Brain herniation is one of the deadliest conditions in medicine. It happens when part of the brain is squeezed out of its normal position due to extreme pressure inside the skull. This shift is not natural. It crushes brain tissue, blocks blood supply, and can stop vital functions like breathing and heartbeat.
Doctors call it a neurological emergency because every minute counts. If ignored, signs of herniation of the brain quickly lead to coma and death. However, with prompt identification and immediate treatment, survival can be achieved.
In this guide, we will break down types of brain herniation, their symptoms, causes, tests, diagnosis, treatment options, complications, and real answers to common questions.
Table of Contents
ToggleTypes of Brain Herniation
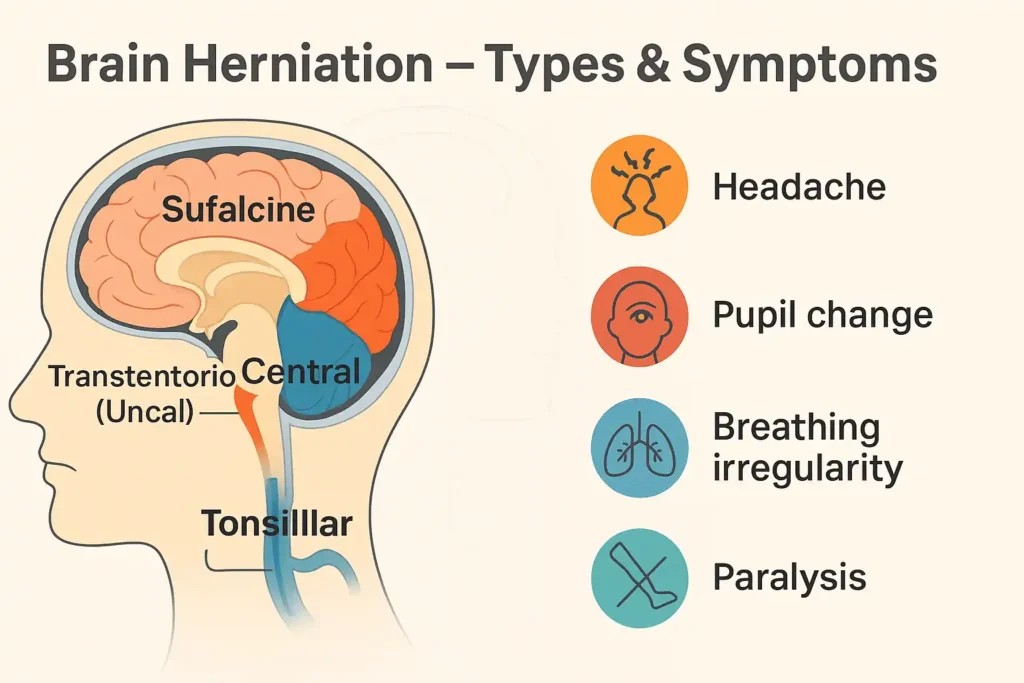
There are different types of brain herniation, each based on how brain tissue moves inside the skull. Understanding these helps doctors act quickly.
- Subfalcine herniation: It is characterized by the displacement of brain tissue beneath the falx cerebri. It is the most common type and may press blood vessels, cutting off blood flow.
- Transtentorial (uncal) herniation: It involves the inner section of the temporal lobe pressing downward across the tentorium. This causes brainstem compression, affecting breathing, blood pressure, and consciousness.
- Central herniation: The brain pushes straight downward. It squeezes midline structures and leads to fast neurologic deterioration, coma, and abnormal breathing patterns.
- Tonsillar herniation: The cerebellar tonsils move down through the foramen magnum. This is the most fatal type since it blocks the lower brainstem that controls breathing and heartbeat.
Doctors also describe herniation syndromes when a group of symptoms clearly matches one of these patterns.
Symptoms of Brain Herniation
The brain herniation symptoms vary but usually progress from mild to severe within minutes or hours. Recognizing them early saves lives.
Classic signs of brain herniation include:
- Severe, constant headache
- Nausea and projectile vomiting
- Decreased consciousness or coma
- Unequal pupils, one larger than the other
- Weakness or paralysis on one side
- Seizures
- Difficulty breathing or irregular patterns
These signs of herniation of the brain show that pressure inside the skull is rising dangerously. In hospitals, doctors also look for posturing (arms stiffly flexed or extended), a late and very serious warning sign.
Causes of Brain Herniation
To understand what brain herniation is, you need to know why it happens. The skull is rigid and cannot stretch. When something takes up extra space inside, pressure builds and the brain gets pushed aside.
Main causes include:
- Traumatic brain injury complications like bleeding, swelling, or hematomas
- Stroke leading to massive cerebral edema and herniation
- Brain tumors that enlarge and shift nearby structures
- Infections such as meningitis or abscesses
- Bleeding disorders or blood clots
- Low sodium levels causing swelling
- Post-surgical swelling or fluid collection
Every case involves increased intracranial pressure, which forces brain tissue to move where it should not.
Exams and Tests
When doctors suspect brain herniation, they must confirm fast. Tests show the cause, type, and severity.
- Neurological exam: Checks reflexes, movement, eye reaction, and mental status.
- CT scan: The quickest way to spot bleeding, swelling, or brain displacement.
- MRI findings in brain herniation: Show early damage, pressure patterns, and finer details of tissue shifts.
- Blood tests: Look for infections, electrolyte imbalance, or clotting problems.
Since herniation is a life-threatening brain injury, imaging is done immediately to decide on urgent care.
Diagnosis
Diagnosis is made by combining symptoms with scan results. Doctors look for:
- Brain herniation signs such as pupil changes or abnormal posturing
- Loss of alertness or worsening neurologic deterioration
- CT or MRI may reveal signs of swelling, tumors, or clots.
- Blood pressure or breathing abnormalities
Rapid diagnosis leads to quicker neurosurgical intervention, which improves survival chances.
Treating Brain Herniation
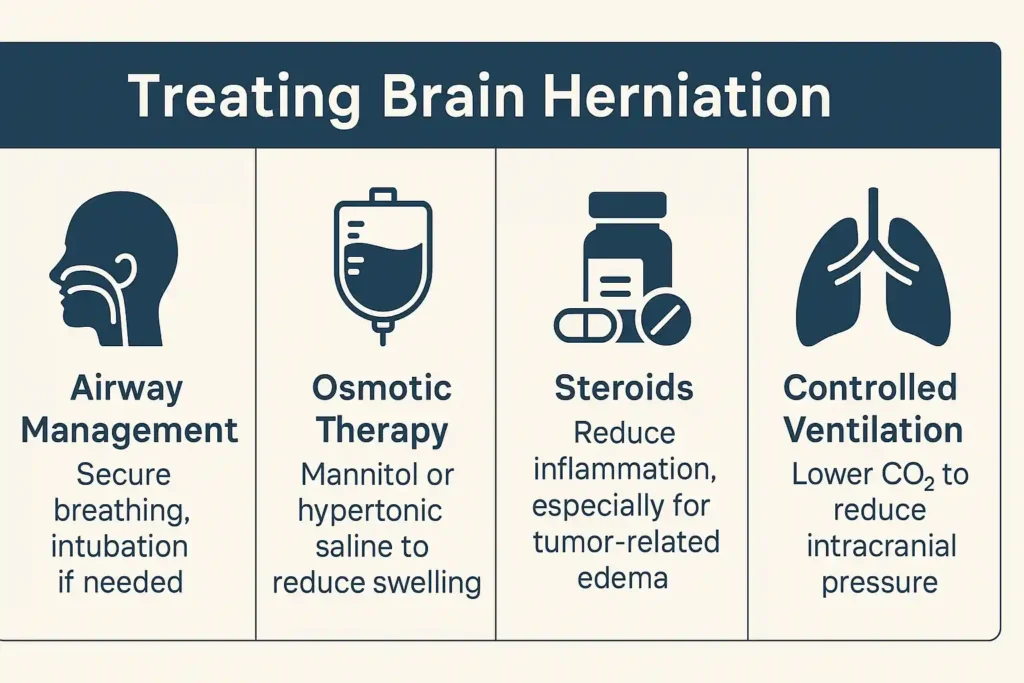
Brain herniation treatment is immediate. The goal is to reduce skull pressure and protect the brainstem.
- Airway management: Patients are intubated to protect breathing.
- Osmotic therapy: It uses mannitol or hypertonic saline, alleviates swelling by drawing fluid away from the brain.
- Steroids: Used for tumor-related swelling.
- Controlled ventilation: Carbon dioxide is lowered to reduce pressure.
- Surgery: Surgical procedures, such as decompressive craniectomy, involve the excision of a section of the skull to relieve pressure. Clot removal or tumor resection may also be done.
- CSF drainage: Tubes may be inserted to drain fluid buildup.
This is one of the few true neurological emergencies where speed directly equals survival.
Complications of Brain Herniation
Even after successful brain herniation treatment, long-term problems often remain. Complications depend on the area affected.
- Permanent weakness or paralysis
- Loss of memory or speech function
- Seizure disorders
- Hormonal changes if the pituitary gland is damaged
- Vegetative state or brain death
- Death in severe cases of life-threatening brain injury
Because the brainstem is vital for survival, damage here carries the worst outcome.
The Bottom Line
Brain herniation is a medical emergency where swelling, bleeding, or tumors push brain tissue into abnormal positions. The signs of brain herniation, unequal pupils, loss of consciousness, and breathing changes must be treated immediately.
While brain herniation treatment can save lives, recovery depends on how quickly care begins and how much damage has already occurred. Awareness, early recognition, and emergency action are the keys to survival.
FAQs
How to explain brain herniation?
Brain herniation is the result of brain tissue displacement due to elevated intracranial pressure. This dangerous movement squeezes vital structures and can quickly lead to death without immediate treatment.
What are the 4 types of brain herniation?
The four main types include subfalcine, transtentorial (uncal), central, and tonsillar. Each type describes how brain tissue shifts and which part of the brain is being dangerously compressed.
How do you treat a brain herniation?
Treatment involves urgent steps: airway support, medications to reduce swelling, surgery like decompressive craniectomy, and draining extra fluid. Immediate neurosurgical intervention often makes the difference between survival and death.
What does brain herniation feel like?
Patients may feel sudden, severe headache, nausea, confusion, and weakness. Some lose awareness quickly. Others may have seizures, unequal pupils, or breathing changes before rapidly slipping into coma.
Can a patient recover from brain herniation?
Recovery is possible, but it is influenced by the speed of treatment, the severity of the condition, and the regions of the brain that are affected. Some patients regain independence. Others may suffer permanent disability, seizures, or need long-term rehabilitation and supportive care.
Which brain herniation is the most life threatening?
Tonsillar herniation is the deadliest. It forces brain tissue down into the spinal canal, compressing the brainstem. Since the brainstem controls breathing and heartbeat, survival chances drop instantly.
What is the most common site of brain herniation?
The most common site is subfalcine herniation, where brain tissue slides under the falx cerebri. While not always instantly fatal, it can still cause serious strokes, weakness, and long-term disability.
What is the mortality rate for brain herniation?
Mortality rates are high, often over 50%. Tonsillar herniation has the worst outlook. Early recognition, imaging, and urgent surgical treatment offer the best chance of lowering the death rate significantly.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.




