How a Pain Doctor Can Help Manage Chronic Pain
If you're dealing with chronic pain, a pain doctor can be a big help. They have the skills and knowledge to diagnose and treat different kinds of pain. This includes headaches, back pain, neck pain, and neuropathic pain, among others.
Pain doctors, or pain management specialists, have extra training after their medical school. They often focus on areas like anesthesiology, neurology, or physical medicine and rehabilitation. This extra knowledge lets them manage your chronic pain in a detailed way.
A pain doctor will work with you to make a treatment plan. This plan might include medicines, procedures, physical therapy, and other therapies. Their aim is to ease your pain, help you function better, and improve your overall health.
Understanding Pain Management
What is Pain Management?
Pain management is a way to treat and manage pain, both acute and chronic. The main aim is to lessen, control, and help people cope with their pain. This improves their life quality. Pain management uses many methods, like medicines, procedures, physical and psychological therapies, and alternative therapies. Specialists in pain management work with patients to create plans that tackle the root causes of pain and offer lasting relief.
A 2018 review found that neuropathic pain affects about 7-8% of adults. Chronic pain, lasting 3-6 months or more, greatly affects life quality. Pain management doctors often need an extra year of training after medical school to specialize.
Pain is a common symptom of many injuries and conditions, from short-term to long-lasting pain. Chronic pain can last years and comes from various health issues, like arthritis, muscle injuries, autoimmune diseases, cancer, and spinal cord problems.

Anyone facing pain, whether new or ongoing, can benefit from a pain management plan. Pain management experts team up with a group that includes anesthesiologists, nurses, mental health professionals, physical and occupational therapists, social workers, and others. Together, they make plans tailored to each patient's needs.
Chronic Pain and Its Impact
Chronic pain is a big issue that can really change how someone lives. It's pain that lasts for 3-6 months or more. It can come from health problems, injuries, or chronic pain disorders. This pain does more than hurt; it can make moving hard, lower life quality, and increase healthcare costs.
People with chronic pain often feel constant or off-and-on pain, get tired easily, feel sad, and anxious. This makes doing everyday tasks hard, makes it tough to work and be social, and hurts their overall health. In fact, chronic pain is very costly in the U.S., causing high medical bills, lost wages, and less productivity.
Seeing a pain doctor is key to handling chronic pain and better living. Pain management plans often bring together many experts like neurologists, orthopedists, physical therapists, and psychologists. They work together to make a full treatment plan. This plan might include medicine, therapy, surgery, and support for the mind and feelings.
By tackling chronic pain from all angles, people can lessen the pain and feel more in charge of their health. With the right care and support, those with chronic pain can improve their physical, emotional, and social health. This helps them live a better life overall.
The Role of a Pain Doctor
Pain doctors, also known as pain management specialists, are experts in treating different types of pain. They know how complex pain works and create treatment plans for each patient. These specialists are key in helping people with chronic pain live better lives.
Expertise in Pain Management
Pain doctors get extra training in pain management after finishing their basic medical training. This training helps them handle a variety of pain issues, like arthritis and migraines. They work with other health experts, such as physical therapists and psychologists, to make a treatment plan for each patient.
These doctors are great at finding the cause of pain with tests and exams. They use things like neurological exams and imaging studies to figure out where the pain comes from. Then, they use different treatments, including medicines and procedures, to help manage chronic pain.
A big part of a pain doctor's job is making sure all healthcare providers work together. This teamwork leads to a better, more complete treatment plan for chronic pain. It helps patients feel better and live fuller lives.

Types of Pain Treated by Pain Doctors
Pain doctors are experts in treating many types of pain. They help with chronic pain that lasts for months or years. They also treat neuropathic pain from nerve damage. Their goal is to relieve your pain and improve your life.
Chronic pain is a common issue they tackle. It's pain that lasts 3-6 months or more. It can come from health issues or injuries. Pain doctors create custom plans to help manage this pain.
Neuropathic pain is another focus for them. It happens when the nervous system is damaged or doesn't work right. This includes pain from diabetic neuropathy, trigeminal neuralgia, and spinal cord injuries. Pain doctors know how to treat this kind of pain.
They also treat nociceptive pain. This is pain from tissue damage, like injuries or arthritis. Their approach helps reduce this pain and boost your health.
Lastly, pain doctors are skilled in handling functional pain. This type of pain has no clear cause, found in fibromyalgia or irritable bowel syndrome. They work with you to create plans that cover both physical and emotional pain.
No matter the pain you face, pain doctors use a detailed approach. They assess, diagnose, and make custom treatment plans for you. Their expertise and commitment ensure you get the best care for your pain.
Comprehensive Pain Management Approach
Managing pain well often means using a team approach. Pain doctors, or specialists in pain management, work with others to give you the best care. This team includes anesthesiologists, physical and occupational therapists, psychologists or psychiatrists, nurses, and others.
Multidisciplinary Team
This team works together to make a plan just for you. They use proven methods to help you, focusing on your body, feelings, and mind. This way, your pain care is well-planned and covers all angles of chronic pain.
Places like Comprehensive Pain Management in Massachusetts and Rhode Island use this team approach. Dr. Chan and Dr. Shwartzman, who are experts in anesthesia and pain medicine, lead the team. They've been helping with pain for over 10 years.
Medical Management of Pain
Pain doctors use many medical treatments to help manage your pain. They might prescribe pain medications like opioids, NSAIDs, antidepressants, and anticonvulsants. These drugs aim to treat the underlying cause of your pain.
Medications and Interventions
Pain doctors also offer minimally invasive procedures. These include nerve blocks, epidural injections, or spinal cord stimulation. These methods target the pain source directly. They aim to lessen your need for oral pain medication.
When using opioid therapy, pain doctors are very careful. They know the risks of addiction and misuse. They work hard to balance pain relief with safety.
The right treatment depends on your pain type and severity, as well as your needs and wishes. Your pain doctor will work with you to create a treatment plan. This plan will address your specific pain concerns and offer the best relief.

Non-Pharmacological Therapies
Pain doctors often look beyond just giving medication for chronic pain. They see the value in using non-pharmacological therapies. These treatments can help traditional medicine and let patients take charge of their pain.
Physical therapy is a key therapy. It uses exercises, manual techniques, and other methods to improve strength, flexibility, and mobility. This can lessen pain and make daily activities easier. It helps patients live better lives and use less medication.
Psychological therapies like cognitive-behavioral therapy (CBT) are also vital. They help patients find ways to cope with pain and deal with the emotional side of it. This approach helps patients handle chronic pain better and feel better overall.
Other therapies like acupuncture, massage, and mindfulness are also used. They aim to balance energy, relax the body, and help it heal naturally.
The aim of these therapies is to give patients more control over their lives and cut down on medication use. With a pain doctor's help, patients can try different options to find what works best for them.
Pain Doctor
Managing chronic pain can be tough, but a pain doctor can really help. They have a lot of training and certification in pain treatment. They know how to find the cause of pain and create treatment plans just for you.
Pain doctors get extra training, often for a year or more, in pain management. This training teaches them about the newest ways to treat pain. They learn about things like procedures, medicines, and non-drug therapies. Many are also board-certified in pain medicine or anesthesiology, keeping up with new research and training.
Comprehensive Pain Treatment Expertise
Pain doctors are experts in treating pain. They can figure out what's causing your pain and make a detailed plan to fix it. They might use a team approach, including things like:
- Interventional pain procedures (e.g., nerve blocks, epidural injections)
- Medications and pain-relieving therapies
- Physical therapy and rehabilitation
- Alternative therapies (e.g., acupuncture, massage)
With their deep knowledge and experience, pain doctors can find the best pain management for you. This helps you take back control of your life.
Improving Quality of Life
Living with chronic pain can really change your life. It affects every part of your day. But, a skilled pain management doctor can help you take back control. They aim to reduce pain, cut down on medication, and help you do more in your daily life and with others.
Pain management doctors work with you to create a plan that covers your body, feelings, and social life. This plan might include medicine, physical therapy, and counseling. Their goal is to boost your ability to function and improve your life quality.
By finding and treating the causes of your pain, these doctors can help you move better, sleep better, and connect with others more. This approach to pain relief lets you play a big part in managing your pain. It helps you live a more independent and fulfilling life.
Remember, managing pain is not just about feeling less pain. It's about living your life fully and finding new ways to enjoy activities. With help from a pain management expert, you can start moving towards a brighter and more meaningful future.
Personalized Treatment Plans
Managing chronic pain requires a tailored approach. Pain doctors create treatment plans that fit each patient's unique needs and likes. They look at your medical history, symptoms, and goals to make a plan. This plan mixes different therapies to tackle your pain's specific causes.
This approach might use medications, procedures, physical therapy, support, and other therapies. Doctors work with you to set goals and check your progress. They adjust the plan as needed to make sure you get the best care.
Personalized pain management is more than just treating symptoms. It looks at the deep causes of your pain, like muscle, nerve, or mixed issues. By understanding your experiences and what you prefer, doctors can make a detailed plan. This plan helps ease your pain and improve your life quality.
Your pain is special, and so should your treatment. Working with a pain doctor who focuses on personalized pain management is a big step towards better health and well-being.
Collaboration with Primary Care Providers
Pain management often needs a team effort between pain doctors and primary care providers. These healthcare workers team up to make sure patients get a full and coordinated plan for chronic pain.
Coordinated Care
Primary care providers are key in the first step of assessing and referring patients to pain management experts. After a patient sees a pain doctor, these teams work together. They share info, plan treatments, and keep an eye on the patient's progress. This teamwork makes sure all parts of the patient's health are looked at and avoids any care issues.
By working as a team, primary care and pain doctors can offer the best care for those with chronic or complex pain. This way of caring for patients improves their outcomes and makes their lives better.
- Pain doctors and primary care providers work together to share info and plan treatments.
- This teamwork ensures a full and smooth patient care experience.
- Working together helps avoid care problems and betters patient results.
The partnership between pain doctors and primary care providers is key in handling chronic pain. This teamwork leads to a detailed and tailored treatment plan. It looks at the patient's physical, emotional, and overall health. By working together, these professionals can offer the best pain management and improve the life quality of those with chronic pain.
Ongoing Monitoring and Adjustment
Pain management is a process that changes over time. It needs close watching and regular changes to your treatment plan. Your pain doctor will work with you to check how well your treatments are working. They will look for any changes in your condition and adjust your treatment as needed.
This might mean changing how much medicine you take, trying new procedures, or adding other therapies that don't involve drugs.
Your doctor will keep an eye on how you're doing and involve you in making decisions. This way, your treatment plan will always match your changing needs. It will keep giving you the best pain management, relief, and better quality of life.
- Regular checks to see if your current treatment is working well
- Finding changes in your pain and adjusting treatments as needed
- Working with you to make sure your treatment fits your changing needs
- Keeping a close watch to give you the best pain management, relief, and better life quality
With this detailed and team effort, your pain doctor can guide you through the changing world of pain management. They make sure you get care that's made just for you and is very effective.
Access to Advanced Treatments
When dealing with ongoing or severe pain, seeing a specialized pain doctor can lead to many advanced treatment options. These doctors have access to special procedures and the newest in pain management. This includes things like nerve blocks, spinal cord stimulation, and radiofrequency.
Pain doctors keep up with the newest research and trials. This lets them offer new therapies and treatments. They use the resources and knowledge at pain clinics to give care that fits each person's needs and likes.
The Department of Pain Management at MGM Healthcare uses the latest robotic technology for non-surgical treatments. Dr. R Madhan Kumar, a top pain doctor, leads the Center for Advanced Pain Management. He works with a team to make treatment plans for each patient.
These plans might use different medical treatments, psychological help, and rehab. The center offers many interventional treatments. This includes things like epidural steroid injections, selective nerve root blocks, and facet injections.
By getting help from a pain doctor, people with ongoing or severe pain can get the newest in pain management. This care can greatly improve their life, work, and overall well-being. It's a big step towards better health and happiness.
Support and Education
Pain doctors know how key it is to support and educate patients with chronic pain. They aim to make patients active in their care. This helps them feel in control and boosts their well-being.
Through education, pain doctors teach patients about their pain and treatment options. They focus on non-pharmacological therapies that can fit into daily life. This way, patients learn to manage their pain better, leading to better outcomes.
Pain doctors also look at the emotional and mental sides of chronic pain. They offer counseling and support groups. These resources help patients deal with the tough parts of living with pain.
By educating and supporting patients, pain doctors help those with chronic pain take charge of their health. This teamwork approach builds trust and leads to safer, more effective pain care.
Conclusion
Pain doctors are key in helping people with chronic pain. They use a full approach to manage pain and boost life quality. This includes looking at physical, emotional, and mental sides of pain.
They combine medical treatments, non-drug therapies, and support to help patients take charge of their health. This helps them lessen pain and get better at doing daily tasks.
For those with chronic pain, seeing a pain doctor is a big step towards better health and a happier life. These doctors know how to tailor treatments to each patient's needs. This helps patients manage their pain better and live more fully.
The need for skilled pain doctors is growing, seen in hospitals and government health centers. This shows how important it is to focus on pain care that puts the patient first. It helps people with chronic pain live healthier lives.
FAQ
What is a pain doctor?
A pain doctor, also known as a pain management specialist, is a medical expert. They focus on treating different kinds of pain, especially chronic pain. They use a special approach to manage pain.
What is the goal of pain management?
The main goal of pain management is to lessen and control pain. This improves a person's life quality. It uses many methods, like medicines, procedures, therapy, and alternative treatments.
What is chronic pain?
Chronic pain lasts for more than 3-6 months. It can come from health issues, injuries, or chronic pain conditions. It affects a person's health, feelings, and social life.
What types of pain do pain doctors treat?
Pain doctors treat many pain types, like chronic, neuropathic, and functional pain. They use a team approach to find and treat pain. They create treatment plans that fit each patient's needs.
How do pain doctors work as part of a multidisciplinary team?
Pain doctors work with a team that includes many healthcare experts. This team helps create a treatment plan that suits the patient's needs. They work together to help patients manage their pain better.
What types of medical interventions do pain doctors use?
Pain doctors use various treatments, like medicines and procedures. They choose the best treatment based on the patient's pain type and needs.
What non-pharmacological therapies do pain doctors incorporate?
Besides medicines, pain doctors use therapies like physical and psychological therapy. These help patients manage pain and improve their life quality.
What qualifications do pain doctors have?
Pain doctors have special training and certification in pain management. They complete extra training after medical school, often in a fellowship program.
How do pain doctors work with a patient's primary care provider?
Pain doctors work with primary care providers for better pain management. They share information and coordinate treatment plans. This ensures patients get the best care.
How do pain doctors ensure ongoing monitoring and adjustment of treatment plans?
Managing pain is ongoing. Pain doctors regularly check how well treatments work and adjust them as needed. They make sure the treatment fits the patient's changing needs.
What types of advanced treatments do pain doctors have access to?
Pain doctors offer advanced treatments not found in primary care. They use their expertise and clinic resources for the best care possible.
How do pain doctors empower and support their patients?
Pain doctors help patients by teaching them about their pain and treatment options. They support patients in using non-medical therapies to manage pain.
Source Links
- Chronic Pain Management
- What does a Pain Clinic Do? | Max Hospital
- What to expect from your pain management specialist
- What does a pain management doctor do?
- Is Pain Management Right for Me?
- Chronic Pain: What Is It, Causes, Symptoms & Treatment
- What Is Chronic Pain Syndrome?
Effective Strategies for Comprehensive Pain Management
Chronic pain affects about 15% of people in the US, causing a lot of suffering and high healthcare costs. It's important to treat pain fully, looking at the biological, psychological, and social sides. Programs that bring together different experts can really help manage chronic pain and its effects.
Handling pain well means using many kinds of therapy together. This includes physical therapy, occupational therapy, pain psychology, and more. The goal is to lessen the need for opioids, which have been overused and led to the opioid crisis. Now, doctors focus on non-drug treatments, teaching about pain, and helping patients get back to their lives.
By using good pain management strategies, doctors in India can help people with chronic pain. They can get their lives back, feel better physically and emotionally, and lessen the cost to society. Working together, we can find better ways to manage chronic pain for good.
The Burden of Chronic Pain
Prevalence and Impact on Quality of Life
Chronic pain affects about 15% of people in the US. It can really change someone's life, making it hard to do everyday tasks and enjoy social activities. It also causes emotional pain, making life less fulfilling.
Economic Costs and Lost Productivity
Chronic pain costs the US healthcare system between $100 to $150 billion a year. This number might be low because it doesn't include lost work time. Conditions like arthritis and nerve pain add a lot to healthcare costs and lost productivity.

We need to tackle chronic pain to help people feel better and save money. Using a mix of treatments that look at the whole person is key. This approach can make life better for those in pain and ease the economic strain.
Understanding Comprehensive Pain Management
Managing chronic pain well means more than just treating the body. The biopsychosocial model of pain shows that chronic pain comes from a mix of biology, mind, and social factors. Over time, these factors keep the pain going, making people less active, isolated, and feeling out of control.
The Biopsychosocial Approach
A chronic pain management approach based on this model looks at pain from all angles. It brings together doctors, psychologists, physical therapists, and others to make a plan just for you. This way, they tackle the physical, mental, and social sides of pain. It helps people with chronic pain live better, do more, and handle their pain better.
The biopsychosocial model sees chronic pain as more than just a body issue. It's a mix of many things. This view helps doctors make better, tailored treatment plans for their patients. It helps them meet the special needs and challenges of each person.
Interdisciplinary Care: A Cornerstone of Comprehensive Pain Management
Managing pain well often means working together as a team. This team looks at the many factors that cause pain. They focus on the body, mind, and social aspects that can make pain worse. The team includes doctors, psychologists, physical and occupational therapists, and others.
The main advantages of this team approach are:
- Comprehensive assessment and treatment planning: With many experts, patients get a full check-up. This looks at physical, emotional, and social factors that affect pain.
- Coordinated care delivery: Teams work together to make sure treatments work well together. This helps give the best pain relief and helps patients function better.
- Improved patient outcomes: Studies show that team-based pain care improves life quality and lessens chronic pain for patients.
Using an interdisciplinary pain management approach helps doctors give a full, personal care plan. This way of treating pain is key to managing it well. It leads to better health results and a better life for patients.

Physical Therapy for Pain Relief
Physical therapy is key in managing pain well. At the start, your therapist will set goals with you. These goals focus on improving flexibility, strengthening your core, and using aquatic therapy. These methods can help reduce your chronic pain and boost your physical function.
Core Strengthening and Flexibility
Targeted core exercises can help a lot with chronic pain. They make your core muscles stronger and more stable. This reduces strain on your joints and spine, lowering pain.
Adding flexibility exercises can also help. They make moving easier and reduce stiffness and tightness. This can lessen the discomfort you feel.
Aquatic Therapy
Aquatic therapy, or water-based physical therapy, is a safe and effective pain management tool. The water lets you do exercises that are hard or painful on land. It also helps strengthen muscles and improve physical fitness.
Working with your physical therapist to create a plan that includes core exercises, flexibility, and aquatic therapy can greatly help. It's a big step towards managing your chronic pain and improving your life quality.

Psychological Interventions
Chronic pain can really affect a person's mental health, causing depression, anxiety, and bad coping habits. Luckily, things like cognitive behavioral therapy (CBT) and relaxation techniques can help a lot with psychological pain management.
Cognitive Behavioral Therapy
CBT is a great way to change negative thoughts and find better ways to cope with chronic pain. It looks at the mental and behavioral things that make pain worse. This can really make someone's life better and help with cognitive behavioral therapy for chronic pain.
Relaxation Techniques
Relaxation techniques are also key for managing chronic pain. Things like deep breathing, meditation, and guided imagery can ease muscle tension and make you feel calmer. These relaxation techniques for pain are often taught in groups, which helps people learn and practice together.

Using both cognitive-behavioral and relaxation methods, people with chronic pain can get a full set of tools to handle their condition. Adding these psychological interventions is a big part of comprehensive pain management.
Comprehensive Pain Management
Finding the right way to manage chronic pain can greatly improve your life. Many programs now use group education to help. These sessions offer insights and create a supportive community for those with ongoing pain.
Group Education and Support
Group education is a key part of pain management programs. It covers topics like nutrition, stress reduction, and how pain affects your health. These sessions are interactive, letting people share their stories and learn from each other.
Group sessions create a sense of community. They offer motivation, information, and emotional support. People can connect with others who understand their pain, reducing the feeling of being alone.
The goal of these programs is to empower participants. They aim to engage people fully, improve comfort and function, and boost self-confidence. The programs also focus on safe and effective treatments, reducing the use of opiates, and overcoming barriers to care. They measure the success of treatments for the best results.

Along with group sessions, the program includes many therapies. These include acupuncture, massage, movement classes, mindfulness, and occupational therapy. By tackling physical, emotional, and social aspects of pain, these approaches help people take back control and enhance their well-being.
Occupational Therapy for Daily Living
Occupational therapy is key in managing pain by making daily activities easier. Therapists help patients overcome the challenges pain brings. They aim to make patients more independent and improve their life quality.
Occupational therapy (OT) helps people do everyday tasks. Chronic pain can make it hard, leading to less independence and mental health issues. To manage pain well, we need a plan that covers physical, mental, and social aspects.
Occupational therapists focus on making life better for those with chronic pain. They look at how pain affects daily life, skills, and work. Then, they create plans with different steps, like:
- Activity analysis and modification
- Ergonomic assessments and recommendations
- Pain education and self-management techniques
- Stress management and relaxation strategies
- Therapeutic exercises and adaptive tools
These steps help people take back control of their lives. They make daily tasks easier and lessen the pain's effect. Occupational therapy works with many healthcare experts for a full approach to managing chronic pain and daily activities.

Medication Management
Managing pain with the right medications is key. Opioid analgesics and non-opioid pain relievers are both vital. But, it's crucial to work with your doctor to avoid side effects or addiction risks.
Opioids and Non-Opioid Analgesics
Opioids like morphine and oxycodone help with severe pain after surgery. Nonsteroidal anti-inflammatory drugs (NSAIDs) are great for mild to moderate pain. They reduce inflammation and pain without the risk of addiction.
Over-the-counter pain relievers, such as acetaminophen, can also ease post-surgery pain. They help without causing stomach problems like NSAIDs can. Your doctor might suggest local anesthetics or PCA and PCEA for targeted pain relief during recovery.
Your healthcare team will create a plan just for you. They'll mix the right medications, treatments, and therapies to help you stay active and healthy. Keeping in touch and regular checks are key to making sure your pain plan works well.
Complementary and Alternative Therapies
People looking for ways to manage pain might want to check out acupuncture and massage therapy. These methods can be used along with regular medical treatments. They offer a full approach to easing pain and boosting health.
Acupuncture for Chronic Pain
Acupuncture is a traditional Chinese medicine that helps with chronic pain. It might ease pain by boosting the body's own pain fighters and helping you relax. Studies show mixed results, but it's safe if done by a trained expert.
Massage Therapy for Pain Relief
Massage therapy is another way to help with pain. It can ease muscle tightness, improve blood flow, and help you relax. Adding regular massages to your pain plan might be really helpful.
Always talk to your doctor before trying new therapies. They can affect your medicines or have other risks. By trying different treatments, you can better manage your pain and live a better life.
Pain Neuroscience Education
Pain neuroscience education is key to managing pain well. It helps patients understand the complex ways chronic pain works. This knowledge lets them take a bigger part in their care, which can lead to better results.
Studies show that teaching patients about pain can change their beliefs and behaviors for the better. It helps with chronic pain from low back pain, chronic fatigue, and musculoskeletal issues.
The Fear-Avoidance model of chronic pain shows how important it is to change how patients see and believe about their pain. By learning about pain's neurophysiology, patients can feel less fear. This leads to better beliefs about pain and a more active way of managing it.
Also, pain neuroscience education can save money. Patients who learned about pain before surgery spent less on care after surgery. If this was done across the country, it could save $1.2 billion a year.
- Pain neuroscience education improves pain beliefs and behaviors in patients with chronic pain.
- Comprehensive pain management strategies should incorporate pain neuroscience education to empower patients and improve outcomes.
- Cost savings associated with pain neuroscience education highlight its potential for healthcare system-wide impact.
By teaching patients about their chronic pain, healthcare providers can help them understand their condition better. This encourages patients to take a more active role in managing their pain. It not only improves their health but also could lessen the economic burden of chronic pain.
Functional Restoration Programs
Functional restoration programs help people with chronic pain get back on their feet. They focus on making people stronger and more able to do daily tasks. These programs tackle chronic pain from many angles, aiming to boost strength, endurance, and overall health.
At the heart of these programs are a team of experts. They include occupational therapists, physical therapists, chronic pain specialists, and care coordinators/social workers. Together, they craft treatment plans that fit each person's needs.
- The program lasts around 4 weeks.
- Participants learn in group sessions how to handle their pain and manage it better.
- Tests like measuring how far you can move, treadmill tests, and lifting tests check your current abilities. They help plan your rehab.
- Success in these programs requires commitment and effort. Changing habits, building strength, and reducing pain are key.
Joining a functional restoration program can help people with chronic pain. They can get their physical abilities back, improve their daily life, and better their quality of life. The program's focus on personal care and group support helps people take charge of their recovery and manage pain better.
For those looking to lessen chronic pain and improve daily life, functional restoration programs are a great choice. They cover physical, mental, and social aspects of pain. This holistic approach can lead to lasting improvements in well-being.
Opioid Stewardship and Safe Prescribing
The opioid crisis has made pain management programs focus on opioid stewardship and safe prescribing. Opioids carry risks like addiction and overdose. So, it's key to look for other ways to manage pain and use opioids only when really needed.
Opioid stewardship means following guidelines to use opioids wisely. Healthcare providers learn how to prescribe opioids right. They watch patients for misuse signs and try to lower the risks.
Key Elements of Opioid Stewardship
- Careful patient selection and risk assessment before starting opioid therapy
- Using non-opioid pain management first, like physical therapy and psychological help
- Prescribing the smallest dose of opioids and limiting how long they're used
- Watching patients for signs of opioid misuse and acting fast if needed
- Using tools to track opioid prescriptions and find misuse
- Teaching patients and their families about safe opioid use and disposal
By taking a full approach to opioid stewardship, healthcare providers can manage chronic pain safely. This helps reduce opioid risks. It leads to better patient outcomes and fewer opioid-related problems.
Personalized Treatment Plans
Managing chronic pain well means creating plans that fit each person's unique needs. These plans mix different treatments like medicine, physical therapy, and mental health support. This approach helps tackle the complex nature of pain.
Creating a good pain management plan means working together, understanding what triggers pain, and choosing the right treatments. It's about using a mix of medicine, physical therapy, and other methods. By making plans that fit each person, doctors can make chronic pain treatment more effective and improve results for patients.
Conclusion
Chronic pain is a complex issue that needs a comprehensive approach. It involves looking at the biological, psychological, and social sides of pain. This often means working together with a team of healthcare experts.
By using different ways to manage pain, people with chronic pain can improve their lives. They can take back control of their health and well-being. This includes things like physical therapy, talking therapies, managing medicines, and using other therapies.
Research is always looking for new ways to help with chronic pain. This leads to better treatments that tackle pain from all angles. As we learn more, we can offer more effective ways to manage pain.
Healthcare workers and those making policies need to focus on a full and team-based way to handle pain. By letting people take part in their care and offering many treatment choices, we can help those with chronic pain live better lives. They can enjoy life more and not be held back by pain.
FAQ
What is the prevalence and impact of chronic pain in the US?
Chronic pain affects about 15% of people in the US. It causes a lot of suffering and costs a lot of money each year. The costs range from 0 to 0 billion. It can make life hard, affecting how people move, socialize, and feel.
What is the comprehensive pain management approach?
This approach looks at pain from a biological, psychological, and social view. Over time, the mind and social factors play a bigger role in keeping pain going. This can lead to less activity, feeling alone, and feeling like you can't control the pain.
How do interdisciplinary treatment programs help manage chronic pain?
These programs combine different types of treatment to tackle pain from all angles. They involve doctors, psychologists, physical therapists, and others working together. This helps address the many factors that keep pain going.
What is the role of physical therapy in comprehensive pain management?
Physical therapy is key in managing pain. It sets specific goals for each patient, focusing on flexibility, core strength, and water therapy. These methods help reduce pain and improve how well you can move.
How do psychological interventions help manage chronic pain?
Psychological help, like cognitive behavioral therapy and relaxation, is crucial. These methods change negative thoughts and teach coping skills. Relaxation techniques also help by easing muscle tension and calming the nervous system.
What is the role of group education and support in comprehensive pain management?
Group sessions teach patients about managing pain, including nutrition, stress, and how pain affects health. They also encourage sharing and motivation, creating a supportive community.
How does occupational therapy contribute to chronic pain management?
Occupational therapy helps patients adapt to daily life despite pain. Therapists help patients overcome pain's impact on daily tasks. This improves independence and life quality.
What is the role of medication management in comprehensive pain management?
Managing medications is crucial in pain care. Both opioids and non-opioids are used to ease pain. Working closely with doctors is key to finding the right treatment to avoid side effects or addiction.
How can complementary and alternative therapies be integrated into a comprehensive pain management plan?
Therapies like acupuncture and massage can add to pain care. They help lessen pain and promote relaxation, supporting other treatments for better pain relief.
What is the importance of pain neuroscience education in comprehensive pain management?
Learning about pain's science is vital. It helps patients understand their pain better. This knowledge lets them take a bigger part in their care, leading to better results.
What is the role of functional restoration programs in chronic pain management?
These programs aim to boost physical and functional abilities in those with chronic pain. They focus on building strength, endurance, and physical fitness. The goal is to help patients live fuller lives.
How do comprehensive pain management programs address opioid stewardship and safe prescribing?
These programs focus on careful opioid use due to addiction risks. They look for other ways to manage pain safely. Opioids are used only when really needed and closely monitored.
How do comprehensive pain management programs tailor treatment plans to individual needs?
These programs create plans that fit each patient's unique needs and likes. They mix different treatments, like medication, physical therapy, and psychological help, to tackle pain from all sides.
Source Links
- Comprehensive pain management as a frontline treatment to address the opioid crisis
- Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care
- Is Pain Management Right for Me?
- Introducing the comprehensive pain management editorial series
- Introducing the comprehensive pain management editorial series | Brazilian Journal of Physical Therapy
- The Cost and Burden of Chronic Pain
Natural Pain Relief: Safe and Effective Home Remedies
If you're dealing with chronic pain, you're in good company. Millions worldwide face various types of discomfort, like joint pain, headaches, and muscle aches. Many turn to natural remedies instead of over-the-counter drugs for relief. This article will cover natural ways to ease pain safely and effectively.
Natural pain relief often targets the root causes of pain, like inflammation. By using these holistic methods, you can ease pain and boost your health. Whether it's joint pain, headaches, or ongoing discomfort, the remedies here might help you feel better and live better.
Essential Oils for Pain Relief
Let's look at the calming effects of lavender oil and rosemary oil. These essential oils for pain relief are getting attention for their healing powers.
Lavender Oil
Lavender essential oil is famous for its calming effects. Studies show that breathing in lavender oil or putting it on the skin can lessen pain during medical procedures. It might also ease pain, reduce swelling, and fight off harmful germs in animals.
Rosemary Oil
Rosemary oil is another option for easing pain. Research finds it helpful for anxiety, depression, and other diseases. It's also good for headaches, muscle pain, and seizures.
Rosemary oil can ease pain in those going through opium withdrawal and lessen swelling. It relaxes muscles and can improve memory too.
Remember, always mix essential oils with a carrier oil like olive oil before use. This makes them safe and effective for skin use or breathing in.

Peppermint Oil: A Natural Analgesic
Peppermint oil is a natural way to ease pain. It comes from the Mentha piperita L. plant. This oil has anti-inflammatory, antimicrobial, and pain-relieving properties. These properties help with various discomforts.
A 2015 review found peppermint oil helps with painful spasms and arthritis issues. You can use diluted peppermint essential oil on your skin. Just rub it gently on the painful area. It can help soothe aches and pains.
Peppermint oil's active parts, menthol and menthone, cause a cooling sensation. This helps with pain relief. It can also help with irritable bowel syndrome (IBS) and functional dyspepsia if taken as a supplement.
But, remember to use peppermint oil safely. Don't swallow it, as it can cause heartburn, nausea, and vomiting. Always talk to a healthcare professional before using peppermint oil for pain relief.

Eucalyptus Oil for Arthritis Pain
If you're looking for natural ways to ease pain, consider eucalyptus oil. This essential oil comes from the Eucalyptus tree. It has been shown to help people with arthritis pain.
A 2022 study found that inhaling eucalyptus oil for just 5 minutes, 3 times a day, helped reduce pain. It also improved the quality of life for people with rheumatoid arthritis. The oil's anti-inflammatory and analgesic properties may help with swelling and discomfort.
Eucalyptus oil is generally safe when used right. But, it should be kept away from children because it can slow down breathing if swallowed. Always mix it with a carrier oil like coconut or almond oil before applying it to your skin. Do a patch test first to check for any skin reactions.

Along with eucalyptus oil, try other natural remedies for arthritic pain. Some good options include:
- Lavender oil for its soothing and anti-inflammatory effects
- Ginger oil to help reduce inflammation and pain
- Frankincense and myrrh for their potential joint-supporting properties
Remember, these natural solutions may help, but always talk to your healthcare provider before trying new treatments. With the right advice, you can use eucalyptus oil and other natural remedies to manage your arthritis pain well.
Cloves: A Traditional Toothache Remedy
For centuries, people have used cloves to ease toothache pain. Clove oil has been a key part of dentistry since the 19th century. It's known for its strong pain relief and germ-fighting properties.
Eugenol in cloves numbs the pain and helps with toothaches. Studies show clove oil works as well as ice and better than some common anesthetics in kids. It's a strong pain reliever.
Clove oil also fights inflammation, fungus, and viruses. This makes it a great natural fix for many dental problems. Zinc oxide eugenol, a common dental filling, uses clove oil too.
But, be careful with cloves. Using clove oil wrong can harm your gums, teeth, and skin. Pregnant women and kids should be extra careful with it.
For quick toothache relief, over-the-counter painkillers like acetaminophen and ibuprofen work well. Dental gels with anesthetics can also numb the pain. But, don't give these to kids under 12.
If your toothache is bad or doesn't go away, see a dentist. Not treating it can lead to serious infections. A dentist can find and fix the real problem.

Cloves have been a go-to for toothaches for a long time. But, use them with care and talk to a doctor if the pain doesn't get better. Knowing the good and bad of cloves can help you choose the best for your teeth.
Capsaicin: Nature's Powerful Painkiller
One ingredient that shines for natural pain relief is capsaicin, found in chili peppers. Studies show capsaicin's power to ease different kinds of pain, like neuropathic pain.
Capsaicin for Neuropathic Pain
A 2020 study showed capsaicin helps with pain, sleep, fatigue, depression, and life quality for those with neuropathic pain. A 2021 study also found topical capsaicin cuts down neuropathic pain. It does this by lowering chemicals that send pain signals from nerve cells in the painful area. This might cause a mild burning or tingling feeling when applied.
Capsaicin makes up about 1% of chili peppers' mass, with more in the seed area. It absorbs well when used on the skin or taken by mouth, reaching up to 94% absorption.

Capsaicin and similar compounds help with many pain issues. They work by targeting specific nerve cells and lowering pain sensitivity in rats and humans. Capsaicin also boosts certain proteins that help the NMDA receptor, a key pain transmitter.
With its natural pain-fighting abilities, capsaicin is a great choice for those looking for natural relief, especially for neuropathic pain. Adding capsaicin-rich foods or products to your daily life could be a safe, effective way to ease your pain.
Ginger: A Natural Anti-Inflammatory
Ginger, also known as Zingiber officinale, is a powerful root. It has been used for a long time to help with pain and reduce inflammation. Studies show it works well for joint pain, muscle soreness, and headaches.
A 2017 study showed ginger powder worked just as well as ibuprofen for pain after surgery. Another study in 2015 found that eating 2 grams of ginger a day helped with muscle pain from exercise. It could make recovery faster and lessen inflammation from working out.
Ginger is known for its anti-inflammatory effects. A review of 16 studies with 1,010 people found that taking 1,000–3,000 mg of ginger daily for 4–12 weeks lowered inflammation. This included reducing C-reactive protein (CRP) and tumor necrosis factor-alpha (TNF-α).
People with osteoarthritis who took 500–1,000 mg of ginger daily saw less joint pain and improved mobility. They also had lower levels of inflammatory markers like TNF-α and interleukin 1 beta (IL-1β). Research suggests ginger can also help with cluster headaches.
While ginger is usually safe, it might increase bleeding risk for those on anticoagulants. It's a good idea to talk to a healthcare professional before using ginger for pain relief.
Feverfew: An Herbal Remedy for Migraines
Feverfew, also known as featherfew or bachelor's buttons, is a plant with a long history. It's been used for many health issues. Some people think it could be a good herbal migraine remedy and natural way to ease pain.
Studies say feverfew has compounds that might lessen inflammation and muscle spasms. These are big factors in causing migraine headaches. The American Migraine Foundation says the results on feverfew for preventing migraines are mixed. But, it thinks it could help some people.
A 2023 study found that feverfew could have anti-inflammatory, antioxidant, and neuroprotective effects. This makes it a promising natural choice for those looking for feverfew, herbal migraine remedy, and natural pain relief. But, finding the best dose and checking safety over time is still being looked into.

If you're thinking about trying feverfew for migraines or pain, talk to your doctor first. Feverfew might not mix well with some medicines or could have side effects, especially for pregnant people. Overall, feverfew looks promising as an herbal migraine remedy and natural pain relief option. But, we need more studies to know for sure how well it works and if it's safe.
Turmeric: A Powerful Natural Pain Reliever
Turmeric is a bright spice often found in Indian dishes. It's known for its health perks. The key ingredient, curcumin, fights inflammation and helps with pain. This makes it a good choice instead of regular painkillers.
A 2021 review showed curcumin can ease pain as well as some over-the-counter drugs. But, experts suggest adding turmeric to your current pain treatment, not replacing it. Turmeric works more slowly and isn't as strong as some medicines.
You can add turmeric to many foods for its pain-relieving benefits. Put it in curries, smoothies, or juices. It makes food taste better and helps your body fight inflammation. This could lessen pain and discomfort.
Even though turmeric is usually safe, talk to your doctor before using it. This is especially true if you're on other medicines or have health issues. Using turmeric can be a natural way to handle pain and improve your health.
Acupuncture for Natural Pain Management
For those looking for natural pain relief, acupuncture could be a good choice. Acupuncture uses thin needles at certain body points to balance energy and help nerves, muscles, and tissues. This ancient Chinese method is now popular in the U.S. as a way to handle chronic pain.
Acupuncture Benefits
Studies show acupuncture can help with pain. The National Center for Complementary and Integrative Health says it can ease musculoskeletal pain, headaches, and osteoarthritis pain. A 2018 study found acupuncture helps with chronic pain, especially for musculoskeletal, headache, and osteoarthritis pain.
More research is needed on acupuncture for other pain issues. But, the evidence shows it can be a great option for managing pain naturally. Many people have seen big improvements, not just in pain, but also in sleep, energy, and stress levels.
Acupuncture is a safe, natural way to ease pain. With skilled practitioners, the risks are low. It's a good choice for those wanting to avoid just relying on drugs. If you're struggling with chronic pain, headaches, or joint pain, acupuncture might be something to think about for your pain relief plan.
Yoga for Pain Relief
If you're looking for natural ways to ease pain, yoga could be a good choice. It's a mix of physical and mental exercises that can help with back pain, neck pain, and chronic issues like arthritis and fibromyalgia. Yoga uses gentle stretches, strengthening moves, and relaxation to lessen pain and boost your health.
Yoga is great for improving flexibility and movement. Poses like Cobra Pose (Bhujangasana) and Child's Pose (Balasana) focus on muscles and joints that often hurt. This can make moving easier and reduce stiffness. Yoga also teaches deep breathing and mindfulness to calm the mind and body, which can lessen pain.
Studies show yoga is effective for different kinds of pain. For example, a 2020 study found yoga cut down lower back pain after 12 weeks. The National Center for Complementary and Integrative Health (NCCIH) says yoga might help with lower back and neck pain. But, more research is needed for other conditions like headaches, arthritis, or fibromyalgia.
Starting with yoga for pain relief? Begin with easy practices and find a skilled teacher to help with proper form and adjustments. Adding yoga to your routine, along with a diet full of nutrients that help with pain, could lead to better health and a more active life.
Mindfulness Meditation: A Mind-Body Approach
If you're dealing with chronic pain, mindfulness meditation might help. It's a mind-body method that's becoming more popular for natural pain relief. Studies show it can lessen pain, improve mood, and enhance life quality.
A 2017 review looked at 38 studies on this topic. It found that mindfulness meditation is a good way to manage chronic pain. More research is needed, but it looks promising as an extra or alternative to usual pain treatments.
- Mindfulness meditation means focusing on now, often by watching your breath or body sensations.
- This helps you notice your thoughts and feelings better. It lets you handle pain and stress with more acceptance and kindness.
- Doing it regularly can make pain less intense and reduce feelings of depression and anxiety.
Starting with meditation? Take it slow and be kind to yourself. Just a few minutes a day can make a big difference over time. Talk to your doctor about adding mindfulness meditation to your natural pain relief plan.
Natural Pain Relief
Many people are now looking for natural remedies instead of traditional pain meds. These options can be safe and effective, especially for those wanting to avoid prescription drug side effects. There are many natural pain relief methods to try, from essential oils to herbal supplements.
Turmeric is a spice from Indian cooking that's known for its pain relief. It has a compound called curcumin that fights inflammation and reduces pain. Ginger is another spice that helps with chronic pain because it's anti-inflammatory.
- Acupuncture, an ancient Chinese practice, helps with chronic pain like knee osteoarthritis, back pain, and fibromyalgia.
- Mindfulness meditation and cognitive-behavioral therapy (CBT) help manage chronic pain by teaching coping skills and reducing stress and anxiety.
- CBD oil, from the hemp plant, is effective for chronic pain from conditions like multiple sclerosis, arthritis, and neuropathic pain.
Remember, not every natural remedy works for everyone. You might need to try a few to see what helps you the most. Always talk to a healthcare professional before starting any new supplements or therapies to make sure they're right for you.
Conclusion
This article looked at many ways to ease pain naturally, like essential oils, herbal remedies, acupuncture, yoga, and mindfulness. While some need more study, many have found relief with these natural methods. Always talk to a doctor before trying new remedies, especially if you have health issues or take other drugs.
Looking into natural pain relief can help you find what works best for you. Essential oils and turmeric can ease pain without the risks of some medicines. You might try acupuncture, yoga, or a mix of therapies to manage pain better. This holistic way can help you control your health and find lasting relief.
Don't be shy to try the natural remedies talked about here and talk to your doctor for a full plan. Starting your health journey with natural solutions can help ease your pain and better your life quality.
FAQ
What are some natural ways to relieve pain?
There are many ways to ease pain naturally, like using essential oils and herbal remedies. You can try lavender oil, rosemary oil, peppermint oil, eucalyptus oil, and cloves. Capsaicin, ginger, feverfew, turmeric, acupuncture, yoga, and mindfulness meditation also help.
How can lavender oil help with pain relief?
Studies show that lavender oil can lessen pain when inhaled or applied to the skin. It's known for its pain-relieving, anti-inflammatory, and antioxidant effects.
What are the benefits of rosemary oil for pain relief?
Rosemary oil might help with headaches, muscle, and bone pain, and seizures. It can also ease pain in those going through opium withdrawal. Plus, it reduces inflammation, relaxes muscles, and boosts memory.
How can peppermint oil be used for pain relief?
Peppermint oil has anti-inflammatory and pain-relieving properties. Applying it to the temples and forehead can ease tension headaches. People often mix it with a carrier oil and rub it on sore areas.
How can eucalyptus oil help with arthritis pain?
A study in 2022 showed that eucalyptus oil helped reduce pain and improve life quality in people with rheumatoid arthritis. It should be mixed with a carrier oil and used carefully, as it can be harmful if swallowed.
How can cloves be used to relieve toothache pain?
Cloves have long been used to ease toothache pain. A 2021 study found that clove oil worked as well as ice and was stronger than a local anesthetic during dental procedures in children.
How can capsaicin help with neuropathic pain?
Capsaicin can lessen neuropathic pain, according to a 2021 study. It does this by reducing chemicals that carry pain signals from nerve cells in the affected area.
What are the pain-relieving benefits of ginger?
Ginger has been shown to be as effective as ibuprofen in reducing post-surgery pain. A 2015 review found that ginger helped reduce muscle pain from exercise and running.
How can feverfew help with migraines?
Feverfew is often used for migraines. While its effectiveness varies, it's thought to help prevent migraine headaches. A 2023 study suggests it has anti-inflammatory and antioxidant effects.
What are the pain-relieving properties of turmeric?
Turmeric contains curcumin, which helps with pain. A 2021 review found that curcumin can reduce pain as well as some drugs do. It's recommended as a supplement to pain medications, not a replacement.
How can acupuncture help with pain management?
Acupuncture can help with pain, including musculoskeletal, headache, and osteoarthritis pain. A 2018 study found it effective for chronic pain.
What are the pain-relieving benefits of yoga?
Yoga has been shown to reduce lower back pain, according to a 2020 study. The National Center for Complementary and Integrative Health suggests it may help with lower back and neck pain, but not other types of pain.
How can mindfulness meditation help with chronic pain?
Mindfulness meditation can improve pain, depression, and quality of life for those with chronic pain, a 2017 review found. However, more research is needed to fully understand its benefits.
Source Links
- 5 Surprising Natural Painkillers: Boswellia, Turmeric, and More
- 13 home remedies for pain
- Try 18 Essential Oils for Sore Muscles
- essential oils for pain relief
- Top 12 herbs and other remedies for natural pain relief
Effective Treatments for severe neck pain and headache base of skull
Neck pain and headaches can really slow you down. They might come from infections, stress, or other health issues. If you're feeling okay at home, that's good. But watch out for a fever or if the pain gets worse. That could mean you need a doctor's help.
Many people suffer from severe neck pain and headache base of skull, often without understanding why it happens or what truly helps. These pains can feel crippling especially when they interfere with your work, sleep, and daily life.
In this blog, we will break down the most effective treatments for severe neck pain and headache base of skull, explain what's causing this pain, and show how to manage and prevent it for good. No fluff. Just real solutions, backed by medical science and explained in simple language you can actually understand.
What’s Causing Your Neck and Skull Discomfort?
Your pain isn't in your head. It often starts deep in the neck or at the base of the skull and radiates out. To treat it, you first need to know what parts of your body are involved and what's triggering the discomfort.
Anatomy of the Upper Neck and Skull Base
The base of the skull and upper neck is packed with sensitive structures that can all contribute to pain:
- Occipital nerves: These nerves run from the upper neck to the scalp. When irritated, they cause sharp or throbbing pain at the base of the skull.
- Cervical spine (C1–C3): The top vertebrae of your spine. Misalignment, disc issues, or arthritis here can lead to pressure and pain.
- Trapezius muscle: This large muscle stretches across your upper back and neck. Tension here can create headaches.
- Suboccipital triangle: A group of small muscles at the skull base, often tight or inflamed in people with chronic neck pain.
Understanding this setup helps pinpoint why the severe neck pain and headache base of skull feels the way it does.
Common Causes Behind the Pain
There isn't just one cause. Your pain may be linked to multiple overlapping issues. Here are the most common ones:
- Occipital neuralgia: Irritation of the occipital nerves that causes stabbing or throbbing pain.
- Cervicogenic headache: Pain that starts in the neck but feels like a headache.
- Muscle strain or tension: Often from poor posture, stress, or long hours at a desk.
- Herniated disc: A slipped disc in the upper cervical spine can press on nerves.
- Poor posture/tech neck: Slouching over phones or computers strains neck muscles.
- Whiplash or trauma: Even minor accidents can throw off alignment and strain muscles.
- Arthritis or degenerative joint disease (DJD): Wear-and-tear in the cervical spine joints.
Stat: Nearly 20% of adults suffer from chronic neck pain, and up to 4% experience occipital headaches, according to the NIH.
Symptoms of Severe Neck Pain and Headache at the Base of Skull
Identifying your symptoms can help you understand whether you’re dealing with a deeper nerve issue or just muscle tension. Either way, the symptoms of severe neck pain and headache base of skull are hard to ignore.
How to Recognize a Suboccipital Headache
This type of headache has some signature signs:
- Throbbing or pulsing pain at the base of the skull
- Pain that radiates to the temples or behind the eyes
- Neck stiffness or difficulty turning the head
- Scalp sensitivity or tenderness when touched
- Visual problems or light sensitivity
- Nausea or dizziness during headache episodes
These headaches are often mistaken for migraines or sinus headaches, but their origin is actually neck-related.
Types of Headaches Caused by Neck Pain
Neck pain can lead to different types of headaches, like cervicogenic headaches and occipital neuralgia. It's important to know how neck problems relate to these headaches for better treatment and relief.
Cervicogenic Headaches
Cervicogenic headaches start in the neck but move to the head. They are usually on one side and may make turning the neck uncomfortable. Studies show these headaches affect 0.4% to 4% of people, especially those aged 30 to 44.
These headaches can come from neck issues like arthritis, a slipped disc, or whiplash. Jobs that involve sitting a lot or sleeping in bad positions can also cause them.
Occipital Neuralgia
Occipital neuralgia is another headache type linked to neck pain. It happens when the occipital nerve in the neck gets pinched or irritated. People with this condition feel sharp, stabbing pain at the back of the head and scalp sensitivity.
Managing cervicogenic headaches and occipital neuralgia often means using medicine, physical therapy, and treatments like nerve blocks. Fixing the neck problems can help relieve these headaches.
Read → Cluster Headaches: How to treat
Types of Headaches That Lead to Neck Pain
Headaches and neck pain often go together. Certain headaches, like tension headaches and migraines, are common causes of neck pain.
Tension Headaches
Tension headaches are the most common type. They can make the neck hurt. These headaches feel like pressure or tightness around the forehead and neck.
The muscles at the base of the skull can get inflamed and sore. This adds to the pain.
Migraines
Migraines are a type of headache that can cause neck pain too. Often, people feel neck pain right when the migraine starts. Doctors aren't sure if the neck pain causes the migraine or if it's a symptom.
It's important to understand how headaches and neck pain are linked. By finding the cause and getting the right treatment, people can feel better and live better lives.
Lifestyle Changes to Prevent Recurrence
Changing small habits can dramatically reduce the chance of future flare-ups.
Desk Ergonomics and Screen Time Limits
Adjusting your workstation setup can prevent strain:
- Keep screens at eye level to avoid forward head posture
- Use chairs with good lumbar support
- Take breaks every 30 minutes to move around
This is essential for neck pain caused by posture.
Sleep Position and Pillow Choice
The wrong pillow can worsen neck issues:
- Use a cervical pillow to support the natural curve of your neck
- Sleep on your back or side, not your stomach
- Avoid pillows that are too high or too firm
Hydration, Diet, and Magnesium
What you eat and drink affects how your muscles feel:
- Drink at least 2 liters of water daily
- Add magnesium-rich foods like spinach, almonds, and black beans
- Eat anti-inflammatory meals: fish, leafy greens, berries
Magnesium may help reduce chronic neck pain relief naturally.
Proven Medical Treatments for Severe Neck Pain and Headache Base of Skull
Once diagnosed, your treatment plan will likely include a combination of therapies. Let's break down what works best for severe neck pain and headache base of skull.
Physical Therapy and Postural Training
Physical therapy is the cornerstone for long-term relief. It targets the root causes.
- Gentle neck stabilization exercises to strengthen deep muscles
- Myofascial release to loosen tight tissues
- Posture correction to fix slouching and forward head position
- Ergonomics training to adjust your workstation
Stat: A study in the Journal of Orthopaedic & Sports Physical Therapy found physical therapy reduced cervicogenic headache symptoms by over 70% in 6 weeks.
Medications
Short-term use of medication can help reduce inflammation and interrupt pain signals.
- NSAIDs like ibuprofen for swelling
- Muscle relaxants to ease tension
- Nerve pain medications like gabapentin
- Corticosteroid injections for occipital neuralgia treatment
These may not cure the condition but are very useful when pain flares.
Nerve Blocks & Injections
For cases that don’t respond to meds, injections can deliver targeted relief.
- Occipital nerve blocks: Inject anesthetic near the nerve to shut down pain.
- Trigger point injections: Calm overactive muscle fibers that generate referred pain
Stat: According to the American Migraine Foundation, occipital nerve blocks provide relief in 85% of patients with occipital neuralgia.
Advanced Interventions
In complex cases, these procedures may offer relief when others fail:
- Radiofrequency ablation (RFA) to deactivate pain-carrying nerves
- Spinal decompression therapy to reduce disc pressure
- Botox injections (off-label) to reduce muscle tension
These are usually done after imaging and evaluation by a specialist.

Seeking Professional Help
If you have ongoing or severe neck pain with headaches, you should get medical help. Look out for these red flags that mean you should see a doctor:
- Headache with fever, weight loss, confusion, or sudden start
- A change in your usual headache pattern
- Severe or ongoing neck pain and stiffness
- Pain that spreads down your arm
- Difficulty moving your head
It's key to get professional help for [when to see a doctor for neck pain and headaches]. Your doctor will do a detailed check-up, order tests, and figure out what's wrong. They can then make a plan to fix the main cause of your [red flags for seeking medical attention].
Cervicogenic Headaches: A Closer Look
Cervicogenic headaches come from a neck issue, not a head problem. They start at the back of the skull and move forward. You might feel stiff in the neck and find it hard to move it.
Symptoms of Cervicogenic Headaches
The main signs of cervicogenic headaches are:
- Pain on one side of the head, starting at the skull base and going to the forehead or eye
- Neck stiffness and less movement in the neck
- More pain when you move or change positions in your neck
- Sensitivity to light and sound
- Nausea or vomiting in some cases
Causes of Cervicogenic Headaches
Several neck issues can lead to cervicogenic headaches. These include:
- Whiplash: Quick, jerky neck movements, often from a car crash, can cause these headaches.
- Arthritis: Neck arthritis can irritate and inflame, leading to headaches.
- Neck Injuries: Neck muscle, tendon, or ligament injuries can also trigger headaches.
The pain comes from the neck and the trigeminal nerve working together. This mix sends pain signals to the head.
Diagnosing Cervicogenic Headaches
Diagnosing cervicogenic headaches can be tricky. They might seem like other headaches, like migraines or tension headaches. Your doctor will work hard to find the real cause by checking if your neck and head are connected to the pain.
Your doctor might do a detailed physical assessment. This means checking if moving your head and spine helps or changes your symptoms. They might also suggest nerve blocks to see if your neck really is the cause of your headaches.
Also, your doctor could order imaging tests, like an MRI. This scan looks at your neck's bones, tissues, and nerves. It helps spot any problems, like disc issues or nerve damage, that might be causing your headaches.
With a full physical check-up, nerve blocks, and imaging tests, your doctor can pinpoint the cause of your cervicogenic headaches. Then, they can make a treatment plan to fix the problem.
Treatment Options for Cervicogenic Headaches
If you're dealing with cervicogenic headaches, there are ways to find relief. The main goal is to fix the neck or spine issues causing the pain.
Physical Therapy
Physical therapy is often the first step for cervicogenic headaches. Experts in physical therapy can pinpoint the pain source. They'll create a plan with exercises to help your posture, strengthen neck muscles, and improve flexibility.
Medications
Your doctor might suggest over-the-counter or prescription drugs for pain relief. Options include non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants. They can help ease the pain and discomfort from cervicogenic headaches.
Interventional Treatments
For severe or ongoing cervicogenic headaches, more advanced treatments might be needed. These include nerve blocks, radiofrequency ablation, and transcutaneous electrical nerve stimulation (TENS). In some cases, neuromodulation surgery to stimulate the occipital nerve could be an option.
The Pain Management NYC clinic in Midtown Manhattan offers advanced treatments for cervicogenic headaches. They work with each patient to find the best solution for neck pain and headaches.
Preventing and Managing Chronic Cervicogenic Headaches
If you have ongoing or frequent cervicogenic headaches, it's key to work with your healthcare provider. Together, you can create a plan that might include physical therapy, medicine, and other treatments. This plan aims to fix the root causes and help you feel better over time.
Preventing these headaches can be done by keeping a good posture, making your workspace comfortable, and managing stress. By doing these things, you can lessen the number and intensity of cervicogenic headaches. This proactive approach helps you take charge of your health.
A study showed that up to 22% of people with ongoing headaches might have cervicogenic headaches. It's important to know the signs like neck pain, limited neck movement, and shoulder pain. This knowledge helps doctors diagnose and treat the condition effectively.
Tests like X-rays, CT scans, and MRI scans can show what's causing cervicogenic headaches. This info lets doctors make treatment plans just for you. These plans might include:
- Physical therapy to improve neck and shoulder movement, strengthen muscles, and help with posture
- Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), to help with pain and swelling
- Interventional treatments, like nerve blocks or radiofrequency ablation, to target specific nerve pain sources
Adding changes to your lifestyle, trying alternative therapies, and using home remedies like relaxation, yoga, and cognitive behavioral therapy can also help. These methods work alongside traditional treatments to manage cervicogenic headaches.
By working with your healthcare provider and using a variety of approaches, you can manage your chronic cervicogenic headaches. This can greatly improve your life quality.
When to See a Specialist for Severe Neck Pain and Headache Base of Skull
You’ve tried at-home care. You’ve taken meds. If pain still lingers, it’s time to see a professional.
Neurologist vs. Orthopedic vs. Pain Management Specialist
Each specialist has a unique role:
| Specialist | What They Do |
| Neurologist | Evaluates nerve-related pain and headaches |
| Orthopedic doctor | Handles bone and spine alignment issues |
| Pain specialist | Offers injections and long-term pain management |
Booking a visit with Dr. Chandril Chugh ensures you’re not left guessing.
Imaging Tests That May Be Needed
These tools help pinpoint the root cause of the problem:
- MRI to view nerves, discs, and soft tissues
- CT scan to examine bone structure and injury
- Nerve conduction tests to assess nerve function
Advanced imaging ensures your treatment is precise.
Conclusion
Severe neck pain and headache base of skull doesn’t have to rule your life. With the right approach, you can stop masking symptoms and actually solve the problem. Whether it’s nerve-related, posture-driven, or stress-induced, a neurologist like Dr. Chandril Chugh can guide you toward relief that lasts.
Dr. Chandril Chugh is a US-trained, board-certified neurologist known for helping patients overcome migraines, suboccipital headaches, tension-related pain, and complex nerve conditions.
If you're tired of living with this pain, don’t wait. Book your consultation with Dr. Chugh today and get the expert care you need.
FAQ
What are some common causes of neck pain and headaches?
Neck pain and headaches can come from many things like infections, stress, and being sick. Poor posture, eye strain, and injuries can also cause these symptoms.
What are the different types of headaches that can be caused by neck pain?
Neck pain can lead to headaches like cervicogenic headaches, occipital neuralgia, tension headaches, and migraines.
How are cervicogenic headaches different from other types of headaches?
Cervicogenic headaches come from a neck problem. They cause pain on one side of the head, neck stiffness, and discomfort with certain neck movements.
What are some of the potential causes of cervicogenic headaches?
Cervicogenic headaches can come from things like whiplash, arthritis, neck sprains, or a neck fracture. These issues can affect the upper cervical vertebrae.
How can cervicogenic headaches be diagnosed?
Diagnosing cervicogenic headaches can be tough. Doctors might use a physical check-up, nerve blocks, and imaging tests to look at the neck's bones, tissues, and nerves.
What are the treatment options for cervicogenic headaches?
Treatments for cervicogenic headaches aim to fix the root cause. Options include physical therapy, medicines, nerve blocks, radiofrequency ablation, TENS, and sometimes surgery.
When should someone seek medical attention for neck pain and headaches?
If you have a headache with fever, weight loss, confusion, sudden onset, or a change in your headaches, see a doctor. Look for signs like severe or ongoing neck pain, pain down the arm, or trouble moving your head.
How can home remedies and self-care measures help with neck pain and headaches?
Home remedies like better workplace setup, good posture, and quality sleep can ease headaches from neck pain. But, if these don't work, you might need medical help.
What are some medical treatments for severe neck pain and headache at the base of the skull?
For severe neck pain and headaches, treatments might include nerve blocks, radiofrequency ablation, and TENS. In some cases, surgery might be an option.
How can chronic cervicogenic headaches be prevented and managed?
To prevent and manage chronic cervicogenic headaches, work with your doctor on a treatment plan. This might include physical therapy, medication, and other treatments. Keeping good posture and managing stress can also help reduce headaches.
Source Links
- Neck pain with a headache: Symptoms, causes, and treatments
- What Is Causing My Neck Pain and Headache?
- Understanding Cervicogenic Headaches & Neck Pain | Advanced Spine
- What Causes Neck Pain?
How to Cope with Central Pain Syndrome
Living with central pain syndrome is tough and can really slow you down. This condition happens when the central nervous system gets damaged. It makes you feel pain more easily and even hurts from things that don't usually bother you. But, there are ways to handle this pain and make your life better.
Understanding central pain syndrome and what causes it is key to coping. Things like stroke, multiple sclerosis, Parkinson's disease, and spinal cord injuries can lead to it. These conditions cause a variety of pains, from burning to sharp pains. Knowing about these can help you and your doctors find the right treatment.
Handling central pain means using both medical and lifestyle changes. Doctors might suggest medicines like antidepressants or anticonvulsants for pain. They might also recommend physical therapy, cognitive-behavioral therapy, and ways to reduce stress. Taking care of yourself by sleeping well, exercising, and managing stress is also important.
You're not alone in fighting central pain syndrome. Joining support groups and finding resources can give you a lot of help. It can make you feel less alone and help you find ways to deal with the pain. Being active in your care and having a caring network around you can make a big difference.
Understanding Central Pain Syndrome
Central pain syndrome is a complex condition that happens when the central nervous system (CNS) gets damaged. This includes the brain, brainstem, and spinal cord. It's different from neuropathic pain, which comes from nerve damage. Central pain syndrome changes how the brain and spinal cord handle pain signals.
What is Central Pain Syndrome?
This condition makes people more sensitive to pain. The brain overreacts to things that wouldn't normally hurt. People with it might feel burning, "pins and needles," aching, or sharp pain.
Causes of Central Pain Syndrome
It can come from injuries to the brain or spinal cord. Conditions like multiple sclerosis, Parkinson's disease, and spinal cord injuries can also cause it. Stress, early trauma, and infections might play a role too.
Studies say genetics and environment both play a part in getting central pain syndrome. Fibromyalgia, which affects the nervous system, shares some risk factors. This might make people more likely to have a hypersensitive central nervous system.
Symptoms of Central Pain Syndrome
Central pain syndrome is a complex condition that affects daily life. It's a type of neuropathic pain with symptoms that are hard to manage. These symptoms can be both physical and emotional challenges.
Types of Pain Experienced
The main symptom is chronic, unexplained pain that lasts over 3 months. This pain can be constant or come and go. People often describe it as burning, sharp, stabbing, or severe itching.
They might also feel numbness, tingling, or a "pins and needles" feeling (paresthesia). This makes everyday activities tough.
Associated Symptoms
- Heightened sensitivity to touch or temperature (hyperalgesia and allodynia)
- Anxiety, depression, and mood disturbances
- Memory problems and cognitive impairment
- Fatigue and sleep disturbances
Having chronic pain, sensory changes, and psychological symptoms can really affect someone's life. It's important to understand these symptoms for better management and support.
Risk Factors for Central Pain Syndrome
Central pain syndrome (CPS) is a complex condition that greatly affects a person's life. Knowing the risk factors helps in early detection and management. Several factors can lead to CPS.
Direct injury to the brain or spinal cord is a big risk. This includes injuries from strokes, multiple sclerosis, or spinal cord trauma. Such injuries can mess with how pain signals work, causing CPS. Chronic pain conditions like fibromyalgia also raise the risk by making the central nervous system more sensitive to pain.
Genetics might also play a part in CPS. If a first-degree relative has CPS, you're more likely to get it too. This suggests there might be a genetic link.
- Emotional stress and trauma can up the risk of CPS. They affect the nervous system and how we feel pain.
- Depression and obesity are also linked to CPS. They can cause chronic inflammation and change how the body processes pain.
Knowing these risk factors helps doctors spot people at higher risk of CPS. Early action can prevent or lessen the effects of this condition.

Diagnosing central pain syndrome
Diagnosing central pain syndrome is complex because there's no single test. Your doctor will start by taking a detailed medical history. They will ask about the onset, location, and nature of your pain. They'll also ask about any related medical conditions or injuries.
Medical History Evaluation
Your doctor will look into your symptoms during the medical history evaluation. They will consider the following:
- The onset and duration of your pain
- The specific location(s) of your pain
- The characteristics of your pain (e.g., burning, stabbing, aching)
- Any factors that seem to aggravate or alleviate your pain
- Any associated symptoms, such as muscle spasms or changes in sensitivity
- Your medical history, including any injuries, illnesses, or conditions that may be related to your pain
Diagnostic Tests
Your doctor may also order diagnostic tests to find the cause of your central pain syndrome:
- Imaging tests, such as MRI or CT scans, to look for any structural changes or damage to the brain or spinal cord
- Blood tests to check for underlying conditions that may be contributing to your pain
- Electromyography (EMG) or nerve conduction studies to assess nerve function
A diagnosis of central pain syndrome is made by considering your symptoms, medical history, and diagnostic test results. Your doctor will work with you to create a treatment plan. This plan aims to manage your pain and improve your quality of life.
Treatment Approaches for Central Pain Syndrome
Dealing with central pain syndrome often means using a mix of treatments. This includes lifestyle and mental health changes. These are key to managing this complex condition.
Lifestyle and Mental Health Strategies
Physical therapy can boost mobility and function for those with central pain syndrome. It helps improve overall well-being. Cognitive-behavioral therapy is also useful. It helps develop ways to cope with chronic pain's mental effects.
Stress management, like mindfulness and meditation, can ease the mental and emotional load of central pain syndrome. Exercise, suited to each person's abilities, helps with pain control and better health.
It's important to tackle any mental health issues, like anxiety or depression, for better pain management. Mental health experts offer valuable advice and strategies. This helps with the emotional and psychological sides of the condition.

- Physical therapy to improve mobility and function
- Cognitive-behavioral therapy to develop coping mechanisms
- Stress management techniques like mindfulness and meditation
- Regular exercise tailored to individual needs
- Addressing mental health conditions like anxiety and depression
By adding these lifestyle and mental health strategies to a treatment plan, people with central pain syndrome can better manage their symptoms. This leads to a better quality of life.
Medication Options for Central Pain Syndrome
Managing central pain syndrome often means using a mix of treatments. Medications are key in helping to ease the pain. Unlike regular pain meds, some drugs target the neurological roots of the pain.
Antidepressants
Antidepressants like duloxetine, amitriptyline, and nortriptyline can help with central pain syndrome. They adjust neurotransmitters in the brain to lessen pain. These can be especially useful for those with depression or anxiety, which can make pain worse.
Anticonvulsants
Anticonvulsants, including gabapentin, carbamazepine, and pregabalin, are also useful for central neuropathic pain. They stabilize electrical activity in the nervous system. This can reduce pain intensity and how often it happens. The right medication and dose depend on the patient's needs and how they react.
Working closely with a healthcare expert, like a neurologist or pain specialist, is crucial. They can tailor a treatment plan for your central pain syndrome. They'll look at your symptoms, any other conditions, and check how well the treatment is working.
Surgical Interventions for Central Pain Syndrome
When traditional treatments don't work, doctors might suggest surgery for central pain syndrome. Two surgeries that help manage this condition are motor cortex stimulation and deep brain stimulation.
Motor Cortex Stimulation
For motor cortex stimulation, doctors place electrodes on the brain's surface. This targets the area that controls movement of the painful area. An implanted device sends electrical pulses to this area, easing the pain for some patients.
Deep Brain Stimulation
Deep brain stimulation puts electrodes deep in the brain's pain areas. An implanted device sends electrical signals to block abnormal pain signals. This surgery is a long-term solution for neuropathic pain from central pain syndrome.
Not every person with central pain syndrome is a good candidate for surgery. But, it's a hope for those who've tried everything else. Doctors and patients work together to find the best treatment plan for each person.
Living with Central Pain Syndrome
Living with central pain syndrome is tough but not impossible. With the right strategies and support, people can manage their symptoms and live better. It's a journey that requires patience and understanding.
Coping Mechanisms
It's key to find ways to cope with central pain syndrome. Techniques like mindfulness, relaxation, and pacing can help. These methods help manage stress and energy levels, making it easier to deal with pain.
Support Resources
- Support from family, friends, and doctors is crucial. Joining support groups online or in person can create a sense of belonging. It helps to share experiences with others who understand.
- It's important to address mental health issues like depression or anxiety. Counseling or therapy can help. These services offer ways to cope and stay positive.
- Trying alternative therapies like acupuncture, massage, or mindfulness can also be helpful. They can be part of a plan to manage pain.
Using coping strategies and support can make a big difference. People with central pain syndrome can improve their lives and adapt to their condition.

Genetic Factors In Central Pain Syndrome
Studies show that genetics are key in developing central pain syndrome. If you have a first-degree relative with the condition, your risk goes up by eight times. This includes parents, siblings, or children.
We haven't found the exact genetic mutations yet. But, it's clear that some people are more likely to get central pain due to their genes. Researchers are looking into how genes and environment work together to cause this condition.
Here are some important facts about the genetics of central pain syndrome:
- Genes might cause about a third (30%) of chronic regional pain syndrome (CRPS), a type of central pain.
- Some genetic changes, like in the ANO10, P2RX7, PRKAG1, and SLC12A9 genes, make CRPS more likely, especially in men.
- The study of pain genetics is moving fast. Researchers use new tech like whole-genome sequencing to understand how genes and pain interact.
As we learn more about the genetics of central pain, we might find new ways to prevent, diagnose, and treat it. This could make life better for those with this condition.

Distinguishing Central Pain Syndrome from Fibromyalgia
Central pain syndrome and fibromyalgia are both chronic pain conditions that affect the central nervous system. But they are different. Central pain syndrome comes from injury or damage to the brain or spinal cord. Fibromyalgia doesn't have a clear change in the central nervous system.
Fibromyalgia is known for widespread musculoskeletal pain, fatigue, headaches, and digestive issues. These symptoms might not always be seen in central pain syndrome.
To figure out which condition someone has, doctors need a detailed medical history, a thorough physical check-up, and sometimes tests. Knowing the differences between these two chronic pain disorders helps doctors make better treatment plans.
- Central pain syndrome is caused by direct injury or damage to the brain or spinal cord.
- Fibromyalgia does not have a clear structural or functional change in the central nervous system.
- Fibromyalgia is often accompanied by symptoms like widespread musculoskeletal pain, fatigue, headaches, and digestive issues.
- Diagnostic testing, including a comprehensive medical history and physical exam, is crucial to distinguish between central pain syndrome and fibromyalgia.
It's important for healthcare providers to know the unique traits of central pain syndrome and fibromyalgia. This knowledge helps them give personalized care to people with chronic pain. By understanding the differences, doctors can make treatment plans that meet the specific needs of each patient.
Emerging Treatments and Research
Researchers are looking into new ways to help with central pain syndrome. They're checking out hypnosis, transcranial magnetic stimulation (TMS), and deep brain stimulation. These methods could change how we treat pain.
Hypnosis might help reduce pain and make it easier to manage for people with central pain syndrome. It works by focusing the mind and making it more open to suggestions. This can affect how the brain processes pain.
Transcranial magnetic stimulation (TMS) doesn't need surgery and uses magnetic fields to reach the brain. It could help lessen central pain syndrome symptoms by changing how the brain handles pain.
- TMS is being looked at as a way to treat chronic pain, including central pain syndrome.
- Studies are checking if TMS is safe and works well over time for central pain syndrome.
Deep brain stimulation (DBS) is another new method being studied. It involves putting electrodes in the brain to send electrical signals. These signals might help reduce pain and improve pain management.
We need more research to see how these new treatments work long-term. But they give hope to people with central pain syndrome who haven't found relief with other treatments. Ongoing studies and trials are key to improving our understanding and care for this condition.
Conclusion
Central pain syndrome is a tough condition that needs a detailed approach to handle. By understanding its causes, finding risk factors, and looking at different treatments, people with central pain syndrome can work with doctors to manage their symptoms. This helps improve their life quality and cope with chronic pain.
There's still much to discover about this condition. But, ongoing research and new treatments offer hope for those with central pain syndrome. From genetic studies to new treatments and focusing on mental health and lifestyle, there are many ways to find relief from pain.
By staying informed, asking for personalized care, and using coping strategies, people in India can manage their central pain syndrome better. Remember, you're not alone in this fight. There are resources and support out there to help you deal with this complex condition.
FAQ
What is central pain syndrome?
Central pain syndrome is a long-term condition. It changes how the brain and spinal cord handle pain signals. This leads to feeling more pain and pain from things that don't usually hurt.
What causes central pain syndrome?
It can happen after injury or damage to the brain or spinal cord. Conditions like multiple sclerosis, Parkinson's disease, and spinal cord injuries can also cause it.
What are the main symptoms of central pain syndrome?
The main symptom is ongoing, unexplained pain that lasts over 3 months. This pain can be constant or come and go. People may feel burning, sharp, stabbing, or severe itching pain.
They might also notice changes in touch, like numbness, tingling, or a "pins and needles" feeling.
What are the risk factors for developing central pain syndrome?
Risk factors include injuries or damage to the brain or spinal cord. Conditions that cause ongoing pain, genetic factors, emotional stress, psychological trauma, depression, and obesity also increase the risk.
How is central pain syndrome diagnosed?
Doctors diagnose it by looking at your medical history, doing a physical check-up, and possibly using imaging tests and blood tests to rule out other conditions.
How is central pain syndrome managed?
Treatment involves a mix of lifestyle changes, mental health support, medicines, and sometimes surgery. This includes things like motor cortex stimulation or deep brain stimulation.
What role do genetics play in central pain syndrome?
Genetics are very important in developing central pain syndrome. If you have a family member with it, your risk is much higher.
How is central pain syndrome different from fibromyalgia?
Both conditions are chronic pain issues affecting the central nervous system. But, central pain syndrome comes from direct injury or damage to the brain or spinal cord. Fibromyalgia doesn't have this specific cause.
What are some emerging treatments for central pain syndrome?
Researchers are looking into new treatments like hypnosis, transcranial magnetic stimulation, and other neuromodulation methods. These aim to change how the central nervous system handles pain.
Source Links
- Centralized pain syndrome: Symptoms and treatment
- Central Pain Syndrome (CPS): Symptoms & Treatment - Dr Deepak Agrawal
- Review of the Treatments for Central Neuropathic Pain
- Antidepressants, Other, Anticonvulsants, Analgesics, Nonsteroidal Anti-Inflammatory Drugs
- Evidence of a genetic background predisposing to complex regional pain syndrome type 1
How to Relieve Carpal Tunnel Pain Naturally
Are your fingers tingling? Do your wrists feel sore after a long day at work? If yes, you might be struggling with carpal tunnel syndrome. This condition causes a lot of discomfort and can affect your daily life. But here's the good news: you don’t always need surgery to feel better. There are natural ways to manage it from the comfort of your home.
In this blog, we will explore proven methods for carpal tunnel pain relief without surgery. You'll learn about easy lifestyle changes, home remedies, and more to help you heal naturally. So, let's begin your journey to pain-free wrists.
What is Carpal Tunnel Syndrome?
Carpal tunnel syndrome happens when the median nerve gets squeezed at the wrist. This nerve travels through a narrow space in your wrist called the carpal tunnel. When the tunnel gets tight, the nerve feels the pressure, leading to pain, tingling, and weakness in your hand.
What causes carpal tunnel syndrome in the first place?
The main reasons why people get this condition include:
- Repetitive hand movements like typing or assembly work
- Poor hand posture or bad wrist position
- Health problems like diabetes or arthritis
- Pregnancy-related fluid retention
According to the NIH and the American Academy of Orthopaedic Surgeons (AAOS), median nerve compression is the core issue behind carpal tunnel.
Who is most at risk for carpal tunnel pain?
Anyone can get it, but some people are more likely to suffer. This includes:
- Office workers who type all day
- Pregnant women
- Manual laborers using tools regularly
The Mayo Clinic reports that women are three times more likely than men to get carpal tunnel syndrome. It is also more common in people over 50.
Can You Relieve Carpal Tunnel Pain Without Surgery?
Not everyone needs surgery for carpal tunnel. Many people find good results with natural methods.
How effective are natural remedies compared to medical treatments?
Natural treatments can work very well, especially if the problem is caught early.
- The Cleveland Clinic says up to 50% of patients feel better with non-surgical care.
- Surgery may help severe cases, but natural care works for mild-to-moderate pain.
- Natural care has fewer side effects and costs less.
In short, you don’t always need surgery for carpal tunnel pain relief.
What are the Best Home Remedies for Carpal Tunnel Pain Relief?
Let’s look at what you can do at home to feel better fast.
Wrist splints ease carpal tunnel pain
If you're dealing with carpal tunnel syndrome, a wrist splint or brace can help. These devices keep your wrist in a neutral position. This reduces pressure on the median nerve, easing symptoms like tingling, numbness, and pain in your hand and fingers.
Wrist splints are great for nighttime use, when symptoms worsen. They prevent your wrist from bending, which can make things worse. During the day, they offer support and relief, especially if your job or activities involve repetitive hand or wrist movements.
A 2012 study showed that a wrist brace at night was better than no treatment for carpal tunnel symptoms. Braces are most helpful for mild to moderate cases. They lead to shorter symptom durations and reduce numbness, tingling, and burning.
Using wrist splints for carpal tunnel or braces may not show immediate results. It might take 3-4 weeks of consistent use to see lasting improvements.
Along with wrist splints or braces, try these strategies to manage carpal tunnel syndrome:
- Avoid extreme wrist positions
- Keep your hands warm
- Take regular breaks to rest your hands and wrists
- Vary your tasks to prevent repetitive motions
- Use a relaxed grip when possible
By adding wrist splints or braces to your treatment plan and making lifestyle changes, you can find relief. This helps prevent the progression of this common nerve condition.

User reviews often say wrist splints give great carpal tunnel pain relief while sleeping. They’re a popular wrist splint for pain.
Cold and warm compresses effective for pain relief
Heat therapy, like soaking in warm water or using a heating pad, boosts blood flow. This reduces inflammation and eases stiff muscles. It offers temporary relief and support for carpal tunnel symptoms. Cold therapy, such as an ice pack or cold compress, helps shrink swelling and dull pain.
Choosing between heat and cold depends on what works for you. Half of those with carpal tunnel find heat more helpful, while the other half prefer cold. You might need to try both to see which suits you better.
It's key to use heat and cold therapy correctly. Apply them for 15-20 minutes, then take a half-hour break. This approach maximizes their benefits without causing more discomfort.
Heat and cold therapy don't cure carpal tunnel syndrome on their own. They should be used with other treatments, like wrist exercises, anti-inflammatory drugs, or the Ovation Hand Technique. If your symptoms don't improve or get worse, see a doctor for a full treatment plan.
| Treatment Type | How to Use | Frequency |
|---|---|---|
| Cold Compress | 15 mins on wrist | 2-3 times daily |
| Warm Compress | 10-15 mins before exercises | Daily |
Use heat to relax and cold to reduce swelling. Physical therapists recommend alternating both for wrist pain treatment at home.
Best hand exercises and stretches for carpal tunnel
Hand exercises help stretch the nerves and tendons in your wrist.
- Flexor Stretch: Straighten your arm, palm up. Use your other hand to pull fingers back.
- Nerve Gliding: Curl your fingers into a fist, then open wide.
- Tendon Exercises: Touch each finger to the thumb, one at a time.
These carpal tunnel home exercises can improve blood flow. The American Academy of Neurology says to stop if pain increases.

While these lifestyle changes and home remedies can help with mild to moderate cases, more severe carpal tunnel syndrome may need medical treatment. If your symptoms don't get better or get worse, it's best to see a healthcare professional.
How Can Diet and Supplements Help Reduce Carpal Tunnel Symptoms?
Your diet affects inflammation in the body, which can impact nerve pain.
Can inflammation-reducing foods actually help?
Yes. Eating anti-inflammatory foods helps reduce inflammation in the wrist.
- Omega-3 rich foods: salmon, walnuts
- Spices: turmeric, ginger
- Fruits/vegetables: berries, spinach
- Vitamin B6 foods: bananas, avocados
A healthy diet can support natural treatment for carpal tunnel.
What supplements are linked to carpal tunnel pain relief?
Some natural supplements help the body fight swelling and nerve pressure.
| Supplement | Dosage | Benefit |
| Vitamin B6 | 50-100 mg/day | Nerve health |
| Magnesium | 300-400 mg/day | Muscle relaxation |
| Turmeric Extract | 500-1000 mg/day | Anti-inflammatory |
| Bromelain | 500 mg/day | Swelling reduction |
Always check with a doctor before starting any supplements.
These treatments may not cure carpal tunnel syndrome, but they can offer temporary relief. For severe or persistent cases, you might need medical help. This could include corticosteroid injections or surgery. If your pain doesn't get better or gets worse, talk to a healthcare professional for advice and care.
Complementary and Alternative Therapies
There are many therapies that can help with carpal tunnel syndrome (CTS) symptoms, besides traditional medicine. Yoga and stretching exercises, acupuncture and chiropractic care are some of these options. They offer a holistic way to deal with CTS.
Yoga and Stretching Exercises
Yoga, stretching, and strengthening exercises can help reduce pain and boost grip strength in people with CTS. These exercises are gentle and focus on specific areas. They help ease pressure on the median nerve, making hands and wrists more mobile.
Acupuncture and Chiropractic Care
Acupuncture and chiropractic care are also helpful for CTS relief. Acupuncture is known to lessen pain in many conditions, including CTS, injuries, and arthritis. Chiropractic care can also help by fixing any misalignments or restrictions in the wrist and hand.
Remember, these therapies should be used along with, not instead of, regular medical treatment. They can add to the benefits, but they shouldn't replace the care from a doctor for CTS.

Ergonomic Adjustments
Making your workspace more ergonomic can really help with carpal tunnel syndrome (CTS). Simple changes like adjusting the height and position of your keyboards and mice can ease wrist and hand pressure. This might even lessen CTS symptoms.
First, make sure your ergonomic keyboard is at the right height. This lets your wrists stay straight and your forearms parallel to the floor. Adding a wrist rest helps keep your hands in the right spot and cuts down on repetitive motions that harm the median nerve.
- Adjust the height of your ergonomic keyboard to keep your wrists straight and your forearms parallel to the floor.
- Use a wrist rest to support your hands and maintain proper positioning when typing.
- Position your ergonomic mouse close to your body, keeping your arm close to your side to reduce reaching and strain.
Good posture and hand placement also matter a lot. Keep your back straight, shoulders relaxed, and don't bend your wrists too much. These small changes can help prevent and ease CTS symptoms.

By adding these ergonomic changes to your daily routine, you can ease the pressure on your carpal tunnel. This might lower the risk of getting or making CTS worse. Always be proactive in making your workspace more ergonomic for your needs.
Over-the-Counter Medications
If you're dealing with carpal tunnel syndrome, over-the-counter (OTC) medications can help. These easy-to-get options can ease the pain, tingling, and numbness. Many people in the U.S. suffer from this condition.
Anti-Inflammatory Drugs for Carpal Tunnel
Drugs like ibuprofen (Advil) or naproxen (Aleve) can lessen inflammation and swelling around the median nerve. This nerve is often affected by carpal tunnel syndrome. By fighting inflammation, these drugs may ease symptoms.
Topical Pain Relievers for Carpal Tunnel
Topical pain relievers with menthol or capsaicin can also help. Apply them directly to your wrist and hand. They can ease pain without the need for pills.
While OTC options can help, they might not fix the root cause of carpal tunnel syndrome. It's key to use these with other treatments like wrist splints, physical therapy, or doctor's advice. This way, you can manage the condition better and for longer.

When to Seek Medical Treatment
If home remedies and lifestyle changes don't help with your carpal tunnel syndrome, you should see a doctor. Signs like numbness, tingling, or weakness in your hand and wrist mean you might need more help. A doctor can check how bad your condition is and suggest treatments like medicines, injections, or surgery for serious cases.
Carpal tunnel syndrome affects about 1-3 people per 1,000 in the U.S. each year. It's more common in women and people aged 40-60. If not treated, it can get worse and cause permanent nerve damage and hand problems. So, it's important to get medical help if your symptoms don't go away or get worse.
Doctors like neurologists, neurosurgeons, and orthopedic surgeons can help with carpal tunnel syndrome. They can suggest treatments such as:
- Prescription medicines to reduce inflammation and pain
- Corticosteroid injections to the affected area
- Surgical procedures, such as open release or endoscopic surgery, to relieve pressure on the median nerve
Getting diagnosed and treated early is crucial for managing carpal tunnel syndrome and preventing nerve damage. If your symptoms keep getting worse, don't wait to see a doctor. They can give you a full check-up and a treatment plan that's right for you.
Corticosteroid Injections
If lifestyle changes and over-the-counter meds don't help with carpal tunnel syndrome, your doctor might suggest corticosteroid injections. These injections go right into the carpal tunnel. They help reduce inflammation and swelling. This takes pressure off the median nerve and helps ease your symptoms.
Corticosteroid injections work better than taking oral steroids for carpal tunnel syndrome. They are usually for cases that don't get better with simpler treatments. Studies show these injections can ease symptoms for up to 6 months. They might also delay the need for surgery for up to a year.
But, it's key to know that these injections aren't without risks. Side effects could include more pain, skin color changes, weaker tendons, and nerve damage. Your doctor will weigh the benefits and risks before suggesting this treatment.
If your doctor thinks corticosteroid injections are best for you, following the right dosage and schedule is crucial. Getting too many injections can cause problems. So, it's important to work closely with your doctor to manage your treatment well.
Carpal Tunnel Surgery
If non-surgical treatments don't help with carpal tunnel syndrome, your doctor might suggest [https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/carpal-tunnel-release]carpal tunnel surgery[/a]. There are two main types: open surgery and endoscopic surgery.
Open Surgery vs. Endoscopic Surgery
Open surgery makes one cut in the palm to free the median nerve. Endoscopic surgery uses a small camera and tiny cuts for the same goal. Both methods work well, but endoscopic surgery might be less painful after.
About 500,000 carpal tunnel release surgeries happen each year in the U.S., says [https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/carpal-tunnel-release]statistics[/a]. Endoscopic surgery heals faster and hurts less than open surgery. The risk of infection or nerve damage is very low for both methods.
Recovery and Prevention
Recovery from carpal tunnel surgery takes weeks to months. It's key to avoid straining the wrist during this time. Follow your doctor's advice, like wearing a splint, taking pain meds, and using ice, for a smooth recovery.
To stop carpal tunnel syndrome from coming back, keep good posture and avoid repetitive tasks. Up to 33% of patients[/a] might still have numbness or pain after surgery. So, prevention is key.
Workplace Accommodations
If you're dealing with carpal tunnel syndrome, your workplace might need to make some changes. Adjusting your workstation, like the height of your keyboard and mouse, and using a wrist rest can help. Taking breaks to stretch your hands and wrists is also key.
Changing your job duties or tasks that involve repetitive motions can also be helpful. Carpal tunnel syndrome affects 7-16% of people, making it a common issue in offices. Talking to your employer about these changes can make your work safer and more comfortable for you.
Improving your workstation means setting the right desk, chair, and monitor heights for good posture. Keeping your wrists straight and using ergonomic keyboards and mice can prevent wrist strain. This can help ease carpal tunnel syndrome symptoms.
Consider using sit-stand workstations to help prevent and manage carpal tunnel syndrome. These setups encourage movement during your workday. Regular breaks, sitting straight, keeping your work in front of you, and doing wrist exercises can also lower your risk of carpal tunnel syndrome.
If these steps don't help, you may need professional treatment. This could include steroid injections or surgery in severe cases. Working with your employer and healthcare providers can help you find the right accommodations to manage your carpal tunnel syndrome and keep you productive at work.
Book a Consultation with Dr. Chandril Chugh Today
If you’re still dealing with wrist pain or numb fingers, don’t wait. Book a consultation with Dr. Chandril Chugh, a US-trained, board-certified neurologist. He has helped thousands of patients with carpal tunnel pain relief using smart, safe, and simple methods.
FAQ
What is carpal tunnel syndrome and what causes it?
Carpal tunnel syndrome (CTS) happens when the median nerve gets pinched in the wrist. This nerve runs from the forearm to the hand. It can get compressed by repetitive hand movements, wrist injuries, pregnancy, arthritis, and other conditions.
What are the symptoms of carpal tunnel syndrome?
Symptoms include numbness, tingling, weakness, and pain in the hand and fingers. These feelings are often worse at night or during repetitive tasks.
How common is carpal tunnel syndrome?
It affects 4 to 10 million people in the U.S. The condition can be mild or severe, impacting daily life if not treated.
What are some natural ways to relieve carpal tunnel pain?
To ease carpal tunnel pain, avoid repetitive hand movements and keep your wrist in the right position. Use wrist splints, apply heat or cold, and do gentle stretching exercises for your hands and wrists.
Can complementary therapies help with carpal tunnel syndrome?
Yes, therapies like yoga, acupuncture, and chiropractic care may help. Use them with, not instead of, regular medical treatment.
How can ergonomic adjustments help with carpal tunnel syndrome?
Ergonomic changes at work, like adjusting your keyboard and mouse, using a wrist rest, and maintaining good posture, can ease wrist and hand pressure. This might reduce CTS symptoms.
When should someone seek medical treatment for carpal tunnel syndrome?
If home remedies and changes don't help, seek medical help. Signs like persistent numbness, tingling, or weakness in the hand and wrist mean it's time for professional care.
What are the treatment options for more severe cases of carpal tunnel syndrome?
For severe cases, treatments include corticosteroid injections or surgery. Injections can reduce swelling, while surgery helps release pressure on the median nerve.
What workplace accommodations can help manage carpal tunnel syndrome?
Adjust your workstation, use a wrist rest, and stretch your hands and wrists regularly. Changing job tasks that involve repetitive motions can also help.
Source Links
- How Do I Know if I’m Getting Carpal Tunnel Syndrome?
- Carpal Tunnel Syndrome
- Help for your hands: Home remedies for carpal tunnel syndrome
- Current options for nonsurgical management of carpal tunnel syndrome
- Alternative medicine - pain relief: MedlinePlus Medical Encyclopedia
- Ergonomic positioning or equipment for treating carpal tunnel syndrome
- Preventing carpal tunnel syndrome: 7 methods to try
Natural and Easy Knee Pain Treatment At Home
Knee pain is a common issue that can often be managed at home. This article will show you natural and easy ways to ease your knee pain. Whether it's mild, moderate, or severe, you'll find ways to help yourself without seeing a doctor.
You'll learn about simple RICE (Rest, Ice, Compression, Elevation) methods and exercises. You'll also discover herbal treatments to help you move better and lessen pain at home.
Knee pain can come from many things like arthritis, overuse, injury, and lifestyle choices. By knowing what causes your pain and using the right methods, you can ease your discomfort and avoid more problems. Let's look at home remedies and strategies to help your knee pain and boost your joint health.
Assess Your Knee Pain
The first step in addressing knee pain at home is to assess the severity of your condition. Understanding the nature and extent of your knee discomfort can help you determine the most appropriate treatment approach.
Mild to Moderate Pain
If you have mild to moderate knee pain, it might be from a sprain, strain, or arthritis. Home remedies can help manage these symptoms. You might notice some swelling, tenderness, or difficulty moving.
In such cases, self-care like the RICE (Rest, Ice, Compression, Elevation) method can offer relief.
Severe or Persistent Pain
But, if the pain is severe or doesn't go away, you should see a doctor. Severe pain, visible deformity, or signs of infection like redness and warmth need professional help. Tests like X-rays, MRI, or CT scans might be needed to find out what's causing the pain.
Remember, seeing a healthcare professional is key if your knee pain is swollen, unstable, or makes moving hard. Getting the right assessment and treatment early can stop things from getting worse and help you recover faster.

It's important to talk to a healthcare professional, especially if your knee pain is swollen, unstable, or makes moving hard. Proper assessment and timely treatment can help prevent the condition from getting worse and ensure a speedy recovery.
Try RICE for Strains and Sprains
The RICE method is a great way to treat knee pain at home. It stands for Rest, Ice, Compression, and Elevation. It's especially good for knee strains and sprains. Start by resting the knee and avoiding hard activities.
Use ice packs on the knee for 15-20 minutes, several times a day. This helps reduce swelling and inflammation. Then, wrap the knee with a compression bandage for support. Elevate the leg above your heart level to lessen swelling.
Following the RICE method can help minor knee injuries heal faster.
Gabe Mirkin, MD, introduced the RICE method in 1978 for sports injuries. In 2015, he updated his advice. He said ice doesn't speed up healing, and too much rest can slow it down.
The RICE method is good for minor injuries like sprains, jammed fingers, and knee injuries. Use it for the first 1-3 days after an injury. If pain and swelling don't go away after 5-7 days, see a doctor.
- Apply ice for 15-20 minutes every 2-3 hours during the first 24-48 hours to reduce swelling.
- Wear appropriate shoes, take breaks, stretch, and stay in good condition to prevent knee injuries.
- NSAIDs and acetaminophen can be recommended along with RICE for pain management, with caution over prolonged use.
Don't use the RICE method for serious injuries like organ breaks, dislocated joints, or broken bones. It's a good way to treat managing knee joint injuries and reducing knee inflammation from knee sprains.

Tai Chi for Osteoarthritis
If you're one of the millions dealing with knee osteoarthritis, tai chi might be a solution. Tai chi has been shown to lessen pain and boost knee movement. It's a great way to handle the symptoms of this common issue.
Tai chi is all about slow, flowing movements, deep breathing, and meditation. It's a mind-body exercise that enhances balance, flexibility, and joint health. The American College of Rheumatology and Arthritis Foundation suggest tai chi for knee osteoarthritis.
A study at Texas Tech University found tai chi helped adults with knee osteoarthritis. They had less pain and better physical function after six weeks. Another study with 152 older adults saw moderate improvements in physical function after 12 weeks of tai chi and water exercises.
Tai chi aims to balance life energy ("qi") and aids in healing by restoring this balance. It leads to better balance, flexibility, and muscle strength. It's best to learn from an instructor to get the right posture and breathing. Classes are available in Arthritis Foundation chapters and fitness centers.
Looking for a natural way to ease your knee osteoarthritis? Try tai chi. This exercise improves knee flexibility and balance. It also offers pain relief and benefits for joint health.
Exercise for Knee Strength
Keeping your knee muscles strong and flexible is key to handling knee pain and boosting joint health. Adding low-impact activities and exercises that strengthen muscles can help ease pain and stop future issues.
Low-Impact Activities
Walking, cycling, swimming, and water aerobics are easy on the knees but still good for your heart. They help keep the joint moving and flexible without too much stress.
Muscle-Strengthening Exercises
Strengthening muscles around the knee, like the quadriceps, gives better support and less strain on the joint. Doing exercises like leg raises, step-ups, and controlled squats can build strength and stability.
It's smart to work with a physical therapist or healthcare provider to create an exercise plan that fits you. They can teach you the right way to do exercises safely and effectively.

Combining low-impact activities with muscle-strengthening exercises can make your knees more mobile, stable, and less painful.
Weight Management for Reduced Pressure
Carrying extra weight puts more pressure on your knee joints, making pain and inflammation worse. The Arthritis Foundation says extra weight can add 15-50 pounds of pressure on your knees. Losing weight through diet and exercise can ease the strain on your knee joints, especially if you have osteoarthritis.
Eating well and doing low-impact exercises can help you lose weight and lower the risk of more joint damage and pain. Here are some tips:
- Try losing weight slowly, about 2 pounds a month, for better knee function and less inflammation.
- Add activities like walking, cycling, water exercises, and strength training to your routine.
- Use a walking aid like a crutch or cane to ease the stress on your knee during everyday tasks.
Even small weight changes can greatly reduce knee joint pressure and help with osteoarthritis. Focusing on weight management is a big step towards easing knee pain and improving your life quality.
Heat and Cold Therapy
Using both heat and cold can help ease knee pain at home. Heat and cold therapies have different benefits for knee health. They help with mobility and reduce swelling.
Applying Heat
Heat, like a heating pad or warm bath, relaxes muscles and boosts circulation. It makes joints more flexible. This is great for chronic knee issues like osteoarthritis. Heat also helps with muscle pain, spasms, and stiffness.
Apply heat for up to 20 minutes, several times a day. This brings more blood, oxygen, and nutrients to the knee. It helps with healing and eases pain. But, be careful not to touch your skin directly with extreme heat to avoid burns.
Applying Cold
Cold therapy, such as ice packs or cold compresses, reduces swelling and inflammation. It's good for sudden knee injuries like sprains or strains. Cold slows blood flow to lessen pain and prevent more damage.
Use cold packs for 20 minutes, several times a day, in the first 48 hours after an injury. You can use a bag of frozen peas, ice in a towel, or cold gel packs. Just don't put ice directly on your skin to avoid frostbite.
Mixing heat and cold therapy, or contrast therapy, is good for chronic conditions like arthritis. It alternates heat and cold to improve flexibility, motion, and lessen pain.
If knee pain gets worse, with more swelling, instability, or after an injury, see a healthcare professional. They can offer personalized advice and help heal your knee faster.
Herbal Ointments and Salves
Some herbal ointments and salves can help with knee pain. A study showed a salve with cinnamon, ginger, mastic, and sesame oil worked as well as over-the-counter creams. Herbs like willow bark, which has compounds like aspirin, may also help with anti-inflammatory properties. These topical ointments for knee relief could be useful for managing knee pain.
But, always talk to a healthcare provider before trying herbal remedies for knee pain. Some herbs might not mix well with your medicines or could have bad effects. Always be careful and listen to your doctor when using natural anti-inflammatory treatments.
- A 2019 review noted that boswellic acid appears to have anti-inflammatory effects that could help people with RA, bronchial asthma, ulcerative colitis, and other inflammatory diseases.
- A small, older study from 2002 showed that cat's claw was effective in reducing joint swelling by over 50% in 40 people with RA.
- Researchers have found evidence that extracts or specific components of green tea may affect arthritis, but more research is needed to determine the most effective form and dose.
Be careful with ginger, as it can affect some medicines like warfarin (Coumadin), a blood thinner. Also, the FDA doesn't check natural remedies like thunder god vine, and the wrong part can be toxic.
Before trying herbal remedies for arthritis, talk to a doctor. Some options might not work well with your current medicines. With a doctor's advice, herbal ointments and salves can be a great part of your knee pain plan.
Ginger Extract for Pain Relief
If you're dealing with knee pain, ginger might help. It has natural anti-inflammatory properties. Studies show ginger extract can ease knee osteoarthritis symptoms.
In a study with 67 people with osteoarthritis, ginger and ibuprofen reduced pain more than a placebo. Another trial with 29 people found ginger lowered pain and disability from the disease more than a placebo.
Ginger is a good option for those looking for natural pain relief. You can take it as supplements, tea, or add it to food. Studies suggest taking 510–1,000 mg of ginger daily for musculoskeletal issues.
More research is needed, but ginger's anti-inflammatory effects look promising for ginger for knee pain and supplemental treatments for knee osteoarthritis. Adding ginger to your treatment plan might help ease knee osteoarthritis symptoms. It's a natural way to fight inflammation.
Knee Pain Treatment At Home
There are many home remedies and natural solutions for knee pain. These go beyond what we've talked about already. Trying a few more techniques might help you feel better.
Keeping a good posture and using things like knee braces or crutches can ease the stress on your knees. Massaging your thigh muscles can also help. It relaxes the muscles and boosts blood flow in the area.
Adding an Epsom salt bath to your routine might also help. The magnesium in the salts can relax your muscles and lessen inflammation. This could make your knee pain better.
If your knee pain doesn't get better or gets worse, see a healthcare professional. They can give you advice tailored to your needs and check if you need more treatment.
Using natural ways to ease knee pain and taking good care of yourself can help a lot. Always pay attention to your body. And don't wait to get help from a professional if the pain is too much.
Posture and Knee Support
Keeping the right posture for knee health and using supports can help ease knee pain. Don't sit in low chairs or couches that make you sink in. This can strain your knees. Use a pillow or a raised surface to keep your knees at a comfy level when sitting.
Wearing shoes with good arch support can also ease pressure on the knee joints. If needed, consider knee braces or sleeves for extra stability and protection. These can lessen stress on your knees, especially during activities that might strain them.
Avoid activities that put too much strain on your knees, like high-impact exercises or standing or sitting for too long. Choose low-impact activities like walking, swimming, or cycling to stay fit without making your knee pain worse.
By keeping good posture, using supports, and being careful with your activities, you can help manage and maybe even lessen your knee pain. Remember, fixing the main cause is crucial for lasting relief.
Dietary Measures and Weight Loss
Your diet and weight management are key to easing knee pain, especially with osteoarthritis. Carrying extra weight puts more pressure on your knee joints, making pain and inflammation worse. To help your joints, the Arthritis Foundation suggests a Mediterranean-style diet. This diet is full of fruits, veggies, whole grains, and healthy fats.
Mediterranean Diet
This diet is balanced and fights inflammation. It helps you keep a healthy weight and gives your joints the nutrients they need. Losing weight with diet and exercise can also ease the load on your knees and lessen pain.
- People who eat fish high in omega-3s are less likely to get rheumatoid arthritis.
- Eating a 3-to-6 ounce serving of fish at least four times a week can cut down on osteoarthritis inflammation and protect your heart.
- Low-fat dairy products can be good for people with osteoarthritis of the knee.
- Studies show that people with osteoarthritis might have high cholesterol levels.
Eating a balanced diet with proteins from nuts, beans, eggs, lean meats, and fish helps your knee health. Add lots of fresh veggies, fruits, and whole grains to your meals. Mix this with walking or swimming for cardio and resistance exercises to strengthen your knee muscles. This approach can greatly improve your diet and knee pain management.
Medications for Pain Management
Home remedies can help with knee pain, but there are also medications that can offer relief. Over-the-counter NSAIDs like ibuprofen or naproxen can lessen inflammation and ease pain. Sometimes, doctors may suggest stronger options, such as topical treatments, steroid injections, or antidepressants like duloxetine, for chronic pain.
Always talk to a doctor before starting any new medication. This ensures safety and addresses the root cause of the pain. Misusing over-the-counter or prescription drugs can cause bad side effects. With a healthcare professional's guidance, you can find the best over-the-counter medications for knee pain or prescription treatments for knee osteoarthritis to manage your pain.
Your doctor might suggest a mix of treatments, including physical therapy, weight management, and alternative therapies. The aim is to find the best way to manage knee discomfort with medication. This helps you move better and improve your quality of life.
Massage for Muscle Relaxation
Massage is a great way to ease knee pain by relaxing muscles and boosting blood flow. The American Massage Therapy Association suggests self-massage techniques for knee pain relief. These methods can help those struggling with knee issues.
One effective technique is to tap the thigh muscle above the knee, then slide your hand down to the knee. Gently pressing on the knee can also ease tension and enhance blood flow. These steps are great for easing knee stiffness and pain.
Massage isn't a top choice for treating osteoarthritis, but it has many benefits. It can help manage stress, which is key for knee pain. Using essential oils like peppermint or eucalyptus during massage can make the experience even better.
Being consistent with massage is important for easing knee pain. Adding these techniques to your daily routine can help relax muscles and improve blood flow. This can lead to less pain over time.
Aromatherapy with Essential Oils
If you're looking for natural ways to ease your knee pain, consider aromatherapy with essential oils. These oils contain aromatic compounds that might help with pain and inflammation in your knees.
Studies show that a mix of cinnamon, ginger, mastic, and sesame oil can ease pain and improve stiffness. The oils' natural anti-inflammatory properties, like those found in ginger and orange, could be why.
Essential oils like lavender, eucalyptus, and lemongrass might also help with knee pain. For example, people with rheumatoid arthritis felt some pain relief after using lemongrass oil for a month. This is thanks to citral, a key component in lemongrass oil.
While more studies are needed, aromatherapy could be a good addition to home remedies for knee pain. Trying different essential oil blends or ways to apply them might help you find what works best for you.
Remember, use high-quality essential oils and mix them with a carrier oil before skin application. Always test a small area first to avoid skin reactions. With their natural anti-inflammatory properties, essential oils could be a soothing way to manage knee pain at home.
Conclusion
Knee pain can be a big problem, but you can tackle it with comprehensive home remedies for knee pain. These natural methods can help ease the pain and boost your knee health. Techniques like the RICE method, Tai Chi, and strengthening exercises are great starts.
Managing your weight and using heat or cold therapy can also help. Plus, herbal remedies offer another option. These methods can help you handle natural treatments for knee discomfort and keep your joints moving well.
If your knee pain doesn't get better or gets worse, see a healthcare provider. But for many, the home remedies for knee pain mentioned here can really help. By changing your lifestyle and trying natural remedies, you can improve knee health without medical intervention. This can make your life better overall.
Being patient and balanced in your approach is crucial for lasting relief from knee pain. With the right strategies and a focus on your health, you can get your mobility back. And you can live a more active, pain-free life.
FAQ
What are some effective home remedies for knee pain?
For knee pain, try the RICE method (Rest, Ice, Compression, Elevation). Also, practice Tai Chi, do strengthening exercises, keep a healthy weight, use heat and cold therapy, and consider herbal remedies like ginger.
How can I assess the severity of my knee pain?
If your knee pain is mild to moderate, home remedies might help. This includes pain from sprains, strains, or arthritis. But, if the pain is severe or doesn't go away, see a doctor for a full check-up.
What is the RICE method and how does it help with knee pain?
The RICE method stands for Rest, Ice, Compression, and Elevation. It's great for treating knee strains and sprains. It cuts down swelling, reduces inflammation, and helps the knee heal.
How can Tai Chi help with knee osteoarthritis?
Tai Chi is a slow, flowing exercise. It has been shown to lessen pain and increase movement in the knee for people with osteoarthritis.
What types of exercises are recommended for knee pain?
Try low-impact activities like walking, cycling, swimming, and water aerobics. These can make the joint more mobile without putting too much stress on the knees. Also, strengthening the quadriceps can give better support and ease the knee's burden.
How does weight management affect knee pain?
Carrying extra weight puts more pressure on the knee joints, making pain and inflammation worse. Losing weight through diet and more exercise can help ease the strain on the knees.
When should I use heat or cold therapy for knee pain?
Heat therapy can relax muscles and boost circulation. Cold therapy reduces swelling and inflammation. Use heat for up to 20 minutes, and cold packs for 20 minutes several times a day, especially in the first 48 hours after an injury.
Can herbal remedies and essential oils help with knee pain?
Yes, some herbal remedies and essential oils may help with knee pain. For example, topical ointments with cinnamon, ginger, and essential oils might have anti-inflammatory effects. But, always talk to a healthcare provider before trying these treatments.
How can ginger help with knee pain?
Ginger extract has anti-inflammatory properties. It might help manage knee osteoarthritis symptoms when used with other treatments.
What other home-based treatments can I try for knee pain?
For knee pain, also try good posture, supportive devices like braces or crutches, massage, and Epsom salt baths. These can help relax muscles and reduce inflammation.
Source Links
- Home remedies for knee pain: Best Remedies are Shared Here
- Need Knee Pain Relief? Here's 7 Natural Home Remedies to Use
- Knee pain - Diagnosis and treatment - Mayo Clinic
- An Overview of Knee Pain
5 Effective Strategies for Sleep Maintenance Insomnia Relief
Insomnia is a common sleep issue that makes it hard to fall asleep or stay asleep. If you're having trouble staying asleep, it's important to get help. The right treatment can improve your sleep quality and overall health. This article will cover five effective strategies to help you sleep better and wake up refreshed.
Good sleep is key for your health and mind. With the right techniques, you can take back control of your sleep. Let's explore the best ways to fight sleep maintenance insomnia.
Understanding Sleep Maintenance Insomnia
Sleep maintenance insomnia makes it hard to stay asleep all night. People with this issue might fall asleep but wake up a lot, feeling tired the next day. It's important to know what it is, its symptoms, causes, and risk factors to manage it well.
Definition and Symptoms
Sleep maintenance insomnia means you can't stay asleep. You might wake up a lot at night. It's hard to fall asleep again, making your night sleep broken and not restful. The main signs of this insomnia include:
- Waking up multiple times during the night
- Difficulty falling back asleep after waking up
- Daytime sleepiness or fatigue
- Irritability or difficulty concentrating
Causes and Risk Factors
Many things can lead to sleep maintenance insomnia. Some common causes and risk factors are:
- Stress and Anxiety: Stress or anxiety can mess with your sleep cycle, making it hard to stay asleep.
- Irregular Sleep Schedules: Not having a regular sleep schedule can disrupt your body's natural sleep rhythm.
- Medical Conditions: Health issues like sleep apnea, chronic pain, or GERD can affect your sleep.
- Lifestyle Factors: Things like caffeine, too much alcohol, and sitting too much can also cause sleep problems.
Knowing what causes and risks sleep maintenance insomnia helps in finding ways to fix it.

Establishing Good Sleep Hygiene
Getting quality sleep is key for your health and happiness. To fight sleep maintenance insomnia, focus on good sleep hygiene. This means making your bedroom sleep-friendly and sticking to a regular sleep schedule.
Creating a Sleep-Conducive Environment
Your bedroom's setup affects how well you sleep. Here's how to make it better:
- Keep your room dark, especially from blue light from devices, to help your body produce melatonin.
- Keep the room cool, between 60 and 67°F (15.6 and 19.4°C), for the best sleep.
- Make sure it's quiet to avoid sleep disruptions.
- Choose a comfy mattress and bedding for your body's support and relaxation.
Developing a Consistent Sleep Routine
Creating a regular sleep pattern is also key. Here are some tips:
- Go to bed and wake up at the same time every day, even on weekends, to keep your body's rhythm.
- Avoid napping to help your nighttime sleep.
- Do relaxing activities, like reading or stretching, 30-60 minutes before bed to signal bedtime.
- Limit caffeine and alcohol to improve sleep quality.
By making your bedroom sleep-friendly and sticking to a routine, you can fight sleep maintenance insomnia and better your sleep.

Exercise for Better Sleep
If you're having trouble sleeping, exercise could help. Studies say moderate cardio exercises are best for sleep. Adding simple stretches and deep breathing before bed can also help.
Weight lifting can reduce anxiety and depression, which helps with sleep. Yoga is especially good for improving sleep for certain groups, like older adults, women with sleep problems, and people with type 2 diabetes.
It's important to exercise at the right time. Stop aerobic exercise 1 to 2 hours before bed to help your brain relax. Try to exercise for at least 30 minutes a day. You might see better sleep in just four weeks.
There's a link between sleep and exercise. Good sleep makes you more energetic for workouts, and exercise helps you sleep better. Adding exercise to your daily routine can lead to better sleep.
Relaxation Techniques for Sleep Maintenance Insomnia
If you're having trouble sleeping, adding relaxation techniques to your day can really help. Mindfulness meditation and yoga are great for reducing stress and anxiety. These are big reasons why people can't sleep well.
Mindfulness Meditation
Mindfulness meditation means focusing on your breath and the now. It helps you stop thinking about stressful things. This makes it easier to relax and sleep better.
Studies show that doing this regularly can make your sleep much better. It's a great way to fight sleep problems.
Yoga and Deep Breathing
Yoga and deep breathing are also good for sleep. They make your body and mind calm. This helps you sleep better.
These activities start your body's relaxation response. They slow down your heart and breathing. This leads to better sleep.
Using these relaxation methods daily can really help with sleep issues. Taking time to relax and reduce stress sets you up for a good night's sleep.
Dietary Changes to Combat Insomnia
What you eat and drink affects your sleep quality. To fight insomnia, cut down on caffeine and alcohol. Add sleep-promoting foods and nutrients to your diet.
Limiting Caffeine and Alcohol
Caffeine keeps you awake, so avoid it in the afternoon and evening. Alcohol might make you sleepy at first but can disrupt your sleep later, making it poor quality.
Incorporating Sleep-Promoting Foods
Some foods can help you sleep better. Foods rich in melatonin, like tart cherries, and those with magnesium, such as leafy greens and nuts, can improve sleep.
By changing your diet and adding sleep-promoting foods, you can improve your sleep and overall health.

Sleep Maintenance Insomnia and Cognitive Behavioral Therapy
If you're not finding relief with lifestyle changes and home remedies, cognitive behavioral therapy (CBT) might help. CBT is a powerful, long-term treatment that changes your thoughts and behaviors to improve sleep. It teaches you how to sleep better and manage insomnia.
CBT-I is great for both short-term and long-term insomnia. Most people who try it see better sleep and quality of life. The treatment usually takes 6-8 sessions, but it depends on your needs. However, finding a therapist skilled in sleep medicine can be hard in the U.S.
In CBT-I, therapists work on changing negative thoughts and beliefs about sleep. They teach you techniques like stimulus control and relaxation to help you sleep better. These methods aim to reduce stress and anxiety related to insomnia.
About 70% to 80% of people with primary insomnia get better with CBT-I. For those with sleep maintenance insomnia, the success rate can hit 80%. If you're dealing with ongoing insomnia, talk to a healthcare provider about cognitive behavioral therapy for insomnia.

Light Regulation for Better Sleep
Getting enough sleep is key to feeling good, and managing your light exposure helps a lot. It's important to avoid blue light since it can mess with your body clock and lower melatonin levels.
Avoiding Blue Light Exposure
Devices like smartphones, tablets, and computers give off blue light. This light can make your brain think it's still day, making sleep hard. To help, cut down on blue light before bed.
Creating a Dark Sleep Environment
It's not just about avoiding blue light; a dark room is also key for good sleep. Any light, from screens or streetlights, can mess with your sleep cycle. Use blackout curtains, an eye mask, or a sleep mask to keep your room dark.
By managing your light and making your bedroom sleep-friendly, you can sleep better and keep your body's clock in check. This boosts your health and happiness.

Natural Sleep Aids and Supplements
If you're having trouble sleeping, natural sleep aids and supplements might help. Melatonin, a hormone your body makes, can make sleep better and help you fall asleep quicker. Herbal remedies like valerian, chamomile, and lavender can calm your mind and body, leading to better sleep.
Melatonin
Melatonin supplements, usually 3-10 mg, can make daytime sleep better and longer. This hormone helps control your sleep cycle, making it easier to fall and stay asleep.
Herbal Remedies
Herbs like valerian, chamomile, and lavender have been used for centuries to help sleep. Valerian root, 300-600 mg, can improve sleep quality and help with sleep disorders. Lavender aromatherapy also helps sleep, especially for older adults with dementia or heart disease.
Always talk to a healthcare professional before trying new sleep supplements. They might not mix well with your medicines or have side effects. By trying natural remedies and changing your lifestyle, you can find ways to improve your sleep.
Managing Stress and Anxiety
Stress and anxiety can really mess with your sleep. Using good stress management methods can help. Try being mindful, doing relaxing things, and talking to people you care about to handle stress and anxiety.
Mindfulness meditation is great for easing stress and helping you sleep better. It means focusing on now and letting go of worries. This can calm your mind and body, making it easier to sleep well.
Yoga and deep breathing are also good ways to reduce anxiety. They can slow down your heart rate, relax your muscles, and make you feel calm. This can lead to better sleep.
If stress and anxiety are really affecting your sleep, think about trying insomnia treatment like cognitive-behavioral therapy (CBT). CBT can help you change negative thoughts and behaviors that hurt your sleep.
Handling stress and anxiety is key to getting better sleep. By adding stress-reducing activities to your daily life, you can stop insomnia and sleep more peacefully.
Sleep Tracking and Monitoring
Tracking and monitoring your sleep can give you key insights into your habits. It helps you find out what affects your sleep. You can use devices, apps, or a simple diary to track your sleep.
Sleep tracking devices come in many types, like watches, bracelets, and mattress sensors. They track your heart rate, breathing, and more. This info helps you see how you sleep and what you can do better.
Remember, sleep trackers aren't a replacement for doctor's advice. They're especially not for people with sleep problems like sleep apnea or chronic insomnia. For accurate sleep quality info, talk to a doctor and get a sleep study.
Unlocking the Power of Sleep Tracking
- Identify patterns in your sleep habits and quality
- Understand the impact of environmental factors on your sleep
- Recognize potential triggers for sleep maintenance insomnia
- Collaborate with your healthcare provider to address sleep-related issues
If you're having trouble sleeping or want to sleep better, try tracking your sleep. It can be a big help. By understanding your sleep, you can make changes to sleep better and feel better overall.
When to Seek Professional Help
If you're still struggling with sleep after trying home remedies and lifestyle changes, it's time to get help. A healthcare provider or sleep specialist can check for health issues and create a plan just for you. They can help with sleep disorders.
Cognitive behavioral therapy (CBT) works as well or better than sleep medicines. Also, don't use sleeping pills for more than a few weeks because they can make you feel groggy during the day and increase the risk of falling.
Exercise can help you sleep better, but taking naps might make it harder to sleep at night. Also, avoiding insomnia treatment substances like caffeine, alcohol, and nicotine can also improve your sleep.
If yoga, tai chi, or supplements like melatonin and valerian don't help, see a sleep specialist. They can check your condition and suggest the right treatment.
Mental health care can also help improve sleep by focusing on mental health and well-being. With a professional's help, you can find out what's causing your sleep disorders and get back to sleeping well.
Sleep Maintenance Insomnia in Special Populations
Sleep maintenance insomnia can be tough for people during pregnancy and after having a baby. Hormones, physical discomfort, and stress from caring for a newborn can lead to insomnia during pregnancy and postpartum insomnia. It's key for these folks to work with their doctors to find safe ways to better their sleep quality.
Pregnancy and Postpartum
Pregnant women often see big changes in their sleep. The first three months can make them feel very tired and sleepy during the day. Later on, they might find it hard to fall asleep and stay asleep. After the baby arrives, new moms might have trouble sleeping because of the baby's needs.
Older Adults
As we get older, our sleep patterns and quality change. Older people might find it harder to sleep well. This can be due to health issues, medicines, or age-related sleep changes. Helping older adults with insomnia might mean making lifestyle changes, therapy, and possibly medication.
Conclusion
Sleep maintenance insomnia can really affect your health and happiness. By using the five tips we talked about, you can fight this sleep issue. These tips include good sleep habits, exercise, relaxing, eating right, and getting help when you need it.
Remember, many older adults, up to 75%, deal with sleep maintenance insomnia. Knowing what causes it and how to improve your sleep can help you take charge. This way, you can enjoy the benefits of good sleep.
If your insomnia doesn't go away or worries about your health grow, don't hesitate to get help. With the right advice and support, you can beat sleep maintenance insomnia. This will help you get the restful sleep you need.
FAQ
What is sleep maintenance insomnia?
Sleep maintenance insomnia means you can't stay asleep all night. You might fall asleep but wake up a lot. This makes you feel tired and worn out during the day.
What are the causes and risk factors for sleep maintenance insomnia?
Stress, anxiety, and depression are common causes. So are uncomfortable sleeping conditions and irregular sleep patterns. Using drugs or alcohol and having sleep apnea can also disrupt your sleep. Changes in your body's natural sleep cycle can lead to insomnia.
How can I establish good sleep hygiene to improve sleep maintenance?
Make your bedroom sleep-friendly by keeping it dark, cool, and quiet. Stick to a regular sleep schedule. This helps improve your sleep.
How can exercise help with sleep maintenance insomnia?
Exercise during the day can make your sleep better. But don't work out too close to bedtime. Exercise can make it hard to fall asleep.
What relaxation techniques can I use to improve sleep maintenance?
Try mindfulness meditation, yoga, and deep breathing exercises. These can reduce stress and anxiety, helping you sleep better. They make it easier to relax and fall asleep.
How can dietary changes affect sleep maintenance insomnia?
Avoid caffeine and alcohol, which can mess with your sleep. Eating foods that help sleep, like those with melatonin and magnesium, can improve your sleep quality.
What is the role of cognitive behavioral therapy (CBT) in treating sleep maintenance insomnia?
Cognitive behavioral therapy (CBT) is a great long-term solution for insomnia. It changes your thoughts and behaviors that affect your sleep. You'll learn healthy sleep habits and ways to cope with insomnia.
How can light regulation help with sleep maintenance insomnia?
Managing light exposure, like avoiding blue light from screens, is key. A dark sleep area also helps you sleep better.
Are there any natural sleep aids or supplements that can help with sleep maintenance insomnia?
Yes, natural sleep aids like melatonin and herbal remedies can help. But talk to a doctor before trying new supplements.
How can I manage stress and anxiety to improve sleep maintenance?
Use stress management techniques like mindfulness and relaxation. Doing things you enjoy and getting support from friends and family can also help.
Source Links
- Remedies for Insomnia
- 8 Insomnia Home Remedies: Exercises, Oils, and More
- 3 Steps for Managing Sleep Maintenance Insomnia
- What Are the Different Types of Insomnia?
How an Apnea Mouthpiece Can Help You Sleep Better
If you have trouble sleeping because of obstructive sleep apnea (OSA), an apnea mouthpiece might be the answer. These devices move your jaw and tongue to keep your airway open. This helps stop episodes of blocked airways, waking up, and falling asleep again.
Using an apnea mouthpiece can make your sleep better, reduce snoring, and make sure your organs get enough oxygen.
Oral appliance therapy is a good option for those who don't want surgery or don't like CPAP machines. These devices fit your mouth perfectly and come in different types. Some move your jaw forward, while others keep your tongue in place.
With the right apnea mouthpiece, you can control your obstructive sleep apnea. This means you can sleep better and more peacefully.
What is an Apnea Mouthpiece?
Oral appliances for sleep apnea are special devices you wear in your mouth at night. They help keep your airway open and improve airflow. This can help manage obstructive sleep apnea (OSA).
Types of Apnea Mouthpieces
There are two main types of devices for treating OSA:
- Mandibular Advancement Devices (MADs): These devices gently move your lower jaw forward. This opens up your airway for better breathing.
- Tongue-Stabilizing Devices (TSDs): These devices use suction to keep your tongue in a forward position. This stops it from blocking your airway while you sleep.
Mandibular advancement devices and tongue-stabilizing devices are effective for mild to moderate sleep apnea. Custom-made devices work better than over-the-counter ones for obstructive sleep apnea.
Mandibular Advancement Devices (MADs)
Mandibular advancement devices (MADs) are a common way to treat sleep apnea. They move your lower jaw forward, which helps keep your airway open at night. This makes it easier to breathe while you sleep.
These devices have two parts that fit over your teeth. They are connected with screws or rubber bands. This lets you adjust how far your jaw moves forward. Moving your jaw helps keep your airway open, reducing sleep apnea symptoms.
- MADs can make you feel more awake during the day, reduce snoring, lower blood pressure, and improve your life quality, just like CPAP therapy.
- They work best for people with mild to moderate sleep apnea, especially the young, side sleepers, women, and those with a receding jaw.
- However, MADs might not work as well for older adults, the obese, those with stiff jaws, people with dental issues, or those with central sleep apnea.
MADs are not as effective as CPAP in stopping breathing pauses or improving oxygen levels. But they are more comfortable and easy to carry around. Custom MADs made by a dentist usually work better than ones you can buy over the counter. They are made just for you.

Working with your healthcare provider is key when using MAD therapy. They can help you choose the right device and check how well it's working. With the right treatment, MADs can help manage your sleep apnea and improve your health.
Tongue-Stabilizing Devices (TSDs)
Tongue-stabilizing devices (TSDs) are another way to help with obstructive sleep apnea (OSA). They don't move your jaw forward like some other devices do. Instead, they use suction to gently pull your tongue forward. This keeps your airway open and helps you breathe better.
These devices might be good for people who can't use MADs because of weak teeth or jaw issues. They help stop your tongue from blocking your airway, which is a common cause of OSA. This can make sleeping much better.
Some popular TSD models include the AveoTSD and Good Morning Snore Solution devices. It's important to get these devices fitted by a doctor to make sure they work well and are comfortable.
Even though they're not as common as MADs, TSDs can be a good choice for some people with OSA. But they might not work for everyone. For example, they're not good for people who can't stick their tongue out, have central sleep apnea, or are kids. It's important to use, clean, and take care of these devices to make sure they work right.
If CPAP therapy doesn't work or isn't comfortable, trying a tongue-stabilizing device might be an option. Always talk to a healthcare provider before trying one to see if it's right for you.
How Effective are Apnea Mouthpieces?
Oral appliances, like apnea mouthpieces, can be a great solution for treating obstructive sleep apnea (OSA). They might not work as well as continuous positive airway pressure (CPAP) therapy. Yet, they can still make your sleep better and boost your health.
Compared to CPAP Therapy
Studies show that MADs, a type of oral appliance, can cut down on breathing pauses and increase oxygen levels while you sleep. But CPAP therapy is still better at these important tasks.
On the other hand, oral appliances can be as good as CPAP in making you feel less sleepy during the day, reducing snoring, and lowering blood pressure. They might also help with symptoms of depression and make life better overall.
One big plus of oral appliances is how comfortable and easy they are to use compared to CPAP. This makes them more likely to be used every night, which is key for treating sleep apnea.

To wrap it up, CPAP therapy is the top choice for treating serious OSA. But for those with mild to moderate sleep apnea who want something easier to use, oral appliances are a great option.
Apnea Mouthpiece Benefits
If you're having trouble with obstructive sleep apnea, an apnea mouthpiece could help. These devices are made to boost your sleep quality and health by tackling the root causes of your sleep apnea.
Using an apnea mouthpiece can cut down the number of times you stop breathing or breathe shallowly at night. It keeps your airway open. This leads to better blood oxygen levels, which means you'll sleep more soundly and feel less tired during the day.
- Decreases snoring frequency and volume
- Enhances quality of life and decreases daytime sleepiness
- Improves diastolic and systolic blood pressure over time
Apnea mouthpieces also help reduce snoring. This means better sleep for you and your partner. It's a win-win situation.

Studies have found that these devices can make your blood pressure better over time. This is great news for people with sleep apnea, as it lowers the risk of heart problems.
The benefits of using an apnea mouthpiece are many. They improve sleep quality, cut down on daytime tiredness, and boost overall health. They're a simpler and more effective option compared to CPAP therapy.
Who Can Use an Apnea Mouthpiece?
An apnea mouthpiece, or oral appliance, is great for people with mild to moderate sleep apnea (OSA). It's for those who can't use or don't like CPAP therapy. These devices move the lower jaw forward to keep the airway open while sleeping.
They are more comfy and easy to carry than CPAP machines. That's why many people choose them. But, they're not for everyone. They don't work for kids, people with severe OSA, or those with dental issues that make them hard to fit.
Sometimes, an apnea mouthpiece is used with CPAP therapy. This is helpful when you're traveling or don't have your CPAP machine. It makes breathing easier and more comfortable.
Always talk to a healthcare expert, like a sleep specialist or dentist, to see if an apnea mouthpiece is right for you. They can check your condition, give you a proper diagnosis, and help with fitting and adjusting the device for the best results.

The success of an apnea mouthpiece can differ for each person. You might need regular checks and adjustments for the best results. With the help of a qualified healthcare provider, you can find the best treatment to improve your sleep and health.
Getting an Apnea Mouthpiece
If you're having trouble with obstructive sleep apnea (OSA), an apnea mouthpiece might be a good option. It's a comfy and effective choice compared to traditional CPAP therapy. First, you need a diagnosis and fitting from a qualified dentist.
Diagnosis and Fitting
To start, you'll go through a sleep study. This can be done in a sleep lab or at home. It measures your breathing, oxygen levels, and other sleep metrics to confirm OSA.
After confirming OSA, your doctor will talk about treatment options. Oral appliance therapy might be suggested. If so, you'll see a dentist who specializes in sleep apnea.
The dentist will check your mouth and jaw. They'll make a custom-fit mouthpiece for you. This ensures it fits well and works effectively, which is key for success with your apnea mouthpiece.
The steps to get an apnea mouthpiece vary, but your healthcare team will guide you. They'll help you find the right solution for better sleep and health.

It's important to keep your mouthpiece clean and follow your dentist's care instructions. With the right treatment and a well-fitting device, you can improve your sleep and health.
Adjusting and Monitoring Your Apnea Mouthpiece
After getting your custom apnea mouthpiece, your dentist will want you to wear it every night. You'll also need to visit them regularly to check on your progress. Over time, your dentist will tweak the device to make sure it fits just right and helps open your airway.
Your doctor might suggest another sleep study after adjusting the mouthpiece to see if it's working well for your sleep apnea symptoms. It's important to keep up with regular visits to your dental and medical teams. This helps make sure your apnea mouthpiece treatment keeps working well over time.
Here are some tips for adjusting and monitoring your apnea mouthpiece:
- Wear the mouthpiece every night, even if it feels odd at first.
- Get used to wearing it during the day too.
- Breathe through your nose with the mouthpiece on to help adjust.
- Talk to your dentist if you keep having problems like gagging, it falling out, or discomfort after three weeks.
- Go to all follow-up appointments for any needed changes to your mouthpiece.
- Have a repeat sleep study as advised to make sure the mouthpiece is doing its job.
Getting your apnea mouthpiece adjusted and checked regularly is crucial for good sleep health.

Side Effects and Risks
Apnea mouthpieces can help manage snoring and sleep apnea, but they have side effects and risks. It's key to know these before choosing an apnea mouthpiece.
Common side effects include teeth discomfort, jaw joint pain, dry mouth, and too much saliva. These issues are usually mild and go away after a few weeks.
- Gum irritation and teeth grinding can happen with long-term use of an apnea mouthpiece.
- Changes to bite and tooth alignment might be seen if the mouthpiece doesn't fit right.
Working closely with your dentist is key to fix any problems and adjust your apnea mouthpiece. Serious risks like worse sleep apnea symptoms are rare but can happen if the device doesn't fit or isn't used right.
The side effects of apnea mouthpieces and risks of using an apnea mouthpiece are mostly mild. Still, talking to your healthcare provider is crucial. They can help you understand the benefits and risks. This way, you can decide if an apnea mouthpiece is right for you.
When Not to Use an Apnea Mouthpiece
Apnea mouthpieces can help those with mild to moderate sleep apnea. But, they're not right for everyone. Knowing when they're not a good choice is key to finding the right treatment.
If your sleep apnea is mild to moderate, an apnea mouthpiece might help. This is true if your AHI score is between 5 and 30. But, if your score is over 30, a mouthpiece might not be enough. Your oxygen levels could still drop too low during sleep.
Apnea mouthpieces aren't good for people with central sleep apnea. This type of apnea happens when the brain doesn't tell the lungs to breathe right. A mouthpiece can't fix this problem.
- Severe obstructive sleep apnea (AHI above 30)
- Central sleep apnea
- Insufficient teeth to hold the device in place
- Significant jaw joint issues
People with certain dental problems might not use an apnea mouthpiece well. This includes not having enough teeth to hold it or jaw joint issues. In these cases, other treatments like CPAP therapy or surgery might be better.
Working with your healthcare provider is key to finding the right sleep apnea treatment. Knowing the limits and when not to use apnea mouthpieces helps you make a smart choice. This way, you can find the best solution for your needs.
Caring for Your Apnea Mouthpiece
Cleaning and Maintenance
Keeping your apnea mouthpiece in good shape is key for its effectiveness and your oral health. Your dentist will guide you on how to care for it. This ensures your mouthpiece stays in top condition.
To clean it, brush the mouthpiece with a soft-bristle toothbrush and mild soap. Then, rinse it well and let it air dry. Check your mouthpiece often for any wear or damage. Have it professionally cleaned and checked every 6 months by your dentist.
Storing your mouthpiece in a protective case when not in use helps too. Regular cleaning and maintenance keep your apnea mouthpiece working well. This means it will continue to help you get the sleep apnea relief you need.
- Brush the mouthpiece with a soft-bristle toothbrush and mild soap, rinse thoroughly, and air dry.
- Inspect the mouthpiece regularly for any signs of wear or damage.
- Have your mouthpiece professionally cleaned and checked by your dentist every 6 months.
- Store the mouthpiece in a protective case when not in use to prevent damage.
By following these tips, your apnea mouthpiece will keep working well. This means you can get the sleep apnea relief you need every night.
Combining Apnea Mouthpiece with Other Therapies
Using an apnea mouthpiece can be paired with other sleep apnea treatments like CPAP therapy. This mix can make treatment more comfy and effective for those with obstructive sleep apnea.
About 50% of people stop using CPAP within a year because it's uncomfortable. Adding an apnea mouthpiece can make CPAP more comfortable. It lets patients use CPAP at lower pressure, which reduces noise and discomfort.
Studies found that using both an oral appliance and CPAP cut down on sleep apnea events. Those using both methods had about 2 events per hour. Those on just CPAP had around 4 events per hour. This shows the combo therapy is more effective.
If an apnea mouthpiece doesn't fully help, doctors might suggest combining it with other treatments. This can make patients stick with their treatment better and use it more consistently.
In summary, mixing an apnea mouthpiece with CPAP therapy is a great way to tackle the issues of each treatment alone. This method boosts comfort, makes patients more likely to stick with treatment, and improves overall results for those with obstructive sleep apnea.
Conclusion
Apnea mouthpieces, or oral appliances, can help many people with sleep apnea who can't use CPAP therapy. These devices fit your mouth and move your jaw or tongue to keep your airway open while you sleep. This reduces pauses in breathing, boosts oxygen levels, and cuts down on snoring and daytime tiredness.
They might not work as well as CPAP in all areas, but oral appliances are often more comfy and easy to use for a long time. This leads to better sticking with the treatment and better results. With the right fit, adjustments, and care, an apnea mouthpiece can make a big difference in sleep quality and health for mild to moderate sleep apnea.
The benefits of using an apnea mouthpiece are clear. These devices are a simple, tailored way to breathe easier and sleep better. They support your long-term health and well-being. If you're new to sleep apnea treatment or looking for a more comfy option, checking out apnea mouthpieces could be the right step for you.
FAQ
What is an apnea mouthpiece?
Oral appliances, or mouthpieces, help treat sleep apnea by keeping your mouth open. They move your jaw forward, which also moves your tongue. This makes more space for air to flow in your throat while you sleep.
What are the main types of apnea mouthpieces?
There are two main types: MADs and TSDs. MADs pull your jaw forward. TSDs use suction to keep your tongue forward. Both help increase airflow in your throat.
How do mandibular advancement devices (MADs) work?
MADs are the most common type for sleep apnea. They move your jaw forward, which also moves your tongue. This opens up space in your throat for better airflow. MADs fit over your teeth and have parts that connect to move your jaw.
How do tongue-stabilizing devices (TSDs) work?
TSDs use suction to keep your tongue forward. This helps open your airway. They're not as popular as MADs but are an option for those who can't use MADs due to dental issues.
How effective are apnea mouthpieces compared to CPAP therapy?
Apnea mouthpieces work well but not as well as CPAP therapy. They reduce breathing pauses and improve oxygen levels during sleep. However, CPAP is better at stopping pauses in breathing. Yet, mouthpieces can be more comfortable and easier to use, making them more likely to be used consistently.
What are the benefits of using an apnea mouthpiece?
Apnea mouthpieces can reduce breathing pauses and improve oxygen levels during sleep. They also decrease snoring, make you feel less sleepy during the day, lower blood pressure, and improve quality of life.
Who can use an apnea mouthpiece?
They're recommended for mild to moderate sleep apnea patients who can't use CPAP or don't respond well to it. They can also be used with CPAP when traveling. But, they're not for everyone, especially those with severe sleep apnea, central sleep apnea, or certain dental issues.
How do I get an apnea mouthpiece?
First, get diagnosed with sleep apnea through a sleep study. Then, your doctor will suggest treatment options, including oral appliances. If recommended, see a dentist who specializes in sleep apnea. They'll make a custom mouthpiece for you.
How do I adjust and monitor my apnea mouthpiece?
Wear your mouthpiece every night and see your dentist for follow-ups. They'll adjust it to fit better and improve its effectiveness. You might need a sleep study after adjustments to check its impact on your sleep apnea.
What are the side effects and risks of using an apnea mouthpiece?
Side effects include discomfort in your teeth and jaw, dry mouth, and gum irritation. These are usually mild and go away over time. Serious risks, like worsening sleep apnea, are rare but can happen if the device isn't fitted right.
When should I not use an apnea mouthpiece?
Don't use them for severe sleep apnea or central sleep apnea. They're also not good for people with certain dental issues or jaw problems. Always check with your dentist to see if it's right for you.
How do I care for my apnea mouthpiece?
Clean and store your mouthpiece as your dentist advises. This usually means brushing it with a soft toothbrush and mild soap, rinsing it, and letting it air dry. Check it for damage and get it professionally cleaned every 6 months.
Can I use an apnea mouthpiece with other sleep apnea treatments?
Yes, you can use them with other treatments like CPAP therapy. Some people use a mouthpiece when traveling because it's portable and doesn't need power. They can also reduce the CPAP pressure, making it more comfortable.
Source Links
- Sleep Apnea Mouth Guard
- Steps to Choosing the Right Sleep Apnea Mouthpiece
- Oral Appliances for Sleep Apnea: Benefits and How They Work
- Sleep Apnea Mouth Devices: Mouth Guards, MAD, and More
- Mandibular advancement device: Benefits, side effects, and more
- Sleep Apnea Mouth Guard
5 Top Strategies for Middle Back Pain Relief
Middle back pain, also known as thoracic spine discomfort, can really get in the way of your daily life. It can cause upper back ache, mid-back muscle tension, or pain in the mid-spine. But don't worry, there are ways to get relief. This guide will show you the best strategies to ease your middle back pain and help you move freely again.
We'll cover everything from self-care tips to exercises that target the right areas. You'll learn how to ease interscapular pain, deal with rhomboid muscle strain, and reduce mid-back spasms and ache. With these strategies, you can take back control of your pain and live a life without discomfort.
Understanding Middle Back Pain
Causes and Symptoms
The middle back, or thoracic spine, has 12 vertebrae (T1 to T12). It's below the neck and above the rib cage. This area protects the spinal cord, which helps the brain talk to the body. Problems with bones, muscles, ligaments, and disks can hurt the nerves, causing pain.
Common causes of middle back pain are muscle strain, poor posture, injury, and more. Symptoms can be mild or severe, like muscle aches, burning, sharp pain, and stiffness. In serious cases, you might feel tingling, numbness, chest pain, weakness, or lose control of bowel or bladder.
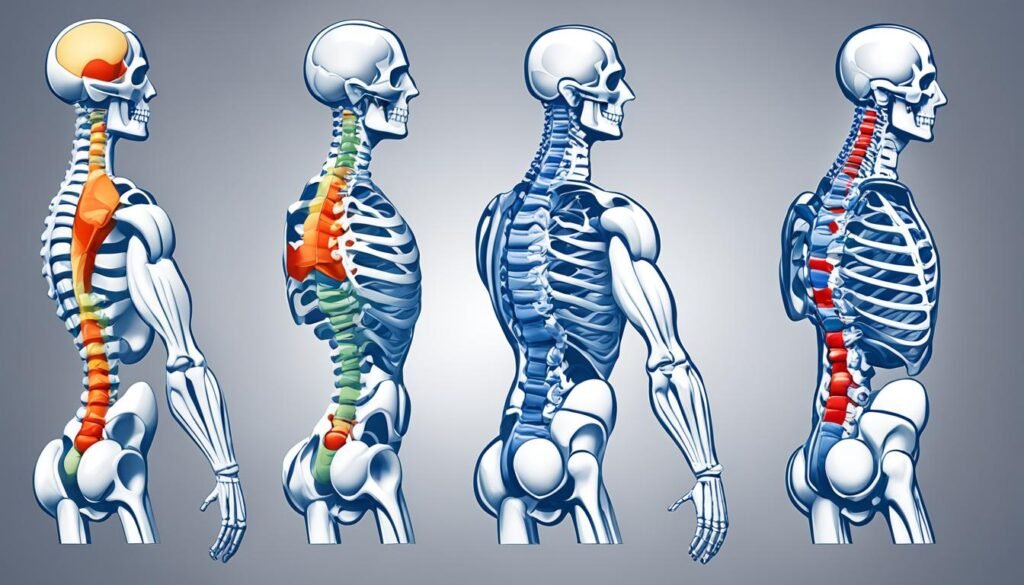
- Poor posture or slouching for a long time
- Muscle tension or imbalances in the mid-back
- Injury or trauma to the thoracic spine
- Degenerative changes like osteoarthritis or disc degeneration
- Osteoporosis causing vertebral compression fractures
- Being overweight and putting more stress on the spine
- Smoking, which can increase the risk of back pain
Knowing what causes middle back pain and its symptoms is key to finding relief and managing it.
Diagnosis and Evaluation
Finding out what's causing your middle back pain is key to getting better. Doctors will do a detailed check-up to figure out the problem. They'll then create a plan just for you. Let's look at how they do this.
Your doctor will start by checking your spine, head, pelvis, and more. They might also test your nerves to see how they're working. This helps spot issues like tight muscles, spine problems, or nerve issues.
Next, your doctor might order tests like X-rays, CT scans, or MRI scans. These tests show your spine in detail. They help find things like broken bones, disc problems, or other causes of middle back pain, thoracic spine discomfort, upper back ache, or mid-back muscle tension.
They might also take blood tests to check for other health issues that could be causing your pain. By using physical checks, tests, and lab results, doctors can find the main cause of your pain. Then, they can make a plan to fix it.
This careful check-up is important for making sure you get the right treatment. Your healthcare team will work with you to understand your symptoms, past health, and lifestyle. This helps them make a treatment plan just for you.
Home Remedies for Middle Back Pain Relief
Dealing with middle back pain can be tough, but you can try simple self-care at home. Using ice packs and heat pads, along with gentle stretches and exercises, can help ease the pain. These methods can make your thoracic spine and upper back feel better.
Simple Self-Care Techniques
Applying an ice pack to your back for 15-20 minutes several times a day can help. It reduces inflammation and numbs the pain. Then, switch to a heating pad or hot water bottle to improve blood flow and relax tight muscles.
Over-the-counter pain relievers like ibuprofen or naproxen can ease middle back pain. They reduce swelling and make you feel less uncomfortable. Gentle stretches and exercises, such as the seated twist and Child's Pose, can also help.
Good posture is key to avoiding middle back pain. Stand up straight, keep your shoulders back, and take breaks from sitting. This can help prevent muscle strain and pain.

If your middle back pain doesn't get better or gets worse, see a healthcare professional. They can find out what's causing your pain and create a plan to help you.
Medical Treatments for Persistent Middle Back Pain
If home remedies don't help your middle back pain in a few days, it's time to see a doctor. They can figure out why your thoracic spine hurts and create a plan to fix it. This plan might include treating your upper back ache or mid-back muscle tension.
Your doctor might suggest some healthcare solutions based on how bad your pain is and what's causing it:
- Physical therapy to strengthen your back muscles, improve flexibility, and teach proper posture and movement techniques
- Prescription pain relievers or muscle relaxers to manage the acute symptoms of your middle back pain
- Chiropractic care to realign the spine and alleviate pressure on the nerves
- Steroid injections to reduce inflammation and provide temporary pain relief
If less invasive medical treatments don't work, your doctor might talk about surgery. This could be a laminectomy, laminotomy, or diskectomy to fix any structural problems.
It's key to work with a healthcare professional to get the right clinical management for your pain. With the right middle back pain medical treatment, you can feel better and do what you love again.

Surgical Options for Severe Cases
If conservative treatments don't help with severe middle back pain, surgery might be an option. Doctors may suggest laminectomy, laminotomy, or diskectomy. These are for cases with structural problems like herniated disks or spinal stenosis.
Recovery from middle back pain surgery, thoracic spine discomfort operative treatment, upper back ache severe intervention, or mid-back muscle tension advanced procedures takes months. It's needed for long-term relief and to help patients with severe pain.
- Laminectomy: Removal of the lamina to decompress the spinal cord
- Laminotomy: Partial removal of the lamina to alleviate a pinched nerve
- Diskectomy: Removal of part of a spinal disk to relieve nerve compression

These surgeries are for severe cases of middle back pain, thoracic spine discomfort, upper back ache, or mid-back muscle tension that don't get better with other treatments. Surgery is chosen based on the patient's condition, symptoms, and health.
Stretches and Exercises for middle back pain relief
Certain stretches and exercises can help ease middle back pain. They also improve flexibility and strengthen the muscles in the thoracic spine. Adding these to your routine can offer much-needed relief and support for your upper back health.
Yoga Poses and Stretches
Yoga has many poses and stretches that target middle back pain relief exercises and upper back ache yoga poses. Some good options include:
- Cat-Cow: Gently flexing and extending the spine to release tension.
- Downward-Facing Dog: Lengthens the thoracic spine discomfort stretches and strengthens the back muscles.
- Cobra Pose: Opens the chest and shoulders, relieving mid-back muscle tension mobility.
- Bridge Pose: Backbend that can help alleviate upper back pain.
Always talk to a healthcare provider before starting any new exercise. Some movements might not be right for your condition.

Other great middle back pain relief exercises are the seated twist, Child's Pose, and Thread the Needle. These gentle stretches can help improve flexibility and reduce discomfort in the thoracic spine.
Adding stretching and strengthening exercises to your routine can support your middle back health well. Remember to listen to your body and adjust the intensity as needed to prevent further injury.
Lifestyle Adjustments for Prevention
Living a healthy life can help prevent middle back pain. Making a few simple changes can keep your thoracic spine strong and flexible. This reduces the risk of upper back ache and mid-back muscle tension.
Improving your posture is key. Don't slouch or hunch over. Keep your shoulders back and your spine straight. Using a supportive chair and adjusting your computer screen can also help.
Being at a healthy weight and exercising regularly helps prevent middle back pain. Try low-impact activities like walking, swimming, or Pilates. These exercises strengthen your core and back muscles without straining your body.
Getting enough sleep and managing stress with techniques like meditation or deep breathing also helps. Smoking nicotine can limit blood flow to spinal disks, making back pain more likely.
By following these lifestyle tips, you can prevent middle back pain and keep your spine healthy and happy.
Key Lifestyle Tips for Middle Back Pain Prevention
- Improve posture by avoiding slouching and keeping shoulders back
- Maintain a healthy weight and engage in regular exercise, such as walking, swimming, or Pilates
- Get enough quality sleep and manage stress through relaxation techniques
- Avoid smoking, as nicotine can restrict blood flow to spinal disks
- Use proper ergonomics at work, including a supportive chair and adjustable computer screen

Complementary and Alternative Therapies
While traditional medicine is key for managing middle back pain, many find relief in complementary and alternative therapies. These natural remedies can be a big help, offering a holistic way to care for your thoracic spine and upper back.
Natural Remedies to Consider
Massage therapy is one option that might ease mid-back muscle tension. Creams with menthol or cannabidiol (CBD) can also numb pain receptors, helping with middle back pain.
Some people like using arnica for its anti-inflammatory effects. But always talk to your doctor before trying new supplements or therapies, especially if you have other health issues or take medicines.

Using complementary and alternative therapies can be a big help for middle back pain. By trying these natural remedies, you might find a better way to handle your thoracic spine and upper back issues.
When to Seek Professional Help
If you're dealing with middle back pain, you might be able to handle it at home. But, there are times when you need to see a doctor. Knowing when to get help is key.
Most middle back pain can be fixed with simple treatments at home. But if the pain lasts over 72 hours, you should see a doctor. Signs like tingling, numbness, weakness, or losing control of your bladder or bowels mean you need help right away.
If your back pain comes on suddenly and is very bad, get help fast. This could mean you have a serious issue like a broken bone or spinal cord injury. These need quick medical care.
- Persistent middle back pain lasting more than 72 hours
- Tingling, numbness, or weakness in the limbs
- Loss of bladder or bowel control
- Sudden, severe back pain after an injury or accident
If you notice any of these symptoms, see a middle back pain doctor. They can figure out what's causing your pain and help you get better. This can also prevent more problems later.
Middle back pain relief Strategies Tailored to Your Needs
Finding relief for your middle back pain requires a personalized approach. The best treatment depends on the cause of your pain, your age, health, activity level, and what you prefer. With a healthcare provider's help, you can create a plan that meets your specific needs for middle back pain relief.
Your healthcare provider might suggest home remedies, physical therapy, medication, or surgery for severe cases. If your pain comes from poor posture or work setup, they might recommend exercises to fix your posture and strengthen muscles. For pain linked to conditions like a herniated disc or kidney stones, you might need specific treatments like painkillers or procedures.
It's important to work with your healthcare provider to create a personalized middle back pain relief plan. This plan should tackle the main cause of your thoracic spine discomfort and help you manage your mid-back muscle tension effectively.
Maintaining a Healthy Back
Preventing middle back pain is key for your long-term thoracic spine discomfort wellness and upper back ache long-term care. After fixing any mid-back muscle tension, focus on healthy habits. This means practicing good posture, doing exercises for your core and back, and stretching every day.
It's also important to keep a healthy weight and sleep well to avoid middle back pain. Plus, be aware of your work setup and take breaks to avoid putting strain on your thoracic spine.
- Prioritize good posture throughout the day
- Engage in regular exercises to strengthen your core and back muscles
- Incorporate daily stretching and mobility exercises
- Maintain a healthy weight to reduce strain on your spine
- Ensure you get enough quality sleep each night
- Pay attention to ergonomics at work and take regular breaks
By following these habits, you can lower the chance of getting middle back pain again. This way, you can keep your spine healthy for life. Always talk to a doctor before starting new exercises or big changes in your life.
Conclusion
Middle back pain, found in the thoracic spine, is common and can be managed. Knowing the causes, like poor posture or injury, helps you take steps to ease the pain. It's important to notice the symptoms, get medical help, and use home remedies and self-care.
If your pain is from muscle tension, joint issues, or health problems, a full approach can help. This includes exercises, stretching, and changing your lifestyle. Keeping a good posture, staying active, and getting professional advice can help manage your pain and prevent future issues.
The key takeaways are that middle back pain is common and can be handled with self-care and medical help. By understanding the causes, symptoms, and treatments, you can make a plan to ease your mid-back muscle tension. This will help improve your overall back health and well-being.
FAQ
What causes middle back pain?
Middle back pain can come from poor posture, injuries, health issues, or aging.
What are the symptoms of middle back pain?
Symptoms include muscle aches, dull pain, and burning sensations. You might also feel sharp or stabbing pain, muscle tightness, or numbness in your limbs. In severe cases, you could have chest pain, weakness, or lose control of bowel or bladder.
How is middle back pain diagnosed?
Doctors use a physical exam and tests like X-rays, CT scans, MRI scans, and neurological tests to find the cause of middle back pain.
What are some home remedies for middle back pain relief?
You can try using ice packs and heat pads, taking over-the-counter pain meds, and doing gentle stretches and exercises at home to relieve middle back pain.
When should I seek medical treatment for middle back pain?
If home remedies don't help after 72 hours, or if you have sudden, severe pain after an injury, you should see a doctor.
What are some medical treatments for persistent middle back pain?
Doctors might suggest physical therapy, prescription pain meds, chiropractic care, or steroid injections if home remedies don't work.
What are the surgical options for severe middle back pain?
For severe pain, surgery like a laminectomy, laminotomy, or diskectomy might be recommended if other treatments don't work.
What stretches and exercises can help relieve middle back pain?
Helpful stretches include the seated twist, Child's Pose, Thread the Needle, and yoga poses like Cat-Cow, Downward-Facing Dog, Cobra Pose, and Bridge Pose.
How can lifestyle adjustments help prevent middle back pain?
Improving your posture, staying at a healthy weight, exercising regularly, sleeping well, and managing stress can help prevent middle back pain.
What complementary and alternative therapies can help with middle back pain?
Massage therapy, topical creams with menthol or CBD, and natural remedies like arnica can offer relief for middle back pain.
Source Links
- 19 Exercises for Upper Back Pain, Neck Pain, Tight Shoulders
- Best Mid Back Stretches and Exercises for Back Pain - BenchMark Physical Therapy
- 10 Daily Habits To Stop Back Pain
- 10 alternative back pain treatments to try before choosing surgery | Orthopaedics and Rehab | UT Southwestern Medical Center
- Treating back pain without surgery: 11 alternative treatment options
- When Can a Doctor Help Your Back Pain?
- Back pain: Symptom When to see a doctor
- Middle Back Pain on Left-Side: Morning Relief Guide
- 6 Ways to Improve Your Back Pain
- Taking care of your back at home: MedlinePlus Medical Encyclopedia
- 16 Ways to Avoid Back Pain
- 10 Tips For Dealing With Lower Back Pain
- Middle Back Pain - Massage & Stretches For Relief
- Understanding and Managing Middle Back Pain: Causes, Symptoms, and Treatment - Singapore Paincare Center
- 7 Exercises to Relief Upper & Middle Back Pain | QI Spine