What Is Stiff Person Syndrome? A Rare Neurological Condition
Stiff person syndrome (SPS) is a rare, challenging to understand neurological disorder. It leads to muscle stiffness and painful spasms. These can be triggered by sudden noises or light touches. Sometimes, even cold can set them off. SPS is linked with the immune system causing trouble in various autoimmune disorders.
The real cause of SPS remains a mystery. However, experts think it's tied to the immune system mistakenly attacking nerve cells. These cells make GABA, which is a key chemical for muscle control. If not managed well, SPS can really affect how someone does their daily tasks and routines.
What is stiff person syndrome?
Definition and Overview
Stiff person syndrome (SPS) is a rare, acquired neurological disorder. It causes muscle stiffness and frequent painful spasms. SPS can vary in how severe it is and how it progresses. The condition develops slowly over months to years. It was first called "stiff man syndrome" but is now known to affect anyone, regardless of age, race, or gender.
Symptoms of Stiff Person Syndrome
SPS shows up as stiff muscles and sudden, painful spasms. It can start with a dull ache, especially in the lower back, hips, or legs. Over time, the legs and other parts of the body may become very stiff. This makes walking hard and slow.
Muscle spasms are a big part of SPS. They can happen for no reason or be set off by loud noises, light touches, or being in a cold or stressful place. The spasms are not only painful but also make the stiffness worse. In bad cases, SPS can make even simple tasks tough to do each day.
Who Is More Likely to Get Stiff Person Syndrome?
Stiff person syndrome, or SPS, affects twice as many females as males. It's a rare neurological disorder tied to other autoimmune illnesses. These include type-I diabetes, thyroiditis, vitiligo, and pernicious anemia.
While earlier seen as very rare, affecting only about one to two people per million, views have changed. Experts think SPS might belong to a group of disorders, making it potentially more common. But, it's still considered rare.

More cases in women match what's seen with other autoimmune diseases. Scientists are looking into why this gender difference exists. They also seek possible causes and risk factors for developing SPS.
Causes of Stiff Person Syndrome
SPS's exact cause isn't known, but it's likely linked to autoimmune issues. This happens when the body attacks its own healthy cells. In SPS, the immune system goes after nerve cells that make GAD. GAD helps produce GABA, a chemical that regulates muscle movement and nerve reactions.
Autoimmune Response
Those with SPS often have trouble with GAD, a key protein in certain nerve cells. This protein is important for making GABA. A drop in GABA due to immune attacks causes SPS symptoms. We're still figuring out the exact link between GAD and SPS development.
Role of Anti-GAD Antibodies
In SPS, many show very high levels of GAD antibodies compared to usual. While high GAD levels happen in diabetes, SPS levels are even higher. They might also appear in the spinal fluid.
Association with Other Autoimmune Disorders
SPS often goes along with other autoimmune diseases. These can include type 1 diabetes, thyroid issues, and more. The link between SPS and these conditions hints at shared causes.
Paraneoplastic Stiff Person Syndrome
Occasionally, an SPS case is linked to cancer, called paraneoplastic SPS. Breast and lung cancer are often associated. Yet, less common cancers like lymphoma and thymoma can also be linked. The symptoms are much like classic SPS.
Types of Stiff Person Syndrome
Stiff person syndrome (SPS) is a group of neurological disorders. There are different types, each showing unique symptoms. Knowing the types is key to proper diagnosis and treatment.
Classic Stiff Person Syndrome
Classic SPS leads to muscle stiffness and painful spasms. They mainly affect the torso and legs instead of the arms. Symptoms show up slowly, and not everyone will have a curved lower spine at first.
Partial Stiff Person Syndrome
Partial SPS focuses the stiffness and spasms on one part of the body. This might be one leg or the torso. Over time, it can spread to affect both legs and more of the body. This makes walking harder and can lead to falls.
Stiff Person Syndrome Plus
SPS-plus includes classic SPS symptoms along with brainstem and/or cerebellar issues. This leads to double vision, vertigo, and more. As time goes on, walking may become very difficult. These people are also at a high risk of falling.
Progressive Encephalomyelitis with Rigidity and Myoclonus (PERM)
PERM involves muscle stiffness and pain like classic SPS but progresses more quickly. Stiffness can come on in days to a few weeks. Other symptoms might include vertigo or seizures. Many with PERM experience myoclonus.
Overlapping Syndromes
Some syndromes don't neatly fall into the other categories of SPS. They can share symptoms with classic SPS and other conditions. This shows that SPS is a range of disorders, not just one disease.
Diagnosing Stiff Person Syndrome
Diagnosing stiff person syndrome (SPS) is hard. Its symptoms are like those from other problems, such as Parkinson's. To confirm, doctors use a blood test. This test measures glutamic acid decarboxylase (GAD) antibodies levels. High levels show someone likely has SPS.
Blood Tests
A blood test to check for GAD antibodies is crucial for SPS. These antibodies are often found in people with SPS. They help separate SPS from other diseases that seem alike.
Electromyography (EMG)
Electromyography (EMG) checks nerve and muscle function. Before an EMG, pause SPS medications. This brief pause makes SPS signs clearer on the test.
Lumbar Puncture
A lumbar puncture, or spinal tap, is useful to exclude other problems. It also looks for SPS markers in the spinal fluid, like anti-GAD65 antibodies.
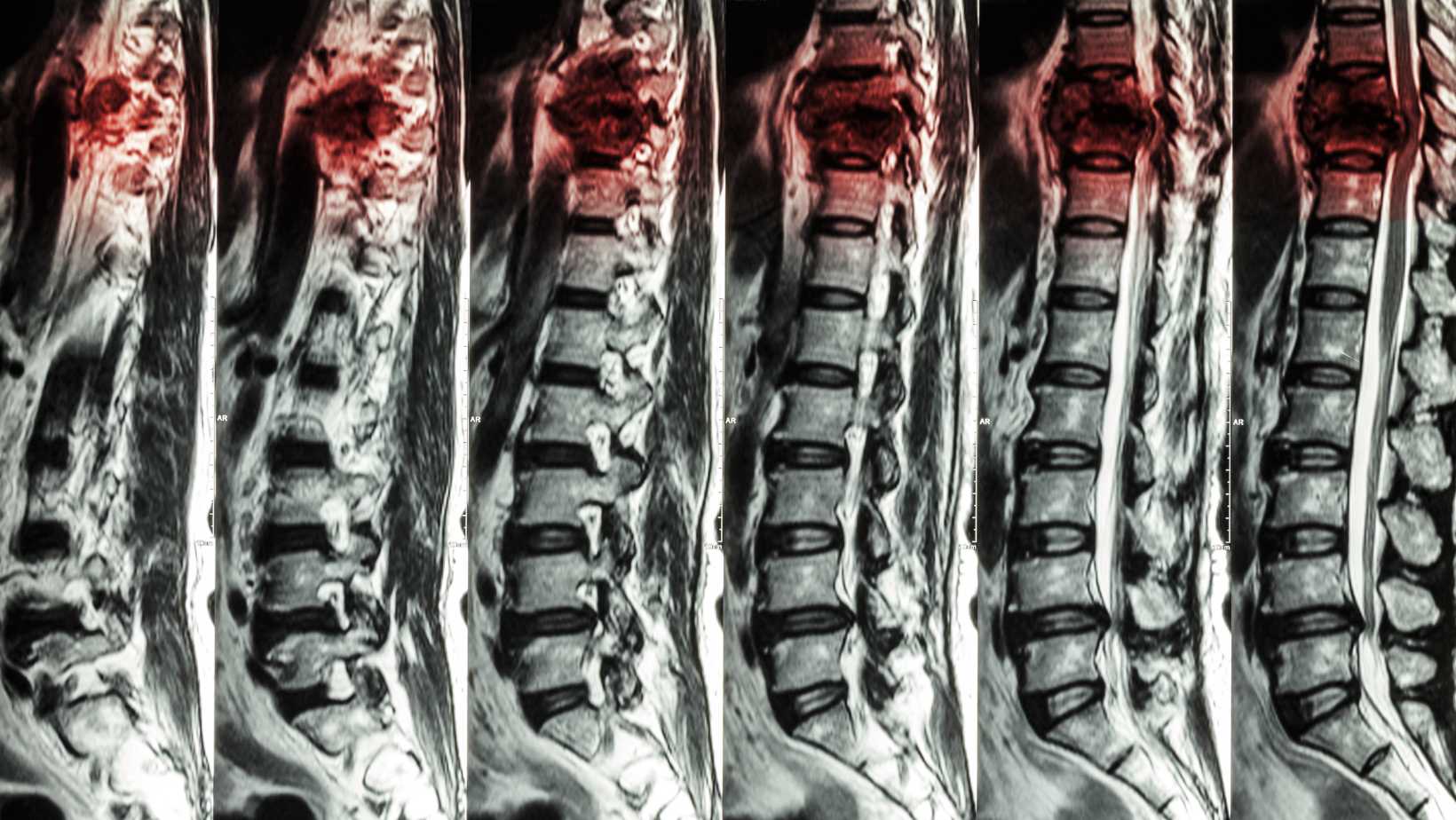
Imaging Studies
Imaging studies like an MRI or FDG-PET with CT scan show body structures. They help rule out other conditions that act like SPS. Sometimes, a mammogram is needed too, especially if cancer is suspected.
Treatment for Stiff Person Syndrome
Stiff person syndrome has no cure. Yet, medicines can help deal with its symptoms. Such as oral muscle relaxers like diazepam and clonazepam. These can ease spasms, stiffness, and pain. Drugs affecting the GABA neurotransmitter, like gabapentin, also play a role. They help lessen the symptoms of this syndrome.
Medications for Symptom Management
For localized muscle spasm, botulinum toxin injections are an option. Antidepressants as well, specifically SSRIs, can be taken. These help manage physical symptoms that anxiety causes.
Immune Therapies
For stiff person syndrome, immune therapies offer another route. They aim to tweak or calm down the immune system, thus addressing its autoimmune side. Options include intravenous or subcutaneous immunoglobulin and plasma exchange. Also, several immunosuppressant therapies like rituximab, mycophenolate mofetil, and azathioprine are used.
Non-Medication Treatments
Aside from drugs, several non-medication methods can also aid in managing the syndrome's symptoms. Physical therapy plays a key role, including deep tissue techniques and stretching. This often involves balance and gait training alongside modalities such as ultrasound and heat. Aquatic therapy, electrostimulation, and stretching exercises are beneficial too. Other options are osteopathic manipulation, qi gong, chiropractic care, massage, and yoga. Cognitive therapies can also help. All these treatments when combined with medication, enhance the quality of life for those with SPS.
Living with Stiff Person Syndrome
Impact on Daily Activities
Stiff person syndrome can make daily tasks hard in serious cases. People may need help like canes or wheelchairs to move. They might worry about sudden muscle spasms and falling, making them afraid to go out. Without treatment, the illness can get worse, making it even harder to move.
Coping Strategies
Though there's no cure, certain strategies can help you live better with SPS. These include physical and heat therapy. Using tools to ease daily work can also be beneficial. Avoiding things that make muscle spasms worse is key. Also, finding others with SPS and leaning on your healthcare team can offer support.

Prognosis and Disease Progression
The severity and progression of stiff person syndrome (SPS) can differ a lot. For some, the issue stays the same over many years. But for others, it can get worse slowly. Medication and treatments can help many manage their symptoms and stay functional.
Yet, if SPS isn't treated well, it could worsen. This might lead to more disability and other health problems because of being less mobile. The outlook for those with SPS changes based on its type, how severe the symptoms are, and how they respond to treatment.
For some, SPS symptoms get worse gradually. But for others, they remain more or less stable. This can affect daily life differently for each person. Some might find it hard to do normal tasks as they get worse.
It's key to see a healthcare provider skilled in treating SPS regularly. A strong treatment plan can help many keep their quality of life. This is despite the difficulties SPS may bring with it, being a rare condition that affects the nervous system.
Research and Clinical Trials
Researchers are working hard to find the causes of stiff person syndrome (SPS) and new treatments. Clinical trials are key in this research. They help us learn more about SPS and test new therapies. If you have SPS, joining a clinical trial could help the research and let you try new treatment options.
The National Institutes of Health (NIH) and other top organizations keep lists of ongoing SPS clinical trials. By keeping up with the latest research and SPS clinical trials, you can find chances to take part. This can lead to better treatments and maybe a better life.
Taking part in clinical trials is not just about helping research. It also lets you use new therapies that aren't available yet. By working with your doctors and keeping up with new research, you can make a big difference in how SPS is treated in the future.
Conclusion
Stiff person syndrome is a rare, complex condition. It causes muscle stiffness and painful spasms. The main cause is likely an autoimmune issue. There might be genetic or environmental factors too. It can change how a person lives day to day. Yet, with the right care, many can lead fulfilling lives.
To diagnose the syndrome, doctors use a mix of exams, tests, and scans. Current treatments help lessen the symptoms. These include certain medicines and therapies. New research is ongoing to find better ways to help those with stiff person syndrome.
If you or someone you know is dealing with this, working with a healthcare team is crucial. They can create a plan tailored to your needs. Joining support groups and using resources can also make a big difference. With care and support, living well with this condition is possible.
FAQ
What is stiff person syndrome?
Stiff person syndrome (SPS) is rare and affects the nerves. It leads to stiff muscles and painful spasms.
What are the first symptoms of stiff person syndrome?
At first, SPS shows up as muscle stiffness that gets worse. It comes with muscle spasms which can be very painful.
People with SPS might feel sore or stiff, mostly in their back, hips, or legs. This could be the early signs.
How is stiff person syndrome treated?
Stiff person syndrome has no cure yet. But there are drugs and therapies to help. These include muscle relaxers, GABA-targeting drugs, and certain immune system treatments.
Therapies like physical and aquatic therapy can also make a difference. They help manage the symptoms of SPS.
What causes stiff person syndrome?
The cause of SPS is not fully understood. It's likely linked to the immune system attacking nerve cells by mistake. This attack focuses on cells that make an enzyme for the neurotransmitter GABA.
Who is more likely to get stiff person syndrome?
Stiff person syndrome affects more women than men. It often occurs with other autoimmune diseases like type-I diabetes and thyroiditis.
What are the different types of stiff person syndrome?
Types of SPS include classic SPS, focal SPS, SPS-plus, and PERM syndrome. There are also similar conditions. These are not clearly part of the main types.
How is stiff person syndrome diagnosed?
It can be tough to diagnose SPS. A blood test checks for specific antibodies against GAD. EMG, spinal taps, and imaging tests might also be needed. They help to check the nerve and muscle health.
How does stiff person syndrome affect daily life?
Sometimes, SPS can make daily life hard. People may need canes, walkers, or wheelchairs. They might also feel scared about muscle spasms and falling.
This fear can make them anxious and not want to leave home.
What is the prognosis for stiff person syndrome?
The effects of SPS vary from person to person. With proper care, many can keep their symptoms under control. But if not treated well, it might get worse, affecting life more.
Are there any clinical trials or research for stiff person syndrome?
Research on SPS and its treatments is ongoing. Clinical trials are key in this research. They look at new therapies' success and safety.
If you have SPS, joining a clinical trial can support research and offer new treatment chances.
Where can I find support and resources for stiff person syndrome?
Many groups, like the Genetic and Rare Diseases (GARD) Information Center, offer help. They share info, connect patients, and discuss treatments and trials.
Source Links
- https://www.ninds.nih.gov/health-information/disorders/stiff-person-syndrome
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/stiff-person-syndrome-sps
- https://my.clevelandclinic.org/health/diseases/6076-stiff-person-syndrome
- https://www.ncbi.nlm.nih.gov/books/NBK573078/
- https://www.healthline.com/health-news/celine-dion-stiff-person-syndrome-details
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7793517/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4461724/
- https://emedicine.medscape.com/article/1172135-overview
Understanding Compression of the Spinal Cord: Key Facts
Facing compression of the spinal cord can feel overwhelming. But learning the main points helps manage this condition well. Your spinal cord is a group of nerves moving messages between your brain and body. Spinal cord compression can happen from the neck to the lower back. It's due to any issue pressing on this critical part of your body.
The signs of spinal cord compression differ a lot. You might feel numb, in pain, weak, or lose control of your bowels and bladder. How quickly these symptoms show up depends on what's causing them. In tough cases, myelopathy might develop. This makes walking hard and causes pain and numbness.
If you face spinal cord compression, whether it hits you fast or slows, team up with your doctors. This step is crucial for the best result. Treatment can involve drugs, physical therapy, or surgery. It all depends on how bad it is and its cause. Knowing about symptoms of spinal cord compression and what to do helps you lead in your health. This can make a big difference in your life quality.
What is Compression of the Spinal Cord?
Spinal cord compression can happen from the neck down to the lower back. Various factors can press on the spinal cord. This disrupts its function and can lead to severe symptoms.
Causes of Spinal Cord Compression
Osteoarthritis, spinal injuries, and tumors are some causes. Also, some bone diseases and spine wear and tear over time. Osteoarthritis usually affects those over 50. It causes the spine to gradually deteriorate.
Symptoms of Spinal Cord Compression
Symptoms can start fast or slowly depending on the cause. Immediate symptoms happen from spine injuries. But, gradual spine wear and tear take years to show effects. Besides pain, symptoms include numbness and coordination issues.
Acute vs. Chronic Compression
Acute compression comes suddenly, often from an injury. It needs quick medical help. Chronic compression, like osteoarthritis, develops slowly. It can be managed with several treatments. Lower back nerve pressure might lead to cauda equina syndrome. This syndrome causes severe symptoms like leg weakness and bladder control loss.

Spinal Anatomy and Function
The spinal cord is like a main road for signals between your brain and body. It's protected by the vertebral column, which is made of 24 vertebrae, or bones. Each vertebra forms a center hole. This creates a tube that shields the spinal cord. The spine has an "S" shape to evenly hold weight and handle stress.
The Vertebral Column
The vertebral column has five parts: cervical, thoracic, lumbar, sacrum, and coccyx. The cervical spine has 7 vertebrae, the thoracic spine has 12, and the lumbar spine usually has 5. However, some people might have an extra lumbar vertebra without problems. The sacrum joins the spine to the pelvis.
The Spinal Cord
The spinal cord starts at the brain's base and goes to just below the second lumbar vertebra. It contains nerve bundles that let your brain and body talk. This is crucial for moving, feeling, and many other body functions.
Nerve Roots and Cauda Equina
Nerve roots come from the spinal cord and pass through small openings in the vertebrae. They then connect the spinal cord to the body. The cauda equina is a bunch of nerve roots below the spinal cord. It's key to know about these for understanding compression and its effects.
Common Causes of Spinal Cord Compression
Spinal cord compression is often caused by the normal wear and tear on the spine. This happens as people age. It includes diseases like osteoarthritis and degenerative disc disease. These affect older adults.
Other causes can be spinal injuries, trauma, and tumors. Spinal tumors can be cancerous or not. They can happen quickly and affect people at any age.
Osteoarthritis and Degenerative Disc Disease
This type of compression mainly affects those over 50. As the spinal discs wear down, they may press on the spinal cord. This causes pain, numbness, and weakness.
Spinal Injuries and Trauma
Accidents or falls can injure the spine and instantly compress the spinal cord. This situation needs urgent medical care. It can happen to anyone and cause sudden severe issues.
Spinal Tumors
Spinal tumors, whether cancerous or not, can compress the spinal cord. This leads to a variety of symptoms. For example, lung cancer and prostate cancer can cause MSCC in a small percentage of cancer patients.
Other Causes
Spinal cord compression can also come from bone diseases and infections like epidural abscess. These less common problems may show up quickly and affect people of any age.
Symptoms of Compression of the Spinal Cord
Symptoms of spinal cord compression vary with its cause and location on the spine. Despite these differences, there are common signs to watch out for.
Back and Neck Pain
Back and neck pain are common in spinal cord compression cases. You might feel sharp, dull, or burning pain. It can spread to the arms, buttocks, or legs. This pain often gets worse when moving or active.
Numbness and Weakness
Spinal cord compression can cause numbness, tingling, or weakness in your extremities. The reason is the pressure on nerve signals in your spinal cord. Feeling loss and coordination problems, including foot drop, are also classic signs.
Bowel and Bladder Dysfunction
In severe cases, like when it affects the lumbar spine, you might lose control over your bowels or bladder. This is a serious sign needing immediate medical help. It could be a cauda equina syndrome episode.
The speed and severity of these symptoms can greatly differ. Some symptoms might take years to show, while others can appear suddenly. If you notice these signs, seek medical attention promptly to avoid possible damage.
Diagnosing Spinal Cord Compression
If you have symptoms of spinal cord compression, your doctor will work hard to find the cause. They will start by talking with you and then examine you. This includes testing your nerves and muscle strength.
Physical Examination
In the exam, your provider will check your body's nervous system. They'll look for signs like numbness and changes in reflexes. They might test your ability to move, your muscle strength, and how you feel touch or vibration.
Imaging Tests
Next, your provider might ask for tests to see inside your body. These tests can show the spinal cord and areas near it. They include x-rays, CT scans, and MRI scans.
- X-rays, which can show abnormal bone growths or alignment issues
- CT (computed tomography) scans, which provide more detailed views of the spinal cord and vertebrae
- MRI (magnetic resonance imaging) scans, which produce high-resolution images that can reveal soft tissue damage or compression
Additional Tests
If necessary, your provider might order more tests to understand the problem better. This could include a myelogram, bone scan, or an electromyography (EMG). Each test gives different information about the spine.
- Myelogram: A dye is injected into the spinal canal, allowing for X-ray or CT imaging to identify areas of compression
- Bone scan: Detects changes in bone metabolism that could indicate underlying conditions affecting the spine
- Electromyography (EMG): Measures the electrical activity in muscles, which can help identify nerve damage or compression
All this information helps your healthcare team figure out what's causing your spinal cord compression. With a clear diagnosis, they can then choose the best treatment for you.
Treatment Options for Spinal Cord Compression
Dealing with spinal cord compression requires special care. Treatments are chosen based on what's causing it and how bad your symptoms are. Doctors might suggest different options for you:
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) help with pain and swelling. Your doctor might also give you high-dose steroids to quickly lower inflammation and pressure on your spinal cord. If the compression is due to tumors, radiation therapy could be used to reduce their size and ease pressure.
Physical Therapy
Physical therapy is key in handling spinal cord compression. A therapist will lead you in exercises. These will make the muscles around your spine stronger, boost flexibility, and help with movement. You'll also learn how to do daily tasks in a spine-safe way and keep a good posture.
Surgical Interventions
If the compression is critical or urgent, surgery might be the best step. This can involve several procedures like removing bone spurs, making space between vertebrae, or stabilizing the spine. It’s often the last option after trying other treatments first.
Your spinal cord compression treatment will be customized to your condition’s cause, where it is, and how severe it is. Your medical team will help figure out the best plan to ease your symptoms and keep your spinal cord healthy.

Preventing Spinal Cord Compression
Spinal cord compression can be hard to prevent, but there are ways to avoid its symptoms. To protect your spine from daily stress, keep a healthy weight. Also, mind your posture, lift carefully, and exercise to make your back muscles strong. Doing these things lowers your chance of having spinal cord problems.
Maintaining a Healthy Weight
Extra weight strains your spine and might lead to spinal cord compression. A good diet and regular exercise can reduce this risk. They help lessen the pressure on your back, making symptoms less likely.
Proper Posture and Lifting Techniques
Spinal cord compression can be prevented by standing and lifting correctly. Keep your back straight and use your legs, not your back, when lifting. This lessens stress on your spine, making compression problems less likely over time.
Regular Exercise and Stretching
Exercise and stretching are key for a strong spine and can cut the risk of spinal cord compression. Activities like walking, swimming, and yoga are great. They keep your spine healthy and flexible, lowering the chance of issues.

Cauda Equina Syndrome
Cauda equina syndrome (CES) is a serious condition. It's caused by the squeezing of nerve roots at the end of the spinal cord. This pressure can cause sudden and severe problems. Quick treatment is crucial to avoid lasting nerve damage.
The main cause of CES is a large herniated disc in the lower back. This disc pushes on the nerves, leading to CES. Other reasons for CES can be spinal lesions, infections, or injuries. Birth defects, blood vessel issues, and surgery problems can also cause it.
If you notice any key symptoms of CES, like bowel or bladder issues, severe leg pain, or numbness in areas like the thighs, get emergency help. A neurosurgeon or spine doctor should see you right away. Early care is vital for preventing nerve damage and helping you get better.
CES is a health emergency often needing surgery within 24 to 48 hours. But, if surgery happens later, symptoms might still improve for some. Yet, if the nerves are severely hurt, some issues like bladder control may not get better. This could last a long time.
Having CES can really change your day-to-day life, impacting work, relationships, and mood. Medications, therapy, and support from friends can help deal with the pain. Your healthcare team and loved ones matter a lot for emotional support too.
While not common, CES affects around 1 in 65,000 people. About 60% have full CES, which may have bladder or bowel problems. The other 40% with incomplete CES might feel urgency but no issues with holding their bladder or bowels.
If you or someone you know gets CES, remember, there is support. Quick medical care, the right treatment, and support from others can improve your life. Always talk to your healthcare team for advice and support.
Managing Spinal Cord Compression
The best way to approach spinal cord compression is by working with your healthcare team. They may include orthopedists, neurologists, and physical therapists. Together, you can create a plan to deal with the root cause and control your symptoms.
Working with Healthcare Providers
Your healthcare team is key in managing your condition. They will explain what's causing your spinal cord compression and suggest treatments. It's important to talk openly with them about how you feel and any changes you notice.
Self-Care and Lifestyle Modifications
Alongside medical treatments, there are things you can do on your own to help. Keeping a healthy weight, having good posture, and exercising regularly can reduce stress on your spine. These habits are crucial for managing your condition.
Complementary Therapies
Some people might get relief from acupuncture or chiropractic care. It's important that these treatments are in addition to, not instead of, what your doctor advises. Always check with your healthcare team before starting any complementary therapy.
When to Seek Emergency Care
If you suddenly can't control your bowel or bladder, or feel severe numbness in your legs, you need to act fast. This includes having difficulty walking due to leg pain or weakness. Don't delay seeking help. Untreated, these conditions can cause permanent nerve damage.
Spinal cord issues might start fast, after an accident, or slowly with time. The cause can be anything from injuries to the regular wear and tear on your back. When the nerves in the lower back are affected, a situation like cauda equina syndrome can happen. This needs immediate treatment usually in the ER.
Doctors use CT scans or MRIs to figure out what's going on with your spine. They give a clear view of the problem. Treating spinal cord problems often means a group of experts working together. They might use drugs, PT, injections, or sometimes, surgery.
If you have any worrying signs, going to the ER right away is key. Quick action can avoid lasting nerve damage and keep you well. Don't wait if you have symptoms that seem related to spinal cord issues.
Living with Spinal Cord Compression
Living with spinal cord compression can be tough, both physically and emotionally. Yet, with the right support, you can boost your life quality. This involves being actively involved in your treatment and care.
Emotional and Psychological Support
It's crucial to understand the emotional impact of spinal cord compression. Dealing with physical limits, pain, and a potential loss of freedom can affect your mental well-being. Getting help through counseling or support groups can improve your mental health and teach healthy ways to cope.
Assistive Devices and Modifications
Using tools and adapting your home can help you stay independent and safe. Things like braces, walkers, or ramps make daily life easier. They help with moving around and lower the chance of accidents.
Support Groups and Resources
Finding a support group can make a big difference. It lets you connect with people who understand what you're going through. Sharing tips and experiences with others can be very helpful. Also, online resources provide valuable info to help you manage your situation.
Key Takeaways
The key points about spinal cord compression are:
- Any issue that squeezes the spinal cord can lead to problems.
- You might start feeling symptoms suddenly or over time. These can be pain, numbness, weakness, and trouble controlling your bladder or bowels.
- Reasons for compression include osteoarthritis, injuries, tumors, and certain diseases.
- Doctors use a physical checkup, scans, and sometimes other tests to find out what's wrong.
- Treatments can be medicine, physical therapy, or even surgery, based on the reason and how severe it is.
- Living a healthy life might lower your risk or ease symptoms, but not all causes can be stopped.
- It's very important to get help quickly if you have severe symptoms. This can stop lasting damage to your nerves.
Knowing these main points about spinal cord compression is crucial. It helps you spot the signs, get the right care, and work on dealing with this issue. With teamwork between you and your healthcare team, along with good habits, you can make a big difference in your health and future.
Conclusion
Compression of the spinal cord is a severe issue that affects health and life quality. It's important to know the causes, symptoms, and how it's diagnosed and treated. This knowledge helps in recognizing when to see a doctor and how to manage it. Working with healthcare professionals, adopting healthy habits, and getting support is key.
Learning more about spinal cord compression helps improve care and support for those with it. Several conditions can cause it, such as cervical spondylosis or a spinal epidural abscess. This shows the need to stay educated and take an active role in your health. By taking the right steps, living with spinal cord compression can be less challenging. You can focus on staying well.
FAQ
What is spinal cord compression?
Spinal cord compression happens when other conditions put pressure on your spinal cord. This cord is a bunch of nerves moving messages from your brain to everywhere else. It can be from your neck down to your lower back.
What causes spinal cord compression?
Various things can cause your spinal cord to get compressed. These include osteoarthritis, spinal injuries, tumors, and certain bone diseases.
What are the symptoms of spinal cord compression?
You might feel pain in your back or neck and have numbness and weakness. There could also be problems with your bowel or bladder. How serious and fast these symptoms appear depends on the cause.
How is spinal cord compression diagnosed?
To find out if you have spinal cord compression, your doctor will talk to you and examine you. They'll also use X-rays, CT scans, and MRIs to get a closer look.
How is spinal cord compression treated?
The treatment changes based on how bad your symptoms are and what's causing them. You might need medicine, physical therapy, or even surgery.
Can spinal cord compression be prevented?
It's hard to prevent all cases of spinal cord compression. But, keeping a healthy weight, good posture, and regular exercise can lower your risk.
What is cauda equina syndrome?
This is a serious issue where the nerve roots at the end of your spinal cord get compressed. It needs to be treated right away to prevent permanent damage.
When should I seek emergency care for spinal cord compression?
Go to the ER if you suddenly can't control your bowel or bladder, get increasing numbness in your legs, have severe leg pain and weakness, or have trouble walking or standing up.
How can I manage daily life with spinal cord compression?
Work closely with your healthcare team and take care of yourself. Using devices to help, and finding emotional support is important.
Source Links
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/spinal-cord-compression
- https://www.ncbi.nlm.nih.gov/books/NBK557604/
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=134&ContentID=13
- https://www.umms.org/ummc/health-services/orthopedics/services/spine/patient-guides/anatomy-function
- https://spinehealth.org/article/spine-anatomy/
- https://www.cancerresearchuk.org/about-cancer/coping/physically/spinal-cord-compression/treatment
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome
- https://my.clevelandclinic.org/health/diseases/22132-cauda-equina-syndrome
- https://www.aafp.org/pubs/afp/issues/2001/0815/p631.html
- https://www.cancerresearchuk.org/about-cancer/coping/physically/spinal-cord-compression/about
What Is Spinal Stenosis? A Comprehensive Overview
Spinal stenosis happens when nerve roots get pressed in the spine. This often causes pain, weakness, and numbness. Different parts of the spine can get affected, leading to various symptoms. Sadly, we can't always tell who will feel the symptoms as they grow older. Luckily, simple lifestyle changes can help slow down the process.
When the spinal canal narrows and nerve roots get squeezed, it's called spinal stenosis. This makes pain, weakness, and numbness show up. Learning about what causes it and how to deal with the symptoms is key to handling this issue.
Introduction to Spinal Stenosis
Definition and Overview
Spinal stenosis happens when the nerve roots in the spine are pressed by various issues. This pressure causes pain, numbness, and weakness. The neck and lower back are often affected, but the middle back can also have this issue, usually due to a herniated disk.
Prevalence and Epidemiology
In the U.S., spinal stenosis is common, especially among older adults visiting the doctor's office. Around 1 out of every 1000 people over 65 and 5 out of every 1000 people over 50 might get it. It is expected that over 18 million Americans will have this condition in the next decade.
Causes of Spinal Stenosis
Spinal stenosis can come from birth defects or happen over time. Only a small number, 9%, are due to being born with certain conditions. Knowing these causes helps doctors treat patients better.
Congenital Causes
Cases of spinal stenosis from birth issues can be because of several conditions. These include achondroplasia and other structural problems. These issues make the spinal canal narrow, putting people at risk for spinal stenosis from an early age.
Acquired Causes
Spinal stenosis can also happen later in life. This might be due to injuries, aging, or medical procedures. Injuries that impact the spine can cause spinal stenosis. So can wear and tear over time. This includes things like disk herniation and the growth of soft tissues within the spine.
Degenerative Changes
The main reason for spinal stenosis is the breaking down of the spine as we age. Arthritis plays a big role. It can lead to the narrowing of the spinal canal. This puts pressure on the nerves in the spine, causing pain and other problems.
what is spinal stenosis
Understanding the Condition
Spinal stenosis is when the spinal canal narrows and puts pressure on the spinal cord. This narrowing can pinch the spinal cord and nerves, affecting how your body works. Many things can cause this, like a bulging disc or too much growth on the spine's bones.
Types of Spinal Stenosis
Spinal stenosis can happen in the neck, chest, or lower back. It's most often found in the lower back and neck. Things like getting older or having an injury can lead to this problem.
Symptoms of Spinal Stenosis
Spinal stenosis is when the spinal canal gets narrow. The symptoms change based on where and how bad the compression is. Knowing these signs helps find and treat the problem early.
Cervical Spinal Stenosis Symptoms
When the cervical spine narrows, it can press on nerves or the spinal cord. This might cause neck or arm pain at first. Over time, you might feel numb, weak, or have trouble balancing.
Lumbar Spinal Stenosis Symptoms
If the lumbar spine narrows, it can lead to leg pain during walking that gets better with rest. This can also cause weakness or odd sensations in the legs.
Cauda Equina Syndrome
If spinal stenosis gets very bad, it could lead to cauda equina syndrome. This is an emergency if you lose control over your bathroom functions, have severe leg numbness, and find it hard to walk or stand. Immediate treatment is necessary to avoid lasting nerve damage.

Diagnosis of Spinal Stenosis
Finding out if you have spinal stenosis starts with a close look at your symptoms and how you're feeling. Your doctor will ask you a lot of questions about your health and what you're going through. They will then check you over, paying close attention to how you move, feel, and react. This involves looking at the way you walk and testing your strength and reflexes.
Physical Examination
Next, your provider will test how well your body moves, the strength in your muscles, and your nerves. They might do special tests like raising your leg while you lie down, or having you stand still with your eyes closed. These can help figure out the cause of your symptoms. They'll also check how you stand, your reflexes, and your walk. This is to see if there are any signs of spinal stenosis.
Imaging Tests
After the exam, your doctor could ask for more tests to pin down spinal stenosis. These might include an x-ray you move through, a CT scan, or MRI. MRI is often the most helpful. It gives clear images that show how much your spine has narrowed. It also spots any changes in the structure of your spine, which can all help in making a diagnosis.
Additional Diagnostic Tests
Along with imaging, your medical team might suggest electric tests to study how your nerves are working. These tests can add more clues to what's causing your issues. They shed light on your nerve health, aiding in the development of a treatment plan.
Treatment Options for Spinal Stenosis
If you've been diagnosed with spinal stenosis, your doctor will go through treatment options with you. They aim to ease your symptoms and stop the condition from getting worse. Treatments fall into two main groups: conservative treatments (non-surgical) and surgeries.
Conservative Treatment
For those with spinal stenosis in the neck but not compressing the spinal cord, doctors first try non-surgical methods. This includes using a brace, resting, and taking NSAIDs to lessen pain and swelling. If spinal cord compression occurs (myelopathy), surgery to decompress the spine might be needed to ease pain and prevent further myelopathy.
In the lower back, initial treatments often involve NSAIDs and physical therapy for the pain. If the pain continues, your doctor might suggest shots of steroids into the spine to reduce swelling and pain.
Surgical Procedures
If conservative treatments do not work, or you begin to have more severe symptoms or spinal instability, surgery could be necessary. The types of surgery for spinal stenosis are:
- Decompression surgeries, like laminectomy, to make more space in the spinal canal
- Discectomy, to fix a herniated or bulging disc
- Spinal fusion, to stabilize the spine
- Foraminotomy, to expand the nerve openings in the spine
- Minimally invasive surgery, which means less scarring and quicker recovery
Your doctor will help you decide on the best plan, looking at your symptoms, how severe the condition is, and your lifestyle.

Spinal Stenosis Treatment
Treating spinal stenosis involves various options. These aim to tackle the causes and symptoms. Your team might suggest both non-surgical and surgical methods. They'll choose based on how bad your stenosis is and how you respond to treatment.
Non-surgical treatments include physical therapy, drugs, and certain pain relief techniques. Physical therapy strengthens your spine's support muscles. It also boosts your flexibility and endurance. Doctors may also give you drugs like NSAIDs, antidepressants, and opioids to lessen pain.
For more serious cases, or if non-surgical methods don't help, surgery could be the next step. Operations like a laminectomy create more room in your spine. This eases the pressure on your nerves. Sometimes, spinal fusion surgery is needed for stability.
Working closely with your healthcare team is key in finding the best treatment. They will guide you through your options, explaining both risks and benefits. Together, you'll make a plan to handle your spinal stenosis effectively.
Risk Factors and Prevention
Spinal stenosis is common and knowing the risks can help prevent it. Most cases occur after age 50. But, younger people with spine issues like scoliosis are at risk too.
Age-Related Risk Factors
The spine naturally wears as we get older. This can cause spinal stenosis. It often comes from spine arthritis. Sometimes, tumors in the spine can lead to it too.
Lifestyle Factors
Bad habits can also make spinal stenosis worse. For example, arthritis may cause extra bone growth. This can press on the spine. To help prevent or slow this, stay at a healthy weight, exercise, and mind your posture.
Preventive Measures
Some spinal stenosis risks, like age, can't be changed. But, you can cut other risks by not smoking, staying fit, and exercising. It's also key to catch it early and work with your doctor for a treatment plan.

Cervical Spinal Stenosis
Cervical spinal stenosis happens when the spinal canal in the neck area gets narrow. It compresses the nerve roots and spinal cord. This leads to symptoms that make life hard.
Causes and Symptoms
The main causes are the wear and tear of aging. This includes things like herniated discs and thickening of joints and ligaments. These changes make the spinal canal smaller over time. People with cervical spinal stenosis often feel pain in their neck or arms. They also have issues like numbness, tingling, and weak muscles. In severe cases, myelopathy can develop, causing more serious problems.
Treatment Options
The way to treat cervical spinal stenosis depends on how bad it is. It also depends on how well someone responds to basic treatments. Sometimes, using a brace, taking anti-inflammatory drugs, and doing physical therapy can help. But if these methods don't work, or things get worse, surgery might be the next step. There are various surgical options, like decompression surgery or spinal fusion, to ease symptoms and improve quality of life.
By learning about what causes cervical spinal stenosis, its symptoms, and treatment options, people can work with their doctors. Together, they can create a plan to manage the condition and lead a better life.
Lumbar Spinal Stenosis
Lumbar spinal stenosis affects the lower back, specifically the lumbar spine. It's when the spinal canal narrows, squeezing nerve roots and the spinal cord. This can cause pain in the back and legs, making it hard to walk or stand.
Causes and Symptoms
Mostly, lumbar spinal stenosis is due to osteoarthritis, which slowly narrows the spinal canal. People usually feel a cramping pain in their leg, calf, or buttocks. They might also have back pain and lose feeling in their feet, or feel weakness and numbness in their legs.
Sometimes, it can cause a severe problem called cauda equina syndrome. This leads to a loss of control over the bowel or bladder, along with severe leg numbness and weakness. It needs quick medical help.
Treatment Options
Treatments may involve physical therapy, medications, and interventional procedures to manage pain. The goal is to make symptoms better and function improve.
If these don't work or if symptoms get worse, surgery may be suggested. Operations can include removing bone spurs or fusing vertebrae to create more space.
To diagnose lumbar spinal stenosis, doctors use X-rays, CT scans, and MRI scans. These tests show how bad the narrowing is and help decide the best treatment.
Staying at a healthy weight, regular exercise, maintaining good posture, and not smoking can lower your risks. Although there's no cure for lumbar spinal stenosis, you can manage it with your doctor's help.
Cauda Equina Syndrome
Symptoms and Urgency
Cauda Equina Syndrome (CES) is very serious. It leads to symptoms such as not being able to fully empty your bladder (urinary retention) and losing control of the bladder or bowels (urinary and fecal incontinence). Other signs include feeling things differently or not at all in your bottom area, and weak or paralyzed legs. Back and leg pain, and issues with sex are also common.
CES is a medical emergency. It needs quick treatment to avoid lasting harm. Such harm could be permanent leg weakness or not being able to move, and the loss of bladder or bowel control.
Emergency Treatment
For CES, quick surgery is key. It should happen within 48 hours of the symptoms starting. This surgery aims to take off the pressure on the spinal nerves, stopping later harm. It can help a lot in improving the person's feeling and movement in their legs.
After the emergency surgery, ongoing care is crucial. This usually includes working with a rehabilitation team. It's to help the patient cope with lasting symptoms and get back to regular life as much as possible.
The impact of CES isn't just physical. It can change your daily life and relationships. Doing things with friends and family is important when handling CES. Support from those close to you can make a big difference.
Plus, medicine, exercise, and therapy to talk through your feelings can help manage the pain and stress of CES.
Living with Spinal Stenosis
Spinal stenosis heavily impacts many people over 50. It's key to look at many ways to ease pain, change habits, and find help. This helps make life better while dealing with this condition.
Pain Management Strategies
Easing spinal stenosis pain is very important. Meds like acetaminophen or NSAIDs are often used. Physical therapy is also a great option. It can help you move better, get stronger, and keep more flexible. Alternative methods like acupuncture could also help.
Lifestyle Modifications
Changing how we live can really help with spinal stenosis. Keeping a healthy weight, being active, and sitting/standing correctly can ease stress on the spine. These steps can really slow down how fast the condition gets worse. It helps especially for women, those with narrow spinal canals, or previous spinal issues or surgeries.
Support Resources
Spinal stenosis can be tough, but you're not alone. Talking to others in support groups and learning from materials can make a big difference. These things can help you learn more about your condition, find treatment choices, and meet people who share your experiences.
Using different strategies, lifestyle changes, and support can help a lot. Remember, while spinal stenosis can't be fully cured, it can be managed. With a good approach, you can ease symptoms and still lead an active life.
Conclusion
In conclusion, spinal stenosis is when the spinal canal gets narrow. This can squeeze nerve roots and the spinal cord. It can happen in different parts of the spine. Symptoms include pain, numbness, weakness, and trouble walking called neurogenic claudication.
The diagnosis for spinal stenosis uses physical exams, imaging tests, and nerve studies. Treatments include physical therapy and medicine. For severe cases, surgery might be needed. Knowing about the condition and its treatments helps you and your doctor manage it. This improves your life quality.
Spinal stenosis often affects those over 50. Being mindful of the symptoms is crucial. With proper medical care and lifestyle changes, controlling spinal health is possible. This aids in keeping an active life.
FAQ
What is spinal stenosis?
Spinal stenosis happens when nerve roots are pressed, causing pain and other issues.
What causes spinal stenosis?
It can be from birth or happen later in life. Birth issues like achondroplasia can lead to it. Later causes include injuries, wear and tear, and general body problems.
What are the symptoms of spinal stenosis?
Symptoms vary. But often there's pain in the back or neck, along with numbness, tingling, and weak arms or legs.
How is spinal stenosis diagnosed?
Doctors check you physically and might take X-rays or do MRI scans. They might also check how your nerves work using special tests.
What are the treatment options for spinal stenosis?
Treatment mixes exercise, medicine, and maybe surgery, depending on how bad it is.
What is the difference between cervical and lumbar spinal stenosis?
Cervical spinal stenosis is in the neck. It can cause arm problems. Lumbar stenosis is lower, leading to leg trouble.
What is cauda equina syndrome, and why is it a medical emergency?
Cauda equina syndrome from spinal stenosis is very serious. It can lead to not controlling the bowel or bladder, along with leg issues. It needs quick care to avoid lasting nerve problems.
What are some risk factors for developing spinal stenosis?
Aging, injuries, and some health problems raise the risk of spinal stenosis. But, keeping fit, a good posture, and no smoking can lower your chances.
How can I manage my spinal stenosis symptoms?
You can deal with the symptoms using medicine, exercise, and by keeping a healthy lifestyle and posture. And, finding support can be very helpful.
Source Links
- https://www.ncbi.nlm.nih.gov/books/NBK441989/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/lumbar-spinal-stenosis
- https://www.mayoclinic.org/diseases-conditions/spinal-stenosis/symptoms-causes/syc-20352961
- https://www.niams.nih.gov/health-topics/spinal-stenosis
- https://www.mountsinai.org/health-library/diseases-conditions/spinal-stenosis
- https://www.mayoclinic.org/diseases-conditions/spinal-stenosis/diagnosis-treatment/drc-20352966
- https://www.niams.nih.gov/health-topics/spinal-stenosis/diagnosis-treatment-and-steps-to-take
- https://www.webmd.com/back-pain/treatments-for-spinal-stenosis
- https://www.webmd.com/back-pain/spinal-stenosis
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome
- https://rheumatology.org/patients/spinal-stenosis
- https://www.honorhealth.com/healthy-living/5-things-know-about-spinal-stenosis
- https://medlineplus.gov/spinalstenosis.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7595829/
What Is Reye’s Syndrome? An Overview of This Rare Condition
If you have a child or teenager, knowing about Reye's syndrome is critical. Reye's syndrome mostly affects those under 18 after getting a viral illness. It can lead to liver and brain swelling, causing confusion, seizures, and even coma.
Symptoms of Reye's syndrome appear a few days after a viral illness starts. It's vital to diagnose early and treat fast. Without care, it can be fatal. It's especially important to avoid giving children aspirin for pain or fever. Instead, use acetaminophen (Tylenol) or ibuprofen (Advil).
If vomiting, confusion, or serious symptoms follow a viral illness, get help right away. Early treatment can save lives and prevent brain damage. Understanding Reye's syndrome and avoiding aspirin can keep your family safe.
Overview of Reye's Syndrome
Definition and Key Facts
Reye's syndrome is a rare disorder that mostly harms kids and teens under 18. It shows fatty liver changes and sudden brain swelling. The exact cause is unknown, but doctors think it's connected to using aspirin with certain viral illnesses.
These illnesses include the flu and chickenpox. Reye's syndrome can be deadly, so it needs quick care.
Rarity and Affected Age Group
Reye's syndrome affects mostly kids and teenagers, especially those aged 5 to 14. It's very rare in babies and adults over 18. The syndrome is related to taking medicines like aspirin, especially in those under 16.

What Is Reye's Syndrome
Reye's syndrome is a rare disorder that affects kids and teenagers under 18. It leads to fatty changes in the liver and swelling of the brain. This happens during the recovery from viral infections like the flu or chickenpox. The main cause is not known for certain, but it's linked to taking aspirin during these illnesses.
Reye's syndrome might appear a few days after the first signs of a virus. Using aspirin seems to make the risk higher. That's why it's very important not to give aspirin to children or teenagers with viral infections. Doctors advise against it to prevent Reye's syndrome.
Unfortunately, there's no cure for Reye's syndrome. But, doctors can focus on stopping brain damage. How well a person gets better just depends. Some fully recover, while others might have lasting brain issues. Getting treatment early is key to increasing the chance of survival.
Symptoms of Reye's Syndrome
The signs of Reye's syndrome often show up 3 to 5 days after getting a viral sickness. This could be simple things like the flu or chickenpox. It's really important to know the early symptoms and when to get help. This helps get the right treatment early, which is key to fighting this rare but severe illness.
Initial Symptoms
At first, you might see diarrhea, fast breathing, throwing up, feeling very tired, and moving slower than usual. If a child under 2 shows these signs, it's important to get them to a doctor right away. Even if these signs are not clear, early attention is crucial.
Additional Symptoms
Reye's syndrome can get worse over time. The mild start might turn into being very moody, not making sense, or feeling weak in the arms and legs. It could lead to seizures, extreme fatigue, and not being fully awake. If any of these signs show, seek emergency medical help immediately.
When to Seek Medical Attention
If a child starts having seizures, faints, or keeps throwing up after being sick with the flu or chickenpox, don't wait. Unusual sleepiness or sudden changes in behavior also signal something serious. Reye's syndrome can be deadly if not treated fast.

Causes of Reye's Syndrome
Experts are still not sure what exactly causes Reye's syndrome. But, they think that taking aspirin while having certain viral illnesses might lead to it. For example, when someone has the flu or chickenpox and uses aspirin, they might get Reye's syndrome. Certain metabolic disorders, like MCAD deficiency, could also be a cause. These are problems with how the body uses fats.
Link with Aspirin Use
Research shows that using aspirin during viral infections is strongly linked to Reye's syndrome. This is why doctors advise against giving aspirin to kids. Aspirin might not be safe for children because of this connection.
Underlying Metabolic Disorders
Some metabolic disorders can make people more likely to get Reye's syndrome. These disorders make it hard for the body to use fats properly. If doctors screen newborns for these disorders, they can spot kids who might be at higher risk for Reye's syndrome. This early detection can be crucial.
Viral Infections Associated with Reye's Syndrome
Getting a viral illness, like the flu, often leads to Reye's syndrome. Signs of Reye's syndrome usually show up 3 to 5 days after a viral infection starts. While some toxins can cause symptoms like Reye's syndrome, they are not the real cause.
Risk Factors for Reye's Syndrome
Many things can make a child more likely to get Reye's syndrome. The main ones are:
- Taking aspirin for a virus, like the flu, chickenpox, or a breathing infection.
- Having a special health issue like a problem with breaking down fats or using energy.
Reye's syndrome hits kids and teens hardest, usually between 5 and 14 years. It doesn't happen often in babies under 1 or people older than 18. Using aspirin, like in teenagers, has a strong link to this disease.
Kids who have rare genetic problems, like MCADD, might also face more risk. This is especially if they also have a viral sickness and take aspirin.

Diagnosing Reye's syndrome can be tricky, leading to slow treatment. But, more studies and joining clinical tests can make care better for those with this illness.
Complications of Reye's Syndrome
Reye's syndrome brings severe, life-threatening complications if not quickly treated. The main issues are liver failure, brain swelling, and high brain pressure.
It often leads to liver failure, which causes a toxic buildup and harms body function. This worsens brain swelling and pressure, key problems in this syndrome.
The brain's high pressure can cause seizures, coma, and fatal outcomes. If someone has seizures or faints, they need medical help right away.
Though many with Reye's syndrome survive, they may face lasting brain damage. This damage depends on the level and length of brain swelling.

If not treated quickly and aggressively, Reye's syndrome can be deadly. Recognizing symptoms early and seeking medical help fast is critical. It can greatly improve the chances of survival.
Diagnosis of Reye's Syndrome
Diagnosing Reye's syndrome early is key. Quick recognition and treatment are vital to lower the risk of life-threatening issues. Doctors look at symptoms, test results, and rule out other causes to diagnose Reye's.
Clinical Criteria
The CDC has set specific clinical criteria for Reye's syndrome. This includes brain dysfunction with consciousness changes. Also, liver problems like high liver enzymes and ammonia levels are checked.
Laboratory Findings
Laboratory tests are important in diagnosing Reye's syndrome. Tests of spinal fluid can find metabolic disorders. A liver biopsy looks for fat changes in the liver. The diagnosis is not by one test but by overall symptoms and test results.
Diagnosing Reye's syndrome usually happens in an emergency. Symptoms like seizures need quick medical attention. This speeds up the chance of getting better.
Treatment and Management
The treatment focuses on supportive care. It targets the metabolic issues and rising pressure inside the brain. These problems can happen with Reye's syndrome.
Supportive Care
Care includes central venous access setup, airway support, and a urine monitor. This monitoring happens in a very careful way in an intensive care unit.
Correcting Metabolic Abnormalities
The goal is to fix issues like low blood sugar, acidosis, and high ammonia. Treatments might use dextrose fluids plus sodium bicarbonate. They might also use medicines like phenylacetate-sodium benzoate to help with these problems.
Reducing Intracranial Pressure
To lower the brain's pressure, some steps are taken. Patients might have their head raised and their fever controlled. Diuretics, like furosemide, could be used. For severe cases, mannitol or hypertonic saline might be needed to decrease pressure.
Reye's Syndrome Prevention
It's key not to give aspirin to kids or teens, especially if they have the flu or chickenpox. Use acetaminophen or ibuprofen for fever and pain instead. Also, newborn screening for metabolic disorders can spot kids more likely to get Reye's syndrome.
Avoiding Aspirin in Children
Doctors say avoid aspirin in kids and teens because it can lead to Reye's syndrome. Use acetaminophen or ibuprofen for fever and pain in viral illnesses. This helps lessen the risk of a severe outcome.
Newborn Screening for Metabolic Disorders
Newborn screening for metabolic disorders finds kids more at risk of Reye's syndrome, like those with fatty acid oxidation disorders. It's important because it lets you take steps early to avoid Reye's syndrome during viral infections.
Vaccination Against Viral Illnesses
Make sure your child gets vaccines, like the influenza and chickenpox vaccines, to avoid the illnesses linked to Reye's syndrome. Lowering the risk of these viral infections is a big step in avoiding this dangerous condition.
Epidemiology and Incidence
Reye's syndrome is a rare condition, with less than 2 cases reported each year in the US since 1994. The real count might be higher, though. This is because reporting it is no longer a must. The peak age for getting it is between 5 and 14 years.
Historical Trends
Before, from 1979 to 1980, there were 555 cases in the US. This was a big worry for public health back then.
Impact of Public Health Warnings
In the 1980s, when people learned about aspirin causing Reye's syndrome, cases dropped a lot. This happened in the US, the UK, and France. The warnings really worked. They made people around the world more aware.
Prognosis and Outcomes
The prognosis for Reye's syndrome can vary. It is a serious condition that can be life-threatening. Luckily, most kids and teens who get it live. But, some may have brain damage. This can happen if not treated early.
It's very important to spot Reye's syndrome early. Then, start strong treatment right away. This helps lower the risk of dangerous problems like brain swelling. It also cuts the chances of seizures and organ failure.
The prognosis for Reye's syndrome depends on a few things. How bad the illness is, the child's age, and getting help quickly matter a lot. Early on, when found and treated soon, kids may heal fully without ongoing problems.
Yet, if the illness gets very severe, it could lead to serious setbacks. These might include lasting brain damage or even death. That's why acting fast and treating it seriously is key.
Related Disorders
Reye's syndrome is a rare disorder, but its signs often look like other problems. For instance, it shares some symptoms with OTC deficiency and fatty acid oxidation disorders. Recognizing these similarities is key to diagnosing and treating patients.
Ornithine Transcarbamylase Deficiency
OTC deficiency is another rare problem that affects how the body deals with toxins. It leads to high levels of ammonia, which can cause vomiting and confusion. Sometimes it happens when someone sick takes aspirin. This makes finding and treating OTC deficiency vital, especially if patients face stress from an illness.
People with OTC deficiency might show signs similar to Reye's syndrome. This often happens if they use aspirin while sick. So, spotting and dealing with OTC deficiency early can help prevent this.
Fatty Acid Oxidation Disorders
Fatty acid oxidation disorders, like MCAD deficiency, can also look like Reye's syndrome. These issues stop the body from using fats properly, leading to dangerous substances in the body. These can harm the liver and brain, especially under stress.
Testing newborns for these disorders is crucial. It helps spot those at higher risk for Reye's syndrome. This is especially important if the child gets sick and takes aspirin.
Conclusion
Reye's syndrome is a rare but serious condition. It mostly affects children and teenagers after they have the flu or chickenpox. Although we don't know the exact cause, using aspirin during these illnesses can lead to Reye's syndrome. It's vital to spot the symptoms early, avoid aspirin, and get quick, aggressive medical help. Doing this can make the chances of severe problems lower.
Thanks to ongoing efforts and better public health, the number of Reye's syndrome cases has dropped. The National Institutes of Health notes that it's now a rare condition, with less than 2 cases yearly in the U.S. since 1994. This achievement is mainly because people have stopped giving aspirin to kids. This change also decreased the number of cases in countries like the United Kingdom.
But, we still need to be careful, especially for children with certain health issues that could make them more at risk. By knowing the risk factors, spotting early signs, and taking steps to prevent it, you can protect your child's health. This is important, especially if they get a viral illness.
FAQ
What is Reye's syndrome?
Reye's syndrome is a rare but serious condition. It causes liver and brain swelling. It affects children and teenagers after viral infections like the flu or chickenpox.
What are the symptoms of Reye's syndrome?
Symptoms include confusion, seizures, and loss of consciousness. They need emergency care. Without quick treatment, Reye's syndrome can be deadly.
What causes Reye's syndrome?
The cause of Reye's syndrome isn't fully known. But, it's linked to using aspirin during viral illnesses. The flu or chickenpox are common triggers.
How is Reye's syndrome treated?
Treating Reye's syndrome is mainly about support. It needs intense care and close watch. Doctors may work on metabolic issues and lower brain pressure to help.
How can Reye's syndrome be prevented?
Avoid aspirin in kids or teens with viral illnesses to prevent Reye's syndrome. Use safer drugs like acetaminophen or ibuprofen for fever and pain.
What is the prognosis for Reye's syndrome?
Thanks to modern care, most patients survive Reye's syndrome. There might be some brain damage. But, without treatment, it can be fatal in days.
What are some disorders related to Reye's syndrome?
Reye's syndrome shares symptoms with some metabolic disorders. These include ornithine transcarbamylase (OTC) deficiency and fatty acid oxidation disorders.
Source Links
- https://www.mayoclinic.org/diseases-conditions/reyes-syndrome/symptoms-causes/syc-20377255
- https://rarediseases.org/rare-diseases/reye-syndrome/
- https://www.ninds.nih.gov/health-information/disorders/reyes-syndrome
- https://www.nhs.uk/conditions/reyes-syndrome/
- https://www.webmd.com/children/what-is-reye-syndrome
- https://www.mayoclinic.org/diseases-conditions/reyes-syndrome/diagnosis-treatment/drc-20377259
- https://emedicine.medscape.com/article/803683-treatment
- https://emedicine.medscape.com/article/803683-overview
- https://www.sciencedirect.com/topics/medicine-and-dentistry/reye-syndrome
- https://www.ncbi.nlm.nih.gov/books/NBK526101/
How I Cured My Sjogren’s Syndrome: Personal Experiences and Insights
Sjogren's syndrome is a long-term autoimmune issue. It mainly affects the salivary and tear glands. This leads to dry mouth and eyes. It also causes tiredness, joint aches, and swallowing trouble. Though Sjogren's has no cure, many people manage its effects by combining traditional methods, natural solutions, and lifestyle adjustments. I'll talk about how I beat Sjogren's and my tips to get healthy again.
Understanding Sjogren's Syndrome
What is Sjogren's Syndrome?
Sjogren's syndrome is when the body's immune system attacks moisture-producing glands. This causes dry mouth and eyes. It's quite common, affecting up to 1% of people worldwide. It can happen by itself or with other autoimmune diseases, like rheumatoid arthritis or lupus.
Symptoms of Sjogren's Syndrome
Its key signs are dry mouth and eyes. But it can cause more issues, including:
- Fatigue and chronic pain
- Joint and muscle aches
- Dry skin, nose, and throat
- Difficulty swallowing or speaking
- Recurrent oral and vaginal yeast infections
- Digestive issues, such as acid reflux or irritable bowel syndrome
- Increased risk of lymphoma and other autoimmune disorders
Causes and Risk Factors
Experts don't fully know what causes it, but they think both genes and the environment play a part. Some things that make a person more likely to get Sjogren's syndrome are:
- Gender: It's more common in women, with nine women getting it for every man who does.
- Age: People usually start showing symptoms between 40 and 60, but it can start earlier.
- Genetics: Certain gene types and family history may make you more likely to have it.
- Having other autoimmune diseases: If you already have conditions like rheumatoid arthritis or lupus, you might also develop Sjogren's syndrome.
My Journey with Sjogren's Syndrome
Initial Symptoms and Diagnosis
My journey with Sjogren's syndrome started with dry eyes and constant fatigue. I first dismissed it as just part of getting older or being stressed. But, the symptoms didn't go away. They got worse over time.
Finally, I went to see a doctor. After many tests and visits, a rheumatologist diagnosed me with Sjogren's. This news brought both relief and worry. I had to learn what this diagnosis meant for me.
Coping with Chronic Fatigue and Pain
The hardest part of having Sjogren's for me is the never-ending tiredness and pain. The fatigue and aches in my body make everyday life hard. I often have to take a break and focus on taking care of myself.
To cope, I've had to make many changes. This includes how I work, how I spend time with people, and what I do for fun. It's been a journey to figure out how to live well with the challenges of this condition.
Conventional Treatments and Their Limitations

After being diagnosed, my team first tried common treatments like eye drops, saliva replacements, and drugs for Sjogren's. They eased some issues. But, they brought new problems like dry skin and headaches. These side effects made me look for other ways to handle my illness.
Medications and Their Side Effects
The medicines I got for dry mouth and eyes had bad effects. The eye drops made my eyes hurt, and the spit substitutes only helped for a bit, causing headaches. Also, pills like immuno-suppressants and anti-inflammatories made my skin dry and upset my stomach.
I faced a big challenge with these meds' side effects. I was often changing doses, trying new drugs, and looking for solutions. This made me doubt if relying only on these regular methods was the right choice. So, I began to seek more natural and full-body ways to cope with Sjogren's.
Exploring Natural Remedies
I deepened my understanding of Sjogren's syndrome and got curious about natural remedies. Changing my diet was a big step. I started eating anti-inflammatory foods and adding more hydrating, nutrient-rich foods. I also tried supplements like omega-3 fatty acids and probiotics. These are known to help people with autoimmune diseases.
Diet and Lifestyle Changes
Changing what I eat was just the start. I also had to look after my mental health. So, I started doing meditation, yoga, and deep breathing exercises every day. These things helped me handle feelings of anxiety and depression. They gave me a more positive attitude.
Stress Management Techniques
I wasn’t just changing my diet and managing stress differently. I also explored other treatments like acupuncture and massage. Using herbs was part of it too. These therapies helped with my symptoms, like pain and tiredness. They seem to offer a whole-person approach. This helped deal with my illness in a more personal way.
The Role of Mindset and Emotional Well-being

Living with Sjogren's syndrome carries a big emotional toll. Days filled with anxiety and depression are common. This happens as you face the unknowns of your health and its effect on daily life. Reaching out for help from a therapist or using mindfulness can help. These actions build strength to face the emotional challenges head-on.
Overcoming Anxiety and Depression
Being part of groups with people who share your struggle is crucial. Through online and face-to-face support groups, you gain a lot. You get to exchange stories, receive much-needed support, and learn valuable lessons from others like you. This connection offers a feeling of belonging and gives power to take charge of your health.
How I Cured My Sjogren's Syndrome
Integrating Multiple Approaches
Beating Sjogren's hasn't been easy for me. It was about mixing conventional medicine, natural cures, and lifestyle changes. This mix has boosted my health a lot. I can handle my symptoms better, use fewer drugs, and feel more in charge of my wellness.
Listening to My Body
Understanding my body better has been a big part of my healing. Now, I pay close attention to how I feel and adjust my life accordingly. This care helps me stay away from bad days and stay energized. I also make smarter health choices because I know myself well.
Perseverance and Consistency
Getting better needed a lot of time and effort from me. There were many challenges and victories. But, sticking to my healing plan and keeping it up made a difference. This effort helped me tackle my symptoms and feel stronger every day.
Life After Sjogren's Syndrome

Renewed Energy and Vitality
Recovering from Sjogren's has changed my life. I now feel a lot more energetic and alive. This change is due to eating better, managing stress, and focused therapies. I don't just feel better physically; I feel happier too. Now, I can do more of what I love without as much pain. This has made everything better in my life.
Embracing a Holistic Lifestyle
Fighting Sjogren's made me look at health in a new way. I do things like mindfulness, meditation, and eating healthy every day. With these changes, my Sjogren's symptoms are easier to handle. But more than that, I feel balanced and happy. I take care of myself better, know my limits, and appreciate the little things. They helped a lot with my recovery.
Lessons Learned and Advice for Others
One big thing I've learned with Sjogren's syndrome is to stand up for your health. This condition often gets missed or misunderstood, so you have to be the one to push for answers and care. I've found that being my own advocate, talking to my doctors and making sure my voice is heard, is key to dealing with Sjogren's. By doing so, I've managed to find what works best for me in handling my symptoms.
Advocating for Your Health
Getting to know as much as I can about Sjogren's has really helped me. I've looked into the latest info and how to take care of myself. I do this by reading reliable articles online and talking to my doctors. Thanks to this, I can make better decisions about my health and understand my condition better.
The Importance of Early Diagnosis and Treatment

Early diagnosis and treatment are crucial for diseases like Sjogren's syndrome. As with many autoimmune issues, my diagnosis came too late. This allowed my symptoms to worsen over time. If you notice constant dry eyes or a dry mouth, see a doctor right away. Ask for a full check-up with a specialist. Doing this early can help a lot.
Doctors find Sjogren's syndrome through a set of tests. This could involve a rheumatologist, an eye doctor, or a dentist. They check your tears and saliva first. Blood tests can show certain antibodies that might mean you have Sjogren's. But these antibodies aren't just in people with Sjogren's. They might also show up in other illnesses. Other tests, like a sialogram, look at your saliva glands. And a lip biopsy can tell if your symptoms are from Sjogren's.
The way to treat Sjogren's syndrome changes based on what parts of your body it affects. You might need medicines, surgery, or just to take better care of yourself. Medicines can help with things like dry eyes or joint pain. Some surgery options can plug your tear ducts to keep more moisture in your eyes. Self-care tips often focus on making your eyes and mouth less dry. This might mean using special eye drops, making the air more humid, and not smoking. Your doctor might also suggest ways to make more saliva.
Getting care early for Sjogren's is key to keeping it in check. Work closely with your healthcare provider. Doing this can make a big difference in how you feel. It gives you a chance to manage the symptoms and enjoy life more.
Managing Sjogren's Syndrome in Daily Life

Living with Sjogren's syndrome, you struggle with symptoms like dry eyes and dry mouth. Yet, you've discovered ways to ease these by using eye drops, saliva subs, and humidifiers. You adjust your habits, like keeping water nearby, to lessen these symptoms.
Dealing with Dry Eyes and Dry Mouth
You tackle dry eyes and mouth with help from your medical team. They suggest treatments you can buy or that need a prescription. You use artificial tears and eye ointments for your eyes.
Also, you try different methods to reduce tear loss. For a dry mouth, using artificial saliva and stimulators helps a lot. These keep you hydrated and comfortable.
Balancing Work and Personal Life
It's hard to manage Sjogren's at work and home. But, you've learned to set limits and take care of yourself. This means adjusting work hours and finding ways to cope with tiredness.
It's also about discussing your needs with your boss and family. By balancing work and rest, you keep your health in check. Not overdoing it helps prevent burnout.
Sjogren's Syndrome and Its Impact on Quality of Life
Physical Limitations and Adaptations
Sjogren's syndrome changes how you live by causing chronic pain and fatigue. It also makes simple tasks like staying hydrated and caring for your eyes difficult. You learn new ways to handle your day, change how you exercise, and conserve your energy. Adapting requires being flexible, creative, and putting self-care first.
Emotional and Social Challenges
Sjogren's syndrome affects more than just your body. It also brings emotional stress and affects your social life. The condition is hard to predict, symptoms always need managing, and to others, it's like you're not really sick. This can lead to feeling alone, anxious, and sad. Dealing with these feelings is as important as treating the physical symptoms.
Finding support, connecting with others going through the same thing, and being kind to yourself are essential steps in handling these challenges.
Staying Positive and Hopeful
Living with Sjogren's syndrome has taught you to find joy in everyday moments. Enjoying a good meal, doing what you love, or noticing nature’s beauty adds happiness. These small actions of care and mindfulness keep you optimistic. Appreciating tiny wins helps you stay strong and focused, even when things are hard.
Finding Joy in the Little Things
Facing Sjogren's syndrome, you've learned to enjoy simple pleasures. A calm walk, a good book, or a warm drink bring peace. Doing these activities daily helps you stay steady and happy. They bring balance and perspective, especially on tough symptom days.
Celebrating Small Victories
Dealing with Sjogren's has been a slow journey, but celebrating wins is key. A day with less pain, a boost in energy, or sticking to a new care plan are achievements. These celebrations keep you going, boost your morale, and show progress, even in unclear moments.
Resources and Support for Sjogren's Syndrome
Patient Organizations and Online Communities
Diving into the Sjogren's syndrome world will open paths to many patient organizations and online communities. These are for folks just like you, offering a gold mine of knowledge and a strong sense of togetherness. The Sjögren's Foundation and online forums stand out as prime examples.
They provide tons of info and resources, from educational content to support groups. Plus, you get to chat with others who are facing the same unique challenges as you. This connection can really boost your recovery journey.
Trusted Sources of Information
It's also good to lean on trusted sources for more information about Sjogren's syndrome. Top medical journals and studies, along with info from places like the Mayo Clinic, offer key insights. They keep you in the loop with the latest treatment news, self-care tips, and a deeper understanding of this autoimmune condition.
Conclusion
My journey with Sjogren's syndrome has changed me a lot. It's been hard, but I've also found moments of joy. I used a mix of traditional medicine, natural remedies, and lifestyle changes to get better. This way, I've gotten back my health and happiness.
I've learned it's key to take charge of my health and to always learn. Even in the face of challenges, I've found reasons to smile. Dealing with Sjogren's has made me stronger and more aware. And I'm grateful for the lessons it's taught me.
It's important to know you're not alone if you're facing Sjogren's. There's help, support, and others who get what you're going through. Keep fighting for your well-being and find joy in the little things. By being persistent and using different ways to heal, like I did, you can get better too.
FAQ
What is Sjogren's syndrome?
Sjogren's syndrome is a long-term disorder that affects the exocrine glands. These include the salivary and tear glands. It causes dry mouth and dry eyes.
What are the common symptoms of Sjogren's syndrome?
The key symptoms of Sjogren's syndrome are dry mouth and dry eyes. This disease can also cause fatigue, joint pain, and dry skin. It can affect the throat, nose, and make it hard to talk or swallow. It can also raise the risk of infections and other autoimmune diseases.
What causes Sjogren's syndrome?
Doctors are not sure of the exact cause of Sjogren's syndrome. But they think it's a mix of genetic and environmental factors. These factors start an immune system attack. This may be why it's more common in women and often starts between the ages of 40 and 60.
How is Sjogren's syndrome treated?
While there's no cure, Sjogren's syndrome can be managed. This includes using prescription eye drops and saliva substitutes. Lifestyle changes like dietary changes and supplements can help too. Complementary therapies and natural remedies might also ease some symptoms.
How can you manage the symptoms of Sjogren's syndrome in daily life?
Daily management involves using eye drops, saliva substitutes, and humidifiers. It's also key to tweak your routine to deal with dryness. Balancing work and self-care is important to fight fatigue and pain.
How can you overcome the emotional and social challenges of living with Sjogren's syndrome?
Dealing with the emotional and social effects of the disease is important. Seeking support, practicing self-kindness, and finding joy are crucial. Connecting with others through patient groups and online forums can help you feel understood.
Why is early diagnosis and treatment important for Sjogren's syndrome?
Getting diagnosed and treated early is crucial. It can prevent the disease from worsening. Seeking guidance from a rheumatologist or another expert is vital. They can offer a proper diagnosis and start a treatment plan without delay.
What resources are available for individuals with Sjogren's syndrome?
For those with Sjogren's syndrome, there's support available. Organizations like the Sjögren's Foundation and online communities offer information and support. They connect you with others facing similar challenges.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4736702/
- https://www.medicalnewstoday.com/articles/233747
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9610846/
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/diagnosis-treatment/drc-20353221
- https://www.niams.nih.gov/health-topics/sjogrens-syndrome/diagnosis-treatment-and-steps-to-take
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/sjogrens-syndrome/sjogrens-syndrome-treatment
What Causes Sjogren’s Syndrome? Exploring the Underlying Mechanisms
Have you ever wondered why some people suddenly develop dry eyes, a dry mouth, and feel tired all the time? What if your immune system turns against you? These are more than just daily annoyances, they could be signs of something deeper. What causes Sjogren’s syndrome is one of the most asked questions in neurology and immunology clinics, yet most explanations barely scratch the surface.
In this blog, we will break it down in the simplest way possible. We’ll explore what causes Sjogren’s syndrome, the role of your immune system, genes, viruses, hormones, and more. This article is backed by science and simplified by Dr. Chandril Chugh, a board-certified U.S.-trained neurologist who makes complex conditions easy to understand.
Let’s understand what causes Sjogren’s syndrome and why knowing this could change how we diagnose and treat it.
What is Sjogren’s Syndrome?
Sjogren's Syndrome is an autoimmune gland disorder. This means your immune system, which normally protects you, starts attacking healthy parts of your body, especially the glands that make moisture.
- It mostly affects the eyes, mouth, nose, throat, and even internal organs.
- It often comes with dry eyes, dry mouth, tiredness, and joint pain.
- It can show up by itself or along with other autoimmune diseases.
It’s more than just dryness, it can affect your whole body.
A Look at Primary vs Secondary Sjogren’s
There are two main types:
| Type | Description |
|---|---|
| Primary | Happens on its own without other autoimmune diseases |
| Secondary | Happens along with diseases like lupus or rheumatoid arthritis |
Knowing the type helps doctors plan the right treatment.
Prevalence and Who It Affects
- Over 4 million people in the U.S. have it (source: NIH)
- 90% of patients are women
- Most people get diagnosed between the ages of 40 and 60
- It often goes undiagnosed for years
This makes it one of the most common autoimmune gland disorders that people haven’t heard enough about.
What Causes Sjogren’s Syndrome?
Let’s get to the heart of the matter: what causes Sjogren’s syndrome? It’s not just one thing. Doctors believe it’s a mix of genes, immune system problems, environmental factors, and hormones.
Is Sjogren’s Syndrome an Autoimmune Disorder?
Yes, Sjogren’s syndrome immune system behavior is the core issue.
- The body mistakenly attacks glands that produce saliva and tears.
- Immune cells invade these glands and reduce their function.
- This leads to the dry symptoms seen in most patients.
So, when people ask what causes Sjogren’s syndrome, the immune system is the first place to look.
Genetic Factors
There is a clear genetic link to Sjogren’s syndrome.
- Specific genes like HLA-DR and HLA-DQ are more common in patients.
- Family history increases your risk.
- Twin studies show that if one twin has it, the other has a higher chance too.
Genetics alone won’t cause it, but it sets the stage.
Environmental Triggers
Many researchers believe viral causes of Sjogren’s play a key role.
- Viruses like Epstein-Barr virus (EBV) and Hepatitis C may trigger the disease.
- Some bacteria could be involved, but the evidence isn’t as strong.
- The virus may wake up immune cells that then attack the glands.
So, catching certain viruses could be a trigger.
Hormonal Influence
This is why 90% of Sjogren’s cases are in women.
- Hormones, especially estrogen, might protect the glands.
- After menopause, estrogen drops, and symptoms often worsen.
- Some researchers think estrogen helps regulate the immune system.
So, hormones may explain both timing and severity.
Other Risk Factors
Age and other health issues can increase your risk:
- Most people get it between ages 40 and 60.
- Having other autoimmune diseases like lupus or rheumatoid arthritis raises your risk.
- Smoking or chronic stress may make it worse, but they are not direct causes.
These factors don’t cause the disease alone, but they add fuel to the fire.
Is Sjogren’s Syndrome Hereditary?
People often ask: is it passed down in families?
Twin Studies and Family History Insights
- Identical twins show a higher match rate for Sjogren’s.
- If you have a family member with it, you’re at greater risk.
But not everyone with the genes will get the disease.
Differences Between Genetic Predisposition and Actual Onset
- Genes can make you prone to it.
- But something needs to "turn it on" (like a virus or hormone change).
- This is why two people in the same family can have very different health.
Mechanisms Affecting Moisture-Producing Glands
In Sjogren's syndrome, the immune system mistakenly attacks the exocrine glands. These include the lacrimal (tear) and salivary glands. Decreased tears and saliva are the result, leading to dry eyes and dry mouth. The immune system damages the glandular tissue with inflammation, which affects their normal tasks. This causes the dryness symptoms in Sjogren's.
Dysfunction of Lacrimal and Salivary Glands
Faulty immune reactions harm the lacrimal and salivary glands. This damage reduces tear and saliva production. Hence, Sjogren's patients face dry eye and dry mouth problems.
Aquaporin Degradation and Impaired Function
Aquaporins are key for creating tears and saliva. But, in Sjogren's, the body attacks these proteins. This hit affects mainly aquaporin-5 (AQP5), found in these glands. The attack makes tear and saliva production go down, causing the syndrome's dryness.
Inflammation and Glandular Damage
In Sjogren's syndrome, the body's defense system mistakenly attacks its own glands. This leads to the release of substances that cause swelling and harm to the salivary and tear glands. These substances pull in immune system cells. Over time, this ongoing swelling stops glands from working as they should.
Role of Inflammatory Mediators
Sjogren's syndrome pushes the body to make things like cytokines. These substances help kick off swelling and injuries in the mouth and eye glands. They draw in immune cells, such as B and T cells, crowding the glands with them. This swelling is long-lasting and hampers gland performance.
Involvement of Toll-Like Receptors
Toll-like receptors (TLRs) are key in spotting threats and starting the immune response. In Sjogren's syndrome, TLR3 is especially important in starting gland inflammation. By sensing harmful signals from both inside and outside the body, TLRs can make the situation worse. They do this by turning on the production of more swelling substances, worsening gland damage and troubles.
Hormonal Imbalances and Sjogren's Syndrome
Sjogren's syndrome may be linked to not having enough of a hormone called dehydroepiandrosterone (DHEA). This hormone helps control the immune system. If someone with Sjogren's doesn't have enough DHEA, it might lead to immune system problems. Not being able to use DHEA well in the salivary glands could be why this happens.
Dehydroepiandrosterone (DHEA) Deficiency
Research shows that DHEA-S levels are lower in people with Sjogren's compared to those without it. DHEA is important for how our immune system works. If there's not enough DHEA, it might play a part in causing Sjogren's. The salivary glands might not work right with DHEA for those with Sjogren's.
When estrogen levels go down in menopause, the chance of getting Sjogren's might go up. This points to how important hormones are in this disease. On the other hand, since men have more testosterone, and that can turn into a strong hormone called dihydrotestosterone (DHT), they're less likely to get Sjogren's. But, it seems that everyone with Sjogren's doesn't change testosterone to DHT very well. This could also add to the hormone problems in the condition.
Autonomic Nervous System Dysfunction
Sjogren's syndrome is linked to a problem with your body's autonomic nervous system. This system controls things you don't think about, like making tears and saliva. When this system doesn't work right, people with Sjogren's have trouble making tears and saliva.
They often have issues with their blood vessels not reacting as they should. This can make dry eyes and mouth worse. In simple terms, their body doesn't manage these things as it normally would.
Experts have done a lot of research on how Sjogren's affects the autonomic nervous system. They found that many patients in a 2012 study had common problems. These problems were connected to how sick they felt and how active their Sjogren's seemed to be. A later study in 2017 also found issues with the autonomic system in people with Sjogren's.
Looking more closely, Sjogren's seems to affect the heart too. A study in 1998 showed that the autonomic system can mess with how the heart works in Sjogren's syndrome. Similarly, another study in 2000 looked at heart rate changes in these patients.
These studies suggest that people with Sjogren's might have trouble with how their blood vessels work. This could be because their autonomic system isn't managing things correctly. Basically, their body's system for controlling blood flow isn't doing its job right.
Recent research points to bigger health risks from this autonomic imbalance. It could signal problems like heart disease and diabetes. A study in 2015 put a spotlight on these risks. Then, in 2018, researchers did a deep dive into how autonomic dysfunction is tied to Sjogren's disease. They looked at how it connects with the signs of the disease and the body's immune reactions.
Muscarinic Receptor Autoantibodies
In Sjogren's syndrome, the body's defense attacks itself. It makes autoantibodies that target muscarinic acetylcholine receptors. These are found a lot in the salivary and lacrimal glands. The antibodies affect these receptors, leading to dry mouth and eyes.
Anti-Muscarinic Antibodies and Glandular Dysfunction
When looking at people with Sjögren's syndrome, their anti-M3R levels were high. This was more than in healthy people or those with lupus or arthritis.
There was a strong link between how much anti-M3R someone had and the seriousness of their Sjögren's syndrome. More anti-M3R meant a worse condition.
Animal Models of Sjogren's Syndrome
Animal models play a key role in Sjogren's syndrome research. The NOD mouse model stands out. It naturally develops a condition like human Sjogren's, affecting salivary and lacrimal glands.
NOD Mouse Model
The NOD mouse model is invaluable for understanding Sjogren's syndrome. It shows symptoms similar to the human disease. This includes gland damage and autoantibody production, helping scientists explore the disease's roots.
MRL/lpr Mouse Model
Next, the MRL/lpr mouse model is also critical. It mimics systemic autoimmune disorders, like Sjogren's. These mice have gland damage and produce autoantibodies. This model aids in studying genetic and immune system influences on Sjogren's development.
Gene Expression Profiles in Sjogren's Syndrome
Salivary Gland Gene Expression
Experts have checked how genes work in the salivary glands of those with Sjogren's syndrome. This shows the key ways our body's reactions can cause the disease. They found changes in genes linked to fighting off illnesses, swelling, and harming tissue. This helps us see how Sjogren's syndrome messes with the salivary glands.
Peripheral Blood Gene Expression
Furthermore, scientists looked at how genes act in the blood of Sjogren's patients. They found unique signs in the blood that could show disease levels and how it goes forward. Looking at gene activities in both key areas and all through the body offers deep insights into Sjogren's syndrome's causes.
Role of Type I Interferons
New findings show that type I interferons are crucial in the early immune response. They are linked to the development of Sjogren's syndrome. In this condition, Sjogren's patients show a distinct pattern known as an "interferon signature." This means they have more interferon-regulated genes active in their tissues and blood. This overactive immune response likely leads to the damage seen in their glands and the overall dysfunction of the condition.
B-Cell Activating Factor (BAFF)
BAFF Expression in Salivary Gland Epithelial Cells
The B-cell activating factor (BAFF) is important for keeping B cells healthy and active. It's also known as B lymphocyte stimulator (BLyS). In Sjogren's syndrome, BAFF is made too much in the salivary gland cells. This overproduction messes with how BAFF should work, leading to issues with the immune system.
This extra BAFF can make B cells that attack the body live longer and work better. These are common features of Sjogren's syndrome. People with this disease have fewer special memory B cells. Yet, their types of B cells in the blood can help doctors diagnose the illness.
Too much BAFF in the salivary glands seems to make B cells overly active in Sjogren's. This has been shown by other studies. Also, comparing B cell behavior from the blood and salivary glands gives us interesting details about how Sjogren's affects B cells.
Lymphoproliferation and Lymphoma Risk
Sjogren's syndrome can increase the chance of getting lymphoma, a blood cancer. This risk is higher because of the ongoing stimulation of B cells. These cells may change and grow abnormally, leading to lymphoma in some Sjogren's patients.
Prelymphomatous Stages
Sjogren's syndrome's risk of lymphoma is tied to its early stages. In these phases, there is a big growth and change in B cells. This can later turn into lymphoma for a few with Sjogren's. Figuring out how this happens is key. It can help find those at risk and start the right care early.
Association with Hepatitis C Virus
Hepatitis C virus (HCV) infection may also matter for Sjogren's. Many who have symptoms like Sjogren's are found to have HCV. This link hints that viruses might help start or worsen Sjogren's. So, it's critical to check for HCV in those dealing with Sjogren's.
Treatment Implications
It's key to understand Sjogren's syndrome to make better treatments. Scientists are looking at many ways to target the autoimmune issues and poor gland function. They plan to cut down on inflammation, fix how interferon works, slow down B-cells, and more. All this could help lessen how bad Sjogren's is and slow how quickly it gets worse.
Targeting Specific Pathways
For instance, a drug called etanercept can tackle a protein called tumor necrosis factor-alpha (TNF-α). But, studies say it can't stop the interferon signature in Sjogren's patients. This shows the need to dig deeper. We need to find and aim at the pathways most important in causing Sjogren's.
Etanercept and Interferon Pathway Activation
The fact that etanercept doesn't fully stop the interferon signature says a lot. It tells us the interferon pathway might be crucial in Sjogren's. This drives the push for more research. By hitting the main pathways, scientists hope to make treatments that really work, easing symptoms and maybe even turning back the harm of autoimmunity in Sjogren's.
Final Thoughts from Dr. Chugh
As a U.S.-trained neurologist, I’ve seen the confusion and delays people face with this disease. The earlier you understand what causes Sjogren’s syndrome, the better your chances of managing it.
Dry eyes, a tired body, or mouth discomfort may seem minor. But when these persist, they need attention.
If you or someone in your family is showing signs, don’t wait.
Book your consultation with Dr. Chandril Chugh and get clarity on what’s happening inside your body.
FAQ
What is Sjogren's syndrome?
Sjogren's syndrome is when the body's immune system attacks its own cells. This often happens to glands making tears and saliva. It causes symptoms like dry eyes and mouth.
What are the symptoms of Sjogren's syndrome?
The key signs of Sjogren's syndrome are dry eyes and mouth. It happens because the immune system attacks the glands. Joints, lungs, kidneys, and nerves can also be affected.
Who is at risk of developing Sjogren's syndrome?
It's more common in women, usually after they're 40. Risk goes up if you have other autoimmune diseases like rheumatoid arthritis. Being female and older also add to the risk.
What causes Sjogren's syndrome?
Sjogren's is an autoimmune problem with different causes. Genes, hormones, and the environment play a part. They make the immune system harm moisture glands.
How does the immune system contribute to Sjogren's syndrome?
The immune system targets and damages tear and salivary glands in Sjogren's. This causes less tears and saliva, leading to dry eyes and mouth.
What genetic factors are associated with Sjogren's syndrome?
Gene variants, especially in the HLA system, relate to a higher Sjogren's risk. These genes control the immune system's actions.
How does the dysfunction of aquaporins contribute to Sjogren's syndrome?
Aquaporins help make tears and saliva. But in Sjogren's, the body attacks them. This affects how moisture is made, leading to dry eyes and mouth.
What is the role of inflammation in Sjogren's syndrome?
In Sjogren's, the immune system starts an inflammatory reaction. This harms moisture glands. It leads to problems producing saliva and tears.
How do Toll-like receptors (TLRs) influence Sjogren's syndrome?
Some TLRs, like TLR3, start inflammation in Sjogren's. They can make the glands more damaged, worsening the condition.
What is the role of hormonal factors in Sjogren's syndrome?
DHEA, an adrenal hormone, is low in Sjogren's patients. It helps control the immune system. Its drop might make the disease worse.
How does the autonomic nervous system dysfunction affect Sjogren's syndrome?
Sjogren's can mess with the autonomic nervous system. It controls things like tears and saliva. This causes more severe dry mouth and eyes.
What is the role of muscarinic receptor autoantibodies in Sjogren's syndrome?
In Sjogren's, the immune system can make autoantibodies that block muscarinic receptors. These are important for moisture glands. This leads to the dryness in the mouth and eyes.
What are the environmental triggers for Sjogren's syndrome?
Besides genes, infections can start Sjogren's. Viruses like Epstein-Barr and hepatitis C might play a role.
What animal models are used to study Sjogren's syndrome?
The NOD and MRL/lpr mouse models help study the disease. They showcase what happens in Sjogren's accurately - from gland issues to autoantibodies.
How are gene expression profiles used to understand Sjogren's syndrome?
Scientists find Sjogren's clues by looking at genes in saliva and blood. This shows what's going wrong, helping understand the disease better.
What is the role of type I interferons in Sjogren's syndrome?
Interferons, proteins in the immune system, heavily influence Sjogren's. They're in high amounts in patients, possibly causing gland harm.
How does B-cell activating factor (BAFF) contribute to Sjogren's syndrome?
BAFF overactivity in glands is a key part of Sjogren's. It helps B-cells survive and work too much. This might worsen the disease.
What is the link between Sjogren's syndrome and lymphoma?
People with Sjogren's have a higher lymphoma risk. This might be because their immune system is too active, putting them at risk.
How is the treatment of Sjogren's syndrome being targeted?
Scientists are looking into ways to fix key issues in Sjogren's, like too much inflammation and autoimmunity. New treatments are on the horizon.
Source Links
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/symptoms-causes/syc-20353216
- https://www.ncbi.nlm.nih.gov/books/NBK459485/
- https://www.niams.nih.gov/health-topics/sjogrens-syndrome
- https://www.webmd.com/a-to-z-guides/sjogrens-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8863725/
- https://www.ncbi.nlm.nih.gov/books/NBK431049/
- https://versusarthritis.org/about-arthritis/conditions/sjoegrens-syndrome/
- https://www.womensinternational.com/blog/sjogrens-syndrome/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6928446/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9248235/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8350514/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5036946/
- https://www.nature.com/articles/3700173
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4425610/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7338666/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6917337/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3273959/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3778845/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7916411/
- https://www.jrheum.org/content/50/9/1103
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6819875/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998301/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8328496/
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/diagnosis-treatment/drc-20353221
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5410683/
Understand Disease Neurofibromatosis Types: Symptoms, Causes, and Treatment
Neurofibromatosis is a group of three genetic disorders leading to nerve tumors. These types include neurofibromatosis type 1 (NF1), neurofibromatosis type 2 (NF2), and schwannomatosis. NF1, the most common, occurs in 1 out of 2,500 people. NF2 affects fewer people, 1 in 40,000. Schwannomatosis is very rare, seen in 1 out of 40,000 individuals. The range of symptoms of neurofibromatosis is broad, from light skin changes to complex issues. Knowing about each type helps in managing this condition.
Overview of Neurofibromatosis
Neurofibromatosis is a set of genetic issues. It makes tumors grow on nerves all over the body. There are three main types: neurofibromatosis type 1 (NF1), type 2 (NF2), and schwannomatosis. It's key to know the differences for treating these conditions well.
What is Neurofibromatosis Type 1 (NF1)?
NF1 is the most common form, found in about 1 in 2,500 people. It changes the color of skin and causes tumors on nerve tissue. The gene mutation for NF1 is on chromosome 17. It's inherited in an autosomal dominant way. This means each child of a parent with NF1 has 50% odds of getting the gene.
What is Neurofibromatosis Type 2 (NF2)?
NF2 is less common, seen in about 1 in 40,000 folks. It creates noncancerous tumors on nerves affecting hearing and balance. This often leads to issues with both hearing and balance.
Schwannomatosis: A Related Disorder
Schwannomatosis causes noncancerous tumors on nerves and is less common still. It affects an estimated 1 in 40,000 people. Like the other types, it's due to genetic mutations. These mutations make cells grow uncontrollably, forming tumors.
Symptoms of Neurofibromatosis Types
The symptoms of neurofibromatosis look different in everyone. It's key to know the specific signs for each type. This helps doctors diagnose and treat this genetic condition better.
Common Symptoms in NF1
Neurofibromatosis type 1 (NF1) shows itself in many ways. People with NF1 might have light brown spots on their skin, like café-au-lait spots. Besides, they could have bumps on their skin, known as neurofibromas, and show some bone issues.
Kids with NF1 might have a large head and be shorter than usual. Finding these signs early helps with the right care.
Symptoms of NF2
Neurofibromatosis type 2 (NF2) mainly affects the nerves that help with hearing and balance. It brings about benign tumors. These tumors, vestibular schwannomas, can lead to hearing loss and trouble with balance. Because of this, regular check-ups are vital to watch for complications.
Signs of Schwannomatosis
Schwannomatosis causes the noncancerous tumors called schwannomas on nerves outside the brain. These tumors often cause long-term pain. They can impact someone's life greatly. This disorder is different from NF1 and NF2 in its symptoms and causes.
The severity of neurofibromatosis symptoms varies widely, even for those with the same type. Some may have very mild signs, while others face serious health issues. Regular doctor visits and early action are crucial for dealing with this condition.

Neurofibromatosis type Causes and Risk Factors
Neurofibromatosis starts when our genes change. This change messes with how our cells grow. NF1 changes the NF1 gene, lowering cell growth control with less neurofibromin protein. NF2's NF2 gene mutation means less merlin protein, affecting cell growth regulation. Schwannomatosis changes come from errors in the SMARCB1 and LZTR1 genes.
Neurofibromatosis spreads in an "autosomal dominant" way. If a parent has it, their child might get it. They have a 50% chance of getting the problem-making gene. Sometimes, NF1 happens in a family with no past cases.
Genetic Causes of NF1
For NF1, a NF1 gene mistake causes little neurofibromin protein, leading to tumor growth. 30 to 50% of NF1 cases start from a new gene mistake.
Genetic Causes of NF2
NF2 is linked to NF2 gene issues, affecting merlin's job in limiting tumor grow. Half of NF2 cases are from a parent. But, many cases start fresh without a family link.
Autosomal Dominant Inheritance Pattern
How NF1 and NF2 spread is called "autosomal dominant." It needs one gene change to show up. Yet, 85% of schwannomatosis cases have no known gene issue.
Having a family with neurofibromatosis raises your risks too. Yet, it can happen even without a family history. This condition leads to problems like losing your hearing, never-ending pain, and a higher chance of getting some cancers.
Diagnosis and Diagnostic Criteria
Diagnosing neurofibromatosis usually involves looking at specific signs. For NF1, doctors check if a person has some key features. These include spots like birthmarks, and freckles in certain areas. They also look for lumps under the skin, tumors on the nerve of the eye, small bumps in the iris, suspicious bone growth, and a family history.
Diagnostic Criteria for NF1
The National Institutes of Health set the rules for diagnosing NF1. They look for things like the coffee-colored spots and skin bumps. Also, lumps under the skin, eye nerve tumors, eye spot bumps, odd bone growth, and family connections help determine a diagnosis. By the age of eight, about 97 percent of people are identified with NF1 based on these signs.
Diagnostic Criteria for NF2
For NF2, doctors check for specific types of tumors. If someone has a tumor on both nerves for hearing and balance, it's a sign. Or, if a close family member has NF2, and the person has a tumor on one hearing and balance nerve or other specific tumors, it helps in the diagnosis. MRI scans are usually needed to spot these tumors.
Diagnostic Criteria for Schwannomatosis
Schwannomatosis is diagnosed when someone has at least two of the same type of tumors. Doctors also must rule out other conditions by checking for specific gene changes. A blood test can confirm NF2 in many cases. But, sometimes, even when a test is negative, the disease could still be schwannomatosis.
Treatment and Management Options
While there's no cure for neurofibromatosis, there are treatment and management options. These help patients deal with symptoms and prevent or treat complications. How treatment is approached depends on the type of neurofibromatosis and the person's needs.
Treatment for Children with NF1
Kids with NF1 need regular check-ups and close symptom monitoring. For any developmental or learning issues, early action is key. Medications can help with symptoms like ADHD or seizures. Surgery might be needed to address larger or symptomatic tumors.
Treatment for Adults with NF1
For adults with NF1, yearly check-ups are important. They should closely watch for certain problems like scoliosis and cancer. Medications and surgery can help manage and address symptoms, with a focus on improving life quality.
Management of NF2 and Schwannomatosis
People with NF2 or schwannomatosis often need MRI scans to watch tumor growth. Treatment might include surgery, radiation, or targeted drugs. The plan is based on tumor size and location, plus the individual's health and symptoms.
The main goal for treating and managing all forms of neurofibromatosis is to help patients live better lives. This involves regular check-ups, early intervention, and support services for those dealing with this genetic condition.
Complications of Neurofibromatosis
Neurofibromatosis can bring many issues, from learning disabilities to attention problems and seizures. It also includes skeletal issues like scoliosis and brittle bones. People with it may have vision and hearing issues, high blood pressure, and a higher cancer risk.
Most growths from neurofibromatosis are noncancerous, but some turn cancerous. The effects can range from minor to serious. Regular medical checkups are vital to stay on top of the condition.
Those with neurofibromatosis have a bigger chance of getting cancer. This includes cancers of the breast, blood, colon, brain, and soft tissues. Brain tumors affecting 15% with NF1 are also seen, with different types such as astrocytoma and optic pathway glioma.
About 65% of people with NF face learning problems and ADHD. Early help with learning and educational support is key. Conditions like scoliosis and frail bones need watchful care too.
Many experience only mild symptoms needing no treatment. But, the risk of severe issues means staying on top of your health is crucial. Good medical care and regular checks can help manage the condition and improve life quality.
Incidence and Prevalence
Neurofibromatosis is a rare genetic disorder. It has different types with varying rates. NF1 is the most common, with about 1 in 2,500 people affected. The studies screening for NF1 found it in 1 in 2,020. However, medical records showed a lower rate, 1 in 4,329.
On the other hand, NF2 is less common, affecting around 1 in 40,000. Schwannomatosis is the rarest, hitting 1 in 40,000. This shows their rarity compared to NF1.
NF1's birth incidence is noteworthy, at 1 in 2,662. Its prevalence, however, is even higher, at 1 in 3,164. This means many more people might have it than those born with it.
The disorder passes from parents to children with a 50% chance. Yet, in half the cases, the mutation happens without a family history.
Resources for Neurofibromatosis Support
If you or someone you care about has been diagnosed with neurofibromatosis, there's help and education available. One key place to start is the Children's Tumor Foundation. They work hard to fight this disease through research and spreading awareness. Another great resource is the Neurofibromatosis Network. They offer tons of support, education, and information for those affected.
If you specifically have Neurofibromatosis Type 2 (NF2) or schwannomatosis, check out the Acoustic Neuroma Association and the British Columbia Neurofibromatosis Foundation. They provide focused help and link you with experts and support groups. They make it easier to handle the unique issues these conditions bring.
There are also big medical places like Harvard Medical School and Johns Hopkins Hospital that offer support for those with neurofibromatosis. They share many resources, from learning about the disease and clinical trials to dealing with its genetic aspects. They also help with financial needs, offer government resources, and support mental health and hearing issues.
The Neurofibromatosis Midwest is a great organization too. You can find lots of info about clinics, awareness campaigns, and the latest research. They provide educational help and support services for those with neurofibromatosis. The National Cancer Institute, National Institutes of Health, and American Brain Tumor Association are also crucial support sources for patients and their families.
Conclusion
Neurofibromatosis is a genetic disorder with three main types. These are NF1, NF2, and schwannomatosis. Each type has its own symptoms and causes. Knowing about them helps manage the disease better.
People with neurofibromatosis should get checked often by a doctor. It's also important to start treatment early. Having support helps both the affected person and their family.
Better treatment and understanding of neurofibromatosis give hope. The community is working hard to improve care. They hope to make life better for those with this condition.
Healthcare pros, researchers, and support groups are teaming up. They want to offer the best care. Staying informed and managing the disease is key. This helps people and their families face the challenge with strength.
FAQ
What is neurofibromatosis and what are its main types?
Neurofibromatosis refers to three genetic disorders. They cause tumors on nerves. The main types are NF1, NF2, and schwannomatosis.
What are the symptoms of the different types of neurofibromatosis?
NF1 causes light brown skin spots, freckles in armpits and groin, and small skin bumps. It also leads to bone issues. NF2 results in hearing and balance problems due to tumors on nerve controls. Schwannomatosis causes chronic pain from nerve tumors.
What causes neurofibromatosis?
Genetic mutations affecting proteins that control cell growth are behind neurofibromatosis. NF1 links to mutations in the NF1 gene. NF2 links to NF2 gene mutations. Schwannomatosis usually involves mutations in the SMARCB1 and LZTR1 genes.
How is neurofibromatosis diagnosed?
Diagnosis is based on certain signs. NF1 includes café-au-lait spots and neurofibromas. NF2 needs vestibular schwannomas or certain symptoms. Schwannomatosis is diagnosed with two or more schwannomas and no NF2 gene mutations.
What are the treatment and management options for neurofibromatosis?
Even though there's no cure, management options exist. For NF1 children, regular check-ups and early actions are key. Medications and surgeries can help. Adults with NF1 need annual checks. People with NF2 or schwannomatosis might need surgeries, radiation, or MRI scans.
What are the potential complications of neurofibromatosis?
Neurofibromatosis can lead to various problems. These include nerve, bone, vision, and heart issues. There's also a small risk of certain cancers.
What is the incidence and prevalence of neurofibromatosis?
NF1 is common, affecting about 1 in 2,500 people. NF2 is less common, affecting roughly 1 in 40,000. Schwannomatosis is the rarest, also affecting 1 in 40,000.
What resources are available for individuals and families affected by neurofibromatosis?
Several groups offer support, including the Children's Tumor Foundation and the Neurofibromatosis Network. They provide help, education, and resources for those with neurofibromatosis.
Source Links
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Neurofibromatosis
- https://www.ncbi.nlm.nih.gov/books/NBK459329/
- https://medlineplus.gov/genetics/condition/neurofibromatosis-type-1/
- https://www.ninds.nih.gov/health-information/disorders/neurofibromatosis
- https://nyulangone.org/conditions/neurofibromatosis/diagnosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8354850/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/neurofibromatosis/neurofibromatosis-type-1
Effective Lumbar Radiculopathy Treatment Options
Lumbar radiculopathy, or sciatica, affects around 5% of Americans. It is when a spinal nerve root is compressed or irritated. Thankfully, many treatments can help without needing surgery. We'll look at the options to treat lumbar radiculopathy.
This issue often starts in midlife. Men in their 40s and women in their 50s and 60s are usually affected. Women in hard-working jobs have a higher risk, while there's more men in the general population. Degenerative spondyloarthropathies cause this problem.
We have many ways to treat lumbar radiculopathy. Both simple methods and more serious procedures can help. We'll talk about how to find out what's causing the issue, what basic treatments to try first, and what to do if those don't work.
Understanding Lumbar Radiculopathy
Lumbar radiculopathy happens when a nerve in the lower back gets pressed or irritated. A herniated or bulging disc and bone spurs are common causes. This issue is also known as sciatica. It causes pain, numbness, and weakness in the lower back, hips, and legs.
Causes and Risk Factors
Causes for this condition include issues like disc herniation or arthritis. It's often linked to getting older. Being overweight, sitting or standing badly, and heavy jobs make it more likely. In some cases, women with tough jobs, like in the military, have a greater risk.
Symptoms and Clinical Presentation
This problem usually starts in midlife. Men in their 40s and women in their 50s and 60s are more often affected. Signs include back pain, leg pain, and numbness. Muscle weakness can also happen. Where the symptoms show up depends on which nerve root is affected. The lower back is usually the main area affected.
Diagnostic Workup
Diagnosing lumbar radiculopathy starts with a detailed look. Your healthcare provider will check your muscles and how you feel things. They'll also test your reflexes to see how your nerves are doing. This physical exam is key to figuring out what's wrong.
Imaging Tests
Imaging tests like MRIs or CT scans help find where the nerve is getting pressed. MRIs are best for looking at nerve problems from herniated discs. But, if your symptoms are very serious, you might need an MRI right away. This could be if you can't control your bowels or bladder, or if a tumor is suspected.
CT scans are great for seeing the bones, but not so much for soft tissue like discs. A myelogram, where they put dye in your spine, is done when surgery might be needed. This test is for people whose condition is getting worse, and other tests haven't helped much.
Electrodiagnostic Studies
Tests like EMGs and nerve studies show if radiculopathy is present and where. They look at how well your muscles and nerves are working. These tests are key, especially if the imaging tests don't give a full answer.
Your healthcare provider will use a mix of exams and tests to figure everything out. With the right information, they can make a clear diagnosis. Then, they can decide on the best plan to help you.
Conservative Treatment Approaches
Managing lumbar radiculopathy often starts with non-surgical methods. These treatments focus on the cause and offer relief without surgery. Let's look at some top conservative ways to treat lumbar radiculopathy.
Physical Therapy and Exercise
Physical therapy and specific lumbar radiculopathy exercises are crucial for treating lumbar radiculopathy conservatively. This helps strengthen spine-supporting muscles, boost mobility, and cut down nerve irritation. Your physical therapist might craft a program with stretching, core work, and posture correction. These can ease your symptoms and ensure a healthier back for the long term.
Medication Management
Medications also have a big role in conservative lumbar radiculopathy treatment. Anti-inflammatory drugs, muscle relaxants, and pain relievers can ease symptoms and inflammation. Make sure to talk with your doctor about your medicine plan to avoid side effects from long-term use.
Alternative Therapies
Some folks might get relief from alternative therapies for lumbar radiculopathy. Acupuncture, chiropractic care, electrical stimulation, and meditation could help reduce its impact for some. While their success varies, these methods might be useful when part of a broader treatment plan.
Working closely with your doctor is key for managing lumbar radiculopathy conservatively. By combining physical therapy, medication, and alternative treatments, you can often get relief without surgery.
Epidural Steroid Injections
Epidural steroid injections are often used to help with lumbar radiculopathy. They place anti-inflammatory medicine right where it's needed. This can cut down on swelling and ease the pain. In the initial stage of lumbar radiculopathy, these injections work well. They're a good option to try before considering surgery.
Doctors have been using epidural steroid injections for sciatica since the 1930s. The method to treat back pain with these injections was first described in 1953. Over time, these injections have gained popularity as a way to manage lumbar radiculopathy.
But, there is a chance that the medicine might not reach the right spot in about 30% of cases. This happens with injections done without imaging guidance. Using imaging for the injections ensures the medicine hits the exact spot. This gives the best results and helps doctors check if the injection worked.
A traditional type of epidural injection shows success about 69.2% of the time. A different method, called the preganglionic approach, works about 90% of the time. The difference in how well these two methods work is almost significant, with a p-value of 0.056.
Medical research shows that lumbar epidural injections may reduce pain for less than three months. But, a transforaminal epidural spinal injection (TFESI) might offer pain relief for up to 20 months. The success rate for TFESI is around 75.4%.
Comparing the two, studies find that TFESI is better than the blindly done interlaminar approach at different times. Injections through the foramina have shown to be more effective. They work better than blind interlaminar injections and the caudal method when guided by fluoroscopy.

Overall, epidural steroid injections can greatly help with managing lumbar radiculopathy. They are most effective when combined with other treatments. Always remember, choosing imaging-guided injections can make a big difference. It ensures the medicine reaches the right place, giving the best possible result.
Trigger Point Therapy
Trigger point therapy aims to relieve pain in those with chronic lumbosacral radiculopathy. It focuses on treating specific spots of muscle tightness, known as trigger points. These areas often worsen the symptoms of trigger point therapy for lumbar radiculopathy. This method aims to reduce pain and boost function for these patients.
A recent study showed positive results. Within 10 days, patients felt less pain after receiving trigger point injection therapy. This means that using trigger point therapy for lumbar radiculopathy as part of a larger treatment plan could be very helpful.
It's important to know that trigger point therapy for lumbar radiculopathy is not a cure-all. But, it can complement other treatments like physical therapy and medications. By discussing this option with your doctor, you can see if it's right for you and your symptoms.
Lumbar radiculopathy treatment
If simple treatments don't work well enough, doctors might look at more intense ways to handle lumbar radiculopathy. There are things they can do before surgery. For example, epidural steroid injections and trigger point therapy can help a lot. But sometimes, surgery becomes the best option.
Non-Surgical Options
Options like epidural, facet, and transforaminal injections can ease symptoms for quite a while. These treatments help with inflammation and stop nerve irritation. Many people see big improvements from them.
Surgical Interventions
If things don't get better after four to eight weeks of trying other treatments, surgery can be considered. Operations like discectomy, laminectomy, and spinal fusion are common for lumbar radiculopathy. A big research study called the Spine Patient Outcomes Research Trial (SPORT) showed surgery might work better than non-surgical methods, but not always by a lot.

Postoperative Care and Rehabilitation
After surgery for lumbar radiculopathy, patients need a careful recovery plan. This plan includes making changes to their daily activities to prevent harm. They also start a physical therapy plan to get stronger and move better. It's very important for the patients to follow this plan to heal well and stop the problem from coming back.
Activity Modifications
Right after spine surgery, patients must be careful with their movements. They can't bend, twist, or lift things, and they should learn to move carefully in bed. These rules help the surgical area heal properly. Sometimes, patients might need to wear a special support device after surgery, depending on what their doctor thinks is best for them.
Physical Therapy and Exercise
Getting physical therapy is key after surgery for lumbar radiculopathy. This program is focused on becoming strong, flexible, and learning the right ways to move. Patients will do exercises that make their core and back muscles stronger. They'll also learn to be more flexible and keep their balance. Doing all this helps the patient in the long run and decreases the chance of the problem happening again.
Preventing Recurrence
To stop lumbar radiculopathy from coming back, we need to work on risk factors and change our lifestyle. First, keep a healthy weight. Then, focus on your posture and how you sit and stand at work or home. Also, do some regular exercise. This will make your core and back muscles stronger. It lowers the chance of nerves getting pinched. Over time, this can lessen the pain of lumbar radiculopathy.
Lifestyle Changes
Changing how you live can do wonders in keeping lumbar radiculopathy away. Here’s what you should do:
- Maintain a healthy body weight with good food and staying active
- Stop smoking, it's bad for your back
- Add stretching and strength exercises to your day to make your body more flexible and strong
- Keep up with good posture at work and at play
- Don’t sit still for too long. Take breaks to move around
Ergonomic Adjustments
Changing how you set up your work and home can also help keep lumbar radiculopathy away. Here's how:
- Make sure your workstation is right for you. Use furniture and tools that can be adjusted for better posture
- Take short breaks to move. Sitting or standing too long can bother your nerves
- Use tools meant for good posture, like lumbar supports or standing desks, to help your lower back
- Avoid movements that stress your back, like lifting, bending, and twisting too much
By making these changes in lifestyle and how you set up your space, you can avoid lumbar radiculopathy from coming back. You can have less pain and more freedom from this tiring issue.
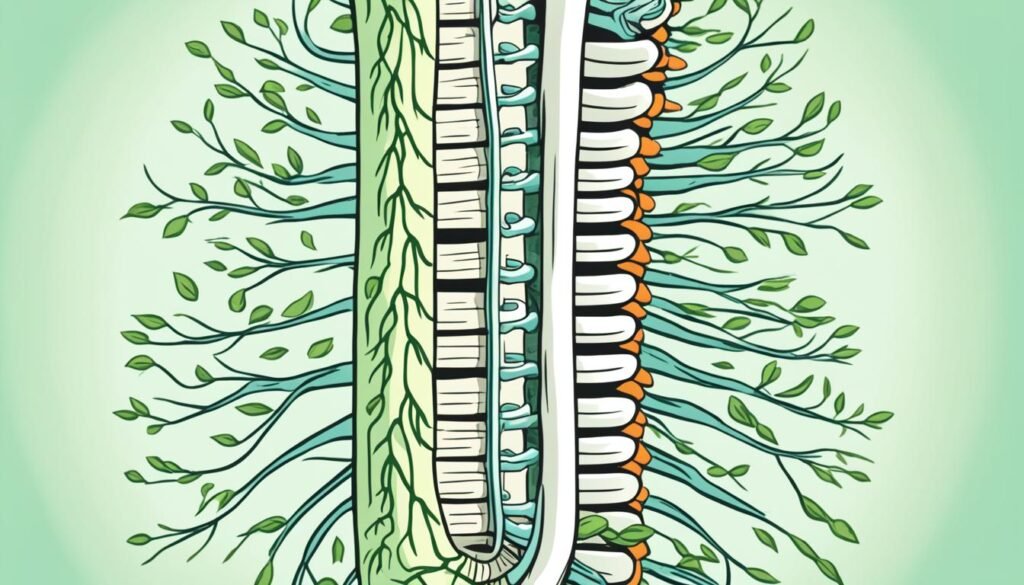
When to Seek Medical Attention
Many cases of lumbar radiculopathy can be treated with basic care. But, some symptoms can be very serious. They need quick medical attention. These include bad motor problems, cauda equina syndrome, and signs of nerve issues.
If these symptoms come on strong, you must see a doctor fast. This could stop more problems and help you heal better.
Red Flag Symptoms
If you notice any of the red flag symptoms for lumbar radiculopathy, get to a doctor right away:
- Severe or progressive muscle weakness in the legs
- Difficulty walking or standing
- Loss of bowel or bladder control (cauda equina syndrome)
- Significant numbness or tingling in the legs or genital area
- Sudden onset of severe pain that is not responding to conservative treatments
These symptoms needing fast medical attention for lumbar radiculopathy could point to severe issues. You should not wait to call your doctor if you notice them.
Conclusion
Lumbar radiculopathy is a common issue that can really affect someone's life. Luckily, treating it has a lot of effective options. These range from simple treatments to more complex ones.
Working closely with a healthcare provider is key. They can help build a treatment plan just for you. This approach can help ease the pain, make things better, and stop the problem from coming back. Early treatment is important for the best results.
There are many paths to treat this condition. These include things like physical therapy, using medicines, and even surgery. By knowing what's causing the issue and its signs, you play a big role in your treatment. You can make choices that suit your needs best. This can improve your life a lot.
Choosing care early is crucial. The right mix of treatments can really help. It may ease the pain, help you move better, and keep the issue from happening again.
FAQ
What is lumbar radiculopathy?
Lumbar radiculopathy is when a spinal nerve in your lower back gets compressed. This compression is usually from a herniated disc or bone spurs. You might feel pain, numbness, or weakness in your back, hips, and legs.
What are the common symptoms of lumbar radiculopathy?
People with lumbar radiculopathy often feel back pain and leg pain. They might also have numbness or weakness. The exact symptoms can change based on which nerve is affected.
How is lumbar radiculopathy diagnosed?
Doctors start by doing a full body check to find out what's wrong. They will check your muscles and how well you can feel things. They might also do tests like MRIs or CT scans. These can show what's pressing on your nerve.
Other tests, like EMGs, can check your nerve functions. All of this helps to name the condition and figure out how to treat it.
What are the first-line treatment options for lumbar radiculopathy?
The first treatments usually don't involve surgery. They include physical therapy, exercises, and medications. People might also try things like acupuncture or chiropractic treatments.
What is the role of epidural steroid injections in the management of lumbar radiculopathy?
Epidural steroid injections can help a lot. They put anti-inflammatory medicine right where you need it. This can cut down on swelling and help with pain, especially at the start of the condition.
How does trigger point therapy help with lumbar radiculopathy?
Trigger point therapy targets tight muscle spots with hands-on work or shots. It can make pain better for a short time in people with lumbar radiculopathy. This method might be used together with other treatments.
When is surgical treatment considered for lumbar radiculopathy?
If the first treatments don't help enough, surgery might be an option. Doctors could do procedures like discectomy or spinal fusion. These aim to solve the main issue causing the nerve pressure and give lasting relief.
What is the importance of postoperative care and rehabilitation for patients with lumbar radiculopathy?
After surgery, patients need careful care and rehab. They might have to change how they do some activities. A lot of focus will be on exercises that build strength and flexibility. Following this plan closely is key to doing well long-term and avoiding the problem coming back.
How can recurrence of lumbar radiculopathy be prevented?
To keep lumbar radiculopathy from coming back, it's important to work on your health. You should keep a good posture, stay at a healthy weight, and exercise your core and back. These things help prevent further nerve compression.
When should you seek immediate medical attention for lumbar radiculopathy?
"Red flag" symptoms like bad motor problems or bladder trouble need quick medical help. If you're seeing signs like these, it's important to see a doctor right away. They can prevent worse issues and help you recover better.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6858271/
- https://emedicine.medscape.com/article/95025-treatment
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/radiculopathy
- https://www.uptodate.com/contents/acute-lumbosacral-radiculopathy-treatment-and-prognosis
- https://emedicine.medscape.com/article/95025-workup
- https://comprehensivespine.weillcornell.org/conservative-treatment-versus-surgery-for-lumbosacral-radiculopathy-with-muscle-weakness-and-loss-of-reflexes/
- https://www.atlasneurosurgery.com/blog/7-treatments-for-lumbar-radiculopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2667591/
- https://my.clevelandclinic.org/health/treatments/22091-lumbar-epidural-steroid-injection
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3265586/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4199211/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5913013/
- https://www.brighamandwomens.org/assets/BWH/patients-and-families/rehabilitation-services/pdfs/operative-spine-acute-bwh.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7170616/
- https://www.choosept.com/guide/physical-therapy-guide-lumbar-radiculopathy-sciatica
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10888666/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10878111/
- https://www.healthline.com/health/lumbar-radiculopathy
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/sciatica-and-radiculopathy-peculiar-names
Understand Lumbar Radiculopathy: An Overview
Lumbar radiculopathy brings pain, numbness, and weakness to the lower back and legs. It's a common issue seen by spine surgeons. About 3-5% of people might experience it.
This condition is mainly due to compressed or irritated nerve roots in the lower back. This can happen because of various issues like herniated discs or bone spurs.
Symptoms include sharp pain, burning feelings, or numbness that spreads down the leg. Proper diagnosis and treatment are key to helping patients feel better.
What is Lumbar Radiculopathy?
Lumbar radiculopathy is a condition where a nerve root in the lower back is squeezed or irritated. This causes pain, numbness, and weakness down the leg. Patients often say the pain feels like electric shocks or burning.
Definition and Symptoms
Radiculopathy means pain spreads down the legs. A main reason for this may be something pressing on a nerve. In the lower back, this can happen where the nerve exits the thecal sac or as it goes through other areas.
Causes of Lumbar Radiculopathy
Many things can lead to lumbar radiculopathy. This includes disc problems, spondylolisthesis, and even cancers. As we grow older, our spines can wear down. This can cause problems like disc bulging or bone spurs, which squeeze nerves.
Infections and growths on the spine can also cause this condition. However, these are not as common.
Diagnosis of Lumbar Radiculopathy
The journey to diagnose lumbar radiculopathy starts with a thorough physical exam. This exam checks your muscles, your sense of feeling, and how your reflexes react. Doctors will also perform a special test called Lasegue's sign.
The test is done while you're lying down. Your leg is straight, with the knee stretched, and the head slightly bent forward. The doctor lifts your leg slowly. If you feel pain that shoots down your leg, it's a sign of lumbar radiculopathy.
Imaging Tests
For a closer look, doctors use MRI scans of your lower back without contrast. These images are great for spotting any nerve compression. If they suspect conditions like a tumor, an infection, or if you had surgery before, they might use a contrast dye during the MRI.
Electrodiagnostic Studies
Electrodiagnostic tests, tests like EMG and NCV, are sometimes needed. These tests help the doctor tell if it's radiculopathy or a different peripheral nervous system issue.
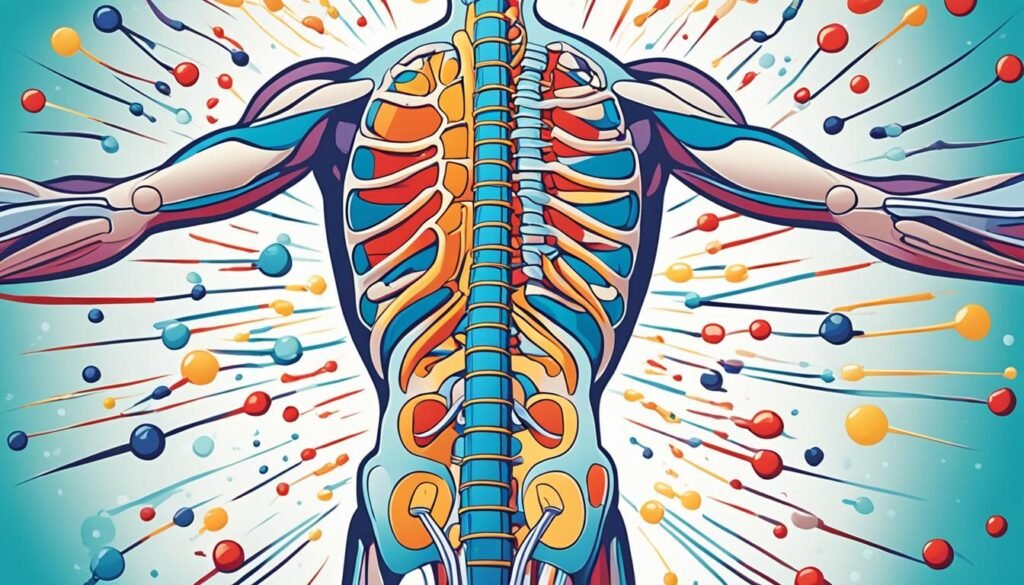
Non-Surgical Treatment Options
Many patients start with non-surgical ways to treat lumbar radiculopathy. They learn about it, do exercises, and stay active. Things like McKenzie exercises can help ease the symptoms at first.
Patient Education and Exercise
Teaching patients about their condition and staying active is key. They learn about their spine and what's causing the issue. They also learn how lumbar radiculopathy exercises can lessen the pain. For activities, they are advised to try walking, swimming, or using the elliptical. These can strengthen their back and core.
Medications and Pain Injections
Doctors might prescribe drugs like NSAIDs or oral steroids to reduce pain and swelling. They can also use injections, like epidurals, to reduce symptoms for a while. These shots often include an anti-inflammatory and a pain blocker.
Surgical Decision-Making
When treatments that aren't surgery don't help, surgery can be looked at for lumbar radiculopathy patients. The period usually takes between four to eight weeks. This time allows for trying other ways to get better without surgery first.
Timing for Surgery
Deciding on surgery means looking at when the patient started feeling bad and how long that's been. It's best to wait four to eight weeks after trying things that aren't surgery. This gives enough time to see if the patient gets better without an operation.
SPORT Trial Findings
The SPORT trial looked at 501 people with herniated lumbar discs, comparing surgery to non-surgery. Both groups got better a lot in two years, but surgery's results were a bit better. However, the difference wasn't big enough to be sure.
What's important is that the SPORT trial talked about when surgery might be better than other treatments for some people.
Lumbar Radiculopathy Causes
Changes in tissues around the nerve roots often cause lumbar radiculopathy. This changes can make the spaces for nerve roots narrow. One common cause is a bulging or herniated disc. It happens when a spinal disc moves out of place or gets damaged, putting pressure on the nerves.
Herniated Discs
Herniated discs often lead to lumbar radiculopathy. When the interior of a disc bulges or ruptures through, it presses on nerve roots. This pressure causes pain, numbness, and tingling in the lower back and legs.
Bone Spurs
Bone spurs, which are extra bone growths, can also cause lumbar radiculopathy. They grow in certain areas, narrowing the foramina. This can then compress the nerve roots, leading to symptoms of radiculopathy.
Other Causes
Less common causes of lumbar radiculopathy include spinal ligaments getting thicker. Spinal infections and cancerous or noncancerous growths in the spine can also press against nerve roots.
Radiculopathy vs. Other Conditions
Radiculopathy can be tough, but knowing how it's different from other issues is key. It often links to myelopathy, where the spinal cord is compressed. This happens when discs push on both nerve roots and the spinal cord. It causes severe problems like trouble walking, bad coordination, and even paralysis.
Radiculopathy's symptoms might mix up with peripheral neuropathy's, like in carpal tunnel syndrome. The crucial difference is that radiculopathy is pinching at nerve roots. But peripheral neuropathy hurts nerves in other parts of the body. Seeing a spine specialist is crucial to tell these issues apart and get the right diagnosis.
Surgical Treatment Options
When other treatments don't work, some people might need surgery for lumbar radiculopathy. The main aim of surgery is to lessen the pressure on the nerve. This is done by making more space where the nerve roots leave the spine. It might mean taking out some of a disc or vertebrae to help the nerve heal.
A cervical posterior foraminotomy is a less invasive surgery. It helps by taking out bone or disc material to ease the pressure on the nerve. The type of surgery performed depends on what’s causing the radiculopathy. It also depends on what the patient needs.
There are different surgeries available for lumbar radiculopathy. These include discectomy, laminectomy, and fusion surgeries like posterior spinal fusion. Microdiscectomy is seen as the best for those with disc herniation only.
People who undergo less invasive surgeries might leave the hospital on the same day or within 24 hours. Those needing more complex fusion surgeries tend to stay longer, maybe 2 to 4 days.
Although surgery can really help some people, there are risks. This includes things like infection, nerve damage, and not fully healing after. The time it takes to recover can also vary, from 4 to 12 weeks.
Prevention and Risk Factors
Preventing lumbar radiculopathy is not always guaranteed. But, you can lower your risk by staying healthy. This means keeping your weight in check and being physically active. These habits reduce spine strain and your chance of getting herniated discs or bone spurs. Also, having good posture and lifting correctly can keep you from hurting your back.
Getting older is also a big risk for lumbar radiculopathy. The condition is often linked to the spine getting worn over time. Symptoms usually start in midlife, hitting men in their 40s and women from their 50s onwards. Women in jobs that are physically tough, like military service, face even more risk.
The main culprit behind lumbar radiculopathy is degenerative spondyloarthropathies. These issues can compress or irritate nerves in the lower back. Knowing these risk factors, you can act to lower your risk. Stay active, keep your weight steady, and be careful with your back to avoid this tough condition.
Anatomy and Pathophysiology
The spine is made of many vertebrae, with a spinal cord in the center. Nerve roots move out and go between the vertebrae to parts of the body. When these roots are squeezed or hurt, it causes radiculopathy. This can happen in the lower back, causing pain, numbness, and weakness in the leg. This is known as lumbar radiculopathy.
Compression might happen inside the thecal sac, when the root leaves it, as it goes through the foramina, or after it leaves. Pushing on the nerves from things like disc problems or bone spurs is usually why this happens.
Studies suggest that lumbar radiculopathy can come from problems with blood flow to the nerves. This can lead to less electrical signals moving through the nerve roots. It takes a lot of pressure to slow these signals down at first but not so much over time.
Less blood flow and trouble getting nutrients to nerve tissue can make the nerves not work right. Even a little bit of pressure can slow down the blood moving through the nerves. But, pressure by itself isn't always the main reason for the pain in lumbar radiculopathy.
If nerves are pressed at two spots, it affects them more than if it's just in one place. This means less blood flow and fewer nutrients can make the nerves work even worse. And that can cause problems in lumbar radiculopathy.
Epidemiology and Prevalence
Lumbar radiculopathy is a big issue for spine surgeons, affecting 3-5% of people. It's common in both men and women, and age plays a big role. It often happens as we get older due to issues in the spine. Symptoms usually start in midlife. Men may start feeling them in their 40s, while women feel them a bit later, in their 50s and 60s.
In general, men are more often affected by lumbar radiculopathy. But, females have a higher risk in some groups, like those with tough jobs. The main cause is degenerative spondyloarthropathies. This can squeeze or irritate the nerve roots in your lower back.
Conclusion
Lumbar radiculopathy is a common problem that mainly affects the lower back and legs. It causes pain, numbness, and weakness. This issue happens when a nerve root in our lower back gets compressed or irritated. This can happen for various reasons like herniated discs, bone spurs, or other spinal problems.
It is important to catch and treat this early, offering relief. Doctors often start with treatments that don't involve surgery. But sometimes, surgery is the best option.
By knowing why lumbar radiculopathy happens and how to treat it, doctors can help their patients better. This condition affects about 3%-5% of people, and it is more common as we get older. Women in physically demanding jobs face a higher risk. But usually, men are more likely to have this problem.
In the end, dealing with lumbar radiculopathy early is key. Good care from the beginning can really make a difference. With patients and doctors working together, we can improve life quality and solve this issue effectively.
FAQ
What is lumbar radiculopathy?
Lumbar radiculopathy happens when a nerve in your lower back gets pressed or irritated. This causes pain, numbness, and weakness in the leg.
What are the common causes of lumbar radiculopathy?
The top reasons for lumbar radiculopathy are herniated discs, bone spurs, and other spine issues. These can press or irritate the nerve roots in the lower back.
How is lumbar radiculopathy diagnosed?
To diagnose lumbar radiculopathy, doctors do a physical exam and use imaging tests like MRI. Sometimes they do electrodiagnostic studies as well.
What are the non-surgical treatment options for lumbar radiculopathy?
At first, treatment aims to avoid surgery. This can include learning about the condition, keeping active, doing certain exercises, taking meds, and getting pain shots.
When is surgical intervention considered for lumbar radiculopathy?
If other treatments don’t work after 4-8 weeks, surgery might be an option. The surgery type depends on what's causing the issue and what works best for you.
How is lumbar radiculopathy different from myelopathy and peripheral neuropathy?
Radiculopathy is the nerve roots being pinched. Myelopathy is the spinal cord itself getting compressed. Peripheral neuropathy is when nerves outside the spinal cord get damaged.
Can lumbar radiculopathy be prevented?
It's hard to always prevent lumbar radiculopathy. But, keeping a healthy weight, sitting and standing right, and lifting correctly can lower your odds of getting it.
What is the prevalence of lumbar radiculopathy?
Many people see a spine surgeon because of lumbar radiculopathy. It's believed to affect 3-5% of people.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6858271/
- https://www.ncbi.nlm.nih.gov/books/NBK430837/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/radiculopathy
- https://my.clevelandclinic.org/health/diseases/22564-radiculopathy
- https://www.atlasneurosurgery.com/blog/5-nonsurgical-treatments-for-lumbar-radiculopathy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10888666/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7080952/
- https://www.sciencedirect.com/science/article/abs/pii/S1356689X14001386
- https://www.neuroendomke.com/spine-conditions-and-treatments/lumbar-radiculopathy/
- https://www.cortho.org/spine/sciatica/sciatica-surgical-treatment/
- https://www.wheelessonline.com/issls/section-2-chapter-8-pathophysiology-of-lumbar-radiculopathy/
- https://www.ncbi.nlm.nih.gov/books/NBK546593/
- https://emedicine.medscape.com/article/95025-overview
Top Lumbar Radiculopathy Exercises for Pain Relieve
Feeling constant lower back pain? The issue might be lumbar radiculopathy, or sciatica. This condition involves damage or injury to your nerve roots. It's often referred to as a pinched nerve and causes tingling and burning pain. The lower back area is known as the lumbar region. Experiencing radiculopathy here can lead to hard-to-handle symptoms like unending pain and numbness.
Physical therapy is a strong option for treatment. There are specialized exercises aimed at helping with lumbar radiculopathy. Doing these lumbar radiculopathy exercises can improve your situation before you see your physical therapist.
Learning the best exercises for lumbar radiculopathy means you can play a big part in your healing process.
What is Lumbar Radiculopathy?
Lumbar radiculopathy, or sciatic neuritis, is a condition that comes from a pinched nerve or herniated disc. But it can also be caused by other things. People often feel weak or have pain, numbness, or tingling. They can mistake it for lower back or leg pain.
Causes of Lumbar Radiculopathy
There are many possible causes for lumbar radiculopathy. These include spinal stenosis, herniated discs, or bone spurs. Others are infections, myelopathy, degenerative disc disease, or spondylolisthesis. It can also happen from a trauma or injury.
Symptoms of Lumbar Radiculopathy
People with lumbar radiculopathy may feel weak, have pain, or experience numbness. They can also feel a tingling sensation. These issues often affect the lower back, buttocks, or legs.
Benefits of Exercises for Lumbar Radiculopathy
Working out can really help with lumbar radiculopathy, or sciatica. This includes exercises that build your core or make you more flexible. Researchers have seen that they can lower pain and boost how well you can move for those with this issue.
Top exercises for lumbar radiculopathy aim to make you more mobile and strengthen your stomach. It's key to have a pro guiding you. They make sure you're doing the exercises right. This avoids any chance of getting worse. Also, getting stronger helps a lot, since many good exercises work your hips and core.
Most people with lumbar radiculopathy get a lot better with exercise. But not everyone. If pain lasts, seeing a doctor is a good idea. They'll help figure out the best plan for your symptoms. The right exercises can be a big part of easing your pain and moving better.

Lumbar Radiculopathy Exercises to Relieve Pain
Dealing with lumbar radiculopathy, or sciatic neuritis, can hurt a lot. But, doing the right exercises can help. Focus on making your core strong and flexible. This can lower your pain and make it easier to move. Always check with a doctor first, though.
Child's Pose

The child's pose comes from yoga. It's great for stretching your lower back. This stretch can ease spine tension and help with lumbar radiculopathy symptoms.
Knee to Chest Stretch

This stretch is easy but effective for lumbar radiculopathy. Pulling your knees to your chest eases pressure on the sciatic nerve. It can cut your pain.
Seated Forward Bend

The seated forward bend helps with this back problem, too. It stretches the hamstrings and lower back. This gives you some relief from the uncomfortable symptoms.
Wall Squats

Wall squats are a fast and effective move for this condition. They make your lower back muscles stronger. As a result, they can help reduce your pain and make you move better.
Piriformis Stretch

Tightness in the piriformis muscle can squeeze the sciatic nerve. This stretch can ease that pressure. It's a direct approach to manage lumbar radiculopathy symptoms.
Lumbar Radiculopathy Exercises
Adding to earlier exercises, several movements target lumbar radiculopathy. They aim to boost hip and core mobility. This helps lessen pain and enhance how well you move.
Hip Flexor Stretch

The hip flexor stretch boosts hip rotation and mobility. It’s key for folks with lumbar radiculopathy. Better hip movement means less stress on the lower back.
To do this stretch, start kneeling with one knee down and the other leg bent in front. Push your hips forward gently, feeling the front hip and thigh stretch. Hold for 30 seconds, then switch to the other side.
Quadriceps Stretch

Stretching your quadriceps helps with back flexibility. Stand near a wall or chair for support. Bend one knee and pull your foot towards your buttocks. Remember: don’t arch your back. Hold for 20-30 seconds. Then, repeat with the other leg.
Knees to Chest

One of the best exercises for lumbar radiculopathy is knees-to-chest. Lie on your back with legs outstretched. Bring your knees up to your chest, holding them with your hands. Hold for 20-30 seconds. Do this motion a few times. It eases back pressure and stretches the area.
Additional Lumbar Radiculopathy Exercises
To help with lumbar radiculopathy, it's good to add a few more exercises to your routine. Two exercises are especially useful: the upward dog yoga pose and crunches (curl-ups).
Upward Dog

Upward dog does wonders for your chest and core. It's a great start to your day, getting your back ready for more exercises. But make sure you're doing it right. A physical therapist can show you the best way to do this pose safely.
Crunches (Curl-ups)

Crunches (curl-ups) are great for your abs. A strong core is key in dealing with lumbar radiculopathy. It can ease lower back stress and reduce sciatica pain. Always work with a therapist to get the technique right and avoid harm.
Adding these extra exercises to your plan improves how you move and cuts down on pain. As always, do things the right way and be careful not to push too hard. Listen to your body and change things up when needed to stay safe.
Precautions and Tips for Exercising
Dealing with lumbar radiculopathy means taking special care. It's important to avoid activities that make your pain worse. Also, change or lessen these movements as necessary. Using ice and heat can reduce pain while you work out.
Doing exercises right is crucial for your back. Remember to keep your body in the correct position. This not only makes the exercises better but also stops you from hurting yourself more. As you get stronger, you can slowly do more without hurting yourself.
Listen to your body and be patient. If your pain gets worse or doesn't go away, talk to a professional. A physical therapist can give you a plan that fits your needs. They will make sure you're doing the right thing for your back.
When to Seek Professional Help
Lumbar radiculopathy often gets better with physical therapy. In six weeks to three months, you may see big improvements. But, sometimes, surgery could be the answer for severe cases. If pain stays or gets worse, talk to a pro.
Exercises for lumbar radiculopathy can help a lot. Yet, if you're not getting better after doing them, or if things are getting worse, it's smarter to see a doctor or therapist.
If you have these signs, seeing a pro is a good idea:
- Persistent or worsening pain that doesn't get better with simple treatments
- Big muscle weakness or tingling in your leg or foot
- Trouble controlling your bladder or bowels
- A sudden, big jump in pain
These signs might point to a bigger issue. If you're worried, don't wait to get help from a pro.
Conclusion
Lumbar radiculopathy is tough, but the right exercises and care can ease your pain. Adding specific exercises to your daily routine helps a lot. Always make sure to exercise right and talk to a doctor if you don't feel better.
Taking charge and really caring for yourself can help you beat lumbar radiculopathy. Keep learning, get the right lumbar radiculopathy treatment, and do the exercises we talked about. This way, you're well on your way to feeling better and moving more.
Remember, getting better is your own journey. It's crucial to team up with your healthcare pro to figure out what's best for you. Through comprehensive care and exercise, you're in control of your treatment. And you will feel the difference in your health over time.
FAQ
What is lumbar radiculopathy?
Lumbar radiculopathy is often called sciatica. It's when a nerve in your spine is pinched. This can happen due to a herniated disc. You might feel weak, have pain, or your leg could go numb.
What are the causes of lumbar radiculopathy?
Many things can cause lumbar radiculopathy. It could be a result of spinal stenosis or a herniated disc. Bone spurs or infections, myelopathy, and spondylolisthesis are other possible causes. Trauma or injury might also lead to this condition.
What are the symptoms of lumbar radiculopathy?
Lower back, butt, and leg pain are common signs. Some may experience weakness in the leg. Pain can also feel like pins and needles.
What are the benefits of exercises for lumbar radiculopathy?
Doing the right exercises can lower your pain. They also help you move better. For many, exercise is the best way to treat lumbar radiculopathy. But in some cases, more help may be needed.
What are some effective lumbar radiculopathy exercises?
Exercises like the child's pose and knee-to-chest stretch are good. Seated forward bend, wall squats, and piriformis stretch also help. They can ease the pain of lumbar radiculopathy.
What other exercises can help with lumbar radiculopathy?
Hip flexor and quadriceps stretches are beneficial. So are knees to chest and upward-facing dog poses. Adding in crunches helps manage lumbar radiculopathy too.
What precautions should I take when exercising for lumbar radiculopathy?
Avoid activities that make the pain worse. Use ice and heat to feel better. Make sure to exercise with good form. Also, slowly build up how long you exercise.
When should I seek professional help for lumbar radiculopathy?
If your symptoms don't get better or get worse, see a doctor. They can give you more advice. Some severe cases of lumbar radiculopathy need surgery.
Source Links
- https://www.webmd.com/back-pain/best-exercises-lumbar-radiculopathy
- https://lattimorept.com/top-lumbar-radiculopathy-exercises/
- https://foreverfitptw.com/blog/5-exercises-for-lumbar-radiculopathy/
- https://southernpainclinic.com/blog/benefits-of-lumbar-radiculopathy-therapy/
- https://www.choosept.com/guide/physical-therapy-guide-lumbar-radiculopathy-sciatica
- https://www.allianceptp.com/5-lumbar-radiculopathy-exercises
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6858271/
- https://commons.und.edu/cgi/viewcontent.cgi?article=1679&context=pt-grad