Surgical Management of Meningitis: When is Surgery Needed?
Introduction: Understanding Meningitis and Its Treatment
Meningitis is a serious infection that causes inflammation of the meninges, the protective membranes covering the brain and spinal cord. It can be caused by bacteria, viruses, fungi, or parasites. While most cases are treated with medications, some severe cases require surgical intervention.
Key Takeaways:
- What is surgical management of meningitis and when is it needed?
- How is tuberculous (TB) meningitis treated surgically?
- What are the first steps in managing meningitis?
- What is the role of nurses in meningitis care?
Let’s explore when surgery becomes necessary and what procedures are used to treat meningitis complications.
What is Surgical Management of Meningitis?
Surgical management of meningitis involves surgical procedures to treat complications caused by the infection. While most cases of meningitis are treated with antibiotics or antiviral drugs, surgery may be required in severe cases, such as:
- Hydrocephalus (excess fluid in the brain)
- Brain abscess (pus-filled swelling in the brain)
- Spinal cord compression
- Severe sinus or ear infections spreading to the brain
How Does Surgery Help?
- Drains excess fluid (to relieve pressure on the brain)
- Removes abscesses or infected tissue
- Prevents permanent brain damage
Now, let’s look at the specific conditions that may require surgery.
When is Surgery Needed for Meningitis?
Surgery is only recommended when meningitis leads to serious complications that cannot be controlled with medications alone.
1. Hydrocephalus (Excess Fluid in the Brain)

Meningitis can block the normal flow of cerebrospinal fluid (CSF), causing fluid buildup in the brain. This leads to dangerous brain pressure, headaches, and confusion.
Surgical Treatment:
Ventriculoperitoneal (VP) Shunt – A small tube is inserted to drain excess fluid from the brain into the abdomen.
2. Brain Abscess (Pus in the Brain)
A brain abscess occurs when pus collects inside the brain, leading to severe infections and swelling. This can cause seizures, headaches, and confusion.
Surgical Treatment:
Craniotomy & Abscess Drainage – A part of the skull is temporarily removed, and the abscess is drained to prevent further infection.
3. Spinal Cord Compression (Due to Epidural Abscess)

In some cases, meningitis causes pus or swelling around the spinal cord, leading to severe pain and paralysis.
Surgical Treatment:
Laminectomy & Abscess Drainage – A small section of the vertebra is removed to relieve pressure and allow the pus to drain.
4. Severe Skull or Sinus Infections

Bacterial meningitis can sometimes spread from ear or sinus infections, damaging nearby bones.
Surgical Treatment:
Debridement Surgery – The infected bone or tissue is removed to stop the infection from spreading further.
What is the Surgical Management of TB Meningitis?
Tuberculous (TB) meningitis is a severe form of meningitis caused by tuberculosis bacteria. It can cause brain swelling, hydrocephalus, and tissue damage.
Surgical Procedures for TB Meningitis:
- VP Shunt Surgery – To relieve fluid buildup in the brain.
- Craniotomy – To drain abscesses and reduce pressure.
- Meningeal Biopsy – A sample is taken from the meninges to confirm TB meningitis if diagnosis is unclear.
What is the First Step in Managing Meningitis?
The first and most critical step in meningitis management is early diagnosis and immediate treatment.
Key Early Actions:
- Hospitalization – Immediate medical care is needed.
- Lumbar Puncture (Spinal Tap) – A test to confirm meningitis by analyzing cerebrospinal fluid.
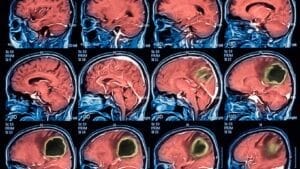
- Blood Tests & Brain Imaging (MRI/CT Scan) – To check for infection severity.
- Empirical Antibiotics – Doctors start treatment immediately, even before confirming bacterial type.
Early treatment saves lives! Delays can lead to severe brain damage or death.
What is the Early Management of Meningitis?
Once diagnosed, meningitis treatment focuses on controlling the infection and preventing complications.
- IV Antibiotics (for bacterial meningitis) – To kill the infection.
- Steroids – To reduce inflammation and brain swelling.
- Oxygen Therapy – Helps breathing in critical cases.
- Pain Management – Controls headaches and discomfort.
If complications like brain abscesses develop, surgical intervention is required.
What is the Management of Surgical Infections in Meningitis?
If surgery is needed, post-operative infection control is essential.
Key Steps:
- Sterile Surgical Techniques – To avoid spreading infection.
- Post-Surgical Antibiotics – To kill remaining bacteria.
- Regular CSF Monitoring – To check for new infections.
- Proper Wound Care – Prevents post-surgical complications.
What is the Role of Nurses in Meningitis Management?
Nurses play a vital role in meningitis care, ensuring early detection and patient recovery.
Key Nursing Responsibilities:
- Monitor Neurological Status – Check for seizures, consciousness, and brain swelling.
- Control Fever & Pain – Medications help manage symptoms.
- Prevent Infection Spread – Proper hygiene and isolation if needed.
- Educate Patients & Families – About treatment, recovery, and prevention.
What Are 5 Symptoms of Meningitis?
- Severe Headache – Constant and worsening.
- High Fever & Chills – Especially in bacterial meningitis.
- Stiff Neck – A classic meningitis symptom.
- Sensitivity to Light – Bright light causes discomfort.
- Seizures or Loss of Consciousness – Occurs in severe cases.
Seek medical help immediately if you notice these symptoms!
Final Thoughts: When is Surgery Needed for Meningitis?
Meningitis is a medical emergency that requires quick action. While most cases can be treated with medications, surgery is necessary in cases of:
- Brain abscesses
- Hydrocephalus (fluid buildup in the brain)
- Spinal cord compression
Early detection and timely treatment are critical! If you suspect meningitis, see a doctor immediately.
Looking for expert medical advice? Stay informed with the latest updates in neurology and infectious disease management!
The Truth About ADHD Medication in India – Expert Advice by Dr. Chugh
Imagine your mind as a symphony, but the instruments are playing out of tune. That’s ADHD. But what if you could conduct that orchestra, bringing harmony and focus? Dr. Chandril Chugh, a leading neurologist, pulls back the curtain on ADHD medication in India, offering a lifeline to clarity and control.
“What’s the best drug for ADHD here?” “Are there safe options?” “Can I truly manage this?” These questions echo in the minds of many. Let’s silence the uncertainty and illuminate the path to effective treatment. So, without wasting any time let’s dive deep, cutting through the noise to provide you with the facts.
10 Proven Strategies to Navigate ADHD Medication in India:
Understanding ADHD Medication in India is crucial for anyone seeking to manage their symptoms effectively.
Navigating the landscape of ADHD treatment can be daunting, especially when considering the available medications and their impact. This guide, drawing on expert insights, aims to provide clarity and direction for those seeking effective solutions.
Decoding Drug Options: ADHD Medication in India
The first step in managing ADHD is understanding the various medication options available. In India, like elsewhere, these primarily fall into two categories: stimulants and non-stimulants.
ADHD Medication in India: Stimulants vs. Non-Stimulants
Stimulants are often the first line of treatment for ADHD. They work by increasing the levels of certain neurotransmitters in the brain, improving focus and attention. Common stimulants include methylphenidate and amphetamine-based medications.
Non-stimulants, on the other hand, offer an alternative for individuals who may not tolerate stimulants or have specific medical conditions. They function differently, often taking longer to show effects but providing a steadier, longer-lasting impact.
1. Common Stimulant ADHD Medication in India Options.
- Methylphenidate (e.g., Ritalin, Concerta)
- Lisdexamfetamine (e.g., Vyvanse)
- Amphetamine (e.g., Adderall)
2. Common Non-Stimulant ADHD Medication in India Options.
- Atomoxetine (e.g., Strattera)
- Guanfacine (e.g., Intuniv)
- Clonidine (e.g., Kapvay)
3. Expert Insights on Effective Treatment
Dr. Chandril Chugh, a leading expert in ADHD treatment in India, unveils that the best medication approach is highly individualized. Factors such as age, symptom severity, and co-existing conditions play a significant role. It is important to have a through consultation with a psychiatrist or a medical professional specialized in ADHD.
4. Managing Side Effects
Like any medication, ADHD drugs can have side effects. Stimulants may cause decreased appetite, sleep disturbances, or increased heart rate. Non-stimulants can lead to fatigue, nausea, or mood changes. Regular monitoring and open communication with your doctor are essential to manage these effects effectively.
5. Dosage and Administration
Finding the right dosage is crucial. It often involves a trial-and-error process, starting with a low dose and gradually increasing it until optimal results are achieved. Adherence to the prescribed dosage and schedule is vital for consistent symptom management.
6. Long-Term Management
ADHD is a chronic condition, and long-term management is often necessary. Regular follow-up appointments with your doctor are essential to monitor progress, adjust medication as needed, and address any emerging concerns.
7. Lifestyle Adjustments
Medication is most effective when combined with lifestyle adjustments. These include:
- Regular exercise
- A balanced diet
- Adequate sleep
- Stress management techniques
- Cognitive behavioral therapy (CBT)
8. Accessing Medication in India
Accessing ADHD medication in India requires a prescription from a qualified psychiatrist. It is important to consult with a specialist who can provide a comprehensive assessment and develop a personalized treatment plan.
9. The Importance of Professional Guidance
Navigating ADHD medication in India requires expert guidance. A qualified healthcare professional can provide accurate information, address concerns, and develop a tailored treatment approach.
10. Empowering Individuals with ADHD
By understanding the available medication options and embracing a holistic approach to treatment, individuals with ADHD can effectively manage their symptoms and lead fulfilling lives.
Addressing Common FAQs
Is ADHD medication addictive?
When taken as prescribed, the risk of addiction is low. However, misuse can lead to dependence.
Q: Can adults benefit from ADHD medication?
Yes, adults with ADHD can experience significant improvements in their symptoms with appropriate medication.
Q: Are there any natural remedies for ADHD?
While lifestyle changes can support symptom management, medication is often necessary for effective treatment.
What Is the Most Recommended Medication for ADHD?
The best medication depends on age, severity, and response to treatment .
- For children: Atomoxetine is the most commonly prescribed as it’s safer and has a long-lasting effect.
- For adults: Modafinil or Bupropion may be used if stimulant medications are unavailable.
- For severe ADHD: Methylphenidate (Ritalin) is effective but requires a strict prescription.
A psychiatrist or neurologist should determine which ADHD medication in India is suitable for you based on medical history and symptoms.
What Are the Dark Sides of ADHD?
While ADHD medications help, untreated ADHD can lead to severe life challenges , including:
- Low academic and work performance due to difficulty focusing.
- Relationship struggles because of impulsivity and forgetfulness.
- Increased risk of anxiety and depression.
- Substance abuse problems as a coping mechanism.
- Low self-esteem and emotional dysregulation.
However, with proper treatment , including medication, therapy, and lifestyle changes , ADHD can be managed effectively.
Does ADHD Get Worse With Age?
ADHD does not get worse , but symptoms change over time .
- Children (5-12 years old): Hyperactivity is the most noticeable symptom.
- Teenagers (13-19 years old): Impulsivity may lead to risky behaviors.
- Adults (20+ years old): Struggles with time management, organization, and focus.
Some people develop coping mechanisms over time, while others continue to experience significant challenges if untreated.
Can You Eventually Get Off ADHD Meds?
Yes, but only under medical supervision. Some individuals outgrow ADHD symptoms or develop coping strategies that reduce their dependence on medication.
However, stopping medication suddenly can cause:
- Difficulty concentrating.
- Increased impulsivity and hyperactivity.
- Emotional instability.
Recommended Approach: If you’re considering stopping ADHD medication, always consult a doctor first. Gradual tapering under medical supervision is essential. For expert advice, reach out to the best ADHD doctor for kids.
At What Age Is ADHD at Its Peak?
ADHD symptoms peak between ages 7-9 , when hyperactivity and impulsivity are most intense.
- Preschool (3-5 years): Early signs like excessive movement and lack of attention.
- School Age (6-12 years): Symptoms become more evident, affecting academics.
- Teenage Years (13-18 years): Emotional and social difficulties arise.
- Adulthood (19+ years): Focus and organizational challenges remain, but hyperactivity often decreases.
Early intervention with therapy and ADHD medication in India can help manage symptoms effectively.
Which Famous People Have ADHD?
Many successful people have ADHD, proving that it does not limit success when managed well.
Famous Personalities with ADHD:
- Michael Phelps (Olympic swimmer) – Used ADHD as motivation in sports.
- Jim Carrey (Actor & Comedian) – Channeled his hyperactivity into creative expression.
- Richard Branson (Founder of Virgin Group) – Credits ADHD for his entrepreneurial spirit.
- Will Smith (Actor & Producer) – Has openly discussed his ADHD struggles.
Their success stories highlight how ADHD treatment, proper guidance, and personal strengths can lead to great achievements.
What Makes ADHD People Happy?
ADHD individuals thrive when they engage in stimulating, rewarding activities that align with their strengths.
Ways to Boost Happiness with ADHD:
- Exercise regularly – Releases dopamine and improves focus.
- Creative outlets – Art, music, and storytelling help with self-expression.
- Structured routines – Reduce anxiety and improve productivity.
- Passion-driven work – ADHD individuals excel in fields they love.
- Social connections – Meaningful relationships help with emotional stability.
Medication, therapy, and lifestyle adjustments together enhance overall happiness and well-being .
Does ADHD Affect IQ?
ADHD does not lower intelligence , but it affects how individuals process and use their intelligence .
- Some ADHD individuals have above-average IQs but struggle with focus.
- Others may excel in creative, problem-solving tasks but struggle with routine work.
- Many have high emotional intelligence (EQ) and strong social skills.
With the right strategies, ADHD individuals can maximize their cognitive strengths and succeed in any field.
Final Thoughts on ADHD Medication in India
ADHD is manageable with the right combination of medication, therapy, and lifestyle changes . While stimulant medications are restricted in India, non-stimulant options like Atomoxetine, Modafinil, and Bupropion can be effective alternatives.
Key Takeaways:
- ADHD medication should be taken under medical supervision .
- Symptoms evolve with age, but proper treatment helps manage them effectively .
- ADHD does not limit success—many famous individuals have excelled despite having it.
- A structured lifestyle, therapy, and tailored ADHD treatment plans lead to better quality of life.
If you or your child has ADHD, consult a neurologist or psychiatrist for the best treatment plan. Early intervention is key to long-term success.
Schizophrenia Treatment: Latest Advances & Effective Therapies
Is There a Cure for Schizophrenia? Exploring the Latest Treatments
Introduction
Schizophrenia is a complex mental health condition that affects how a person thinks, feels, and behaves. It has long been misunderstood, leading to stigma and confusion. However, advances in medical science are bringing new hope to people with schizophrenia and their families.
As we step into 2025, doctors and researchers are developing new medications, innovative therapies, and groundbreaking approaches to improve treatment. While schizophrenia remains a lifelong condition, the latest treatments help individuals manage symptoms, regain independence, and lead fulfilling lives.
According to Dr. Chandril Chugh, a leading neurologist, early diagnosis and personalized care play a crucial role in helping patients stabilize and thrive. In this article, we will explore the latest advancements in schizophrenia treatment and how they are transforming lives.
Is Schizophrenia Curable?
One of the biggest questions people ask is: Can schizophrenia be cured?
Right now, schizophrenia has no cure, but it is highly treatable. With the right medication, therapy, and support, most people can control their symptoms and live independently.
Is Schizophrenia a Lifelong Condition?
Yes, schizophrenia is a chronic condition, meaning symptoms may appear at different points in life. However, many people can achieve long-term stability and remission with proper medical care and lifestyle adjustments.
Key Facts About Schizophrenia Treatment:
Early diagnosis leads to better outcomes
A combination of medication and therapy works best
Lifestyle changes, support groups, and family involvement are essential
According to Dr. Chandril Chugh, the key to managing schizophrenia effectively is customized treatment that addresses each patient's unique needs.
What Is the Best Treatment for Schizophrenia?
1. Medications: The Foundation of Treatment
Schizophrenia is primarily treated with antipsychotic medications, which help control symptoms like hallucinations, delusions, and disorganized thinking.
Types of Antipsychotic Medications:
First-generation (typical) antipsychotics (e.g., Haloperidol, Chlorpromazine) – Effective but may have more side effects.
Second-generation (atypical) antipsychotics (e.g., Risperidone, Olanzapine, Clozapine) – Newer drugs with fewer side effects.
Long-acting injectable antipsychotics (LAIs): A great option for those who struggle with taking daily pills.
2. Therapy & Psychosocial Support
Medication alone is not enough—therapy is just as important for managing schizophrenia.
Cognitive Behavioral Therapy (CBT): Helps patients recognize and change negative thoughts.
Social Skills Training: Teaches communication and daily living skills.
Family Therapy & Support Groups: Helps loved ones understand the condition and offer better support.
3. New & Emerging Treatments in 2025
Medical research is constantly evolving, leading to new and promising treatments for schizophrenia:
Cutting-Edge Advances:
Transcranial Magnetic Stimulation (TMS): A non-invasive brain therapy that may help with symptoms.
Deep Brain Stimulation (DBS): A surgical treatment for severe, treatment-resistant schizophrenia.
AI & Digital Mental Health Tools: Mobile apps that track symptoms and provide virtual therapy.
Gut-Brain Connection Research: Scientists are studying how gut bacteria influence mental health.
According to Dr. Chandril Chugh, these innovations could revolutionize schizophrenia treatment in the coming years.
Can You Live a Normal Life with Schizophrenia?
Yes! Many people with schizophrenia live fulfilling, independent lives—especially with the right treatment and support.
How to Improve Life with Schizophrenia:
Stick to medication and therapy
Build a strong support system
Follow a healthy lifestyle (exercise, good sleep, and stress management)
Seek ongoing care and check-ups
Dr. Chandril Chugh emphasizes that a strong support system and medical supervision are key to long-term success in managing schizophrenia.
Common Questions About Schizophrenia
Can People with Schizophrenia Get Married?
Yes! With proper treatment and understanding, people with schizophrenia can have successful relationships and marriages.
Can Schizophrenia Patients Fall in Love?
Absolutely! Schizophrenia does not stop someone from experiencing love and companionship.
Is Schizophrenia Genetic?
Schizophrenia has a genetic component, but lifestyle, stress, and environmental factors also play a role.
Does Schizophrenia Show Up on MRI?
MRI scans cannot diagnose schizophrenia, but research shows subtle brain changes in people with the condition.
What Is the "25% Rule" for Schizophrenia?
The 25% Rule suggests that:
- 25% of patients fully recover
- 50% experience major symptom improvement
- 25% have persistent symptoms despite treatment
What's Next? The Future of Schizophrenia Treatment
Schizophrenia treatment is evolving rapidly, offering new possibilities for recovery. Scientists are exploring:
Gene Therapy & Personalized Medicine – Using DNA to develop customized treatments
Neuroinflammation Research – Studying how brain inflammation affects schizophrenia
Psychedelic-Assisted Therapy – Researching the use of psilocybin for severe cases
These breakthroughs could redefine schizophrenia treatment in the future.
Final Thoughts: Hope for the Future
Schizophrenia remains a challenging condition, but modern medicine is transforming how it is treated.
Key Takeaways:
Schizophrenia is not curable but is highly treatable
New therapies and medications are improving outcomes
Early intervention leads to better long-term results
A strong support system is essential for recovery
Need expert advice? Visit Dr. Chandril Chugh's website for professional care and guidance.
Nerve Pain Relief: Strategies for a Better Quality of Life
Unleash Yourself from the Grip of Nerve Pain: Discover 10 Transformative Strategies for a Life Redefined
Are you tired of nerve pain dictating your life? Does it steal your sleep, limit your activities, and cast a shadow over your days? You're not alone. Millions grapple with the relentless sting of nerve pain, but there's hope. Imagine a life where you're not held hostage by throbbing, burning, or stabbing sensations. Picture yourself reclaiming your passions, rediscovering restful nights, and embracing each day with renewed vigour.
This isn't just a dream; it's a possibility. Within these pages, we unveil 10 evidence-based strategies to help you break free from the clutches of nerve pain and embark on a journey toward a better quality of life. From natural remedies and lifestyle adjustments to cutting-edge therapies, we'll explore a range of options to empower you on your path to healing.
Embrace a future where nerve pain no longer defines you. Let's embark on this transformative journey together.
What is the Fastest Way to Get Relief from Nerve Pain?
Immediate relief is often sought by individuals suffering from nerve pain. Here are some quick-acting strategies:
- Topical Treatments – Applying capsaicin cream or lidocaine patches can numb pain receptors.
- Cold & Heat Therapy – Ice packs reduce inflammation, while warm compresses improve circulation.
- Stretching & Light Exercise – Helps release tension and enhances nerve function.
- Deep Breathing & Meditation – Reduces stress, which exacerbates nerve pain.
Is Heat or Ice Better for Nerve Pain?
Both heat and ice can help, but the choice depends on your symptoms:
- Ice Therapy: Best for acute pain, inflammation, and swelling.
- Heat Therapy: Ideal for chronic pain and muscle relaxation.
What is the Best Treatment for Nerve Pain?
A combination of the following treatments offers the best results:
1. Anti-Inflammatory Diet
- Foods to include: Fatty fish, nuts, berries, and leafy greens.
- Foods to avoid: Processed foods, excessive sugar, and alcohol.
2. Physical Therapy & Exercise
- Gentle Yoga & Tai Chi – Enhances flexibility and reduces nerve-related stress.
- Strength Training – Supports muscles affected by neuropathy.
- Walking – Improves circulation and nerve function.
3. Supplements & Vitamins
- Vitamin B12 & B6 – Essential for nerve repair.
- Alpha-Lipoic Acid – A potent antioxidant that reduces nerve pain.
- Magnesium – Helps relax nerves and reduces cramping.
How to Calm an Irritated Nerve?
- Acupuncture: Stimulates healing and improves circulation.
- Massage Therapy: Eases muscle tension and enhances blood flow.
- Essential Oils: Lavender and peppermint oils provide soothing relief.
How Do You Calm an Irritated Nervous System?
- Deep Breathing & Meditation – Help reduce stress and improve nerve health.
- Progressive Muscle Relaxation – Eases tension throughout the body.
- Hydration – Keeps nerve cells healthy and functioning properly.
What Are 7 Foods That May Heal Nerve Damage?
- Salmon & Mackerel – Rich in Omega-3s.
- Avocados – Packed with healthy fats and B vitamins.
- Nuts & Seeds – Contain essential minerals for nerve health.
- Dark Leafy Greens – Provide antioxidants and fibre.
- Eggs – A good source of Vitamin B12.
- Turmeric – Contains curcumin, a powerful anti-inflammatory.
- Berries – High in antioxidants that support nerve function.
What Drink is Good for Nerve Pain?
- Turmeric Milk – Contains anti-inflammatory curcumin.
- Green Tea – Packed with antioxidants to protect nerves.
- Carrot & Beetroot Juice – Supports circulation and nerve health.
How to Sleep Through Nerve Pain?
- Use a Weighted Blanket – Provides soothing pressure that calms nerves.
- Sleep Positioning – Elevate legs or use a body pillow for support.
- Relaxation Techniques – Try deep breathing exercises before bed.
What is the Best Cream for Nerve Pain?
- Capsaicin Cream – Helps reduce pain sensitivity.
- CBD Cream – May relieve inflammation and pain.
- Lidocaine Patches – Numbs the affected area for temporary relief.
Does Nerve Pain Go Away?
Nerve pain can be managed and, in some cases, reduced significantly. Early intervention, lifestyle changes, and targeted therapies can help prevent worsening symptoms.
Is Hot Water Good for Nerve Pain?
Warm baths or hot compresses can help relax muscles and improve blood flow, providing temporary relief from nerve pain.
Does Massage Help Nerve Pain?
Yes, massage therapy can:
- Stimulate Circulation – Enhances blood flow to damaged nerves.
- Reduce Muscle Tension – Helps relieve associated discomfort.
- Encourage Healing – Aids in toxin removal from the body.
How Can I Stop Nerve Pain Permanently?
- Identify & Treat Underlying Causes – Such as diabetes or vitamin deficiencies.
- Adopt a Healthy Lifestyle – Prioritize diet, exercise, and stress management.
- Seek Professional Guidance – Consult a doctor for tailored treatments.
What is the Best Exercise for Nerve Damage?
- Low-Impact Workouts: Walking, swimming, and cycling.
- Stretching & Yoga: Helps improve flexibility and nerve function.
- Strength Training: Builds muscle support for weakened nerves.
Do Bananas Help Nerve Pain?
Yes, bananas are high in potassium and magnesium, which are beneficial for nerve function and reducing muscle cramps.
Conclusion
Nerve pain doesn't have to control your life. By integrating these 10 proven strategies, you can take charge of your symptoms and regain mobility, comfort, and well-being.
For expert insights on managing nerve pain and exploring the latest treatments, visit Dr. Chandril Chugh's website for professional advice.
Mind-Body Techniques for Nerve Healing: Stress Reduction & More
Ever feel like your nerves are frayed, buzzing with phantom pain or tingling sensations long after an injury should have healed? Like a tangled Christmas light string, sometimes our nervous system gets a little…wonky. While medical interventions are crucial, what if you could actively participate in your nerve-healing journey?
Imagine rewiring your internal circuitry, not with scalpels and sutures, but with the power of your mind and body. This isn't some mystical, far-fetched concept. We're talking about scientifically-backed mind-body techniques – practical tools like meditation, mindfulness, and targeted movement – that can soothe an agitated nervous system, reduce stress (a notorious nerve irritant!), and pave the way for healing. Ready to ditch the "pins and needles" anxiety and discover how to harness your inner pharmacy for nerve regeneration? Let's explore the fascinating world where ancient wisdom meets modern science and unlock the potential for a calmer, more connected you.
Understanding Nerve Damage
Nerve damage, also known as neuropathy, occurs when nerve fibres become injured, leading to pain, numbness, and muscle weakness. Diabetes, trauma, infections, vitamin deficiencies, and chronic inflammation can cause it.
Common Causes of Nerve Damage:
- Diabetes: High blood sugar levels damage nerves over time.
- Nutritional Deficiencies: Lack of essential vitamins, especially B-complex vitamins.
- Autoimmune Disorders: Conditions like lupus and multiple sclerosis can lead to nerve damage.
- Toxic Exposure: Heavy metals, alcohol, and certain medications can harm nerves.
Can Nerve Damage Be Healed Naturally?
Yes, nerve damage can be repaired naturally with the right strategies, including nutrition, lifestyle changes, and stress management.
1. Nutrient-rich diet for Nerve Repair
Certain foods and vitamins are essential for nerve regeneration.
- Vitamin B12: Supports nerve function and prevents further damage.
- Omega-3 Fatty Acids: Found in salmon, flaxseeds, and walnuts, these promote nerve health.
- Antioxidant-Rich Foods: Berries, leafy greens, and turmeric help combat inflammation.
- Magnesium: Helps with nerve relaxation and reduces nerve pain.
What Makes Nerves Heal Faster?
Speeding up nerve healing requires a combination of proper nutrition, blood circulation, and stress reduction.
1. Exercise for Nerve Regeneration
- Gentle Stretching: Improves flexibility and reduces stiffness.
- Low-Impact Activities: Walking, swimming, and yoga enhance circulation and nerve healing.
- Strength Training: Builds muscle support for weakened nerves.
2. Mind-Body Techniques for Stress Reduction
Chronic stress can exacerbate nerve pain and slow healing. Incorporating relaxation techniques can significantly aid recovery.
- Meditation & Deep Breathing: Reduces nerve-related stress and promotes overall well-being.
- Tai Chi & Yoga: Gentle movements help improve nerve function and reduce inflammation.
- Progressive Muscle Relaxation: Helps calm the nervous system and ease nerve pain.
What Are 7 Foods That May Heal Nerve Damage?
Including the following foods in your diet can accelerate nerve repair:
- Fatty Fish (Salmon, Mackerel) – Rich in Omega-3s.
- Avocados – High in healthy fats and B vitamins.
- Nuts & Seeds (Almonds, Chia Seeds) – Contain essential minerals for nerve function.
- Dark Leafy Greens (Spinach, Kale) – Packed with antioxidants.
- Eggs – A great source of Vitamin B12.
- Turmeric – Contains curcumin, a powerful anti-inflammatory agent.
- Berries – High in antioxidants that combat nerve damage.
Can Damaged Nerves Be Restored?
Yes, nerves can regenerate if given the right conditions. Proper nutrition, hydration, and exercise are key components in this healing process.
Additional Strategies:
- Cold & Hot Therapy: Alternating ice packs and warm compresses can improve nerve function.
- Essential Oils: Lavender and peppermint oils may help alleviate nerve pain.
- Hydration: Drinking enough water supports cell regeneration and nerve function.
FAQs
Q: Can nerves take 2 years to heal?
A: Yes, nerve regeneration is slow. It can take months to years, depending on the severity of the damage.
Q: Which vitamin is best for nerve repair?
A: Vitamin B12, B6, and Alpha-Lipoic Acid are essential for nerve healing.
Q: Which fruit is best for nerve health?
A: Berries and avocados are rich in antioxidants and healthy fats that support nerve repair.
Q: What is the best exercise for nerve damage?
A: Low-impact exercises like yoga, tai chi, and swimming improve circulation and aid nerve healing.
Q: Is milk good for nerves?
A: Yes, milk contains calcium and B vitamins that help maintain nerve health.
Q: Which juice is good for nerves?
A: Carrot and beetroot juices are excellent for promoting nerve health.
Q: Can fasting reverse nerve damage?
A: Intermittent fasting may help reduce inflammation and promote cellular repair.
Q: What stops nerve pain immediately?
A: Applying ice, deep breathing, and using capsaicin cream can provide temporary relief.
Q: Can you live a long life with nerve damage?
A: Yes, with proper management, lifestyle adjustments, and care, many people live long and fulfilling lives with neuropathy.
Q: What is the best drink for nerve pain?
A: Green tea, turmeric milk, and herbal teas can help soothe nerve pain.
Q: Is egg good for nerve pain?
A: Yes, eggs are rich in choline and B vitamins, which support nerve health.
Conclusion
Healing damaged nerves naturally is a journey that combines proper nutrition, exercise, and stress reduction. While nerve regeneration takes time, incorporating these mind-body techniques and lifestyle changes can significantly improve nerve health and reduce pain.
For expert guidance on managing nerve damage, visit Dr. Chandril Chugh's website for professional advice on holistic nerve healing.
Call-to-Action: Ready to start your nerve repair journey? Implement these natural strategies today and share your progress in the comments below!
Foot Neuropathy and Diabetes: Special Considerations
Imagine your feet as your body's roots, grounding you in the world. Now, picture those roots slowly losing sensation, becoming numb to the very ground you walk on. This is the reality for millions living with diabetes and foot neuropathy. But it doesn't have to be a future of fear and uncertainty. Understanding the connection between diabetes and nerve damage is the first step towards protecting your 'roots' and stepping confidently into a healthier tomorrow.
In this article, we'll explore the best foot neuropathy treatment options, focusing on natural remedies, lifestyle adjustments, and holistic approaches that can help soothe nerve pain and improve mobility.
Understanding Foot Neuropathy
Foot neuropathy is a condition that affects the peripheral nerves, leading to numbness, tingling, burning pain, and weakness in the feet. It is commonly linked to diabetes, infections, vitamin deficiencies, and prolonged nerve damage.
Causes of Foot Neuropathy
- Diabetes – High blood sugar levels damage nerve fibres over time.
- Vitamin Deficiencies – Lack of B vitamins can lead to nerve dysfunction.
- Infections and Autoimmune Disorders – Conditions like Lyme disease and lupus can contribute to nerve pain.
- Chronic Alcohol Use – Excessive alcohol consumption can cause nerve damage.
How to Relieve Neuropathy in Feet?
Managing neuropathy symptoms involves a combination of lifestyle changes, natural remedies, and self-care practices.
1. Improve Blood Circulation
Good circulation helps nerves function properly. Here are a few ways to enhance blood flow:
- Massage Therapy – Gently massaging your feet increases circulation and relieves pain.
- Warm Foot Soaks – Soaking feet in warm water with Epsom salt can relax muscles and improve circulation.
- Compression Socks – These help promote blood flow and reduce discomfort.
2. Anti-Inflammatory Diet for Nerve Health
A balanced diet can help reduce inflammation and improve nerve function.
- Omega-3 Fatty Acids – These are found in fish, flaxseeds, and walnuts and reduce inflammation.
- Leafy Greens and Berries – Packed with antioxidants to protect nerve cells.
- Whole Grains – Help stabilize blood sugar levels, which is crucial for diabetic neuropathy.
What is the Most Effective Treatment for Neuropathy?
The best treatment depends on the severity of the condition and underlying causes.
1. Vitamin and Supplement Support
- Vitamin B12 – Essential for nerve repair and protection.
- Alpha-Lipoic Acid – A powerful antioxidant that reduces pain and improves nerve function.
- Magnesium – Helps relax nerves and reduce cramping.
2. Acupuncture for Pain Relief
This ancient therapy helps improve circulation, stimulate nerve healing, and reduce pain intensity.
3. Physical Therapy and Exercise
- Walking and Stretching – Keeps nerves active and prevents muscle loss.
- Balance Training – Reduces the risk of falls due to numbness.
- Yoga and Tai Chi – Promote relaxation and improve nerve function.
Is Vicks VapoRub Good for Neuropathy in Feet?
Vicks VapoRub contains menthol and camphor, which provide a cooling sensation and temporary pain relief. While it may help ease symptoms for some, it is not a long-term solution for neuropathy.
Can I Live a Long Life with Neuropathy?
Yes, neuropathy can be managed effectively with the right lifestyle and medical interventions. By maintaining blood sugar control, adopting a healthy lifestyle, and following treatment recommendations, individuals with neuropathy can enjoy a long and active life.
Conclusion
Foot neuropathy doesn't have to define your life. By implementing natural foot neuropathy treatment strategies like dietary changes, exercise, and holistic remedies, you can regain control and improve your quality of life.
For expert insights on managing neuropathy and diabetes-related nerve damage, visit Dr. Chandril Chugh's website.
FAQs
Q: What are the early signs of foot neuropathy?
A: Numbness, tingling, burning sensations, and weakness in the feet are common early symptoms.
Q: Can neuropathy in feet be reversed?
A: Early intervention, blood sugar control, and lifestyle modifications can help slow progression and, in some cases, improve symptoms.
Q: What home remedies help with foot neuropathy?
A: Foot massage, warm soaks, essential oils, and an anti-inflammatory diet can provide relief.
Q: Should I see a doctor for foot neuropathy?
A: Yes, if symptoms persist or worsen, consult a healthcare provider for proper evaluation and treatment.
Natural Remedies for Neuropathy: Healing Nerve Pain Without Medication
Say Goodbye to Neuropathy: Natural Treatments That Work
Tingling toes? Burning feet? Is that electric shock sensation shooting up your leg? If these unwelcome guests have crashed your party of pain-free living, you might be dealing with neuropathy. This frustrating nerve condition can steal your comfort and limit your mobility, making even simple tasks feel like climbing a mountain. But before you resign yourself to a life of discomfort, take a deep breath.
"Say Goodbye to Neuropathy: Natural Treatments That Work" is your guide to reclaiming your well-being. We'll delve into the world of natural remedies for neuropathy and explore effective and accessible options that can help soothe those irritated nerves and get you back on your feet – literally! From dietary tweaks and targeted supplements to mindful movement and ancient healing practices, discover the power of nature to combat neuropathy and rediscover the joy of a pain-free life. Are you ready to say goodbye to neuropathy and hello to a healthier, happier you? Let's explore!
Understanding Neuropathy
Neuropathy is a condition that affects the peripheral nerves, leading to symptoms such as numbness, tingling, burning sensations, and even muscle weakness. Diabetes, autoimmune diseases, infections, or prolonged exposure to toxins often cause it.
To better understand how to tackle neuropathy naturally, visit Dr. Chandril Chugh's website for expert insights on nerve health and holistic healing approaches.
Natural Remedies for Neuropathy
1. Optimize Your Diet for Nerve Health
What you eat plays a crucial role in nerve function. Nutrient-rich foods can support nerve repair and reduce inflammation.
- Healthy Fats: Omega-3 fatty acids found in salmon, flaxseeds, and walnuts help reduce inflammation.
- Antioxidant-Rich Foods: Berries, spinach, and carrots protect nerve cells from oxidative damage.
- Whole Grains: Brown rice, quinoa, and oats stabilize blood sugar levels, which is essential for diabetic neuropathy.
For more on how diet influences nerve health, check out Dr. Chugh's recommendations on neurological care.
2. Herbal Treatments for Neuropathy
Herbs have been used for centuries to support nerve function and reduce pain naturally.
- Turmeric: It contains curcumin, a powerful anti-inflammatory compound that eases nerve pain.
- Ginkgo Biloba: Improves blood circulation, enhancing nerve regeneration.
- Cayenne Pepper: Contains capsaicin, which is known to reduce pain perception when used topically.
3. Vitamins and Supplements for Nerve Regeneration
Certain vitamins and minerals can help prevent and even reverse neuropathy symptoms.
- Vitamin B12: Essential for nerve repair and myelin sheath protection.
- Alpha-Lipoic Acid: A potent antioxidant that reduces nerve pain and improves function.
- Magnesium: Supports nerve transmission and can help ease muscle cramps.
4. Acupuncture for Nerve Relief
Acupuncture is an ancient Chinese therapy that involves inserting thin needles into specific points on the body. Research suggests that it can improve blood circulation, reduce nerve pain, and stimulate healing in neuropathy patients.
To explore holistic approaches to nerve pain management, read more on Dr. Chugh's neurology expertise.
5. Exercise and Movement Therapy
Gentle physical activity helps improve circulation, strengthen muscles, and alleviate neuropathic pain.
- Walking: Increases blood flow to nerves, reducing numbness and tingling.
- Yoga: Enhances flexibility and promotes relaxation, reducing nerve stress.
- Strength Training: Helps maintain muscle mass and prevent weakness caused by neuropathy.
6. Essential Oils for Neuropathy Relief
Aromatherapy can provide soothing relief for nerve pain and inflammation. Some beneficial essential oils include:
- Lavender Oil: Known for its calming and anti-inflammatory properties.
- Peppermint Oil: Provides a cooling sensation and reduces nerve pain.
- Eucalyptus Oil: Enhances circulation and relieves muscle tension.
7. Mind-Body Techniques
Stress can exacerbate neuropathic symptoms, making relaxation techniques essential.
- Meditation and Deep Breathing: Help lower stress levels and promote overall well-being.
- Progressive Muscle Relaxation: Eases nerve-related tension and pain.
- Tai Chi: A gentle exercise that improves balance and nerve function.
What is the Best Herb for Neuropathy?
Suppose you’re looking for the most effective herbal remedy for neuropathy. In that case, turmeric stands out due to its strong anti-inflammatory effects. Studies suggest that curcumin, the active compound in turmeric, can help alleviate nerve pain and reduce inflammation.
What Drink is Good for Neuropathy?
Staying hydrated and choosing the right beverages can make a difference.
- Green Tea: Loaded with antioxidants that support nerve health.
- Warm Water with Lemon: It aids in detoxification and improves circulation.
- Golden Milk (Turmeric Latte): Combines turmeric with warm milk for an anti-inflammatory boost.
What Vitamin Gets Rid of Neuropathy?
Among essential vitamins for nerve health, Vitamin B12 plays a crucial role in nerve repair and function. Deficiency in B12 can lead to worsening neuropathy symptoms, so ensuring an adequate intake through diet or supplementation is vital.
Conclusion
Neuropathy doesn’t have to control your life. By embracing natural remedies for neuropathy, you can take significant steps towards healing and pain relief. From nutrient-rich foods and herbal treatments to exercise and relaxation techniques, these holistic approaches can provide lasting relief.
If you're struggling with neuropathy and want expert guidance, visit Dr. Chandril Chugh's website for professional advice on nerve health and natural treatments.
Nerve Pain Relief: Beyond the Pills
Nerve pain can be a relentless, disruptive force, impacting every aspect of your life. It's often described as a burning, stabbing, or electric-like sensation that can make even simple tasks unbearable. Whether it’s diabetic neuropathy, sciatica, post-surgical nerve damage, or another condition, living with nerve pain can feel like a daily battle.
While medications for nerve pain can play a role in managing symptoms, they’re not always enough—and in some cases, they come with unwanted side effects. That’s why many people seek alternative solutions to find relief and reclaim their quality of life.
This article explores a range of strategies that go beyond pills to address nerve pain. We’ll delve into:
The best medications for nerve pain and how they work
Lifestyle changes that support long-term relief
Complementary therapies like acupuncture and physical therapy
Self-management techniques to improve daily function
If you’re tired of constant discomfort and want a holistic approach to managing nerve pain, keep reading. Relief is possible!
Understanding Nerve Pain: Why Is It So Difficult to Treat?
What Causes Nerve Pain?
Nerve pain, also called neuropathic pain, occurs when nerves are damaged or misfire, sending faulty pain signals to the brain. Unlike regular pain from injuries or muscle strain, nerve pain persists even when there’s no clear external cause.
Common Causes of Nerve Pain:
Diabetes (Diabetic Neuropathy) – High blood sugar damages nerves over time.
Injuries & Surgeries – Trauma or surgery can lead to nerve damage.
Autoimmune Diseases – Conditions like multiple sclerosis (MS) and lupus attack nerves.
Shingles (Postherpetic Neuralgia) – The shingles virus can leave lasting nerve pain.
Chemotherapy (Chemo-Induced Neuropathy) – Certain cancer treatments damage nerves.
Why Is Nerve Pain Hard to Treat?
Unlike muscle pain or arthritis, nerve pain doesn’t always respond to traditional painkillers like ibuprofen or acetaminophen. Instead, doctors often prescribe medications designed for nerve function—but even these don’t work for everyone.
So, what’s the best medication for nerve pain, and what other options exist for lasting relief? Let’s explore.
Best Medication for Nerve Pain: What Really Works?
Medications for nerve pain work by modulating nerve signals or reducing inflammation. Here are the most commonly prescribed options:
1. Anticonvulsants (Nerve-Stabilizing Medications)
Best for: Diabetic neuropathy, postherpetic neuralgia, sciatica
How They Work: Originally developed for epilepsy, these drugs calm overactive nerve signals, reducing pain intensity.
Gabapentin (Neurontin) – One of the most common nerve pain meds
Pregabalin (Lyrica) – FDA-approved for fibromyalgia & nerve pain
Side Effects: Drowsiness, dizziness, weight gain
2. Antidepressants (Mood & Pain Modulators)
Best for: Fibromyalgia, chronic nerve pain, migraines
How They Work: These drugs increase serotonin and norepinephrine, helping dampen nerve pain signals.
Amitriptyline – A tricyclic antidepressant often prescribed for nerve pain
Duloxetine (Cymbalta) – FDA-approved for diabetic neuropathy & fibromyalgia
Side Effects: Dry mouth, fatigue, nausea
3. Pain Relievers (NSAIDs & Opioids: Limited Use)
Best for: Short-term relief of severe nerve pain
How They Work: These medications reduce inflammation or block pain signals in the nervous system.
NSAIDs (Ibuprofen, Naproxen) – Mild relief for inflammation-related nerve pain
Tramadol – A weak opioid sometimes used for severe neuropathic pain
Warning: Opioids are not a first-line treatment for nerve pain due to the risk of addiction and tolerance development.
4. Topical Treatments (Creams & Patches)
Best for: Localized nerve pain (post-shingles, small fiber neuropathy)
How They Work: Directly applied to the skin, these treatments desensitize nerves.
Lidocaine Patches – Blocks nerve signals to reduce pain
Capsaicin Cream – Uses chili pepper extract to “burn out” pain receptors
Signal Relief Patch - Uses a unique non-chemical approach to help disrupt pain signals, offering reusable relief without any active ingredients
Side Effects: Skin irritation, redness
Beyond Medications: Alternative Treatments for Nerve Pain Relief
While medications for nerve pain can be helpful, they’re only part of the solution. Let’s explore alternative therapies that can work alongside medications—or even replace them.
1. Physical Therapy & Exercise
Why It Works: Improves circulation, strengthens muscles, and reduces nerve compression.
Gentle stretching & strengthening exercises
Nerve glide exercises for carpal tunnel & sciatica
Low-impact activities like swimming or yoga
2. Acupuncture & Chiropractic Care
Why It Works: Stimulates nerve function and releases pain-blocking endorphins.
Acupuncture improves nerve circulation and reduces inflammation
Chiropractic adjustments can relieve nerve pressure
3. Nerve Stimulation Therapies (TENS & PEMF)
Why It Works: Sends mild electrical impulses to disrupt pain signals.
TENS (Transcutaneous Electrical Nerve Stimulation) – Helps retrain nerves
PEMF (Pulsed Electromagnetic Field Therapy) – Enhances nerve regeneration
4. Supplements for Nerve Health
Why They Work: Certain vitamins and minerals help repair damaged nerves.
Vitamin B12 – Crucial for nerve repair
Alpha-Lipoic Acid (ALA) – Reduces nerve inflammation
Magnesium – Supports nerve signaling and muscle relaxation
Omega-3s – Repairs nerve membranes
5. Mind-Body Techniques (Stress Management)
Why It Works: Chronic stress worsens nerve pain by increasing inflammation.
Meditation & deep breathing exercises
Biofeedback therapy to control pain perception
Cognitive Behavioral Therapy (CBT) for pain coping strategies
Lifestyle Changes That Support Nerve Pain Management
While medications help manage symptoms, long-term relief requires lifestyle changes.
Healthy Diet – Focus on anti-inflammatory foods like leafy greens, salmon, and nuts.
Regular Movement – Even short walks increase circulation to nerves.
Better Sleep – Poor sleep worsens nerve pain sensitivity.
Limit Alcohol & Sugar – Both can damage nerves over time.
Final Thoughts: Finding the Best Medication for Nerve Pain
If you’re struggling with chronic nerve pain, remember: there’s no one-size-fits-all solution. The best approach often involves a combination of medications, alternative therapies, and lifestyle adjustments.
Key Takeaways:
Gabapentin & Pregabalin – Best for nerve signal regulation
Duloxetine & Amitriptyline – Modulate pain perception
Topical treatments (Lidocaine, Capsaicin) – Offer localized relief
Physical therapy & exercise – Strengthen the nervous system
Acupuncture & nerve stimulation – Promote healing naturally
Supplements & diet changes – Support long-term nerve health
If medications aren’t enough, don’t lose hope! Many alternative solutions exist that can provide lasting relief.
Nerve Damage Doesn't Have to Be Forever: Exploring the Possibilities of Repair
Imagine waking up every morning with numb fingers, a burning sensation in your feet, or a sharp, stabbing pain that won't go away. Everyday tasks—like buttoning a shirt, holding a coffee cup, or even walking—become frustrating challenges. If this sounds familiar, you might be dealing with nerve damage, a condition that affects millions of people worldwide.
For many, the biggest question remains: Can nerve damage be repaired?
The nervous system is complex, and traditional medicine has long suggested that once nerves are damaged, there's no going back. But recent scientific advancements are proving otherwise. Nerve regeneration is possible, and while it may not happen overnight, the right therapies, nutrients, and lifestyle changes can help nerves heal and even regrow.
If you've been told that nerve damage is permanent, don't lose hope just yet. This article dives deep into the science of nerve repair, exploring:
How nerves regenerate and what slows the process
Cutting-edge treatments and therapies that stimulate healing
Natural remedies, supplements, and exercises that support nerve repair
How long it really takes for nerves to heal
Let's break the myth that nerve damage is a life sentence—because healing is possible.
Understanding Nerve Damage: What's Really Happening?
How Do Nerves Get Damaged?
Your nervous system is a vast network of cells that transmit signals between your brain, spinal cord, and the rest of your body. When nerves are damaged, these signals are disrupted, leading to:
- Tingling, numbness, or burning sensations
- Weakness or muscle atrophy
- Pain that ranges from mild to debilitating
- Loss of reflexes or motor control
Common causes of nerve damage include:
- Diabetes – High blood sugar levels damage nerves over time.
- Physical injuries – Car accidents, surgeries, or repetitive strain can crush or sever nerves.
- Autoimmune diseases – Conditions like multiple sclerosis or lupus attack nerve tissue.
- Toxic exposure – Heavy metals, alcohol, and chemotherapy drugs can impair nerve function.
- Vitamin deficiencies – Lack of B vitamins, magnesium, or omega-3s can slow nerve repair.
Types of Nerve Damage
There are different kinds of nerve damage, and understanding them helps determine the best repair strategies:
- Peripheral Neuropathy – Damage to nerves outside the brain and spinal cord, often in hands and feet.
- Autonomic Neuropathy – Affects automatic functions like digestion and blood pressure.
- Motor Neuropathy – This leads to muscle weakness and movement issues.
- Sensory Neuropathy – Causes tingling, pain, or numbness in affected areas.
Now that we know what nerve damage is, let's dive into the big question: Can nerve damage be repaired?
The Science of Nerve Regeneration: Fact or Fiction?
Do Nerves Actually Regrow?
Yes—but it depends on the type and extent of damage.
- Central Nervous System (CNS) Damage (Brain & Spinal Cord):
- Nerves in the brain and spinal cord are the hardest to regenerate because scar tissue forms quickly, blocking repair.
- However, new research in stem cell therapy and nerve grafting is promising.
- Peripheral Nervous System (PNS) Damage (Arms, Legs, Hands, Feet):
- Peripheral nerves CAN regenerate, but slowly—at about 1 millimetre per day.
- With the right nutrients, therapies, and nerve stimulation, the process can be accelerated.
So, while nerve repair isn't instant, science confirms that recovery is possible—especially with targeted treatments.
Breakthrough Therapies for Nerve Repair
If you're wondering, "Can nerve damage be repaired?” these cutting-edge approaches are proving that it's possible:
1. Stem Cell Therapy: The Future of Nerve Repair
Stem cells can regenerate nerve tissue and reduce inflammation.
Some studies show success in spinal cord injury repair and severe neuropathy cases.
2. Electrical Stimulation Therapy (TENS & PEMF)
TENS units (Transcutaneous Electrical Nerve Stimulation) help retrain nerves to send proper signals.
PEMF therapy (Pulsed Electromagnetic Field) stimulates nerve regrowth.
3. Platelet-Rich Plasma (PRP) Therapy
PRP uses growth factors from your blood to repair damaged nerves.
Used for injuries and post-surgical nerve healing.
4. Hyperbaric Oxygen Therapy (HBOT)
Increases oxygen to damaged nerves, speeding up regeneration and reducing pain.
These advanced therapies are changing the game for people with severe nerve damage. But what about natural remedies?
Natural Strategies to Boost Nerve Healing
While high-tech treatments are exciting, natural approaches also play a crucial role in nerve repair.
1. The Best Diet for Nerve Repair
What you eat directly impacts nerve regeneration.
Eat More:
- Leafy greens (spinach, kale)
- Fatty fish (salmon, sardines)
- Nuts & seeds (walnuts, flaxseeds)
- Avocados & olive oil
- Turmeric & ginger
Avoid:
- Processed sugars & refined carbs
- Alcohol & artificial sweeteners
- Fried & processed foods
2. Supplements for Nerve Repair
Certain vitamins and minerals help regenerate nerves faster.
Best Supplements for Nerve Healing:
- Vitamin B12 – Essential for nerve regeneration
- Alpha-lipoic acid (ALA) – Reduces inflammation
- Acetyl-L-Carnitine – Boosts nerve function
- Magnesium – Supports nerve signals
- Omega-3 Fatty Acids – Repairs nerve membranes
3. Exercise & Movement Therapy
Gentle movement increases circulation, delivering oxygen to healing nerves.
- Walking (15-30 minutes a day)
- Yoga & stretching
- Strength training (with low impact)
4. Mind-Body Therapies
- Managing stress is crucial for nerve healing.
- Best Relaxation Techniques:
- Deep breathing exercises
- Meditation & mindfulness
- Acupuncture for pain relief
5. Sleep & Nerve Recovery
- Nerves heal the most while you sleep!
- Sleep Hacks for Faster Healing:
- Keep a consistent bedtime
- Avoid screens before bed
- Try magnesium or chamomile tea for relaxation
FAQs: Can Nerve Damage Be Repaired?
1. How Long Does It Take for Nerves to Regrow?
Peripheral nerves grow 1mm per day—meaning full recovery can take weeks to years, depending on the damage.
2. What Foods Speed Up Nerve Healing?
Fatty fish, leafy greens, nuts, avocados, and turmeric all help reduce inflammation and support nerve repair.
3. Can Exercise Help Repair Nerves?
Yes! Movement increases circulation, helping deliver nutrients to damaged nerves.
4. Are There Any Medications That Help Nerve Regeneration?
Some medications like Gabapentin help manage symptoms, but natural therapies often work better for repair.
Final Thoughts: Can Nerve Damage Be Repaired?
YES! While nerve repair takes time, the right nutrition, therapies, and lifestyle changes can stimulate healing and restore function.
Start today: Every small change helps.
Be patient: Nerve healing takes time.
Stay consistent: The best results come with a routine.
Is It Possible to Reverse Neuropathy Fast? What a Neurologist Says
Tired of simply coping with the relentless tingling, numbness, and pain of neuropathy? It’s time to take charge and explore long-term solutions that can truly make a difference.
This article serves as your comprehensive guide, empowering you to:
- Understand neuropathy and its causes
- Identify personal triggers
- Implement effective, evidence-based strategies
- Reclaim your quality of life
Many people search for quick fixes, wondering if they can reverse neuropathy in 7 days. But is that fact or fiction? While nerve regeneration is a slow process, significant improvements can begin in a week if you take the right approach.
With a proactive mindset focused on long-term management, you can minimize neuropathy’s impact and improve your overall well-being. We’ll explore practical lifestyle adjustments, emerging therapies, and proven strategies that will empower you on your journey to better neuropathy management.
Can You Reverse Neuropathy in 7 Days?
Fact or Fiction?
Many people suffering from neuropathy want immediate relief, leading to claims that you can reverse neuropathy in 7 days. But here’s the truth:
You CAN start reducing symptoms in 7 days with the right approach.
You CAN’T completely reverse nerve damage in a week—nerve regeneration takes time.
So, what’s possible in 7 days?
- Reducing inflammation that worsens nerve pain
- Improving circulation to help nerves heal faster
- Boosting essential nutrients for nerve repair
- Minimizing triggers that aggravate neuropathy
If you stick to long-term strategies, you can dramatically improve neuropathy symptoms over weeks or months.
Understanding Neuropathy: Why Do Nerves Get Damaged?
Neuropathy happens when nerves become damaged or dysfunctional, affecting how they communicate with the brain. This leads to symptoms like:
- Tingling or numbness in hands and feet
- Sharp, burning, or stabbing pain
- Muscle weakness and poor coordination
- Sensitivity to temperature or touch
What Causes Neuropathy?
- Diabetes – High blood sugar damages nerves over time.
- Vitamin Deficiencies – Lack of B12, folate, and vitamin D weakens nerves.
- Autoimmune Diseases – Conditions like lupus and rheumatoid arthritis can trigger nerve damage.
- Toxin Exposure – Alcohol, heavy metals, and certain medications harm nerves.
- Injuries & Pressure – Pinched nerves from repetitive stress or trauma.
The good news? If you address the root cause, nerve regeneration is possible!
7-Day Plan to Jumpstart Neuropathy Recovery
While full nerve regeneration takes time, here’s what you can start doing TODAY to see improvements in just 7 days.
Day 1: Anti-Inflammatory Diet for Nerve Repair
What you eat directly impacts nerve health. A high-inflammation diet makes symptoms worse, while a nerve-friendly diet speeds up healing.
Eat More:
- Leafy greens (spinach, kale)
- Fatty fish (salmon, sardines)
- Nuts & seeds (almonds, flaxseeds)
- Avocados & olive oil
- Turmeric & ginger
Avoid:
- Processed sugars & refined carbs
- Alcohol & artificial sweeteners
- Fried & processed foods
Day 2: Hydration & Electrolyte Balance
- Nerves need proper hydration to function. Dehydration leads to poor circulation and nerve damage.
- Drink at least 8 glasses of water daily.
- Add electrolytes (magnesium, potassium) for better nerve signalling.
Day 3: Targeted Supplements for Nerve Healing
- Certain vitamins and minerals help regenerate nerves faster.
- Best Supplements for Neuropathy:
- Vitamin B12 (1,000-5,000 mcg daily) – Essential for nerve repair
- Alpha-Lipoic Acid (ALA) (600-1,200 mg daily) – Reduces nerve pain
- Acetyl-L-Carnitine (500-1,500 mg daily) – Boosts nerve regeneration
- Magnesium (300-400 mg daily) – Supports nerve function
- Omega-3 Fatty Acids (1,000-2,000 mg daily) – Reduces inflammation
Day 4: Gentle Exercise & Movement
- Exercise increases blood flow to nerves, improving healing.
- Best Exercises for Neuropathy:
- Walking (15-30 minutes)
- Yoga & stretching
- Swimming or cycling
- Resistance band training
- Avoid high-impact workouts that worsen nerve pain.
Day 5: Stress Reduction & Better Sleep
- Chronic stress raises cortisol, which damages nerves. Poor sleep slows healing.
- Best Relaxation Techniques:
- Deep breathing (4-7-8 method)
- Meditation or mindfulness
- Herbal teas (chamomile, valerian root)
- Sleep Hacks for Nerve Repair:
- Keep a consistent bedtime
- Use a cool, dark room
- Avoid screens 1 hour before bed
Day 6: Alternative Therapies for Nerve Pain
- Some emerging therapies help relieve neuropathy symptoms faster.
- Infrared Light Therapy – Increases circulation, reduces nerve pain
- Acupuncture – Stimulates nerve healing
- TENS Therapy – Blocks nerve pain signals
Day 7: Tracking Progress & Long-Term Adjustments
By Day 7, you should start feeling less inflammation, better circulation, and slight symptom relief. Now, it’s time to track what works and adjust for long-term success.
Neuropathy Symptom Journal:
- Record pain levels, triggers, and improvements
- Track diet, supplements, and exercise habits
- Adjust your routine based on what helps most
Beyond 7 Days: Long-Term Strategies for Neuropathy Management
The first 7 days lay the foundation, but real nerve repair takes months. Here’s how to keep improving:
- Stick to an anti-inflammatory diet
- Continue nerve-healing supplements
- Stay active with gentle exercise
- Prioritize stress management & sleep
- Try physical therapy or acupuncture
With consistency, many people experience significant neuropathy relief in 3-6 months.
FAQs About Reversing Neuropathy
1. Can Neuropathy Really Be Reversed?
Yes! If you identify the cause and use targeted strategies, nerve healing is possible.
2. How Long Does It Take to Reverse Neuropathy?
Some people see improvements in weeks, while full nerve healing can take months to years, depending on severity.
3. What Foods Help Heal Nerves?
Eat omega-3-rich foods, leafy greens, nuts, turmeric, and magnesium-rich foods for faster recovery.
4. Are Medications Necessary for Neuropathy?
Not always. Medications manage pain but don’t fix nerve damage. A holistic approach is often more effective.
5. Can Exercise Help Neuropathy?
Yes! Movement improves circulation, which speeds up nerve healing.
Final Thoughts: Take Control of Your Nerve Health
While you can’t fully reverse neuropathy in 7 days, you CAN kickstart your recovery and see real improvements. By combining nutrition, supplements, exercise, and stress reduction, you’ll feel better every week.
Start today – Every small change helps.
Be patient – Nerve healing takes time.
Stay consistent – The best results come with a routine.