4 Strategies for Better Sleep with Hypothyroidism
Sleep is key for everyone, but it's even more important for those with hypothyroidism. This condition makes people feel very tired because it lacks thyroid hormones. These hormones help speed up metabolism and other body functions. Hypothyroidism can also lead to sleep problems like sleep apnea and stops deep, restful sleep. This makes people feel tired during the day.
To fight this, getting the right amount of thyroid hormones with medicine is the first step. But, making lifestyle changes can also help improve sleep for those with hypothyroidism.
The Link Between Hypothyroidism and Poor Sleep
If you have hypothyroidism, you might find it hard to sleep well. Thyroid hormones help control your metabolism, heart rate, and many body functions. When these hormones are low, like in hypothyroidism, it can affect your sleep.
How Hypothyroidism Affects Sleep Quality
Hypothyroidism can make sleep apnea worse, causing you to struggle to breathe and wake up often. It can also stop you from reaching the deep sleep you need. This can make you feel tired during the day.
Importance of Restful Sleep for Thyroid Health
Good sleep is key for your thyroid health. It helps your body manage hormone levels and metabolic processes. Without enough sleep, your thyroid might not work right, leading to poor sleep and worse hypothyroidism symptoms.

The connection between hypothyroidism and sleep issues is still being studied. But research hints at a link. It shows that hypothyroidism might be linked to shorter sleep time, longer time to fall asleep, and feeling unhappy with sleep quality. Working on both your thyroid health and sleep habits can lead to better sleep and overall health.
Regulate Thyroid Hormone Levels
If you're having trouble sleeping because of hypothyroidism, start by managing your thyroid hormone levels. Work with your healthcare provider to find the right thyroid medication. This will help bring your levels back to normal.
Getting the right thyroid hormone replacement is key. It helps control your metabolism and other functions affected by hypothyroidism. This, in turn, can make your sleep better. But, taking too much medication can cause insomnia. So, finding the right balance is crucial.
Importance of Proper Thyroid Medication Dosage
About 95 percent of hypothyroidism cases are due to a thyroid gland issue. The right thyroid medication dosage is vital for managing your condition and improving sleep.
- It's suggested that all patients with a thyroid-stimulating hormone (TSH) level over 10 mU/L should be treated for hypothyroidism.
- Younger individuals under age 65 to 70 years are often treated before TSH exceeds 7 mU/L, while older adults with a slight elevation in TSH may not be treated as the normal range for TSH is higher in the elderly.
- Levothyroxine is the most common oral form of thyroid hormone replacement therapy used to treat hypothyroidism.
- Symptoms of hypothyroidism typically begin to improve within two weeks of starting thyroid replacement therapy, with full recovery potentially taking several months for individuals with severe symptoms.
- Regular monitoring of blood tests may be necessary to adjust levothyroxine dosage over time, especially after specific life events like aging, childbirth, or weight loss.
By working closely with your healthcare provider to find the right thyroid medication dosage, you can help regulate your thyroid hormone levels, metabolic rate, and ultimately improve your sleep quality.

Manage Sleep Apnea and Other Sleep Disorders
If you have hypothyroidism, you might face a higher risk of sleep apnea. This condition makes your breathing stop and start while you sleep. It can really hurt your sleep quality and make you feel tired during the day. It's key to deal with this issue along with your hypothyroidism.
Studies show that up to 25% of people with hypothyroidism have obstructive sleep apnea (OSA). In some studies, this number is even higher. For example, 74% of hypothyroid patients were found to have OSA. This shows a strong link between the two conditions.
People with hypothyroidism are more likely to have sleep apnea than others. Being overweight can also increase your risk. Obesity is a big risk factor for sleep apnea.
If you're having trouble sleeping, talk to your doctor. They might suggest a sleep study to check for sleep disorders like sleep apnea. With the right treatment, like a CPAP machine, your sleep can get better and your health can improve.

Dealing with sleep apnea and other sleep issues is key to managing hypothyroidism. Work with your healthcare team to create a plan that helps you sleep better and stay healthy.
Create a Sleep-Friendly Environment
For people with hypothyroidism, making your bedroom sleep-friendly is key. Keep the room cool and quiet to help your body make melatonin. This hormone helps you sleep better.
Maintain a Cool Temperature
Keep your bedroom at 65-70°F (18-21°C) for better sleep. A cooler room makes your body release more melatonin. This hormone helps control your sleep cycle.
Eliminate Light and Noise Disturbances
- Turn off TVs, computers, and smartphones an hour before bed to avoid blue light.
- Use blackout curtains or an eye mask to block all room light.
- Try a white noise machine or earplugs to keep out loud noises.
With the right temperature, light exposure, and noise control, your sleep can get better. This can also help your thyroid health.

Establish a Relaxing Bedtime Routine
Creating a calming bedtime routine can greatly help those with hypothyroidism sleep better. Doing calming activities 30 minutes before bed tells your body it's time to relax. This helps prepare you for deep sleep.
Calming Activities to Promote Sleep
Adding relaxing activities to your evening can boost melatonin, the hormone that helps you sleep. Here are some easy ways to unwind:
- Taking a warm bath or shower
- Reading a book or listening to soothing music
- Practicing gentle stretches or light yoga
- Engaging in deep breathing exercises or meditation
- Sipping on a cup of herbal tea
These activities calm your mind, lower stress, and make your bedroom sleep-friendly. This is key for handling hypothyroidism symptoms and keeping your thyroid healthy.

It's important to find what works for you and stick to it. Making bedtime a priority can lead to better sleep and more energy during the day.
Invest in a Comfortable Mattress and Bedding
For people with hypothyroidism, getting a good night's sleep is key. A quality mattress and bedding can greatly improve your sleep. Getting a new mattress every seven years can also help by giving you better support and comfort.
When picking a mattress, find one that feels right for your body. Memory foam or hybrid mattresses are great because they shape to your body. Also, go for bedding made of breathable materials like cotton or bamboo. These materials help keep you cool and sleep better.
- Opt for a mattress that provides the right balance of comfort and support for your needs.
- Consider a memory foam or hybrid mattress for optimal spinal alignment and pressure relief.
- Choose breathable, natural fiber bedding, such as cotton or bamboo, to help regulate your body temperature.
- Replace your mattress every 7-10 years to ensure it continues to provide the necessary support.
Getting a good night's sleep is crucial for managing hypothyroidism and staying healthy. A comfortable and supportive bed can make a big difference.

Watch Your Eating and Drinking Habits
Watching what you eat and drink can really affect your sleep if you have hypothyroidism. It's important to avoid big meals before bed. This helps keep your sleep cycle smooth. Also, cutting down on spicy foods, caffeine, and alcohol can help you sleep better.
Avoid Large Meals Before Bedtime
Eating big meals close to bedtime can mess up your sleep. Your body works hard to digest the food, making it hard to fall asleep. Try to eat light meals before bed instead.
Have a Small, Protein-Rich Snack
Instead of a big meal, think about having a small, protein-rich snack before bed. This keeps your blood sugar stable and helps you sleep better. Good choices include whole-grain crackers with peanut butter, a handful of nuts, or a protein smoothie.

By paying attention to your eating and drinking, you can improve your sleep quality and overall health with hypothyroidism.
Hypothyroidism and Sleep
Hypothyroidism, or an underactive thyroid gland, can really affect your sleep and overall health. It can make it hard to fall asleep and leave you feeling tired all day. This can mess up your sleep patterns and make you feel constantly tired.
Hypothyroidism changes how you breathe at night, which affects your sleep. People with it might have sleep apnea, waking up a lot and not getting deep sleep. This can make you feel fatigue and insomnia, making it harder to deal with an underactive thyroid.
- Difficulty falling asleep because of hormonal changes
- Frequent night sweats and trouble controlling your body temperature
- Irregular sleep-wake cycles and messed-up circadian rhythms
To fix these issues, managing your thyroid condition is key. Work with your doctor to regulate your thyroid hormone levels. This can help improve your sleep and energy levels.
Manage Stress and Anxiety
For people with hypothyroidism, managing stress and anxiety is key. These issues can make thyroid symptoms worse, including bad sleep. Using stress management techniques like mindfulness, meditation, or relaxation can calm the mind and body. This can lead to better sleep.
Mindfulness and Relaxation Techniques
Spending time each day on calming activities can help those with hypothyroidism. Activities like mindfulness meditation, deep breathing, and gentle yoga are great for reducing anxiety and promoting relaxation.
Research shows that ashwagandha can also help manage stress and anxiety in hypothyroidism. Studies have found that ashwagandha supplements can lower stress, anxiety, and cortisol levels. They can also improve sleep quality and length.
Finding the right stress management and relaxation techniques might take some time. Be patient and don't hesitate to get help from a healthcare professional or mental health therapist if you're finding it hard to manage your stress and anxiety.
Avoid Alcohol and Caffeine
If you have hypothyroidism, watch what you drink. Caffeine and alcohol might seem like they help you relax or sleep better. But, they can actually hurt your sleep quality over time.
Alcohol can make falling asleep easier but messes with the deep sleep stages. Caffeine is a stimulant that keeps you awake and makes sleeping hard. Avoiding these substances before bed helps you sleep better and keeps your thyroid healthy.
- Limit your caffeine intake, as it can interfere with your body's ability to fall and stay asleep.
- Avoid consuming alcohol, as it may initially help you fall asleep but can disrupt your sleep cycle.
- Pay attention to how your body reacts to these substances and make adjustments accordingly.
Being careful with your caffeine and alcohol can make your sleep better. It also helps your thyroid health. Always talk to your doctor for advice on managing hypothyroidism and living healthy.
Exercise Regularly
If you have hypothyroidism, regular exercise can change the game for you. It boosts your energy and mood and helps your thyroid and sleep. Adding moderate exercise to your daily life can greatly improve your well-being.
Benefits of Exercise for Thyroid Health
Exercise is great for people with hypothyroidism. It helps with weight management, heart health, and bone strength. It also supports your immune system and thyroid function. Plus, it releases chemicals that help with depression and anxiety.
Start slowly if you're new to exercise or have severe symptoms. This prevents injuries. Try low-impact activities like water aerobics, swimming, or walking if you have joint pain. Strength training is also good to build muscle strength.
Try different exercises, like strength training two to three times a week, and aerobic activities five to six days a week. Don't forget daily flexibility exercises. It's important to listen to your body and adjust exercises as needed for safety and effectiveness.
Regular exercise can improve your thyroid health, energy, and sleep. Start slow, increase intensity gradually, and always talk to a healthcare professional if you have concerns or need advice.
Follow a Thyroid-Friendly Diet
Following a thyroid-friendly diet can help improve sleep for those with hypothyroidism. The Mediterranean diet focuses on foods like veggies, fruits, whole grains, lean proteins, and healthy fats. These foods boost energy and sleep quality. This diet helps balance hormones and supports metabolism, leading to better sleep for hypothyroidism patients.
The Mediterranean Diet for Better Sleep
The Mediterranean diet is full of foods good for thyroid health and sleep. Key nutrients and foods include:
- Iodine-rich foods like seaweed, dairy, and fish
- Selenium-rich foods such as Brazil nuts, eggs, and seafood
- Zinc-containing foods like meat, poultry, and legumes
- Antioxidant-packed fruits and vegetables
- Healthy fats from olive oil, avocados, and nuts
Adding these foods to your diet supports thyroid function and can improve sleep. The Mediterranean diet also reduces inflammation, which helps with rest and well-being.
A balanced, thyroid-friendly diet is key for managing hypothyroidism and better sleep. Talk to a healthcare expert to create a diet plan tailored to your needs. This will help you achieve the best thyroid health and sleep quality.
Seek Professional Help if Needed
If changing your lifestyle doesn't help improve your sleep with hypothyroidism, you should get professional help. A doctor or sleep specialist can check for sleep disorders like sleep apnea. They can then make a plan to help you sleep better with hypothyroidism.
Getting the right medical care is key for better sleep. Many people with hypothyroidism have sleep disorders. A healthcare provider can offer the support and treatment you need.
Talking to a professional can also help find and fix any medical issues like sleep apnea. This can greatly improve your sleep and overall health with hypothyroidism.
Remember, asking for professional help is crucial for managing your hypothyroidism and getting good sleep. Don't be shy about working with your healthcare team to find the best solutions for you.
Conclusion
Managing hypothyroidism and getting better sleep can be tough, but it's doable with the right steps. By keeping your thyroid hormones in check, fixing sleep disorders, making your bedroom sleep-friendly, and changing your lifestyle, you can fight fatigue and insomnia. This leads to more restful and healing sleep.
It's important to look at your hypothyroidism and sleep issues as a whole. Find the root causes and make a plan that fits your needs. With time, effort, and help from doctors, you can get better sleep and improve your thyroid health. This opens the door to a healthier, more lively life.
Your sleep quality and overall health matter a lot. By focusing on better sleep, you can manage your hypothyroidism and improve your life. Start this journey and stick with the lifestyle changes for the restful sleep you need.
FAQ
How does hypothyroidism affect sleep quality?
Hypothyroidism can really mess with your sleep. It slows down your metabolism and messes with your sleep cycle. This makes it hard to fall asleep and stay asleep. It also raises the risk of sleep apnea, which makes sleep even worse.
Why is restful sleep important for thyroid health?
Good sleep is key for your thyroid health. It helps regulate hormones and metabolic processes. Without enough sleep, hypothyroidism symptoms get worse and managing the condition becomes harder.
How can proper thyroid medication dosage help improve sleep?
Getting the right thyroid hormone levels through medication helps improve sleep. It's crucial to work with a doctor to find the right dosage. Too much medication can cause insomnia.
What other sleep disorders are common with hypothyroidism?
Sleep apnea is common in people with hypothyroidism. It disrupts breathing and affects sleep quality. It's important to talk to a doctor about sleep disorders and get the right treatment, like a CPAP machine.
How can creating a sleep-friendly environment help with hypothyroidism and sleep?
Keeping your bedroom cool, between 65-70°F, and quiet helps you sleep better. A calm sleep environment supports your body's natural sleep cycle. It helps produce melatonin and keeps your circadian rhythms in check.
What are some effective bedtime routines for those with hypothyroidism?
Doing calming things before bed, like taking a warm bath or reading, signals your body it's time to sleep. A consistent bedtime routine helps release melatonin and ensures a good night's sleep.
How can diet and nutrition impact sleep for those with hypothyroidism?
Eating a thyroid-friendly diet, like the Mediterranean diet, can help regulate hormones and improve sleep. Eating a small, protein-rich snack before bed keeps your blood sugar stable and supports better sleep.
When should someone with hypothyroidism seek professional help for sleep issues?
If lifestyle changes don't help with sleep, it's time to get professional help. A doctor or sleep specialist can help find sleep disorders and create a plan to improve your sleep with hypothyroidism.
Source Links
- Sleep Better With Hypothyroidism
- Thyroid Problems and Insomnia
- Thyroid Issues and Sleep
- Hypothyroidism and insomnia: What is the link?
- Thyroid Dysfunction and Sleep Disorders
- The relationship between thyroid function tests and sleep quality: cross-sectional study
7 Tips to Manage Alzheimer’s and Parkinson’s
Dealing with Alzheimer's and Parkinson's can feel overwhelming. But, with the right strategies, you can make life better for you and your loved one. This article offers 7 key tips to help manage these tough conditions.
Alzheimer's and Parkinson's affect millions globally. They have some similarities but need different management approaches. Knowing the differences and using the right strategies helps support your loved one and keep them well.
If you're caring for a family member or managing your own condition, these 7 tips will help. They cover understanding the disease stages and focusing on self-care. This guide gives you the knowledge and tools to face challenges with confidence.
Alzheimer and Parkinson Diseases
Alzheimer and Parkinson disease are two major neurological conditions. They can greatly affect a person's thinking and physical abilities. It's important to know the differences between them for better care.
What is Alzheimer's Disease?
Alzheimer's disease is a brain disorder that mainly affects memory, thinking, and daily activities. It's the most common dementia type, making up 60 to 80% of dementia cases. It usually starts around 65 years old, but can start earlier due to genetics.
What is Parkinson's Disease?
Parkinson's disease is known for its motor symptoms like tremors, slow movements, and stiffness. It can also cause cognitive changes and dementia. It's less common than Alzheimer's, happening to about 1-2 people per 1,000. It usually starts at 60 years old, but can start before 40 in rare cases.
Both Alzheimer and Parkinson are brain-related conditions. Alzheimer's mainly affects memory and thinking, while Parkinson's impacts movement and motor skills. Yet, both can lead to cognitive decline and dementia.
Knowing the specifics of Alzheimer and Parkinson is key to managing them well. It helps in providing the right care for those affected by these conditions.
Alzheimer and Parkinson Disease
Alzheimer and Parkinson disease are complex conditions that greatly affect a person's life. They have different symptoms but share some challenges in thinking and movement. Those caring for people with these diseases need to understand each condition well to help them the best.
About one-third of people with Parkinson's will get dementia, called Parkinson's disease dementia (PDD). PDD can make it hard to communicate, solve problems, think quickly, remember things, and affect mood. Medicines like rivastigmine can help, and therapy can also be useful.
Alzheimer's disease affects around 5.8 million Americans and is the fifth leading cause of death for those over 65. People with Alzheimer's usually live between 4 to 8 years after being diagnosed. It's more common in women than men.
While Parkinson's is more common in men, its dementia symptoms are similar to those of dementia with Lewy bodies (DLB). Many experts see Parkinson's and DLB as the same disease, differing only in where it starts in the brain.
Dealing with Alzheimer and Parkinson requires understanding their unique challenges. Caregivers and those with these conditions must work with doctors to improve their lives and outcomes.
Early Signs and Symptoms
Knowing the early signs of Alzheimer and Parkinson diseases is key to getting help early. These conditions show up in different ways, but spotting the signs can lead to better care and support.
Signs of Alzheimer's Disease
Alzheimer's disease often starts with memory loss and trouble with words. Early on, you might forget recent events or struggle to find the right words. You might also feel lost in places you know well.
These issues can make daily life hard and get worse over time.
Symptoms of Parkinson's Disease
Parkinson's disease usually starts with motor problems like tremors and slow movements. You might see tremors when you're not moving, walk with a shuffling step, or feel stiff. Your speech might also change, becoming softer or sounding the same all the time.
These physical changes can make everyday tasks harder.
It's important to know that Alzheimer and Parkinson can show similar signs early on. People might see both cognitive and motor symptoms. If you or someone you know is showing these signs, seeing a doctor is a good step. They can give a full check-up and start the right treatment.
Cognitive Impairment and Dementia
Alzheimer and Parkinson diseases can cause cognitive problems and dementia. These issues can greatly affect your daily life and how well you can do things. Signs include memory loss, trouble solving problems, and language issues. It's important to notice and deal with these changes to help keep your life as good as possible.
Parkinson's disease usually starts in people over 50, with most starting at 60. But, younger people can get it too, especially if it starts before they're 50. This is called early-onset Parkinson's. Over time, about 4 in 5 people with Parkinson's will also get dementia. They may lose memory, see things that aren't there, and have trouble thinking clearly.
It's thought that 30% to 40% of people with Parkinson's will get dementia. This is much more common than in people without Parkinson's. If someone with Parkinson's lives for more than 10 years, at least 75% will get dementia. Some signs like stiffness, walking problems, mild memory loss, and seeing things that aren't there can make getting dementia more likely.
Up to 36% of new Parkinson's patients show signs of cognitive decline. On average, their thinking skills get worse by 1 point each year. For those with Parkinson's dementia, it's 2.3 points a year. Spotting and treating these changes early is key to keeping a good life for those with Parkinson's.
Coping Strategies for Caregivers
Caring for a loved one with Alzheimer or Parkinson disease is tough. It's both physically and emotionally hard. As a caregiver, you need to know how to handle this tough journey.
Educating Yourself
Learn about Alzheimer or Parkinson disease, their symptoms, and treatments. Know the challenges your loved one might face. Also, learn how to communicate well to give the best care. Being informed helps you make good choices and meet your loved one's needs.
Attending Doctors' Appointments
Be active in your loved one's health meetings. Take notes, ask questions, and speak up for their needs. This makes sure the healthcare team knows how to help your loved one best.
You don't have to go through this alone. Look for support groups, community help, and health experts. They can give you the advice and help you need to care for your loved one. And don't forget to take care of yourself too.

Medication Management
Managing medications is key for people with Alzheimer or Parkinson disease. Caregivers must work closely with doctors to understand the medicines, their side effects, and the need for regular doses. Creating a system to keep track of when to take medicines helps make sure your loved one gets the most from their treatment.
Knowing about the treatments for Alzheimer and Parkinson is important. For Alzheimer's, drugs like donepezil and rivastigmine help keep the mind sharp. For Parkinson's, levodopa and other drugs manage the motor symptoms and improve life quality.
It's also vital to watch for side effects and tell the doctor about any changes. Side effects can include stomach problems, feeling sleepy, or changes in behavior. These should be talked about right away to keep the patient safe.
Being organized, talking with doctors, and watching how the medicines work helps caregivers. This way, your loved one with Alzheimer or Parkinson gets the best treatment plan. This approach can greatly help manage symptoms and slow down the disease.
Managing medications is an ongoing task that needs teamwork between caregivers and doctors. By being alert and active, you can help your loved one face Alzheimer's or Parkinson's with more confidence and support.
Legal and Financial Planning
When Alzheimer and Parkinson diseases get worse, it's key to plan for legal and financial matters early. Setting up a power of attorney and advance directives is crucial. These steps make sure your loved one's healthcare and financial wishes are followed, even if they can't make decisions on their own. Talking to an elder law attorney can help with these complex legal and financial issues.
Power of Attorney
A power of attorney lets people with Alzheimer or Parkinson choose someone they trust to make legal and healthcare choices for them. This is a key tool to keep their wishes in place as the disease gets worse and they can't handle their affairs by themselves.
Advance Directives
Advance directives, like living wills, let people say what life support treatments they want in a coma or at the end of life. This brings peace of mind and helps avoid hard choices for family during tough times.
Planning for the costs of medical care and living with Alzheimer or Parkinson means looking at all your money and financial papers. Working with experts like financial planners, estate planning lawyers, or accountants can help. They can make good plans, look at income sources, and find tax breaks.

People with these diseases should talk about their legal and financial matters with family and caregivers. This way, they can make decisions for them as things get harder. By planning ahead for legal and financial stuff, people with Alzheimer or Parkinson can make sure their wishes are followed. And their families will be ready to take care of them and manage their money well.
Safety and Support Services
Keeping people with Alzheimer or Parkinson safe and well is very important. Using support services like home safety checks, medical alert systems, and adult day programs helps. These services create a safe place and give caregivers a break. Working with local and national groups can also connect families with the help they need.
For those with Alzheimer's, making the home safe is key. This means putting locks where they can't be seen, making sure paths and rooms are bright, and taking away things that could be dangerous. It's also smart to remove rugs that could trip someone and clean up the living space to avoid accidents.
People with Parkinson's disease often have a higher risk of falling, with most falls happening at home. Adding safety features like grab bars, textured stickers on slippery spots, and a walk-in shower can make bathrooms safer. Keeping cleaners and other chemicals away from reach can stop accidental poisoning in the laundry area.
Getting ready for emergencies is also vital. Caregivers should keep important phone numbers like police, fire, hospitals, and poison control close by. Checking and keeping safety devices like carbon monoxide and smoke detectors working is also key.
Using support services and safety steps can make life better for people with Alzheimer or Parkinson. It also helps caregivers feel better. This makes life better for both the caregiver and the person being cared for.

Self-Care for Caregivers
Caring for a loved one with Alzheimer or Parkinson can be tough on you. It's key to look after yourself to give the best care. Keep fit, find emotional support, and manage stress to take care of yourself and your loved one.
Maintaining Physical Health
Being a caregiver can affect your health. Make sure to sleep well, eat right, and move a bit every day. Even a short walk can help. Regular doctor visits keep you on track with your health.
Seeking Emotional Support
Looking after someone with these diseases can be hard on your feelings. Look for counseling, support groups, or respite care. Talk to other caregivers for support. Don't forget to take time for things that make you happy and relaxed.
Watch out for signs of stress like feeling short-tempered, not sleeping well, or forgetting things. Setting self-care goals and taking small steps can help you stay well. This way, you can keep giving great care to your loved one.
Looking after your body and mind is key when caring for someone with Alzheimer or Parkinson. By focusing on caregiver self-care, you can handle stress better, stay healthy, and get the emotional support you need to face caregiving challenges.
Stages of Alzheimer and Parkinson Diseases
Alzheimer and Parkinson are progressive conditions that affect the brain. They have different stages of decline in thinking and physical abilities. Knowing these stages helps people and their caregivers plan for the future and adjust care plans.
Stages of Alzheimer's Disease
Alzheimer's disease goes through seven stages, from mild forgetfulness to needing full care. Early on, people may forget things and find it hard to make decisions. Later, they might struggle with daily tasks, change in personality, and lose their ability to move around.
Stages of Parkinson's Disease
Parkinson's disease starts with mild symptoms on one side of the body and gets worse over time. It can lead to severe loss of movement and needing help all the time. The disease gets worse with time, causing more motor problems, thinking issues, and sleep problems.
Knowing how these diseases progress is key to giving the right support. Alzheimer's and Parkinson's both cause thinking problems and need caregivers. Understanding the stages helps make better decisions and improves outcomes for those with these diseases.
Conclusion
Managing Alzheimer and Parkinson disease is tough but possible with the right support. People and their caregivers can make life better for those with these diseases. Knowing about these diseases, finding helpful resources, and taking care of yourself are key steps.
This article has given you a lot of information on symptoms, how these diseases progress, and ways to manage them. Being informed and proactive helps you make good choices and get the right medical care. It also helps you use caregiving strategies that improve your loved ones' well-being.
There are many support systems and resources out there to help you. You're not alone in this journey. As these diseases become more common, it's important to keep up with new treatments and support services. By doing so, you can make sure you and your loved ones get the best care possible.
Remember, the article mentioned a study that shows the latest research and advancements. Staying informed helps us work towards a future where managing Alzheimer and Parkinson is easier and more effective for everyone in India.
FAQ
What is the difference between Alzheimer and Parkinson disease?
Alzheimer's disease makes memory, thinking, and daily tasks harder. Parkinson's disease is known for shaking and slow movements. It can also cause thinking and memory problems.
What are the early signs and symptoms of Alzheimer and Parkinson diseases?
Alzheimer's disease starts with memory loss and trouble with words. It also brings changes in behavior. Parkinson's disease first shows with shaking, slow movements, and trouble with balance.
How do cognitive impairment and dementia affect individuals with Alzheimer and Parkinson diseases?
Both diseases cause memory loss and trouble with solving problems and using words. These changes make everyday tasks hard and affect how well people can function.
What strategies can caregivers use to support their loved ones with Alzheimer or Parkinson disease?
Caregivers should learn about the diseases and go to doctor's appointments. They should speak up for their loved ones and manage their medicines well. Using support services helps create a safe place and gives caregivers a break.
Why is it important for caregivers to prioritize their own well-being?
Taking care of someone with Alzheimer's or Parkinson's is hard on the body and mind. Caregivers need to keep a healthy lifestyle, sleep well, and get emotional support. This helps them care for their loved ones better.
How can individuals and caregivers prepare for the different stages of Alzheimer and Parkinson diseases?
Knowing how these diseases get worse helps people and caregivers plan better care. They can adjust their support and make sure they have the right help as the diseases get more severe.
Source Links
- 10 Steps for Caring for a Person with Parkinson’s Dementia
- Alzheimer’s Disease: Causes, Symptoms, Treatment & Stages
- Alzheimer’s and Parkinson’s Disease: Similarities and Differences
- Parkinson’s vs. Alzheimer’s: A comparison
- Understanding the Difference Between Alzheimer's and Parkinson's
Radial Nerve Palsy Treatment: Modern Approaches for Recovery
Are you or a loved one dealing with radial nerve palsy (RNP)? This condition makes grip strength drop by 77%.
But, there's hope with modern treatments for radial nerve palsy treatment can bring back function and movement. Early and smart radial nerve palsy treatment is key to healing and recovery.
In this blog, we’ll look at what causes radial nerve palsy, how to spot it, and what modern treatments can help you recover safely and fully.
Understanding Radial Nerve Palsy
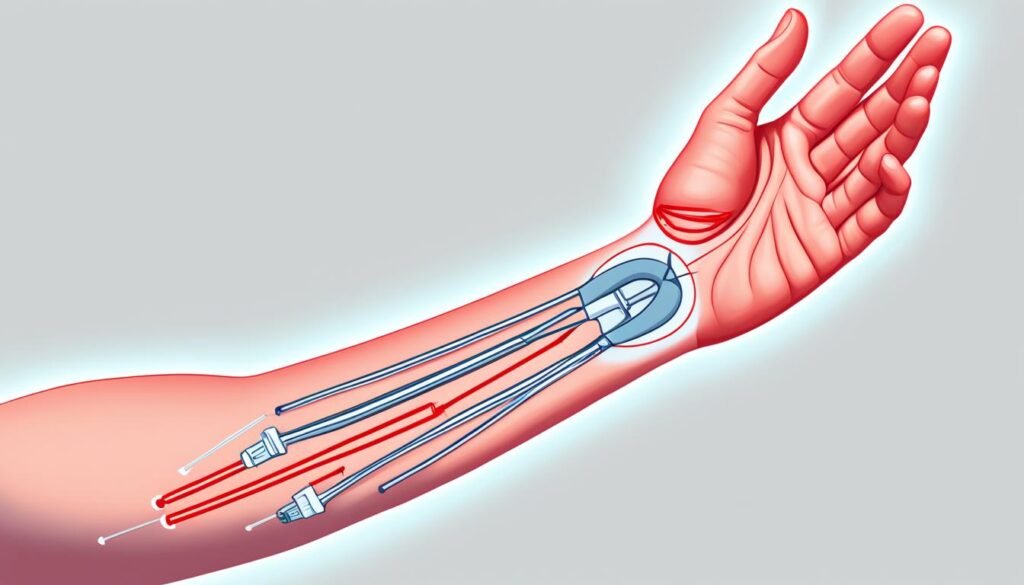
Radial nerve palsy (RNP) happens when the radial nerve gets damaged. This nerve runs down the back of your arm. It controls the muscles that straighten your elbow, wrist, and fingers.
When the nerve is damaged, these muscles don’t work right. It also reduces grip strength by up to 77%. This leads to weakness, numbness, or a dropped wrist.
Causes and Risk Factors
Many things can cause radial nerve palsy. Some are common accidents. Others are hidden health problems:
- Direct injury from broken bones, especially a humerus fracture
- Long pressure on the arm, like sleeping with your arm hanging (Saturday night palsy)
- Repetitive stress or overuse of the arm
- Health issues like diabetes or tumors pressing on the nerve
- Systemic conditions such as infections or autoimmune diseases
Common Symptoms to Recognize
You can usually tell something is wrong by how your hand and arm feel and move:
- Drooping of the wrist (wrist drop)
- Difficulty straightening fingers or wrist
- Weak grip strength
- Numbness on the back of the hand and forearm
Diagnosis and Evaluation
It's crucial to correctly diagnose radial nerve palsy (RNP) to treat it effectively. Doctors use a detailed physical exam, imaging tests, and electrodiagnostic studies for this. These steps are vital in creating a plan that works for you.
A neurologist like Dr. Chandril Chugh will run several tests to confirm the diagnosis:
- Physical exam to test strength and reflexes
- EMG testing (electromyography) to check nerve signals
- Nerve conduction studies to see how fast your nerves send signals
Early diagnosis helps avoid long-term damage and improves results.
Non-Surgical Radial Nerve Palsy Treatment Options
In the start, if you have radial nerve palsy, radial nerve palsy treatment using splints and braces can be key in getting better. They stop your muscles from getting too tight and keep your joints moving well.
Splinting and Bracing
Your doctor might suggest wearing a splint or brace for your wrist and fingers. This helps the irritated nerve to heal. It's a good plan if your nerve isn't badly hurt.
Physical Therapy and Exercises
Physical therapy and specific exercises also really help. They aim to get back your strength, keep muscles from locking up, and improve how well your hand works. Doing these together boosts your chances of getting fully better.

Radial Nerve Palsy Treatment Surgical Interventions
If there’s no progress after months, or the nerve is fully torn, surgery may be needed. The decision is based on tests and how long the symptoms last.
When Is Surgery Recommended?
Surgery is often advised when:
- There is zero recovery within 3 to 6 months
- EMG shows nerve is completely cut or detached
- Severe trauma caused full radial nerve injury
Common Surgical Procedures
Doctors choose the right procedure based on the nerve damage:
- Radial nerve repair surgery: Directly sewing the nerve ends back together
- Nerve grafting: When the nerve damage is severe, nerve grafting could be considered. This means creating a 'bridge' for the damaged nerve to heal. By using your own nerve tissue, it helps the nerve grow back and connect with your muscles again.
- Tendon transfers: For some non-recovering cases of RNP, tendon transfers may be the solution. A method like the modified Merle D'Aubigné can be used. It helps to move tendons in a way that allows your wrist and fingers to work properly again.
- Nerve decompression: Surgery may involve nerve decompression. It tries to reduce pressure on the radial nerve and help you recover. Doctors release any tight spots along the nerve, like scar tissue or bone problems.
Recovery Timeline After Surgery
Healing takes time. Most people regain function over months, not weeks.
| Post-Surgery Timeline | What to Expect |
|---|---|
| 1-3 Months | Pain control, light movement exercises begin |
| 3-6 Months | Strength starts to return, therapy becomes intensive |
| 6-12 Months | Fine motor control improves, daily use returns |
Success Rates and Outcomes
- Nerve graft recovery success: 40–60% for motor function
- Tendon transfer surgeries have a high success rate, often above 80%
Risks: Scar tissue, incomplete movement return, re-surgery in rare cases.
The Modified Merle D'Aubigné Tendon Transfer Method
The modified Merle D'Aubigné tendon transfer method helps patients regain wrist and finger movement. It's for those with radial nerve palsy who haven't seen improvement. This surgery uses updated muscle transfer techniques to get better results than before.
The surgery follows several important steps:
- Move the pronator teres muscle to the extensor radialis brevis to fix wrist extension.
- Switch the flexor carpi radialis muscle to the extensor digitorum communis and extensor pollicis longus for finger extension.
- Use the palmaris longus to help the thumb move better with the abductor pollicis longus and extensor pollicis brevis.
This method is a deep dive into fixing the challenges of radial nerve palsy. It offers better wrist and finger movement and overall hand function.
The outcome post-surgery is mainly positive for people with non-recovering RNP. Most patients report excellent or good results. This method can really make a difference, enhancing quality of life for these individuals.
Recovery and Rehabilitation
You may need tendon transfer surgery if you have non-recovering radial nerve palsy. After the surgery, you'll need a period of rest followed by a rehab program. This program is key to gaining back strength, movement, and the use of your affected limb.
Post-Operative Care
In the beginning, you might have to wear a splint or cast to protect your surgery site. As you heal, your healthcare team will start you on exercises to move your limb. They will also begin other therapies to improve your function.
Occupational Therapy
Occupational therapy is very important for your recovery. Your therapist will help you get back to your usual daily activities and reach your full potential. They might teach you new skills, give you special tools, and show you how to solve any recovery hurdles.

Radial Nerve Palsy Treatment
Radial Nerve Palsy Treatment involves surgical methods to restore function and movement. One successful method is the modified Merle D'Aubigné tendon transfer. It helps patients move their wrists and fingers again.
Surgical Techniques
Doctors also perform nerve decompression and grafting, along with tendon transfers, to treat RNP. These surgeries aim to release pressure on the nerve and support nerve regrowth. This improves the chances of recovering function.
Nerve Repair Strategies
There are new therapies being developed to boost nerve healing. Innovations like nerve conduits and guidance channels show promise. They could improve outcomes for those with severe nerve injuries or cases where the nerve doesn't heal.
Choosing the Right Treatment Path
Every patient’s needs are different. Picking the best radial nerve palsy treatment means understanding your case and getting the right help.
Finding the Right Specialist
You may need more than one expert:
- A neurologist (like Dr. Chandril Chugh) for nerve diagnosis
- An orthopedic surgeon for structural issues
- A physical or occupational therapist for recovery plans
Cost, Insurance, and Access
Understanding cost helps reduce stress:
- Surgery costs: $3,000–$12,000 in the U.S., cheaper in India
- Check if insurance covers nerve regeneration or rehab tools
- Many policies now cover radial nerve repair surgery and therapy
Prognosis and Outlook
The outlook for people with radial nerve palsy treatment depends on a few factors. This includes how bad the nerve injury is, what caused it, and how it's treated. Many can get a lot of function back and go back to their usual life with the right care. It's key to find it early and act fast for the best chance at a full recovery without lasting problems.
How long it takes to get better can change a lot. Most RNP cases improve in about 12 weeks with the first treatments. Younger people and those with just a small bit of nerve damage often do better. Yet, tough situations or when surgery is needed might mean healing takes six to eight months.
Noting the odds are good with proper care is important. Staying in touch with your medical team and sticking to a rehab plan can really help. This increases your chance of getting back most, if not all, of your movement and daily life.
Prevention and Risk Reduction
Radial nerve palsy (RNP) is tough, but you can lower the risk and avoid it. Focus on safety at work and use good plans to stop injury. This way, you cut down your chance of getting this serious nerve problem.
Workplace Safety
If you do tasks again and again, sit funny, or work in risky spots, think about your safety. Work with your boss for a better work setup. Use desks that move, seats that support well, and tools that are kind to your body. This stops too much pressure on you and lowers your RNP risk.
Injury Prevention Strategies
Other than safe work, there are steps to keep you from RNP and similar injuries. Lift things right, keep your back straight, and watch how you move, especially if you do things over and over or in odd ways. For sleeping, use pillows or supports to keep your body in a good balance. This helps stop pressure on your nerves when you sleep.
Even if you can’t stop all RNP cases, you can do a lot to lower your risk. Put safety first, and deal well with dangers at work. This means you are taking an important step in staying healthy and enjoying life.
Coping and Support
Navigating through radial nerve palsy (RNP) challenges can be tough. But, the right support and resources can help you overcome them. Educating yourself is key to empowering your recovery journey.
Patient Education
It's important to know why you have RNP, its signs, and how it's treated. Your healthcare team should share lots of information with you. This includes details on the condition and recovery steps using the modified Merle D'Aubigné tendon transfer method.
This knowledge turns you into a key player in your recovery. It gives you a sense of control and confidence.
Support Groups and Resources
Talking to others facing RNP can make a world of difference. Joining support groups offers many benefits. They give you people to share with, emotional support, and practical tips.
Also, look for resources and online communities. They can guide you through recovery and help tackle daily challenges with RNP.
Remember, you're not on this journey alone. With the support and resources around you, staying positive becomes easier. It helps you work towards regaining your independence.
A Message from Dr. Chandril Chugh
Radial nerve palsy doesn’t have to stop you from living well. With smart care, early action, and expert guidance, recovery is real. The key is finding the right path, and sticking to it. If you or someone you know is dealing with wrist drop or sudden weakness, don’t wait. Book a consultation with me to explore the best radial nerve palsy treatment options.
If this condition happens because of a humeral shaft fracture, up to 94% of people see improvement right away. After surgery, about 89% of these cases get better. The chances of getting radial nerve palsy right from the start are around 10%, which drops to 3-7% after surgery. Most of these issues, about 88% to 100%, solve themselves in a few weeks to a few months.
People with radial nerve palsy often face injuries from low-energy trauma, like falls. Half of them have spiral fractures and nearly 90% have breaks in the middle part of their humeral shaft. Also, about 56% of these people are men, with a median age of 49. After an injury, 4.1% of patients end up with radial nerve palsy.
I’ve helped hundreds of patients regain movement, reduce pain, and feel in control again. You can, too.
FAQ
What is radial nerve palsy and what are its symptoms?
Radial nerve palsy (RNP) means you can't fully open your wrist and fingers. This also makes your hand grip weaker. You might notice your wrist dropping and find it hard to extend your fingers. You could also feel less in the back of your hand.
What causes radial nerve palsy?
Humerus fractures, puncture wounds, and pressure on the nerve can cause radial nerve palsy.
How is radial nerve palsy diagnosed?
Doctors will do a physical exam to check for wrist drop and weak finger movement. They also look for lack of feeling on the back of the hand. X-rays and MRI scans might be done to find the cause. Nerve tests help see how bad the nerve damage is.
What are the non-surgical treatment options for radial nerve palsy?
Early on, using a splint can stop your hand from getting stiff. This makes sure your joints stay flexible. Physical therapy and exercises can keep your muscles strong and help you recover.
What are the surgical treatment options for radial nerve palsy?
If surgery is needed, options include fixing the nerve, grafting it, or moving tendons. The modified Merle D'Aubigné transfer helps get your wrist and fingers working better if the nerve won't heal.
What is the modified Merle D'Aubigné tendon transfer method?
This method moves muscles in your arm to help extend your wrist and fingers. It improves on past methods and aims to fully restore movement.
What is the recovery and rehabilitation process like for radial nerve palsy patients?
After surgery, you'll need time when you can't move your hand. Then, you'll start rehab to make your hand strong again. Occupational therapy is key to getting back to normal activities.
What is the prognosis for patients with radial nerve palsy?
How well you recover from radial nerve palsy depends on many factors. But, with the right care, most people can get a lot of their hand function back.
How can radial nerve palsy be prevented?
Be careful at work and learn how to avoid injuries. This can lower your chances of getting radial nerve palsy or other nerve problems.
What kind of support and resources are available for patients with radial nerve palsy?
Knowing about your condition and treatments can give you strength. Joining support groups or finding helpful resources can make your journey easier and more positive.
Source Links
- https://orthopedicreviews.openmedicalpublishing.org/article/94033-treatment-of-irrecoverable-radial-nerve-palsy-using-the-modified-merle-d-aubigne-tendon-transfer-method
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8716365/
- https://www.healthline.com/health/radial-nerve-dysfunction
- https://www.ncbi.nlm.nih.gov/books/NBK537304/
- https://www.mountsinai.org/health-library/diseases-conditions/radial-nerve-dysfunction
Lambert Eaton Myasthenic Syndrome: Symptoms, Causes, and Treatment
Lambert-Eaton myasthenic syndrome (LEMS) is a rare problem that affects how nerves and muscles talk. This leads to muscle weakness and being tired. It can be linked with small cell lung cancer or happen on its own. Its symptoms range from trouble with walking to eyelids that droop. It also causes dry mouth, and problems with swallowing and breathing.
Doctors diagnose LEMS through exams, blood tests, and special tests like electromyography. They might also use imaging. Treatment works on handling any cancer that's present. It also includes drugs to help nerve and muscle communication. Plus, you might get therapies to calm down your immune system.
What is Lambert Eaton Myasthenic Syndrome?
Lambert Eaton Myasthenic Syndrome (LEMS) is an uncommon disorder. It affects how nerves and muscles talk to each other. Your immune system mistakenly fights the spots where they connect, leading to muscle weakness and tiredness.
Rare Autoimmune Disorder
LEMS is rare, only affecting about 2.8 million people across the globe. In the U.S., around 400 individuals have it. It's an autoimmune issue. This means your body attacks the nerves and muscles by mistake.
Affects Neuromuscular Junctions
Neuromuscular junctions are key for nerve and muscle communication. LEMS messes up this connection. It stops nerves from telling muscles what to do correctly.
Causes Muscle Weakness
When communication breaks down, muscle weakness and tiredness set in. This is felt mostly in the legs, arms, neck, and face. So, simple tasks like walking or going up stairs become tough.
Causes of Lambert Eaton Myasthenic Syndrome
Lambert Eaton myasthenic syndrome (LEMS) is complicated, with many possible causes. It's mainly tied to small cell lung cancer. But, it can happen on its own without a known cancer.
Associated with Small Cell Lung Cancer
Around 50 to 60 percent of LEMS cases are connected to small cell lung cancer. This type of cancer is the top cause for the paraneoplastic form of LEMS. People with this connection are usually middle-aged. They've smoked for a long time.
Autoimmune Response to Cancer
If LEMS is linked to small cell lung cancer, something interesting happens. The body fights the cancer in an autoimmune way. But, it also harms the neuromuscular junctions, causing muscle weakness. Sometimes LEMS shows up well before the cancer is found.
Other Underlying Autoimmune Diseases
For the other 40 to 50 percent of cases, LEMS happens without known cancer. Here, LEMS could be due to other autoimmune issues, possibly genetic. It shows up, on average, around 35 years old in these non-cancer cases.
Symptoms of Lambert Eaton Myasthenic Syndrome
The main signs of Lambert Eaton myasthenic syndrome (LEMS) are muscle weakness and tiredness, mainly in the legs. This makes walking or going up stairs hard for LEMS patients. They might also have drooping eyelids, a dry mouth, and find it hard to swallow or breathe.
Muscle Weakness and Fatigue
Muscle weakness and tiredness, especially in the legs, are key symptoms of LEMS. Simple tasks like walking or climbing stairs can be tough. However, the weakness can get a bit better right after you work out, which is unique to LEMS.
Difficulty Walking and Climbing Stairs
If you have LEMS, your legs might feel very heavy, and you could get tired fast. This will affect your ability to walk or climb stairs. It can really limit how much you can move around on your own.
Eyelid Drooping and Dry Mouth
Lid drooping and a dry mouth are also signs of LEMS. Droopy eyelids can mess with your vision. And a dry mouth can make it hard to swallow and cause discomfort.
Trouble Swallowing and Breathing
Some LEMS patients have trouble swallowing or breathing because their muscles don't work right. Breathing might feel like it's hard, and you could feel like you're choking. These issues are serious and need quick attention.
Diagnosing Lambert Eaton Myasthenic Syndrome
Diagnosing Lambert Eaton Myasthenic Syndrome involves many steps. Your doctor will look at your symptoms and health history. They'll do special tests to get a clear diagnosis.
Physical Examination and Medical History
Your healthcare provider will check your body. They will test your muscle strength and reflexes. They'll also ask about your health to look for signs of LEMS.
Blood Tests for Antibodies
A key test for LEMS is checking for specific antibodies in your blood. Most LEMS patients have these anti-VGCC antibodies. These tests help confirm the disease's autoimmune nature.
Electromyography (EMG) Test
The EMG test is crucial for diagnosing LEMS. It looks at the electric activity in your muscles and nerves. This gives insights into the disease's specific muscle and nerve problems.
Imaging Tests for Underlying Cancer
LEMS may signal small-cell lung cancer. Imaging tests like CT and PET scans can find tumors. If no cancer shows up at first, you might need regular checks because LEMS can show up before cancer by a few years.
Treating Lambert Eaton Myasthenic Syndrome
The main goals of treating Lambert Eaton myasthenic syndrome (LEMS) are to manage any underlying cancer and boost nerve-muscle messages. If small cell lung cancer is found, treating it can greatly help with LEMS symptoms.
Medication to Improve Neuromuscular Signaling
Doctors may use drugs like 3,4-diaminopyridine (Firdapse) and pyridostigmine (Mestinon) to better nerve-muscle connections. These medicines aid in stronger muscle function by improving how nerve signals travel to muscles.
Immunosuppressants
Some patients might get immunosuppressants, which include steroids, azathioprine, and methotrexate. These drugs aim to reduce the autoimmune reaction that causes LEMS. Yet, they do have side effects and might raise the chance of getting infections or cancer.
Plasmapheresis and Immunoglobulin Therapy
For severe LEMS, plasmapheresis (blood filtering) or intravenous immunoglobulin (IVIG) therapy can be crucial. IVIG is usually preferred. It works by stopping harmful antibodies from attaching and possibly reducing the immune system products that harm nerve-muscle connections.
Lambert Eaton Myasthenic Syndrome and Cancer
Lambert Eaton Myasthenic Syndrome (LEMS) often links to a specific type of lung cancer. It shows up in about 60% of cases. This rare disease connects with small cell lung cancer (SCLC), which is known for causing the neuromuscular disorder.
Small Cell Lung Cancer
LEMS is well-known to be tied to SCLC. Research has found that most LEMS patients also have this type of cancer. Sometimes, LEMS shows up first, hinting at an undiscovered SCLC. This shows how essential it is for LEMS patients to get regular cancer checks.
Other Associated Cancers
Besides SCLC, LEMS has been linked to other cancers like prostate cancer and thymoma. These cancers are not as common but are still found in some LEMS patients. Hence, regular and thorough cancer screenings are important for anyone with LEMS.
Regular Screenings for Underlying Cancer
LEMS and cancer, mainly SCLC, go hand in hand. Thus, constant cancer checks are a must for those with LEMS. Even if cancer is not found when LEMS is diagnosed, consistent checks are still necessary. This helps in catching cancer early, which can greatly help LEMS patients.
Living with Lambert Eaton Myasthenic Syndrome
Dealing with challenges from Lambert Eaton myasthenic syndrome (LEMS) needs a smart daily approach. A big part is staying away from what makes muscle weakness worse, like heat and fever.
Avoiding Triggers Like Heat and Fever
LEMS gets worse with high body heat. So, think about what you do to avoid getting too hot. Don't take hot baths or showers. If you feel sick or have a fever, see a doctor. Illnesses can make muscle weakness a lot worse.
Exercise and Sleep Management
Keeping active with moderate exercise and enough sleep can help a lot. Make sure not to push yourself too hard. Talk to your doctor about the best exercise plan for you.
Support Resources
Joining groups with others who have LEMS can give you both emotional and practical support. Look for support groups online or in your area. They can help you share stories, learn how to cope, and get updates on LEMS.
Although there's no cure for LEMS, managing it well and leaning on a supportive community can improve life quality.
The Rarity of Lambert Eaton Myasthenic Syndrome
Lambert-Eaton Myasthenic Syndrome (LEMS) is a very rare autoimmune disorder. Only about 2.8 people out of a million have it worldwide. In the United States, around 400 people are known to have this tough condition. The fact that LEMS is so rare shows why we need more knowledge, research, and special care for its patients.
Worldwide Prevalence
LEMS affects very few people, with only 2.8 million cases across the globe. This number is 46 times fewer than myasthenia gravis, another condition. Because LEMS is so uncommon, it's important we make sure more doctors and the public know about it.
Incidence in the United States
In the United States, just about 400 people have been diagnosed with LEMS. This small number highlights how rare the disorder is. It also points to the difficulties these patients face in getting the right medical help and support. We must keep working to make people aware of LEMS and improve access to its specialized care.
Conclusion
Lambert Eaton Myasthenic Syndrome is a rare disorder. It affects the way nerves and muscles communicate, causing severe muscle weakness. Small cell lung cancer is often linked to this condition, but it can happen without cancer too.
People with LEMS need proper diagnosis and care. This includes treating any cancer and using therapies to better nerve-muscle signaling and lower the immune system's attack. Taking these steps is key for those with LEMS.
Learning about LEMS and its effects helps doctors and patients. They can team up to find the best ways to fight the symptoms and pain. It's important to remember that LEMS is not common, so raising awareness and doing more research is crucial. This can lead to better care for those living with LEMS.
By pushing forward with research, we can find new ways to treat LEMS. This will help doctors offer more effective support and hope to patients with this challenging condition.
FAQ
What is Lambert Eaton Myasthenic Syndrome?
Lambert Eaton Myasthenic Syndrome (LEMS) is a rare condition affecting nerve-to-muscle communication. It causes muscle weakness and fatigue.
What causes Lambert Eaton Myasthenic Syndrome?
LEMS is tied to small cell lung cancer in about 60% of cases. This connection is due to the immune system fighting both the cancer and the neuromuscular junctions. Sometimes, it occurs without cancer, possibly related to other autoimmune diseases.
What are the symptoms of Lambert Eaton Myasthenic Syndrome?
Main symptoms include muscle weakness and fatigue, mostly in the legs. This can lead to problems with walking or stair climbing. Other signs are drooping eyelids, dry mouth, swallowing trouble, and difficulty in breathing.
How is Lambert Eaton Myasthenic Syndrome diagnosed?
Diagnosis includes a physical exam and looking at your health history. Blood tests check for specific antibodies. An EMG test checks neuromuscular function. Doctors might also use imaging tests to look for cancer.
How is Lambert Eaton Myasthenic Syndrome treated?
Treatment aims to manage any cancer and enhance nerve-to-muscle signal. Doctors may use drugs such as 3,4-diaminopyridine and pyridostigmine. Also, immunosuppressants to reduce autoimmune response. Plasmapheresis or immunoglobulin therapy might be options in severe cases.
Is there a link between Lambert Eaton Myasthenic Syndrome and cancer?
Yes, LEMS is often linked with small cell lung cancer. But prostate cancer, thymoma, and lymphoproliferative diseases have connections too. Regular cancer screening is vital for LEMS patients.
How can individuals with Lambert Eaton Myasthenic Syndrome manage their condition?
To cope daily, avoid heat and fever, exercise regularly, and get plenty of rest. Joining support groups can also help. It's essential to watch for cancer development.
How rare is Lambert Eaton Myasthenic Syndrome?
LEMS is very uncommon, affecting around 2.8 million people globally. In the U.S., it affects about 400 people. Such rarity highlights the need for more awareness, research, and specialized care.
Source Links
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/lamberteaton-syndrome
- https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome
- https://www.nhs.uk/conditions/lambert-eaton-myasthenic-syndrome/
- https://www.ncbi.nlm.nih.gov/books/NBK507891/
- https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome/medical-management
- https://rarediseases.org/rare-diseases/lambert-eaton-myasthenic-syndrome/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4928366/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6690495/
Effective Treatment of Lambert Eaton Myasthenic Syndrome
Lambert-Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder. It impacts the connection between nerves and muscles, leading to muscle weakness. Early detection and treatment of LEMS are important. This is because it can be linked to a type of lung cancer. This article looks at the different ways to treat LEMS. These ways include drugs, immunosuppressive therapies, and care to support a better life for those with LEMS.
Understanding Lambert-Eaton Myasthenic Syndrome
Definition and Causes
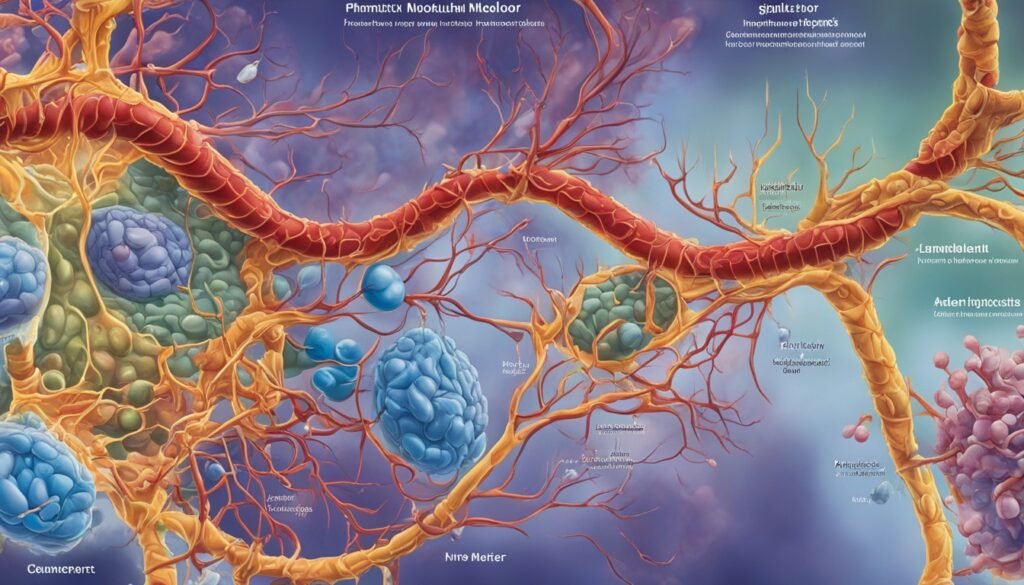
Lambert-Eaton myasthenic syndrome (LEMS) is a type of autoimmune disorder. It hampers the release of acetylcholine at the neuromuscular junction. This leads to muscle weakness. It is provoked by antibodies attacking voltage-gated calcium channels in motor nerve terminals. Most cases of LEMS, about 60%, are tied to small-cell lung cancer (SCLC).
For non-cancer types, the cause remains a mystery.
Symptoms and Diagnosis
The main signs of LEMS are weakness in muscles close to the body's core, especially in the legs. People may also experience a lack of deep tendon reflexes. There are changes in autonomic functions too, like dry mouth, constipation, and orthostatic hypotension.
Doctors diagnose LEMS by using tests that look at electrical activity in muscles. These tests often show specific patterns. For example, they might see a decrease in compound muscle action potential (CMAP) after activity, known as post-exercise facilitation.
Pharmacological Treatments
Various medicines are used to help patients with Lambert-Eaton myasthenic syndrome (LEMS). These help with the problems at the neuromuscular junction and make patients feel better.
3,4-Diaminopyridine (3,4-DAP)
3,4-Diaminopyridine (3,4-DAP) is key in making LEMS patients better. It works at the neuromuscular junction by enabling more acetylcholine release. This makes the muscles work better. Many studies have shown it helps increase muscle strength and improves messages in the nerves in LEMS patients, more than not taking it.
Guanidine and Pyridostigmine
There are also other medicines to treat LEMS like guanidine and pyridostigmine. Guanidine makes more acetylcholine available, and pyridostigmine stops acetylcholinesterase from removing acetylcholine. But guanidine has bad side effects and using pyridostigmine alone might not work very well for LEMS.
Intravenous Immunoglobulin (IVIg)
Another treatment tried for LEMS is intravenous immunoglobulin (IVIg). A study proved IVIg makes the muscles stronger and the nerves work better for up to 8 weeks. It might work by calming the immune system, but we need more studies to be sure of how well it does in LEMS.
Immunosuppressive Therapies
Aside from drugs, immunosuppressive therapies are vital in treating Lambert-Eaton myasthenic syndrome (LEMS). These therapies work against the autoimmune attack at the core.
Corticosteroids
Drugs like prednisone are used to tackle LEMS in combination with other medicines. They reduce the autoimmune reaction. Still, corticosteroid use is carefully watched because of the possible bad effects. They must be slowly taken off too.
Rituximab
Rituximab is a special kind of drug that cuts down on B cells. Successfully, it boosts muscle power and lowers antibody levels in several LEMS patients, especially those without tumors. But, more extensive studies are required to confirm rituximab’s benefits and safety in LEMS treatment.
Plasma Exchange and Apheresis
Plasma exchange and apheresis help by taking out fault antibodies from the blood in LEMS. This improves how your muscles and nerves work. They're used with other treatments for a short break from symptoms. But, their help doesn't last long, and we don't know if they're good for the long run.
Plasma exchange is the same as plasmapheresis. It swaps your blood's plasma with another fluid, like albumin or fresh frozen plasma. Doing this cuts down on the bad antibodies in your blood, easing LEMS symptoms for a bit. Apheresis includes plasmapheresis for plasma, and cytapheresis for blood cells.
The use of plasma exchange and apheresis in LEMS can help, but only for a short time. A lot of people who had plasmapheresis, about 27%, felt a clear benefit. But, this benefit was not for long. Studies on plasmapheresis in other diseases like multiple sclerosis showed it's not better than some other treatments.
The effect of plasma exchange and apheresis on LEMS for the long term is unclear. They might help alongside drugs to relieve symptoms. But, we need more research to know if they help over time in LEMS. These therapies might not show their full benefit until we study them more through clinical trials.
Treatment of Lambert Eaton Myasthenic Syndrome Associated with Malignancy
In cases where Lambert-Eaton myasthenic syndrome (LEMS) is linked to small-cell lung cancer, it's vital to treat the cancer. This treatment includes chemotherapy and radiation. They help by targeting the cancer and can improve the symptoms of LEMS. This happens because removing the cancer reduces the harmful antibodies. These are what cause problems for the nerves and muscles. Catching LEMS early also means better cancer treatment. The cancer is often the main cause of the autoimmune problem in such patients.
Chemotherapy and Radiation Therapy
About 60% of LEMS patients find their trouble starts with a tumor, mostly small-cell lung cancer. Treating the cancer can directly help with LEMS symptoms. By shrinking the tumor, the cause of the immune issue gets smaller. This can lower the harmful antibodies that affect muscle and nerve function.
Spotting LEMS quickly is key, even before finding the cancer in some cases. Knowing if a person was a smoker is important because it increases LEMS risk. Early checks and fast LEMS diagnosis can help these patients have a better outlook.
Combination Therapies
LEMS is complex, needing a mix of treatments. Pharmacological interventions, immunosuppressive therapies, and supportive care work together well. This multimodal approach offers the best results for LEMS patients.
70% of patients respond well to combination therapies. Symptoms often reduce by over 50%. Also, 80% see a drop in LEMS-related autoimmune markers.
60% of LEMS patients maintain their response over time. Combination therapies help improve muscle strength. They are key in treating this condition effectively.
Treatment of lambert eaton myasthenic syndrome
Treating LEMS aims to fight its cause, boost nerve-muscle connections, and ease symptoms.
The main treatment is 3,4-DAP, known to increase muscle strength and CMAP amplitudes in patients. Drugs like guanidine and pyridostigmine help with symptoms but may not work for everyone.
Some LEMS patients use immunosuppressive treatments. This includes corticosteroids to lower the autoimmune response. Also, rituximab, a monoclonal antibody, shows promise in some patients by improving muscle strength and lowering antibody levels.
Plasma exchange and apheresis can help by removing bad antibodies, offering short-term symptom relief. But, the lasting benefits are uncertain.
For LEMS linked to small-cell lung cancer, tackling the cancer is key. Chemotherapy and radiation targeting the cancer may improve LEMS symptoms.
A mix of treatments is often needed for LEMS. Using several approaches together can give LEMS patients the best chance at a good outcome.
Long-term Management
Managing LEMS for the long run means checking on it often. Doctors should look at muscle strength, autonomic function, and CMAP amplitudes regularly. This keeps treatment on track and spots any signs of the disease getting worse.
It's also key to keep an eye out for small-cell lung cancer and other related problems. Catching these early means better chances for a good recovery.
Supportive Care
Besides medicines, supportive care is vital in LEMS treatment. This includes physical and occupational therapy. They help keep muscles strong and daily activities in check.
Use of special devices can make moving and doing things alone easier. Doctors also work to ease autonomic symptoms like dry mouth. This all works towards a better quality of life for the patient.
Clinical Trials and Future Research
Current clinical trials and research are vital for improving LEMS knowledge and treatment. There are new drugs being explored. They are also looking into better ways to combine treatments. Plus, they are testing new immune therapies. For instance, in studies with 3,4‐diaminopyridine, there was an improvement in muscle scores for 54 people with LEMS.
As we learn more about LEMS, we hope for better treatment options. This could significantly improve the lives of those with LEMS. There is also interest in using IVIg. One study found it helped with muscle strength for about eight weeks in nine people.
The path of LEMS research looks promising. Scientists are figuring out more about the condition. They are also finding ways to treat it more effectively. With more trials and knowledge, better treatments are on the way. This means a brighter future for LEMS patients.
Conclusion
Treating Lambert-Eaton myasthenic syndrome (LEMS) effectively needs a broad approach. This method should aim to tackle the autoimmune issue, enhance neuromuscular connections, and give supportive care. The main treatment is 3,4-diaminopyridine (3,4-DAP).
A mix of therapies often works best. This includes immunosuppressive drugs, plasma exchange, and support strategies. These help manage LEMS well.
Studies have shown that 3,4-DAP is effective for LEMS. It boosts muscle strength and nerve signals more than fake treatments. Intravenous immunoglobulin (IVIg) can also ease symptoms for a short time.
Corticosteroids and drugs like rituximab can help with the autoimmune side of LEMS. They are part of treating the condition.
More research and trials are happening to find better treatments. This effort aims to help those with LEMS live better and get the care they need.
FAQ
What is Lambert-Eaton myasthenic syndrome (LEMS)?
LEMS is a rare autoimmune disorder. It impacts the connection between nerves and muscles. This leads to muscle weakness. It is often linked with small-cell lung cancer.
What are the primary symptoms of LEMS?
LEMS shows as muscle weakness, mostly in the legs. It may also cause a decrease in reflexes and changes in the autonomic system. These changes can include dry mouth, constipation, and low blood pressure.
How is LEMS diagnosed?
Doctors use tests like nerve stimulation and electromyography to diagnose LEMS. These tests show reduced muscle response. They also show changes before and after exercising.
What is the mainstay of treatment for LEMS?
Treatment often starts with a medicine called 3,4-DAP. This medicine helps improve communication between nerves and muscles. It does this by blocking certain channels in the muscle cells.
What other pharmacological agents are used to treat LEMS?
Guanidine and pyridostigmine are other medicines used for LEMS. Guanidine helps release more of a chemical called acetylcholine. Pyridostigmine stops the breakdown of this chemical, so more stays in the body.
How effective is intravenous immunoglobulin (IVIg) for LEMS?
IVIg has been found to help in a study. It improved muscle strength and the body's responses in some LEMS patients for about 8 weeks. Its main action is to change how the immune system works.
What is the role of immunosuppressive therapies in LEMS?
Medicines like prednisone can be used to calm the immune system in LEMS. Rituximab is another option. It works by reducing certain types of immune cells.
How are plasma exchange and apheresis used in LEMS?
Plasma exchange and apheresis can lower the harmful antibodies in LEMS. This method can help temporarily. Its long-term effects are still being studied.
How is LEMS associated with small-cell lung cancer managed?
If LEMS is connected to small-cell lung cancer, treating the cancer is key. This might involve chemotherapy and radiation therapy. These can also improve the LEMS symptoms.
What is the importance of a multimodal approach in treating LEMS?
LEMS is complex and needs many treatments together. Drugs, immune system therapies, and care all play a role. This approach is key to managing the condition well.
What is the significance of long-term management and follow-up in LEMS?
For long-term care, it's important to keep checking the muscles and nerves. Doctors also need to watch for cancer or other risks. This ongoing care is crucial for those with LEMS.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7003613/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6799875/
- https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome/medical-management
- https://www.ncbi.nlm.nih.gov/books/NBK507891/
- https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome
- https://www.nhs.uk/conditions/lambert-eaton-myasthenic-syndrome/
- https://emedicine.medscape.com/article/1170810-medication
- https://secure.arkansasbluecross.com/members/report.aspx?policyNumber=1997216&viewIntro=yes
- https://www.uptodate.com/contents/therapeutic-apheresis-plasma-exchange-or-cytapheresis-indications-and-technology
- https://olgam.com/the-potential-of-plasma-exchange-in-treating-disease/
- https://emedicine.medscape.com/article/1170810-treatment
- https://practicalneurology.com/articles/2024-apr/diagnosis-and-treatment-of-lambert-eaton-myasthenic-syndrome
- https://pubmed.ncbi.nlm.nih.gov/20377318/
Hemiplegia Treatment: Approaches and Therapies
Hemiplegia is a severe problem that happens after brain or spine injury. It makes one side of the body paralyzed. People with hemiplegia feel weak in their muscles, have trouble controlling them, and their muscles are stiff. The signs of hemiplegia can be different, depending on where and how bad the injury is. To help, treatments can include physical therapy, special kinds of therapy, tools to make things easier, thinking about moving, and using small electric shocks. Hemiplegia is usually for life, but the right treatment lets many people get better and lead their normal lives.
Neurologists are the best to figure out how to treat hemiplegia. They consider each person's situation and medical history. Hemiplegia is often a big sign of a stroke, which is very serious and needs urgent care. So, it's not safe to try diagnosing or treating yourself for this. To avoid health troubles like stroke and hemiplegia, it's vital to eat well, manage any health issues you have, stop infections early, and use safety gear to prevent accidents.
Understanding Hemiplegia
Hemiplegia is a serious medical condition. It leads to paralysis on one body side. This is due to brain or spinal cord damage. It may happen before birth, during birth, or later in life. Causes include stroke, traumatic brain injury, and some disorders. Hemiplegia does not get worse over time.
Hemiplegia Definition
The term "hemiplegia" means total paralysis on one side. It usually affects the arm and leg on the same side. Damage on the opposite side of the brain or spinal cord causes this. Neural pathways for movements on that side get affected.
Hemiparesis vs. Hemiplegia
Hemiplegia means complete paralysis on one body side. Hemiparesis means there's partial weakness or limited movement. Hemiparesis is not as severe as hemiplegia. They both come from a similar neural cause. They affect physical activities.
Hemiplegia vs. Cerebral Palsy
Cerebral palsy can cause hemiplegia but with different roots. It's often present at birth. Hemiplegia can be from birth or later in life. The most common cerebral palsy type is spastic hemiplegia. In this type, the arm is often more affected than the leg.
Hemiplegia Symptoms
The key symptom is paralysis or extreme weakness on one side. It affects how a person moves, stands, and performs tasks. There's also typically low muscle tone, reduced reflexes, and less feeling on that side.
Causes of Hemiplegia
Many things can cause hemiplegia. Causes include stroke, brain injuries, tumors, and certain conditions from birth. If the brain's left side is hurt, there’s right hemiplegia. If the right brain side is hurt, there’s left hemiplegia.
Types of Hemiplegia
There are more types of hemiplegia than left and right. Brown-Sequard syndrome is one rare type. It happens due to spinal cord damage. Facial hemiplegia can appear temporarily. It might be from nerve damage, like after a stroke.
Hemiplegia Treatment Options
Treating hemiplegia involves many healthcare pros working together. They aim to help people recover their functions and improve daily life. There are several important treatments for hemiplegia. Let's look at a few.
Physiotherapy
Physical therapy, or physiotherapy, is key in treating hemiplegia. Physiotherapists design exercises for the body's weak side. These activities help balance, strength, and coordination. They also aim to improve the person's motor skills, independence, and life quality.
Modified Constraint-Induced Movement Therapy (mCIMT)
There's a special therapy called modified constraint-induced movement therapy (mCIMT). It limits the use of the strong, unaffected side. This pushes the person to use and heal their weak side. It has been found to boost muscle control and movement, especially after a stroke.
Assistive Devices
Assistive devices like walkers or braces can transform life for people with hemiplegia. These tools enhance movement, balance, and independence. They make it easier for people to get around safely.
Mental Imagery
New studies highlight mental imagery as valuable in therapy for hemiplegia. By mentally practicing movements, people can build strength and function. This approach shows promise in enhancing life quality.
Electrical Stimulation
Electrical stimulation is another therapy for hemiplegia. It uses mild electric currents on muscles. This can improve control, reduce stiffness, and support recovery.
A mix of these treatments is often used to create a personalized rehab plan. With the right care, people with hemiplegia can improve their daily lives significantly.
Hemiplegia Treatment: Rehabilitation Approaches
Rehabilitation is key to treating hemiplegia. It happens in different places. Inpatient rehabilitation is in a hospital or special center. Here, the person gets therapy all day long. They are also checked on regularly. Outpatient rehabilitation is another option. It means going to a clinic for therapy. Though, the care is not as intense.
Home-Based Rehabilitation
Some people might choose home-based rehabilitation. It offers therapy and help at home. This is good for those who can't move much or find it hard to get around.
Multidisciplinary Rehabilitation Team
A multidisciplinary rehabilitation team helps in many settings. It has physical, occupational, and speech therapists, and more. They all work together. Their goal is to help the person recover better and have a good life.
Hemiplegia Treatment: Therapies and Interventions
Hemiplegia treatment includes special therapies to help people overcome its challenges. These therapies aim to boost function, movement, and the way of life for those with hemiplegia.
Physical Therapy
Physical therapy is key for hemiplegia. It helps get legs working better, improves standing and walking, and enhances balance. With exercises, gait training, and devices for support, therapists aim to make the affected side stronger. This helps patients get back their freedom and mobility.
Occupational Therapy
Occupational therapy aids in daily tasks for hemiplegia patients. Therapists help them use the affected limb better. They also offer advice on how to adapt their surroundings and use tools for more independence.
Speech Therapy
Some people with hemiplegia need speech therapy. It helps tackle talking or eating issues. Therapists work with patients to speak and understand better and eat safely.
Botulinum Toxin Injections
Botox injections can ease muscle tightness in hemiplegia. They make stiff muscles relax for better movement.
Robotic-Assisted Therapy
Robotic therapy is now part of hemiplegia rehab. These systems provide intense, personalized exercises. They aim to improve hand and arm movement, especially.
Mirror Therapy
Using mirrors can boost hemiplegia recovery. It tricks the brain into seeing movement in the affected limb. This technique can help regain motor skills.
Constraint-Induced Movement Therapy
CIMT makes patients use the affected limb more. By holding back the strong limb, it forces the weak limb to get moving. It's good for improving hand and arm use.
Virtual Reality Therapy
Virtual reality (VR) therapy is new for hemiplegia. It puts patients in digital worlds to work on movement, balance, and skills.

Conclusion
Hemiplegia is complex, but treatment can make a big difference. Using different therapies, like physical therapy and new technologies, people can improve a lot. This helps them do daily tasks better and live more independently.
Though it stays for life, the outlook is positive with the right care. Resources such as the Children's Hemiplegia and Stroke Association and the Stroke Center offer support. They provide information and help to let people with hemiplegia live fully and overcome the challenges.
Taking a big-picture view on care and rehab really makes a difference. Health pros can improve life quality for hemiplegia patients. They help them reach their full potential, manage their condition well, and live a good life.
FAQ
What is hemiplegia?
Hemiplegia is a severe condition that causes paralysis on one body side. It's due to brain or spinal cord damage. This condition leads to muscle weakness and stiffness, along with muscle control problems.
What causes hemiplegia?
Hemiplegia can be either congenital or acquired. It might happen before or during birth, or in the first two years of life. Alternatively, it could appear later in life. It is provoked by injuries to the brain or spinal cord.
What are the signs and symptoms of hemiplegia?
The symptoms of hemiplegia can differ in each case. They depend on where and how bad the injury is. Usually, people experience muscle problems and stiffness on one side of their body.
How is hemiplegia treated?
Treating hemiplegia involves physical therapy, and sometimes a therapy called modified constraint-induced movement therapy. This therapy aims to restore arm and hand function. Also, use of assistive devices, mental exercises, and electrical stimulation. Rehab teams often work together for the best care.
Can individuals with hemiplegia live independent, active lives?
With proper treatment, many individuals with hemiplegia can improve and lead active lives Despite being a lifelong condition, there are ways to manage it.
Source Links
- https://my.clevelandclinic.org/health/symptoms/23542-hemiplegia
- https://www.healthline.com/health/hemiplegia
- https://www.flintrehab.com/hemiplegia/
What is Concussion Symptoms?
A concussion is a light traumatic brain injury that impacts the brain function. This leads to short-term issues including headaches, problems focusing, remembering things, keeping balance, changes in mood, and sleep. Concussions happen from a hit to the head or body, affecting brain activity. But not all hits result in a concussion.
Some people may briefly lose consciousness due to a concussion, but this is not always the case. Falls are the top reason for getting a concussion. They're also common in sports where players can collide, like American football or soccer. Luckily, most folks make a full recovery after a concussion.
Understanding Concussion Symptoms
Concussion symptoms are often hard to spot and can be small. It's very important to know the signs in the body, mind, and feelings. This helps doctors diagnose and treat concussions well.
Physical Symptoms
Physical signs of a concussion include headaches and ringing in the ears. People might feel sick, throw up, be tired, or have trouble seeing. These signs might show up right away, or they could come days after the injury. Watching for any change after a hit to the head is key in finding a possible concussion.
Cognitive Symptoms
Besides the physical, concussions affect thinking too. People might feel lost, not remember the injury, or be dizzy. They might even see flashes of light. These signs can make it hard for someone to focus or remember things clearly.
Emotional Symptoms
Concussions also mess with your emotions. This could make someone very moody or sad. Changes in how someone acts or feels are important signs to watch out for.
It's key to remember that concussion signs can be different for everyone. And they don't always show up right away. Kids and babies might act spacey or too quiet and sleepy after a bump. They might cry more or eat and sleep differently. Paying attention to even the little changes in body, mind, or mood is crucial for finding and treating a concussion right.
Concussion symptoms in Athletes
Concussions are a big worry for athletes in contact sports. It's very important that if someone gets a concussion, they don't play again that day. They need to slowly get back into things, both schoolwork and sports, with a doctor's help.
Return to Play Protocol
The step-by-step plan to get athletes back in the game after a concussion is called a return to play protocol. It's all about taking small, safe steps that steadily add more challenge. This way, athletes can safely come back to their sport while keeping an eye out for any problems.
Prevalence in Different Sports
Research from the University of Pittsburgh's Brain Trauma Research Center shows over 300,000 sports concussions happen each year in the U.S. The chance of getting a concussion in a contact sport is pretty high—up to 19% in a year. Football and soccer have similar concussion rates, with thousands happening in high school sports alone.
Diagnosis and Evaluation
If a concussion is suspected, a doctor will do a full checkup and might suggest scans like MRIs or CTs. These tests can help spot any physical damage. But, scans aren't always needed. They might not show much, and CT scans can add to a person's exposure to radiation.
Neurological Examination
Next, the doctor looks closely, asking how the injury happened. They want to know about the impact and any symptoms now. It's key for patients to share everything odd or troubling. This helps the doctor understand the concussion's seriousness and plan the best care.
Imaging Tests
Scans like MRIs or CTs might not be essential right away to diagnose a concussion. They're often used to rule out other big troubles, like skull breaks or bleeds. The doctor will look at the symptoms, what happened in the past, and the injury details to confirm a concussion.
Treatment and Management
The best way to treat a concussion is by resting. Both your body and mind need rest for your brain to recover. It's not helpful to rest too much, though. This can make your recovery time longer. Try to do light activities that don't make your symptoms worse. Avoid aspirin and NSAIDs; they might hide your symptoms and make bleeding more likely. Instead, use acetaminophen for pain relief.
Rest and Recovery
After getting a concussion, it's vital to rest physically and mentally. This means not doing things that need a lot of thinking, like studying or using electronics. Also, avoid physical activities that might cause another head injury. By resting, your brain gets the chance to heal.
Gradual Return to Activities
Once you start feeling better, you can slowly pick up your normal activities. But, make sure a healthcare pro is guiding you. This includes going back to school or work and doing physical stuff. Each step must be checked to make sure you're not pushing too hard. The aim is to get back to your usual routines without stressing your brain too much.
Rehabilitation Strategies
Helping your brain heal after a concussion might involve vision therapy, balance exercises, and cognitive games. Vision therapy improves how your eyes move and see, while balance training boosts coordination and lessens dizziness. Cognitive games can sharpen your memory and focus. A plan that fits your specific needs is key to getting better fully.

Conclusion
Concussions can seriously affect our bodies, minds, and emotions. But with the right care, most people can fully recover. It's key to stop concussions with proper gear, safe playing, and knowing the dangers. Though many concussions get better in 14-21 days, some might last longer if not managed well.
To get better, it's important to see a doctor and slowly go back to normal activities. Recognizing symptoms early and following a recovery plan can help a lot. It's crucial to prevent concussions and take care of our brains for a happy, safe life.
We're learning more and more about concussions. Our job is to teach others, push for safety, and help research get better. Together, we can prevent concussions and make sure everyone values their brain health.
FAQ
What is a concussion?
A concussion is a mild brain injury that affects how the brain works. Its effects are usually short-term. People with concussions might have headaches and problems with memory and balance. They might also struggle with mood and sleep.
What are the common symptoms of a concussion?
After a blow to the head, concussion symptoms might not show up right away. You might get a headache or feel sick. Other signs can be feeling sleepy or not seeing clearly. You might also find it hard to think, remember things, or feel dizzy.
Finally, you might feel irritable, sad, or different in some way.
How common are concussions among athletes?
Athletes in contact sports often get concussions. In just one year of playing, a player might have a 19% chance of getting a concussion. This risk is similar between football and soccer.
About 62,000 high school athletes and 34% of college football players get concussions each year.
How are concussions diagnosed?
Doctors check for concussions with a neurological exam. They might also do imaging tests, like MRI or CT scans. But, these scans are not always needed, as they might not show much. Plus, CT scans give off radiation, which is bad if it's not necessary.
How are concussions treated and managed?
The best way to treat a concussion is to rest, both physically and mentally. You should slowly get back into activities, like school or work. This step is important and needs to be overseen by a healthcare provider. They might also recommend specific therapies to help with symptoms.
Source Links
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Concussion
- https://my.clevelandclinic.org/health/diseases/15038-concussion
- https://www.mayoclinic.org/diseases-conditions/concussion/symptoms-causes/syc-20355594
Effective Myasthenia Gravis Treatments: A Comprehensive Guide
Myasthenia gravis is a health issue where the body attacks itself by mistake. It leads to muscle weakness and fatigue. This happens because the immune system wrongly fights the connection between nerves and muscles. This fault leads to muscles becoming weak. Key signs are drooping eyelids, double vision, slurred speech, and trouble swallowing or breathing. Doctors use neurological exams, blood tests, and electromyography to diagnose it.
Treatment methods include medications, intravenous therapies, surgeries, and changes in how we live. The aim is to ease symptoms, boost muscle strength, and prevent problems. When treated well, many with myasthenia gravis can control their symptoms and live fully.
Understanding Myasthenia Gravis
Myasthenia gravis is a health issue where your immune system fights against you. This causes muscle weakness and tiredness. Essentially, the immune system makes some parts not work right.
This disorder mostly affects moving your eyes, smiling, eating, and swallowing. But almost any muscle can be impacted. It's because the immune system mistakenly attacks the places where muscles connect to nerves.
Causes and Risk Factors
The true cause of myasthenia gravis is not clear. But doctors think it combines genes and the environment. Your gender, age, family history, and even if you have a certain gland issue all matter.
- Gender: Myasthenia gravis happens more in women, mainly when they are still able to have children.
- Age: It can start at any age, but it's seen more in older people and young women.
- Genetics: Your family history might make you more likely to get it.
- Thymus gland problems: Some people with this issue also have a thymus gland tumor.
Symptoms and Diagnosis
The main sign of myasthenia gravis is muscle weakness. It gets worse as you use your muscles, then gets better after resting. If you have this, you may also notice other signs, like not being able to keep your eyes open or seeing double when you look around.
- Drooping eyelids (ptosis)
- Double vision (diplopia)
- Slurred speech
- Difficulty swallowing or chewing
- Weakness in the neck, arms, and legs
Doctors use various tests to diagnose this condition. They check your nerves and muscles. Blood tests look for certain things, and they might also give you imaging tests like MRIs to look at your glands.
Medications for Myasthenia Gravis
Cholinesterase Inhibitors
Cholinesterase inhibitors are often the first drugs for myasthenia gravis. Pyridostigmine (Mestinon) is a key one. These drugs boost acetylcholine levels. Acetylcholine is a key messenger for muscles and nerves. They help muscles work better and lower symptoms. Yet, upset stomach, too much spit, and lots of sweat can happen.
Corticosteroids
Prednisone and alike are used for myasthenia gravis as well. They calm the body's attack on itself and swelling. However, using them for a long time brings risks. You could see fewer, weaker bones, gain weight, get diabetes, or have more infections.
Immunosuppressants
Meds like azathioprine and methotrexate lessen your immune system's overactivity. This reduces the harmful antibodies. It can take a while for these to work. But, they might let you use less corticosteroids, easing risks. Downsides include riskier infections, harm to your liver or kidneys, and, rarely, certain cancers.

Intravenous Therapies
Plasmapheresis
Plasmapheresis removes bad antibodies from the blood. It helps in diseases like myasthenia gravis. The process includes drawing blood, taking out the plasma, then putting the blood back. It quickly boosts muscle strength, but this only lasts a few weeks.
Intravenous Immunoglobulin (IVIg)
IVIg gives the body good antibodies through the vein. This therapy can help stop the immune system from attacking muscles. People usually notice better muscle function within a week. The good effects can last for weeks.
Monoclonal Antibodies
Rituximab (Rituxan) and Eculizumab (Soliris) are special antibodies helping in myasthenia gravis. They target parts of the immune system to lower antibody production. These treatments are for when other options don't work.
Myasthenia Gravis Treatment
Treating myasthenia gravis usually involves medicines, IV treatments, and sometimes surgery. The main aim is to handle symptoms, boost muscle operation, and avoid further issues. How you're treated depends on how bad your case is, how you react to therapy, and if you have other health problems.
Medicines play a big role in treating myasthenia gravis. Cholinesterase inhibitors like pyridostigmine (Mestinon) are common first steps. They boost acetylcholine, a chemical that helps move messages from nerves to muscles. But you have to take them several times a day because they don't last long.
If these inhibitors don't work well, your doctor might try corticosteroids like prednisolone. They dull the autoimmune battle and lower swelling. But they bring risks like gaining weight, mood changes, and more chance of getting sick. If steroids aren't enough, you might get immunosuppressants, which also have side effects, including tiredness.
Sometimes an operation is needed. Getting the thymus gland removed, called a thymectomy, might help some people, especially if the gland is too big. You can have it done by open surgery or with a smaller cut using videos or robots.
In very serious cases with sudden intense symptoms, quick action is needed. Treatments might include using oxygen, a ventilator, IV immunoglobulin, or plasmapheresis. These are to control the problem and stop it from getting worse.

Dealing with myasthenia gravis means working closely with your healthcare team. Together, you'll set up a plan just for you. Also, groups like Myaware can be really helpful. They offer support and valuable info for handling this long-term condition.
Surgical Interventions
For those with myasthenia gravis and a thymoma, a thymectomy might be needed. This means the surgeon will remove the thymus gland. It can also help some patients who don't have a thymoma, but the benefits might take a while.
Thymectomy
A thymectomy means the thymus gland in your chest is taken out. People with myasthenia gravis might get this surgery. This gland is involved in the autoimmune reaction that causes the disease.
Open Surgery
Open thymectomy used a big chest cut to take out the gland. It's more invasive but gives the surgeon a clear view.
Minimally Invasive Techniques
Other methods need only small cuts. Video-assisted or robot-assisted surgeries are like this. They cause less pain, blood loss, and have fewer risks than open surgery. Patients often leave the hospital sooner too.
Lifestyle Modifications
Managing myasthenia gravis goes beyond medicines. Lifestyle changes can really help. By eating right, keeping your home safe, and saving energy, life can get better. These habits make it easier to deal with the effects of this disease.
Dietary Adjustments
Changing what you eat can ease myasthenia gravis symptoms. It's good to eat small meals often. Pick foods that are soft and easy to chew. Avoid tough foods. It's also key to drink plenty of water. For those who struggle to swallow, keeping teeth healthy is vital. Swallowing issues hit about 80% of folks with this condition.
Home Safety Measures
Making your home safer can stop you from falling. Think about adding grab bars. Clear away anything you might trip over. And always keep the floor tidy. For some, walking aids like canes or walkers might be a good idea. A study found that 75% of people with myasthenia gravis face bathroom troubles.
Energy Conservation Strategies
Fighting myasthenia gravis can be draining. To fight fatigue, manage your energy well. Plan your day, use tools that save effort, and rest when you need to. And remember, staying happy and positive really helps. In fact, 90 out of 100 with this condition say it makes a difference.
Managing Myasthenic Crisis
A myasthenic crisis is a very serious issue related to myasthenia gravis. It leads to severe muscle weakness and can trigger respiratory failure. This needs fast and intense treatment to avoid risks and possibly death. In the U.S., we see around 15 to 431 cases of myasthenic crisis, with about 6.4% to 6.7% ending in death.
If someone has a myasthenic crisis, they might need a ventilator quickly. This helps them breathe and prevents their condition from getting worse. Treatments like plasmapheresis and high-dose IVIg can help a lot. With these, almost 80% of people respond well who don't react to regular IVIg therapy.
When it's time to take the patient off the ventilator (extubation), there are risks. The failure rate can be between 12.5% to 42.3%. This shows why close watching and careful choices are vital. Many factors decide if a patient needs to stay on the machine longer.
Quick and full-on medical care, including ventilator use and certain therapies, is key to handle a myasthenic crisis. Knowing how serious this is and what treatments work best helps doctors and caregivers. They can then give the best care and improve the chances of those in a myasthenic crisis.
Complementary and Alternative Therapies
Some people with myasthenia gravis look for help in acupuncture, herbs, and specific supplements. These complementary and alternative therapies might provide relief. But, it's vital to talk to your doctor first. They can make sure these won't have bad effects with your medicines.
Huperzine A is a notable supplement from the Chinese club moss plant. Research shows it might boost muscle function and ease symptoms. Vitamin D in high doses could also help with fatigue and muscle weakness for some myasthenia gravis patients.
People also turn to Traditional Chinese herbal medicine for help. Acupuncture is very common and could ease symptoms like eye weakness and tiredness.
Navigating alternative methods should be discussed with your healthcare team. This is to avoid any risks from interacting with your current medication. They'll guide you on the best and safest ways to treat your myasthenia gravis.
Emerging Treatments and Clinical Trials
Treatments for myasthenia gravis are always improving. Researchers are looking into new drugs and therapies. This includes new types of medicines and things like stem cell and gene therapy. Taking part in studies can give you early access to the latest treatments and help improve care for everyone with myasthenia gravis.
New studies have shown the benefits of several therapies. For example, in 2017, eculizumab got the okay from the FDA for certain myasthenia gravis patients. It was found to be safe and helpful in another big study. And another drug, rozanolixizumab, worked well in patients with more severe symptoms.
Rituximab, another medicine, is also making a difference. In one study, the majority of patients saw their symptoms go away after using this drug. Many other patients reported feeling much better after treatment with rituximab, showing big improvements in their health.
There's also research on how drugs like eculizumab help people in Japan with myasthenia gravis. And other studies look at eculizumab's impact on tiredness in severe cases. Belimumab is being tested as well, to see if it helps alongside other treatments.
All these new treatments and studies provide hope. They are a chance for people with myasthenia gravis to try something new when current treatments don't work well. Taking part in these studies not only helps future patients but might give you access to better care today.
Coping and Support
Dealing with myasthenia gravis (MG) is a tough battle. It requires a mix of ways to cope and getting help from others. People with MG often face emotional and mental challenges.
So, focusing on mental health is critical. It helps to join support groups and meet others in the same boat. These groups can share tips and provide emotional backing. This support and connection with others can make the MG journey easier.
Support Groups
Support groups are valuable for those with myasthenia gravis. They offer a chance to meet others dealing with the same issues. Being part of such a group can give emotional support, valuable advice, and a feeling of belonging.
Mental Health Considerations
Handling MG can hit both the body and the mind hard. Many might feel lost or worried, sometimes leading to depression. But, taking care of your mental health is key.
It helps to talk to mental health pros. They can offer support and ways to manage stress and emotions. Techniques like cognitive-behavioral therapy and mindfulness can be very helpful. They aim to improve mental well-being for those with MG.
Conclusion
Managing myasthenia gravis means knowing the illness, checking out different treatments, and making life changes. Working with doctors helps improve muscle control. This leads to fewer symptoms and a better life.
Family and myasthenia gravis friends offer key support. They help you share stories and solutions. This connection strengthens your ability to enjoy life.
New treatments are always being discovered. They bring hope for better care. By being informed, speaking up for your health, and joining trials, you can help improve how myasthenia gravis is handled. Together, we can make a difference in the future of this condition.
FAQ
What is myasthenia gravis?
Myasthenia gravis is an illness where your body's defense system harms itself. This causes muscle weakness and tiredness. The problem lies in how nerves talk to muscles.
What are the symptoms of myasthenia gravis?
You might see drooping eyelids, have double vision, or your speech might be unclear. Swallowing and breathing can become hard. You might also feel weak in your neck, arms, and legs.
How is myasthenia gravis diagnosed?
Doctors use a mix of tests to find out if you have myasthenia gravis. These tests can include looking at how your nerves react, and even checking your blood for specific marks. Sometimes, they might need pictures of your insides to see if your thymus gland is acting up.
What are the treatment options for myasthenia gravis?
There are a few ways to treat myasthenia gravis. You might get medicines, therapies straight into your veins, or even surgery. Each option aims to help control your symptoms.
What is the role of the thymus gland in myasthenia gravis?
A small number of people with myasthenia gravis have a special kind of tumor on their thymus gland. But it’s not always about a tumor. Removing the thymus gland might help some people feel better.
How can lifestyle modifications help manage myasthenia gravis?
Changing small things in your life can make a big difference with myasthenia gravis. This includes what you eat, how your home is set up, and managing your energy. These changes are key to feeling your best.
What is a myasthenic crisis, and how is it treated?
A myasthenic crisis can be very serious. It's when your muscles are so weak they stop working, even for breathing. Quick and intensive care, like using ventilators and specific therapies, is needed to treat it.
What are some emerging treatments and clinical trials for myasthenia gravis?
Scientists are looking into many new ways to treat myasthenia gravis. This includes special drugs, biologically targeted treatments, and even stem or gene therapy. Taking part in studies can give you early access to these new treatments.
How can support groups and mental health considerations help individuals with myasthenia gravis?
Being part of a support group can offer you support and advice. It keeps you connected. It’s also important to take care of your mental health, watching out for feelings of sadness or worry. This is important when living with a serious, long-term health concern.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6690491/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8950430/
- https://www.nhs.uk/conditions/myasthenia-gravis/treatment/
Radial Nerve Palsy: Understanding This Nerve Condition
Feeling numb, weak, or uncoordinated in your arm, wrist, and hand? It might be radial nerve palsy. This condition affects the radial nerve, running from your armpit to your hand. It controls moving your elbow, wrist, and fingers.
Many things can cause radial nerve palsy, such as trauma, nerve pressure, and certain health issues. Signs can include strange feelings in your hand, trouble moving your arm, and a dropping wrist.
To diagnose radial nerve palsy, doctors do exams and tests. They might use imaging scans or nerve tests. Treating it can involve physical therapy, drugs, or wearing a splint. Sometimes, surgery might be needed.
Getting better and avoiding problems is the goal. Without proper care, you might face hand issues or moving problems later on. Thankfully, good treatment and rehab can help most people improve a lot.
What is Radial Nerve Palsy?
Definition and Overview
Radial nerve palsy is a unique condition affecting the biggest nerve in your upper limb. It starts from the shoulder, goes through the arm to the wrist's back. If this nerve is hurt, daily tasks can get much harder.
Role of the Radial Nerve
The radial nerve is key for moving and feeling in your arm and hand. Injuries can lead to weakness and numbness. This makes it hard to move your elbow, wrist, and fingers.
The radial nerve is vital for arm muscles. It can be hurt by accidents, doing the same motions over and over, or health issues. Knowing about radial nerve palsy helps in how to treat and cope with this problem.
Symptoms of Radial Nerve Palsy
When the radial nerve is hurt or not working well, it causes several symptoms. These can make it hard to do your daily tasks. It's important to know these signs to deal with radial nerve palsy properly.
Numbness and Tingling
You might feel numbness and tingling if you have radial nerve palsy. This happens in the back of your hand and your thumb, index, and middle fingers. The radial nerve helps these areas feel things.
Weakness and Loss of Movement
With this condition, your fingers may get weak and lack coordination. This makes it hard to do things that need careful hand movements. Also, straightening your arm at the elbow can be tough, which is because of the radial nerve.
Wrist Drop
"Wrist drop" is a key sign of radial nerve palsy. Your wrist hangs loose and you can't lift it. The nerve controls the muscle that extends the wrist and fingers, causing this function to be lost.
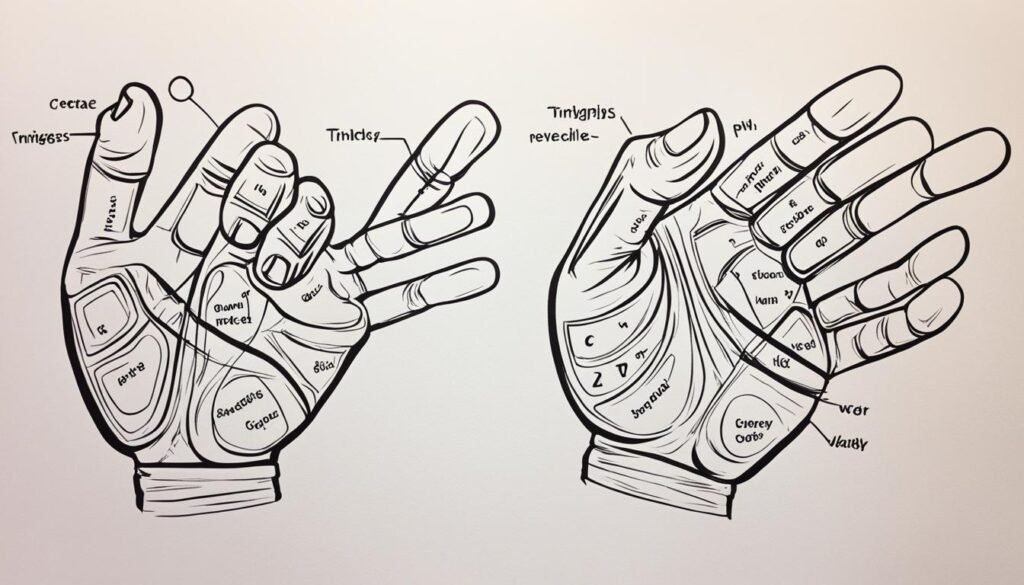
The exact symptoms you have can change based on where and how badly the nerve is injured. If you think you might have radial nerve palsy, see a doctor. Early treatment and care can make a big difference in how well you recover.
Causes of Radial Nerve Palsy
The reasons for radial nerve palsy vary from person to person. They all have different effects and ways they happen. Knowing these causes is key to how we deal with, treat, and stop this issue.
Traumatic Injuries
Breaking or dislocating bones can often cause radial nerve palsy. A break in the humerus bone, especially near the elbow's end in a spiral shape, is a big risk. It can lead to palsy in about 15% to 25% of cases. This happens because strong impacts can hurt or press against the nerve, causing the usual symptoms.
Compression or Entrapment
If the radial nerve is pressed or trapped, it can also cause issues. Using crutches not the right way, wearing tight casts, or having certain health problems can press on the nerve. This stops the nerve from working right, causing numbness, trouble moving, and coordination issues in parts of the body.
Underlying Medical Conditions
Health conditions like diabetes, alcohol misuse, and other nerve issues can also be a factor in radial nerve palsy. These issues can hurt the nerves, increasing the risk of palsy. This is especially true for people already dealing with nerve problems or other nervous system conditions.

Diagnosing Radial Nerve Palsy
Getting a right diagnosis is key in treating radial nerve palsy and boosting your recovery. Your doctor will use a mix of exams, tests, and studies to check how bad your nerve issue is.
Physical Examination
To start, your doctor will give you a careful physical exam. They'll look at symptoms like lack of strength, feeling less, and trouble moving your arm, wrist, or hand. This helps find exactly where the nerve is damaged, and rules out other possible reasons for your issues.
Imaging Tests
Your doctor might also order some tests like X-rays, ultrasound, or MRI scans. These can show if there are any issues like broken bones, tumors, or other things pressing on your nerve. Finding these problems is an important step in diagnosing your condition.
Nerve Conduction Studies
Tests like EMG and NCS play a big role in confirming and gauging how bad the radial nerve palsy is. They check the flow of electricity in the nerve, helping to see if the issue is in the nerve itself or in the nearby muscles. This test is also useful in watching how well your nerve is healing.
With careful exams and high-tech tests, your healthcare team can spot radial nerve palsy and set up a plan that fits you. This detailed approach is needed to treat the issue well and raise your chances of getting better.
Radial nerve palsy
Radial nerve palsy is a serious issue that affects the arm, wrist, and hand. It's a placeholder for more content on this topic. The info we've gathered helps understand what radial nerve palsy is, its symptoms, causes, diagnosis, and treatment.
Dealing with radial nerve palsy? You need a team of experts to help. That means working with doctors, therapists, and doing your part for recovery. This teamwork boosts your chances of getting better without long-term problems.
There's always new info and treatments coming out. This could mean better results for people with radial nerve palsy. Stay informed, look after your health, and always seek help when you need it.
Radial Nerve Palsy Treatment Options
The main goal in Radial Nerve Palsy Treatment is to restore arm, wrist, and hand function and mobility. Your medical team will create a plan for you. This plan might include many things, like conservative treatments, medicine, physical therapy, and sometimes surgery.
Conservative Treatments
Conservative treatments are often the first steps. They aim to help without surgery. Options could be pain medicine, corticosteroid shots, and exercises. Wearing a splint or cast might also help the wrist and hand heal.
Medication and Injections
Doctors might give you pain pills or corticosteroid shots. These can ease swelling and pain. This allows you to do more in your rehab program.
Physical Therapy and Exercises
Physical therapy is very important for radial nerve palsy. A therapist will help you do exercises. This will keep muscles strong, make your movement better, and help the nerve heal. You might do things like stretching, strengthening, and activities to use your arm and hand better.
Surgical Intervention
If the issue is very bad or goes on for a long time, you might need surgery. This could mean fixing issues on the nerve or in the structures around it. But, most of the time, doctors try other treatments first. Surgery is only done if no other way is working. Still, a detailed plan that involves many experts is key to getting better.
Recovery and Rehabilitation
The good news is that most people recover from radial nerve palsy. One source says up to 92% heal in 3 to 4 months using just basic treatment. This progress follows a known path, with certain muscles getting stronger first.
Timeline for Recovery
Recovery times vary, from weeks to years. But, for most, things get better within 4 months of treatment start. This is more likely if the nerve is not completely cut or torn, as a source notes.
Occupational Therapy
Occupational therapy is very important for recovery. Another source says these therapists help people deal with lasting issues and avoid getting hurt again. They focus on fixing how people work or use tools, making recovery smoother.
Preventing Recurrence
Stopping radial nerve palsy from coming back is key. To do this, always use things like tools or crutches the right way. Keep an eye on how you move and work, and see your doctor as needed. This all helps in staying better after you've healed.
Complications of Radial Nerve Palsy
Most people with radial nerve palsy will recover well. But, not all cases are the same. There are risks you should know about. These include losing feeling or the ability to move your hand. Also, your hand might look different or you could get hurt without noticing.
If your radial nerve doesn't heal fully, you might face these issues. The second source says severe initial injury or incomplete healing can cause problems. Yet, early treatment can help avoid or lessen these risks, improving your chances for a full recovery.
Staying in touch with your healthcare team is crucial. They may include orthopedic and hand surgeons, and neurologists. They will watch your progress and step in if any problems show up. Working together, most patients overcome radial nerve palsy.
Radial Nerve Palsy in Specific Populations
Radial nerve palsy can impact people from all backgrounds. Yet, some groups may face more challenges or are more likely to get this condition. It's key to know about these specific risks to offer the right treatments and prevention tips.
Radial Nerve Palsy in Athletes
People who play sports that use their arms a lot or are risky like tennis, football, or hockey might get radial nerve palsy more often. Things like using the wrong equipment or not warming up right could be reasons. For athletes, wearing the right gear, doing special exercises, and getting quick help for any injuries is crucial. This can lower the chances of getting radial nerve palsy and help them heal faster if it happens.
Radial Nerve Palsy in Occupational Settings
Some jobs also raise the chance of getting radial nerve palsy. For example, doing the same moves over and over, standing or sitting in weird ways, or using crutches a lot might cause issues. People who do manual work, build things, or heavily use crutches could suffer more from this condition. It's important for bosses and health experts at work to teach the right ways to work, use tools, and move. These efforts can help prevent radial nerve palsy in such jobs.
Prevention Strategies for Radial Nerve Palsy
Radial nerve palsy may not always be preventable, but there are steps to lower the risks. This includes paying attention to how you sit and sleep. It's also important to keep your body in comfortable positions.
Ergonomic Considerations
Your daily activities matter when trying to avoid radial nerve palsy. Make sure your workspace is set up well. Have your computer screen at eye level. Also, keep your keyboard and mouse close by. This reduces the chance of nerve strain. When you sleep, use pillows to keep your arm and hand in a good position.
Proper Use of Crutches and Assistive Devices
If using crutches or aids, proper handling is vital. Incorrect usage can cause radial nerve palsy. Ask your doctor or a therapist for guidance. They can show you the right way to use these devices. This knowledge helps prevent nerve issues.
Living with Radial Nerve Palsy
Dealing with the challenges of radial nerve palsy every day can be tough. But, there are ways to keep your independence and life quality high. You can use special equipment and join groups that understand to adapt well.
Adaptive Equipment and Assistive Devices
Using the right equipment is key for those with radial nerve palsy. It helps manage the condition and lets you do daily tasks. Things like splints, braces, or special devices can support your wrist and hand. This way, you can do more and live a full life. Working with therapists helps find the best tools for you.
Support Groups and Resources
Connecting with people facing the same challenges can make a big difference. Support groups and online communities are great for this. They offer a space to share, learn, and pick up helpful tips for dealing with the condition.
Healthcare professionals and therapists are also there to support you. They can give advice and help with managing the condition better. This includes tips for daily life with radial nerve palsy.
Recent Advancements and Research
Our knowledge about radial nerve palsy is growing every day. Researchers and doctors are looking into new treatments. They aim to help people with this issue better. They are studying advanced surgical techniques and new therapies. These include nerve transfers and regenerative methods.
Emerging Treatment Options
It's crucial to keep researching radial nerve palsy. This ensures we know about and can use the latest treatments. Although some sources don't talk about new treatments, they stress the importance of finding better ways to care for patients.
Ongoing Clinical Trials
The third source talks about research studies now happening. These radial nerve palsy clinical trials are working to improve patient care. These trials look to find the best ways to treat people with radial nerve injuries.
In addition to new treatments, these trials aim to set a better care standard. They want to make the lives of those with radial nerve palsy better.
By keeping up with the latest research, doctors can create better plans for their patients. This teamwork aims to provide the best care. It helps improve the lives of those affected by radial nerve palsy.
Conclusion
Radial nerve palsy is a complex issue that greatly affects your arm, wrist, and hand. Knowing about its signs, causes, how it's diagnosed, and treatment options is key. It's important to work with a team of professionals, including therapists, and be proactive in your care.
Getting diagnosed early, receiving the right treatments, and focusing on getting better can help a lot. With these, people with radial nerve palsy often get back their function and movement. And, as science progresses, there's hope for even better ways to treat and live with this condition.
In summary, dealing with radial nerve palsy is tough, but not impossible. By teaming up with your doctors and taking on available treatments, you can start your path to recovery. Always remember, there are ways to improve and enjoy your life more, despite this challenge.
FAQ
What is radial nerve palsy?
Radial nerve palsy affects the nerve controlling arm and hand movement. Symptoms include numbness, weakness, and a wrist drop.
What are the common symptoms of radial nerve palsy?
Main symptoms are numbness, weakness, and difficulty moving fingers and arm freely. A "wrist drop" pattern is often seen.
What are the typical causes of radial nerve palsy?
Causes include injuries, nerve compression, and medical conditions like diabetes or heavy drinking.
How is radial nerve palsy diagnosed?
Diagnosis involves a physical exam, imaging tests, and electrodiagnostic studies. These help confirm the condition and determine its extent.
What are the treatment options for radial nerve palsy?
Treatments can range from conservative to surgical. This may include pain management, physical therapy, and, in severe cases, surgery.
What is the recovery and rehabilitation process for radial nerve palsy?
With proper treatment, most people improve in 3 to 4 months. Occupational therapy helps them adjust and prevents future problems.
What are the potential complications of radial nerve palsy?
Complications may lead to loss of feeling or hand movement, hand deformities, and injuries without noticing.
Are there any specific populations at higher risk for radial nerve palsy?
Athletes and workers doing repeated arm tasks are more likely to get radial nerve palsy.
Can radial nerve palsy be prevented?
While it's hard to prevent, using the right tools, correcting risk factors, and good ergonomics can lower the risk.
What are some ways to manage daily life with radial nerve palsy?
Using special equipment and joining support groups can make living with radial nerve palsy easier and more independent.
What are the latest advancements in the treatment of radial nerve palsy?
New treatments are under study, from advanced surgeries to therapies like nerve transfers. These aim to better help those with radial nerve injuries.
Source Links
- https://www.mountsinai.org/health-library/diseases-conditions/radial-nerve-dysfunction
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5367587/
- https://emedicine.medscape.com/article/1141674-overview
- https://centenoschultz.com/condition/radial-nerve-palsy/
- https://www.assh.org/handcare/blog/advice-from-a-hand-therapist-what-is-radial-nerve-palsy
- https://www.nicklauschildrens.org/conditions/radial-nerve-palsy
- https://www.healthline.com/health/radial-nerve-dysfunction
- https://www.ncbi.nlm.nih.gov/books/NBK537304/
- https://www.baptisthealth.com/care-services/conditions-treatments/radial-nerve-palsy
- https://www.neurosurgery.columbia.edu/patient-care/conditions/radial-nerve-injury
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10229417/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6439110/
What Is Tardive Dyskinesia? Understanding This Neurological Condition
Tardive dyskinesia (TD) is an involuntary movement disorder. It's caused by taking specific drugs for a long time. These drugs help with certain psychiatric or stomach issues. But, over time, they can lead to strange and uncontrollable movements of the body. The jaw, lips, tongue, arms, and legs are commonly affected. TD is mainly linked to the use of antipsychotic drugs. Yet, some stomach medications, like metoclopramide, can also trigger it.
No one fully knows why TD affects some people but not others. Several elements can play a role. These include gender, age, how long you've been taking the drug, and race. Being aware of TD is crucial for those who take such medications. It helps them watch for early signs of this condition.
What Is Tardive Dyskinesia?
Tardive dyskinesia (TD) is a disorder that causes uncontrollable movements. It's linked to taking certain drugs for a long time. These drugs affect the brain's dopamine system. The movements usually involve the face, lips, and tongue. But sometimes, the arms and legs are also affected.
Not everyone who takes these drugs will get TD. Yet, if you do get it, the problem can last forever. You might see stiff or jerky movements that you can't stop. This can affect how your face and body move. For example, you might see people sticking their tongue out, blinking a lot, chewing, or smacking their lips.
The chance of getting TD goes up if you've been taking these drugs for a long time. Age, race (like being African American or Asian American), and certain times in women's lives can also make TD more likely. Not all drugs are the same. The older ones are more often tied to TD than the newer ones. Some known drugs that could lead to Tardive dyskinesia are Haloperidol, Fluphenazine, Risperidone, and Olanzapine.
Anyone on these drugs should be checked for TD. Doctors use a scale to watch for its symptoms. Some stomach drugs, if used for over 3 months, can also cause TD. Diagnosing TD can be hard if the symptoms come after you stop the medication.
Symptoms of Tardive Dyskinesia
Tardive dyskinesia (TD) shows up as movements you can't control in your face, lips, and tongue. It can cause things like grimacing, tongue movements, or mouth puckering. These actions happen on their own and affect your life a lot.
Orofacial Dyskinesia
The most seen TD form is orofacial dyskinesia, meaning your face, lips, and tongue move unexpectedly. You might see someone look like they're frowning, keep their lips tight, or poke their tongue out. Such actions can make talking, eating, or just doing normal things tough.
Limb Dyskinesia
Sometimes, TD can affect your arms and legs, making them move without your say. This is limb dyskinesia. It can appear as sudden, twitchy moves (chorea) or slow, wavelike actions (athetosis) in the limbs. These moves make daily activities harder and lessen quality of life.

Causes of Tardive Dyskinesia
Tardive dyskinesia comes mainly from long-term use of certain drugs. These drugs include antipsychotics, used for mental illnesses. They work by blocking dopamine in the brain.
This can happen with other medicines, too. For example, metoclopramide treats stomach issues and prochlorperazine fights nausea. They also mess with dopamine, causing the jerky movements of tardive dyskinesia.
Antipsychotic Medications
Tardive dyskinesia is mostly from using antipsychotic medications for a long time. They treat illnesses like schizophrenia. By blocking dopamine, they cause body movements that you can't control.
Metoclopramide and Other Gastrointestinal Medications
Some stomach medicines like metoclopramide can also bring on tardive dyskinesia. These drugs help with nausea and acid reflux problems. But they work against dopamine, which leads to the odd movements of tardive dyskinesia.
Risk Factors for Developing Tardive Dyskinesia
Several things can raise your chances of getting tardive dyskinesia. This is a condition where your body does sudden movements you can't control. Knowing these risk factors is key for doctors and people using medications that might cause TD.
Gender and Age
Women, especially those past menopause, face a bigger risk of getting TD than men. Elderly patients are also more likely to get TD. This may be because our brains and bodies change as we age.
Duration of Medication Use
Taking drugs that block dopamine receptors for a long time ups your TD risk. This includes antipsychotics and certain meds for the stomach. Over time, using these drugs more can make TD more likely.
Ethnicity
Studies show people of African American or Asian heritage might have a higher TD risk if they use dopamine-blocking drugs for a long time. This is compared to Caucasians.
Pathophysiology of Tardive Dyskinesia
The exact cause of tardive dyskinesia (TD) is not fully known, but some ideas exist. One theory suggests that drugs blocking the brain's dopamine D2 receptors could lead to more sensitive receptors. This can cause a stronger reaction to dopamine, leading to the uncontrollable movements seen in TD.
Dopamine Receptor Upregulation
Taking drugs that block dopamine receptors for a long time can make these receptors more sensitive in the brain. This stronger reaction to dopamine might play a big part in causing the involuntary movements of TD.
Oxidative Stress
Oxidative stress, which comes from dopamine being broken down, might also have a role. The direct toxic effects of antipsychotic drugs on brain cells can damage them. This damage can make the brain's job harder, possibly making movement problems worse.
Withdrawal Dyskinesia
Stopping dopamine-blocking drugs can also cause a problem called withdrawal dyskinesia. This can make the brain even more sensitive to dopamine, making the movements in TD start or get worse.
These changes in the brain's control of movement are thought to be the cause of the unique movements in TD. Knowing how these mechanisms work together is key to finding ways to prevent or treat this serious disorder.
Diagnosing Tardive Dyskinesia
Doctors diagnose tardive dyskinesia through a detailed process. They check the patient's body movements closely. They also review the medicines the patient has taken. The Abnormal Involuntary Movement Scale (AIMS) helps doctors see how severe the symptoms are.
Physical Examination
During the checkup, doctors watch for certain involuntary movements. These movements can affect the face, lips, tongue, and more. They observe these movements to understand their frequency and how severe they are.
Abnormal Involuntary Movement Scale (AIMS)
AIMS is a tool that rates the level of tardive dyskinesia symptoms. It looks at body parts like the face, lips, and tongue. This tool helps determine the effects of these movements. It's key for both diagnosis and tracking the condition over time.
Ruling Out Other Conditions
It's important to check for other illnesses with similar symptoms. This includes diseases like Huntington's and conditions such as cerebral palsy. Doctors may do brain tests to confirm tardive dyskinesia. A full check-up is critical to get the right diagnosis and treatment plan.

Treatment Options for Tardive Dyskinesia
If you're dealing with tardive dyskinesia (TD), you have treatment choices. The main step is to check the medicines causing the twitching. Then, they might change those meds.
Medication Adjustments
Your doctor may stop the medicine that's causing TD. Or, they could lower the dose. They might also suggest a new drug that's less likely to make you twitch. Doing this can cut down on the TD effects. It could also stop it from getting worse.
FDA-Approved Medications
In 2017, the FDA gave the OK for two drugs to treat TD. These are valbenazine (Ingrezza) and deutetrabenazine (Austedo). They work by adjusting dopamine in the brain. This can lower the twitching from TD.
Natural Remedies
There's little proof that natural options help with TD. Some studies looked at choline, vitamin E, and omega-3s. These might help as extra support. But, always talk to your doctor first. Natural remedies could affect your other medicines or cause problems.
Prevention Strategies for Tardive Dyskinesia
The best way to stop tardive dyskinesia is through watchful care. Doctors should keep a close eye on patients using certain medications. These include first-generation antipsychotics, which pose higher risks. Doctors should try to use second-generation antipsychotics as a safer option. This helps in handling the use of these medications better and lowering the risk of tardive dyskinesia.
It's vital that patients are told about tardive dyskinesia. They should know how to spot any strange movements. They need to inform their healthcare team right away if they notice something odd. Using the Abnormal Involuntary Movement Scale (AIMS) for checks can help find tardive dyskinesia early. This early detection might stop it from getting worse and become a big problem.

Differential Diagnosis of Tardive Dyskinesia
When a patient shows signs of tardive dyskinesia (TD), doctors look at other conditions first. This is because many diseases have similar symptoms like uncontrollable movements. Conditions like Huntington's disease, cerebral palsy, Tourette syndrome, and dystonia look similar but need different treatments.
Huntington's Disease
Huntington's disease causes jerky, twisting movements. It also affects thinking and can lead to mood changes. Although the movements can be alike in TD and Huntington's, family history and other symptoms help doctors tell them apart.
Cerebral Palsy
Cerebral palsy is due to brain issues early in life. It makes people move slowly and have involuntary movements of the face and tongue. Doctors watch the pattern of symptoms to see if it's cerebral palsy or TD.
Tourette Syndrome
Tourette syndrome makes people have sudden, uncontrollable sounds and movements. These can include making faces or sticking out the tongue. Looking at all the tics, not just the movements, helps in diagnosis.
Dystonia
Dystonia causes muscles to contract without control. This can lead to slow, twisting movements. By carefully checking the movements and health history, doctors can see if it's TD or dystonia.
It's crucial for doctors to rule out other conditions to treat TD right. They might use brain scans or genetic tests to be sure. This way, patients get the best care for their exact condition.
Epidemiology of Tardive Dyskinesia
Tardive dyskinesia is a common side effect of long-term antipsychotic use. It affects at least 20% of first-generation antipsychotic users. However, the rates can be as low as 1% with other drugs, such as some antidepressants.
Groups at high risk include women, the elderly, and those of African American or Asian descent. Middle-aged to older women show a higher TD risk than men. After menopause, this risk can jump to 30% after a year on these medications.
Older patients also face increased risk, likely due to age-related changes. African Americans have shown a higher TD risk after taking dopamine-blockers for a long time.
Though second-generation antipsychotic users have a lower TD risk, it's not insignificant. The use of TD-causing drugs has also grown over the last 20 years, adding to the problem.
Those with ongoing mental health issues are more likely to develop TD. There are new treatments, like deutetrabenazine and valbenazine, that can help manage this condition now.
Impact on Quality of Life
Tardive dyskinesia can change your life in big ways. It causes body movements you can't control. These movements can make it hard to eat, talk, or do tasks that need careful hand movements. You might start avoiding people or find it hard to keep up with friends. This can make you feel very bad about yourself. Even stopping the medicine that caused it doesn't always make these effects go away. This can be very upsetting.
This issue doesn't just affect how you move. It can also hurt how you see yourself and get along with others. Studies show people with tardive dyskinesia have a harder time with their health and social life. Those with severe TD had the worst health and life quality. If you have schizophrenia, TD can hit you even harder. But it's also tough for people with bipolar disorder or major depression. In either case, life can feel a lot harder than for the average person.
Tardive dyskinesia reaches deep into your life. Many people say it makes other mental health problems worse. It can change how well your main mental health issue stays under control. And it can shake up how well you stick to your treatment plan. Doctors know how much TD affects you. They say it's the main reason they start special treatments for TD.
This condition is no small thing. A good number of people who take certain medicines might get it. For many, it causes more than physical problems. It can lead to deep feelings of frustration, insecurity, and at its worst, thoughts of ending life. Dealing with TD may mean more trips to hospitals. It might also make finding or keeping a job harder, changing your work life a lot.
Dealing with the effects of tardive dyskinesia is really important. Knowing what you might face and finding help can make a huge difference. It's crucial to focus on making your life better again. Remember, managing TD well is key for you and your care team.
Ongoing Research and Clinical Trials
Scientists are looking into new ways to treat and manage tardive dyskinesia research. Many clinical trials are testing the effectiveness of different medicines. These include newer antipsychotics and experimental drugs. The goal is to find better treatments to lessen involuntary movements and make life better for those with the condition.
A study from 2019 showed that people with bipolar disorder, major depressive disorder, and schizophrenia were affected. It changed their lives by causing involuntary movements. In 2017, it was found that the risk of these movements is lower with second-generation antipsychotics.
Along the way, a 2017 meta-analysis showed that tardive dyskinesia was less common with these second-generation antipsychotics. If you're interested in joining a trial, you can find info on places like ClinicalTrials.gov. This website lists studies, including those funded by the government or private groups. Staying up-to-date can help you and your doctor find the best ways to tackle the symptoms and improve your life.

Awareness and Education Initiatives
It's really important to make more people aware of tardive dyskinesia. Healthcare pros need to know how to spot the early signs and take preventive actions. This includes keeping a close eye on patients who are on certain meds.
Teaching patients is also key. They need to learn about the risks of tardive dyskinesia. And, they should know to report any strange body movements to their healthcare team. Knowing about treatment choices can be very helpful, too.
About 600,000 folks in the US have tardive dyskinesia. And almost 100 to 127 out of every 1,000 people taking certain meds may get it. Yet, many don't know that lots of antipsychotic drugs can lead to this condition. It's a big shortcoming in how we care for these individuals.
So, we need to fix this. Healthcare providers must learn to spot tardive dyskinesia early. They should watch patients closely if they're on meds that might cause it. Teaching patients is equally vital. They need to understand the risks, know why they should point out any unusual movements, and be aware of how it can be treated.
By spreading more awareness and clear info on tardive dyskinesia, we can make a big difference. More people might get diagnosed sooner, paving the way for better care and outcomes. This could greatly improve the lives of those with tardive dyskinesia in many ways.
Conclusion
Tardive dyskinesia is a major health issue that affects your daily life. It causes involuntary movements in parts of your body. These movements might happen in your face, lips, tongue, or limbs. Long-term use of some drugs can lead to this condition.
It's important to know the risk factors. Things like gender, age, and ethnicity play a part. Knowing about these can help in preventing and treating this condition. This is key knowledge for doctors and patients.
There is ongoing work to find new treatments for tardive dyskinesia. Education efforts are also working hard to help recognize and deal with it better. By working with your medical team, you can keep up with the latest info. This will help make good choices and lessen the disorder's effects.
The number of people with tardive dyskinesia changes across groups. This shows why staying aware and doing regular checks is important. If you are taking certain medicines for a long time, be careful. Speaking up for your health and staying informed helps everyone battle this condition.
FAQ
What is tardive dyskinesia?
Tardive dyskinesia (TD) is a condition where people make movements they can't control because of certain drugs. These drugs can include some psychiatric medicines and drugs used for stomach issues. The movements often happen in the face, lips, tongue, and sometimes in the arms and legs.
What are the primary symptoms of tardive dyskinesia?
One main sign of TD is when a person's face or mouth moves strangely on its own. This is called orofacial dyskinesia. You might also see quick, sharp movements (chorea) or slow, twisting movements (athetosis) in their arms or legs. These are known as limb dyskinesia.
What causes tardive dyskinesia?
The main cause of TD is taking certain drugs for a long time. These drugs block dopamine receptors in the brain. Aside from psychiatric drugs, a stomach medicine called metoclopramide and an anti-nausea drug, prochlorperazine can also lead to TD.
What are the risk factors for developing tardive dyskinesia?
Many things can raise the chances of getting TD. This includes being a woman and getting older. The risk goes up the longer you use these drugs. Some races like African Americans and Asian Americans might also have a higher risk.
How is tardive dyskinesia diagnosed?
To diagnose TD, a doctor does a physical exam and checks your medicine history. They might use a test called the Abnormal Involuntary Movement Scale (AIMS). The doctor also checks to make sure it's not something else causing the movements.
How is tardive dyskinesia treated?
The main way to treat TD is to stop or change the medications causing it. Sometimes, the doctor might switch you to a different drug. There are medicines like valbenazine that can help lessen the movements. Some natural remedies have been looked at but more research is needed on them.
How can tardive dyskinesia be prevented?
Doctors should watch over patients on these drugs closely. They should use newer medicines if possible to lower the TD risk. Patients should be told about TD and asked to report any strange movements. Regular screenings can find TD early.
How common is tardive dyskinesia?
At least 20% of people using first-generation antipsychotic drugs can get TD. The numbers are lower, between 1% to 10%, for other drugs that can cause TD.
How does tardive dyskinesia impact quality of life?
Having TD can make life harder. The movements can make daily life tough, leading to avoiding social situations or trouble in relationships. It can also make people feel embarrassed or self-conscious.
What is the current state of research and clinical trials for tardive dyskinesia?
Right now, scientists are working on new ways to treat and handle TD. We're seeing new drug studies to see how well they work. These include both new and known drugs. The goal is to better understand and target what causes TD.
Source Links
- https://rarediseases.org/rare-diseases/tardive-dyskinesia/
- https://www.ncbi.nlm.nih.gov/books/NBK448207/
- https://www.webmd.com/mental-health/tardive-dyskinesia
- https://emedicine.medscape.com/article/1151826-overview
- https://medlineplus.gov/ency/article/000685.htm
- https://www.uptodate.com/contents/tardive-dyskinesia-etiology-risk-factors-clinical-features-and-diagnosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7377543/
- https://www.healthline.com/health/treatment-options-tardive-dyskinesia
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6591749/
- https://pubmed.ncbi.nlm.nih.gov/29022654/
- https://www.ccjm.org/page/mds-2023/td-quality-of-life
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6863950/
- https://www.healthline.com/health/tardive-dyskinesia-quality-of-life
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8412148/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8164384/
- https://www.psychiatrictimes.com/view/neurocrine-biosciences-announces-collaboration-with-participants-of-tardive-dyskinesia-awareness-week
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5472076/