Viral meningitis happens when a virus infects the thin membranes around your brain and spinal cord. These covers are called the meninges. The infection makes them swell, which causes pain and other strong symptoms. Viral infections are the most common cause of meningitis, even though bacterial meningitis is usually more deadly.
Viral meningitis often gets better in healthy people, but you still need urgent medical checks because early symptoms look the same as dangerous bacterial meningitis.
Table of Contents
ToggleWhat Is Viral Meningitis?
Viral meningitis is swelling of the lining around your brain and spinal cord caused by a virus. This swelling upsets nearby nerves and raises pressure in your head. That is why you feel feverish, sore, dizzy, or confused.
Doctors see viral meningitis in newborns, children, adults, and older adults. It is usually milder than bacterial meningitis, yet it can still make you very sick for days. Many people recover fully, but some feel tired or have headaches for weeks after the main illness ends.
How Viruses Infect The Meninges (Brain & Spinal Cord Tissue)
Most viruses that cause viral meningitis enter through your nose, mouth, or gut. They first infect your throat or intestines, then move into your blood. From there, they pass into the fluid that bathes your brain and spinal cord, called cerebrospinal fluid.
Some viruses, such as herpes simplex virus and varicella zoster virus, can travel along nerves instead of just the blood. They may stay quiet inside nerve cells for years. When they wake up again, they can irritate the meninges and trigger viral meningitis . Researchers still study the details of these nerve routes, so doctors combine lab tests with your symptoms and risk factors when they decide how to treat in your case.
Difference Between Viral Vs Bacterial Meningitis
Viral meningitis and bacterial meningitis both can start with fever, headache and a stiff neck. Because bacterial meningitis can cause brain injury or death in only a few hours, doctors treat every suspected meningitis as an emergency.
In bacterial meningitis, symptoms often grow very fast. Confusion, seizures and a dark or purple rash are more common and usually more severe. Viral meningitis tends to be milder and rarely causes death in healthy adults, but it still needs hospital checks until tests prove that bacteria are not present. Viruses cause more total meningitis cases, while bacteria cause more deaths and long-term disability.
Who Is Most At Risk? (Infants, Elderly, Immunocompromised)
Anyone can get viral meningitis , but some groups have higher risk or worse outcomes. Older adults often have weaker immunity and other health problems such as diabetes or heart disease.
People with HIV, cancer, organ transplants or long-term steroid use also have reduced defence against viruses. In these groups, viral meningitis can last longer and is more likely to leave effects such as tiredness, memory trouble or balance problems.
Contacting or living close to people with viruses that cause viral meningitis . You see this in student hostels, day care centres, crowded homes and military camps. Hand washing, mask use during outbreaks and up to date vaccines all lower risk, but no step can remove it completely.
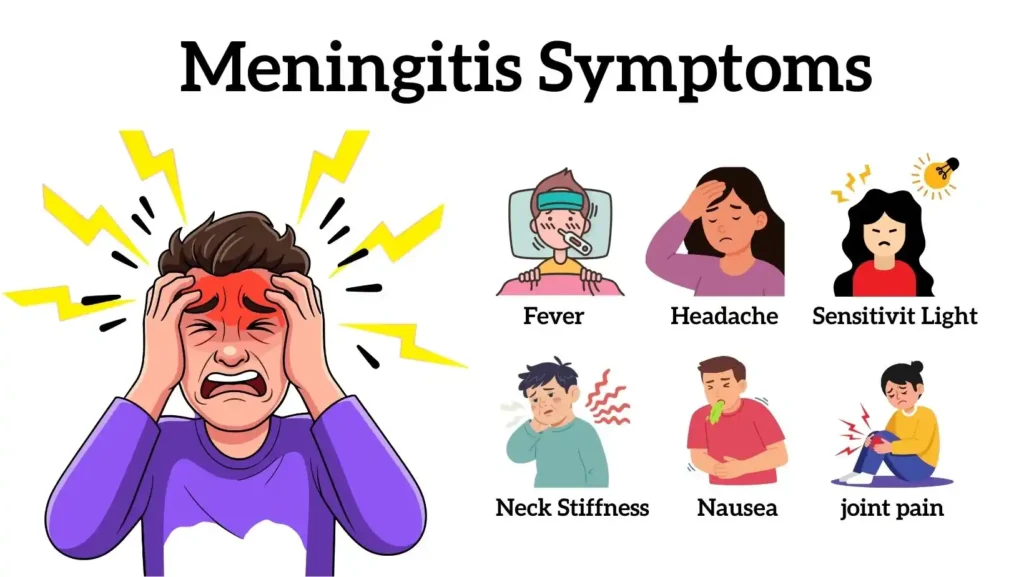
Viral Meningitis Symptoms
The early picture of viral meningitis often looks like a bad flu or stomach bug. That is why many people wait at home at first.
Early Symptoms: Fever, Headache, Nausea
You may notice fever, chills or just feel hot and cold. A strong headache is very common with viral meningitis . It often feels deep and different from your usual headaches, and it gets worse when you move your head or look at bright light.
Nausea and vomiting are also frequent. You might not want to eat or drink, which can lead to dehydration. Dehydration then makes the headache and dizziness worse. For this reason, doctors watch your fluid intake carefully even in mild viral meningitis cases.
Neck Stiffness, Sensitivity To Light, Body Aches
As viral meningitis progresses, swelling around your brain irritates the nerves in your neck. You may find it painful or even impossible to bend your chin down toward your chest. Doctors test this gently, since forcing the neck can increase pain.
Many people notice that light hurts their eyes. This is called photophobia. You might prefer dark rooms or keep your eyes closed much of the time. General muscle and joint aches also appear because your immune system releases chemicals that fight the virus but also cause soreness and fatigue.
Symptoms In Infants: Irritability, Poor Feeding, Bulging Soft Spot
Babies with viral meningitis look different from adults. They often have fever, yet their neck may look normal. Instead, you may see nonstop crying, unusual fussiness or a weak, moaning cry. The baby may feed poorly, suck weakly or refuse feeds.
Another warning sign is a bulging soft spot on top of the head, called the fontanelle. This can suggest raised pressure inside the skull. Because these signs can also mean sepsis or other severe infections, any young baby with fever and behaviour changes needs urgent medical review, not watchful waiting at home.
When Symptoms Indicate A Medical Emergency
You should seek emergency care right away if you have a sudden strong headache with fever and a stiff neck, especially if light harms your eyes. New confusion, trouble speaking, fits, trouble walking or difficulty staying awake are also red flag signs.
Doctors treat these signs as meningitis until tests show otherwise. They prefer to act fast rather than risk delay, because untreated bacterial meningitis can harm the brain or cause death. Quick hospital assessment and spinal fluid tests when safe is required, instead of waiting to see if symptoms pass.
Causes Of Viral Meningitis
Across the world, enteroviruses are the top cause in many studies, followed by herpes viruses and, in some regions, mumps, measles and HIV.
Enteroviruses (Most Common Cause)
Enteroviruses live mainly in the gut and throat. Examples include coxsackieviruses and echoviruses. They spread easily in schools and day care centres and are responsible for a large share of viral meningitis in children and young adults.
These viruses move through stool, saliva and unwashed hands. Many infections stay mild and never reach the brain. Only a small number lead to viral meningitis , but because the viruses are so common, they still cause many cases overall.
Herpesviruses (HSV, VZV, CMV, EBV)
Herpes simplex virus type 2 is a well-known cause of viral meningitis , especially in sexually active young adults. Herpes simplex type 1 and varicella zoster virus, which causes chickenpox and shingles, can also infect the meninges.
Cytomegalovirus and Epstein-Barr virus rarely cause viral meningitis in healthy people but become more important when your immune system is weak..
Mumps, Measles, HIV-Related Viral Meningitis
Before strong vaccine programmes, mumps triggered many viral meningitis outbreaks. In places where MMR coverage drops, health agencies still see mumps-related meningitis rise again. Measles infection can also affect the brain and meninges, especially in under vaccinated communities.
HIV can link to viral meningitis in two ways. Early HIV infection can irritate the meninges directly. Later on, a weak immune system allows other viruses to cause central nervous system infections more easily. The exact risk depends on your CD4 count, treatment status and local virus patterns.
How Viral Meningitis Spreads (Droplets, Saliva, Close Contact)
Most viruses that cause viral meningitis pass from person to person. You can get infected when a sick person coughs or sneezes near you, when you share drinks or cutlery, or when you touch a dirty surface then touch your mouth, nose or eyes.
Some viruses spread through stool, for example, during nappy changes. Others, like West Nile virus, spread through mosquito bites. Only a small share of people with these infections ever develop viral meningitis , which makes exact risk hard to measure. This is why experts focus on simple actions such as hand washing, safe sex, insect protection and staying home when you have fever or stomach illness.
Diagnosis: How Doctors Identify Viral Meningitis
Doctors diagnose viral meningitis by listening to your symptoms, examining you and studying your test results. Their main goal is to confirm that you truly have meningitis and to check whether the cause is viral, bacterial or something else, such as fungi, cancer or a medicine reaction.
Clinical Exam: Neck Rigidity, Neurological Signs
During the exam, your doctor checks your temperature, heart rate and blood pressure. They gently test neck movement, look into your eyes and shine light to see how your pupils react. They check your strength, speech, balance and reflexes to find any signs that the brain itself is affected.
Certain classic findings, such as Brudzinski sign where bending the neck makes the hips and knees flex, can point strongly toward meningitis. However, these signs do not appear in every case of viral meningitis , so your doctor treats them as helpful clues rather than a final answer.
Lumbar Puncture (Spinal Tap) Findings
The key test for meningitis is a lumbar puncture, also called a spinal tap. A thin needle takes a small sample of the fluid that surrounds your brain and spinal cord. This lets the lab measure white blood cells, sugar and protein levels, and look for germs.
In viral meningitis , the fluid usually has more white blood cells, a normal or slightly high protein level and a normal sugar level. Modern PCR tests can detect genetic material from specific viruses. As test panels improve, guidelines change, so doctors follow current local and international advice instead of one fixed rule.
Blood Tests, Imaging (CT/MRI)
Blood tests help show how your immune system is reacting and whether other organs are under stress. Imaging such as CT or MRI of the brain is used when doctors worry about bleeding, stroke, abscess or very high pressure inside the skull. Not every person with viral meningitis needs a scan, and the choice depends on your symptoms and exam.
Differentiating Viral Vs Bacterial Meningitis During Diagnosis
To decide if you have viral meningitis or bacterial meningitis, doctors put all the information together. They look at how fast symptoms started, what the spinal fluid shows, whether bacteria grow in culture and what PCR tests reveal.
In many hospitals, doctors first start broad treatment that covers bacteria, then narrow the plan once tests confirm that the cause is viral and not bacterial. This careful approach helps protect you while still avoiding unnecessary medicines when evidence becomes clear.
Viral Meningitis Treatment
When doctors confirm viral meningitis , they focus on two big goals. They support your body so you stay safe and comfortable. They also treat the virus directly when a specific drug helps that virus. Most mild cases of viral meningitis get better in 7 to 10 days with good supportive care, according to CDC and other large health groups.
Supportive Care: Rest, Fluids, Pain Relief
For many people, treatment for viral meningitis mainly means strong supportive care. You rest in a quiet, dark room. This reduces headache and light sensitivity. You drink plenty of fluids or receive fluids through a vein if you cannot drink enough. Doctors and nurses check your temperature, heart rate and blood pressure often.
Pain relief medicine helps with headache and body aches. Doctors usually choose drugs like paracetamol or ibuprofen, if they suit your health history. Dosage varies by age, weight and other illnesses, so your doctor decides the exact dose. This supportive treatment for viral meningitis does not kill the virus, but it helps your body fight it safely.
Antiviral Medications (When Needed For HSV Or VZV)
Some viruses that cause viral meningitis respond to antiviral drugs. The clearest examples are herpes simplex virus and varicella zoster virus. In those cases, doctors often use medicines like acyclovir or valacyclovir. These drugs slow down virus growth and may lower the risk of serious nerve problems.
Not every case needs antivirals. Research on herpes virus meningitis shows mixed results, and some studies find limited proof that antivirals change long-term outcome in every patient.
Because of this, some guidelines suggest you start antivirals when doctors strongly suspect herpes infection, then adjust once lab tests give a clear answer. Your doctor explains the expected benefit and any side effects before they start this part of treatment for viral meningitis .
Treatment Guidelines For Infants And Immunocompromised Patients
Babies, older adults and people with weak immune systems face more risk from viral meningitis . Doctors usually admit them to the hospital even if they look only mildly unwell. They often receive both antibiotics and antivirals at first, because doctors cannot safely wait while they sort out the exact cause.
In newborns, treatment for viral meningitis always includes close monitoring in a hospital ward. Nurses watch breathing, feeding, urine output and alertness. Doctors may repeat scans or spinal fluid tests if the baby does not improve as expected. In people who live with HIV, cancer or organ transplants, teams also adjust other medicines so the immune system can work as well as possible without causing rejection or other problems.
When Hospitalization Is Required
You need hospital care for viral meningitis if you cannot drink, if pain control fails or if you show any brain warning signs. These warning signs include confusion, fits, trouble walking or problems with speech. Studies on “red flag” symptoms show that headache with fever plus neck stiffness or an altered level of consciousness points strongly toward serious meningitis.
In the hospital, staff can give quick treatment when you suddenly get worse. They can move you to intensive care if breathing or blood pressure drops. This close watch lowers the chance that complications of viral meningitis go unnoticed.
Complications Of Viral Meningitis
Most healthy people recover from viral meningitis without permanent damage. Even so, you should know about possible problems that can appear during or after the illness.
Persistent Fatigue, Headaches And Memory Issues
Many people feel drained for weeks after the main illness ends. They report headaches, poor focus, mood swings and sleep problems. Recent studies show that even mild viral meningitis can leave long-term effects in a small number of patients, although most people still recover well.
Doctors call these problems “post-meningitis” symptoms. They may come from tiny changes in brain networks or from the stress of severe illness. Whatever the cause, they count as real complications of viral meningitis . You can ask for a follow-up with a neurologist or rehabilitation team if they limit your work or daily life.
Neurological Complications (Rare But Serious)
A smaller group of patients develop more serious complications of viral meningitis . These can include seizures, hearing loss, balance trouble and weakness in arms or legs. Risk appears higher when the infection also involves brain tissue, called encephalitis, or when the disease lasts a long time.
These severe problems stay rare in common enteroviral meningitis. Large reviews in children and adults show overall good outcomes, but they also warn that some patients do develop lasting neurological disorders and need long-term follow-up.
Complications In Infants And High-Risk Groups
In babies and in people with weak immune systems, complications of viral meningitis appear more often. These can include delayed milestones, learning problems or problems with speech and hearing. Because early support helps brain growth, paediatric teams often arrange regular checks after discharge for children who had viral meningitis in the first years of life.
Prevention Of Viral Meningitis
You cannot avoid every case of viral meningitis , but you can cut your risk. Prevention focuses on vaccines and simple hygiene.
Vaccines That Prevent Viral Meningitis (MMR, Varicella, Hib)
There is no single “viral meningitis shot”. Instead, several common vaccines protect you from infections that often lead to viral meningitis . The MMR vaccine protects against measles and mumps. Both infections can reach the brain and meninges, especially in unvaccinated groups.
The varicella vaccine stops chickenpox and lowers the chance of later shingles. Both stages of varicella infection can act as causes of viral meningitis . Hib, pneumococcal and meningococcal vaccines mainly stop bacterial meningitis, yet they still cut down overall meningitis in the community and help doctors focus on likely viral causes when a vaccinated person gets sick.
Hygiene, Avoiding Exposure, And Reducing Transmission
Most viruses that cause viral meningitis spread through saliva, stool or tiny droplets from coughs and sneezes. Good hand washing with soap and water after toilet use, after changing nappies and before eating reduces this spread. You should not share bottles, cups, cigarettes or lip balm with others.
If you feel sick with fever and stomach or breathing symptoms, you stay home from school or work until you improve. In mosquito season, you can cut the risk of vector borne causes of viral meningitis by using repellents, wearing long sleeves and removing standing water near your home.
Protecting High-Risk Individuals
If you live with a newborn, an older adult or someone with a weak immune system, hygiene matters even more. You keep vaccines current, wash hands often and avoid close contact when you feel unwell. In healthcare settings, staff follow strict infection control steps to avoid passing viruses like varicella zoster to vulnerable patients who might develop viral meningitis .
When To Seek Emergency Medical Care
You need urgent medical care when possible symptoms of viral meningitis show up together. These include high fever, a sudden strong headache, neck stiffness, confusion, light sensitivity and repeated vomiting. Studies on secondary headaches and meningitis agree that headache plus fever and neck stiffness counts as a red flag pattern.
You also treat a purple or dark rash that does not fade when you press it as an emergency. That rash often points to dangerous bacterial disease, not viral meningitis , but you cannot separate them at home. If you feel unsure, you always choose to seek help.
FAQs
How Serious Is Viral Meningitis?
In healthy adults, viral meningitis often causes severe short-term illness but a good long-term outlook. In babies, older adults and people with weak immunity, the disease can cause serious problems and even death without fast care.
Can Viral Meningitis Go Away On Its Own?
Mild viral meningitis can improve on its own with rest, fluids and careful monitoring. You still need a doctor to rule out bacterial infection first, because that form needs fast antibiotics and hospital treatment.
How Long Does Viral Meningitis Last In Adults?
Most adults with viral meningitis feel much better after 7 to 10 days, yet tiredness and headaches may last for several weeks. If problems continue for months, you should ask for specialist review.
Is Viral Meningitis Contagious? How Does It Spread?
Many viruses behind viral meningitis spread from person to person through saliva, droplets, stool or close contact. You lower risk by washing hands, avoiding shared drinks, covering coughs and staying home when you feel ill.
What Is The Difference Between Viral And Bacterial Meningitis?
Bacterial meningitis usually progresses faster, needs urgent antibiotics and has a higher death rate. Viral meningitis often has milder course, but early symptoms overlap, so doctors rely on spinal fluid tests to tell them apart safely.
What Are The First Warning Signs Of Viral Meningitis?
Early symptoms of viral meningitis include fever, a strong headache, nausea, light sensitivity, and general fatigue. When fever, headache, and neck stiffness appear together, you should seek emergency medical care quickly.
When Should Someone With Viral Meningitis Go To The Hospital?
You should go to the hospital when you suspect viral meningitis , especially if you have confusion, repeated vomiting, trouble drinking or any new seizure. High-risk groups should never stay at home without medical assessment.
Can Viral Meningitis Cause Long-Term Complications?
Yes, some people develop long-term complications of viral meningitis , such as headaches, memory problems, mood changes, or hearing loss. These problems stay uncommon, but they matter and deserve follow-up with your healthcare team.
How Is Viral Meningitis Treated At Home?
After hospital checks, mild viral meningitis can be managed at home with rest, fluids, pain relief and a dark, quiet room. You must return to care if new confusion, severe headache or repeated vomiting starts.
Do Antibiotics Work For Viral Meningitis?
Antibiotics target bacteria, not viruses, so they do not treat viral meningitis directly. Doctors may start antibiotics until tests exclude bacterial infection, then stop them and focus on supportive and antiviral care when appropriate.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.