Migraine brain is a term doctors and researchers use to describe the brain of someone who experiences migraines. Unlike a regular headache, migraine is considered a neurological disorder where the brain behaves differently.
People often ask if this means the brain is permanently damaged or just highly sensitive. Understanding this concept requires looking at brain structures, imaging studies, and how the brain responds before, during, and after migraine episodes.
Table of Contents
ToggleUnderstanding the Concept of a Migraine Brain
What Is a Brain Migraine?
Brain migraine is how the condition goes beyond pain. Migraine is a neurological condition that affects sensory networks, blood vessels, and nerve signaling. During an attack, the brain cells become unusually active, which sets off changes in blood flow and pain transmission. Unlike simple tension headaches, migraines often involve aura, sensitivity to sound, and nausea.
For example, a person may see zigzag lights twenty minutes before pain starts, or they may crave chocolate and feel unusually tired a day before. These pre-attack signals come from the brain, not from the muscles of the head. This is why migraine is not just pain in the head but a migraine brain disorder that affects multiple systems.
Migraine as a Brain Disorder
Doctors now describe migraine as a migraine brain disorder because it reflects a brain that processes sensory information differently. The condition is chronic, meaning it can last for years, sometimes a lifetime.
Patients often notice that ordinary things such as bright light or strong smells cause more discomfort compared to people without migraine. This heightened sensitivity is linked to changes in brain wiring.
Scientists studying brain migraine, a brain disorder, confirm that the nervous system of patients is hypersensitive, especially in the pain pathways. The brain stem, hypothalamus, and cortex often show abnormal activation during migraine episodes.
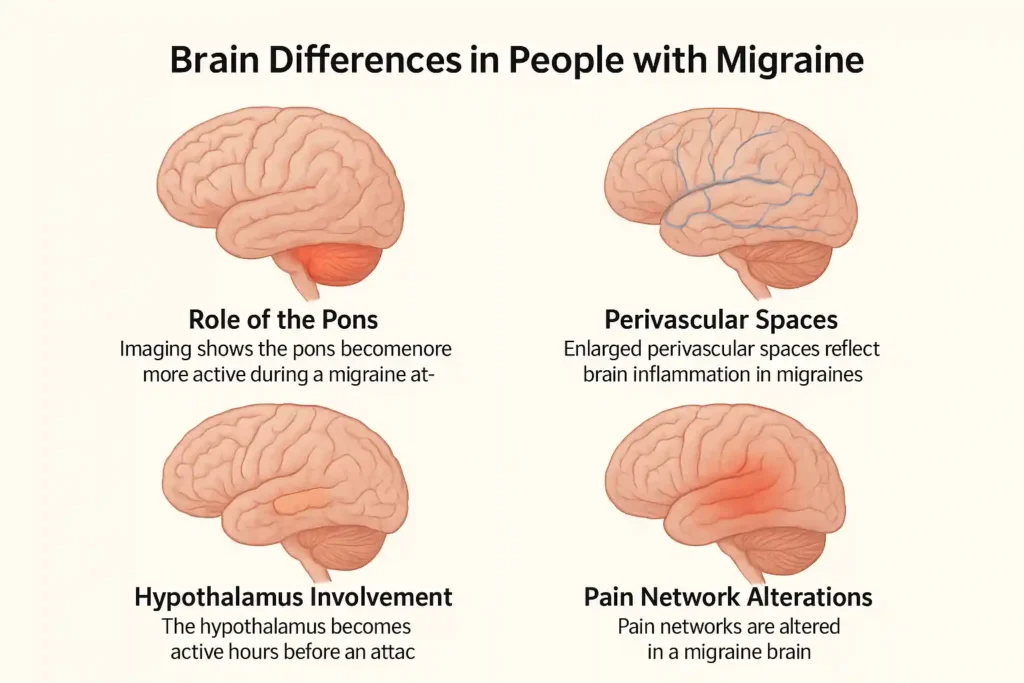
Brain Differences in People with Migraine

Role of the Pons
The pons is a small region in the brainstem that helps regulate sleep, breathing, and alertness. Imaging studies show the pons become more active during a migraine attack.
This activity may trigger nausea, eye pain, or dizziness. Patients often report feeling “off balance” or unusually sleepy before an attack, which links back to the pons.
Perivascular Spaces
Recent studies found differences in perivascular spaces in people with migraine. These are tiny fluid-filled areas around brain blood vessels. Enlarged perivascular spaces may reflect brain inflammation in migraines.
This could explain why migraine often worsens during stress or infections, when inflammation is higher in the body.
Hypothalamus Involvement
The hypothalamus controls hunger, sleep, and hormones. Many migraine patients report yawning, food cravings, or mood changes before the pain begins. This shows the hypothalamus becomes active hours before an attack.
For example, someone may suddenly crave sweets in the morning, and by the afternoon, the migraine strikes. Scientists link these early changes directly to hypothalamus activity.
Pain Network Alterations
Pain in migraine is not just a local sensation. It involves a whole-body network, including the thalamus and cortex. In a migraine brain, these pain networks are altered.
This explains why some people cannot tolerate even gentle touch during attacks. Researchers call this migraine brain hypersensitivity. It makes normal signals feel overwhelming.
Cortical Thickness Changes
Brain imaging shows that people with chronic migraine may have slightly different cortical thickness in certain brain areas. These differences are subtle but suggest that repeated attacks may gradually shape the brain.
Still, these changes are not signs of permanent damage, but they highlight how adaptable and plastic the brain is.
MRI Images of Migraine Brain vs. Average Brain
Structural Brain Changes
MRI scans show that brain structure changes in migraine patients can include small white matter spots. These spots are more common in women with long-term migraines. They usually do not cause disability, but they show that the brain of a migraine patient is not the same as a person without migraine.
Functional Brain Changes
Functional MRI looks at brain activity during attacks. It shows clear differences in a migraine brain vs normal brain.
For instance, during aura, the visual cortex lights up with abnormal waves of activity. Researchers call this spreading depression, which matches the patient’s description of flashing lights or zigzag lines.
Structural vs. Functional Brain Changes with Migraine
Long-Term vs. Short-Term Brain Effects
One of the most asked questions is does migraine affect brain health long term. Short-term changes include abnormal blood flow, brainstem activation, and sensory hypersensitivity during attacks.
Long-term changes may involve small structural alterations in cortical thickness or white matter. These differences do not usually translate into functional disability, but they are evidence of how repeated attacks leave a fingerprint on the brain.
Do Migraine Episodes Cause Brain Damage?
Can Migraines Cause Brain Damage?
But, the question is “do migraines cause brain damage?”. The evidence so far says no. Migraine does not kill brain cells like stroke or trauma. Instead, it causes temporary dysfunction. However, people with very frequent or severe migraines may show subtle long-term structural changes. These do not mean loss of intelligence or permanent decline.
What Happens to the Brain During Migraine Attacks?
Electrical activity spreads across brain networks, blood vessels widen, and chemicals like CGRP are released. This creates pain, sensitivity, and nausea. In short, what happens to your brain during a migraine is a cascade of overactive signaling that resets once the attack ends.
What Happens in the Brain During Migraine Aura?
Visual Disturbances
Migraine aura is an early sign of brain activity changes. Patients may see bright spots, zigzag lines, or even temporary vision loss. This is due to electrical waves moving through the visual cortex.
Sensory and Cognitive Symptoms
Aura is not limited to vision. Some patients feel tingling in the arms or face, or even temporary speech problems. These signs reflect migraine triggers in the brain spreading beyond vision centers to other areas.
Managing and Protecting the Migraine Brain
Lifestyle Changes
Protecting a migraine brain starts with lifestyle. Consistent sleep, regular meals, hydration, and stress management reduce attack frequency. Keeping a diary of triggers helps. For example, noticing that attacks come after skipped meals helps patients plan better.
Medical Treatments
Doctors may use triptans, anti-seizure drugs, or new treatments that block CGRP. These options target pathways identified in migraine brain research studies. Some patients benefit from Botox or newer antibody treatments, which reduce attack frequency significantly.
Preventive Strategies
Preventive strategies include magnesium, vitamin B2, and relaxation techniques. Regular exercise and yoga have been shown to help. The goal is to lower attack frequency and reduce long-term neurological impact of migraine attacks.
The Bottom Line
Yes, there is such a thing as a migraine brain. It is not damaged but sensitive, different, and more reactive. Migraines do not usually cause permanent brain damage, but they leave traces in brain scans that show how unique this condition is.
Understanding that migraine is a migraine brain disorder helps patients and doctors approach treatment in a more holistic way. By combining lifestyle, medication, and prevention, it is possible to live well with migraine.
FAQs
What does the term ‘migraine brain’ mean?
It describes a brain that processes sensory signals differently, making it more sensitive to light, sound, and pain compared to a non-migraine brain.
Is migraine considered a brain disorder?
Yes, migraine is recognized as a neurological disorder involving abnormal brain signaling, hypersensitive sensory pathways, and structural or functional changes seen on imaging studies in some patients.
How does migraine affect the brain?
Migraine changes both brain structure and function, with short-term hypersensitivity during attacks and subtle long-term alterations in cortical thickness or white matter without causing permanent damage.
What are the signs of a migraine brain?
Hypersensitivity to sound, light, smell, brain fog, aura, cravings, and mood changes are early signs showing the brain reacts differently before and during migraine episodes.
Is brain fog a symptom of migraine brain?
Yes, brain fog often occurs during and after migraines, making concentration, memory, and decision-making more difficult. This temporary effect comes from changes in brain networks during attacks.
How does migraine affect memory and focus?
Migraine can cause short-term difficulty with focus and memory, especially during aura and brain fog phases. These effects usually improve after the attack resolves, without permanent damage.
Does migraine cause permanent brain damage?
No, migraine does not usually cause permanent brain damage. Long-term scans show small differences in structure, but patients generally maintain normal brain function and quality of life.
About The Author

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
Dr. Chandril Chugh is a U.S.-trained neurologist with over a decade of experience. Known for his compassionate care, he specializes in treating neurological conditions such as migraines, epilepsy, and Parkinson’s disease. Dr. Chugh is highly regarded for his patient-centered approach and dedication to providing personalized care.
→ Book a consultation to discover which remedies suit your needs best.