Hemiparesis means weakness on one side of your body that reduces strength and control in the arm, leg, or face on that side. Hemiplegia means complete loss of movement on one side, where the muscles cannot respond at all.
Both problems occur when the brain or spinal cord pathways that control movement are damaged, often from stroke, trauma, or other neurological conditions.
They share the same basic pattern of one-sided motor loss, and both can affect balance, walking, hand use, speech, and daily tasks. What separates them is the degree of movement you can still produce; hemiparesis allows some motion, while hemiplegia removes voluntary control entirely.
This difference changes how doctors diagnose the condition, how rehabilitation is planned, and how much independence you can expect in early recovery.
Table of Contents
ToggleWhat Is Hemiparesis Vs Hemiplegia?
Medical Definitions And How The Conditions Differ
Hemiparesis describes partial loss of strength on one side of the body while hemiplegia describes complete or near-complete loss of movement on one side. You can think of hemiparesis as reduced force and hemiplegia as no usable force. Clear labeling helps clinicians plan rehabilitation and set realistic daily goals.
What Happens In The Brain Or Nerves To Cause One-Sided Weakness Or Paralysis
Motor signals start in the motor cortex and travel down long nerve tracts to spinal nerves. If a blood clot, bleeding, tumor, or trauma disrupts those tracts, the message never reaches muscles and you get hemiparesis or hemiplegia.
The exact pattern of weakness tells clinicians which brain region or spinal level is damaged. Small, focal injuries usually cause hemiparesis, while larger, deeper injuries are more likely to cause hemiplegia. Imaging confirms the location and size of the lesion.
Hemiparesis Vs Hemiplegia Severity Scale (Mild → Complete)
Doctors grade muscle power on a simple scale to measure severity. You may have mild weakness that shows only with exertion, moderate weakness that limits tasks, severe weakness with minimal movement, or complete paralysis with no voluntary motion.
This grading guides therapy intensity and safety needs. Over weeks to months, strength can improve or plateau depending on the cause and treatment you receive.
Difference Between Hemiparesis And Hemiplegia
Weakness Vs Paralysis: The Core Clinical Difference
The core clinical difference is force. With hemiparesis, you still move the side, even if slowly and with poor control. With hemiplegia, you cannot voluntarily move the side. That single distinction affects how you dress, eat, or walk, and it determines whether braces, a cane, or a wheelchair will help. Rehabilitation goals change based on whether you retain voluntary movement.
How Doctors Diagnose The Difference
Doctors assess strength, tone, reflexes, and coordination during bedside testing. They compare sides, test specific muscle groups, and may use standardized scales. Imaging like CT or MRI confirms the site of injury and rules out causes such as hemorrhage or tumor.
If needed, nerve studies or spinal imaging help find non-brain causes. Accurate diagnosis informs your hemiparesis treatment or hemiplegia treatment plan.
Functional Impact Comparison (Balance, Mobility, Independence)
Hemiparesis typically reduces speed and endurance so you may need a cane or supervision. Hemiplegia often causes major loss of balance and mobility, requiring a wheelchair and home changes.
Both conditions can affect independence for feeding, dressing, and personal care, and both increase fall risk. Therapy focuses on restoring function and adapting tasks so you can do more safely at home.
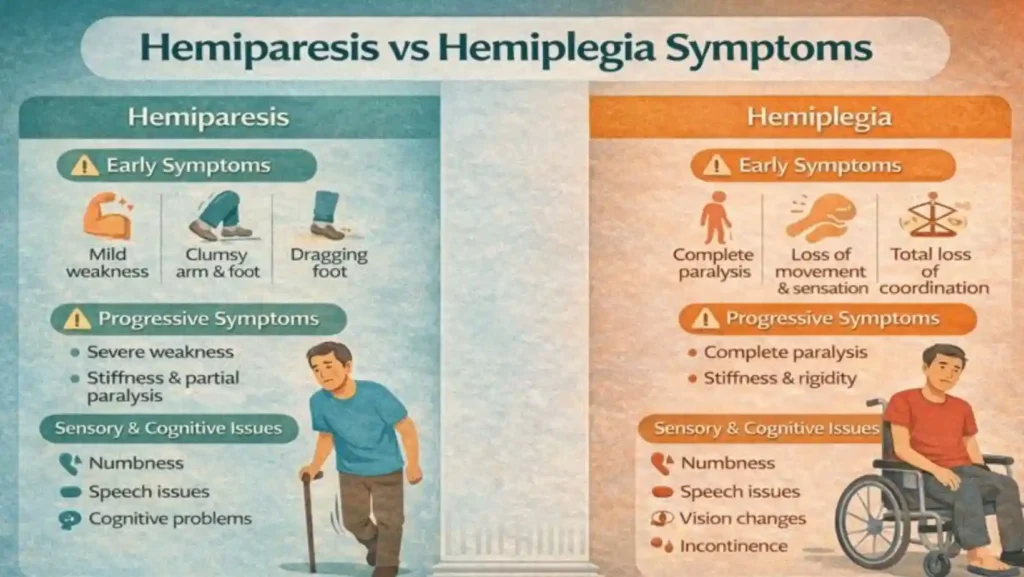
Hemiparesis Vs Hemiplegia Symptoms
Early Symptoms: Mild Weakness, Coordination Problems, Gait Changes
Early signs often include a heavy or clumsy arm, a foot that drags, or trouble using one hand. You may stumble more, drop objects, or struggle to button clothing. Speech may become slurred and your smile may look uneven. These early changes often reflect hemiparesis and warrant urgent medical review because they may signal a stroke.
Progressive Symptoms: Severe Weakness, Stiffness, Or Complete Paralysis
If damage spreads or swelling increases, initial weakness can worsen into stiffness or paralysis. Spasticity may make limbs rigid and painful. Loss of voluntary movement can leave joints at risk for contractures. You must get medical care and start rehabilitation early to prevent long-term loss and to reduce complications such as skin breakdown.
Sensory Changes, Speech Issues, And Cognitive Symptoms
Along with motor loss, you may lose touch, temperature, or position sense on the affected side. Speech problems range from slurred words to trouble finding words. Thinking, memory, or attention may decline if brain regions beyond motor pathways are involved. These combined symptoms change therapy priorities and may require speech and cognitive therapy.
When Symptoms Indicate A Medical Emergency
Sudden onset of face droop, arm weakness, or speech trouble merits immediate emergency care. Acting quickly may make you eligible for clot-busting drugs or clot removal that reduces the chance of lasting hemiparesis or hemiplegia. Do not wait. Time matters for stroke treatments that work best in the first hours
Hemiplegia Vs Hemiparesis Causes
Stroke (Ischemic And Hemorrhagic)
Stroke is the leading cause of one-sided weakness and paralysis. An ischemic stroke blocks blood flow and starves brain cells of oxygen. A hemorrhagic stroke bleeds into brain tissue and raises pressure.
Which type you have and where it hits the motor cortex largely determines whether you develop hemiparesis , hemiplegia , or hemiparesis or hemiplegia with sensory and speech problems. Early hospital care that restores blood flow can limit permanent damage.
Traumatic Brain Injury
A blow to the head can bruise or tear motor pathways. Swelling after the injury can worsen damage over hours to days, so early neuroimaging and monitoring matter. Trauma may produce focal weakness that begins as hemiparesis and becomes hemiplegia if swelling or bleeding increases. Rehabilitation plans often start while you are still in the hospital.
Brain Tumors, Infections, Inflammation
Tumors press on or invade motor areas, and infections such as encephalitis or abscesses injure tissue and nerve connections. Autoimmune inflammation can produce patchy damage similar to multiple sclerosis. These causes can create a slow or stepwise onset of hemiparesis or hemiplegia , and treatment targets both the underlying disease and the motor deficit.
Neurodegenerative Conditions And Spinal Cord Causes
Diseases like multiple sclerosis, ALS, or rare regional spinal cord syndromes may lead to progressive one-sided weakness. Spinal cord lesions and congenital brain malformations can produce lifelong hemiparesis or hemiplegia . The pattern of sensory loss, progression speed, and imaging guides precise diagnosis and therapy choices.
Hemiparesis Vs Hemiplegia Treatment Options
Acute Emergency Treatment (Stroke Protocols, Trauma Care)
In acute ischemic stroke, doctors may give clot-dissolving medicines such as tPA or perform endovascular clot removal when you arrive within guideline windows. For hemorrhagic stroke or expanding brain bleed, surgical control and pressure relief may be required.
Rapid imaging with CT or MRI determines the correct path. Early treatment reduces the risk you will go from hemiparesis to hemiplegia or limits the area of paralysis.
Physical Therapy And Occupational Therapy
Therapy is the central long-term treatment. Physical therapy focuses on strength, balance, and gait. Occupational therapy focuses on hand use, dressing, and daily tasks. Therapy uses repeated practice, graded tasks, and safe progressions so you regain function. Intensive, task-focused rehab improves outcomes more than minimal or delayed therapy.
Mirror Therapy, Constraint-Induced Therapy, Gait Training
Mirror therapy provides visual feedback that can help retrain the brain to move an affected limb; evidence shows benefit as an adjunct but studies are limited in size.
Constraint-induced movement therapy forces use of the affected arm by limiting the healthy arm and has strong evidence when you have some voluntary movement. Gait training uses treadmills, body-weight support, and balance work to improve walking. These are part of modern hemiparesis and hemiplegia treatment toolkits.
Medications: Muscle Relaxants And Anti-Spasticity Drugs
Spasticity (muscle stiffness) is common after brain injury. Doctors may use oral agents such as baclofen or tizanidine and targeted botulinum toxin injections to reduce focal tightness.
Pain control, bone health, and prevention of blood clots are also medical priorities. Medication choices depend on symptoms, side effects, and overall goals; dosing varies by age and condition.
Assistive Devices And Neurological Rehabilitation Technology
Braces, ankle-foot orthoses, walkers, and wheelchairs restore mobility and safety. Electrical stimulation and emerging robotic gait trainers can boost practice intensity.
Adaptive tools for eating and dressing increase independence while therapy continues. Technology supports both hemiparesis and hemiplegia treatment but does not replace skilled therapy. Evidence supports their use as part of a tailored plan.
Diagnosis: How Doctors Determine Hemiparesis Vs Hemiplegia
Physical Exam And Neurological Testing
A detailed exam grades muscle strength, tone, reflexes, and coordination. Your doctor looks for patterns that point to the brain, brainstem, spinal cord, or peripheral nerve. Repeated exams track change over time and guide therapy intensity.
Imaging Tests (CT Scan, MRI)
CT is rapid and rules out bleeding; MRI shows finer detail of ischemia, tumor, or inflammation. Guidelines recommend imaging quickly in suspected stroke and use MRI when the diagnosis is unclear. Imaging identifies the lesion responsible for your hemiparesis or hemiplegia and guides acute treatments.
Muscle Strength Grading And Mobility Assessment
Clinicians use standardized scales to grade strength and function. Mobility tests measure walking speed and endurance and help set rehabilitation goals. These scores let therapists track progress and adjust interventions.
Identifying Underlying Brain Or Spinal Cord Damage
Lab tests, lumbar puncture, vascular studies, and nerve conduction tests may be used to find infections, autoimmune causes, or peripheral nerve problems. Correct identification of the cause ensures that both the root problem and the motor deficit are treated.
FAQs
Can Hemiparesis Turn Into Hemiplegia?
Yes. If the underlying injury expands or is not treated, hemiparesis can worsen to hemiplegia . Early medical care and rapid stroke treatment reduce this risk and improve recovery chances.
Is Hemiparesis Or Hemiplegia Permanent?
Both can be permanent, but many people regain function with early, intensive rehabilitation. The extent of brain or spinal damage is the main factor that predicts long-term recovery.
What Are The Early Warning Signs Of Hemiparesis?
Look for sudden face droop, arm drift, slurred speech, clumsy hand use, or a leg that drags. These signs may indicate stroke and require immediate emergency care.
How Is Hemiparesis Diagnosed?
Diagnosis uses a focused neurological exam and urgent imaging (CT or MRI) to find stroke, bleed, tumor, or other causes. Further tests may include blood work, spinal imaging, or nerve studies.
Can Stroke Rehabilitation Improve Hemiplegia?
Yes. Rehabilitation can improve strength, reduce spasticity, and increase independence even in severe cases. Gains depend on injury size, timing of therapy, and therapy intensity. Evidence supports structured, repetitive practice.
How Long Does Recovery From Hemiparesis Take?
Recovery varies. Some people see rapid gains in days to weeks; others improve slowly over months to years. Early, sustained rehabilitation produces the best outcomes.
Can Children Develop Hemiparesis Or Hemiplegia?
Yes. Children can develop one-sided weakness from birth injuries, stroke, infection, or trauma. Early pediatric therapy uses play-based interventions to support development and function.
What Complications Can Occur With Hemiplegia?
Complications include joint contractures, pressure sores, pneumonia, blood clots, and depression. Preventive care, skin checks, and active rehabilitation reduce these risks.
Is Hemiplegia A Type Of Paralysis?
Yes. Hemiplegia is paralysis affecting one side of the body. Hemiparesis means partial weakness on one side. Both describe the degree of motor loss.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.