Ocular migraine is a condition that causes temporary vision changes, often frightening the person experiencing them. Although most attacks resolve without permanent damage, they can mimic serious eye or brain problems. Understanding the difference between ocular migraine and retinal migraine and other types of visual disturbances is important for safety and proper care.
Table of Contents
ToggleOverview
What Is An Ocular Migraine?
An ocular migraine is a type of migraine that mainly affects vision. Doctors describe it as a condition where one or both eyes experience temporary visual disturbances, sometimes followed by headache. It can lead to blind spots, flickering, or even complete temporary vision loss in one eye. Some people feel a mild headache afterward, while others only notice the visual episode.
An Ocular migraine (retinal migraine) can appear suddenly, usually lasting minutes, and often resolves without treatment. But since vision loss in one eye can also signal other medical emergencies, it is always best to get checked by an eye specialist.
Ocular Migraine Vs. Retinal Migraine: Key Differences
The terms ocular migraine and retinal migraine are frequently mistaken for one another; however, there are nuanced distinctions between them. A retinal migraine is defined as repeated attacks of temporary blindness or visual changes in one eye caused by reduced blood flow to the retina. Ocular migraine is a broader term that sometimes refers to visual aura affecting both eyes.
| Feature | Ocular Migraine | Retinal Migraine |
| Vision affected | One or both eyes | One eye only |
| Symptoms | Flickering lights, zigzag lines, scotomas | Temporary blindness, blind spots |
| Cause | Brain or eye-related vascular changes | Reduced blood flow to retina |
| Risk level | Usually harmless but distressing | Can mimic serious eye disease |
Understanding this ocular migraine vs retinal migraine difference helps patients and doctors decide when urgent care is needed.
Ocular Migraine Vs. Migraine With Visual Disturbances (Aura)
Migraine with aura causes flashing lights, zigzag lines, or scotoma / scintillating scotoma in both eyes, linked to brain changes rather than eye problems. Retinal migraine, on the other hand, causes changes in only one eye. Because both look similar to patients, diagnosis often requires an ophthalmologist (eye specialist) and sometimes brain scans.
How Common Are Ocular Migraines?
Ocular migraines are considered a rare migraine type. While nearly 20–25% of people with migraine (general) experience visual symptoms, only a small fraction develop retinal migraine. This is why many cases require careful review to exclude more serious causes such as central retinal artery occlusion (CRAO) or stroke-like vision symptoms.
Symptoms And Causes

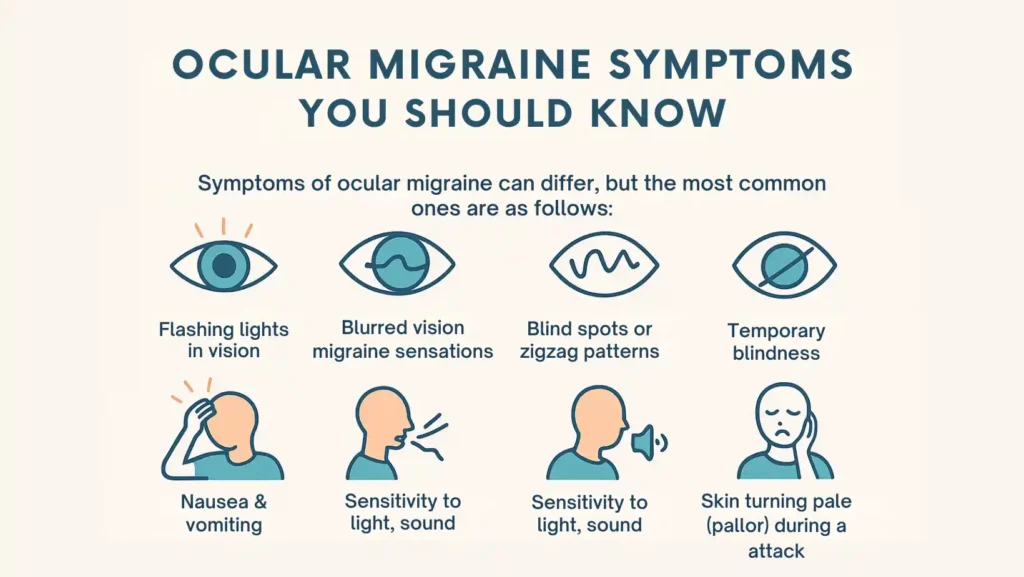
Ocular Migraine Symptoms You Should Know
Symptoms of ocular migraine can differ, but the most common ones are as follows:
- Flashing lights in vision
- Blurred vision migraine sensations
- Blind spots or zigzag patterns
- Temporary blindness in one eye
- Headache that may follow the vision changes
- Nausea & vomiting in some cases
- Sensitivity to light/sound/odors
- Fatigue / tiredness afterward
- Skin turning pale (pallor) during the attack
Because the visual loss can mimic a detached retina or a stroke, urgent evaluation is recommended during the first attack.
How Long Do Ocular Migraines Last?
Most ocular migraines last 5 to 30 minutes. In rare cases, symptoms may last for as long as an hour. Any loss of vision lasting longer than one hour or causing permanent blind spots requires immediate medical attention.
What Causes Ocular And Retinal Migraines?
Doctors believe that both types result from changes in blood flow and nerve activity. A retinal migraine may occur when blood vessels supplying the retina temporarily narrow. In contrast, an ocular aura comes from electrical changes in the brain’s visual pathways.
Other factors linked with retinal migraine causes include:
- Genetic component / family history of migraine
- Changes in blood flow to retina and migraine nerves
- Problems with eye health and migraines affecting circulation
- In rare cases, vascular spasm leading to ischemia of choroid or optic nerve
Ocular Migraine Triggers
Common ocular migraine triggers include:
- Stress and anxiety
- High blood pressure (hypertension)
- Hormonal contraceptives or hormonal changes
- Exercise / physical exertion
- Hypoglycemia (low blood sugar)
- Hyperthermia (excessive heat)
- Certain foods or drinks like alcohol and caffeine
- Skipped meals or dehydration
- Bright light exposure
Identifying your personal triggers is one of the best ways to prevent attacks.
Complications Of Ocular Migraine
While most ocular migraines resolve without damage, repeated or severe attacks may raise the risk of more serious events. Rare complications include:
- Central retinal artery occlusion (CRAO)
- Branch retinal artery occlusion (BRAO)
- Central retinal vein occlusion
- Retinal hemorrhage / edema
- Rare ischemic injury to the optic nerve
Because some of these conditions can cause permanent vision loss, doctors take every report of sudden one-eye blindness seriously.
Diagnosis And Tests
How Is An Ocular Migraine Diagnosed?
Diagnosis begins with a full history. Patients often indicate whether the vision loss impacted one eye or both. The doctor may use an ophthalmoscope to check for swelling, bleeding, or blockage.
Other tests may include:
- Visual field tests to check blind spots
- Retinal imaging
- Brain MRI or CT scan if aura or stroke is suspected
- Blood pressure and glucose testing
Specialists like an ophthalmologist (eye specialist) and a neurologist often work together to exclude vitreous hemorrhage, stroke, or structural eye disease.
Management And Treatment

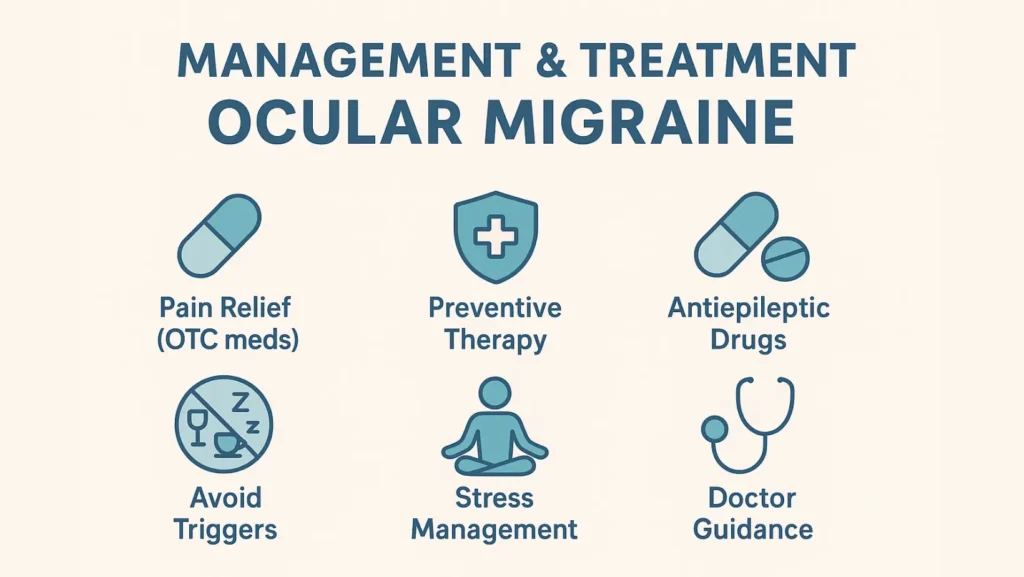
Ocular Migraine Treatment Options
Treatment depends on severity and frequency. For mild episodes, rest in a dark room and hydration may be enough. For frequent or disabling cases, ocular migraine treatment may include:
- Pain relief with non-prescription medication
- Preventive therapy with calcium channel blockers (nifedipine, verapamil)
- Antiepileptic drugs in selected cases
- Avoiding known triggers like alcohol, caffeine, or lack of sleep
- Stress management techniques such as relaxation therapy
Your doctor may also recommend adjusting hormonal contraceptives or managing high blood pressure if they contribute to attacks.
Outlook / Prognosis
What Is The Prognosis For Ocular Migraine?
Most individuals with ocular migraine have a positive prognosis. Episodes usually pass quickly and cause no permanent damage. However, a small risk of retinal artery occlusion or stroke exists, so regular follow-up is advised.
Prevention
How To Prevent Ocular Migraines?
Effective migraine prevention strategies include:
- Keeping a headache diary to track triggers
- Sleeping and waking at consistent times
- Staying hydrated and eating regular meals
- Managing stress with breathing or meditation
- Avoiding excess caffeine and alcohol
- Controlling high blood pressure and blood sugar
- Limiting exposure to bright flashing lights
Preventive medicines may be recommended if attacks are frequent.
Living With
When Should I See My Healthcare Provider About Ocular Migraines?
You should see your doctor if you experience:
- Your first-ever episode of temporary vision loss
- Episodes that last longer than one hour
- Symptoms that increase in frequency
- Associated warning signs like weakness, speech changes (aphasia, dysarthria), loss of balance (ataxia, vertigo)
These could indicate conditions beyond migraine, including stroke or central retinal artery occlusion.
The Bottom Line
Ocular migraine may seem harmless, but its similarity to more dangerous conditions means it should never be ignored. Quick evaluation can rule out emergencies. With proper care, lifestyle changes, and sometimes medication, most people can manage attacks safely. Partnering with an ophthalmologist (eye specialist) and neurologist ensures peace of mind and good vision health.
FAQs
Is retinal migraine the same as ocular migraine?
They are often used interchangeably, but retinal migraine usually means temporary vision loss in one eye, while ocular migraine can also refer to visual aura affecting both eyes.
Why am I suddenly getting retinal migraines?
Sudden retinal migraines may be due to new triggers like stress, blood pressure changes, hormonal shifts, or low blood sugar. An eye exam helps rule out more serious causes.
What are the 4 stages of ocular migraine?
The stages include prodrome with mood changes, aura or visual disturbance, headache with nausea or sensitivity, and resolution with fatigue. Not every patient experiences all four phases.
How to tell the difference between an ocular migraine and a detached retina?
Ocular migraine usually resolves within minutes, while a detached retina causes sudden, persistent floaters, flashes, and vision shadows. An ophthalmologist exam is the only way to confirm.
Is retinal migraine curable?
There is no permanent cure, but treatment and trigger management reduce frequency. Some people outgrow episodes with age, while others need ongoing preventive care and medical supervision.
Is ocular migraine a mini stroke?
No, ocular migraine is not a mini stroke. However, symptoms can mimic stroke or artery blockages. That is why urgent evaluation is important to ensure safety and proper treatment.
Can stress and anxiety cause retinal migraine?
Yes, stress and anxiety are common retinal migraine triggers. Managing stress through relaxation, good sleep, and balanced lifestyle habits can reduce the frequency and intensity of attacks.
About The Author

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
Dr. Chandril Chugh is a U.S.-trained neurologist with over a decade of experience. Known for his compassionate care, he specializes in treating neurological conditions such as migraines, epilepsy, and Parkinson’s disease. Dr. Chugh is highly regarded for his patient-centered approach and dedication to providing personalized care.
→ Book a consultation to discover which remedies suit your needs best.