Hydrocephalus treatment focuses on lowering harmful brain pressure and keeping fluid flow stable over time. You face this condition when cerebrospinal fluid builds up inside the brain spaces called ventricles.
Modern hydrocephalus treatment focuses on controlling fluid flow rather than offering a one-time cure. Options include surgery, long-term monitoring, and supportive care based on how your brain handles fluid. Some cases need urgent action, while others allow careful observation. The right approach depends on scans, symptoms, and progression speed.
Table of Contents
ToggleWhat Is Hydrocephalus?
Hydrocephalus is a brain condition caused by excess cerebrospinal fluid. This clear fluid surrounds your brain and spinal cord. It protects them and removes waste. Your body makes and absorbs this fluid every day. Problems begin when production and drainage lose balance.
Fluid may block at narrow brain pathways. Absorption may fail after bleeding or infection. Pressure then rises inside the skull. In babies, soft skull bones expand, so head size increases. In older children and adults, the skull cannot expand. Pressure then injures brain cells.
Hydrocephalus treatment aims to restore safe fluid movement. Doctors rely on brain scans, pressure tests, and symptom patterns. Untreated pressure can affect memory, movement, vision, and behavior.
Why Hydrocephalus Treatment Is Necessary
Brain tissue does not tolerate pressure well. Even mild pressure over time causes damage. You may notice headaches, nausea, blurred vision, or balance trouble. Children may show delayed learning or growth problems. Adults may struggle with thinking speed and walking.
Hydrocephalus treatment prevents permanent injury. Early pressure control improves brain development in children and functional independence in adults. Delays increase the risk of disability. Treatment decisions focus on long-term brain protection rather than short-term symptom relief.
Doctors avoid exaggeration. Surgery does not repair damaged brain tissue. It only stops further harm. That fact shapes honest care planning.
Types Of Hydrocephalus Requiring Treatment
Hydrocephalus is not a single disease. Type matters because it shapes treatment choice and outcome.
Congenital Hydrocephalus
This form exists at birth. Causes include genetic changes, brain structure differences, or infections during pregnancy. Ultrasound scans sometimes detect it before birth. Babies may show rapid head growth, bulging soft spots, poor feeding, or downward-looking eyes.
Treatment for congenital hydrocephalus starts early to protect learning and movement skills. Early pressure control supports better brain growth. Long-term care often continues into adulthood.
Acquired Hydrocephalus
This type develops later in life. Causes include head injury, brain tumors, bleeding after stroke, or brain infections. Symptoms depend on how fast fluid builds up. Sudden blockage causes severe headache and vomiting. Slow buildup causes memory loss, balance problems, and behavior changes.
Hydrocephalus treatment for acquired cases targets the cause when possible. Tumor removal or infection control may support fluid drainage, but surgery to manage pressure is still common.
Communicating Vs Non-Communicating Hydrocephalus
Doctors classify hydrocephalus based on fluid flow.
- Communicating hydrocephalus means fluid moves through brain pathways but fails to be absorbed properly. This often follows bleeding or infection.
- Non-communicating hydrocephalus means a physical blockage stops fluid flow. Tumors, cysts, or narrow channels cause this type.
Brain MRI scans help doctors decide. Hydrocephalus treatment depends heavily on this distinction because some surgeries only work for certain flow patterns.
Hydrocephalus Surgery Treatment Options
Medicines do not correct fluid buildup in most cases. Surgery remains the main option once pressure rises or symptoms worsen.
When Surgery Is Required
Doctors recommend surgery when scans show ventricle enlargement with symptoms. Surgery also becomes urgent when pressure rises quickly. Delaying care risks vision loss, seizures, or brain damage.
The treatment for hydrocephalus surgery focuses on restoring balance, not removing fluid permanently. Surgery does not cure the condition. It manages it.
Goals Of Surgical Treatment
The main goal is pressure control. Secondary goals include symptom relief and long-term stability. Surgeons aim to reduce repeat procedures when possible.
Outcomes improve when surgery matches the hydrocephalus type. Honest counseling matters because no surgery guarantees lifetime success. Hydrocephalus treatment planning always includes long-term monitoring.
VP Shunt Surgery For Hydrocephalus
What Is a Ventriculoperitoneal (VP) Shunt?
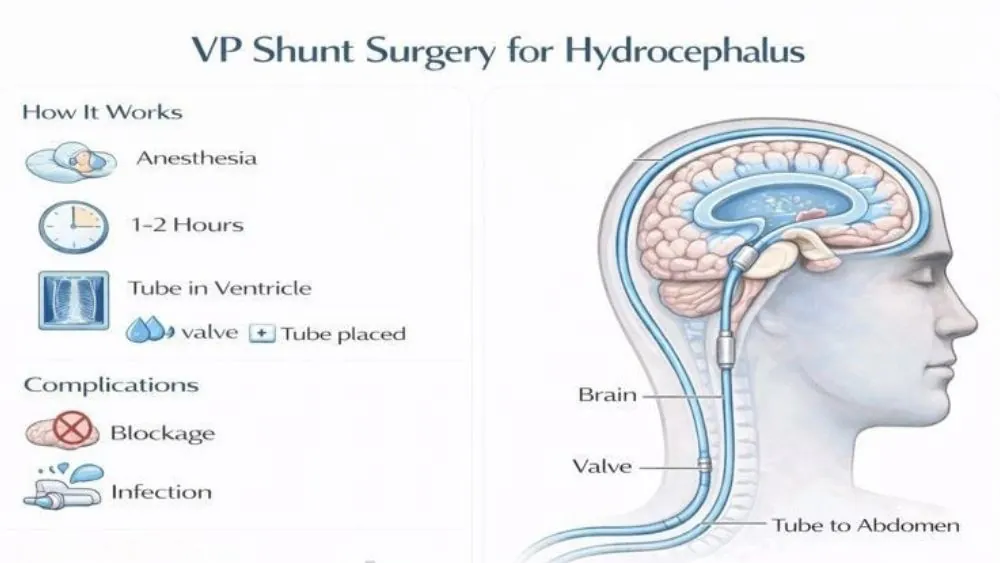
A ventriculoperitoneal shunt is a medical device that drains excess cerebrospinal fluid from your brain to your abdomen. The fluid then absorbs safely into your body. This system stays inside your body and works continuously. Hydrocephalus treatment often relies on this method because it works for many causes and age groups.
Doctors use VP shunts when fluid cannot drain naturally. Research from long-term neurosurgery studies shows VP shunts remain the most widely used option worldwide due to reliability across many hydrocephalus types.
How VP Shunt Surgery Works
During VP shunt surgery for hydrocephalus , a surgeon places a thin tube into a brain ventricle. A valve connects this tube to another tube that runs under your skin to the abdomen. The valve controls how much fluid drains. This prevents sudden pressure drops, which can damage brain tissue.
You stay under anesthesia during surgery. Most procedures take one to two hours. Imaging tests confirm proper placement before recovery begins. Hydrocephalus treatment does not end after surgery. Ongoing monitoring remains critical.
VP Shunt Complications And Risks
VP shunts can fail over time. Blockage is common, especially in children. Infection risk is highest in the first few months. Overdrainage may cause headaches or bleeding around the brain.
One-third of shunts need revision within the first few years. This does not mean failure of care. It reflects the long-term nature of hydrocephalus treatment .
Life After VP Shunt Surgery
Most people return to school or work after recovery. You should watch for warning signs like headaches, vomiting, fever, or behavior changes. These may signal shunt trouble.
Lifelong follow-up is required. Many patients live full lives with proper monitoring. VP shunt surgery for hydrocephalus supports long-term brain protection rather than a cure.
Endoscopic Third Ventriculostomy (ETV)
What Is Endoscopic Third Ventriculostomy?
Endoscopic third ventriculostomy (ETV) is a surgical method that creates a small opening in the floor of the brain’s third ventricle. This opening allows fluid to bypass a blockage and flow naturally. No device stays inside your body.
ETV reduces dependency on implants. This approach suits specific blockage patterns.
Who Is A Candidate For ETV?
ETV works best for non-communicating hydrocephalus. Older children and adults respond better than infants. Doctors use MRI scans and flow studies to assess candidacy. Success varies by age and cause. Doctors explain limits clearly before choosing endoscopic third ventriculostomy (ETV) .
ETV Vs VP Shunt: Key Differences
ETV avoids foreign devices. VP shunts work for more conditions. ETV failures usually occur early. Shunt failures can happen anytime.
Neither option is superior in all cases. hydrocephalus treatment selection depends on anatomy, age, and long-term risk tolerance.
Success Rates And Limitations Of ETV
ETV success ranges widely. Some patients remain stable for decades. Others need later shunt placement. Scar tissue may close the opening over time.
Doctors emphasize follow-up scans even when symptoms improve. Endoscopic third ventriculostomy (ETV) still requires lifelong awareness.
Normal Pressure Hydrocephalus Treatment
Treatment Approach For NPH
Normal pressure hydrocephalus mainly affects older adults. Symptoms include walking difficulty, memory decline, and bladder control problems. Pressure readings may appear normal despite fluid buildup. Normal pressure hydrocephalus treatment focuses on symptom response testing before surgery. Temporary drainage tests help predict benefit.
Shunt Surgery Outcomes In NPH
Shunt surgery improves walking most reliably. Memory and bladder control may improve more slowly or less fully. Outcomes depend on how early treatment begins.
Studies from geriatric neurology journals show that delayed care reduces benefit. Hydrocephalus treatment timing matters greatly in NPH.
Symptom Improvement Timeline
Walking often improves within weeks. Memory gains may take months. Some symptoms may remain. Rehab therapy improves results. Normal pressure hydrocephalus treatment works best with realistic expectations.
Congenital Hydrocephalus Treatment
Early Diagnosis And Intervention
Prenatal scans sometimes detect hydrocephalus before birth. Early planning allows safer delivery and timely care. Rapid treatment protects brain growth. Treatment for congenital hydrocephalus prioritizes early pressure control rather than waiting for symptoms to worsen.
Surgical Options In Infants
Shunts remain the most common option in infants. Some centers use ETV with additional techniques in select cases. Surgeons choose methods based on brain structure and age.
Infant brains are sensitive to pressure. Hydrocephalus treatment aims to preserve development during critical growth periods.
Long-Term Follow-Up In Children
Children require years of monitoring. Learning difficulties may appear later. Physical and speech therapy often support progress. Children treated early achieve better independence. treatment for congenital hydrocephalus continues into adulthood.
Non-Surgical Management And Supportive Care
Monitoring Mild Or Stable Hydrocephalus
Not all cases need immediate surgery. Some remain stable with regular scans and exams. Doctors monitor symptoms closely. Hydrocephalus treatment may involve observation when the risk stays low.
Rehabilitation And Developmental Support
Therapies support strength, balance, speech, and learning. Adults benefit from gait training. Children benefit from early educational support. Supportive care improves the quality of life alongside hydrocephalus treatment .
Risks, Complications, And Prognosis
Shunt Failure And Revision Surgery
Shunts may fail due to blockage or infection. Revision surgery restores function. Repeat surgeries are part of long-term care planning. This reality does not equal poor treatment. It reflects the chronic nature of hydrocephalus treatment .
Infection And Neurological Risks
Infections require urgent care. Prompt treatment reduces brain injury risk. Long-term neurological outcome depends on cause and timing.
Long-Term Outcomes After Treatment
Many people live independently. Outcomes vary by cause, age, and treatment speed. Early intervention improves prognosis. Hydrocephalus treatment protects function rather than offering a cure.
FAQs
Can Hydrocephalus Be Cured Permanently?
Hydrocephalus usually requires lifelong management. Some patients remain stable after ETV, but long-term monitoring is still necessary because fluid flow can change over time.
How Long Does A VP Shunt Last?
Shunts do not have a fixed lifespan. Some last many years, while others fail sooner due to blockage or infection, which is why lifelong follow-up is essential.
Is ETV Better Than Shunt Surgery?
ETV works well for certain blockages. Shunts work for more causes. Doctors choose based on anatomy, age, and long-term risk profile.
What Happens If Hydrocephalus Is Untreated?
Untreated hydrocephalus can cause permanent brain damage, vision loss, walking problems, and even death due to rising brain pressure.
Can Adults Develop Hydrocephalus Later In Life?
Yes. Brain injury, bleeding, infection, or tumors can cause hydrocephalus in adults, often requiring prompt hydrocephalus treatment .
What Is A VP Shunt Used For Hydrocephalus?
A VP shunt drains extra brain fluid to another body area, reducing pressure and preventing further brain injury.
What Is A Ventriculoperitoneal (VP) Shunt?
It is a device made of tubes and a valve that safely moves excess brain fluid to the abdomen for absorption.
How Does VP Shunt Surgery Work?
Surgeons place a controlled drainage system that continuously moves excess fluid away from the brain to maintain safe pressure.
What Are The Common Complications Or Risks Of VP Shunts?
Common risks include blockage, infection, overdrainage, and the need for revision surgery at some point in life.
What Is Life Like After VP Shunt Surgery?
Most people return to normal routines with monitoring. Regular checkups help detect problems early and support long-term brain health.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.