces the brain to build a network of tiny and weak blood vessels. These new vessels are not strong. They can get even smaller, risking breakage and causing health problems.
Causes and Risk Factors
The main reasons behind moyamoya disease are not clear. But, scientists know that genes and environmental factors might be involved. A gene called RNF213 is often linked to the disease, especially in Asian people.
Autoimmune issues and some medical conditions, like neurofibromatosis type 1 and Down syndrome, can also raise the risk.
Symptoms and Diagnosis
Moyamoya disease can show in various ways, like strokes or bleeding in the brain. People with the condition may have headaches, seizures, or problems with movement. How bad these symptoms are can change, based on the blood vessels’ condition.
Doctors usually diagnose it with tests that look at the blood vessels in the brain. Tests like MRA and cerebral angiography can spot the typical changes in the blood vessels.
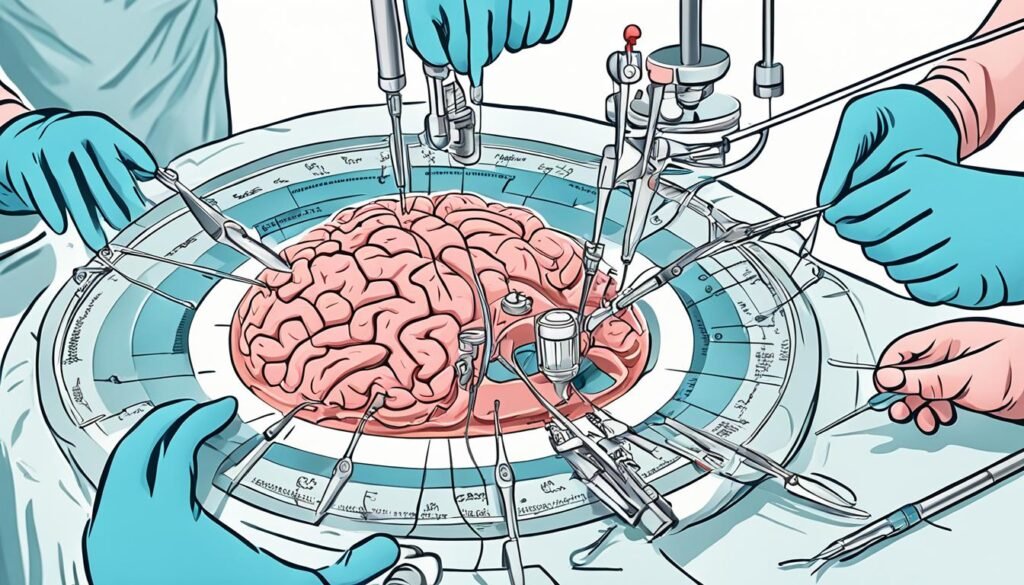
Surgical Treatment Options
The main way to treat moyamoya disease is with surgery to improve blood flow in the brain. There are many ways to do this surgery, each designed for the special needs of this disease.
Direct Revascularization
One type of surgical technique is direct revascularization, for example, the STA-MCA bypass. This method connects an artery outside the skull to one inside directly. A 2015 study showed it can keep patients with moyamoya from having a stroke.
Indirect Revascularization
Another approach is indirect revascularization. This method, like EDAS or EMS, helps the body grow new blood vessels to the brain from the neck. A 2012 study points out its success in children with moyamoya disease.
Combined Revascularization Techniques
Some surgeries mix direct and indirect methods for better results and fewer risks. A 2014 study looked at how well this works in adult moyamoya patients over time.

Moyamoya Disease Treatment: Options and Advances
The way we treat moyamoya disease has changed a lot in recent years. New surgeries, better ways to look inside the body, and deeper knowledge of the disease have all helped. Today, surgery to create new blood vessels is still key. But, new methods aim to make surgery better and safer.
One big step is monitoring blood flow during surgery. Tools like indocyanine green videoangiography and Doppler ultrasonography let doctors check the new blood pathways live. This helps them adjust their work as needed, leading to better results for patients.
Scientists are also learning more about moyamoya disease at a genetic and molecular level. This deeper understanding is opening doors to new possible treatments. Researchers are looking into what causes the arteries to shrink and block, which might lead to focused therapies in the future.
Indirect revascularization methods have improved as well. For example, there is now a surgery that helps grow more blood vessels called bifrontal encephalogaleo synangiosis. This surgery aims to boost the blood flow in the brain even more. It works alongside direct revascularization methods, offering a fuller treatment approach.
This progress in treating moyamoya disease is exciting. The future looks bright with ongoing advancements in surgery, imaging, and scientific understanding. Together, these steps promise better ways to handle this challenging brain disorder in the years to come.
Novel Surgical Techniques
Healthcare experts are always looking for better ways to treat moyamoya disease. They have come up with new surgical techniques focusing on blood flow during operations. This includes better methods to check blood flow and improve how we reroute it.
Intraoperative Blood Flow Monitoring
Now, during surgery, doctors can closely watch the blood flow. They use special tools like indocyanine green videoangiography and Doppler ultrasound. These tools help check if the bypass or rerouting of blood is working well right then. This means doctors can make quick decisions to make sure the blood flow gets back to where it’s needed in the brain.
Indirect Revascularization Advancements
Advances in sawing bones as part of the surgery (like bifrontal encephalogaleo synangiosis) are also making progress. This method helps the body direct more blood to the brain. It works along with other surgeries, giving doctors more ways to help patients based on what they need.
Postoperative Management
After surgery, patients with moyamoya disease need ongoing care. This is important for good recovery and to prevent problems. A key issue is hyperperfusion syndrome. This can happen when the brain gets more blood suddenly after surgery.
Hyperperfusion Syndrome
Hyperperfusion can cause brain swelling, seizures, or bleeding. Doctors closely watch the blood flow in the brain after surgery to avoid this. They might use special tests like indocyanine green videoangiography and Doppler ultrasonography.
Long-Term Follow-up
Long-term care is vital for moyamoya patients too. They need regular check-ups to see how well the surgery is working over time. This also helps spot any new problems early and keeps the surgery’s benefits strong.
Imaging and Monitoring Moyamoya Disease
Technology has moved forward, making it easier to spot and watch moyamoya disease. MRI, a type of imaging technique, is key. It uses special imaging methods to look at blood flow in the brain and find areas where tissue might be lacking oxygen. These methods help doctors see how severe the disease is. They also help plan surgeries and the care to follow.
Positron Emission Tomography
PET scans are becoming very important in checking people with moyamoya. They can look at the brain’s blood flow and find places in danger of not getting enough oxygen. PET scans tell doctors about the changes happening in the brain because of moyamoya. This information helps them choose the best ways to treat the disease and keeps an eye on how it’s doing over time.
Genetic and Molecular Insights
Scientists have made big strides in understanding moyamoya disease. They’ve found that changes in the RNF213 gene are key, especially in people from Asia. This discovery marks a major breakthrough in the genetic understanding of moyamoya disease.
RNF213 and Other Genetic Mutations
Besides the RNF213 gene, other genetic changes and immune reactions play a role in moyamoya disease emergence. The study of family genes has shown that various parts of the genetic code contribute to this complex condition.
Pathophysiological Mechanisms
Knowing how moyamoya disease works is key to finding better treatments and care for patients. Discoveries point to the RNF213 gene as crucial. It seems to trigger both inflammation and the growth of new blood vessels in the brain, affecting artery health.
Asymptomatic Moyamoya Disease
Even people without symptoms face risks with asymptomatic moyamoya disease. These risks include major cognitive decline due to a lack of oxygen in the brain over time. So, finding and treating it early is crucial.
Early treatment can stabilize or enhance cognitive skills and life quality. Experts continue studying how moyamoya disease affects thinking and everyday abilities. This is especially true for those who don’t show any symptoms.
Cognitive Decline and Quality of Life
People with moyamoya disease may find simple tasks difficult. This can lead to a lower quality of life. But, spotting the issue early and treating it can reduce these impacts.
Doctors should keep an eye on asymptomatic individuals for any signs of cognitive decline. Recognizing the problem early is key to improving outcomes.

Medication and Conservative Management
Medication and conservative care are key for those with moyamoya disease. They help lower the chance of strokes or other problems. For those not choosing surgery, aspirin and similar drugs are used to prevent stroke risks. These can be important tools in caring for moyamoya patients.
Some may choose conservative management for moyamoya. It involves lifestyle changes and regular follow-ups. This is a good option for those with few symptoms, avoiding the need for quick surgery.
Choosing the right treatment is crucial. Your medical team will craft a plan just for you. They’ll take into account your health and what’s best for your situation.
Pediatric Moyamoya Disease
Moyamoya disease can affect both kids and adults. Still, managing it in kids is different. Kids might have more bleeding in their brains. They need special care.
Unique Considerations
In kids, moyamoya can show up differently than in adults. They might bleed into their brains more often. This is in contrast to adults who mostly have problems because of poor blood flow. Because of this, doctors must look at each case carefully and treat them in a unique way.
Treatment Strategies
For kids with moyamoya, doctors often use surgeries that indirectly help blood flow. These surgeries, like EDAS and EMS, help new blood vessels grow. This is very helpful for kids’ brains that are still developing.
Surgery for moyamoya in children has had good outcomes. One study looked at 410 kids and found an operation worked in 92% of cases. Another study using brain scans found surgery was successful in 68% of kids. Predicting how a child will do after surgery with a special brain scan was successful in 85% of cases.

After surgery, watching the child closely is important. Checking the child’s brain blood flow and how their blood vessels react is key. These tests have shown great results, with 78% doing well right after surgery. In the long term, after a special type of bypass surgery, 92% of the children continued to do well.
Conclusion
Moyamoya disease is a rare issue in the brain’s blood vessels. It needs special care. Surgery is the main way to treat it. This can be done in a few different ways. As time goes on, these surgeries and how they are done keep getting better. Doctors also now know a lot more about how this disease works. This helps them find it and treat it earlier.
Research keeps going to make treating moyamoya better. New treatments may help patients live better lives. It’s very important we learn more about this disease. This way, we can help those with moyamoya more.
Doctors should always keep up with the newest info on how to treat moyamoya. This helps them give the best care to their patients. By working together to study and know more, we can find even better ways to help those with moyamoya in the future.
FAQ
What is Moyamoya Disease?
Moyamoya disease is rare and gets worse over time. It affects the blood vessels at the base of the brain. This leads to the growth of abnormal blood vessels.
What are the causes and risk factors of Moyamoya Disease?
Doctors don’t fully understand what causes Moyamoya disease. They think genes and the body attacking itself might play a role. It leads to different symptoms like strokes and bleeding in the brain.
How is Moyamoya Disease diagnosed?
Doctors use special pictures to diagnose Moyamoya. These can include magnetic resonance angiography (MRA) or cerebral angiography.
What are the treatment options for Moyamoya Disease?
Surgery is the main treatment for Moyamoya. The goal is to increase blood flow to the brain. This can be done directly, indirectly, or with both methods.
What are the advancements in Moyamoya Disease treatment?
There have been new advances in surgery for Moyamoya. These include better ways to monitor blood flow during surgery. Also, improved techniques for creating new blood pathways in the brain have been developed.
How is Moyamoya Disease managed in the postoperative period?
After surgery, it’s very important to watch the patient closely. This is to prevent complications like hyperperfusion syndrome. Doctors also keep an eye on the blood flow in the brain for a long time after the surgery.
How do imaging techniques help in the management of Moyamoya Disease?
Special images like MRI and PET scans are very helpful for Moyamoya. They improve how doctors plan and care for patients before and after surgery.
What is the role of genetic and molecular research in Moyamoya Disease?
Studying genes and molecules has helped find key information about Moyamoya. For example, the RNF213 gene is important, especially in Asians. This work is helping to develop better treatments and care for patients.
How does Moyamoya Disease affect cognitive function and quality of life?
Even if people don’t show symptoms, Moyamoya can still hurt their thinking ability. Getting treatment early can make these problems better or stop them from getting worse.
What are the considerations for the management of Pediatric Moyamoya Disease?
Managing Moyamoya in kids is different. They might have more bleeding in the brain. Surgeries that improve blood flow, like EDAS and EMS, are often the best choice for them.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4747064/
- https://www.mayoclinic.org/diseases-conditions/moyamoya-disease/diagnosis-treatment/drc-20355591
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1151701/
- https://shop.thieme.com/Surgical-Techniques-in-Moyamoya-Vasculopathy/9783131450616
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9437590/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8397113/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4747070/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4337618/
- https://www.uptodate.com/contents/moyamoya-disease-and-moyamoya-syndrome-treatment-and-prognosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533338/
- https://www.mayoclinic.org/medical-professionals/neurology-neurosurgery/news/moyamoya-new-protocol-for-managing-a-complex-disease/mac-20513216
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3700478/
- https://www.ncbi.nlm.nih.gov/books/NBK535455/
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




