What is Guillain Barre Syndrome? An Overview
If you're unfamiliar with Guillain Barre Syndrome (GBS), it's a rare but serious nerve problem. Our…
Recognizing Guillain Barre Syndrome Symptoms: Early Signs
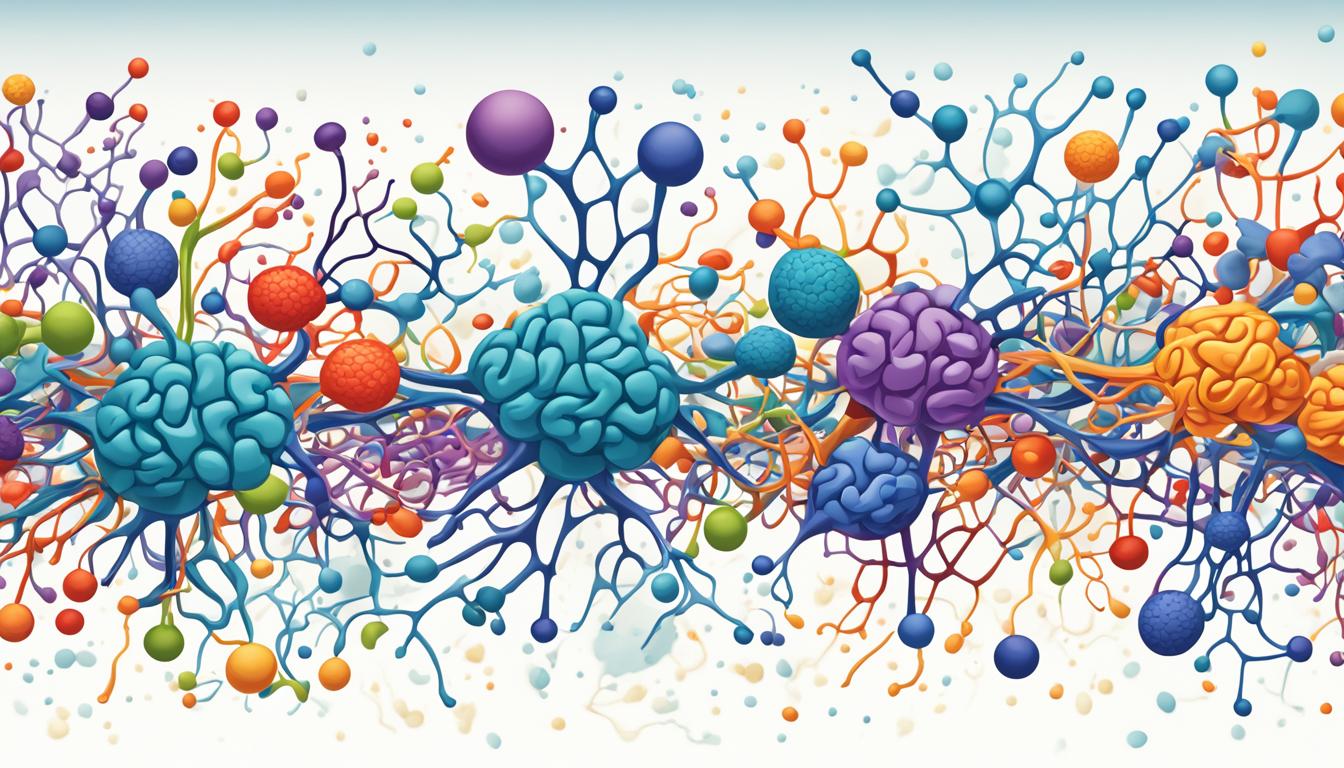
Guillain Barre Syndrome (GBS) is rare. It makes your immune system attack your nerves. This leads…
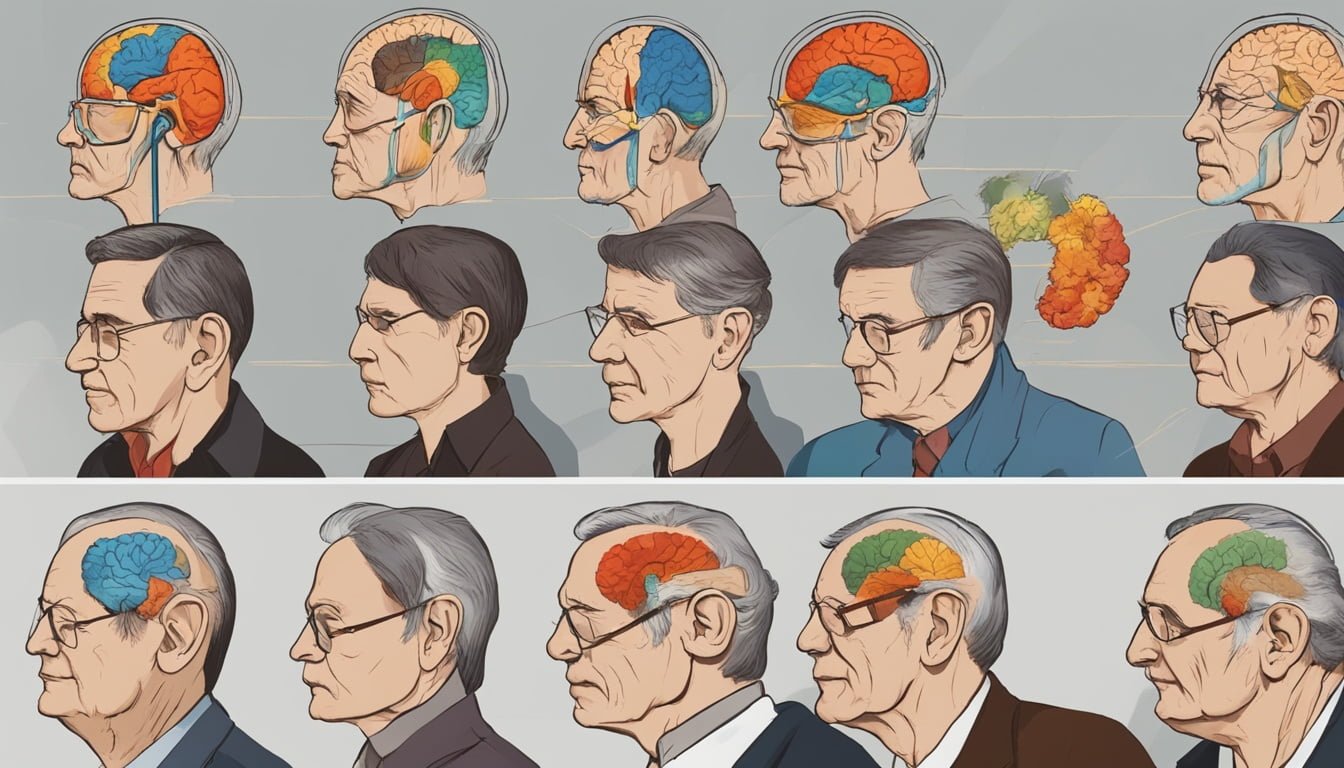
The 7 Stages of Frontotemporal Dementia: A Progression Overview
Frontotemporal dementia (FTD) is a slow and steady brain disorder. It mainly affects how we act,…
What is Frontotemporal Dementia? A Detailed Explanation
Frontotemporal dementia (FTD) is a group of disorders. They happen when nerve cells in the brain's…
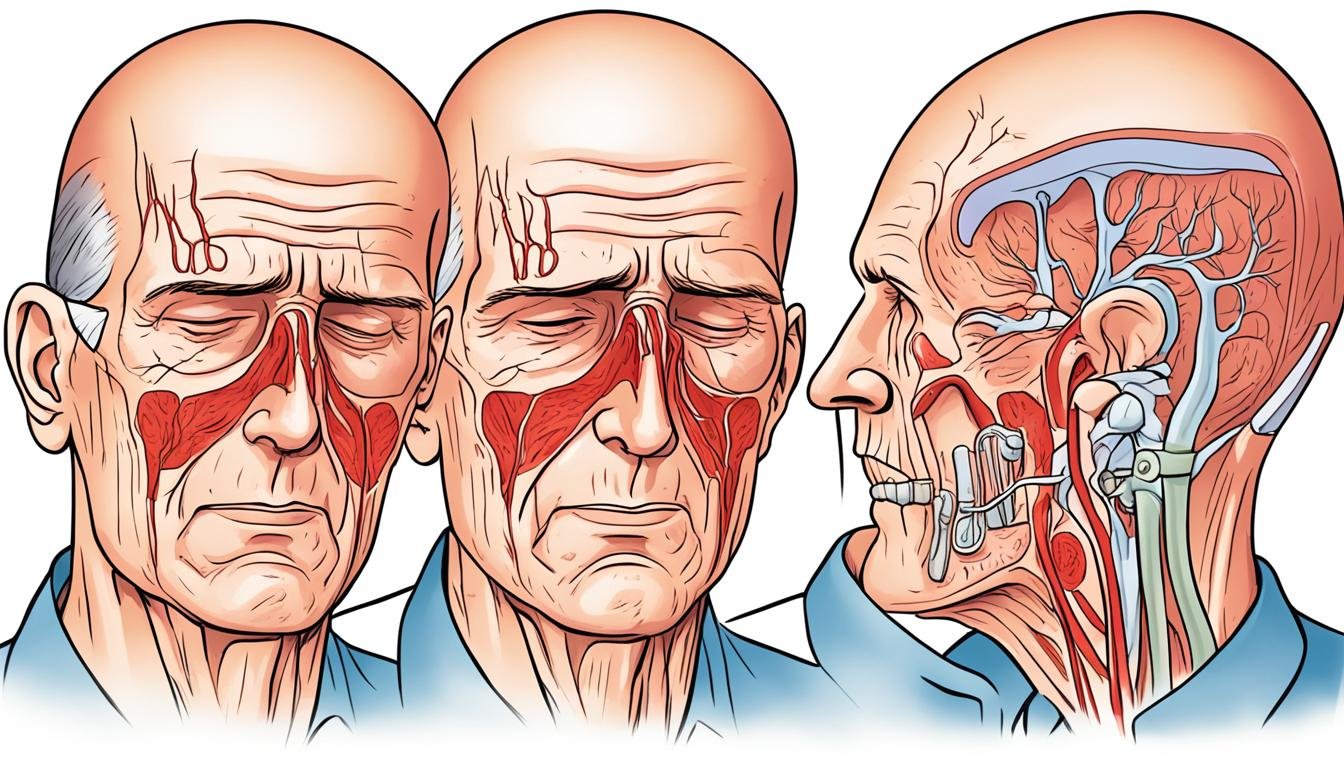
Essential Tremor Symptoms: Recognizing the Signs
Essential Tremor Symptoms: Recognizing the Signs Essential tremor is a type of movement disorder.…
Overview of Gerstmann Straussler Scheinker Syndrome
Gerstmann-Sträussler-Scheinker (GSS) syndrome is very rare. It is an inherited brain disorder. The…
Giant Cell Arteritis Treatment: What to Expect
If you've been diagnosed with giant cell arteritis (GCA), it's normal to feel worried. This type of…
What is Giant Cell Arteritis? An In-Depth Look
Giant cell arteritis (GCA) is the most common vasculitis in adults. It causes inflammation of…
Identifying Epilepsy Symptoms: What You Need to Know
Epilepsy is a disorder that causes seizures. Seizures are bursts of electrical activity in the…
Epilepsy Treatment: Modern Medical Approaches
Epilepsy is a chronic neurological disorder. It is known for causing seizures. These seizures are…