Posterior Reversible Encephalopathy Syndrome (PRES) is a brain condition that causes sudden neurological symptoms like seizures, confusion, or vision problems. It happens when the back part of the brain swells due to fluid leakage called vasogenic edema.
The condition is usually reversible with timely treatment, but if left unchecked, it can cause permanent brain damage.
In this blog, we’ll break down everything you need to know about PRES, from its signs to diagnosis, treatment, and recovery.
Table of Contents
ToggleWhat is Posterior Reversible Encephalopathy Syndrome (PRES)?
Posterior Reversible Encephalopathy Syndrome (PRES) is a brain disorder where swelling in the brain’s back region disrupts its normal function. This swelling, often from leaky blood vessels, leads to confusion, seizures, and blurred vision. The brain can recover if the condition is treated early, which is why it’s called “reversible.”
The meaning of PRES can be broken down as follows:
- “Posterior” refers to the back of the brain
- “Reversible” means symptoms often go away
- “Encephalopathy Syndrome” means brain dysfunction.
PRES may sound rare, but it’s increasingly being diagnosed due to better imaging tools. It’s linked to many triggers, especially sudden spikes in blood pressure, kidney failure, autoimmune disease, and certain medications.
Symptoms of Posterior Reversible Encephalopathy Syndrome
PRES syndrome symptoms can manifest rapidly, occurring within hours or a few days. Some people may only have mild signs. Others might need emergency care.
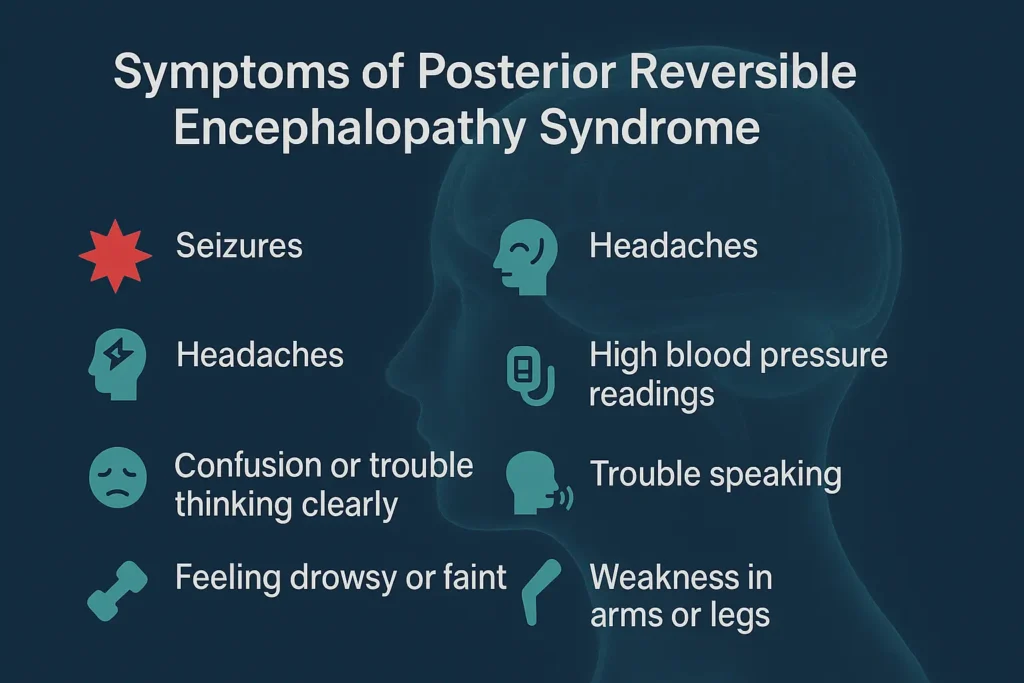 Here are the most common symptoms:
Here are the most common symptoms:
- Seizures (most common)
- Headaches
- Vision problems (blurry or even temporary blindness)
- Confusion or trouble thinking clearly
- Feeling drowsy or faint
- High blood pressure readings
- Trouble speaking
- Weakness in arms or legs
Because these symptoms look like other brain problems, diagnosing PRES can be tricky. But the pattern of these signs, especially when they come on fast, helps doctors figure it out.
What causes PRES, and who’s at risk?
No one knows exactly what sets off PRES. But doctors believe that swelling in the brain comes from leaking blood vessels, caused by sudden changes in blood pressure or toxins in the blood.
Health issues that have been linked to the onset of PRES include:
- High blood pressure (hypertension): This is one of the most common causes of PRES. The brain’s blood vessels cannot withstand the pressure if your blood pressure rises too quickly.
- Kidney failure: If your kidneys aren’t filtering blood properly, waste builds up—this can lead to swelling in the brain.
- Eclampsia and preeclampsia: These are pregnancy problems that can lead to seizures and brain changes.
- Cancer or chemotherapy: Certain cancer drugs can harm brain blood vessels.
Autoimmune disorders
Some autoimmune diseases can trigger PRES:
- Lupus
- Rheumatoid arthritis
- Vasculitis
- Crohn’s disease
- Scleroderma
These illnesses confuse the body’s immune system, which may then attack healthy tissues, including brain vessels.
Toxin exposure
PRES can also be triggered by some toxins, such as:
- Cocaine
- LSD
- Scorpion stings
- Alcohol overdose
- Ephedra
These may directly harm the brain or have an impact on blood pressure.
Medications
Some powerful drugs can lead to PRES. These include:
- Chemotherapy drugs (like cisplatin)
- Immunosuppressants (like cyclosporin, tacrolimus)
- IV contrast agents
- Steroids
- Anti-rejection drugs used in transplant patients
These drugs affect the blood vessels or immune system, making the brain more likely to swell.
How do doctors diagnose Posterior Reversible Encephalopathy Syndrome?
Doctors look out for signs like seizures, vision loss, or confusion; classic posterior reversible encephalopathy syndrome symptoms.
Once PRES is suspected, the following steps are taken:
- MRI scan: The most reliable test. It indicates fluid accumulation in the posterior region of the brain. This is key in spotting posterior reversible encephalopathy MRI findings.
- CT scan: Used to exclude the possibility of a stroke or cerebral hemorrhage.
- EEG: Helps detect seizure activity.
- Blood tests: Conducted to assess infections, kidney function, and toxin concentrations.
- Urine tests: Identify toxins or drug reactions.
An MRI may disclose brain edema, which confirms the presence of vasogenic edema associated with PRES. In most cases, imaging results are enough for diagnosis, especially when symptoms and triggers match up.
How is Posterior Reversible Encephalopathy Syndrome treated?
The primary treatment for PRES syndrome involves addressing the underlying cause. Since PRES is often triggered by high blood pressure or medication, fixing that trigger can stop symptoms.
Here’s what treatment may include:
- Managing blood pressure: Elevated blood pressure is a significant contributor to PRES.
- Stop the problem drug: Medications like immunosuppressants or chemotherapy can trigger PRES. Doctors may pause or adjust doses.
- Seizure control: Anti-seizure drugs are often given to prevent brain damage.
- Dialysis: For patients with kidney failure, dialysis may be needed.
- Treat underlying illness: If autoimmune disease, cancer, or infections triggered PRES, those are treated immediately.
- ICU care: For severe cases, close brain monitoring and breathing support may be necessary.
Each patient’s treatment for PRES syndrome depends on their root cause. But acting fast is what makes this condition reversible.
What’s the outlook for someone with Posterior Reversible Encephalopathy Syndrome?
Most people recover fully if Posterior Reversible Encephalopathy Syndrome is diagnosed early and treated well. The swelling reduces in days to weeks, and brain function goes back to normal.
However, not everyone gets a perfect recovery. When PRES is ignored, or treatment is delayed, complications may include:
- Long-term seizures (epilepsy)
- Vision problems
- Memory or focus issues
- In rare cases, death
The PRES syndrome prognosis depends on the root cause and how fast it’s treated.
Takeaway
Posterior Reversible Encephalopathy Syndrome is characterized by brain swelling that results in severe yet reversible symptoms.
- Early symptoms include seizures, confusion, and vision changes.
- Main causes of PRES are high blood pressure, kidney failure, autoimmune disease, or drug reactions.
- An MRI is the gold standard to confirm PRES by spotting posterior reversible encephalopathy MRI findings.
- Treatment for PRES syndrome involves removing the trigger and managing symptoms like blood pressure and seizures.
- Most people recover, but delays can cause permanent brain damage or death.
FAQs About PRES
What is posterior reversible encephalopathy syndrome?
A condition causing brain swelling, usually in the back part of the brain. It leads to seizures, vision issues, and confusion, but can be reversed with treatment.
What is the treatment for PRES syndrome?
Doctors treat the root cause, often high blood pressure, kidney failure, or medication side effects and control symptoms with meds or ICU support if needed.
Can you recover from PRES syndrome?
Yes. Most patients recover completely if diagnosed and treated early. Delayed care may result in long-term brain issues or repeated episodes.
What are the risk factors for posterior reversible encephalopathy syndrome?
Risks include high blood pressure, autoimmune disease, kidney failure, cancer treatment, and certain drugs.
What is the recovery time for PRES?
Recovery usually takes a few days to weeks depending on the cause and how quickly treatment begins.
What is the main cause of encephalopathy?
Brain swelling can be caused by toxins, infections, liver or kidney failure, or changes in blood pressure.
What is the survival rate of PRES syndrome?
Most people survive PRES, especially with early treatment. Delayed care may lead to permanent brain injury.
What is the most common symptom of PRES?
Seizures are the most common symptom. Headaches and confusion also happen often.
How to prevent PRES syndrome?
Keep blood pressure under control, avoid harmful drugs, and monitor medication side effects.
Does PRES cause blindness?
Yes, but usually temporary. The swelling affects visual areas in the brain, but vision usually returns with treatment unless damage is permanent.
Is PRES curable?
Yes. It’s reversible in most cases if treated quickly and correctly.
What is the age range for PRES syndrome?
It mostly affects people between 30 to 50 years old but can happen at any age.
Can PRES cause brain damage?
If not treated early, yes. Permanent damage like memory issues or seizures can happen.
Can stress cause PRES?
Stress alone doesn’t cause PRES, but it may worsen blood pressure and other triggers.
Is PRES a type of stroke?
No. But it may look like a stroke because of the symptoms. Brain scans help tell the difference.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




