A stroke starts when blood flow to the brain drops or stops, and brain cells begin failing almost immediately. If someone is having a stroke , your response in the first few minutes can decide whether the person walks, speaks, or survives.
Call emergency services right away, even if symptoms seem mild or come and go. Note the exact time the symptoms started because doctors rely on this to choose treatment. Keep the person still, calm, and awake, and position them safely to protect breathing. Do not give food, water, or medicine, since swallowing can fail without warning.
Use simple checks like face movement, arm strength, and speech clarity to confirm urgency, then hand over clear details to paramedics. A stroke is always a medical emergency. There is no safe waiting period or home fix.
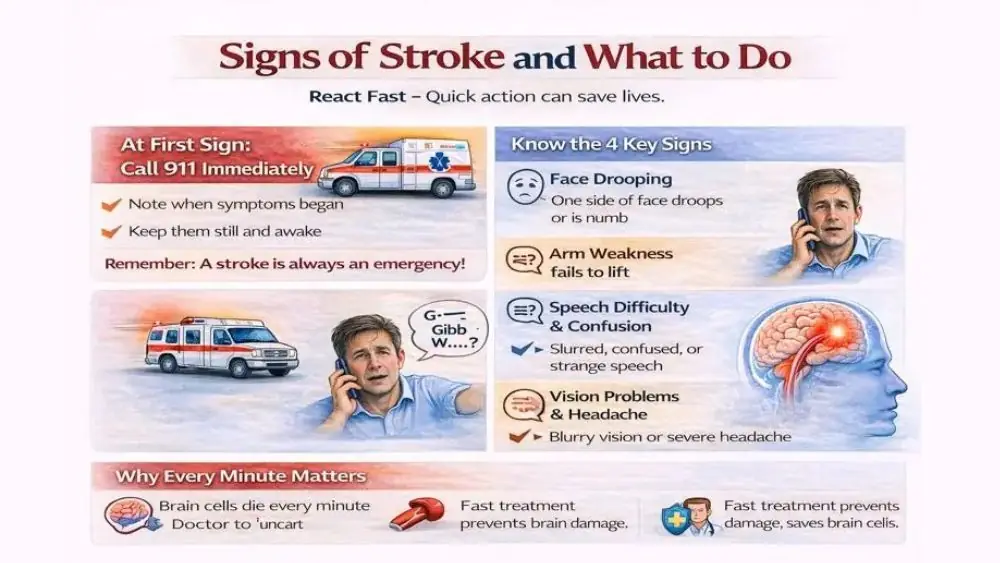
Signs of Stroke and What to Do
The signs of stroke appear because brain cells lose oxygen and glucose. Each sign points to a specific brain area failing. These signs often come suddenly, but they may also build over minutes.
Sudden Face Drooping and Weakness
One side of the face may droop or feel numb. When you ask the person to smile, the mouth may pull to one side. This happens because the facial nerve loses signals from the brain. Facial droop often links to damage in the brain’s motor cortex, which controls voluntary movement.
If someone is having a stroke and facial drooping appears, do not assume it is fatigue or stress. Facial weakness from a stroke does not improve with rest. It often worsens.
Arm Weakness and Loss of Coordination
Arm weakness is one of the clearest signs of stroke . One arm may feel heavy. The person may drop objects or fail to lift the arm fully. Coordination can fail, causing clumsy or jerky movement.
Arm weakness often signals blockage in the middle cerebral artery, a major brain vessel. This type of stroke can spread fast. When someone is having a stroke , arm weakness is a clear sign of a medical emergency.
Speech Difficulty and Confusion
Speech problems happen when a stroke affects the language centers. Words may sound slurred, and sentences may not make sense. The person may understand you, but cannot respond. Or they may speak clearly but say the wrong words.
Confusion also appears. The person may seem alert but cannot follow simple commands. When someone is having a stroke , speech trouble is one of the strongest reasons to call emergency services.
Vision Problems and Severe Headache
Vision loss can affect one eye or both. Some people see dark areas, while others see double. This happens when a stroke damages the occipital lobe or visual pathways.
A sudden, severe headache can signal bleeding in the brain. This type of headache often starts within seconds and feels different from past headaches. When someone is having a stroke , a sudden headache with vision changes is a red flag.
Why Early Action Saves Brain Cells
Brain cells cannot store oxygen. When blood flow drops, cells stop working within seconds. Nearly two million brain cells die every minute during an untreated stroke. Early treatment can reopen blocked vessels or control bleeding. When someone is having a stroke , early action limits permanent damage.
How to Recognize a Stroke Quickly
Quick recognition depends on pattern awareness, not medical training. Most strokes show predictable signs if you know what to look for.
Common Early Stroke Warning Signs
Early signs of stroke include sudden numbness, trouble walking, dizziness, speech trouble, or vision loss. These signs appear without injury or a clear cause. They do not improve with rest or food. Many people delay help because symptoms feel mild. Mild strokes still cause lasting disability if untreated.
Stroke Symptoms in Elderly vs Young Adults
Older adults often show classic symptoms like face drooping and arm weakness. Younger adults may show headache, confusion, or vision changes first. Young stroke patients are often misdiagnosed because they lack traditional risk factors.
Silent Stroke Symptoms to Watch For
Silent strokes cause brain damage without obvious early symptoms. Over time, they lead to memory loss, balance issues, or personality changes. Silent strokes are common in people with high blood pressure or diabetes.
Silent strokes still increase the risk of major stroke later. When someone is having a stroke , even subtle signs matter.
Difference Between Stroke and Seizure
A seizure causes uncontrolled shaking and loss of awareness. A stroke causes weakness, drooping, and speech problems. Seizures usually stop on their own. Stroke symptoms persist or worsen.
Medical guidelines advise treating all sudden neurological symptoms as stroke first. When someone is having a stroke , a delay caused by confusion can be deadly.
FAST Stroke Test Steps
The FAST stroke test steps are used worldwide because they work. Emergency teams rely on them because they identify the most dangerous strokes quickly.
Face Drooping Assessment
Ask the person to smile. Look closely. One side may not move. Facial asymmetry is one of the strongest signs of stroke seen in emergency care.
Arm Weakness Test
Ask the person to raise both arms. One arm may drift down or fail to lift. This shows loss of motor control from a brain injury. When someone is having a stroke , arm drift often predicts severe outcomes if untreated.
Speech Difficulty Check
Ask the person to repeat a short sentence. Listen for slurred words or wrong phrases. Speech trouble signals damage to language centers.
Time to Call Emergency Services
If any FAST sign appears, call emergency services immediately. Do not wait for all signs or wait to test again later. I f someone is having a stroke , time is the most important factor.
Stroke First Aid Steps
I f someone is having a stroke , the goal is to protect the brain until professionals take over. These first aid steps for stroke reduce risk while time-sensitive care is arranged.
Call Emergency Services Immediately
Calling emergency services is the first and most important action. Do this even if symptoms seem mild or start improving. Stroke symptoms often fade briefly and return worse.
Emergency teams can start care before hospital arrival. When someone is having a stroke , calling fast can open access to clot-removal treatment that only works within hours.
Note the Time Symptoms Started
Doctors decide treatment based on when symptoms began. If the exact time is unknown, note when the person was last seen well. Unclear timing often blocks advanced treatment because time details matter as much as symptoms.
Keep the Person Calm and Still
Stress raises blood pressure and worsens brain injury. Speak slowly using simple sentences. Ask them to stay still and do not let them walk around. Movement increases fall risk and brain strain.
Positioning the Person Safely
If awake, help them sit upright with their head supported. If lying down, keep the head slightly raised. If vomiting or drowsy, turn them onto their side. This protects the airway. When someone is having a stroke , safe positioning prevents choking.
Monitoring Breathing and Consciousness
Watch chest movement, and listen for breathing changes. If breathing stops and you are trained, begin CPR. Loss of consciousness can happen suddenly, especially with bleeding strokes.
First Aid for Stroke at Home
Many strokes happen at home. Knowing first aid for stroke at home helps bridge the gap before emergency teams arrive.
What to Do While Waiting for the Ambulance
Stay with the person. Keep them warm with a light cover and observe changes. Worsening speech or weakness should be reported to paramedics immediately. If someone is having a stroke , never leave them alone.
Recovery Position if Unconscious
If unconscious but breathing, place them on their side with the mouth angled downward. This prevents saliva or vomit from entering the lungs, which can cause pneumonia later.
Loosening Tight Clothing
Loosen collars, belts, or tight waistbands. This improves breathing comfort and reduces pressure around the neck and chest.
Preventing Choking and Aspiration
Do not give food, water, or pills. Swallowing muscles may not work. Studies show aspiration is a common cause of stroke-related complications.
What Information to Give Paramedics
Tell them when symptoms started, what changed first, known medical conditions, and current medicines. This speeds decision-making when if someone is having a stroke .
What Not to Do During a Stroke
Wrong actions cause harm. Avoid these errors even if they seem helpful.
Do Not Give Food, Water, or Medication
Aspirin is often misunderstood. It helps some strokes but worsens bleeding strokes. Only doctors decide this after scans.
Do Not Let the Person Sleep
Sleep hides neurological changes. Doctors need to see real-time symptoms. Letting them sleep delays care.
Do Not Attempt Home Remedies
Ice packs, massage, oils, or herbal remedies do nothing for blocked or bleeding brain vessels. They waste time.
Do Not Delay Emergency Care
Waiting is the leading cause of preventable stroke disability. When if someone is having a stroke , delay equals damage.
Stroke Types and Why Response Matters
Doctors treat strokes differently based on type. Fast response helps them choose correctly.
Ischemic Stroke Overview
This type comes from a blocked artery. It accounts for most strokes. Treatments focus on restoring blood flow. Timing is critical.
Hemorrhagic Stroke Overview
This type comes from bleeding inside the brain. It raises pressure and damages tissue quickly. Treatment focuses on controlling bleeding and pressure.
Why Treatment Differs by Stroke Type
Clot treatments help ischemic strokes but worsen bleeding strokes. This is why imaging comes first. When someone is having a stroke , early hospital arrival allows safe decisions.
What Happens After Emergency Treatment
Stroke care does not stop after the first hours.
Hospital Evaluation and Imaging
Doctors use CT or MRI scans to identify stroke type and location. Blood tests check clotting and infection risks.
Clot-Busting Treatment Window
Some medicines work only within a few hours of symptom start. Mechanical clot removal may work longer in selected cases. Delayed arrival often removes these options.
Possible Complications
Complications include swelling, infection, speech loss, and movement problems. Early care lowers these risks.
Early Rehabilitation Planning
Therapy may start within days. Early rehab improves independence, especially for speech and movement.
When to Seek Emergency Help Immediately
Never wait when warning signs appear.
Stroke Symptoms That Require Urgent Care
Face drooping, arm weakness, speech trouble, vision loss, confusion, or sudden headache all require emergency care.
Stroke Symptoms During Sleep
Waking with symptoms means the stroke started earlier. Emergency care is still required immediately.
Recurrent or Worsening Symptoms
Symptoms that return or worsen signal expanding damage. Call again even if help was already contacted.
FAQs
Can Stroke Symptoms Go Away on Their Own?
Symptoms may fade briefly, but brain injury often continues. Temporary improvement does not mean safety. Emergency care is still required if someone is having a stroke .
How Long Can a Stroke Last Before Damage Occurs?
Brain damage begins within minutes of blood flow loss. The longer the treatment is delayed, the greater the risk of permanent disability or death.
Can a Stroke Happen Without Pain?
Yes. Many strokes cause no pain at all. Lack of pain does not mean lack of danger. Weakness or confusion alone is enough to act.
Is It Safe to Drive Someone to the Hospital?
No. Ambulances provide oxygen, monitoring, and early treatment. Driving delays care and increases risk if symptoms worsen suddenly.
What Are the Most Common Signs of a Stroke?
The most common signs of stroke are face drooping, arm weakness, and speech difficulty. These are the core signals used to recognize a stroke quickly .
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.