Chronic migraine is more than just a bad headache. It is a disabling brain condition that affects millions worldwide and can interfere with work, family life, and personal well-being. Unlike the occasional migraine that comes and goes, chronic migraine brings headache pain on most days of the month, making it one of the most challenging neurological disorders to manage. Understanding the causes, recognizing the symptoms, and knowing the treatment options are the first steps to controlling it.
Table of Contents
ToggleWhat Is Chronic Migraine?
Chronic migraine is identified by healthcare providers as experiencing headaches on at least 15 days each month, with a minimum of eight of those days showing migraine features, for more than three months in a row. This makes chronic migraine different from ordinary headaches because it is frequent, long-lasting, and disabling.
Chronic migraine pain often feels throbbing or pulsating. It can affect one or both sides of the head and is often joined by nausea, vomiting, and sensitivity to light and sound. The attacks can last for hours or even days. Because of their frequency, they affect daily routines, sleep, work productivity, and quality of life.
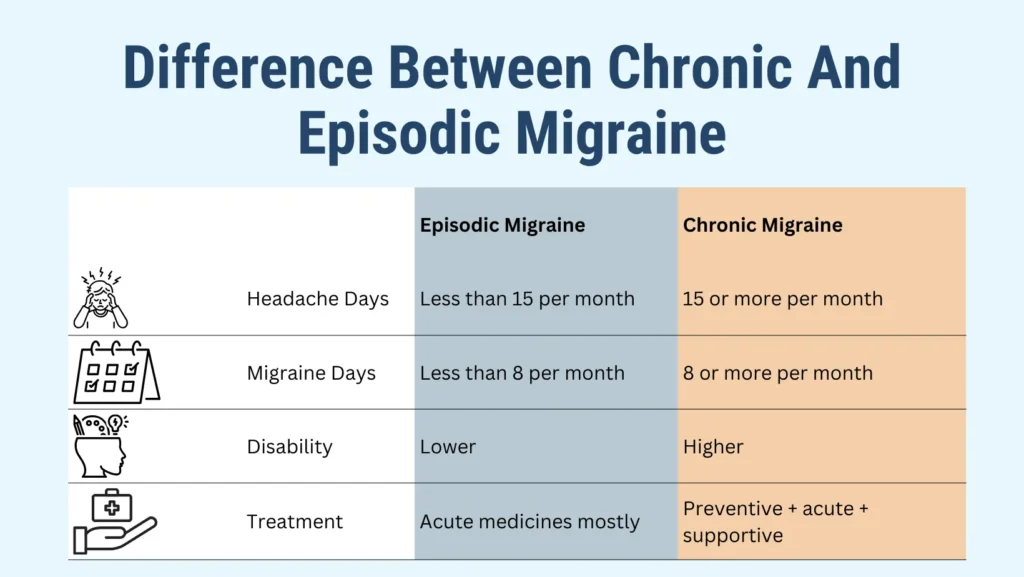
Difference Between Chronic And Episodic Migraine

The primary difference between chronic and episodic migraine is based on their frequency. Episodic migraine refers to having fewer than 15 headache days monthly, whereas chronic migraine indicates 15 or more headache days per month for a duration exceeding three months.
- Episodic migraine: Attacks happen fewer than 15 times per month. They may still be severe but occur less often.
- Chronic migraine: Attacks happen 15 or more times per month. At least 8 of those days have migraine-like symptoms such as nausea or aura.
This difference between chronic and episodic migraine is important for treatment. Episodic cases may be managed with acute medicines, while chronic cases often require preventive treatment. Recognizing the difference between chronic and episodic migraine helps patients and doctors make better choices.
| Feature | Episodic Migraine | Chronic Migraine |
| Headache Days | Less than 15 per month | 15 or more per month |
| Migraine Days | Less than 8 per month | 8 or more per month |
| Disability | Lower | Higher |
| Treatment | Acute medicines mostly | Preventive + acute + supportive |
Chronic Migraine Symptoms

Chronic migraine symptoms are more complex than a typical headache. They can include:
- Pulsating or throbbing head pain
- Pain that worsens with activity
- Nausea or vomiting
- Sensitivity to light, sound, smell, or touch
- Dizziness or blurred vision
- Neck stiffness and fatigue
Many patients experience warning signs before the pain starts. This is known as the prodrome / postdrome / attack stages. Prodrome may bring mood changes, food cravings, or yawning. The aura stage may bring flashing lights, zigzag patterns, or numbness. The attack stage is the actual headache pain, followed by the postdrome where patients feel drained or confused.
Because of their intensity and frequency, chronic migraine symptoms often lead to missed workdays, reduced concentration, and lower quality of life.
Chronic Migraine Causes
There is no definitive explanation for the causes of chronic migraine. Instead, it is a combination of genetic, biological, and environmental factors. Some of the most common triggers include:
- Medication overuse headache (MOH): Taking too many painkillers can make migraines worse and more frequent.
- Women hormones (menstruation, pregnancy, menopause, birth control): Hormone fluctuations are strong triggers.
- Sleep (lack of sleep, rest): Poor sleep or irregular sleep cycles make migraines more likely.
- Stress: Both physical and emotional stress are prevalent triggers.
- Foods & additives (MSG, aspartame, nitrates, alcohol, aged cheese, chocolate): Some foods increase the chance of attacks.
- Caffeine: Too much or sudden withdrawal can trigger migraines.
- Genetics: A family history increases risk.
To put it simply, chronic migraines causes include lifestyle habits, medication use, food triggers, and biological factors.
Chronic Migraines And Depression: The Connection
The relationship between chronic migraines and depression is strong and well documented. Individuals who suffer from frequent migraines are at a higher risk of developing depression. In the same way, depression can worsen migraine attacks. The constant pain, unpredictability of attacks, and loss of daily function can affect mood and lead to feelings of hopelessness.
Depression is not just a reaction to pain. Brain chemistry, serotonin levels, and stress hormones link both conditions. Treating both migraine and depression together often leads to better results than treating either one alone. Recognizing the overlap of chronic migraines and depression helps patients get holistic care and reduces long-term disability.
Can I Prevent Chronic Migraines?
Yes, prevention is possible. Lifestyle changes are the foundation of prevention. These include:
- Keeping a regular sleep schedule and avoiding lack of sleep
- Managing stress through relaxation, breathing exercises, or yoga
- Avoiding food triggers such as alcohol, MSG, aspartame, chocolate, and nitrates
- Staying hydrated and eating balanced meals
- Limiting caffeine intake and avoiding sudden withdrawal
- Exercising moderately without overexertion
Certain vitamins and supplements may also assist in decreasing the frequency of migraines. Research shows that magnesium, riboflavin (Vitamin B2), and Vitamin D may reduce migraine risk for some people. Regular follow-ups with a doctor ensure that prevention strategies are safe and effective.
Chronic Migraine Treatment Options
Effective chronic migraine treatment combines acute medicines, preventive therapies, and non-drug methods.
Acute treatments (used when pain starts)
- OTC medications (acetaminophen, NSAIDs, naproxen)
- Triptans (work best when taken early in an attack)
- Ergot alkaloids (less common today but useful for some patients)
- Anti-emetics for nausea and vomiting
Preventive treatments (to reduce attack frequency)
- Preventive medications like beta-blockers, antidepressants, and seizure medicines
- Botox injections every 12 weeks for proven prevention in chronic cases
- CGRP monoclonal antibodies (new targeted drugs with strong results)
- Gepants (oral drugs that block migraine signals)
Supportive treatments
- Home remedies (dark room, compress, caffeine, nap) for quick comfort
- Alternative therapies (ginger, acupuncture, massage, supplements, aromatherapy) for added relief
The right chronic migraine treatment depends on each patient. A doctor may mix medicines, lifestyle changes, and therapies to find the best fit.
Living With Chronic Migraine
Living with chronic migraine is challenging, but practical strategies can make life easier:
- Keep a headache diary to track triggers, duration, and medicines used
- Educate family, friends, and colleagues about your condition
- Prepare a “migraine rescue kit” with medicine, water, an eye mask, and earplugs
- Build a supportive care team including doctors, mental health experts, and therapists
- Join migraine support groups to share experiences and reduce isolation
Combining medical care with lifestyle adjustments can help patients regain control and live with fewer limitations.
The Bottom Line
Chronic migraine is a serious medical condition that affects millions of people. While the pain can feel overwhelming, effective treatments exist. With the right mix of prevention, medicines, and lifestyle changes, chronic migraine does not have to control your life. The key is early diagnosis, consistent management, and open communication with healthcare providers.
FAQs
How to treat constant migraines?
Constant migraines require preventive medicines, lifestyle changes, and professional care. Acute pain relievers, Botox, or CGRP therapies may be prescribed depending on frequency and severity.
What is the cause of chronic migraines?
Chronic migraines result from genetics, brain sensitivity, hormonal fluctuations, stress, sleep issues, and medication overuse. Lifestyle and diet triggers may worsen the condition in many people.
What vitamin deficiency causes migraines?
Low levels of magnesium, Vitamin D, and riboflavin (Vitamin B2) are linked with higher migraine risk. Supplements may help, but medical advice is necessary before starting them.
Is chronic migraine a disease?
Yes. Chronic migraine is recognized as a neurological disease with clear diagnostic criteria. It requires medical evaluation, treatment, and long-term management to reduce disability.
What foods trigger chronic migraines?
Common triggers include chocolate, aged cheese, processed meats, alcohol, MSG, and aspartame. Not all patients react the same way, so tracking food intake helps identify personal triggers.
Which migraine is serious?
All migraines can be serious when frequent and disabling. Chronic migraine requires medical attention. Sudden, severe headaches with other symptoms should be treated as emergencies.
What are the early warning signs of a migraine?
Early signs include mood changes, yawning, food cravings, neck stiffness, or visual aura. Recognizing these symptoms early may help prevent full-blown migraine attacks with quick treatment.
About The Author

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
Dr. Chandril Chugh is a U.S.-trained neurologist with over a decade of experience. Known for his compassionate care, he specializes in treating neurological conditions such as migraines, epilepsy, and Parkinson’s disease. Dr. Chugh is highly regarded for his patient-centered approach and dedication to providing personalized care.
→ Book a consultation to discover which remedies suit your needs best.