Drugs That Cause Myoclonus: What You Need to Know
Myoclonus is a sudden muscle jerk that happens unexpectedly. It can be because of certain medicines. We will talk about drugs that can trigger myoclonus, how it happens, who is more at risk, how to diagnose and treat it, and what life is like with it.
Myoclonus is a movement disorder where muscles jerk without us wanting them to. This can be in one area, several areas, or all over the body. It happens due to a fast muscle tightening (positive myoclonus) or a quick stop in muscle movement (negative myoclonus).
If you're facing sleep myoclonus, looking for myoclonus treatment, or just want to understand the symptoms of myoclonus, we’ve got you covered. This article has all the info you need about this condition.
Understanding Myoclonus
Myoclonus is a disorder that makes your muscles jerk quickly and without warning. These jerks can happen in just one muscle, a few muscles, or all over your body. They happen because your muscles either suddenly tighten up or relax.
What is Myoclonus?
Myoclonus is when your muscles suddenly contract and relax. These jerks can range from small twitches to big, disruptive movements. It can be caused by many things like brain problems, changes in your body's metabolism, or certain drugs.
Types of Myoclonus
There are different kinds of myoclonus, each with its unique signs and reasons:
- Cortical myoclonus: Comes from the brain’s outer layer and mostly affects the hands and face.
- Subcortical myoclonus: Starts between the brain’s outer layer and the spinal cord. It includes types like brainstem myoclonus and palatal myoclonus.
- Essential myoclonus: Shows as muscle jerks without any other signs.
- Stimulus-sensitive myoclonus: Jerks that get triggered by sudden movements, loud sounds, or bright lights.
- Sleep myoclonus: Muscle jerks while falling asleep or during sleep.
Symptoms of Myoclonus
The main symptom is the sudden muscle jerks or twitches. They can affect just one muscle or many at once. They might happen all of a sudden and can be set off by certain movements or things like light and noise.
Also, people with myoclonus might feel like their muscles are trembling or twitching even when they're not moving.
Drugs That Cause Myoclonus
Antiepileptic Drugs
Some antiepileptic drugs can cause myoclonus. This is a twitching or jerking of a muscle. Examples include:
- Carbamazepine: May cause negative myoclonus with drugs like clobazam.
- Lamotrigine: Can make myoclonus worse or start it in some epilepsy patients.
- Pregabalin: Linked to myoclonus in epilepsy patients taking it as an extra medicine.
Antidepressants
Various antidepressants can lead to myoclonus. This includes:
- Clomipramine and maprotiline, which are tricyclic antidepressants.
- Sertraline, a selective serotonin reuptake inhibitor (SSRI).
- Venlafaxine, a serotonin-norepinephrine reuptake inhibitor (SNRI).
Antipsychotics
Both typical and atypical antipsychotics can cause myoclonus. Some examples are:
- Haloperidol
- Clozapine
- The misuse of Quetiapine
Opioids
Opioid drugs are also linked to myoclonus. This is especially notable with:
- Fentanyl, which can cause it during withdrawal
- Tramadol
- Methadone

Mechanisms Behind Drug-Induced Myoclonus
The reasons why some drugs cause myoclonus are not fully clear. But, we do have some ideas. These include problems with certain brain chemicals like gamma-aminobutyric acid (GABA) and serotonin.
Drugs used to treat epilepsy, for instance valproate, can lead to negative myoclonus. This happens when someone is nearly unconscious from the drug. With tests, doctors found this type of myoclonus does not come from epilepsy itself (Aguglia U et al., 1995).
Plus, drugs for depression like tricyclic antidepressants and SSRIs can also cause myoclonic jerks. Experts think this is because these drugs mess with serotonin levels in the brain (Casas M et al., 1987; Alonso-Navarro H et al., 2006).
Antipsychotic and pain-relief drugs have been blamed for myoclonus too. The reasons are not totally clear. But, scientists think these drugs might harm the brain's dopamine system. Or, they may trigger too much excitement in nerve cells or too much stress on cells (Barak Y et al., 1996; Dib EG et al., 2004; Dominguez C et al., 2009).
Remember that we're still learning about how some drugs spark myoclonus. More studies are needed to figure out the exact ways they do this (Brefel-Courbon C et al., 2006).
Risk Factors for Drug-Induced Myoclonus
Several factors can up the risk of drug-induced myoclonus. This condition makes muscles jerk or twitch without control. Knowing these risks helps doctors spot and handle this side effect of some drugs.
Age
Older folks tend to face higher chances of drug-induced myoclonus. This is often because the body's way of handling drugs changes with age. Also, older people take more meds and have more health issues.
Underlying Medical Conditions
Some health problems can make myoclonus more likely. These include epilepsy, Parkinson's, and issues with the kidneys or liver. Problems with electrolytes can also play a role.
Drug Interactions
Using certain drugs together can increase the risk. For instance, combining antidepressants with lithium, or epilepsy drugs with CNS depressants, can up your chances. The same goes for mixing antibiotics with antipsychotics.

Diagnosis of Drug-Induced Myoclonus
Diagnosing drug-induced myoclonus starts with a detailed medical history. This includes when the muscle jerks started and what they're like. Your current and past medications are also checked, as well as any existing health problems. The doctor will then do a physical exam. They'll look at how the jerks are distributed and what may set them off. They'll also check neurological functions like reflexes, and for other movement issues or damage.
Medical History
Your medical history is key to finding out what's causing the myoclonus. Doctors will ask about when the jerks began and their characteristics. They'll also look into the medications you're taking now or have taken before. This includes checking for any health issues that might be linked to the myoclonus.
Physical Examination
During the exam, the healthcare provider looks at how the muscle jerks are spread around your body. They aim to find what makes them happen. They'll test your reflexes and other neurological functions. This is to see if there are other movement or nerve problems.
Diagnostic Tests
To get a clear diagnosis, more tests might be needed. Some of these could be an EEG, which looks at brain wave patterns. An EMG may also be done to study the muscle activity. And there could be blood tests to check for metabolic or toxic issues.
Managing Drug-Induced Myoclonus
Dealing with drug-induced myoclonus needs a mix of steps. The goal is to lessen muscle jerks and twitches. Start by making sure the medicine dose is right.
Adjusting Medication Dosages
To fight myoclonus, cutting back on the medicine might work. It's done slowly to avoid bad effects after stopping the medicine.
Switching Medications
If lowering the medicine dose doesn't help, your doctor might suggest trying another drug. They could pick a new medicine or a different treatment to cut myoclonus risks.
Treating Underlying Conditions
If an illness causes myoclonus, treating that illness can help. This might mean changing epilepsy or Parkinson's drugs. Or fixing issues like not well-functioning body organs.
Drugs That Cause Myoclonus: What You Need to Know
Various medications have been tied to causing myoclonus as a side effect. The drug groups often involved are:
- Antiepileptic Drugs: Medicines for epilepsy, like carbamazepine, lamotrigine, and pregabalin, can lead to myoclonus. The mix of carbamazepine and clobazam can result in negative myoclonus. Meanwhile, lamotrigine might worsen or trigger myoclonus in those with epilepsy.
- Antidepressants: Myoclonus can be seen with tricyclic antidepressants such as clomipramine, SSRIs like sertraline, and SNRIs including venlafaxine.
- Antipsychotics: Both typical and atypical antipsychotic drugs could cause myoclonus. Haloperidol, clozapine, and quetiapine (if misused) are often linked to myoclonus cases.
- Opioids: Opioid drugs, especially fentanyl during withdrawal, tramadol, and methadone, are known to cause myoclonus.
Many other drugs, such as antibiotics and Parkinson's disease medications, can also induce myoclonus. This shows how broad the list of possible culprits is.
Preventive Measures
To prevent drug-induced myoclonus, healthcare providers should check a patient's medication history and risks. They must watch for myoclonus symptoms when starting or changing drugs. They need to keep a close eye on at-risk patients to catch and treat myoclonus early.
Medication Monitoring
Doctors are key in stopping drug-induced myoclonus. They must go over a patient's meds, looking at any use of specific drugs. This includes antiepileptics, antidepressants, antipsychotics, and opioids which can cause myoclonus. By watching closely, they can spot myoclonic symptoms early, and adjust meds as needed, especially for patients with other health issues.
Lifestyle Modifications
Patients can lower their myoclonus risk too. They should steer clear of triggers like sudden movements or loud sounds, which make muscle jerks worse. It's also good to keep a regular sleep schedule and manage stress, as these factors increase the risk of myoclonus. If they see any unusual muscle movements, it's important to tell their doctor right away.

When to Seek Medical Attention
If you start having sudden, uncontrolled muscle jerks, go see a doctor fast. This is especially true if they are strong, keep happening, or make it hard to do your usual things. If you notice these along with other nerve problems like seizures, shaking, or trouble with balance, it's urgent to get checked.
Also, if the muscle jerks begin when you start a new drug or change how much of one you take, tell your doctor. It might be the medicine causing it. Getting this checked early helps handle the issue better.
Seeing a doctor early for muscle jerks is wise. They can find what's causing it and offer the right treatment. This is key to managing your condition well and avoiding future problems. The doctor will run some tests and then plan how to help you feel better and live well.
Living with Myoclonus
Life with myoclonus brings unique hurdles. Yet, with the right strategies and support, people can cope well. They can enjoy life to the fullest.
Coping Strategies
If you have myoclonus, try these strategies:
- Keep a diary to note when muscle jerks happen.
- Use meditation or deep breathing to reduce stress.
- Avoid things that make your muscle jerks worse.
- Talk to loved ones and doctors for support.
Support Resources
Many support options are out there for myoclonus, such as:
- Joining a support group, either in your area or online.
- Gaining knowledge from groups like the Myoclonus Research Foundation.
- Finding the right doctors and care providers for myoclonus.
By following these strategies and reaching out for support, managing myoclonus gets easier. This can lead to a better life quality.

Conclusion
Myoclonus is a movement disorder marked by sudden muscle jerks or twitches. Some medications, like antiepileptics, antidepressants, antipsychotics, and opioids, can cause it. Knowing how these drugs can induce myoclonus helps both patients and doctors deal with it.
People with myoclonus can improve their lives by working with healthcare providers. They should take preventive actions and regularly check their condition. Adjusting medications and treating other medical problems also helps a lot.
Being proactive and well-informed is crucial in handling drug-induced myoclonus. With proper care, you can manage the condition and reduce its effect on your everyday life.
FAQ
What is myoclonus?
Myoclonus is when your muscles suddenly jerk or twitch without you controlling it. Things like some medicines can lead to this happening.
What are the different types of myoclonus?
There are a few types of myoclonus. This includes myoclonus that happens in the cortex, below the cortex, essential types, those that react to triggers, and also ones that happen while sleeping.
What are the symptoms of myoclonus?
The key sign is sudden muscle jerks or twitches. This may be in one muscle, several muscles, or all over the body.
What medications can cause myoclonus?
Myoclonus might happen because of some drugs. These include medicines for seizures, depression, psychosis, and strong painkillers.
How do medications trigger myoclonus?
We're still learning about how drugs lead to myoclonus. But it could be linked to changes in some parts of the brain or how our body processes energy.
Who is at higher risk of developing drug-induced myoclonus?
Older people, those with health issues affecting the nervous system, and certain people on specific medications are more likely to get myoclonus from drugs.
How is drug-induced myoclonus diagnosed?
Doctors use a few steps to diagnose this. They gather a detailed medical history, check your body, and might do special tests like an EEG or EMG.
How is drug-induced myoclonus managed?
The first step is often to change the drug that's causing it or the dose. Doctors also work on treating any other health problems a person might have.
How can drug-induced myoclonus be prevented?
To prevent this, doctors should always look closely at a patient’s medication history. Patients should try to stay away from things that might trigger their symptoms and keep stress low.
When should someone seek medical attention for myoclonus?
If someone has serious muscle jerks that just won't stop, they should see a doctor. Especially if they also have other strange symptoms.
How can individuals living with myoclonus cope with the condition?
Things like writing down your symptoms, learning to relax, and finding support from others who understand can help a lot.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5533847/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036960/
- https://www.medicalnewstoday.com/articles/myoclonus
- https://pubmed.ncbi.nlm.nih.gov/14728056/
- https://www.mdsabstracts.org/abstract/drug-induced-negative-myoclonus-a-case-report/
- https://www.cambridge.org/core/books/medicationinduced-movement-disorders/myoclonus-and-asterixis/7BA120F282E06F84FEB1F722EA02421D
- https://www.ncbi.nlm.nih.gov/books/NBK537015/
- https://www.mayoclinic.org/diseases-conditions/myoclonus/diagnosis-treatment/drc-20350462
- https://www.mayoclinic.org/diseases-conditions/myoclonus/symptoms-causes/syc-20350459
- https://www.ninds.nih.gov/health-information/disorders/myoclonus
- https://link.springer.com/article/10.1007/s00415-016-8357-z
What is Myoclonus? A Comprehensive Guide
Myoclonus is a unique and puzzling movement issue. It's marked by quick, sudden muscle movements that are hard to control. These muscle jerks can happen in one spot, many areas, or everywhere on the body. This condition stands as a sign of something else going on, like certain health problems, brain issues, or changes in how the body works.
For some, myoclonus is a minor, short-lived problem. But for others, it's a major ongoing issue linked to genes, brain disorders, or even the way the body processes things. It can also be caused by taking certain medicines. Knowing about myoclonus is key for doctors and those affected, as it can truly change how one lives.
Definition and Overview of Myoclonus
Myoclonus is when your muscles move suddenly and without you controlling it. It shows up as quick, short, lightning-like jerks. It's a sign that something might be wrong, not a problem all by itself. This sign can point to many illnesses, and they can affect different parts of the body.
Sudden, Involuntary Muscle Contractions
These jerks happen fast and you can't stop them. They can happen in just one muscle or a bunch of them, even your whole body. Depending on the cause, myoclonus can be a one-time thing or stick around and make life harder. Many things can trigger it, like certain genes, issues with how your brain works, problems with how your body uses energy, and even some medicines.
Diverse Causes and Presentations
Myoclonus doesn’t always point to one clear problem in your brain or nerves. It can happen for many reasons. For example, it might tag along with conditions like multiple sclerosis, epilepsy, Parkinson's, or Alzheimer's. Knowing the broad range of reasons for myoclonus is key for doctors to figure out what's wrong and how to help.
Types and Classification of Myoclonus
Myoclonus can be sorted into different types to help with figuring out the issue and treating it. The main split is between primary myoclonus and secondary myoclonus.
Primary vs. Secondary Myoclonus
Primary myoclonus has a few types: physiologic, essential, and epileptic. Secondary myoclonus happens because of other health issues, like those affecting your nervous system or metabolism. It's key for doctors to know this division to treat myoclonus effectively.
Classification by Body Distribution
Another way to look at myoclonus is where it affects the body. This can range from focal (impacting a single muscle or muscle group) to multifocal or generalized (spreading to many parts or your whole body). Knowing this helps in deciding how to best treat the myoclonus.
Classification by Neurophysiology
Myoclonus can also be split up by the brain and nervous system parts causing it. Types include cortical, subcortical, or spinal. This breakdown helps choose the right treatments because the source of the myoclonus affects what works best.
Physiologic and Essential Myoclonus
Physiologic myoclonus talks about the normal, sudden muscle twitches most people feel. Think of hiccups or sleep jerks. These quick muscle movements are a sign our nervous system is working okay. They usually don't mean there's a health problem.
Physiologic Myoclonus: Hiccups, Sleep Starts
Myoclonic jerks can happen one at a time or in a row. They might be rare or occur often in a minute. Such twitches are pretty common and often don't need any special treatment, unless they start bothering you.
Essential Myoclonus: Isolated and Non-Progressive
Essential myoclonus is more of a stand-alone condition. It's the main symptom for many, sometimes the only one. People might get this with no hints of it in their family history, which means it just happens. But it can also run in families. Usually, it doesn't get worse over time, and it does not affect other parts of the nervous system.
Myoclonus-Dystonia: Hereditary Essential Myoclonus
Myoclonus-dystonia is a type of essential myoclonus that's hereditary. It shows up as repetitive, rhythmic muscle twitches, often in the arms. There might also be dystonia, which twists the body into unusual positions. In some cases, it's linked to a gene called ε-Sarcoglycan (SGCE).
Epileptic Myoclonus and Seizure Disorders
Epileptic myoclonus is a type of seizure disorder. It may involve jerking or twitching movements. These movements can be the entire seizure or just a part of it.
Myoclonus might happen alone or with other seizure types. It can also be a part of a bigger epilepsy syndrome, which includes various seizure forms.
Myoclonus as a Seizure Manifestation
Myoclonic seizures are quite common. They are often seen in juvenile myoclonic epilepsy (JME). JME accounts for 5%-10% of all epilepsy cases.
These seizures are common in generalized or genetic epilepsy. Sometimes, people with focal epilepsy have them, affecting just one side of the body.
Juvenile Myoclonic Epilepsy (JME)
JME seizures typically start soon after waking up. They often begin in adolescence or early adulthood. Sometimes, these seizures can be triggered by tiredness or flashing lights.
Progressive Myoclonic Epilepsy (PME)
Progressive Myoclonic Epilepsies involve myoclonic and tonic-clonic seizures. Unfortunately, these seizures often resist long-term treatment. Myoclonic seizures in Lennox-Gastaut Syndrome affect the neck, shoulders, and upper limbs.
Lennox-Gastaut Syndrome starts in early childhood. It is hard to manage and control.
What is myoclonus: Secondary or Symptomatic Causes
While primary myoclonus can happen on its own, secondary myoclonus comes from other health problems. The causes can vary widely. They include diseases that damage your brain, infections, and issues with your body's chemistry.
Neurodegenerative Diseases
Neurodegenerative diseases affect your brain and nervous system. This includes conditions like Alzheimer's and Parkinson's. They can cause you to have myoclonus, which is when your muscles jerk without control.
Inflammatory and Infectious Conditions
Illnesses that involve swelling or are caused by germs can also lead to myoclonus. This encompasses conditions such as multiple sclerosis and certain viral infections. Rabano-Suarez P et al.'s study noted myoclonus in COVID-19 patients, shedding light on its link with the virus.
Metabolic Derangements and Toxidromes
Problems like kidney failure or certain body chemical imbalances can induce myoclonus. They hamper your body's normal functions, creating the perfect environment for myoclonus to occur. This can lead to uncontrolled muscle jerks.
People or diseases may show more than one type of myoclonus. This overlap makes diagnosis tricky. Doctors must do a full review to pinpoint the root cause and plan the best treatment. This is key for those battling secondary or symptomatic myoclonus.
Pathophysiology and Mechanisms
The specific mechanisms underlying myoclonus aren't fully known. But, we think several things could be involved. This includes too much activity in the motor cortex, issues with how nerve cells communicate, problems with brain chemicals, and network issues in the brain and nerves.
Hard work is being done to understand myoclonus better at the molecular and brain level. This is key for finding new ways to diagnose and treat this complicated condition.
Motor Cortex Hyperexcitability
Myoclonus might happen because the motor cortex is too active. This leads to sudden muscle jerks seen in myoclonus.
Neurotransmitter Imbalances
Imbalances in chemicals that help nerve cells talk, like GABA and serotonin, could cause myoclonus. Changes to these chemicals might affect how nerve cells talk, leading to the jerky movements of myoclonus.
Network Abnormalities
Problems with how parts of the brain work together may also cause myoclonus. When areas like the basal ganglia and cerebellum aren't working right, it can mess up muscle control. Then, you might see the symptoms of myoclonus.
Clinical Evaluation and Diagnosis
Diagnosing myoclonus starts with a detailed and focused approach. It involves a complete history and a thorough physical check-up. Doctors look at your symptoms, past health, and anything that might trigger the muscle jerks. This first step is crucial for finding out what's wrong.
History and Physical Examination
Your doctor will carefully study how your myoclonus acts. They note where it happens, how often, and what might set it off. They also check for any linked health problems. A detailed exam checks the body's nervous system to pinpoint the problem areas.
Electroencephalography (EEG)
An EEG is a key tool to evaluate myoclonus. It measures brain activity, which can show where the jerks are coming from. This helps figure out the root cause and plan the right treatment.
Neuroimaging and Other Tests
Tests like MRIs can spot any brain or spine issues causing the jerks. Tests that measure muscle and nerve activity (EMG and nerve conduction studies) give more info. They help narrow down the problem and confirm the diagnosis.
A team effort is needed to diagnose myoclonus accurately. This team includes doctors, testers, and you, working together. They aim to fully understand your condition and apply the best treatment.
Treatment Approaches for Myoclonus
Myoclonus treatment is based on what's causing it. The first step is usually using medicines. This includes drugs like clonazepam, levetiracetam, valproic acid, and 5-hydroxytryptophan to help with the symptoms.
Pharmacological Treatments
Clonazepam is a common choice to treat the symptoms. But it might make you less coordinated and tired. Other drugs, like levetiracetam, valproic acid, zonisamide, and primidone are also used. They can make symptoms better but might cause side effects like nausea and dizziness.
Botulinum Toxin Injections
For certain types of myoclonus, Botox can be a good option. This is especially true for myoclonus that affects just one part of the body. Botox injections can stop muscle spasms and help you move better. The results, however, may not be the same for everyone.
Deep Brain Stimulation (DBS)
Sometimes, myoclonus is very tough to treat with medicines. In these cases, deep brain stimulation might help. Surgeons place electrodes in the brain to change the way it sends signals. This can reduce myoclonus symptoms.
Doctors often use a mix of treatments to fight myoclonus. This might include medicine, Botox, or even surgery. By using different therapies together, they aim to make life better for those with myoclonus.

Impact on Quality of Life
Myoclonus makes a big difference in how people live. The sudden jerks and twitches can limit what they do physically. They might also feel embarrassed when this happens around others. This can lead to them feeling upset or scared, especially if the spasms are strong or stop them from doing daily tasks like eating or walking. All of this really affects how they feel and live their life.
Doctors need to look at the whole picture with myoclonus. They should work closely with the patients, their families, and other experts to come up with plans that help in every way.
This approach should fix the physical issues, help with daily tasks, and make life better overall. By looking at and treating myoclonus this way, doctors can lessen the hard impact and make life better for those dealing with it.
Myoclonus in Specific Disorders
Myoclonus stands out in some neurological diseases. This makes it vital for doctors to know its many forms. In Creutzfeldt-Jakob disease, myoclonus can appear as "startle myoclonus." This means that sudden muscle jerks happen when something unexpected touches the person.
Creutzfeldt-Jakob Disease and Startle Myoclonus
The "startle myoclonus" is a key sign of Creutzfeldt-Jakob disease. This condition is very serious, caused by damaging proteins in the brain. The muscle jerks happen quickly and affect daily life. It's hard for people with the disease and those who care for them.
Myoclonus in Multiple Sclerosis
People with multiple sclerosis often experience myoclonus too. This is a long-term disease where the body’s own defense mistakenly attacks the nervous system. Specific damage in the brain and spinal cord leads to jerks in the muscles. Knowing why and when this happens can help control the symptoms better.
Other Neurological Conditions
Myoclonus isn't just in Creutzfeldt-Jakob disease and multiple sclerosis. It's also found in other illnesses like Parkinson's and Alzheimer's. These are diseases that damage the nerves. Others, like paraneoplastic syndromes, come from the immune system going after the body. Knowing these signs helps doctors make the right calls and treat patients effectively.
Conclusion
Myoclonus is a diverse movement disorder. It causes sudden, involuntary muscle contractions. These can vary from mild and temporary to severe and ongoing. The reasons can include things like issues with the brain, metabolism, or infections.
Dealing with myoclonus needs a combined effort. This includes checking symptoms, doing tests, and creating custom treatment plans. Health professionals need to be alert to the signs of myoclonus. They should work closely with patients to make care plans that help in many ways.
Myoclonus can really change how a person lives their life. But, research and new findings are helping us understand it better. With the knowledge of the latest updates, doctors and others in healthcare can offer better care. This leads to better results and a better life for those with myoclonus.
In summary, myoclonus is a complex issue that affects people in many ways. Knowing the recent findings in research and care is vital. It helps in offering full and supportive care to people facing this challenging condition.
FAQ
What is myoclonus?
Myoclonus is a movement disorder that makes muscles contract suddenly. These contractions are fast and feel like a surprise. They could happen in one muscle, several, or across the whole body.
What are the different types of myoclonus?
There are two types, primary and secondary. Primary myoclonus is not caused by another health problem. It includes different forms like physiologic and epileptic. Secondary myoclonus is due to other conditions, such as neurological or metabolic issues.
What causes myoclonus?
Many things can lead to myoclonus. It could be genetics, a neurological disorder, or a reaction to medications. The impact might just be temporary, or it could be a long-term struggle.
How is myoclonus diagnosed?
Diagnosing myoclonus starts with a detailed health history and exam. Doctors may do tests like EEG or imaging scans. These help find the root of the problem.
How is myoclonus treated?
Treatment depends on what's causing myoclonus. Doctors often use medicines like benzodiazepines. Sometimes, botulinum toxin or deep brain stimulation is an option.
How can myoclonus impact a person's quality of life?
Myoclonus can make daily life hard if the muscle twitches are frequent or strong. It's important for health teams to help patients cope by considering their emotional and social needs.
Can myoclonus be a feature of other neurological conditions?
Yes, it can be linked to other conditions like Creutzfeldt-Jakob disease. Knowing how it acts in each condition is vital for correct treatment.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8370153/
- https://www.mayoclinic.org/diseases-conditions/myoclonus/symptoms-causes/syc-20350459
- https://www.ninds.nih.gov/health-information/disorders/myoclonus
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036960/
- https://www.bcm.edu/healthcare/specialties/neurology/parkinsons-disease-and-movement-disorders/myoclonus
- https://my.clevelandclinic.org/health/diseases/23172-myoclonic-seizure
- https://www.epilepsy.com/what-is-epilepsy/seizure-types/myoclonic-seizures
- https://www.ncbi.nlm.nih.gov/books/NBK537015/
- https://www.mayoclinic.org/diseases-conditions/myoclonus/diagnosis-treatment/drc-20350462
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3899494/
- https://www.beaconhealthsystem.org/library/diseases-and-conditions/myoclonus?content_id=CON-20155102
What is Hereditary Spastic Paraplegia? An Overview
Hereditary spastic paraplegia (HSP), or familial spastic paraparesis, is a group of inherited disorders. It causes weakness and stiffness in the legs. Symptoms can worsen over time without getting better.
In early stages, walking may become a little difficult. Stiffness is also common. This usually progresses slowly, making aids like canes or wheelchairs necessary. Diagnosing HSP involves a neurological exam and other tests.
HSP comes in different inheritance forms. Not everyone in a family might show symptoms. But they could carry the gene. The time when symptoms start may vary, depending on the gene. Unfortunately, there are no known cures or ways to slow down HSP. But, muscle relaxers and physical therapy can help some.
Understanding Hereditary Spastic Paraplegia
Hereditary spastic paraplegia (HSP) is a rare problem passed down in families. It makes leg muscles weak and tight. Over time, these signs can get worse. It’s also called familial spastic paraparesis or Strümpell-Lorrain syndrome.
Definition and Key Features
Around 90% of folks with HSP show only leg problems. They can have weak legs and muscle tightness (spasticity). The other 10% might have more issues. These could include nerve damage, epilepsy, and trouble with balance.
Types: Pure and Complicated Forms
Pure HSP shows up with weak legs and muscle tightness. You might have trouble controlling your bladder. Sometimes, your feet may not feel things properly. Complicated HSP adds more symptoms. This can mean eye issues, nervous system problems, and more.

Symptoms of Hereditary Spastic Paraplegia
HSP's signs can change a lot, affecting people differently. About 90% face the "pure form." They mainly struggle with weak legs and muscle stiffness and spasms. The "complicated" form, affecting about 10%, brings more symptoms.
Pure HSP Symptoms
Those with pure HSP often start with weaker legs. They also feel stiffer and have a higher muscle tone. They might find it hard to control their bladder or feel their feet. These issues get worse over time.
Complicated HSP Symptoms
Complicated HSP causes more than leg issues. People could also deal with nerve damage, epilepsy, trouble balancing, poor vision, or thinking problems. What they face can change, based on the type of HSP and their life situation.
What Causes Hereditary Spastic Paraplegia?
The main cause of hereditary spastic paraplegia (HSP) is a genetic issue. Most often, people get a bad gene from one parent. If it's a more severe type, they might get bad genes from both parents. These genes affect how the nerves in the spine work. Normally, these nerves help control muscle tone and movement in the legs.
Genetic Mutations and Inheritance Patterns
Scientists have found over 80 places in our genes that can cause HSP. The most seen types usually happen when one of the genes passed down is wrong. The main types are from a parent, like SPG4, SPG3A, and SPG6. Less common types come from both parents, found in SPG5, SPG7, and SPG11. Sometimes, extra genetic changes can show up, causing more symptoms.
For those with pure HSP, getting one bad gene starts it. But for the more complex kinds, inheriting bad genes from both parents is what happens. Knowing which gene is bad and how it's passed helps plan for the disease. It shows what might happen and how best to treat it.

What is hereditary spastic paraplegia
Hereditary spastic paraplegia is found through a detailed clinical check and recognizing its signs. It's crucial to eliminate other conditions first, like multiple sclerosis or cerebral palsy.
Diagnostic Process and Tests
Tests for this condition often include MRI scans on the brain and spine, along with genetic testing. This process specifically aims to confirm if someone has HSP and to find what genetic changes may be the cause.
Ruling Out Other Conditions
Recognizing HSP helps doctors plan for its effects and how to manage it for each person. It also ensures other possible disorders are ruled out, like those causing leg weakness.
Managing Hereditary Spastic Paraplegia
Hereditary spastic paraplegia (HSP) has no cure, but several treatments can help. These treatments aim to make life better for people with this rare condition. They work to lower muscle stiffness, keep muscles strong, and support more independence.
Treatment Options
The use of muscle relaxants can be quite helpful. Medicines like baclofen, tizanidine, and botulinum toxin (Botox) injections target tight muscles. This helps ease stiffness and movements that you can't control.
Physical therapy is another key part of managing HSP. Working with a physical therapist regularly keeps your muscles strong. It also helps you move better, which keeps you doing things on your own.
Physical Therapy and Rehabilitation
Physical therapy for HSP often focuses on leg muscle strength and stretching. This helps prevent muscles from getting too tight. It also includes balance exercises to lower the chance of falling. Occupational therapy is also important. It teaches you how to adjust your home and daily activities so you can be more independent.
If walking is hard, your doctor might suggest using braces or shoe inserts. These help you walk better and stop your muscles and joints from getting worse. For some, surgeries like muscle lengthening might be needed to help with severe stiffness or tightness.
Treating HSP needs a team. This includes doctors, therapists, and sometimes surgeons. They work together to come up with a plan just for you. With this team, living with HSP can be more manageable, and life can get better.
Complications and Outlook
People with HSP might deal with various issues as it gets worse. Their calf muscles can get shorter and tougher. This makes moving harder. They could also get cold feet and feel very tired.
Back and knee pain are common, as are stress and feeling sad.
Potential Complications
How HSP affects someone can differ a lot. Some may need a wheelchair, but others might not. People with hereditary spastic paraplegia usually live as long as others.
However, if the condition is more complex, life expectancy might change. It all depends on the symptoms and how bad they are.
Prognosis and Life Expectancy
Treatment can make a big difference for HSP. It involves physical therapy and other care strategies. By working closely with a health team, people can improve their health.
Regular check-ins with neurologists and physical therapists are key. They help to make a care plan that meets each person's unique needs.
Conclusion
Hereditary spastic paraplegia (HSP) is a rare disorder that affects the legs. It causes them to weaken and stiffen over time. Sadly, there is no cure for HSP yet.
But there's hope. Those with HSP can work with their doctors and therapists. They can create a plan to keep their independence and quality of life.
It's important to know the different types of HSP and their genetic causes. This helps in providing the best care. Researchers are working hard to find new ways to diagnose and treat HSP.
By keeping up with the latest in HSP, you can play an active part in your health. Work closely with your healthcare team. This way, you can live a full life despite HSP.
FAQ
What is hereditary spastic paraplegia?
Hereditary spastic paraplegia (HSP) is a group of inherited disorders. It causes leg weakness and stiffness, which get worse over time.
What causes hereditary spastic paraplegia?
HSP comes from genetic mutations. These mutations affect the nerves in the spine. This leads to muscle tone and movement problems in the lower body.
What are the different types of hereditary spastic paraplegia?
HSP has two main forms. There's the “pure” form with mostly leg issues. And the “complicated” form that has more neurological symptoms.
What are the symptoms of hereditary spastic paraplegia?
In pure HSP, you may see leg weakness, muscle stiffness, and bladder problems. Complicated HSP adds more neurological issues on top of these.
How is hereditary spastic paraplegia diagnosed?
Doctors diagnose HSP by checking for typical symptoms. They also use tests like MRIs and sometimes genetic testing.
How is hereditary spastic paraplegia treated?
There's no cure for HSP, but treatments can help. These include muscle relaxants, therapy, and surgery in severe cases.
What is the prognosis for people with hereditary spastic paraplegia?
The outcome for HSP patients varies. With proper symptom management, some people can live without severe impact on their lives.
What is the role of physical therapy in hereditary spastic paraplegia?
Physical therapy is important for HSP patients. It helps keep muscles strong, improves movement, and maintains flexibility.
Source Links
- https://www.nhs.uk/conditions/hereditary-spastic-paraplegia/
- https://www.ncbi.nlm.nih.gov/books/NBK1509/
- https://www.ninds.nih.gov/health-information/disorders/hereditary-spastic-paraplegia
- https://rarediseases.org/rare-diseases/hereditary-spastic-paraplegia/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6349696/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8835766/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4045499/
Signs and Symptoms of Hemiplegia: What to Look For
If you see signs of hemiplegia in you or someone you love, it's key to know what's going on. Hemiplegia happens when there is damage to the brain or spinal cord. This damage causes one side of the body to be paralyzed. It can lead to weak muscles, trouble controlling them, and stiffness. How bad these hemiplegia signs and symptoms are changes depending on where and how bad the damage is.
Hemiplegia can be congenital or acquired. Congenital hemiplegia is from brain damage before, during, or right after birth until 2 years old. Acquired hemiplegia shows up later due to things like stroke, brain injury, tumor, or infection. It's important to know that hemiplegia is non-progressive. This means its symptoms don't suddenly get worse over time.
Hemiplegia affects either the left or right side of the body. Symptoms range from mild weakness to full paralysis. You might notice weak or stiff muscles, poor ability to move, trouble walking, and balance issues. If the brain damage is bad, there could also be problems with memory, focus, speaking, and behavior. Kids with hemiplegia might hit their walking milestones later, use one hand more, and walk on their toes.
Getting quick help if sudden hemiplegia symptoms show up is crucial. It might be a stroke, which is very serious. Knowing what to look for is the first step to right diagnosis and treatment.
Understanding Hemiplegia
Hemiplegia is when brain damage or a spinal injury causes paralysis on one body side. This makes moving that side very hard. The term hemiplegia is used when one side is completely paralyzed. Hemiparesis is similar but with less severe muscle weakness.
Definition of Hemiplegia
Someone with hemiplegia has severe weakness or paralysis on one side. This happens due to brain or spinal cord damage. It makes everyday activities and moving difficult.
Hemiparesis vs. Hemiplegia
The terms hemiplegia and hemiparesis differ slightly. Hemiplegia means one body side is completely paralyzed. Hemiparesis is when there's only some muscle weakness and less function.
Congenital and Acquired Hemiplegia
Hemiplegia can be born with or develop later. If it's at birth or before age 2, it's congenital. After that, due to things like stroke or brain injury, it's acquired.
Hemiplegia signs and symptoms
Physical Symptoms
Hemiplegia shows up with muscle weakness or stiffness. You might see spasticity, which is a fancy word for tight muscles. This can lead to difficulty walking, balancing, or grabbing things. It really affects how someone moves and lives.
Cognitive and Behavioral Symptoms
When brain damage causes hemiplegia, there can also be issues with thinking and behavior. These might include being forgetful, having a hard time focusing, or trouble speaking. It can even change how someone acts or gets along with others.
Symptoms in Children
Kids with hemiplegia might hit milestones later than other kids. They often use just one hand for activities, or the hand stays in a fist. The symptoms can be mild or severe, depending on the brain injury's location and size.
Causes of Hemiplegia
Hemiplegia can happen for many reasons. Each cause needs a special way to help and care for it. It's key to know the reasons behind it to make a good care plan. Here are some of the usual reasons for hemiplegia.
Stroke
A stroke is a major cause of hemiplegia. It can harm brain tissue and block the messages that control body movement. This damage is often on one side of the body, causing hemiplegia. Strokes during pregnancy or after birth are common in kids who get hemiplegia.
Brain Injury
Hurting the brain suddenly, like in an accident or fall, might result in hemiplegia. If only one side of the brain gets hurt, the opposite side of the body might stop moving. Fast medical help and therapy are key to treat this kind of hemiplegia.
Brain Tumor
Brain tumors, whether cancerous or not, can press on the brain and disrupt its function. This might lead to hemiplegia and other nerve problems. It’s vital to treat the brain tumor to manage hemiplegia that it causes.
Brain Infection
Some infections, especially those attacking the brain, can bring on hemiplegia. For instance, meningitis is a serious infection that affects the brain's protective layers. It can lead to hemiplegia when the brain's one side is damaged.
Genetics
Oddly, genetics play a small role in some hemiplegia cases. Alternating Hemiplegia of Childhood (AHC) is one such condition. It's linked to a gene issue and causes off-and-on bouts of hemiplegia, often in infants and young children.
Types of Hemiplegia
Hemiplegia comes in different types, each with unique signs and causes. Knowing the kinds of hemiplegia helps with finding the right treatment.
Facial Hemiplegia
Facial hemiplegia means one side of the face can't move. It can happen from a facial nerve or brain injury. This is often seen after strokes or head injuries.
Spinal Hemiplegia
Spinal hemiplegia, or Brown-Sequard syndrome, leads to muscle loss on one side and feeling loss on the other. It happens after spinal cord injuries or nerve damage.
Contralateral Hemiplegia
Contralateral hemiplegia causes opposite-side body paralysis. It comes from brain damage affecting the other side. Strokes or brain injuries commonly lead to this type.
Spastic Hemiplegia
Spastic hemiplegia is a kind of cerebral palsy marking one body side with tight muscles. Birth-related brain damage often causes this kind.
Alternating Hemiplegia of Childhood
Alternating hemiplegia of childhood (AHC) is a rare disorder that affects kids. Episodes of one-sided body weakness or both occur. It starts by 18 months and links to ATP1A3 gene issues.
Diagnosis and Testing
Diagnosing hemiplegia starts with a detailed check-up by your doctor. They look at your muscle strength, how well you move and think, and more. This helps figure out what's causing the issue in your brain or spinal cord.
Imaging Tests
Your healthcare provider might also order special imaging tests for hemiplegia like CT scans or MRIs. These tests show if there are problems like tumors or strokes in your brain. Knowing this helps plan the best way to help you move better.
Genetic Testing
If your hemiplegia began when you were very young, genetic testing for hemiplegia might be needed. Some rare genetic issues can lead to one-sided paralysis. Figuring out if it's due to genes can suggest the right treatment approach.
A full picture of your hemiplegia comes after these tests. This includes physical checks, imaging, and sometimes genetic tests. Knowing the exact cause guides your treatment plan, making it more effective for you.
Treatment Options
If you or someone you know has hemiplegia, it's important to have a good treatment plan. This plan should help manage the condition and make life better. Treatment usually combines different therapies and tools, all based on what the person needs.
Physical Therapy
Physical therapy is key for hemiplegia. It helps improve muscle strength, balance, and coordination using targeted exercises and stretches. With a physical therapist's help, people with hemiplegia can move better, walk more easily, and improve their body's overall function.
Occupational Therapy
Learning how to live day to day is the focus of occupational therapy for those with hemiplegia. This includes tasks like getting dressed, taking a bath, and caring for themselves. Therapists make changes in the home too, adding special tools and tips for safety and independence.
Modified Constraint-Induced Movement Therapy (mCIMT)
mCIMT is a special way of helping that involves making someone use their weaker side. They might strap up their normally stronger arm. This method can make the affected side work better, improving things like hand-eye coordination.
Assistive Devices
For some, using tools like braces, canes, or walkers can make things easier and safer. These devices are chosen to fit the person's needs and help them do daily tasks more on their own.
Medications
Sometimes, doctors might suggest medicines to help with certain symptoms of hemiplegia. For issues like muscle stiffness, medication could be part of the treatment plan. Your healthcare team will decide if this is right for you.
How hemiplegia is treated depends on what's causing it and how severe it is. Working with a team of healthcare experts, you can create a tailored plan. This plan should address your physical, thinking, and daily-task challenges from hemiplegia.
Conclusion
Hemiplegia is a long-term issue that has no cure at the moment. Yet, many people with hemiplegia lead full and independent lives with the right care. This care includes a good treatment plan and rehab. The symptoms can get better through things like physical and occupational therapy, plus the use of helpful devices.
Living with hemiplegia, it's key to stay active and make your home safer and easier to move around in. It's also crucial to follow your doctor's advice closely. With support and proper management, you can deal with the challenges of hemiplegia. This way, you can have a happy and fulfilling life.
Even though hemiplegia is a lasting issue, its effects can improve over time with the right care. Working with your healthcare team and staying active is vital. They can help you adapt and enjoy life. With the right attitude and support, you can reach your dreams. They offer hope as methods and tech for assistive care get better.
FAQ
What is hemiplegia?
Hemiplegia happens when there's damage to the brain or spinal cord. This leads to paralysis on one side of the body. It brings weakness and issues in muscle control.
What are the differences between hemiplegia and hemiparesis?
Hemiplegia means a severe loss of muscle strength or full paralysis. Meanwhile, hemiparesis shows a milder loss of muscle strength.
What are the different types of hemiplegia?
There are many types, like facial, spinal, and others. Among them are spastic and alternating hemiplegia of childhood.
What are the common causes of hemiplegia?
The top causes are stroke, brain injuries, tumors, infections, and genetics.
How is hemiplegia diagnosed?
Doctors diagnose it through exams and tests. These include CT scans, MRIs, and, if needed, genetic testing.
What are the treatment options for hemiplegia?
Treatments include physical and occupational therapy. Also, there's modified constraint therapy and sometimes medicines.
Can people with hemiplegia live independent and active lives?
Yes, many can lead full lives with the right plan. While it's a permanent condition, managing it is possible.
Source Links
- https://my.clevelandclinic.org/health/symptoms/23542-hemiplegia
- https://www.medicalnewstoday.com/articles/hemiplegia
- https://www.healthline.com/health/hemiplegia
- https://www.healthline.com/health/hemiparesis-vs-hemiplegia
- https://www.sciencedirect.com/topics/medicine-and-dentistry/hemiplegia
What is Neuropathy? An Overview
Neuropathy is when your nerves are damaged or not working right. It often affects the peripheral nerves. These nerves link the brain and spinal cord to the body. You might feel numbness, weakness, and pain in your hands and feet. Causes range from diabetes to autoimmune disorders and more. Learning about neuropathy helps in its recognition, diagnosis, and treatment.
Understanding Peripheral Neuropathy
Peripheral neuropathy is a problem that affects the nerves outside the brain and spinal cord. These nerves send and receive messages from the brain to the body. It includes nerves that control muscles, feel sensations, and manage body functions automatically. The signs of peripheral neuropathy change based on the kind of nerves involved and the cause of the problem.
Types of Peripheral Nerves
The peripheral nervous system has three main types of nerves:
- Motor nerves: They carry messages from the brain to the muscles. This helps with movement and muscle action.
- Sensory nerves: They send feelings like touch, heat, and pain from the body to the central nervous system.
- Autonomic nerves: They handle involuntary actions in the body, like heart rate, blood pressure, digestion, and sweat production.
Issues with these nerve types can cause the symptoms and problems linked to peripheral neuropathy.
Common Symptoms of Neuropathy
Peripheral neuropathy leads to a wide range of symptoms. These symptoms differ based on the damaged nerves. It's key to know the types of nerve damage and their symptoms. This helps in dealing with the condition effectively.
Sensory Nerve Symptoms
With sensory nerve damage, you may feel numbness or tingling. This often happens in the hands, feet, or other body parts. You might also lose feeling in those areas or feel sharp, jabbing, or burning pain. Some people become extremely sensitive to touch or changes in temperature.
Motor Nerve Symptoms
Motor nerve damage can cause muscle weakness or loss of muscle tone. Lack of coordination and a higher risk of falling are also common. Moving the affected muscles or limbs might become hard.
Autonomic Nerve Symptoms
Damaged autonomic nerves show different symptoms. These include not handling heat well, or sweating too much or too little. Some people experience digestive issues like constipation or diarrhea. They may also feel dizzy due to low blood pressure.
Causes of Peripheral Neuropathy
Peripheral neuropathy has many causes. It can be due to autoimmune diseases or metabolic disorders. Infections, inherited conditions, and even exposure to toxins can also lead to it. It's important to know these causes for the right diagnosis and treatment.
Autoimmune Diseases
Autoimmune diseases make the immune system attack the body. This can cause peripheral neuropathy. Sjogren's syndrome, lupus, and rheumatoid arthritis are some autoimmune diseases. They can lead to neuropathy. So can conditions like Guillain-Barré syndrome and paraneoplastic syndrome, which are related to certain cancers.
Diabetes and Metabolic Syndrome
Diabetes, especially when blood sugar isn't controlled well, is a big cause of peripheral neuropathy. This condition can also be linked to metabolic syndrome. Metabolic syndrome includes high blood sugar, blood pressure, and obesity.
Infections
Infections by certain viruses and bacteria can damage the peripheral nerves. For example, Lyme disease and shingles can lead to neuropathy. So can hepatitis B and C, HIV, and leprosy.
Inherited Disorders
Some people inherit the risk of peripheral neuropathy. Charcot-Marie-Tooth disease runs in families. It's a group of disorders affecting the peripheral nerves.
Tumors and Bone Marrow Disorders
Tumors, both cancerous and non-cancerous, and bone marrow disorders may press on nerves or damage them. Monoclonal gammopathies and amyloidosis, for example, are such conditions.
Other Diseases and Conditions
Certain other diseases can also cause peripheral neuropathy. These include kidney disease, liver disease, and an underactive thyroid (hypothyroidism).
Exposure to Toxins and Medications
Some chemicals and toxins can harm the nerves. This can include industrial chemicals and heavy metals like lead and mercury. Also, some medications, especially some chemotherapy drugs, list neuropathy as a side effect.
Injury or Nerve Compression
Physical injuries from accidents or falls can hurt the nerves. Even activities like sports can be a cause. Nerve compression, which happens in carpal tunnel syndrome, can also bring on neuropathy.
Vitamin Deficiencies
Not getting enough certain vitamins and minerals can hurt your nerves. Deficiencies in B vitamins (like B1, B6, B12), copper, and vitamin E can lead to peripheral neuropathy.
Risk Factors for Neuropathy
Many factors can raise the chances of getting peripheral neuropathy. These include:
- Diabetes, especially with poor blood sugar control
- Alcohol misuse
- Low levels of vitamins, particularly B vitamins
- Infections, such as Lyme disease, shingles, hepatitis, and HIV
- Autoimmune diseases like rheumatoid arthritis and lupus
- Kidney, liver, or thyroid disorders
- Exposure to toxins and chemicals
- Repetitive motions, such as those performed in certain jobs
- Family history of neuropathy
Complications of Peripheral Neuropathy
Without treatment, peripheral neuropathy can cause serious problems. These include skin injuries, burns, and wounds, often on the feet. People may not feel these injuries and end up with infections.
Falls and balance issues are also common. This comes from weaker muscles and loss of feeling. This is especially risky for those with diabetes. It's crucial to manage and prevent peripheral neuropathy.
Diabetic foot ulcers are a major issue with this condition. It happens because high blood sugar harms blood vessels. This cuts off blood supply to the feet, slowing wound healing and raising the risk of gangrene.
Another problem is cardiovascular autonomic neuropathy (CAN). It can make exercise hard and cause low blood pressure. This can lead to dizziness or even faints. Steps to combat low blood pressure include standing up slowly and drinking more fluids. Wearing compression stockings and taking certain drugs like fludrocortisone and midodrine can also help.
Heart arrhythmias and, in the worst case, cardiac arrest can happen due to CAN. Doctors may prescribe medications like flecainide to help manage these heart problems. It's vital for people with CAN to regularly check their heart health. This can help doctors treat any issues quickly and effectively.
Preventing Peripheral Neuropathy
The best way to stop peripheral neuropathy is by handling the health problems that start it. This means keeping your blood sugar level right if you have diabetes. It also means treating autoimmune diseases and infections linked to nerve damage.
Managing Underlying Conditions
If you have diabetes, it’s crucial to keep your blood sugar levels in check. Over half of diabetes patients face some neuropathy. Keeping diabetes under control helps avoid or slow down nerve damage.
Problems like Sjogren's, lupus, and rheumatoid arthritis can also trigger neuropathy. You can reduce the risk by treating these diseases with medications or other treatments.
Some infections, like Lyme disease and HIV, can harm your nerves. If you catch these early and treat them fast, it can help prevent neuropathy.
Adopting Healthy Lifestyle Habits
Stay healthy by eating right and exercising. This helps protect your nerves. And avoid things that can hurt your nerves, like toxic chemicals and too much alcohol.

By managing your health and life choices, you lower the risk of peripheral neuropathy. This also cuts down on its related problems.
What is neuropathy
Neuropathy is a broad term for issues with peripheral nerves, which are outside the brain and spinal cord. It causes symptoms like numbness, tingling, weakness, and pain, especially in the hands and feet. Various things, like diabetes, autoimmune diseases, infections, and even vitamin shortages can trigger neuropathy. So, knowing what neuropathy is helps in spotting, diagnosing, and treating it.
Diagnosis and Evaluation
To diagnose peripheral neuropathy, doctors start with a detailed medical history and a physical exam. They ask about symptoms, medical conditions, things you've been exposed to, and family disease history. This helps find out the possible reasons for the neuropathy.
Medical History and Physical Examination
In the medical history, you'll talk about where, how bad, and how it changes your numbness or pain. Doctors also look into your medical past, lifestyle, anything toxic you've encountered, how much you drink, and if your family has nerve diseases.
Next, the physical exam checks things like your tendon reflexes, how strong your muscles are, and if you feel things as you should. It also looks at your balance and coordination, key in diagnosing neuropathy.
Laboratory Tests
Doctors might order many lab tests to figure out peripheral neuropathy. They check your blood for vitamin shortages, autoimmune problems, and infections. And they look at your liver, kidneys, and thyroid.
Your urine might be tested for Bence-Jones proteins, a sign of multiple myeloma.
Nerve Conduction Studies and Electromyography
Nerve conduction studies and electromyography (EMG) are special tests that doctors might do. These tests show how your peripheral nerves are working. They help find out what's wrong and how bad it is.
Imaging Tests
In some situations, imaging tests like MRIs or CT scans are needed. These look for things like compressed nerves, tumors, or other issues in your body. They're important as they show hidden problems.
Nerve Biopsy and Genetic Testing
Sometimes, for very challenging cases, a nerve biopsy or genetic test is done. This is more for rare or inherited forms of neuropathy. These tests are crucial for finding the exact cause.

Treatment and Management Strategies
The main goal of treating peripheral neuropathy is to deal with its main cause, if we can. Steps may include:
- Keeping blood sugar in check for those with diabetes
- Using drugs or therapies to fight autoimmune issues
- Treating any infections beneath the surface
Medications for Symptom Relief
Besides the root cause, doctors might give medications to ease peripheral neuropathy symptoms. These can include:
- Medicines for pain, like certain antidepressants and anti-seizure drugs
- Creams or ointments for pain in certain spots
Physical and Occupational Therapy
Physical and occupational therapy is key to peripheral neuropathy management. It aims to help patients:
- Better their muscle strength and coordination
- Improve balance and avoid tumbles
- Master skills to handle symptoms and keep doing daily tasks alone
Pain Management
For those with ongoing pain from peripheral neuropathy, docs might suggest pain relief methods. These can be:
- Drugs to ease the pain
- Scrambler therapy, an alternative method. It uses electrical pulses to lower chronic pain levels
Conclusion
Peripheral neuropathy is a serious issue that challenges life quality. It's vital for both doctors and patients to know the causes, symptoms, and how to diagnose and treat it. This knowledge helps in spotting the disease early and dealing with it the right way.
It affects about 2.4% of the world and reaches 8% in the elderly, making it a big health issue. Causes like diabetes, infections, and genetic disorders signal the need for careful check-ups and specific treatments.
Keeping up with the latest neuropathy info is important for healthcare workers and patients. It aids in success in dealing with this complex illness. By working together, they can make real improvements in life quality and reduce the impact of this severe disorder.
FAQ
What is neuropathy?
Neuropathy is nerve damage or dysfunction. It mainly affects the nerves that link the brain and spinal cord to the body parts. You might feel numb, weak, or in pain, especially in your hands and feet.
What is peripheral neuropathy?
Peripheral neuropathy affects the nerves outside the brain and spinal cord. These nerves help you feel and move your body parts by sending messages to and from the brain.
What are the main types of peripheral nerves?
The peripheral nervous system has motor nerves, sensory nerves, and autonomic nerves. Motor nerves help you move your muscles, sensory nerves let you feel touch, and autonomic nerves handle automatic body functions.
What are the common symptoms of neuropathy?
Peripheral neuropathy's symptoms vary but often include numbness, tingling, and pain in the hands and feet. You might also notice weakness, coordination problems, or changes in how you feel hot or cold.
What are some of the causes of peripheral neuropathy?
Many things can cause peripheral neuropathy. This includes diseases, like diabetes, and autoimmune conditions. Infections and physical injuries are also common culprits. Even exposure to certain toxins can play a role.
What are the risk factors for developing neuropathy?
Several things can raise your risk of getting peripheral neuropathy. These include diabetes, alcohol abuse, and low vitamin levels. Infections, autoimmune diseases, and a family history of neuropathy also increase your risk.
What are some of the complications of peripheral neuropathy?
Left untreated, peripheral neuropathy can lead to severe issues. These include injuries or infections due to reduced sensation. Balance problems and falls can also occur, making it crucial to manage the condition.
How can I prevent peripheral neuropathy?
To prevent peripheral neuropathy, handle related health issues like diabetes. Also, live a healthy life. Eat well, exercise, and avoid harm to your nerves. These steps can keep or slow neuropathy from getting worse.
How is peripheral neuropathy diagnosed?
Doctors use various tests to diagnose peripheral neuropathy. These may include checking your medical history, doing physical exams, and running lab tests. They might also use special nerve tests or even look at nerve tissue closely with a biopsy.
How is peripheral neuropathy treated?
There's no cure for peripheral neuropathy, but treatments can help. These include pain medicines, therapies to improve movement, and sometimes alternative methods for pain relief. The aim is to ease symptoms and help you live better.
Source Links
- https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
- https://www.healthdirect.gov.au/neuropathy
- https://my.clevelandclinic.org/health/diseases/14737-peripheral-neuropathy
- https://www.webmd.com/brain/understanding-peripheral-neuropathy-basics
- https://www.houstonmethodist.org/blog/articles/2024/mar/what-are-the-early-warning-signs-of-neuropathy/
- https://www.nhs.uk/conditions/peripheral-neuropathy/causes/
- https://www.foundationforpn.org/types-risk-factors/
- https://www.nhs.uk/conditions/peripheral-neuropathy/complications/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-neuropathy
- https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- https://www.dana-farber.org/health-library/tips-for-managing-neuropathy
- https://www.foundationforpn.org/living-well/lifestyle/managing-peripheral-neuropathy/
- https://www.ncbi.nlm.nih.gov/books/NBK542220/
Neuromyelitis Optica Spectrum Disorder: A Comprehensive Guide
Neuromyelitis optica spectrum disorder (NMOSD) is a rare autoimmune condition. It mainly affects the optic nerves and spinal cord. It was once thought to be a type of multiple sclerosis. Now, it's seen as a unique disease with different features. This guide will cover what we know, the symptoms, treatment, and how to manage NMOSD.
The global cases of neuromyelitis optica spectrum disorders vary. It goes from 0.3 to 4.4 per 100,000. NMOSD affects more females (80%) than males. Most cases show up in people between 30 and 40 years old. Rarely, kids get NMOSD, making up less than 5% of cases. Some insights find that people of African descent with NMOSD might be older. They tend to have more lesions on their MRI scans. They also might have more frequent relapses than other groups.
Understanding Neuromyelitis Optica Spectrum Disorder
Neuromyelitis optica spectrum disorder (NMOSD) is a rare autoimmune condition. It differs from multiple sclerosis (MS). This is because, in the 2000s, scientists found the aquaporin-4 (AQP4) antibody. This discovery showed that NMOSD is its own unique disease.
Definition and Diagnostic Criteria
In 2015, new diagnostic criteria for NMOSD were set. These criteria help doctors know if a person's inflammatory lesions are from NMOSD. They are also important for telling NMOSD apart from other diseases like MS.
Pathophysiology and Aquaporin-4 Antibodies
The cause of NMOSD is due to autoantibodies attacking the AQP4 water channel. This channel is found a lot in the brain and spinal cord. The attacks lead to the inflamed areas characteristic of NMOSD.
Epidemiology and Risk Factors
Neuromyelitis Optica Spectrum Disorder (NMOSD) is a rare autoimmune disease. It affects 0.5-10 people in every 100,000. Such cases vary by region, with more found in some places.
Prevalence and Incidence
More women get NMOSD than men. For every 9 female cases, there's only 1 male case. It usually first appears when people are in their 30s to 50s.
Pediatric cases are not common, making up under 5%. It's essential for doctors to know about this since children may show different symptoms.
Demographic and Clinical Features
Worldwide, NMOSD makes up 1-2% of demyelinating diseases, similar in the US and Italy. Yet, this figure soars to over 30% in Thailand. If someone of African descent gets NMOSD, they might have more recurring issues and a later start of symptoms.
Genetic and Environmental Factors
NMOSD has links to other autoimmune conditions like systemic lupus erythematosus. After certain triggers, such as an infection or a vaccination, the disorder might show up in 20-30% of people.

Clinical Manifestations
Neuromyelitis optica spectrum disorder (NMOSD) shows up as severe episodes. These hit the optic nerves, spinal cord, and brain hard. The results can be devastating, greatly lowering the patient's quality of life.
Optic Neuritis
Optic neuritis is a common sign of NMOSD. It causes loss of vision in one or both eyes. This loss can be very severe and may become permanent. This is more likely in NMOSD than in other similar diseases.
Transverse Myelitis
Transverse myelitis causes sudden and severe weakness and feeling changes in the arms and legs. It's a key feature of NMOSD. This can lead to many problems, from paralysis to issues with bladder and bowel control.
Brain Stem and Diencephalic Manifestations
NMOSD isn't just about the eyes and spinal cord. It can also affect the brain stem and the diencephalon. Brain stem issues can cause constant hiccups, nausea, vomiting, and trouble breathing. Some research also links NMOSD to narcolepsy.
Diagnosis and Differential Diagnosis
Finding out if someone has NMOSD involves looking at their symptoms, test results, and pictures of their body, called imaging. A key test looks for AQP4 antibodies. These help doctors tell NMOSD apart from MS and other illnesses.
MRI Findings
In NMOSD, MRI scans often show long spots in the spinal cord, spanning three or more segments. These spots are usually in the middle of the spinal cord, in the gray matter. The brain's MRI can show lesions near certain brain parts and a special zone in the medulla.
Laboratory Tests
Finding AQP4 antibodies in the blood is a key difference between NMOSD and MS. But, some NMOSD patients are still diagnosed without these antibodies, if their symptoms fit the disease.
Myelin Oligodendrocyte Glycoprotein (MOG) Antibodies
A new finding is another antibody, called MOG, linked to a condition named MOGAD. This finding broadens the disorders related to NMOSD. It stresses the importance of thorough diagnostic and care strategies.

Neuromyelitis Optica Spectrum Disorder Treatment
The approach to treating neuromyelitis optica spectrum disorder (NMOSD) is broad. It aims to handle both immediate and ongoing control. Knowing the available treatments enables doctors to give the best care for this rare autoimmune disease.
Acute Relapse Management
During acute relapses, doctors often use high-dose corticosteroids first. But if they don't work well, other options like plasma exchange or intravenous immunoglobulin might be tried. These help limit the damage and stop further harm.
Disease-Modifying Therapies
For the long term, therapies that change the disease's course are vital. They lower the chance of future attacks and better the patient's outlook. Drugs like Eculizumab, Satralizumab, and Inebilizumab show they can reduce relapses. Rituximab is also effective, though it's not officially approved for NMOSD. Medications that suppress the immune system, such as azathioprine, mycophenolate, and methotrexate, may also form part of the treatment.
Emerging Therapies
Research is rapidly introducing new NMOSD treatments. For instance, scientists are looking into blood markers like GFAP and serum neurofilament light chain. These may help detect and watch for relapses. Also, intravenous immunoglobulins appear to lower neuromyelitis optica's relapse rate.
Dealing with NMOSD fully needs teamwork among health professionals, patients, and their support systems. Knowledge of treatment options and keeping up with new developments are crucial. This way, people with NMOSD get the best, most personalized care.
Prognosis and Monitoring
The outlook for neuromyelitis optica spectrum disorder (NMOSD) varies, but it can be very serious. People with NMOSD are at a high risk of having lasting nerve damage. This can happen if relapses are not treated quickly and well.is essential for spotting and dealing with relapses early. It also helps check if the treatment is working.
New treatments have helped, but NMOSD can come back in more than 90% of cases. Till recently, about half of NMOSD patients needed a wheelchair or became blind within 5 years of getting the disease.
Being careful and keeping an eye on things is key to avoiding serious problems. Your medical team will look at your symptoms, eyesight, movement, and other nerve-related signs often. This is to catch any new signs of the disease fast. Regular MRIs and lab tests are also crucial to understand how the disease is changing. These help doctors choose the best treatments and see how well you're doing.
Staying closely connected with your doctors and following their advice for regular check-ups is very important. This partnership is vital for how well you'll do in the long run. Regular checks and watching out for any new problems can save your nerve health and keep your life quality high.

Neuromyelitis Optica Spectrum Disorder and Quality of Life
Impact on Activities of Daily Living
Neuromyelitis Optica Spectrum Disorder (NMOSD) may heavily affect a person's life quality. It brings physical, emotional, and mental challenges. Vision loss and trouble moving reduce a patient's independence, making them rely more on others.
Emotional and Psychological Well-being
NMOSD can lead to emotional problems like depression and anxiety. Sleep issues are also common. Around 44.3% might feel depressed, while anxiety and sleep problems affect 45% and 55% of patients.
Health-Related Quality of Life Measures
The impact on a patient's health-related quality of life is well-studied. Tests show that NMOSD affects both physical health and mental well-being. Symptoms like pain and fatigue, along with difficulties at work, lower the quality of life for these patients.
Ongoing Research and Future Directions
The NMOSD research field is quickly growing. Scientists are trying to understand the disease more, make better tools for diagnosing it, and create treatments that work better. They're looking at different antibodies, like MOG, to see what role they play in the disease. They're also studying if certain genes or the environment make someone more likely to get NMOSD.
Just how common NMOSD is and where it shows up is another focus. Recent studies shed light on how often it occurs and where, helping doctors better diagnose and treat it.
Scientists are also studying the disease's building blocks. They're looking closely at autoantibodies, especially ones against aquaporin-4 and MOG, to piece together the disease's process. New research, like Teles and team's in 2021, is showing us more about how these antibodies work. This might lead to treatments that target them.
Better ways to diagnose NMOSD are also being sought. Researchers are checking if different lab tests, like looking for specific autoantibodies, can help spot the disease sooner and more accurately.
There's a lot happening in testing and studying therapies, thanks to clinical trials and reviews. These include work by Siritho and colleagues published in 2021. They're testing both new and old treatments for NMOSD. Looking into treatments that act on IL-6 and aquaporin-4 shows promise. Tests on using plasma exchange and stem cell transplants are happening too.
Researchers are not just looking at the disease itself but also at its effects on life quality. They want to see how to give NMOSD patients better care. By meeting all needs of NMOSD patients, health providers hope to make their lives better and their conditions easier to manage.

Neuromyelitis Optica Spectrum Disorder Patient Education
Support Groups and Resources
It's crucial to teach NMOSD patients and caregivers about the disease. This knowledge helps manage the disease better. It also improves their quality of life. Patients need to know about NMOSD - its symptoms, treatments, and where to get support.
The NMOSD Support Group is a great resource. It lets patients and families connect and share their stories. They can get helpful info from meetings and online discussions. This support group offers a way to deal with NMOSD's challenges together.
Also, patients should use top online resources, like the National Institutes of Health (NIH) site. These sites give details about NMOSD, its diagnosis, and treatment. Doctors can show patients these sites. This way, patients can get the info they need to handle their condition well.
Knowing about NMOSD and joining a support group can make a big difference. It helps patients live better with this autoimmune disorder. Healthcare professionals play a key part in linking patients to this support and knowledge.
Conclusion
Neuromyelitis optica spectrum disorder (NMOSD) is a rare condition that's caused by the body attacking its own cells. It needs a detailed, team-based management plan. This involves knowing the disease's characteristics, symptoms, how to diagnose it, and the best treatments.
This article has shown NMOSD can have various symptoms and effects on the body's immune system. It's key to diagnose it early and act fast. Also, having other autoimmune diseases with NMOSD can change how we manage it. That highlights the value of treating the whole patient, not just the NMOSD.
Staying updated through research and educating patients are vital for making things better for those with NMOSD. The field of NMOSD is always learning more, so healthcare professionals need to keep up. This way, they can offer the best treatments based on new evidence to their patients.
FAQ
What is neuromyelitis optica spectrum disorder (NMOSD)?
NMOSD is a rare, autoimmune disease. It mainly affects the optic nerves and the spinal cord. It was once thought to be a type of multiple sclerosis. But now we know it's different, with its own features.
What are the key symptoms of NMOSD?
NMOSD shows up as sudden, serious attacks. These attacks affect the optic nerves, spinal cord, and brain. Some major signs include vision loss in one or both eyes and weakness in the limbs.
How is NMOSD diagnosed?
To diagnose NMOSD, doctors look at various factors. This includes symptoms, results from MRIs, and blood tests for AQP4 antibodies. MRIs might show specific brain and spinal cord lesions.
How is NMOSD treated?
NMOSD treatment is complex, targeting both short-term and long-term needs. During acute attacks, the first treatment is often high-dose steroids. Long-term, there are specific therapies to manage the disease.
What is the prognosis for individuals with NMOSD?
The outlook for NMOSD varies. It can lead to major, lasting effects if not treated quickly. Regular check-ups and appropriate treatments are key to managing the disease.
How does NMOSD impact a patient's quality of life?
NMOSD affects more than just the body. It also touches the mind and emotions. The condition's impact on vision and ability to move can significantly reduce independence.
What are the latest developments in NMOSD research?
NMOSD research is moving fast. Scientists are looking into new antibodies and searching for genetic and environmental causes. The goal is to better understand and treat NMOSD.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6454358/
- https://www.ncbi.nlm.nih.gov/books/NBK572108/
- https://www.sumairafoundation.org/wp-content/uploads/2022/01/MS_NMOSD_Guide_EN.pdf
- https://www.mayoclinic.org/diseases-conditions/neuromyelitis-optica/symptoms-causes/syc-20375652
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7332882/
- https://jnnp.bmj.com/content/89/6/555
- https://www.neurologylive.com/view/differential-diagnosis-and-types-of-nmosd
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5476332/
- https://www.mayoclinic.org/diseases-conditions/neuromyelitis-optica/diagnosis-treatment/drc-20375655
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8395403/
- https://wearesrna.org/living-with-myelitis/disease-information/neuromyelitis-optica-spectrum-disorder/prognosis-management/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9075919/
- https://www.sciencedirect.com/science/article/abs/pii/S2211034822000153
- https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1099376/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10373306/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7998461/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8464318/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4481785/
- https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-014-0162-7
Recognizing the Leukodystrophy Symptoms: What to Look For
Leukodystrophies are rare genetic disorders. They affect the white matter of the brain. The conditions harm the sheath around nerve fibers. This sheath acts as an insulator. It slows down or stops messages from the brain to the body. This leads to issues with movement, talking, vision, hearing, and growth.
Symptoms begin to show during infancy or childhood. They can be tough to spot early on. Look out for signs like a backward step in development. Also, watch for difficulty with movement and seizures. There might also be a decline in how well someone thinks and understands.
As time goes on, symptoms can get more severe. You may see changes in body and muscle tone. Talking might become harder. Vision, hearing, and overall growth could slow down. Recognizing these signs early is important. It can help in getting the right care sooner.
Understanding Leukodystrophy
Leukodystrophy is a collection of genetic disorders. They mainly target the white matter in the central nervous system. The white matter comprises axons, which are like nerve fiber bundles.
These axons have a special cover called myelin. It protects them and helps in sending messages within the brain.
What is Leukodystrophy?
When myelin is damaged or lost, signals in the brain slow or stop. This can cause many neurological issues. These disorders worsen over time and affect the white matter.
Types of Leukodystrophy
There are more than 50 types of leukodystrophies. Each is due to a specific gene problem, impacting myelin growth. Some familiar types are Alexander, Canavan, Krabbe, and metachromatic leukodystrophy.
Every year, we find and name new types, growing our understanding of these diseases.
Common Leukodystrophy Symptoms
Leukodystrophy often shows up as a slow change in how a kid moves and does things. At first, they seem healthy, but then they start having more trouble. This can show in many ways.
They might have problems with how their muscles work, keeping their balance, and moving around. Walking, talking, eating, seeing, and hearing can get harder too. Even their actions and how they behave might change. There can also be issues with learning, going to the bathroom, or breathing.
Each child may show different symptoms. It all depends on what type of leukodystrophy they have and which parts of their brain are affected.

leukodystrophy symptoms
Early Signs and Symptoms
Leukodystrophy's early signs can be hard to spot. Kids seem healthy at first. Yet, symptoms get worse slowly. Signs may include losing skills they've learned, trouble with moving, new seizures, and thinking less clearly.
Progressive Symptoms
Leukodystrophy's effects get stronger as time goes on. This can mean odd muscle or body tone. It might get hard to walk or move normally. Speech problems can also arise. Eating might become a challenge. Vision, hearing, and overall growth can begin to fade.
Diagnosing Leukodystrophy
Diagnosing leukodystrophy requires many steps. Doctors look at medical background and family health history first. Then, they perform physical and nerve tests along with advanced imaging like MRIs. Genetic tests play a big role. This whole process pinpoints the exact type of leukodystrophy. It also helps plan the best care.
Medical and Family History
Doctors begin by checking your or your child's medical past and family info. This detective work often reveals genetic clues or early disease signs. Information about learning progress, nerve symptoms, and issue rates helps with the diagnosis.
Imaging Tests
MRI scans are key in spotting leukodystrophy. They show certain types of brain white matter issues. Other tests, like CT scans, may also be used to look closer at the brain and nerves.
Genetic Testing
Genetic tests are a must for a final leukodystrophy diagnosis, including finding the specific genetic change. Doctors often suggest DNA tests, using full exome sequencing or gene panels. Knowing the genetic roots of the disease is crucial for treatment planning and understanding how the disease might progress.
Diagnosing leukodystrophy is complex, especially early on when signs are faint. Plus, new types are still being found. Your medical team will do their best to reach a clear diagnosis. This is the crucial beginning to finding the right care and treatment for leukodystrophy symptoms, leukodystrophy disease, and leukodystrophy treatment.

Leukodystrophy Treatment Options
There's no current cure for most leukodystrophy types. Yet, a mix of treatments can help. They manage symptoms and try to slow the disorder's progress. The main goal of treatment is to give supportive care. This meets each person's specific needs.
Symptomatic and Supportive Care
Treating leukodystrophy often involves handling symptoms and giving care. Medications are used for issues like seizures or behavior. Therapies such as physical, occupational, and speech are vital. They maintain functional abilities and life quality.
Eating support, educational adjustments, and fun activities are essential. They complete a full care plan.
Bone Marrow Transplantation
For some, like cerebral ALD, a bone marrow transplant might work. It slows the disease, but mainly if done early. Not everyone can get this treatment. It depends on their type of leukodystrophy and when they were diagnosed.
New treatment paths are being researched. This includes enzyme replacement and gene therapy. These methods are being tested in clinical trials. They might offer new hopes of managing these severe disorders in the future.
Living with Leukodystrophy
Living with leukodystrophy, a rare group of genetic disorders, brings complex challenges. These affect the brain’s white matter. To cope, people need medicines, therapies, and special tools.
Managing Symptoms
Leukodystrophy makes daily life harder as it progresses. It can lead to spasticity, seizures, trouble feeding, and moving. Medications can help, as well as physical and speech therapies.
Using devices like wheelchairs and communication aids increases day-to-day independence. They make life easier despite the hardships.
Support and Resources
Families facing leukodystrophy often find it tough. But, help is available. Special care teams, palliative services, and advocacy groups offer support.
These resources provide info, emotional help, and connections to others in similar situations. They aim to improve the lives of those with leukodystrophy.

Ongoing Research and Clinical Trials
Researchers are looking into leukodystrophies to understand them better. They aim to identify more treatment options. The National Institute of Neurological Disorders and Stroke (NINDS) is at the forefront of this effort. It seeks to increase our basic brain and nervous system knowledge. This knowledge helps in lessening the impact of neurological diseases such as leukodystrophy.
NINDS works with other NIH groups on research and clinical trials. These trials look into treatments like bone marrow transplantation, enzyme replacement, and gene therapy. While a cure for most leukodystrophies is yet to be found, ongoing research is focused. It aims to slow down the diseases and make life better for those suffering from leukodystrophy.
Leukodystrophy Prognosis
The outlook for people with leukodystrophy can differ. This depends on the type and how severe it is. Most types get worse over time. But, if caught early and managed well, some may keep a better life for longer.
For a type like cerebral adrenoleukodystrophy, getting help early matters a lot. A bone marrow transplant can slow down the disease heading to the future. Yet, it won't fix the harm already done.
The chance of getting better depends on the leukodystrophy type and when it's found. Treatment options also play a big role.
Seeking Specialized Care
Getting the right care is vital for those with leukodystrophy. The Leukodystrophy Center at Children's Hospital of Philadelphia has top-notch specialists. They work together from many fields to give patients the best treatment and support.
Comprehensive Care Teams
Leukodystrophy centers’ teams are key for managing symptoms, the disease, and treatments. These teams unite various experts to create a care plan just for the patient. This plan meets the patient's needs exactly.
Follow-Up and Monitoring
Keeping track of things regularly is critical in leukodystrophy care. Patients see their team every 6-12 months. This is to check on their health, adjust their care, and offer help.
If the family lives far, the center helps work with the local doctors. This ensures patients still get expert care. This is important to handle such a complex illness well.
Receiving specialized care makes a big difference in living with leukodystrophy. Patients and their families get strong, all-around support. This helps them deal with the difficulties of the disease.
Conclusion
A key first step in dealing with leukodystrophy is recognizing its symptoms. This allows for early intervention and better management. Despite the difficulties in early diagnosis, understanding signs like developmental regression and issues with motor skills is crucial.
As the disease moves forward, these signs can get worse. This impacts how a person can move, talk, see, hear, and think. Sadly, there's no cure for most leukodystrophies yet. But, specialized care can help a lot. It can manage symptoms, slow down the disease, and make life better. Also, ongoing research looks into new treatments, which brings hope.
Learning about leukodystrophy's early detection and comprehensive care is key. This helps those who are affected. It gives them the support they need on their journey.
FAQ
What are the symptoms of leukodystrophy?
Leukodystrophy symptoms include a slow decline in function. This can lead to trouble with muscle tone, balance, and more. Each person's symptoms can be different based on their type of leukodystrophy.
How is leukodystrophy diagnosed?
To diagnose leukodystrophy, doctors look at medical history and do physical exams. They also use imaging tests like MRI. Genetic tests are crucial to pinpoint the specific genetic mutation causing the illness.
What are the treatment options for leukodystrophy?
Treating leukodystrophy is about managing the symptoms and providing support. This includes medications, therapies, and sometimes special equipment. In some cases, early bone marrow or stem cell transplants might be possible.
How can individuals and families cope with living with leukodystrophy?
Families and individuals can cope by getting help from a team of specialists. They should also reach out to support groups and patient advocacy organizations. These steps can make the challenge of leukodystrophy easier to face.
What is the prognosis for individuals with leukodystrophy?
The outlook for leukodystrophy depends on the type and how severe it is. Most types steadily get worse over time. Early and proper symptom management is key to a better quality of life. Unfortunately, there is no known cure for most types.
Source Links
- https://www.chop.edu/conditions-diseases/leukodystrophy
- https://www.ninds.nih.gov/health-information/disorders/leukodystrophy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10410460/
- https://www.webmd.com/brain/leukodystrophy-types
- https://rarediseases.org/rare-diseases/leukodystrophy/
- https://www.mayoclinic.org/diseases-conditions/metachromatic-leukodystrophy/symptoms-causes/syc-20354733
- https://www.aurorahealthcare.org/services/neuroscience/neurology/neurological-conditions/neuromuscular-disorders/leukodystrophy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10770198/
- https://rarediseases.info.nih.gov/diseases/6895/leukodystrophy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10117409/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5964825/
Understand Landau Kleffner Syndrome: Overview and Key Facts
Landau Kleffner syndrome (LKS) is a rare disorder found in children. It causes them to lose their ability to understand and speak language. This happens along with abnormal brain wave patterns during sleep and seizures in many cases.
In 2022, the International League Against Epilepsy said that LKS is a type of developmental/epileptic encephalopathy. It's specifically marked by a certain brain wave activity during sleep. Children with LKS might enter other similar epilepsy syndromes as they grow.
What is Landau Kleffner Syndrome?
Landau Kleffner syndrome (LKS) is very rare. It affects how children learn language. Kids with LKS suddenly or slowly lose their ability to understand and speak.
It usually starts when they are between 3 and 7 years old. But sometimes it happens in kids as young as 18 months. LKS is part of a group of epilepsy disorders in children. It's marked by a specific brain wave pattern and different levels of learning loss.
Rare Childhood Language Disorder
It's a rare issue with the nervous system. Kids with it lose the ability to get and use language. This is called auditory verbal agnosia and aphasia.
Sudden Loss of Language Skills
Kids suddenly or gradually lose their language abilities. This is troubling for the child and their family. The situation can be puzzling and challenging.
Affects Children Between 5-7 Years Old
It mainly affects children between ages 3 and 8. Most cases are in kids 5 to 7 years old. Sometimes younger kids, as little as 18 months old, can also be affected.
Signs and Symptoms
Kids with Landau Kleffner syndrome might find it hard to understand speech at first. They might look like they are deaf or have autism. Later, they might stop talking.
These kids often come up with new ways to communicate. They might use gestures or signs. Also, about 70% of them might have seizures.
Auditory Agnosia
Children with this syndrome might have auditory agnosia. This makes it tough for them to understand what people are saying. They might seem deaf or like they have autism.
Difficulty Understanding Speech
Having trouble understanding speech is common in Landau Kleffner syndrome. The child may not understand what people say. This can be very challenging for them.
Appearing Deaf or Autistic
Kids with this syndrome might look like they're deaf. Or, they might act in ways that remind us of autism. It's because they struggle to understand language.
Loss of Speech Ability
Children with this syndrome may eventually stop speaking. They find new ways to talk without words, like with gestures. Losing the ability to speak is a big change for them.
Seizure Disorder
Many kids with Landau Kleffner syndrome get seizures. These can take different forms, like focal seizures. Sometimes, they might seem to blank out for a bit.
Development of Alternative Communication Methods
As their speech goes away, these children find other ways to share their thoughts. They may use their hands or specific signs. This helps them communicate with others.

Causes of Landau Kleffner Syndrome
The reasons behind Landau Kleffner syndrome (LKS) are still not fully clear. But, experts think it's a mix of genetics and the environment. Several things could lead to this rare disorder in kids.
Possible Genetic Factors (GRIN2A Mutations)
Changes in the GRIN2A gene might cause LKS. This gene helps make a part of the glutamate receptor. This connection shows genes could influence how LKS begins.
Autoimmune or Inflammatory Dysregulation
Some LKS patients get better with immune-suppressing drugs like corticosteroids or IVIG. This finding hints that the immune system or inflammation might be linked to LKS in some kids.
The true causes of LKS are still a mystery. But, scientists are hard at work trying to understand the role of genetics and the immune system. This knowledge is key to finding better, targeted treatments for LKS and helping those living with it.
Diagnosis and Evaluation
Diagnosing Landau Kleffner syndrome (LKS) needs a close look and many tests. The main steps include:
Electroencephalogram (EEG)
EEG is key in spotting LKS. It often shows strong seizure signs, especially during non-REM sleep. These signs are usually clear over the back of the head, near the Sylvian fissure.
Audiometric Examination
A hearing test is done to rule out hearing loss. This is important to tell LKS apart from other conditions that look similar.
Neuropsychiatric Evaluation
Doctors must do a full checkup to understand the syndrome. This includes tests on how the child thinks, acts, and feels. It helps rule out other possible causes for the speech problems.
Speech and Language Assessment
Evaluating the child's speaking and language skills is critical. It shows where they struggle in understanding and talking. This also helps plan how to help them get better.
Brain Imaging (MRI)
An MRI scan looks for brain issues that could be behind LKS. But it's common for the scans of those with LKS to be normal.
Using these tests, plus careful questions and watching the child, doctors can make a correct LKS diagnosis. This rules out other reasons for the speech and brain problems.
Landau Kleffner Syndrome Treatment
The standard treatment for Landau Kleffner syndrome is complex. Doctors rely on antiepileptic medications as the first line of defense. These drugs, like valproate, ethosuximide, and benzodiazepines, are crucial for managing the seizures common in this syndrome.
Antiepileptic Medications
For kids with Landau Kleffner syndrome, treatment often involves antiepileptic drugs. Examples include divalproex, ethosuximide, levitiracetam, and benzodiazepines. They work to control the spike-wave EEG patterns and reduce seizures.
Speech and Language Therapy
Helping kids with Landau Kleffner improve their communication skills is key. Speech and language therapy play a big part in this. These sessions aim to restore the child’s ability to understand and use language.
Sign Language Instruction
Some children with Landau Kleffner may benefit from learning sign language. This can be alongside the traditional therapies. Sign language offers an extra way for kids to express themselves.
Immunotherapy (Corticosteroids, IVIG)
Immunotherapy might also be used, with options like corticosteroids or IVIG. This is for cases where autoimmune or inflammatory issues are suspected. It works by adjusting the immune system. The goal is to boost the child’s language and thinking skills.
Landau Kleffner Syndrome Prognosis
The outlook for Landau Kleffner syndrome (LKS) varies a lot. Some kids recover well in terms of speaking, while others might still have trouble. It's really important to start helping these kids early.
Variable Outcomes
The situation can differ greatly for children with LKS. Some might get much better at speaking as time goes by. But others might find it hard to communicate despite efforts.
This shows why each child needs a customized care plan. Such a plan brings in different experts to help in different ways.
Early Intervention Crucial
Getting the right treatment quickly is key for kids with LKS. This includes using drugs to stop seizures, and speech therapy. For some, trying immunotherapy might also be helpful.
The sooner we help, the better the chances for kids to speak well later. This early support is critical in improving how well they do overall.
Potential for Language Recovery
Even with their challenges, children with LKS can improve their speaking. The right mix of treatments and aid can really help them understand and talk again.
Landau Kleffner Syndrome Epidemiology
Landau Kleffner syndrome (LKS) is very rare, affecting about 1 in a million kids. It seems to happen more often in boys than in girls. But, we don't know why this is the case.
In Japan, a study found LKS occurs in about 1 in a million children. From 1957 to 1980, there were 81 reported cases. But between 1981 and 1991, this number rose to 117. This shows LKS is rare but not unheard of.
There is a pattern in LKS, with boys getting it more than girls. Scientists are still figuring out why this is. They believe more research is needed to understand the Landau Kleffner Syndrome Epidemiology.
Landau Kleffner Syndrome Research
Research on Landau Kleffner syndrome (LKS) is making significant progress. Scientists are looking into both genetic and other causes of this rare childhood condition. They're focusing on the GRIN2A gene mutations and potential autoimmune links.
Ongoing Studies on Genetics and Pathophysiology
GRIN2A gene mutations, related to the NMDA glutamate receptor, are linked to various epileptic conditions, including LKS. Specialists are studying how these genetic issues might disrupt a child's language and cognitive growth.
Some LKS kids have shown improvement with treatments that suppress the immune system. This has led to investigation of autoimmune or inflammatory involvement in the syndrome. The goal is to find better treatments based on these findings.
Clinical Trials for New Treatments
Scientists are also exploring new ways to help LKS kids through clinical trials. They're looking at the benefits of drugs that block calcium channels and a surgery called multiple subpial transection. These aim to help children who don't get better with the usual therapies.
These trials are trying to bring more treatment choices for those with Landau Kleffner syndrome. It's about finding better ways to help, aiming to enhance the lives of those dealing with this disorder.
Differential Diagnosis
Landau Kleffner syndrome might look like other childhood disorders. These include autism spectrum disorders, Rett syndrome, or epilepsy. It's key to look closely at how the disorders show up and do the right tests. This helps tell Landau Kleffner apart from them.
Autism Spectrum Disorders
Autism spectrum disorders (ASD) affect social skills and behaviors. Both ASD and Landau Kleffner can make it hard to talk and understand others. Yet, they have different reasons and signs. Doctors need to carefully check the child's behavior and skills to know which problem they have.
Rett Syndrome
Rett syndrome is rare and mostly hits girls. It causes kids to lose skills, their hands do unusual movements, and they have seizures. Even though it impacts talking, too, Rett syndrome is different from Landau Kleffner. The changes happen in unique ways, and there are special signs like hand movements to help doctors tell them apart.
Epilepsy
Epilepsy covers many disorders that lead to seizures. Landau Kleffner syndrome is a kind that mainly affects talking and understanding. It's important to use tests like EEG and study how the child's language and thinking change. This helps see if it's Landau Kleffner or another epilepsy type.
Support and Resources
Many resources are available for families and individuals living with Landau Kleffner syndrome.
The Landau-Kleffner Syndrome Foundation is one of these. They offer info, help, and a place for a community to form around this rare condition.
Online support groups are also great for sharing stories and finding support. They are a place for those affected by Landau Kleffner to connect and help each other.
Educational Resources
Educational websites and materials can help families and caregivers understand Landau Kleffner syndrome better. They cover the condition, treatments, and tips for helping children learn and grow.

Conclusion
Landau Kleffner syndrome is a rare and complex childhood disorder. It can significantly impact a child's language development and their well-being. The exact causes of Landau Kleffner syndrome are not fully known.
Yet, ongoing research and clinical trials seek to understand and treat it better. With early intervention and the right support, many children can improve their language skills. They can also enhance their quality of life.
By raising awareness and giving comprehensive care, we can support these children and their families. This helps them face the challenges of this rare disorder. It also lets them aim for a better future.
FAQ
What is Landau Kleffner syndrome?
Landau Kleffner syndrome (LKS) is a rare disorder that kids can get. It makes them lose the ability to understand and use words. This problem is part of some types of epilepsy that happen in children.
What are the symptoms of Landau Kleffner syndrome?
Kids with LKS often find it hard to understand speech at first. They may seem like they can't hear or they act like they are autistic. Later, they might not be able to talk themselves and start using other ways to communicate, like by signing. Around 70% of these kids will also have seizures.
What causes Landau Kleffner syndrome?
The exact reasons for LKS are not clear. Experts think it's because of both things in the genes and things in the environment. Changes in a gene called GRIN2A have been tied to some types of epilepsy, including LKS. Sometimes, medicines that weaken the immune system help some kids. This tells us the immune system might attack the body in a way that causes LKS.
How is Landau Kleffner syndrome diagnosed?
Doctors need to look at a lot of things to tell if a child has LKS. They look at brain wave tests (EEG), how well the child can hear (audiometric tests), and how the brain and behavior work (neuropsychiatric tests). They also check how the child speaks and understands speech, and they do brain scans with MRI. All these tests help make sure it's LKS and not something else causing the problem.
How is Landau Kleffner syndrome treated?
Treating LKS uses many methods. Doctors use certain medicines to control seizures. Teaching the child how to talk again is also a big part of treatment. For some, learning sign language can be helpful. If the immune system attacking itself seems to be the cause, special medicines might be used to stop this.
What is the prognosis for Landau Kleffner syndrome?
How well a child with LKS does can be different. Some get much better at talking, and others do not. Starting treatment early is very important for the best chance of getting language skills back. Even though the outcomes are not always the same, many kids can improve a lot over time.
How rare is Landau Kleffner syndrome?
LKS is very rare, affecting about 1 in a million children. It seems to be more common in boys than in girls, but we don’t know why that is yet.
What is the current research on Landau Kleffner syndrome?
Scientists are still looking into what causes LKS. They study genes and how the body's hidden army (immune system) could be involved. There are also tests to find new ways to help kids who don't get better with the usual treatments.
How is Landau Kleffner syndrome differentiated from other conditions?
Sometimes, LKS might get confused with other problems like autism or epilepsy. Doctors must do careful tests to make sure they know what the child might have.
What support resources are available for Landau Kleffner syndrome?
There are many places to turn for help with LKS. Groups like the Landau-Kleffner Syndrome Foundation give info and connect families. Online groups can also be a good support. It's important to learn as much as possible to help take care of someone with LKS.
Source Links
- https://rarediseases.org/rare-diseases/landau-kleffner-syndrome/
- https://www.ncbi.nlm.nih.gov/books/NBK547745/
- https://lluch.org/conditions/landau-kleffner-syndrome
- https://www.verywellhealth.com/landau-kleffner-syndrome-lks-4691954
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7124882/
- https://www.childneurologyfoundation.org/disorder/landau-kleffner-syndrome/
- https://www.childrens.com/specialties-services/conditions/landau-kleffner-syndrome
- https://pubmed.ncbi.nlm.nih.gov/31613525/
- https://www.sciencedirect.com/topics/psychology/landau-kleffner-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC320814/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7445094/
- https://rarediseases.info.nih.gov/diseases/6855/landau-kleffner-syndrome/living
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3162843/
- https://www.sciencedirect.com/science/article/abs/pii/S0165587610004684
- https://aepi.biomedcentral.com/articles/10.1186/s42494-021-00067-9
What are the Causes of Narcolepsy? An In-Depth Look
Narcolepsy is a lifelong challenge. It directly affects how our brains manage when we sleep or are awake. People with often feel tired, even after a full night's sleep. They may also have trouble staying awake during the day. This sickness makes it hard for them to stay alert, even while doing things they love.
The effects of go beyond just feeling sleepy. Sudden muscle weakness, vivid dreams or images during sleep, and even feeling paralyzed as they fall asleep or wake up can happen. This can be quite scary for those experiencing it. Yet, it is important to know that doesn't get worse with time. In fact, some of its symptoms can get better as one grows older. However, the condition itself does not go away entirely. Managing requires lifelong care and attention.
Understanding Narcolepsy: A Chronic Neurological Disorder
Narcolepsy is a long-term issue with the brain's central system. It doesn't create enough of a chemical for nerve communication. This problem can change someone's daily routine a lot. It often causes extreme sleepiness during the day and other tough symptoms.
Excessive Daytime Sleepiness: The Hallmark Symptom
A central sign of narcolepsy is feeling very tired throughout the day. Even if they wake up feeling refreshed, fatigue hits them hard. They might have sudden bouts of sleepiness, known as "sleep attacks." These can happen no matter how much they've slept.
But, during tasks that need focus, like work, their alertness might be normal. This makes handling daily life quite challenging for many with narcolepsy.
Other Symptoms: Cataplexy, Sleep Paralysis, and Hallucinations
Besides feeling very tired, narcolepsy might bring about other tough symptoms. Cataplexy, for example, makes muscles suddenly weak when someone feels strong emotions. Then there's sleep paralysis. It locks you in place, unable to move or talk, either when waking up or falling asleep.
And let’s not forget about the vivid dreams. They can be so clear, they seem real, and sometimes really scary. These occur when moving from being awake to falling asleep.

It's key to know the wide range of symptoms of narcolepsy. This knowledge helps in both recognizing and treating the disorder. With understanding and cooperation, patients and healthcare pros can create a plan that fits their needs.
The Two Major Types of Narcolepsy
Narcolepsy is a complicated condition that affects people in different ways. Understanding the types is key. There are two main types of narcolepsy - Type 1 and Type 2. They come with their own characteristics and effects.
Type 1 Narcolepsy: Cataplexy and Low Hypocretin Levels
Type 1 narcolepsy is also known as narcolepsy with cataplexy. It's marked by low levels of a brain hormone called hypocretin. Or, it shows itself through cataplexy, which is a sudden loss of muscle control. Those with Type 1 often feel very sleepy during the day. They may have very low hypocretin levels. This is a chemical in the brain important for staying awake and REM sleep.
Type 2 Narcolepsy: Excessive Daytime Sleepiness without Cataplexy
Type 2 narcolepsy doesn't include cataplexy. It's mainly just extreme sleepiness during the day. This is different from Type 1, where emotions can trigger muscle weakness. People with Type 2 experience less severe symptoms.
Knowing the difference between Type 1 and Type 2 narcolepsy is crucial. It helps doctors diagnose and treat it properly. Since the causes and effects differ, this understanding is very important. It leads to better, more personalized care for those dealing with narcolepsy.
Autoimmune Disorders and the causes of narcolepsy
The cause of narcolepsy isn't fully known, but research suggests it could be linked to different factors. When someone has cataplexy, it's often because they've lost cells in their brain. These cells make a chemical called hypocretin, which helps keep us awake. It seems an autoimmune disorder, where the body attacks itself, might target these brain cells. This could happen because of a mix of genetics and the environment.
Autoimmune Attack on Hypocretin-Producing Neurons
In some families, you might find clusters of narcolepsy cases. Up to 10% of people with narcolepsy and cataplexy have a family member with alike symptoms. This suggests there's a family link to narcolepsy. It shows a complex mix of genes and things around us might cause the immune system to attack hypocretin-making cells, causing narcolepsy.
The Role of Genetic and Environmental Factors
Studies have pinpointed various genetic and environment factors in narcolepsy causes. For example, a specific form of the HLA gene is in 98% of narcolepsy cases but only in 25% of the general population. Alongside genetics, things like infections seem to play a part. Cases increased during the 2009 H1N1 swine flu pandemic in China, suggesting a link.
The Genetic Link in Narcolepsy
The HLA system of genes helps control our immune system. It affects our risk for narcolepsy. A gene called HLA-DQB1*06:02, part of this family, is crucial. Those with it have a bigger chance of narcolepsy, especially with cataplexy.
This gene variation makes an immune attack on certain brain cells more likely. This can cause these brain cells to die.
The HLA Gene Complex and Immune System Regulation
Many people with narcolepsy have the HLA-DQB1*06:02 variation. And they often share similar versions of related genes.
However, this gene is not rare in the general population. Only a small group gets narcolepsy. This tells us that other factors also play a role.
The Significance of the HLA-DQB1*06:02 Variation
HLA-DQB1*06:02 is key in narcolepsy, especially with cataplexy. Changes in genes like the HLA-DQB1 gene and others are common in those with narcolepsy.
This highlights the significant role the HLA gene complex plays in explaining and treating narcolepsy. This underlines the importance of the HLA gene complex in understanding and treating narcolepsy.

Brain Injuries and Tumors: Rare Causes of Narcolepsy
Narcolepsy is mainly caused by issues with the immune system or by genes. But, it can also be caused by brain injuries or growths. These problems affect how our brain controls when we sleep and dream. This leads to narcolepsy's key signs, like falling asleep a lot during the day.
These brain-related issues are rare. More often, narcolepsy comes from autoimmune diseases or genes. When the brain is hurt, its sleep-wake cycle gets messed up. This causes narcolepsy signs, such as feeling very tired during the day or suddenly losing muscle control.
Understanding these rare brain causes is vital. It's something doctors and patients should know. Even if it's not common, it's important to recognize when such a cause might be there. This knowledge can lead to better care, no matter why someone has narcolepsy.

Narcolepsy: A Multifactorial Disorder
Narcolepsy seems to happen because of both our genes and things around us. It's a blend of genetic traits and environmental causes. The main issue in type 1 narcolepsy is the loss of specific neurons in our brain's hypothalamus.
This loss is linked to an auto-immune response. This auto-immune process starts after being affected by something in the environment. This happens mainly to those with certain genes.
The Interplay of Genetic and Environmental Factors
The ways genes and the environment mix to cause narcolepsy are still a puzzle. This mystery makes it hard to fully understand what leads to narcolepsy. Studies have found some genetic differences that might make some people more likely to get narcolepsy.
The HLA system is important. It helps control our immune system. It has a key role in who might get narcolepsy.
The Complexity of Narcolepsy Causation
The main problem in type 1 narcolepsy is the loss of certain neurons. But what starts this process isn't fully known yet. Odd things like narcolepsy cases increasing after certain diseases, or in certain seasons, show that the environment might trigger it.
Patterns suggest that environmental factors could be crucial in understanding narcolepsy's complex causes.
Demographic Factors and Narcolepsy
Narcolepsy can start in both children and adults. It often begins during childhood, the teenage years, or early adulthood. There are more cases among people aged 15 to 35. This condition affects both genders equally. Still, some studies show it might be a bit more common in males.
The reasons for these patterns are not completely clear. It could be linked to genetics, hormones, or the environment. These factors play a big role in the development of narcolepsy's root causes.
Age of Onset: Peaks in Adolescence and Young Adulthood
Narcolepsy usually kicks in during childhood, the teen years, or early adult life. There are two main times when symptoms peak: at about age 15 and then again at 35. This shows there might be key biological or environmental triggers at these ages.
Gender Differences in Narcolepsy Prevalence
Studies suggest narcolepsy is slightly more common in males than in females. Why this happens is not fully understood. But, it's likely due to a mix of hormones, genetics, and the environment. These factors shape how the disorder occurs and shows in different people.
The Impact of Narcolepsy on Daily Life
Narcolepsy can make life very challenging. It brings on extreme tiredness during the day and surprise sleep attacks. These can mess with your mind and mood, making it hard to focus or be happy. Also, sudden muscle weakness, or cataplexy, can be dangerous, especially when doing things like driving.
Impaired Cognitive and Psychological Function
Feeling very sleepy during the day is a major issue in narcolepsy. It can stop you from being alert when you need to be. This can mess with learning, remembering things, and making good choices. The sleep problems and ups and downs of narcolepsy can even lead to feeling down or anxious.
Increased Risk of Accidents and Injuries
Having narcolepsy means you’re more likely to get hurt or have an accident. Especially if what you're doing needs focus and coordination. Sleepiness or muscle weakness can happen suddenly and be very risky, even life-threatening. But, proper treatment and care can help lower these dangers. This way, you can feel safer and more sure about your day.
FAQ
What is narcolepsy?
Narcolepsy is a long-lasting health issue affecting the brain. It makes it hard for people to control when they sleep and wake up. They might feel like they've just slept, then suddenly get very tired during the day. This can make them fall asleep without meaning to, even while doing something.
What are the symptoms of narcolepsy?
Narcolepsy has a few main signs. These include feeling very sleepy during the day, muscle weakness that comes on suddenly, seeing vivid things that aren't really there, and a period of being unable to move right before sleep or right after waking.
What are the two major types of narcolepsy?
Doctors have split narcolepsy into two main types. Type 1 is when a person feels really sleepy during the day and can also have muscle weakness, especially when feeling strong emotions. It’s often linked to not having enough of a certain brain chemical. Type 2 narcolepsy is similar but doesn’t include the muscle weakness part.
What causes narcolepsy?
We're not entirely sure what causes narcolepsy, but scientists think it's probably a mix of genes and things in the world around us. In some cases, if a person has cataplexy, or muscle weakness tied to narcolepsy, it's because their body attacks brain cells that help them stay awake. This happens because of a problem with their immune system.
How do genetics and the immune system play a role in narcolepsy?
Certain genes can make a person more likely to have narcolepsy, especially the type with muscle weakness. These genes make it easier for the body to mistakenly attack the brain cells that help us stay awake.
Can brain injuries or tumors cause narcolepsy?
In very rare cases, narcolepsy might be caused by injuries to the brain or by certain types of tumors. These can mess up how the brain controls sleeping and waking. As a result, narcolepsy symptoms might develop.
Who is affected by narcolepsy?
Narcolepsy can start in people of any age. But it usually begins when they're young, between the teen years and early adulthood. It affects men and women about the same. But some studies think it might be a bit more common in men.
How does narcolepsy impact daily life?
Narcolepsy can really change how someone lives each day. It can make thinking hard and may cause emotional issues. Feeling super tired during the day and suddenly falling asleep can get in the way of school, work, and spending time with others. People with narcolepsy should be careful when doing things that need focus, like driving, to avoid accidents.
Source Links
- https://www.ninds.nih.gov/health-information/disorders/narcolepsy
- https://www.sleepfoundation.org/narcolepsy
- https://www.nhs.uk/conditions/narcolepsy/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/narcolepsy
- https://my.clevelandclinic.org/health/diseases/12147-narcolepsy
- https://www.healthline.com/health/narcolepsy
- https://www.nature.com/articles/nature.2013.14413
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5773260/
- https://rarediseases.org/rare-diseases/narcolepsy/
- https://medlineplus.gov/genetics/condition/narcolepsy/
- https://www.ncbi.nlm.nih.gov/books/NBK22236/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6325123/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9688775/
- https://www.ncbi.nlm.nih.gov/books/NBK459236/
Understand Muscular Dystrophy Symptoms
Muscular dystrophy is a set of genetic diseases that make your skeletal muscles weaker over time. There are more than 30 types of muscular dystrophy. Each type has its specific symptoms and gets worse at its own pace.
Muscular dystrophy means your muscles get weaker and lose function gradually.
Knowing the symptoms of muscular dystrophy is vital for early detection and right management. Types like Duchenne and Becker are more common. Others are less known, bringing their unique difficulties.
Each kind needs a specific plan for treatment.
Overview of Muscular Dystrophy
Muscular dystrophy is not just one illness but over 30. Each one leads to muscle weakness and other symptoms. They slowly make the muscles weaker, so over time, it's hard for the body to work properly.
Definition and Types
The term 'muscular dystrophy' covers many types. For example, there's Duchenne MD, which is common, and Becker MD, which is less severe. What stands out is how each type starts at different ages and affects various muscles.
Progressive Nature of the Disease
They may all vary, but one thing they share is getting worse over time. This gets in the way of how well someone can do things alone. It changes their life significantly as time goes by.
Common Muscular Dystrophy Symptoms
Progressive muscle weakness is the main sign of muscular dystrophy. Over time, the muscles lose their strength. This makes it hard to do daily tasks and move around.
Progressive Muscle Weakness
The muscles weakening slowly is a key symptom. With muscular dystrophy, muscle fibers break down. They are then replaced by fibrous and fatty tissue. This makes it tough to lift things, climb stairs, or walk.
Muscle Mass Loss
People with muscular dystrophy often lose muscle mass. This is called muscle atrophy. The affected muscles look smaller and thinner. They might even be replaced by fat and connective tissue.
Frequent Falls and Clumsiness
With their muscles getting weaker, balance and coordination suffer. This can lead to falling often and feeling clumsy. Daily tasks become hard and the risk of injury goes up.
Muscular Dystrophy Symptoms in Children
Muscular dystrophy often shows up in early childhood. Kids who have it might be slow to sit, stand, walk, or move like other kids their age. This can be pretty noticeable as they miss milestones.
Delayed Motor Development
Kids with muscular dystrophy might not sit, stand, or walk when expected. They fall behind other kids their age significantly. It’s often the first clear sign that something is wrong.
Difficulty Walking and Running
As the disease keeps getting worse, children find it harder to walk and run. They might fall a lot. You could notice they walk in a funny way or can’t do physical activities like before.
Enlarged Calf Muscles
A big sign of muscular dystrophy can be larger calf muscles. But this doesn’t mean they’re strong. It’s because muscle is replaced with fat, making them look bigger than they should.
Duchenne Muscular Dystrophy Symptoms
Duchenne muscular dystrophy (DMD) is a severe type of muscle condition. It happens mostly in young boys. Signs of DMD start showing early in life, many times before the age of 5.
Early Childhood Onset
DMD shows up early, usually in a child's first years. It mainly affects boys, but girls can carry the gene too.
Waddling Gait
Kids with DMD can start walking in a waddling way. They'll stand with their feet wide apart, find it tough to lift their feet. This happens as the muscles in their hips, thighs, and calves get weaker.
Cognitive and Behavioral Issues
Beyond physical signs, DMD can cause thinking and behavior challenges. About a third of boys with DMD face some learning issues. This can affect how they pay attention, remember, and connect with others.
Becker Muscular Dystrophy Symptoms
Becker muscular dystrophy (BMD) is a form of muscular dystrophy that's less severe than Duchenne. The symptoms show up later in life, often in the teenage years or early adulthood. This is different from Duchenne which starts in early childhood.
Later Onset than Duchenne
Unlike Duchenne, BMD's signs first appear later, sometimes not until the mid-20s or beyond. This makes one of the main differences between the two types of muscular dystrophy. People with BMD might not show symptoms until their teenage years or even into adulthood.
Milder Progression
Becker muscular dystrophy progresses more slowly and is not as severe as Duchenne. Folks with BMD sometimes keep walking for a longer time. They might not face as intense muscle weakness and degeneration as those with Duchenne.
Congenital Muscular Dystrophy Symptoms
Congenital muscular dystrophy is a group of disorders noticeable at birth or by age 2. They affect boys and girls differently. Muscle weakness varies based on the disorder.
Present at Birth or Before Age 2
Unlike some types that show up later, symptoms of congenital muscular dystrophy are clear from the start. This affects a child's development and how they can move.
Restricted Motor Function
Congenital muscular dystrophy limits how muscles work. Kids might have trouble sitting, standing, or walking. This makes everyday tasks and moving around hard for them.

Distal Muscular Dystrophy Symptoms
Distal muscular dystrophy, or distal myopathy, affects specific muscles in the body. These are the muscles far from the shoulders and hips. For example, it targets the muscles in the hands and feet. This makes it different from other forms of the disease. Distal muscular dystrophy has unique symptoms.
Distal Muscle Weakness
One key sign of this illness is weak muscles in the hands and feet. It starts here, affecting activities like holding things and keeping steady. Later, it may hurt the ability to move your hands and walk. This gets worse as the illness moves on.
Difficulty with Fine Motor Skills
Distal muscle weakness really hits fine tasks. Just grabbing things, buttoning a shirt, or using a fork can get tough. And as the illness gets worse, this can make life harder. People may feel less able to do things on their own, affecting how they live.
Muscular Dystrophy Symptoms in Adults
Muscular dystrophy is often linked to childhood. Yet, some types show up in adulthood. Adults with this condition face symptoms that start slowly and change over time. This is different from how it leaps in children.
Gradual Onset
In adults, muscular dystrophy slowly weakens the muscles over time. At first, you might not notice the signs. But as it develops, it becomes harder to do everyday things.
Varying Severity
The effects of muscular dystrophy vary from person to person. Some feel a slight impact, while for others, it's more severe. This depends on the specific gene changes and how quickly it progresses.
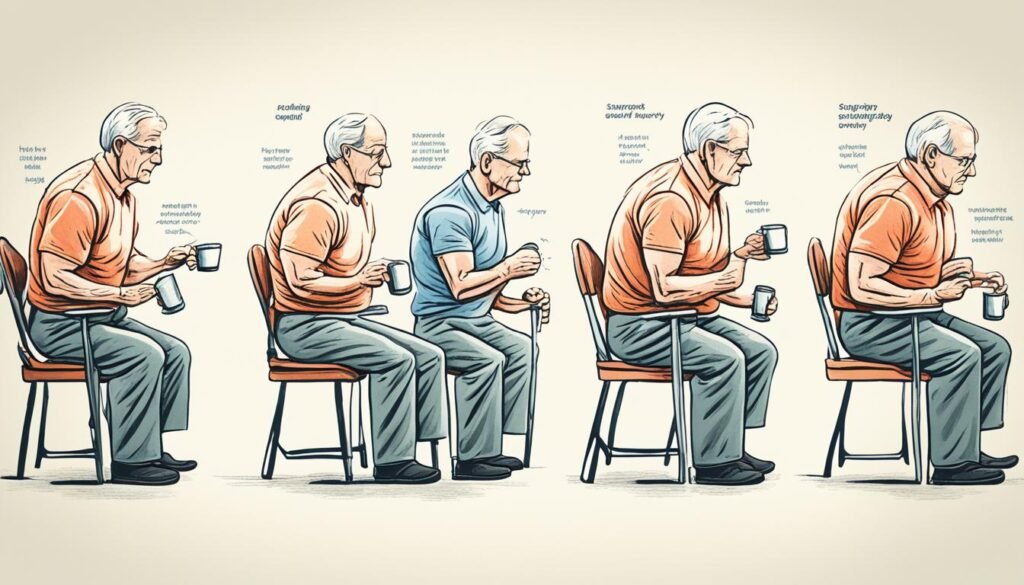
Respiratory and Cardiac Muscular Dystrophy Symptoms
Many types of muscular dystrophy can impact how the heart and lungs work. This can change a person's health and life quality a lot.
Breathing Difficulties
Muscular dystrophy makes the breathing muscles weaker over time. So, those with this disease might find it hard to take deep breaths. They might also feel like they can't catch their breath easily. Plus, they're more prone to getting lung infections.
These problems get worse as time goes on. People might need machines to help them breathe better, like ventilators or BiPAP.
Heart Problems
Duchenne and Becker muscular dystrophies can make the heart muscle weak. This is also called cardiac muscular dystrophy. It can lead to heartbeat issues, weak heart muscles, and even heart failure.
People with muscular dystrophy need to keep a close watch on their heart health. They might need special care to avoid serious heart problems.
Diagnosing Muscular Dystrophy Symptoms
Diagnosing muscular dystrophy involves many steps. It starts with a physical exam and looking at your medical history. Genetic testing and other tests may also be part of the process. This detailed approach helps figure out which type of muscular dystrophy you have. It also guides healthcare providers in making a treatment plan just for you.
Physical Examination
The first thing doctors do is a careful physical exam. They check your muscle strength, reflexes, and how well you move. They'll also look for signs like muscle shrinking or poor muscle tone. These are common in muscular dystrophy.
Genetic Testing
Genetic testing plays a big part in diagnosis. It looks at your DNA to find specific changes or faults. Knowing these details confirms the disease. Plus, it helps in figuring out what type of muscular dystrophy it is. This is crucial for treatment and managing the disease.
Other Diagnostic Tests
Other tests may be used along with the physical exam and genetic testing. For example, you might get a muscle biopsy. This looks at a tiny piece of muscle under a microscope. It shows how your muscle fibers are doing.
- Electromyography (EMG): Records the electrical activity in your muscles. It can show patterns linked with muscular dystrophy.
- Magnetic resonance imaging (MRI): Gives detailed pictures of your muscles. It can find any issues in their structure or how they work.
- Blood tests: These can measure creatine kinase levels. High levels can point to muscle damage from muscular dystrophy.
Putting all these tests together helps diagnose muscular dystrophy accurately. It tells doctors the type you have. Then, they can plan a treatment that considers your specific needs.
Conclusion
Muscular dystrophy is a group of genetic disorders affecting the muscles. It varies in symptoms and progression but always leads to a loss of muscle function. This challenges both children and adults with these conditions.
Diagnosis and treatment are crucial to help those affected. With the help of genetic testing, we now understand more about these diseases. This allows for better care tailored to the individual.
The fight against muscular dystrophy is ongoing. Research and clinical trials look for new treatments and maybe a cure. Through awareness and teamwork, we can make life better for those with muscular dystrophy. We can also offer hope for a future without it.
FAQ
What is muscular dystrophy?
Muscular dystrophy is a group of genetic diseases that weaken and break down muscles over time. There are over 30 types, each with its own signs and progress.
What are the main symptoms of muscular dystrophy?
The key symptom is a steady muscle weakness. People with this condition gradually lose strength and function in their muscles.
When do the symptoms of muscular dystrophy typically appear?
Signs often show in early childhood as kids miss motor skill milestones. This leads to delays in sitting, standing, walking, or other movements.
What is Duchenne muscular dystrophy?
Duchenne muscular dystrophy (DMD) is a common, severe type hitting mostly boys. Kids usually show signs before turning 5.
How does Becker muscular dystrophy differ from Duchenne?
Becker muscular dystrophy (BMD) is similar but less intense than Duchenne. Its signs come later, during teens or early adulthood, unlike Duchenne that starts in childhood.
What is congenital muscular dystrophy?
This type affects babies or toddlers, before they turn 2. Its symptoms and how they progress vary widely, based on the specific type.
What is distal muscular dystrophy?
Distal muscular dystrophy mainly weakens muscles far from the body's core. These include forearms, hands, lower legs, and feet.
Can muscular dystrophy also affect the respiratory and cardiac systems?
Definitely. It’s common for muscular dystrophy to impact both breathing and heart health, in addition to muscle issues.
How is muscular dystrophy diagnosed?
Doctors use physical exams, medical history, genetic tests, and specific diagnostic tests to diagnose this condition.
Source Links
- https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/symptoms-causes/syc-20375388
- https://www.ninds.nih.gov/health-information/disorders/muscular-dystrophy
- https://www.webmd.com/children/what-is-muscular-dystrophy
- https://www.childrens.com/specialties-services/conditions/muscular-dystrophy
- https://www.mda.org/disease/duchenne-muscular-dystrophy/signs-and-symptoms
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/becker-muscular-dystrophy
- https://www.mountsinai.org/health-library/diseases-conditions/becker-muscular-dystrophy
- https://rarediseases.org/rare-diseases/congenital-muscular-dystrophy/
- https://www.musculardystrophyuk.org/conditions/a-z/congenital-muscular-dystrophy/
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/d/distal-muscular-dystrophy.html
- https://medlineplus.gov/musculardystrophy.html
- https://www.ncbi.nlm.nih.gov/books/NBK560582/