Alternative Treatments for Epilepsy: Exploring Non-Traditional Options
If you or a loved one has epilepsy, you might look at treatments beyond the usual drugs. In the United States, choosing other ways to treat epilepsy is not that common anymore. Yet, there are always new alternative methods appearing. It is good to know the pluses and minuses of different treatments to make smart health choices.
Big names in medicine check traditional epilepsy treatments closely. They tell us what works, the side effects, and the dangers. However, not all new or different treatments get this same tight check. So, we might not know as much about how safe and helpful they are. Even so, some of these less common treatments could help, even if we don't have as much proof.
Disclaimer: Never leave or change your epilepsy medications without talking to your neurologist. Whenever you try alternative forms of treatment remember to discuss the same with your neurologist.
Understanding Complementary and Alternative Treatments
In healthcare, people are more interested in alternative and complementary treatments. These happen apart from the usual medicine. They can be used with, or instead of, standard treatments for health conditions like epilepsy. Knowing about these different therapies and integrative medicine can help you make better health choices.
Defining Complementary and Alternative Approaches
Complementary treatments work with standard medicine. Alternative treatments replace standard medicine. Often, using a mix of both can be the best.
Types of Complementary and Alternative Therapies
There are many types of these therapies for epilepsy and more. They include natural products and mind-body practices. Researchers study these therapies to find out how well they work and if they're safe.
Integrative Medicine: Combining Traditional and Non-Traditional Treatments
Integrative medicine combines traditional and alternative care. It offers a complete treatment that looks at physical and mental health. In the U.S., more doctors are using alternative therapies alongside standard care.
The Need for alternative treatments for epilepsy
Prevalence and Impact of Epilepsy
Epilepsy affects over 70 million worldwide. No matter your age, gender, race, or where you live, you could have it. The causes can be from your family, health issues, infections, and other reasons. Some causes are still not known.
Limitations of Conventional Antiepileptic Drugs
Today, many with epilepsy use common drugs to keep their seizures under control. But these drugs can cause problems. They might mix badly with other drugs, not work for some people, and bring strong side effects. Because of this, many are looking into natural ways to help.
Potential Benefits of Natural and Alternative Therapies
People are looking at natural ways to fight epilepsy for a few good reasons. First, they hope to find ways that work better with fewer bad effects. Second, they believe these ways will fit better with taking care of the whole body. For example, using herbs, changing your diet, and doing specific exercises could help in unique ways. They might change how epilepsy works inside you, cut down on stress, and make you feel better.

| Therapy | Potential Benefits | Limitations |
|---|---|---|
| Ketogenic Diet | Helps prevent seizures in children whose epilepsy isn't well-controlled with medicine | Not well-studied in adults, can be difficult to maintain long-term |
| Music Therapy | May decrease frequency of seizures in some patients | Inconsistent effects, more research needed |
| Melatonin | May reduce seizure risk in children, but results are conflicting | Lack of conclusive evidence on efficacy |
| Cannabidiol (CBD) | FDA-approved synthetic CBD oil (Epidiolex) for treating rare, severe forms of epilepsy | Only one FDA-approved CBD product, legality and access vary across states |
Mechanisms of Action of Natural Therapies for Epilepsy
It's key to understand how natural therapies work against epilepsy. They target key pathways. These include changing how neurotransmitters and receptors work. They also reduce oxidative stress and neuroinflammation. Plus, they aim to fix mitochondrial dysfunction.
Modulating Neurotransmitters and Receptors
The wrong activity by some brain cells can lead to seizures. This happens when certain brain cells stop working right. They try to fix this by affecting GABA and glutamate, two key neurotransmitters. This helps keep a healthy balance in the brain.
Reducing Oxidative Stress and Neuroinflammation
Epilepsy is linked to oxidative stress and heightened brain inflammation. These can happen due to too many seizures. Natural treatments that fight these conditions might help with epilepsy.
Targeting Mitochondrial Dysfunction
Bad mitochondria might also be part of why someone has epilepsy. Some natural therapies try to fix this by improving how mitochondria work. This could help protect the brain and slow down epilepsy.
Herbal and Natural Remedies for Epilepsy
Many people with epilepsy look for natural remedies. They use them along with or instead of medicine. Herbal and natural remedies for epilepsy are getting more popular, especially where standard medicines are hard to get. Though we still need more proof, some natural things can help with epilepsy.
Flavonoids and Their Antiepileptic Properties
Flavonoids are natural chemicals that come from plants. They are showing promise in managing epilepsy. These chemicals can work against seizures. They help by changing how our brain messengers, and stress and inflammation are involved in epilepsy.
Alkaloids as Potential Anticonvulsants
Then, there are alkaloids. They have been shown to have anticonvulsant effects. Alkaloids are made of nitrogen and found in plants. They can help stop seizures by affecting how our brain’s systems and ion channels work. We are still learning about how effective alkaloid-heavy plant extracts might be.
Other Plant-Based Compounds with Antiepileptic Effects
Besides flavonoids and alkaloids, several other plant-based compounds could be helpful. Terpenoids, coumarins, and glycosides are some examples. These substances have shown antiepileptic effects in studies on animals, offering more natural options that need exploring.
Mind-Body Therapies and Lifestyle Interventions
Complementary and alternative therapies for epilepsy go beyond natural products. They also include mind-body practices. Techniques like meditation and relaxation exercises can help. They've shown good results in managing seizures and boosting well-being for people with epilepsy.
Meditation and Relaxation Techniques
Stress-reduction methods like yoga and meditation can help control seizures. They do this by improving how we handle stress and by helping us relax. In a study, 38% of those using the ketogenic diet saw their seizures drop by over 50% due to meditation and other mind-body therapies.
Dietary Approaches: The Ketogenic Diet
The ketogenic diet is a high-fat, low-carb diet that's being looked at for epilepsy. It has shown to stop seizures completely in about 16% of patients. In 32% of cases, there was a more than 90% reduction in seizures. By the 12-month mark, about 40-50% of those on the diet saw over a 50% reduction in seizures.
A study at Johns Hopkins Hospital saw significant results with the diet. After 3 months, 3% were seizure-free. Over 90% of patients saw a drop of more than 90% in seizures, and 26% had a 50-90% drop. At the 12-month point, 7% were seizure-free, 20% saw over a 90% drop, and 23% had a 50-90% drop in seizures.
In another study, the diet group had a 75% decrease in seizures at the 3-month mark. This was compared to only 6% in the control group. Additionally, 38% in the diet group saw over a 50% reduction in seizures.
Exercise and Physical Activity
Regular exercise is also beneficial for managing epilepsy. Moderate-intensity activities like walking can improve seizure control and life quality. They also help with stress, heart health, and relaxation. Exercise can support the effects of other therapies and lifestyle changes for epilepsy.
Conclusion
The research into how natural compounds help with epilepsy is very promising. Flavonoids, alkaloids, and terpenoids might lead to new epilepsy treatment. These natural elements can change how our brain's chemicals work. They can also lower stress in the brain and fight against swelling. What's more, they fix problems in our cell's powerhouses.
About 25% of children with epilepsy see no improvement with standard drugs. The search for new drugs continues. Natural treatments, like the ones discussed, are becoming more popular. They offer hope for future treatment advances.
The chance to use natural remedies for epilepsy is very exciting. More research could find better ways to help. This could make life better for people with epilepsy.
FAQ
What is epilepsy?
Epilepsy is a widespread and serious brain condition. It affects over 70 million people globally. It can happen to anyone, no matter their age, gender, or where they live.
What are the Epilepsy symptoms ?
The brain's nerve cells sometimes act differently and cause seizures. These seizures can happen because of many reasons. Some include changes in brain cell activity, problems with brain chemicals, and changes in the way brain cells work together.
What causes epilepsy?
Many things can lead to epilepsy. This includes genetic factors, brain structure issues, infections, immune system problems, and other health issues. Sometimes, doctors can't find a specific cause.
What are the treatment options for epilepsy?
For treating epilepsy, some people use natural products or herbs. Others choose mind and body therapies. These can include things like meditation, yoga, or hypnotherapy. They can be used along with regular medical treatments.
What is the difference between complementary and alternative treatments?
Complementary treatments work with regular medicine. They are used together. Alternative treatments are used in place of regular medicine. People may choose one over the other depending on their culture or personal beliefs.
How effective are natural and alternative treatments for epilepsy?
Some natural substances show promise in treating epilepsy. For example, flavonoids, alkaloids, and terpenoids can help change how brain cells communicate. They can also reduce stress and inflammation in the brain. These effects are vital in managing epilepsy.
Source Links
- https://www.epilepsy.com/treatment/alternative-therapies
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8690245/
- https://www.webmd.com/epilepsy/epilepsy-alternative-therapies
- https://epilepsyfoundation.org.au/managing-epilepsy/health-and-wellbeing/complementary-therapies/
- https://cureepilepsy.org/for-patients/understanding/treatments/alternative-therapies-for-epilepsy/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7969896/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8146518/
- https://www.medicalnewstoday.com/articles/317922
- https://www.epilepsy.com/treatment/alternative-therapies/herbal-therapies
- https://www.healthline.com/health/natural-treatments-epilepsy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3200033/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6094950/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2082960/
What is Epilepsy? Understanding This Neurological Disorder
Epilepsy is the fourth most common neurological disorder in the world. It affects around 3 million people in the United States. This brain disorder causes recurring, unprovoked seizures. These are sudden surges of abnormal electrical activity in the brain. They make a person look or act differently.
Having epilepsy can change many parts of your life. It can affect your safety, relationships, work, and even driving. The key is to understand when seizures might happen. Not every seizure is the same. People with epilepsy could have different types of seizure disorder.
In this blog, we will break down what is epilepsy, explore its symptoms, causes, and treatment options, and clear up many of the common myths. We’ll also hear from a doctor who deals with this every day – Dr. Chandril Chugh, a US-trained neurologist.
What is Epilepsy?
Epilepsy is a neurological condition where the brain's activity becomes abnormal. This leads to recurrent seizures. A seizure is like a temporary glitch in your brain's electrical system. But not all seizures look the same. Some people shake violently, while others might just stare blankly for a few seconds.
According to the World Health Organization (WHO), over 50 million people around the globe live with epilepsy.
Around 3 million people in the United States have epilepsy. This makes it the fourth most common neurological disease after migraine, stroke, and Alzheimer's. This shows why knowing the basic facts about epilepsy is crucial.
There are two main types of seizures:
- Generalized seizures: These affect both sides of the brain.
- Focal seizures: These start in just one part of the brain.
Many people think epilepsy always means falling and shaking. That’s a myth. Some seizures involve just strange feelings or smells. Others are just a few seconds of confusion.
The reasons behind what is epilepsy vary. It can happen due to:
- Genetic factors (runs in families)
- Brain injury from trauma or surgery
- Infections like meningitis or encephalitis
- Strokes or tumors
But here’s a surprising fact:
“In up to 70% of cases, no clear cause is found.” – Epilepsy Foundation
So even with all our medical tools, sometimes the exact cause remains unknown.
Causes of Epilepsy
Now that we understand what is epilepsy, let’s dive into the reasons why it happens. Doctors usually split causes into two groups:
- Idiopathic epilepsy: No clear cause. It might be genetic.
- Symptomatic epilepsy: A known reason like trauma or a brain disease.
Common causes include:
- Genetics: Some people inherit a tendency for seizures.
- Stroke: In older adults, strokes cause about 10–20% of new epilepsy cases.
- Brain tumors or injuries: Any damage to the brain can trigger seizures.
- Infections: Like meningitis or brain inflammation.
- Developmental disorders: Conditions like autism can also be linked to epilepsy.
Idiopathic epilepsy: In many cases, doctors can't find a clear reason.
Sometimes even things like lack of oxygen during birth or severe head injuries from accidents can trigger epilepsy years later.
Symptoms and Signs of Epilepsy
It's key to know the Epilepsy symptoms .
Seizures look different in different people. You may not even realize someone is having one. That’s why it's important to know the warning signs.
Some common symptoms include:
- Blank staring
- Sudden jerking of arms or legs
- Loss of consciousness
- Confusion or foggy memory
- Unusual smells or tastes (called auras)
Aura is like a warning sign. Some people feel strange right before a seizure. It could be a funny taste, dizziness, or even fear.
There are different types of seizures, which are described below:
| Type of Seizure | Description | Duration | Risk Level |
|---|---|---|---|
| Absence | Brief staring spells | 10-20 seconds | Low |
| Tonic-Clonic | Stiffening + shaking | 1-3 minutes | Moderate to High |
| Myoclonic | Sudden jerks | A few seconds | Low |
| Atonic | Sudden limp collapse | A few seconds | Moderate |
| Simple Focal | Aware during seizure | Under 1 minute | Low |
| Complex Focal | Confused, unaware | 1-2 minutes | Moderate |
Understanding these seizure types is key in knowing what is epilepsy and how to respond properly.

What is Epilepsy? Understanding the Condition
Epilepsy is a complex condition affecting the brain. It can be hard to spot because its symptoms are like other health issues. These include heart problems and mental health disorders.
Diagnosis is the first big step to proper epilepsy treatment. Doctors use a mix of tests and tools to find out what’s going on.
- Neurological Exam: Tests your reflexes, balance, and memory.
- Patient History: What happened before, during, and after your seizures?
- EEG (Electroencephalogram): This test shows brain waves. It helps spot abnormal patterns.
"EEG identifies abnormalities in up to 50% of epilepsy patients"
- MRI or CT Scans: These show the structure of the brain. They help find tumors, injuries, or scars.
- Seizure Diary: Keeping a record of when seizures happen, what triggers them, and how long they last.
- Witness Accounts: What other people saw can help your doctor understand the type of seizure.
Diagnosis isn’t always easy, but it’s essential. It tells us what type of epilepsy you have and how best to treat it.
Treatment Options for Epilepsy
Once diagnosed, there are several epilepsy treatment options. The right choice depends on the person.
- Anti-Epileptic Drugs (AEDs): These help control seizures. There are many types. Your doctor may try a few before finding the one that works.
"Two-thirds of people with epilepsy become seizure-free with medication"
- Surgery: If medications don’t work, brain surgery might be considered.
- Vagus Nerve Stimulation (VNS): A device is implanted to help control seizures.
- Ketogenic Diet: High-fat, low-carb diet helps some people, especially kids.
- Lifestyle Changes: Good sleep, stress control, no alcohol. These can lower seizure chances.
Some treatments need time. Your neurologist will guide you every step of the way.
Living with Epilepsy
Living with epilepsy can bring tough times. But, with the right support and changes in life, people can handle it well. It's important to know what triggers seizures, like missing medicine, not enough sleep, stress, and body changes. Avoiding these things can make seizures happen less often.
Here are some safety and emotional health tips:
- Avoid swimming alone
- Check your country/state driving laws
- Use helmets if you bike or hike
- Get enough sleep every night
- Avoid flashing lights if they trigger you
Emotionally, people with epilepsy may face anxiety or depression. Talking to a counselor helps.
Being open about epilepsy can fight stigma. Support groups are also a great place to share stories.
Life with epilepsy isn’t about fear. It’s about being informed and supported.
Epilepsy in Children vs. Adults
What is epilepsy can look very different in kids and adults.
- In children, epilepsy might be due to birth issues or genetic causes.
- In older adults, it's often due to strokes or Alzheimer’s.
Some childhood epilepsy syndromes include:
- Lennox-Gastaut Syndrome
- Dravet Syndrome
- Benign Rolandic Epilepsy
In seniors, medications and diagnosis can be tricky. They may already be on several drugs. That’s why close medical care matters.
Can Epilepsy Be Prevented?
In some cases, yes. You can lower the chances of developing epilepsy with basic health steps.
- Prevent Head Injuries: Always wear seatbelts and helmets.
- Treat Brain Infections Early: Don’t delay treatment for meningitis.
- Control High Blood Pressure: Reduces stroke risk.
- Prenatal Care: Helps prevent brain injury in babies.
- Genetic Counseling: For families with a history of seizures.
"25% of epilepsy cases are preventable" – World Health Organization
Epilepsy prevention is not always possible, but it’s definitely worth the effort.
When to See a Doctor?
Not every seizure means epilepsy. But certain signs mean it’s time to get checked.
- First-time seizure
- Seizure lasting over 5 minutes
- Injury during a seizure
- More than one seizure in a short time
When you visit your neurologist:
- Share video of the seizure if you have one
- Bring a seizure diary
- Ask about side effects of medications
Always go for a second opinion if you’re unsure. Your brain health matters.
Common Myths about Epilepsy
Many false beliefs surround epilepsy. Let’s clear them up with some truth.
| Myth | Fact |
|---|---|
| Epilepsy is contagious | It is not. You can’t catch it from someone. |
| Only children get epilepsy | It can happen at any age. |
| Everyone with epilepsy loses consciousness | Some seizures only cause brief changes in awareness. |
| Put something in a person’s mouth during a seizure | Never do this. You can harm them. Instead, turn them on their side and keep them safe. |
| People with epilepsy can’t live a normal life | With treatment and support, most live full, active lives. |
| Seizures are always dramatic | Some are subtle, like brief staring spells or confusion. |
| Epilepsy is a mental illness | It’s a neurological disorder, not a psychiatric condition. |
| People with epilepsy can’t work or go to school | Many hold jobs, study, and contribute just like anyone else. |
| Epilepsy always runs in families | While some types are genetic, many cases are not. |
| Flashing lights trigger all seizures | Only a small percentage of people have photosensitive epilepsy. |
| You must restrain someone during a seizure | This is dangerous. Keep the person safe but never hold them down. |
| You always need to call an ambulance | Not always. Call if the seizure lasts more than 5 minutes or if it's the person's first seizure. |
Breaking these myths helps us support those with epilepsy better and removes stigma from the conversation.
Dr. Chugh’s Advice on Epilepsy
If you or someone close has epilepsy, don’t wait. Early diagnosis and proper treatment can make a big difference. Schedule a consultation with Dr. Chandril Chugh – a US-trained, board-certified neurologist who treats epilepsy with the latest tools and years of expert knowledge.
Dr. Chandril Chugh specializes in treating complex neurological disorders, including epilepsy, migraines, stroke recovery, memory loss, sleep issues, and ADHD in children. You can trust his advice. You can trust his care.
FAQ
What is epilepsy?
Epilepsy is a brain disorder causing sudden, unprovoked seizures. These are bursts of abnormal brain activity.
What are the different types of seizures?
Two main types exist: focal and generalized seizures. They both show different symptoms but involve uncontrolled brain activity. Symptoms may include altered emotions, blank stares, or shaking.
How common is epilepsy?
Around 3 million Americans have epilepsy. It is the fourth most common neurological disease in the U.S., after migraine, stroke, and Alzheimer's.
What causes epilepsy?
The causes of epilepsy vary. They can relate to genes, brain injuries, infections, or be unknown. When the cause is unknown, it's called idiopathic epilepsy.
How is epilepsy diagnosed?
Doctors diagnose epilepsy through blood, brain scans, and EEG tests. These tools find the seizure type and possible causes. They guide treatment.
What are the treatment options for epilepsy?
Treating epilepsy often starts with medicine. Over half of cases can be controlled this way. If pills don’t work, there are other options like diet changes, surgery, or nerve stimulation.
How can I manage epilepsy in my daily life?
Managing epilepsy involves watching for triggers, getting enough sleep, and staying away from things like alcohol. This can lower how often seizures happen. Joining support groups and educating others is also important.
Source Links
- https://www.mayoclinic.org/diseases-conditions/epilepsy/symptoms-causes/syc-20350093
- https://www.nationwidechildrens.org/conditions/epilepsy
- https://www.ninds.nih.gov/health-information/disorders/epilepsy-and-seizures
- https://www.epilepsy.com/what-is-epilepsy/understanding-seizures
- https://www.webmd.com/epilepsy/understanding-epilepsy-basics
- https://www.nhs.uk/conditions/epilepsy/symptoms/
- https://www.epilepsy.com/causes
- https://www.mayoclinic.org/diseases-conditions/epilepsy/diagnosis-treatment/drc-20350098
- https://www.nhs.uk/conditions/epilepsy/treatment/
- https://my.clevelandclinic.org/health/diseases/17636-epilepsy
- https://www.verywellhealth.com/coping-with-epilepsy-1204447
- https://www.epilepsy.com/stories/tips-tricks-people-living-epilepsy
- https://www.epilepsy.com/lifestyle
- https://www.uspharmacist.com/article/an-overview-of-epilepsy
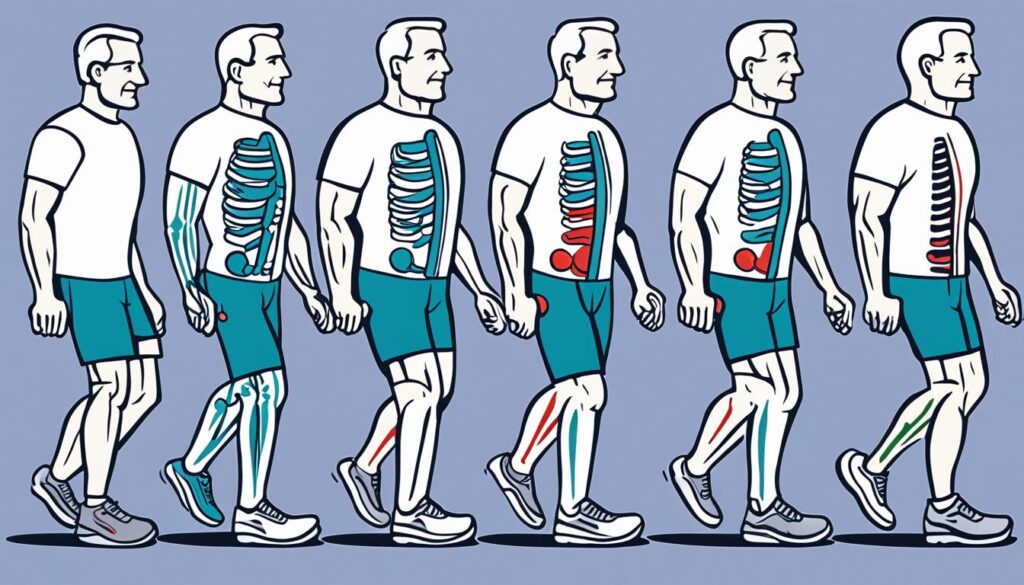
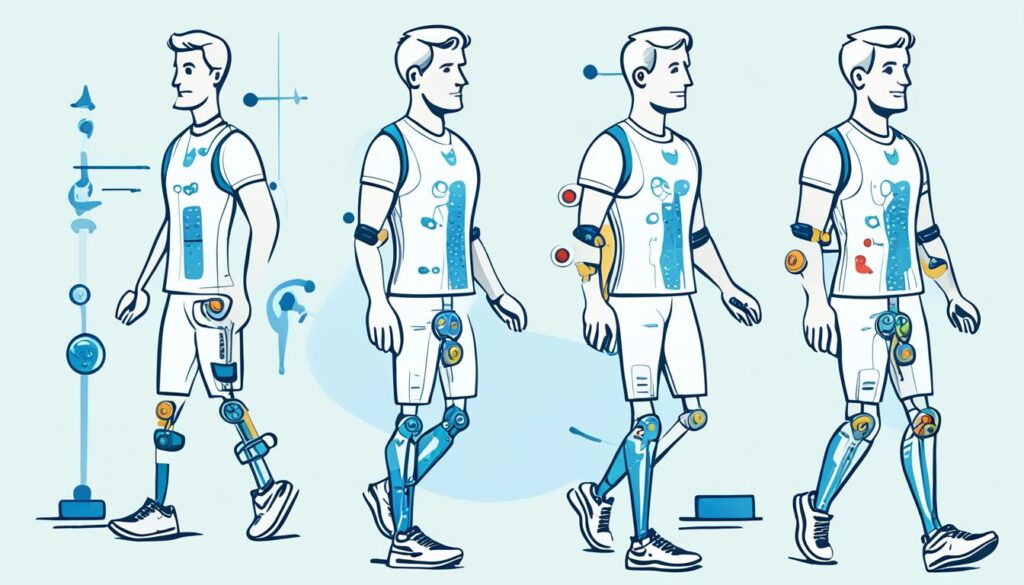
Effective Treatments for Gait Disorders: Approaches and Therapies
Gait disorders are about how people walk in strange ways. They can be caused by different things. Some reasons include problems with bones or joints, or diseases that affect the brain. As we get older, they become more common. They can make walking very hard, affecting daily life.
Physical therapy is key in treating gait disorders. It works on strengthening the body, making it more flexible, improving balance, and helping with coordination. By doing this, people can often walk more normally again. Therapy plans are made to fit each person's needs.
Understanding Gait Disorders
Gait disorders may come from many gait disorder causes. These include health issues like Parkinson's, stroke, and multiple sclerosis. These conditions affect how the nervous system manages muscle movement. They can also come from problems in the bones or muscles such as arthritis or fractures. In older people, decline in strength, balance, and senses can often lead to gait issues.
Causes and Prevalence
Older adults are more likely to have gait disorders. For example, while 85% of 60-year-olds walk normally, only 20% of 85-year-olds do. It's interesting to note that men usually face more nerve-related gait problems. On the other hand, women often deal with gait issues caused by other health conditions.
Impact on Daily Life
Gait disorders greatly affect daily life. They can reduce how much a person can move around and their independence. They also lower life quality. Having a gait disorder means a higher risk of falling and getting hurt. This makes things even more difficult for those with these disorders.
The Role of Physical Therapy
Physical therapy is very important in helping people with [gait disorder treatment]. First, a full checkup is done. This includes looking at how the person walks and their health history. The therapist then makes a plan just for that person's needs.
Comprehensive Evaluation
At the start, the therapist checks many things to understand the [gait disorder treatment] better. They watch how the person walks, how fast they go, and if they can balance well. They also check the person's muscle strength. Plus, they may test reflexes, feeling, and watch their heart and blood pressure. All this checking helps build a plan that will work well.
Customized Treatment Plans
After looking at the test results, the therapist makes a plan just for the patient. This plan might have exercises to get stronger and more balanced. It could also include learning how to walk better. If needed, they might use hands-on therapy to help move easier. In some cases, the patient might need to use special tools, like canes or braces. This custom plan addresses the main problem and helps the patient walk better. It also boosts their daily life and how well they function.

Therapeutic Interventions
Physical therapy helps fix reasons behind walking problems. It aims to get people back to walking normally. This makes life easier for those dealing with walking issues.
Strength and Balance Training
Strength and balance exercises are key in therapy. They work on weak muscles and balance. This lowers fall risks and helps people move confidently.
Mobility and Gait Retraining
Learning movement patterns and using big movements help. They get the brain and body in sync again. This makes walking easier and smoother.
Assistive Device Usage
Some people may need tools like walkers for safety. Physical therapists recommend and show how to use these devices. This helps make daily activities safer and easier.
Therapists know which tools and exercises fit each person best. They create a plan to meet each individual's needs. This approach helps people walk better, be more independent, and enjoy life.
Gait Disorder Treatment
Treating gait disorders needs a careful plan, often led by physical therapy. Physical therapists do a full check-up to make a special plan. This plan targets the causes of a person's gait problem. It could involve training to get stronger and more balanced, learning how to walk better, and using aids to move easier. All this helps the patient walk better and have a better life. Working with the patient, physical therapists use the best methods to help them walk normally again.
To start treating a gait disorder, the therapist looks at the patient's health and how they walk. Then, they make a plan that fits the patient's needs. This plan might have exercises to build strength and balance, ways to walk better, and tools like canes or braces for support. The goal is to fix the reasons for the gait issue.
Building strength and balance is key in gait disorder treatment. These exercises get to the root of muscle problems, making the body work better. When therapists add tough exercises that test stability, they're setting up for natural and easy walking. Also, learning certain walking ways helps the brain learn to walk right again.
For some, walking safely means using help like canes or walkers. Therapists pick the right tools and teach their patients how to use them. This and other treatments mean patients can move better, getting back their freedom and a better life.

Successful gait disorder care comes from a team effort between the therapist and the patient. They together work on the real causes and use proven methods. This teamwork helps people with gait issues lead active, free lives again.
Neurological Gait Disorders
Conditions like Parkinson's disease, stroke, and multiple sclerosis often cause gait problems. These issues can make it hard for the brain to control how muscles move. As a result, people experience different walking problems.
Parkinson's Disease
Parkinson's disease leads to issues like slow walking and trouble staying balanced. The brain changes with this disease can slow down or stop smooth walking. This can lead to a walk that looks shuffle or unsure.
Stroke and Multiple Sclerosis
Stroke and multiple sclerosis can also cause problems with walking. People may have shorter steps, feel unsteady, or walk in a shuffle. These issues come from the brain not being able to control movements well enough for walking.
Dealing with these walking problems means finding a plan that fits each person. Physical therapy is a great help. It includes exercises, learning better ways to move, and using tools to support walking. This approach can really improve walking and give people more freedom.
Musculoskeletal Gait Disorders
Neurological conditions change the way we walk. But, issues with our muscles and bones can also affect our gait. Arthritis is a big reason for gait troubles. Affecting our joints, it can cause pain and make moving hard. This makes walking smoothly very tough.
Arthritis and Joint Issues
Osteoarthritis is the top arthritis type. It affects joints we need for walking like our hips, knees, and ankles. When the cartilage in these joints wears down, it causes pain and stiffness. This often messes up how we walk, making it shaky or tough. Solving arthritis gait problems helps people move more normally again.
Fractures and Injuries
Broken bones or injuries in our legs, ankles, or feet make it hard to walk right. This messes up our body's walk-supporting systems. In these cases, physical therapy is key. It aims to strengthen and make the body more flexible. This, alongside other treatments, helps people walk like they did before the injury.
For issues linked to our muscles and bones, physical therapists can create special plans. These help people with gait problems walk better and with confidence. With the right care, they can often get back their walking skills.
Age-Related Gait Disorders
As we get older, walking can become harder. This is often due to our strength, balance, and how well we feel things changing. When our muscles are weak and our joints stiff, moving can be tough. This leads to unsteady or slow movements. Such changes can make us more likely to fall. They also affect how we live every day and the joy we find in life.
Gait problems are seen more as we age. For example, some 60 to 69-year-olds might have trouble walking, but this jumps to more than half of those over 80. A study also found that 35% of people over 70 experienced walking difficulties. So, you can see that these issues greatly impact our oldest citizens.
Thankfully, there is help. Physical therapy can do a lot to improve our walking. Therapists use exercises and training to boost our balance and mobility. This not only helps us stay on our feet but also boosts our well-being. For the elderly, how fast they walk might show how long they will live. Steps that make us move better could even prevent some cases of dementia in the future.
| Age Group | Percentage of Individuals Walking Normally |
|---|---|
| 60-year-olds | 85% |
| 85-year-olds | 20% |
The table shows that walking well decreases as we get older. Therefore, it's vital to take steps to keep walking and moving. By teaming up with physical therapists, older people can tackle walking troubles. This can bring back their joy, freedom, and life quality.
Conclusion
Gait disorders can affect your ability to move independently. They come from many different causes and can vary in how severe they are. However, physical therapy offers helpful treatment for these issues.
This kind of treatment focuses on the exact cause of the problem. It might be from your nerves, muscles, or getting older. Physical therapists make plans just for you. These plans include exercising, learning how to move better, and using equipment that helps.
With this help, people can learn to walk better again. This brings back their confidence and makes their life better overall. Physical therapy is always getting better, which means more hope for people with gait disorders.
By working closely with physical therapists, you can beat gait disorders. This opens the door to a life with more freedom and independence. The journey to improved gait disorder treatment starts with you, and it can make a big change in how you live your life.
FAQ
What are gait disorders?
A gait disorder is a condition that changes how people walk. It can happen due to many reasons. For example, it could be because of a bone or joint problem like arthritis. Or, it could relate to issues in the brain or nerves, such as with Parkinson's Disease.
Multiple diseases can affect how someone walks, such as Multiple Sclerosis. They can make people walk differently or find it hard to walk at all.
How prevalent are gait disorders?
They become more common as people grow older. They might affect around 20% of those over 60 years old.
How do gait disorders impact daily life?
Gait disorders change how people can move and get around. They can make someone less independent. They also lower the quality of life for those with the disorder.
What is the role of physical therapy in treating gait disorders?
Physical therapy is crucial for treating gait disorders. It all starts with a thorough check of how a person walks and their health history.
After this, a personalized plan is made. This plan may include special exercises to get stronger, improve balance, and learn to walk better. Hands-on treatments can also help make muscles and joints more flexible.
What types of therapeutic interventions are used for gait disorders?
There are several ways to help with gait disorders. Physical therapy uses methods like getting stronger and better at balancing.
People might also need to learn how to walk in a different way. Plus, sometimes tools like canes or walkers can be useful.
How do neurological conditions contribute to gait disorders?
Brain and nerve issues can really change the way someone walks. Conditions like Parkinson's Disease and stroke mess up how the nervous system controls the muscles.
This can make walking hard and affect balance, causing a gait disorder.
How do musculoskeletal disorders affect gait?
Bone and joint problems can also disrupt our walk. Injuries or diseases in the legs can impact how we move, causing gait issues.
What role does aging play in the development of gait disorders?
As we get older, gait disorders can become more common. It is often because our bodies naturally weaken with age. This includes our strength, balance, and how we feel with our senses.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2816030/
- https://www.aafp.org/pubs/afp/issues/2010/0701/p61.html
- https://www.hindawi.com/journals/aneu/2014/573862/
- https://www.webmd.com/brain/types-gait-disorders
- https://www.ncbi.nlm.nih.gov/books/NBK560610/
- https://ptunlimitedinc.com/physical-therapy-services/gait-disorders/
- https://www.choosept.com/guide/physical-therapy-guide-gait-dysfunctions
- https://www.myactionpt.com/physical-therapist-s-guide-to-gait-dysfunctions
- https://pubmed.ncbi.nlm.nih.gov/35787837/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2872829/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6850501/
Gait Disorder Causes: An Informative Guide
Gait is how you walk, and it's key to moving smoothly and staying balanced. But some injuries or health issues can mess with your gait. This can lead to problems like dragging your toes or feeling unsteady. Some of these problems are just for a short time, but others might need long-term care. Knowing why gait issues happen is a big first step in handling them well.
Many things can cause gait troubles, from conditions like Parkinson's to problems with your bones and joints. In this guide, we will look at what makes gait problems happen. You'll learn more about why this part of your health is so important.
Introduction to Gait Disorders
Gait is how we walk, and it's very important for moving around. Different things can change how we walk, like injuries and getting older. These changes can cause gait disorders. It's key to know about gait and these issues to manage them well.
Understanding Gait and Its Significance
Gait shows how well our muscles, brain, and thinking work together when we walk. A healthy gait is smooth and lets us move well. But, if something is wrong, we might walk strangely. For example, we could drag our toes or feel wobbly.
Prevalence and Impact of Gait Disorders
Issues with walking are quite common, especially as people get older. At 60, most people walk normally. Yet, by 85, only a few still do. Men and women seem to face different walking problems as they age.
Gait problems can really lower life quality and freedom, especially for older people. They make falling more likely, which is a major risk for severe injuries. Surprisingly, a slow walk in older folks without dementia could predict getting dementia later.
Neurological Gait Disorder Causes
Neurological conditions often cause gait disorders. They have a big impact on life quality, and can even be deadly. The NCBI Bookshelf says they're more common than other causes.
Parkinson's Disease and Parkinsonism
Parkinson's disease can show up with small changes in how someone walks. A key sign is a slow to start balancing reaction, leading to falls. A shuffling walk, less arm movement, and problems starting or turning are typical.
Stroke and Cerebrovascular Diseases
Vascular diseases, like stroke, can affect your walk. These issues can often be found with an MRI. Smoking, high blood pressure, high cholesterol, and diabetes raise your odds of these gait problems.
Dementia and Cognitive Impairments
Dementia and Alzheimer's can make walking hard and risky. These patients may walk slower, but somehow end up walking too fast and falling. Boosting their thinking ability is very important for their gait rehab.
Peripheral Neuropathies
Peripheral nerve issues can make it hard to walk. This can cause balance problems, coordination trouble, and a funny way of picking up your feet. It's all because the lower body's sense isn't working right.
Musculoskeletal Gait Disorder Causes
Neurological conditions often Gait Disorder Causes Problem. Yet, musculoskeletal issues are also key. The NCBI Bookshelf shows that osteoarthritis in the hips and knees, and foot and ankle problems, matter a lot.
Osteoarthritis of the Hips and Knees
Osteoarthritis is a joint disease that changes how you walk. It brings pain and less movement in your hips and knees. This makes walking difficult. So, people may walk with a limp or favor one leg to reduce pain.
Foot and Ankle Deformities
Problems like bunions, hammertoes, or weak ankles can also affect how you walk. These issues change how weight is placed on your feet. This can make your walk uneven or unsteady. It is important to check and treat these foot and ankle problems for a better gait.
Systemic and Metabolic Gait Disorder Causes
Gait disorders can come from problems that affect the whole body. Such issues include systemic and metabolic conditions. It's important to look into these areas to help with gait problems.
Electrolyte Imbalances
Things like low sodium, potassium, and magnesium levels can make it hard to walk well. Having the right balance of these electrolytes is key for your muscles and bones to work right. This directly impacts how well you can walk.
Vitamin Deficiencies
Running low on vitamins like B12, E, and copper can mess with your ability to walk. Making sure you eat foods rich in these nutrients can better your walking and body movement.
| Electrolyte Imbalance | Impact on Gait |
|---|---|
| Hyponatremia (low sodium) | Affects proper musculoskeletal function, leading to gait disorders |
| Hypokalemia (low potassium) | Disrupts muscle contraction, contributing to gait disturbances |
| Hypomagnesemia (low magnesium) | Impairs neuromuscular coordination, resulting in gait imbalances |
Improving your gait starts by looking at these broader health and body issues. It's about making sure your body is healthy for applying a balanced walking steps.
Gait Disorder Causes
Aging and Gait Changes
As you age, the chance of having a gait disorder goes up. By the time people reach over 80, more than half may have this issue. It shows how much age affects the way you walk.
Getting older means walking slower and taking shorter steps. Yet, the amount of steps you take each minute stays similar. Older adults also walk with steps that are about 40% wider than young adults. These changes may lead to falling more often, which can limit your freedom.
Acute Illnesses and Medication Side Effects
Short-term sicknesses and some drugs' side effects can cause gait issues too. Things like infections, fever, or not having enough water can mess up how you walk for a bit. Medications for brain or mood problems might also make walking harder.
When you get sick or your meds change, your ability to walk might get worse. But fixing the main problem and making any needed drug changes can return your walking to normal. This could help you avoid falling and other problems.
Diagnosis and Assessment of Gait Disorders
Figuring out why someone has a gait disorder is really important. It helps doctors treat and manage it well. Doctors start by carefully looking at a person's walk and asking about their health. Then, they do exams to find out more. They use these steps to pick the best tests to do.
Clinical Evaluation and Observation
The first step in checking a gait problem is a full evaluation. Doctors and experts watch how you walk. They ask about your health history and check your body. This helps them figure out what's causing the walking issues. From there, they know what tests to do and how to help.
Diagnostic Tests and Imaging
For diagnosis, doctors might call for some tests and scans. These can include:
| Diagnostic Test | Purpose |
|---|---|
| Electrodiagnostic studies (EMG, nerve conduction tests) | Finding out if there are nerve or muscle problems that might be causes |
| Magnetic resonance imaging (MRI) | Show if the brain, spine, or bones have issues affecting how you walk |
| Computerized tomography (CT) scan | Looking closer at bones and other structures to see if they're causing problems |
| Blood tests | Checking for things like not enough vitamins or minerals in your body |
These tests, along with what doctors see, pinpoint the real cause. They guide the treatment. The goal is to make you move better and feel well.
Management and Treatment Strategies
Gait disorder treatment requires a multi-step plan. It uses different methods to help people get around better. This can involve taking certain medicines, using special exercises, and getting help from tools and devices.
Pharmacological Interventions
If a specific health issue Gait Disorder Causes problem, doctors might give medicine to help. People with Parkinson's disease might take drugs like levodopa or dopamine agonists to reduce their symptoms. Medicines for fixing low vitamin levels or imbalanced electrolytes can also help improve someone's gait.
Physical and Occupational Therapy
Therapy that focuses on movement is key in managing gait issues. Therapists work with patients on exercises to make their muscles stronger, improve flexibility, and better their balance. They also teach how to deal with limits in movement and ways to move better.
Assistive Devices and Mobility Aids
Support from devices like walkers, canes, or orthotics is very helpful for those with gait issues. Sometimes, wheelchairs or scooters are needed for more freedom. These items can make a big difference in how well someone can move.
Conclusion
Gait disorders can come from many causes, like problems with your nerves, bones, or whole body. It is key to know what causes the issue to find the best way to treat it. Doctors look closely at your walking and check your body to pick the right tests and treatment.
Helping with gait disorders needs a team from different fields working together. With the right care, people can walk better, lower the chance of falling, and stay active. Finding and treating gait issues early, with a plan just for you, is the best way to help you walk better.
Want to learn more about gait disorders? You can get great tips from top doctors and researchers in this area.
FAQ
What is gait and how can it become abnormal?
Gait is how you walk. It can change because of an injury or health problem. This may lead to dragging toes, walking with high steps, or feeling off balance. Some changes in gait can be fixed, but others need lifelong care.
What are the most common neurological causes of gait disorders?
Neurological issues often cause gait disorders. These include problems like sensory ataxia from polyneuropathy, Parkinson's, vascular encephalopathy, and dementia. They can affect how someone walks or moves.
What are the common non-neurological causes of gait disorders?
Gait problems not related to the brain often stem from muscle and joint issues. Things like hip and knee arthritis can lead to pain and trouble moving. This affects how a person walks.
How can electrolyte imbalances affect gait?
Imbalances in electrolytes like sodium, potassium, and magnesium can change gait. Proper balance of these substances is key for healthy muscles and bones. This in turn affects how someone walks.
How does age impact gait disorders?
Gait problems become more common as people get older. They might start after 60 and increase after 80. With age, walking might get slower and steps might get shorter. However, some aspects like cadence may not change as much.
How is the diagnosis of gait disorders approached?
Doctors first watch how a person walks and listen to their health story. Then they do tests to check the body, brain, and joints. These steps help find out the cause of gait issues. They also guide further tests and treatments.
What are the treatment options for gait disorders?
Treating gait problems can involve using medicines, doing therapy, or using special tools to help move. It's about finding the best way to improve walking based on what's causing the problem.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/
- https://www.ncbi.nlm.nih.gov/books/NBK560610/
- https://www.pacificneuroscienceinstitute.org/movement-disorders/conditions/gait-disorders/
- https://www.webmd.com/brain/types-gait-disorders
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2922365/
What is a Gait Disorder? A Comprehensive Overview
Have you seen someone walk oddly, like dragging their toes or taking big steps? This shows they might have a gait disorder. A gait disorder means walking differently than usual. It could happen after an injury or because of a health problem. It really changes how someone lives.
Walking seems easy, but it's super complex. It involves your nervous system, muscles, and heart and lungs all working together. If something goes wrong with any of these, a gait disorder might show up. These problems could be short-term or last a lifetime, needing regular care.
We're going to talk about gait disorders, how common they are, and how they affect life. We'll cover what causes them, the different types, and how doctors diagnose and treat them. You'll finish knowing more about gait disorders and how to deal with them well.
Understanding Gait Disorders
Definition and Prevalence
Gait disorders happen when someone walks differently than usual. They're caused by problems with the body’s nervous, muscle, and breathing systems. These issues are often seen in older people.
Impact on Quality of Life
Gait disorders can really change someone’s life. They can lead to less freedom, falls, and getting hurt. Problems with balance and how we walk can make people more likely to fall. This is a big reason why the elderly can get hurt so badly. Sadly, these issues are not often found or treated early enough.
Causes of Gait Disorders
Gait disorders have many gait disorder causes, from issues in the brain to bone and muscle problems. Knowing these causes helps doctors diagnose and treat you better.
Neurological Conditions
Problems in the brain or nervous system can mess up your walking. For example, issues with feeling or moving can make you walk funny. Conditions like parkinsonism or balance difficulties can cause these problems.
Musculoskeletal Issues
Conditions that affect your bones and muscles can also be to blame. Things like arthritis or being born with the wrong body shape might change how a person walks. Seniors often have several reasons for their gait issues, such as bad balance, not seeing well, or problems in the brain that affect movement.
Medical Conditions
Many health problems can make your gait weird, too. Heart or lung issues and not enough blood getting to your legs can be culprits. Sometimes sudden problems walking can show there’s something bad happening in your brain or spine, a reaction to medicine, or a mental health condition.

Types of Gait Disorders
Healthcare pros often face different types of gait disorders. These include sensory ataxia, parkinsonism, and frontal gait disorder. Each has unique traits and causes.
Sensory Ataxia
Sensory ataxia comes from a problem in the proprioceptive system. This system tells us where our limbs are and how they move. People with this disorder may have trouble walking steadily. They often find it hard to keep balanced. This is because they can't coordinate their body movements well. A few things can cause this, like damage to the nerves (peripheral neuropathy) or injuries to the spinal cord.
Parkinsonism
Parkinsonism makes a person walk in a specific way. They shuffle, stand bent over, and find it tough to start moving. This type of walking is common in Parkinson's disease and other similar disorders. These illnesses hurt the brain, making it hard for the person to walk smoothly.
Frontal Gait Disorder
Frontal gait disorder is often linked to brain disorders like Alzheimer's. People with this problem walk slowly, taking very small steps. They also find it hard to turn while walking. Their feet might feel like they're stuck to the ground. This makes walking smoothly very hard for them.
Knowing these gait disorders helps doctors aim treatment better. They can help people with walking issues do better. This improves how they move, stay safe, and their life quality.
Gait disorder
A gait disorder affects the way someone walks. It can be due to many health issues. These problems change how we walk because of issues with our muscles, nerves, and hearts.
It's important to know what causes different gait disorders. This helps doctors give the right treatment. Gait issues can make life hard, increasing the chance of falling. But with the right care, we can help people feel better and walk safer.

Diagnosing Gait Disorders
To start, doctors watch how a patient walks and ask about their health history. They look at how the patient stands and takes their first steps. They check step length, speed, how the arms move, and if the patient can do special walking tests. These steps are key to finding out more about gait disorders.
Clinical Observation
Healthcare professionals pay close attention to how a patient walks. They notice any unusual walk signs. This detailed look helps them understand if there are problems with the brain, body, or health causing the unusual walk.
Neurological and Orthopedic Examination
A detailed check of the nervous system and bones is also done. By learning about the patient's history, they can plan these checks well. This step is important for deciding which gait disorders tests, like images or lab work, are needed.
Ancillary Diagnostic Tests
Based on what could be causing the problem, more tests might be needed. These could include brain images, nerve function tests, and lab checks. These tests give more details about the patient's condition. They help the healthcare team make the best treatment plan.
Gait Disorder Treatment
The Gait disorder treatment works to fix the root problem. This could be from nerve, muscle, or other health issues. Patients might need drugs, therapy, or sometimes surgery to help.
Addressing Underlying Causes
If a gait disorder comes from a brain issue like Parkinson's, medicines might help. Or, if it's because of bad joints or a crooked spine, then physical or occupational therapy could be needed. For some, surgery might be the best option.
Physical and Occupational Therapy
Therapies are key in helping with gait disorders. They focus on making the body stronger, more balanced, and coordinated. They also teach how to use devices that make moving easier.
This helps people be more self-sufficient and enjoy life more.
Assistive Devices
Canes, walkers, or scooters all help by making moving safer and easier. The right one is chosen to match the person's needs. This considers their balance, strength, and how bad their gait disorder is.

The Role of Cognition in Gait
Your cognition and gait work closely together. Executive function, visuospatial perception, and attention are vital for walking safely. When these cognitive skills are impaired, you might have issues walking. This can lead to more falls and other dangers.
Executive Function and Attention
Executive function and attention are crucial for a strong gait. Older adults with mild cognitive issues face a higher fall risk. This shows how important these skills are for safe walking. People with mild cognitive issues also often have trouble walking. It shows the tight link between cognition and gait.
Multitasking and Dual-Task Paradigms
Multitasking and dual-task paradigms help us understand this link better. People are asked to do mental tasks while walking. It's interesting that older adults may fall more if they stop to talk. This shows how critical thinking is for walking safely. The ability to multitask keeps you balanced and mobile.
Conclusion
Gait disorders are complex and can really impact how you live. It's key for healthcare folks to know about the different causes. They must also understand how thinking affects walking. This helps them treat and care for you better, improving your life.
Healthcare providers, by knowing the many causes of gait issues, can make care more personalized. They can combine ways to help, like focusing on how you think and move. The goal is to find the best ways to help you move better and do more on your own.
Managing gait disorders needs teamwork between you, your doctors, and using the best tools. Everyone working together can help you beat gait problems. This way, you can feel more sure moving around every day.
FAQ
What is a gait disorder?
Gait is how someone walks. An injury or a medical problem may change the way a person walks. This can include dragging toes, taking big steps, or feeling unsteady.
What causes gait disorders?
Gait disorders have many reasons. These include problems with the brain or nerves, issues with muscles and bones, and certain health problems. Things like not feeling where your body is (proprioception) or heart failure can change how someone walks.
What are the common types of gait disorders?
Popular gait issues are sensory ataxia, parkinsonism, and frontal gait disorder. Sensory ataxia comes from issues in feeling where your body is. Parkinsonism leads to a walk where you take small steps and lean forward. Frontal gait disorder is mostly seen in older people and those with certain brain diseases.
How are gait disorders diagnosed?
To find the cause of a gait disorder, doctors first watch how a person walks. They also ask about the person's medical history and do certain tests. These can include watching the patient try different tasks. Sometimes, they also need to do more tests like brain scans.
How are gait disorders treated?
The focus of treating gait issues is to fix the main problem that's causing the walk to change. This can involve taking medicines, doing physical or occupational therapy, or even having surgery. Therapies and devices like canes can make walking safer and easier.
How does cognition impact gait?
The mind's job directly affects how we walk. Things like being able to plan, see space, and focus help us walk around safely. If these skills are not as good, a person might have trouble walking smoothly, even when just thinking while walking.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/
- https://www.movementdisorders.org/MDS/About/Movement-Disorder-Overviews/Gait-Disorders.htm
- https://www.sciencedirect.com/topics/neuroscience/gait-disorder
- https://www.webmd.com/brain/types-gait-disorders
- https://www.aafp.org/pubs/afp/issues/2010/0701/p61.html
- https://www.pacificneuroscienceinstitute.org/movement-disorders/conditions/gait-disorders/
- https://www.healthline.com/health/gait-and-balance-problems
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3498517/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2922365/
- https://www.sciencedirect.com/science/article/abs/pii/S0002934317312950
Recognizing Encephalopathy Symptoms: Early Signs and Indicators
Encephalopathy is a change in how the brain works. It can cause various mental and physical problems. Symptoms like confusion, restlessness, or changes in awareness are common.
It's caused by several conditions like liver problems or infections. Early signs need quick attention. This helps avoid more severe problems and gets better results. We'll talk about the usual signs and what might cause them.
What is Encephalopathy?
Encephalopathy is a big word for a brain problem. It causes the brain to work differently, either for a little while or forever. This issue can show up in many ways, like not thinking clearly or having trouble moving. Things like infections, bad metabolism, or even a bump on the head can lead to encephalopathy. Also, health problems with the liver or kidneys are common causes.
Types of Encephalopathy
Different kinds of encephalopathy exist, each with its unique reasons and effects. Here are a few common types:
- Hepatic encephalopathy: It happens when a damaged liver can't get rid of harmful substances that then reach the brain.
- Chronic traumatic encephalopathy (CTE): People get this from many head hits, often seen in sports like boxing and football.
- Hypoxic-ischemic encephalopathy: This type comes from not enough oxygen or blood to the brain, causing harm.
- Metabolic encephalopathy: Due to body chemical problems, often from liver or kidney issues.
- Infectious encephalopathy: It's from brain infections, like bacterial or viral meningitis.
- Toxic encephalopathy: Due to harmful toxins or chemicals affecting the brain.
These are just a few kinds of encephalopathy, and there are many more. Knowing the type is key to getting the right help.
Common Encephalopathy Symptoms
Mental State Changes
Encephalopathy can change how we think and remember things. It leads to confusion, memory loss, and shifts in our personalities. People with this condition may also have trouble focusing and speaking clearly.
Physical Symptoms
Encephalopathy doesn't just affect the mind. It also brings physical changes like weak muscles and uncontrollable twitches. Other encephalitis symptomsinclude issues with eye movements and problems swallowing. Feeling tired and experiencing seizures are also common.

Encephalopathy Symptoms: Early Warning Signs
At first, encephalopathy may show subtle symptoms that are easy to miss. Key signs that something is wrong are:
- Cognitive changes: You might see small shifts in memory, focus, and how fast you react. These can signal encephalopathy is early stages.
- Personality shifts: Someone might act confused or forget more than usual. Mood changes without reason could point to encephalopathy.
- Difficulty with tasks: Problems could pop up with writing, figuring things out, or other thinking tasks.
The early signs are easy to overlook. But, picking up on them is key to early treatment and limiting brain damage. So, if you or someone you know is feeling any of these early warning signs, get medical advice very soon.
Causes of Encephalopathy
Encephalopathy often starts with liver disease, like cirrhosis. Cirrhosis makes the liver scarred and hard, not working right. This lets toxins, such as ammonia, build up in the blood. Too much of these toxins can cause hepatic encephalopathy.
Liver Disease and Cirrhosis
When the liver can't get rid of toxins, they stay in the blood. This includes ammonia, affecting the brain and causing hepatic encephalopathy. Patients with liver issues or cirrhosis are more likely to get encephalopathy because their livers can't work well.
Acute Liver Failure
Acute liver failure is sudden and can happen for different reasons, like viral hepatitis. When the liver stops working, toxins stay in the blood. This quickly affects the brain, causing serious symptoms of encephalopathy.
Portosystemic Shunts
If blood doesn't flow through the liver because of shunts, it can lead to encephalopathy. Shunts can occur with cirrhosis or after surgeries like TIPS. Without the liver filtering the blood, toxins build up and harm the brain.
Risk Factors and Precipitating Conditions
Encephalopathy can start because of different issues or events, like infections. Infections like viral meningitis can directly affect the brain, leading to encephalopathy. And, systemic infections can cause more liver or kidney problems. This makes it harder for the body to clear harmful toxins.
Medications and Toxins
Some medications and being around certain toxins can up the risk of encephalopathy. Drugs that make you sleepy or some painkillers can make encephalopathy symptoms worse. And, coming into contact with things like heavy metals or carbon monoxide can hurt the brain. This can cause encephalopathy.
Metabolic Imbalances
If your body's metabolic balance is off, it can also cause encephalopathy. This might happen if your organs aren't working right or if you're really dehydrated. For example, kidney failure or very high blood sugar can stop your brain from getting what it needs. This can spur on encephalopathy.
Diagnosing Encephalopathy
Diagnosing encephalopathy uses clinical checks and tests. Doctors do a full exam. They look at mental, nerve, and movement functions. They ask family about any behavior or thinking changes.
Clinical Assessments
Doctors check the patient's mind closely. They check awareness, direction, and recall. The team also looks at the patient's talking, moving, and reflexes for issues.
Doctors get details on the patient's past sickness, or contact with harmful things. This helps find encephalopathy causes.
Imaging and Laboratory Tests
Doctors may order tests like:
- Imaging tests: CT or MRI to check brain for issues.
- Blood tests: They check ammonia, body salts, and liver stuff for clues on encephalopathy causes.
- EEG: A test to look for brain issues through electric signals.
- Lumbar puncture: They take spinal fluid to test for infections or inflammation that might cause encephalopathy.
- Specialized tests: If needed, more tests like gene checks or liver function tests might be done to find the main issue.
These tests together help doctors find the type of encephalopathy. This lets them plan a right treatment to deal with the causes and help with symptoms.

Treatment and Management Strategies
Encephalopathy treatment is a mix of steps to handle its causes, cut down toxins in blood, and ease your symptoms. This mix involves medicines, changing how you live, and giving supportive help.
Treating encephalopathy linked to liver issues, like hepatic encephalopathy, often focuses on lowering ammonia in the blood. Doctors use drugs like lactulose, rifaximin, or neomycin to help with this. They might also advise eating less protein to lessen ammonia production.
Managing encephalopathy from metabolic problems or organ failure means dealing with the base issue. This can include drugs to fix electrolyte levels, help organs work better, or fight infections. These treatments target what's causing the problem.
For cases caused by sudden issues, like a brain injury or stroke, the care is about easing the brain, preventing more damage, and supporting recovery. This might include fluids through a vein, meds to stop seizures, or a machine to help breathing if needed.
Medications for general encephalopathy are used to tackle your main symptoms, like being confused, upset, or having seizures. You might get anti-psychotic, benzodiazepines, or anticonvulsant medicines. It's key to team up with your doctor to pick the right meds and doses for you.
No matter what's causing your encephalopathy, the main aim is to make you stable, treat the main factors, and help your brain work better. This work helps you get back to living your life fully.
Conclusion
Encephalopathy is very serious and affects your brain's work and health. Knowing the early signs helps you get quick medical help. This might help you get better, depending on the cause.
Problems like chronic traumatic encephalopathy from hits to the head or hepatic encephalopathy because of liver issues need early attention. Learning the signs and risks lets you act fast. You can work on the root issue and avoid more harm to your brain.
Encephalopathy is tricky and has many sides. But, with the right care, people can control the symptoms and keep a good life. Knowing about encephalopathy helps you spot signs early and get the help you need. This is key to safeguarding your brain health.
FAQ
What is encephalopathy?
Encephalopathy is a term for a change in brain function. It can show up as mental or muscle symptoms. These can include confusion or coordination problems.
What are the common types of encephalopathy?
Common types include hepatic, traumatic, and hypoxic-ischemic. Each has its own causes and challenges.
What are the common symptoms of encephalopathy?
It can bring on mental changes like confusion and physical signs like muscle twitches. Seizures may also happen.
What are the early warning signs of encephalopathy?
Early signs include small changes in thinking or behavior. You might feel tired, nauseous, or have weak muscles.
What are the common causes of encephalopathy?
Liver problems, infections, and toxins can lead to encephalopathy. Liver disease is a main cause, along with acute liver failure.
What are the risk factors and precipitating conditions for encephalopathy?
Infections, toxins, and certain meds can up the risk. So can metabolic problems, like from organ failure or dehydration.
How is encephalopathy diagnosed?
Doctors use tests and exams to diagnose it. Clinical tests and brain scans might be done. Blood tests are also used to find the cause.
How is encephalopathy treated and managed?
Treatment varies by cause and symptom severity. It focuses on fixing the root issue, easing toxin build-up, and managing symptoms.
Source Links
- https://www.healthdirect.gov.au/encephalopathy
- https://my.clevelandclinic.org/health/diseases/21220-hepatic-encephalopathy
- https://www.ncbi.nlm.nih.gov/books/NBK430869/
- https://www.webmd.com/brain/what-is-encephalopathy
- https://www.aurorahealthcare.org/services/neuroscience/neurology/neurological-conditions/encephalopathy
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/encephalitis
- https://www.mayoclinic.org/diseases-conditions/encephalitis/symptoms-causes/syc-20356136
- https://www.advocatehealth.com/health-services/brain-spine-institute/brain-care-center/conditions-treatments/encephalopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8917954/
- https://www.medicinenet.com/encephalopathy/article.htm
Exploring Encephalopathy Causes: A Comprehensive Guide
Encephalopathy is a neurological disorder that affects brain function. It can greatly impact health and well-being. This guide offers a deep dive into potential causes. It covers common triggers like encephalopathy causes such as cirrhosis and alcohol abuse. It also mentions metabolic issues and exposure to toxins. By understanding the encephalopathy symptoms and diagnosis, you'll be better prepared. You'll learn about different forms of encephalopathy. This includes issues like neurotoxic and manganese-related problems. Our aim is to help you work with your healthcare team. Together, you can find the cause and explore encephalopathy treatment options.
This guide dives into the various causes of encephalopathy. It starts with common causes, like cirrhosis and alcohol use. It goes on to discuss rare but important factors like toxic substances. Knowing the causes is key to diagnosis and care. It includes blood tests, images, and brain checks. These tools help work with your healthcare team. Together, you can find the best treatment. With this knowledge, facing encephalopathy becomes easier. You can strive for the best health outcomes.
Introduction to Hepatic Encephalopathy
What is Hepatic Encephalopathy?
Hepatic encephalopathy happens when the brain is harmed by severe liver issues. Toxins not removed by the failing liver can build up. These toxins affect the brain, causing a variety of symptoms. At first, someone may just seem a bit confused. But, this can get much worse, even leading to coma in the worst cases.
Prevalence and Impact
About 30% of people with cirrhosis may face hepatic encephalopathy. This shows how common and serious the condition is. It can disrupt daily life and cause severe complications. This makes it a major worry for those with liver diseases, especially cirrhosis.
Encephalopathy causes
The main cause of hepatic encephalopathy is cirrhosis. Cirrhosis is a severe liver disease. It happens when the liver gets scared and can't work right. This causes toxins to build up in the blood. These toxins can harm the brain. Drinking too much alcohol over a long time can also lead to alcoholic liver disease. This can cause cirrhosis and hepatic encephalopathy.
Cirrhosis
Hepatitis can lead to cirrhosis too. Hepatitis is liver inflammation, often due to viruses. Over time, this can increase the risk of hepatic encephalopathy. Also, taking drugs that are bad for the liver can lead to hepatic encephalopathy.
Alcohol Abuse
Sometimes, metabolic encephalopathy can be linked to hepatic encephalopathy. Metabolic encephalopathy is a problem with the brain's biochemical functions. It may happen with liver diseases too. Wernicke encephalopathy is a rare problem. It's caused by not getting enough thiamine, which is vitamin B1. This problem is mostly linked to alcoholism and malnutrition but can also affect liver health.
Hepatitis
Other less common causes of encephalopathy are low blood sugar, carbon monoxide poisoning, and fluid build-up in the brain without high pressure.
Drug Intoxication
Metabolic Encephalopathy
Problems like diabetes, liver diseases, kidney failure, or heart problems can cause metabolic encephalopathy.
Wernicke Encephalopathy
Wernicke encephalopathy happens because of not enough thiamin or vitamin B1. It's often found in people who drink too much and are malnourished.
Other Rare Causes
Hypoglycemia, carbon monoxide poisoning, and normal pressure hydrocephalus are other uncommon reasons for encephalopathy.
Diagnostic Evaluation
Diagnosing hepatic encephalopathy means running many tests, looking at liver function and blood. We check blood ammonia levels to see if the liver isn't working well. Liver function tests show how the liver is doing by checking blood for certain enzymes.
A complete blood count and electrolyte panel give hints about liver disease's effects. Arterial blood gas analysis shows if there are issues with oxygen and carbon dioxide. Imaging tests like CT scans and MRIs look for liver changes. A test called EEG (Electroencephalogram) finds brain activity changes in hepatic encephalopathy.
Doing all these tests helps doctors make sure it's hepatic encephalopathy and not something else.
Neurotoxic Encephalopathy
Neurotoxic encephalopathy is caused by harmful substances affecting the brain. It shares some symptoms with hepatic encephalopathy. Both can happen when the brain gathers too many toxins.
Symptoms and Diagnosis
This illness may change how you think, remember, see, and feel. It could cause dizziness, headaches, nausea, and shift your mood. Doctors figure out if you have it by checking your work, medicines you've taken, and doing brain tests.
Imaging Findings
By looking at the brain with MRI vision, doctors can spot some key signs. They might find issues like too much dopamine, parts of the brain that are smaller, nerve damage, and unusual brain activity.
Toxic Exposure Sources
Living near industrial sites or using certain drugs may raise your risk. Lead, in things like pills and perfumes, is a common culprit. Figuring out what's harming you is vital to stop the damage.
Finding some types of this disease is not easy but very important. Misusing antipsychotic drugs or being around certain fumes can badly affect your nerves. Stories, like JetBlue’s Andrew Myers, show the real risk.
Testing includes brain scans and checking your brain waves. There's no cure, so doctors focus on easing symptoms. Sometimes surgery or special diets are needed. But steering clear of the toxin is the best way to protect your brain.
Manganese Neurotoxicity
Manganese neurotoxicity, or manganism, is linked to too much exposure to manganese. It shows up like Parkinson's disease with symptoms like shaking, stiff muscles, and trouble moving. Brain scans can reveal changes in the part of the brain that controls movement.
Parkinsonism and Manganese
Too much manganese can lead to issues similar to Parkinson's, affecting how you move. This can include shaking, stiff muscles, and problems with balance. In a case, a man who welded steel developed these issues after seven years without protection.
Neurocognitive Effects
Being around manganese a lot can harm how your brain works. You can have trouble thinking, remembering things, and your mood might change. It's very important to find this early and help the person to avoid lasting damage.

Carbon Monoxide Poisoning
Carbon monoxide poisoning can lead to brain problems with both quick and slow neurological effects. When someone is first exposed to it, they could get confused, feel dizzy, or even fall into a coma. Later on, they might have issues like Parkinsonism, which affects how they move.
Acute and Delayed Effects
Some people might not feel the worst effects until days or weeks after breathing in carbon monoxide (CO). These effects include memory loss and a more severe type of nerve damage. People who breathed in a lot of CO showed fewer cells that help protect the brain, making their nerve damage worse.
Neuroimaging Findings
Doctors can use CT and MRI scans to see brain damage linked to carbon monoxide. This damage often shows up on both sides of the brain, especially in a part called the globus pallidus. The scans might show the damaged area as a low signal on T1 and a high signal on T2/FLAIR.
Prevention and Treatment
It's important to avoid breathing in carbon monoxide with good air flow, CO detectors, and quick poisoning treatment. Treating someone may mean giving them more oxygen, drugs, and therapy to help with brain issues. Things like broken heaters, cars without enough fresh air, and house fires are big causes of carbon monoxide problems.
Other Encephalopathy Causes
There are various causes of encephalopathy. Liver issues are the main ones. But, there are rare but important causes to know. For example, Methyl mercury poisoning can cause different symptoms like issues with vision and problems with moving. Methyl bromide toxicity, from breathing in chemicals, can hurt the brain and the part that controls movement. Poisoning from organotins, found in some work and farm chemicals, can also make movement difficult. Knowing about and treating these causes early can help stop severe brain issues.
Methyl Mercury Poisoning
Methyl mercury poisoning is a serious issue. It happens from eating fish with too much mercury. This mercury harms the brain. It causes problems with vision and movement.
Methyl Bromide Toxicity
Being exposed to Methyl bromide can also be harmful. This substance is used in certain jobs and on farms. It can cause problems in the brain and with movement. It's vital to have good safety rules to prevent this harm.
Organophosphate Poisoning
Organophosphate poisoning comes from certain chemicals in work and on farms. It can make moving and daily life hard. People need to be very careful with these chemicals to avoid getting sick.
Conclusion
This guide has covered many reasons for encephalopathy, a brain issue that limits function. We looked at common causes like cirrhosis and drinking too much. Not as often, things like chemicals and body issues play a big part too. Learning these reasons is key to finding the right care.
Understanding encephalopathy is our aim here. We want you to feel ready to face this problem with your doctors. If you worry about what causes it, how it's found, or what to do, this guide helps. Now you can take an active part in your health journey.
FAQ
What is encephalopathy?
Encephalopathy is a complex brain problem. It makes brain work bad. Many things can cause it, like liver issues, toxic things, and problems with how the body uses energy.
What are the common causes of encephalopathy?
Encephalopathy is often seen with liver damage, drinking too much, liver viruses, and drug overdose. It also happens with body energy problems and a specific brain injury called Wernicke encephalopathy.
How is hepatic encephalopathy diagnosed?
Doctors use many tests to find hepatic encephalopathy. They do blood tests to check ammonia and liver health. They also use brain scans like CT or MRI, and tests that look at brain waves (EEG).
What are the symptoms of neurotoxic encephalopathy?
Neurotoxic encephalopathy has symptoms like being confused, not thinking right, and changes in the brain's way of working. Tests like special brain images show these changes.
How is manganese neurotoxicity (manganism) diagnosed?
Doctors find manganism by looking at symptoms like those in Parkinson's disease. They also use brain imaging, especially MRI, to confirm the disease.
What are the effects of carbon monoxide poisoning on the brain?
Carbon monoxide can harm the brain right away or later. This may cause confusion, dizziness, coma, and Parkinson's or other problems with moving. Special brain images can show certain damages from carbon monoxide.
What are some other rare causes of encephalopathy?
Rarer causes of encephalopathy are poisoning by methyl mercury, methyl bromide, and organotin. These can cause unique nerve issues and brain changes.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7930293/
- https://www.ncbi.nlm.nih.gov/books/NBK430869/
- https://my.clevelandclinic.org/health/diseases/21220-hepatic-encephalopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668878/
- https://www.webmd.com/brain/what-is-encephalopathy
- https://www.advocatehealth.com/health-services/brain-spine-institute/brain-care-center/conditions-treatments/encephalopathy
- https://www.mayoclinic.org/diseases-conditions/encephalitis/diagnosis-treatment/drc-20356142
- https://www.medicinenet.com/encephalopathy/article.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3521923/
- https://en.wikipedia.org/wiki/Toxic_encephalopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10166376/
- https://www.e-jmd.org/journal/view.php?doi=10.14802/jmd.20123
- https://pubmed.ncbi.nlm.nih.gov/30578768/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8011735/
- https://radiopaedia.org/articles/carbon-monoxide-poisoning-1?lang=us
- https://www.healthdirect.gov.au/encephalopathy
Understanding Encephalitis Symptoms: What to Look For
Encephalitis is a serious illness that causes the brain to swell. This swelling can happen because of a virus or bacteria. Or, your immune system might fight your brain by mistake. It's very important to know the encephalitis symptoms. This knowledge can save lives, making it critical to get early diagnosis and treatment.
There are two main kinds of encephalitis. Infectious encephalitis comes from a virus, while autoimmune encephalitis is when your immune system attacks your brain. But no matter the cause, it's key to watch for possible symptoms of encephalitis. If you or anyone you know shows these signs, seeking medical help right away is advised.
What is Encephalitis?
Encephalitis (en-sef-uh-LIE-tis) means your brain is inflamed. It can happen from viruses, bacteria, or your own immune system attacking. This can be very serious.
Overview of Encephalitis
Encephalitis can have big effects. It can even cause death. What's interesting, is we don't know the cause about half of the time.
Types of Encephalitis
There's infectious and autoimmune encephalitis. Infectious means a germ causes it. Autoimmune happens when your body attacks your brain.
Infectious vs. Autoimmune Encephalitis
Infectious encephalitis starts with the flu, then gets worse. You might get confused or have seizures. Autoimmune encephalitis shows up slower. You could lose your memory or see things that aren't there.
Common Encephalitis Symptoms
It's crucial to know the common symptoms of encephalitis for quick diagnosis and treatment. Encephalitis shows different symptoms. This depends on its cause and type.
Physical Symptoms
At first, encephalitis can feel like the flu. You might have a headache, fever, and feel tired. As it gets worse, you could also feel confused, have seizures, or see changes in how you move or hear.
Cognitive Symptoms
In some cases, symptoms show up more slowly, over weeks. You might start acting differently, have trouble remembering, or even see things that aren't there. These symptoms can really change how a person lives day to day.
Symptoms Due to Specific Types
The signs of encephalitis change based on its root cause. For instance, if a virus is the cause, it might seem like the flu at first. But if it's autoimmune, the changes might happen more slowly, with shifts in behavior and thinking. Knowing these differences can help with diagnosis.
Encephalitis symptoms
Early Warning Signs
Encephalitis warning signs can feel like the flu. You might have a headache, fever, and feel tired. It's easy to miss these symptoms, but seeing a doctor quickly is important.
Severe Symptoms Requiring Immediate Care
Some signs of encephalitis are severe and need quick attention. These include being confused, acting strange, or having seizures.
You may also find it hard to move some parts of your body or pass out. If these happen fast over hours or weeks, you need to get treated right away.
Symptoms in Infants and Children
Babies and young kids can show different signs of encephalitis. They might not eat well, feel stiff, or be upset a lot.
Watch for a bulging soft spot on their head, throw up, or be very fussy. A doctor should check them out right away.
Causes and Risk Factors
Encephalitis is often caused by viruses. Types like herpes, Epstein-Barr, and West Nile are common. These viruses can make the brain swell, which can cause serious problems.
Viral Causes
In the U.S., herpes types 1 and 2 are a big cause. They impact about 10% of cases. Unfortunately, this kind of encephalitis is very severe, with a high death rate if not treated.
Bacterial and Other Infectious Causes
But it's not just viruses; bacteria and other germs can also lead to encephalitis. Some bacteria, like those spread by mosquitoes, can cause serious issues like encephalitis.
Autoimmune Encephalitis Causes
Less often, the body's immune system can wrongly attack the brain. This leads to swelling and serious conditions. Special treatments like removing tumors might be needed in these cases.
Risk Factors for Encephalitis
Age plays a big part in who gets encephalitis. Young kids and older people are more at risk, as are those with weak immune systems. Where and when you are also matter, as certain infections are more common in some places and during warmer times.
Diagnosing Encephalitis
Diagnosing encephalitis needs a detailed medical history and a full physical exam. Tests are also critical. Doctors will try to figure out what's causing your symptoms and how to treat it.
Medical History and Physical Exam
Your doctor will first ask about your health history. They'll want to know about recent sickness, where you've been, and what you've been around. Then, they'll do a careful exam. They'll look for things like swelling and problems with the nerves, which could be signs of encephalitis.
Diagnostic Tests for Encephalitis
Tests can vary based on your symptoms and possible causes. But they may include:
- Neuroimaging (MRI or CT scan) to look for brain swelling or issues
- Lumbar puncture (spinal tap) to check your cerebrospinal fluid for infection
- Electroencephalogram (EEG) to see your brain's activity and any seizure signs
- Blood, urine, or throat samples to find viruses or other germs
- Imaging studies to find tumors that might be causing a reaction in your body
In complex cases, a brain tissue biopsy or intracranial pressure monitoring might be needed. This helps with a certain diagnosis and treatment plan.
Treatment Options
If you're diagnosed with encephalitis, treatment depends on its cause and symptoms' seriousness. The main goals are to treat the cause, handle symptoms, and avoid problems. You may get antiviral or antibiotic drugs, immunotherapies, and help for day-to-day activities. Rehabilitation might also be part of the plan.
Antiviral and Antibiotic Medications
Viral encephalitis might need antiviral drugs like acyclovir, foscarnet, or ganciclovir. They fight the virus and make symptoms less severe. If a bacterial infection causes it, you might take antibiotics.
Immunotherapy for Autoimmune Encephalitis
If autoimmune encephalitis is the issue, you might need immunotherapies. These include corticosteroids, IVIg, or plasma exchange to lower the immune system's attack and brain inflammation.
Supportive Care and Symptom Management
Supportive care is vital, no matter the cause. It includes help with breathing, IV fluids, anti-inflammatory drugs, and anti-seizure meds. They aim to reduce symptoms and avoid lasting issues. Rehabilitation like physical or speech therapy also helps recovery.
For a sudden or severe encephalitis case, prompt medical care is essential. An expert team, with infectious disease and neurology specialists, will create a treatment plan just for you.
Conclusion
Encephalitis outcomes vary a lot, based on the cause, how bad it is, and how quickly it's treated. In mild cases, people often fully recover. But in severe cases, there might be lasting brain problems or even death. Lately, encephalitis cases have been increasing, with 7 to 15 out of every 100,000 people worldwide facing it.
Prognosis and Recovery
If someone has severe encephalitis, getting better can take a long time and it's hard. They might need months or years of rehab and help from lots of doctors. About half of those who survive Japanese encephalitis could have lasting mental and brain issues. And for some viruses, like West Nile, the chance of dying is as high as 30%.
Prevention Tips
To stop encephalitis, it's key to keep clean, get all your shots, and avoid mosquito and tick bites, especially in risky places. The chance of getting encephalitis from dengue, Zika, or chikungunya viruses is between 0.5% and 20%. This tells us we should be active in protecting ourselves and our family.
FAQ
What is encephalitis?
Encephalitis is brain tissue inflammation. It can come from a virus, bacteria, or the body attacking itself. There are two main types - infectious and autoimmune encephalitis.
What are the common symptoms of encephalitis?
Symptoms include confusion, personality changes, and seizures. You might have trouble moving and see or hear things differently. Infectious encephalitis symptoms are like the flu at first, then worsen. Autoimmune encephalitis signs show up slowly over weeks.
What are the early warning signs of encephalitis?
Look out for the flu's early signs plus confusion, seizures, or trouble moving parts of your body. If you lose consciousness, get help right away.
What causes encephalitis?
Viruses, like herpes simplex and mosquito-borne ones, cause most infectious encephalitis cases. Autoimmune encephalitis happens when the body attacks the brain by mistake, sometimes due to a tumor.
How is encephalitis diagnosed?
Diagnosis involves medical history, a physical exam, and tests like neuroimaging and a lumbar puncture. EEG, and blood/urine/stool tests also help.
How is encephalitis treated?
Treatments vary by cause and include antiviral drugs, antibiotics, and immunotherapies. You might need help controlling seizures, and some cases rely on supportive care.
What is the prognosis for encephalitis?
Outlooks depend on the cause, how bad it gets, and quick treatment. Mild cases might fully recover, but severe ones can cause lasting problems or death. Healing from serious encephalitis can take months to years and needs a lot of rehab.
How can encephalitis be prevented?
Avoiding encephalitis means good hygiene, getting vaccines, and preventing bites from mosquitoes and ticks.
Source Links
- https://www.mayoclinic.org/diseases-conditions/encephalitis/symptoms-causes/syc-20356136
- https://www.webmd.com/a-to-z-guides/understanding-encephalitis-basics
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/encephalitis
- https://www.nhs.uk/conditions/encephalitis/
- https://www.ninds.nih.gov/health-information/disorders/encephalitis
- https://www.healthline.com/health/encephalitis
- https://www.mayoclinic.org/diseases-conditions/encephalitis/diagnosis-treatment/drc-20356142
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8668867/
Duchenne Muscular Dystrophy Treatment Options
Duchenne muscular dystrophy (DMD) is a rare and serious genetic condition. It causes progressive muscle weakness and wasting. This leads to heart and breathing problems that can be life-threatening.
While there's no cure yet, several treatment options are available. These can help manage the symptoms and make life better for those with DMD. Options include mobility and breathing help, steroid drugs, and new treatments like gene therapy. Skipping faulty parts of the gene (exon skipping) is another area of hope.
Support is key in living with DMD. It involves managing swallowing, nutrition, and heart issues. Also, surgery might be needed. Learning about the condition and finding support are crucial.
Understanding Duchenne Muscular Dystrophy
Duchenne muscular dystrophy hurts young boys mostly today. It comes from a bad gene that makes a key protein missing. This protein keeps muscles strong.
Without it, muscles get weak and waste away. This makes moving hard, your breath might not work well, and your heart could get sick.
What is Duchenne Muscular Dystrophy?
This illness is because of a missing protein called dystrophin. It helps keep muscle cells strong and working right. Without it, the body's muscles start to break down.
This happens in the arms, legs, heart, and even the muscles you breathe with. The loss of muscle strength and function leads to serious trouble moving and breathing.
Symptoms and Progression
Signs of Duchenne start showing in early childhood, perhaps by age 3-6. Children start having trouble walking and going up stairs. Over time, this gets worse.
It makes it hard to move and breathe. The heart might also face big problems.
Causes and Genetic Factors
A change in the dystrophin gene causes this disease. It's on the X chromosome. Most cases happen when a part of this gene is missing or added extra. This change stops the body from making enough dystrophin protein.
It passes from parents to children in an X-linked way. Boys are often more affected. Girls can have a milder form if they're carriers, but not all carriers show signs
.
Duchenne muscular dystrophy treatment: Conventional Approaches
There's no cure for Duchenne muscular dystrophy yet. But, many traditional treatments can help ease the symptoms and slow the disease down. For example, physical therapy, using special devices, and getting help with breathing are very important. They all help to stay mobile and enjoy life with more ease.
Mobility and Breathing Assistance
For people with Duchenne muscular dystrophy, it's vital to keep moving. This can be done with physical therapy, special braces, and gadgets. Also, support for breathing, through devices like ventilators, is crucial. It helps avoid breathing problems.
Steroid Medications
Corticosteroids, a type of steroid, are proven to make muscles stronger in this disease. They slow down how fast the sickness gets worse. But, these steroids can have side effects.
Ataluren for Ambulatory Patients
Ataluren is a medicine for kids with Duchenne who can still walk. It works by targeting the disease's gene problem. This may help keep muscles working better and possibly delay not being able to walk.
By using these traditional and new treatments, along with good care, the goal is to make life better for those with Duchenne muscular dystrophy.
Emerging Therapies and Clinical Trials
Researchers keep finding new ways to treat Duchenne muscular dystrophy, like through clinical trials. The FDA has recently approved Elevidys. It's the first gene therapy for DMD in kids. This therapy brings a gene that makes a short version of the needed dystrophin protein. This protein is key to keeping the muscles working well.
Gene Therapy: Elevidys
The FDA approving Elevidys, by Sarepta Therapeutics, is a big step in gene therapy for DMD. It uses a special virus to carry a mini-dystrophin gene to the muscles. Early trials had over 140 kids, and later 120 more joined. The results are exciting. Boys using this therapy for years are getting better at things like standing up, jumping, and running. These improvements are rare in older DMD patients.
Exon Skipping
Exon skipping is another new approach. It tries to go around the genetic mistakes causing DMD. This may help make more working dystrophin, slowing down the disease.
Stem Cell Research
There's hope in stem cell research too. Scientists aim to use stem cells to fix muscle damage and make muscles work better. This might help manage DMD more effectively and slow it down.
With gene therapies, exon skipping, and stem cell research, new doors are opening for treating DMD. As research goes on, there's hope for better care and outcomes for patients and their families in the future.
Supportive Care and Quality of Life
Supportive care is essential in managing duchenne muscular dystrophy and making life better for those with it. People facing this disease could have problems eating and swallowing. However, dietary changes and help with feeding can solve these issues.
It's vital to keep the heart healthy for those with Duchenne muscular dystrophy. This condition might cause heart problems like irregular heartbeats and a weak heart. Doctors should check the heart regularly. Sometimes, using medicines or devices such as pacemakers is needed to keep the heart strong.
In serious cases, surgeries might be needed to help with problems like a curved spine or stiff joints. These issues can make it harder to move and live well. This caring approach helps tackle many of the problems Duchenne muscular dystrophy brings. It aims to give the best life to those touched by the disease.

Patient Education and Support Resources
Dealing with Duchenne muscular dystrophy (DMD) can be a lot for patients and families. It's important to learn about the disease and find help. This way, those with DMD and their family members can take part in making choices about their care.
Connecting with Support Groups
Joining support groups, near and far, is very helpful. They can offer both emotional and useful support. These groups let people share their stories and ways of dealing with the disease.
Organizations like the Family Caregiver Alliance (FCA) and the PACER Center also help a lot. They have special programs and tips for those caring for someone with DMD.
Accessing Clinical Trial Information
Knowing about new treatments through clinical trials is key. Websites like ClinicalTrials.gov share lots of info on studies worldwide. This can help patients look into new treatments.
Plus, programs like the Duchenne Scholarship by Route 79 help with education after high school. This can give young people extra support in their journey.
Conclusion
Duchenne muscular dystrophy is a serious genetic condition that affects the muscles. It needs a lot of different kinds of care. Right now, there's no cure. But, we have treatments that help with symptoms and make life better.
There are many ways to help, from helping with moving and breathing to new gene therapy. Everyone is working to slow down the disease and make life better for those with it.
Staying updated on Duchenne muscular dystrophy treatments and getting support helps. Families can feel more confident by being part of the treatment process. With new research and treatments, there is hope for the future.
As the disease grows, using all available treatments and care is important. This can help those affected live better. Working with doctors and using available support can bring hope.
FAQ
What is Duchenne muscular dystrophy?
Duchenne muscular dystrophy is a rare, serious genetic condition. It causes muscle weakness and wasting over time. This happens because of a missing protein called dystrophin.
What are the symptoms of Duchenne muscular dystrophy?
It starts showing in early childhood, around 3 to 6 years old. Kids with this disease lose muscle strength. They face trouble moving, breathing, and their hearts can get weak.
What causes Duchenne muscular dystrophy?
A problem with a gene leads to not having enough dystrophin. This affects how muscles work. Understanding this gene helps in finding better treatments.
What are the conventional treatment options for Duchenne muscular dystrophy?
Doctors use many ways to help, like physical therapy and special devices. Steroids can make muscles stronger. Also, there's ataluren, a medicine for some patients.
What are the emerging therapies for Duchenne muscular dystrophy?
Scientists are looking into new treatments. This includes gene therapy, exon skipping, and stem cells. They hope these will help slow down the disease.
How does supportive care help manage Duchenne muscular dystrophy?
Care that supports daily life is very important. It helps with eating, heart health, and surgeries for body issues. This kind of care makes life better for those with Duchenne.
How can patients and families navigate Duchenne muscular dystrophy?
Coping with Duchenne is hard, but there are ways to get through it. Learning from support groups and trials is key. It helps patients and families take better care of themselves.
Source Links
- https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapy-treatment-certain-patients-duchenne-muscular-dystrophy
- https://www.nhs.uk/conditions/muscular-dystrophy/treatment/
- https://www.mda.org/disease/duchenne-muscular-dystrophy/medical-management
- https://www.ncbi.nlm.nih.gov/books/NBK482346/
- https://emedicine.medscape.com/article/1259041-treatment
- https://www.nature.com/articles/s41572-021-00248-3
- https://www.drugtargetreview.com/article/145291/developing-an-mrna-therapy-for-duchenne-muscular-dystrophy/
- https://www.urmc.rochester.edu/news/story/new-gene-therapy-for-duchenne-muscular-dystrophy-a-monumental-advance
- https://www.sciencedirect.com/science/article/abs/pii/S1474442222001259
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4966503/
- https://www.duchenne.com/community-resources/resources-and-support
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6014617/
What Is Duchenne Muscular Dystrophy?
Duchenne muscular dystrophy (DMD) is not common. It affects mostly young boys. They face issues with their muscles that get worse over time. This disease harms their heart and lung muscles too.
It is because of a changed dystrophin gene. This gene helps make a special protein for muscles. Missing this protein makes the muscles break down. Boys usually show signs when they are 2 or 3.
Normally, DMD is found in boys only. But, girls may also get it, though it’s rare. In Europe and North America, around 6 out of every 100,000 people have DMD.
Understanding Duchenne Muscular Dystrophy
Duchenne muscular dystrophy (DMD) is a genetic disorder that weakens muscles. It's one of four related conditions.
The others are Becker muscular dystrophy, an in-between form, and DMD-associated dilated cardiomyopathy.
Definition and Overview
Duchenne muscular dystrophy is a common hereditary disease. It affects about 2 in 10,000 people in the U.S.
This disease happens when a specific gene isn't working right. This gene makes a protein called dystrophin that our muscles need.
Without enough dystrophin, our muscles can't work well or fix themselves. This leads to muscle problems over time.
Prevalence and Affected Population
Worldwide, DMD affects about 6 in every 100,000 people. It mostly hits young boys. Around 1 in 3,600 baby boys are born with this each year.
Not long ago, boys with DMD didn't live very long. But, better medical treatments have changed that. Now, they can live up to 30 years or more.
| Statistic | Value |
|---|---|
| Prevalence of DMD in Europe and North America | Approximately 6 per 100,000 individuals |
| Estimated incidence of DMD | 1 in 3600 male live-born infants |
| Prevalence of DMD in the United States | Approximately 2 per 10,000 individuals |
| Percentage of DMD cases due to new mutations | 30% |
| Percentage of carrier females affected by muscular weakness | 2.5% to 20% |
A woman who carries the faulty gene might not feel weak herself. But, 2.5% to 20% may have some muscle issues.
Also, many cases of DMD come from new mutations. They are not always inherited from a parent.
Duchenne muscular dystrophy Symptoms
The main symptom of Duchenne muscular dystrophy is muscle weakness. It can start when a child is 2 or 3. This weakness usually begins in muscles near the core of the body.
Then, it moves to muscles closer to the hands and feet.
Early Signs and Indicators
Early signs of DMD include issues with jumping and running. Boys might have a hard time walking and have a waddling walk. You might also notice their calf muscles getting bigger.
These signs can show up when they're still toddlers.
Progression of Muscle Weakness
The muscle weakness in DMD keeps getting worse. It starts to affect more and more muscle groups. By school age, children with DMD may walk on their toes and have trouble using their arms.
Often, they end up using a wheelchair by age 12 as the disease progresses.
Impact on Respiratory and Cardiac Function
DMD also affects how the heart and lungs work. Those with DMD don't usually live past their 20s. They might die from breathing problems or a weak heart. If not managed well, the effect on breathing and heart health can be very serious.

Causes and Genetic Factors
Duchenne muscular dystrophy (DMD) happens due to a gene mutation. This mutation affects the dystrophin protein, key for muscle function. Without it, muscles can't work or heal well, leading to their weakness in DMD.
Role of Dystrophin Protein
The dystrophin protein is vital for muscle cell structure. It links parts inside the cell to its outer layer. But, if the gene for dystrophin is mutated, this connection fails, and muscles start breaking down.
X-Linked Inheritance Pattern
DMD is inherited in an X-linked recessive way, so the faulty gene sits on the X chromosome. Thus, males with a mutation develop DMD because they have one X chromosome. Females, with two Xs, can be carriers if the mutation is on one X. The other X might usually have a healthy copy.
In some families, DMD appears without a past history because mutations can start anew. Women carrying the gene have a 50% chance of passing it to their children. This means a 50% chance of their sons having Duchenne.

| Genetic Factor | Explanation |
|---|---|
| Dystrophin Protein | The dystrophin protein is vital for muscle cells’ health. But if its gene has a mutation, a non-working or missing protein leads to muscle problems. |
| X-Linked Inheritance | DMD's inheritance pattern is X-linked recessive, placing the faulty gene on the X chromosome. Males with one mutation suffer from DMD. Females, having one healthy X, are often just carriers. |
| Spontaneous Mutations | One-third of DMD cases surprise families with no past record, due to new mutations. Carrier women have the same 50% risk of passing the mutation on to their children. |
Diagnosis and Testing
Diagnosing Duchenne muscular dystrophy (DMD) mixes physical checks with genetic tests. Doctors will look at the child's muscle strength, flexibility, and reflexes. They also search for muscle wasting and big calf muscles.
Physical Examination
A doctor measures the child's muscle use and growth. They watch how the child walks and stands from a sit. They also test other movement skills to spot early DMD signs. Doctors look for big calf muscles, a key DMD clue.
Genetic Testing and Analysis
Genetic tests pin down DMD and its specific gene issue. A muscle or blood sample is checked for mutations in the DMD gene. Around 70% to 80% of DMD cases have these mutations.
| Diagnostic Marker | DMD | BMD |
|---|---|---|
| Creatine Kinase (CK) Levels | They hit 10-20 times the limit by age 2, then drop 25% yearly | Elevated 5 times or more |
| Dystrophin Quantity | Less than 5% of normal | Usually more than DMD |
| Age of Onset | Starts in early years, usually age 2-3 | Can begin at 5-60 years, sometimes loss of walking later |
Exam and genetic test results combined give a DMD diagnosis. This diagnosis shows the exact genetic issues. Knowing this helps plan the best treatments.
Treatment and Disease Management
There's no cure for Duchenne muscular dystrophy (DMD) yet. But, its treatment helps manage symptoms and improve life quality. Supportive care and therapies are key for DMD management.
Supportive Care and Therapies
Steroids like prednisone and deflazacort can boost muscle strength for 6 months to 2 years in DMD patients. Physical and occupational therapy, with assistive devices, improve life quality and length for those with DMD.
For a few, creatine supplements help make muscles stronger. In later DMD stages, eating and swallowing trouble might happen. This is called dysphagia. It needs special care.
Sometimes, surgery is needed for issues like scoliosis, or tight tendons. This can make life better for DMD patients by fixing serious muscle problems.
Emerging Treatments and Clinical Trials
Today, researchers look for new ways to treat Duchenne muscular dystrophy. They are testing "exon skipping" for DMD in the UK and the Netherlands. This might be a new duchenne muscular dystrophy treatment approach.
There are now more medicines to fight DMD. Duvyzat helps slow down the disease and makes moving easier. Medicines like Eteplirsen (Exondys 51) and Ataluren (Translarna) target specific types of DMD. These increase dystrophin, an important protein for muscle health.
Gene therapies are also in development, aiming for future FDA approvals. Many clinical trials are ongoing. They look for new ways to help people with muscular dystrophy.

Living with Duchenne Muscular Dystrophy
Living with Duchenne muscular dystrophy (DMD) includes many challenges. But with support and strategies, both the person and their family can enjoy life. It's about managing the physical, emotional, and social parts of DMD well, to thrive.
Coping Strategies and Support
It's important to have good ways to cope with DMD. Talking to other families dealing with the same issues can be a big help. This includes joining support groups both online and in person to feel less alone and to share advice.
And don't forget about getting professional support like therapy. A counselor can help you and your family handle the tough feelings that may come up. They offer advice on dealing with stress and worry, and help you find ways to feel better.
Quality of Life Considerations
Focusing on a good life quality is crucial for those with DMD. You may need to adjust your living space, use tools that help, and maybe change how you learn or work. Adapting to new needs and limits over time is important.
Working with your healthcare team, teachers, and local groups is key. They can help you get the support and changes you need to live well. By standing up for what you require and being open to new ways of doing things, you can feel more independent and fulfilled.
| Coping Strategies | Quality of Life Considerations |
|---|---|
|
|
Conclusion
Even though Duchenne muscular dystrophy (DMD) is rare and hard to deal with, we've made great strides in its care. More is known about its causes. We have better ways to help. Plus, there are new treatments that give families hope for a better life. This isn't the end of the fight. But, with more research and teamwork, things are looking up for those with Duchenne muscular dystrophy.
It's important to keep learning about the latest treatments and getting support. This helps you face the challenges with strength. As we push forward, there is hope for better days. Together, we can make life better for those with Duchenne muscular dystrophy.
The search for a cure is ongoing. And the progress that's been made is uplifting. There's a strong drive to beat this disorder. Through awareness and working together, we aim for a future where this disease is less of a burden. There is hope for a better tomorrow for everyone touched by Duchenne muscular dystrophy.
FAQ
What is Duchenne muscular dystrophy (DMD)?
Duchenne muscular dystrophy (DMD) is a rare genetic disorder. It affects mainly young boys. They have weakening muscles because certain muscles are lost over time. This includes muscles in the skeleton, heart, and lungs.
What are the primary symptoms of Duchenne muscular dystrophy (DMD)?
The main symptom of DMD is muscle weakness. It often begins when the child is 2 or 3 years old. First, muscles close to the core weaken, then those near the hands and feet.
What causes Duchenne muscular dystrophy (DMD)?
DMD happens because of a missing protein. This protein, called dystrophin, is vital for muscles. Without it, muscles can't work or repair themselves right. That's why they become weaker over time.
How is Duchenne muscular dystrophy (DMD) diagnosed?
Doctors diagnose DMD with a physical check-up and genetic tests. They test muscle strength, flexibility, and reflexes. They also look for certain signs in the muscles, like how the calf muscles change.
How is Duchenne muscular dystrophy (DMD) treated?
There's no cure for DMD yet. But treatments aim to improve quality of life and manage symptoms. Supportive care and certain therapies are very important for people with DMD.
What is it like to live with Duchenne muscular dystrophy (DMD)?
It's not easy living with DMD. But having the right support and strategies helps. People with DMD and their families can still have a good life.
Source Links
- https://www.ncbi.nlm.nih.gov/books/NBK482346/
- https://www.parentprojectmd.org/about-duchenne/what-is-duchenne/
- https://www.mda.org/disease/duchenne-muscular-dystrophy
- https://www.mda.org/disease/duchenne-muscular-dystrophy/signs-and-symptoms
- https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/symptoms-causes/syc-20375388
- https://www.parentprojectmd.org/about-duchenne/what-is-duchenne/genetic-causes/
- https://www.genome.gov/Genetic-Disorders/Duchenne-Muscular-Dystrophy
- https://www.mda.org/disease/duchenne-muscular-dystrophy/diagnosis
- https://www.nhs.uk/conditions/muscular-dystrophy/treatment/
- https://www.webmd.com/children/duchenne-muscular-dystrophy
- https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/diagnosis-treatment/drc-20375394
- https://duchenneandyou.com/living-with-duchenne/