Understanding Early Childhood Trauma: A Comprehensive Guide
As a parent or caregiver, you are key in helping children who have faced early childhood trauma. Trauma deeply affects a child's growth in many ways. This guide aims to give you the knowledge and tools to make a safe, caring space for these children.
Early childhood trauma can take many forms, like neglect, abuse, or big life events. Knowing about trauma's signs and effects helps you support children who have been through it. This guide will cover how trauma affects kids and the important role caregivers play in helping them heal.
Working with mental health experts is crucial for helping trauma-affected children. This guide will show why this partnership is important. It will also offer strategies for working together to help children heal and become resilient.
This guide is for parents, teachers, or community leaders. It aims to give you the power to create a safe, caring space. This space helps children deal with early childhood trauma and grow strong.
What is Early Childhood Trauma?
Early childhood trauma means going through hard times that can deeply affect a child's mind, body, and feelings. These tough events include neglect, abuse, seeing violence, and losing someone close. It's key to understand early childhood trauma to help children who have gone through it.
Types of Traumatic Events in Early Childhood
The National Child Traumatic Stress Network lists many traumatic events that kids might face early on. These include:
- Psychological, physical, or sexual abuse
- Community or school violence
- Seeing or going through domestic violence
- Natural disasters or acts of terrorism
- Sudden or violent loss of a loved one
These traumatic events, or ACEs, can greatly affect a child's growth and health. Knowing about these traumas helps us give the right support and help.
Understanding early childhood trauma and its forms is vital. It helps us tackle this big issue and support our young ones in growing strong and resilient.
Prevalence of Early Childhood Trauma
Early childhood trauma affects millions of young lives. At least 1 in 7 children faced abuse or neglect last year. The true number of traumatized children is likely higher. In 2019, a shocking 1,840 children died from abuse and neglect in the U.S.
Childhood adversity has a big impact every day. Over 1,000 youth go to the emergency room for assault injuries daily. About 1 in 5 high school students were bullied at school last year. These numbers show how common trauma is among young children.
We must pay attention to early childhood trauma. By understanding this issue, we can help children, support families, and create a healing society. This way, we can lessen the effects of childhood adversity and give our young people a better future.
Signs and Symptoms of early childhood trauma
It's key to spot trauma signs in young kids to help them. Kids react differently to traumatic events. Knowing the signs helps us support them better.
Some common signs of trauma in young children include:
- Fear of separation from parents or caregivers
- Excessive crying or screaming
- Poor appetite or weight loss
- Recurring nightmares
- Increased anxiety or fearfulness
- Difficulty concentrating or paying attention
- Sleep disturbances
As kids get older, trauma symptoms change. Elementary school kids might feel sad, lonely, or have trouble in school. Teenagers might turn to harmful behaviors like drugs, self-harm, or risky sex to deal with their feelings.

Spotting trauma early in kids can really help them. By knowing how trauma shows up in kids, we can give them the right help. This way, they can heal and do well in life.
The Body's Alarm System and Trauma Response
Our bodies have a built-in alarm system to keep us safe. When it goes off, it starts a stress response called the "fight or flight" reaction. This can deeply affect kids who faced trauma early on.
The body's trauma response is automatic when we feel danger. If a child feels threatened, their brain tells the body to release hormones like adrenaline and cortisol. These hormones get the body ready for a fight or flight reaction, making the heart race, blood pressure go up, and muscles tense.
But, this stress response in children can happen in non-threatening situations too. It can make kids feel scared, angry, or pull away. The physiological effects of trauma can really affect a child's health, both body and mind. It's key to know and deal with this.
To help kids with their alarm system, teaching them how to spot stress triggers is vital. Also, showing them how to relax, like through deep breathing, is important. By helping kids understand and control their body's trauma response, we can help them be more resilient and get past early trauma.
Impact of Early Childhood Trauma
Childhood trauma can have lasting effects that go beyond the early years. Survivors often face challenges like learning problems, more health and mental health services, and issues with child welfare and justice. They may also have physical health issues like diabetes and heart disease.
Early trauma greatly increases the risk of mental health problems. It's a big risk factor for many behavioral and substance use disorders. Kids who go through trauma might deal with anxiety, depression, PTSD, and other mental health issues into adulthood.
Long-term Consequences
The effects of trauma in early childhood can be deep and complex. Trauma can harm brain development, make it hard to manage emotions, and affect how well a child forms relationships. This can cause many challenges, including:
- Academic and learning difficulties
- Increased risk of substance abuse and addiction
- Difficulty keeping stable jobs or relationships
- Physical health problems such as traumatic brain injury, diabetes, and heart disease
- Involvement with the child welfare or juvenile justice systems
But, with the right support and help, kids can overcome early childhood trauma. They can lead happy, healthy lives. By tackling the effects of trauma and giving kids the tools to heal, we can lessen the long-term effects and help them succeed.
Supporting Children's Recovery from Trauma
Helping young children recover from trauma takes a lot of effort. Caregivers and support systems play a huge role in this. By supporting children from trauma, we help them feel safe, strong, and hopeful again.
Recovery strategies include making a safe space for kids. This means:
- Telling them they are safe and their feelings are okay
- Explaining the traumatic event wasn't their fault
- Being patient and understanding with their feelings
- Getting help from mental health experts when needed
It's crucial to give trauma-informed care to young children. This helps caregivers support their healing. By helping kids deal with trauma, we build their resilience. This lets them face challenges with strength and kindness.

Recovery isn't always easy, but with the right support, kids can get past trauma. They can feel safe, trust others, and be happy again. By focusing on trauma recovery, we help young people and make the world a better place for everyone.
Role of Caregivers and early childhood trauma
As a caregiver, you are key in helping children who have gone through trauma. By knowing how trauma affects them, you can offer care that helps them heal and grow. Trauma-informed care means making a safe space where kids can feel in control and trust again.
Supporting children from trauma means building strong, caring relationships. This includes:
- Creating a steady, predictable routine for security
- Supporting them in expressing feelings in a healthy way
- Accepting their feelings and experiences without judging
- Teaching them ways to handle stress and overwhelm
It's also vital to look after your own feelings. Taking care of yourself helps you stay connected to the child's needs. Self-care lets you manage your feelings and support the children better.
Your job goes beyond just physical care. You are a source of emotional strength, safety, and healing for kids who have been through trauma. By understanding their needs and taking care of yourself, you can change their lives for the better.
Collaborating with Mental Health Professionals
When a child faces early childhood trauma, working with mental health experts is key. These include child therapists, social workers, and trauma specialists. They bring skills and knowledge that help childcare providers care for the child better.
Teaming up with mental health pros has many benefits. You get insights into what the child needs and can plan a full support plan. They offer therapies like trauma-focused therapy to help the child heal.
These experts also teach how to make a safe, caring space for the child. They help you tackle any emotional or behavioral issues the child has.
Working together on childhood trauma is crucial. With mental health pros, you make sure the child gets all-around support to recover and do well. This teamwork leads to better results for the child and a stronger community.
You're not going it alone. Asking for help from mental health experts shows you're dedicated to giving the best care to the kids. Together, you can tackle the tough issues of early childhood trauma. You'll help these young ones move forward on their healing journey.
Conclusion
Helping children recover from early trauma takes a team effort. Childcare workers like you are key in supporting kids on their healing journey. You can help by spotting trauma signs, using supportive methods, and working with mental health experts. This creates safe spaces for kids to heal and grow.
Understanding early childhood trauma shows us the need for a full approach to help kids. Caregivers play a big part in this. They must know how to care for kids who have been through trauma. With this knowledge, you can change lives, helping kids look forward to a bright future.
Your work in making a safe, caring place for kids shows your commitment. By using trauma-informed care, you help kids grow and do well. You give them the tools to beat early trauma and flourish.
FAQ
What is early childhood trauma?
Early childhood trauma is when bad experiences deeply affect a child's health. This includes neglect, abuse, violence, and losing someone close.
What are the types of traumatic events in early childhood?
Traumatic events for young kids include abuse, violence, seeing violence, and losing someone suddenly. Natural disasters and terrorism also count.
How prevalent is early childhood trauma?
About 1 in 7 kids face abuse or neglect yearly. In 2019, 1,840 kids died from abuse. Every day, over 1,000 youth go to the ER for assault injuries. Also, 1 in 5 high schoolers were bullied last year.
What are the signs and symptoms of early childhood trauma?
Traumatic stress shows differently in each child. Young kids might be scared of being apart from their caregivers. They could also cry a lot, not want to eat, or have bad dreams.
Older kids might feel anxious, have trouble focusing, or sleep poorly. Teens might feel sad, eat too much or too little, or use harmful substances.
How does the body's alarm system respond to trauma?
Our body has an alarm to keep us safe. It gets ready to fight or run when it senses danger. This can make kids feel scared, angry, or withdrawn.
Children can calm down by knowing what scares them, checking if it's real danger, and using deep breathing.
What are the long-term consequences of early childhood trauma?
Trauma can lead to learning issues, more health and mental health visits, and problems with child welfare. It can also cause long-term health issues like diabetes and heart disease. Trauma increases the risk of mental health and substance use disorders.
How can caregivers support children's recovery from trauma?
Caregivers can help by being nurturing and consistent. They should keep routines steady and let kids express feelings. It's also important for caregivers to take care of their own feelings to be fully there for the child.
Why is it important to collaborate with mental health professionals?
Working with mental health experts like therapists and social workers helps kids with trauma. These professionals have the skills to support childcare providers. Their advice can really help kids heal.
Source Links
- Understanding Trauma in an Early Childhood Context | ECLKC
- Supporting Healing: Early Childhood Trauma and Recovery Techniques in Childcare
Dealing with Childhood Trauma: Steps to Recovery
Trauma brings strong feelings that don't go away unless you deal with them. If you don't process these feelings when they happen, they stay in your mind and body. The best way to handle childhood emotional wounds is to understand the harm done, feel the right emotions, and know it doesn't define you.
But this doesn't always happen naturally. Often, you might push away your feelings instead of facing them. This can lead to carrying those emotional scars into adulthood. They can affect your relationships, job, happiness, and health.
To heal from childhood trauma, you must finish the healing process that started long ago. This is crucial for your well-being.
Therapies focused on trauma, learning to cope, and finding support are key steps towards healing. With hard work and the right help, you can overcome childhood trauma and improve your life.
Understanding Childhood Trauma
Our childhood experiences shape us in ways we might not realize. Some events can be traumatic, known as adverse childhood experiences (ACEs). These are negative events that affect a child's well-being and health. They include abuse, neglect, or being in harmful environments.
Types of Childhood Trauma
Childhood trauma comes in many forms, including abuse and neglect. Here are some examples:
- Physical or sexual abuse
- Sudden death of a loved one due to murder or suicide
- Kidnapping
- Witnessing violence in the household
- Emotional or physical neglect
These adverse childhood experiences can deeply affect a person's mental, emotional, and physical health. Knowing about the different types of childhood trauma helps us understand and deal with its effects.
Recognizing the Signs of Childhood Trauma in Adults
If you've faced childhood trauma, you might notice its effects in adulthood. The signs of childhood trauma in adults can be varied. They often include trouble forming healthy relationships, being overly alert, feeling depressed, and anxious.
As an adult trauma survivor, you might always feel on edge. Even in safe places, you might feel threatened. Childhood trauma can also lead to post-traumatic stress disorder (PTSD). This can cause flashbacks, nightmares, and panic attacks.
Adult trauma survivors often struggle with unhealthy relationships, depression, and anxiety. They may also experience dissociative episodes. The journey to healing is tough, but recognizing these signs is the first step to taking back your life.
You're not alone in this fight. There are resources and support out there to help you deal with childhood trauma's lasting effects. With the right tools and support, you can manage these effects and move towards healing and growth.
The Impact of Childhood Trauma on the Brain and Psyche
Childhood trauma can deeply affect both the brain and the mind. When kids go through traumatic events, their brains change in big ways. This can lead to lasting effects. The brain changes can make it hard for kids to handle emotions, remember things, and make good choices.
How Early Life Distress Affects the Brain and Psyche
When kids face trauma, their stress system gets too sensitive. This messes with the brain's balance. It can make parts of the brain that control feelings, memories, and decisions not develop right.
These kids often feel a lot of fear, anxiety, and always be on the lookout for danger. Trauma can also make it hard for them to trust others or feel safe in relationships. If not treated, trauma can cause anxiety, depression, social issues, PTSD, and trouble with forming healthy relationships.
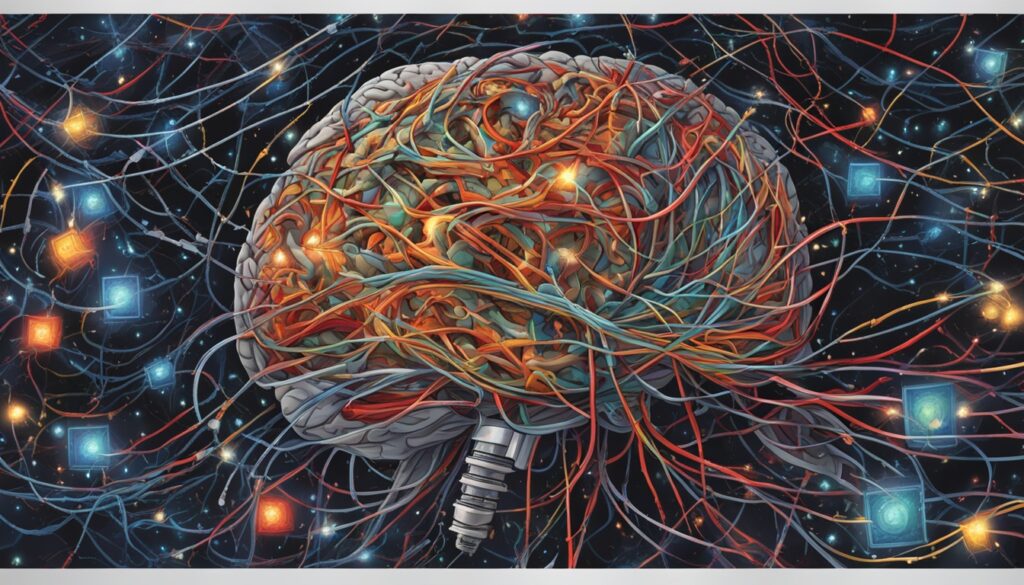
It's important to see how big of an impact childhood trauma can have on the brain and mind. By understanding this, we can help those who have been through trauma. We can guide them towards healing and building resilience.
Emotional Regulation and Childhood Trauma
Childhood trauma can deeply affect how well someone can handle their feelings. Those who have gone through this often find it hard to notice and share their emotions. They might act impulsively or avoid feeling things altogether. Learning to manage emotions is key to healing for adults dealing with childhood trauma.
Sudden memories of trauma can bring strong feelings that are hard to deal with. Therapies like trauma-focused cognitive-behavioral therapy (TF-CBT) and dialectical behavior therapy (DBT) offer help. These methods teach skills for dealing with emotions and stress, improving emotional health.
Working on emotional control and finding better ways to cope, adults with past trauma can take back control of their feelings. With help from mental health experts and a dedication to healing, they can learn to handle all kinds of emotions better.
Attachment Styles and Relationships
Childhood trauma can deeply affect how we connect with others in adulthood. Trauma during our early years can make it hard to trust and depend on people. It can also make us fear being open, set unclear boundaries, and struggle with trust.
This trauma can make forming healthy relationships tough. It's key to understand how trauma impacts our attachment styles. This knowledge helps us heal and build better relationships.
How Trauma Affects a Child's Attachment Styles and Relationships
Kids who go through trauma, like abuse or loss, might develop insecure attachment styles. These styles can make relationships in adulthood hard.
- Avoidant attachment: Trouble trusting others, avoiding closeness, and fearing being open.
- Anxious-ambivalent attachment: Feeling intense, mixed emotions in relationships, needing closeness but fearing being left.
- Disorganized attachment: Feeling confused and unsure in relationships, lacking a clear way to find comfort or safety.
These styles can stick with us into adulthood, affecting our relationships. Therapy, like trauma-informed approaches, can help. It can teach us to form secure attachments, set clear boundaries, and trust ourselves and others.
Dealing with childhood trauma and Addiction Risk
Recent studies have found a strong link between childhood trauma and the risk of addiction in adults. People who faced trauma, like abuse or neglect, during their youth are more likely to develop substance abuse and addictive behaviors. It's key to understand this link to tackle addiction's root causes and offer the right treatment.
The Effects of Childhood Trauma on the Brain and Psyche
Childhood trauma deeply affects the brain and mind, raising the risk of addiction. It can cause problems with managing emotions, making poor choices, and a strong stress response. These issues make people more prone to use addictive substances or behaviors to cope with hard feelings.
Also, trauma changes the brain's reward and motivation systems. It makes it tough for people to feel joy or satisfaction without addictive substances or behaviors. This can start a cycle where the person keeps seeking these substances or behaviors to ease their pain, making the addiction worse.
- Emotional dysregulation
- Impaired decision-making
- Heightened stress response
- Altered brain reward and motivation systems
Dealing with the trauma is key for those with addiction and a past of childhood trauma. By grasping the link between childhood trauma and addiction, we can create better ways to help those in need. This can help break the cycle of addiction.

Healing from Childhood Trauma
Healing from childhood trauma is a deep journey of self-discovery and growth. It can feel tough at first, but it's also rewarding. The first step is to understand the trauma and see how it affects you.
Be patient with yourself as you heal. Trauma often makes us feel bad about ourselves, making healing harder. Getting support from loved ones or mental health experts is key.
Talking to therapists who know about trauma can help. They use methods like cognitive behavioral therapy and EMDR. These methods help you deal with feelings, learn to cope, and grow stronger. They guide you to feel safe, in control, and valuable again.
Healing from trauma is not straight forward; it has ups and downs. Be gentle with yourself, celebrate your wins, and ask for help when needed. With time, kindness, and support, you can move past your past and create a better future.
You're not alone in this journey. Many have been where you are, and there's help and communities out there for you. Embrace the healing process, and believe you can overcome childhood trauma with time and effort.
Trauma-Informed Therapies
Healing from childhood trauma can seem tough, but the right therapies can help. These therapies are made to meet the special needs of people who've faced trauma. This includes abuse, neglect, and other tough experiences from childhood.
Effective Trauma-Informed Therapies
Some of the best therapies for trauma are:
- Cognitive Behavioral Therapy (CBT): This therapy looks at how your thoughts, feelings, and actions are linked. It helps you change negative patterns.
- Dialectical Behavior Therapy (DBT): This method helps you handle strong feelings, learn healthy ways to cope, and improve your relationships.
- Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT): Made for those affected by trauma, this therapy aids in managing emotions and learning to live healthier.
These therapies offer a safe space for you to look into your trauma, feel your emotions, and learn new skills. With a skilled therapist who knows about trauma care, you can start healing. You can build a life that's more fulfilling and resilient.
Developing Healthy Coping Mechanisms
Dealing with the effects of childhood trauma can feel overwhelming. But, by learning healthy ways to cope, you can take back control and grow stronger. Using tools like mindfulness, meditation, and journaling can help manage your feelings and work through your trauma.
Mindfulness and meditation can make you feel more grounded and present. They lessen the effect of scary thoughts and memories. Journaling is great for expressing and understanding your feelings safely.
Physical activity is also a key way to cope. It helps release stress, boosts your mood, and releases happy chemicals in your brain. Having a circle of friends and family who get you is crucial too. They offer a safe place to talk and feel supported.
Healing from childhood trauma is a personal journey. But, by using healthy coping methods, you can move forward and look to the future with hope.
- Practice mindfulness and meditation to regulate emotions
- Engage in journaling to process and express your feelings
- Incorporate physical activity to release tension and improve well-being
- Surround yourself with a supportive network of trusted individuals
Seeking Support and Building Resilience
Healing from childhood trauma takes a lot of effort. It's important to seek support and build resilience. Getting help from professionals and connecting with others who have gone through similar things can be very helpful. It gives you a sense of not being alone and understanding others better.
Self-care is key to building resilience. This means getting enough sleep, eating well, and doing things that make you happy. Over time, you can grow stronger and learn to handle your feelings better.
There are many resources out there for trauma recovery. You can find articles, books, and support hotlines online. These can give you new ways to deal with your feelings and help you feel better.
Remember, healing from childhood trauma is a long journey. Be kind to yourself and don't rush. With the right support and tools, you can overcome the past and move forward.
Conclusion
Childhood trauma deeply affects your mental, emotional, and physical health. But, healing is possible with the right support and strategies. Understanding different types of trauma and recognizing signs in adulthood helps you start healing.
Talking to therapists and using therapies like cognitive-behavioral therapy and EMDR can help. Building healthy coping skills and a strong support network is also key. This can be through therapy, support groups, or self-care.
Recovering from trauma is hard, but it's worth it. By facing the trauma, you can take back your life and look forward to a better future. You're not alone, and there are many resources and professionals ready to help you. With determination and kindness towards yourself, you can beat the effects of childhood trauma and live well.
FAQ
What is the healthiest response to childhood emotional wounds?
The best way to deal with childhood emotional wounds is to understand the trauma's impact on your self-image. It's important to feel the emotions that come with it. Realize that the trauma doesn't define who you are.
But, this process isn't easy. Many people hide their feelings instead of facing them.
How can childhood trauma affect adults?
Childhood trauma can make it hard to form healthy relationships. Adults may feel always on guard, suffer from depression and anxiety, and even have PTSD. They might act in unhealthy ways in relationships, feel threatened all the time, and struggle with depression and anxiety.
They might also have flashbacks, nightmares, and panic attacks.
How does childhood trauma impact the brain and psyche?
Trauma in childhood changes the brain, making the stress response too strong. This messes with the brain's balance. It affects areas that handle emotions, memory, and making decisions.
This leads to a lot of fear, anxiety, and always being on high alert. People may see the world in a twisted way. Trusting others and feeling safe becomes hard.
How does childhood trauma affect emotional regulation and expression?
Traumatic memories can come back without warning, making emotions stronger. Adults with childhood trauma often feel more sensitive and have trouble controlling their emotions. They might not know how they feel, act impulsively, and avoid dealing with emotions.
They might also act in self-destructive ways or avoid feeling anything at all.
How does childhood trauma influence attachment styles and relationships?
Trauma can make it hard to trust others and feel safe in relationships. People may have trouble forming close bonds. They might fear being open, struggle with setting boundaries, and keep repeating patterns from the past.
This can make forming healthy relationships as an adult tough.
How does childhood trauma increase the risk of addiction and mental health disorders?
Trauma can lead people to use substances or behave addictively to cope with their feelings. It changes the brain and makes it easier to become addicted. This includes problems with managing emotions, making decisions, and handling stress.
What are the steps to heal from childhood trauma?
First, acknowledge the trauma and its effects on you. Be kind to yourself, as self-blame is common. Getting help from loved ones or professionals is key.
Talking to a therapist can help you process your feelings and learn to cope better. This can help you build strength and resilience.
What types of trauma-informed therapies can be effective in treating childhood trauma?
Good therapies include cognitive behavioral therapy (CBT), which links thoughts, feelings, and actions. Dialectical behavior therapy (DBT) helps manage emotions and find healthy ways to cope. Trauma-focused cognitive-behavioral therapy (TF-CBT) is made for dealing with trauma's effects.
What are some healthy coping mechanisms for individuals dealing with childhood trauma?
Good ways to cope include mindfulness, journaling, and exercise. Having a strong support network of friends and family is also crucial for healing.
How can seeking support and building resilience aid in the healing process for individuals dealing with childhood trauma?
Joining support groups or online communities with others who've gone through trauma can be very helpful. Taking care of yourself, like sleeping well, eating right, and doing things you enjoy, can also boost resilience.
With the right support and ways to cope, people can learn to deal with trauma's effects. They can grow stronger and feel better about themselves over time.
Source Links
- 9 Steps to Healing Childhood Trauma as an Adult
- How to Heal from Childhood Trauma: 3 Steps to Start Coping
- Want to Heal Childhood Trauma? 10 Great Treatments to Recover
Anxiety from Childhood Trauma: Understanding the Link
Childhood trauma can deeply affect us, especially linking to anxiety disorders later. Trauma includes physical, emotional, sexual abuse, neglect, and more. Even if it wasn't dangerous, feeling overwhelmed or unsafe can still impact you.
Many people live with anxiety from childhood trauma without even knowing it. What happened to us when we were little, things we may not even remember clearly, can leave deep emotional scars that show up as anxiety when we grow up.
In this blog, we will talk about the strong link between childhood trauma and anxiety. We’ll explain how the brain reacts to early trauma, the signs to look for, and most importantly, what you can do to heal. If you suspect your anxiety is more than just stress, this article is for you.
What is Childhood Trauma?
Not every bad memory is trauma. But some experiences in childhood, especially when repeated or very scary, can hurt the brain, body, and emotions deeply. Let’s explore what those experiences are.
Childhood trauma happens when a child feels unsafe, scared, or alone for a long time. These experiences can change how their brain grows and how they feel later in life.
- Physical, emotional, or sexual abuse: Hitting, shouting, or unwanted touch.
- Neglect: Being ignored or not cared for properly.
- Household violence or addiction: Living where there’s yelling, hitting, or drug use.
- Loss of a parent or caregiver: A sudden death, divorce, or separation can shake a child’s world.
Even if it happened once, trauma can leave deep emotional marks if it’s not addressed early.
The ACE Study & Its Relevance
One of the most important studies on this topic is the ACE Study. ACE stands for adverse childhood experiences (ACEs). This study by the CDC showed how early trauma affects adult health.
According to the CDC:
- 61% of adults had at least one ACE.
- 1 in 6 had four or more.
The more ACEs a person has, the higher their risk of problems like heart disease, depression, addiction, and anxiety disorders.
Unpredictable Environments and Anxiety Development
Growing up in an unpredictable childhood environment can lead to anxiety disorders, like Generalized Anxiety Disorder. Kids who had parents who were hard to predict didn't know when they would be there, if they were sober, or how they would act. This made it hard for them to feel safe.
This unpredictability made kids always be on guard, trying to guess the worst. They learned to always expect bad things to happen. This is how they started to develop anxiety disorders.
- Unpredictable parents respond in unpredictable ways, sometimes being loving and sometimes angry or absent.
- Kids in these unpredictable environments had to figure out what was happening all the time. This kept them always ready for danger.
- Always expecting the worst is a big reason why anxiety disorders develop.
The link between erratic parental behavior and unpredictable childhood environments and anxiety disorders is complex. It's important to understand this to help those who faced childhood trauma.
Perception of Physical Sensations and Hypervigilance
Childhood trauma can deeply affect how you feel and react to physical sensations in your body. If you've gone through trauma, you might feel more sensitive to small physical signs. This can make you always be on high alert.
This happens because trauma can change the nervous system. While others might just notice some physical feelings or think they're normal, you might see them as signs of a big health issue. This can lead to more panic attacks and health worries.
Heightened Sensitivity to Physical Symptoms
Studies show a strong link between childhood trauma, how you feel physical sensations, and being always on guard. People who have been through trauma pay more attention to their bodies, looking for any changes. This can make you react strongly to small physical signs, like a fast heartbeat or chest tightness.
This increased focus on physical feelings often starts a cycle of panic attacks and health anxiety. The more you worry about your body, the more you might feel these symptoms, which can make you worry even more about your health.
Knowing how childhood trauma affects your feelings and physical sensations is key to fighting anxiety and getting better. By understanding these patterns and getting help, you can manage your anxiety. This helps you take back control of your body and mind.
Neurological Changes and Childhood Trauma
Childhood trauma can change your brain in lasting ways. It often makes the amygdala, which handles emotions, bigger or more active. This can make you feel like there's danger everywhere, even when there isn't.
Alterations in Brain Structure and Function
Research shows that those who experienced trauma as kids have different brains. The amygdala, key for emotions, gets bigger or more reactive. This makes you feel always on guard, leading to ongoing worry, Anxiety And Depression.
The Role of the Amygdala in Anxiety
The amygdala is called the "emotional center" of the brain. If it's too active, it can make you overreact to things that aren't really threats. This can lead to anxiety disorders as your brain can't control your feelings well.
Learning about how childhood trauma changes the brain helps you understand your anxiety better. Knowing how the amygdala affects your feelings is a key step to better managing your anxiety.
Anxiety from Childhood Trauma
Not everyone who had a tough childhood will get anxiety or panic. Many things in your life and who you are can change how trauma affects you. Yet, many folks who had a hard time as kids end up with anxiety and/or panic. And, not all anxious people had a tough childhood, but many find big and small traumas from their past when they look back.
The link between childhood trauma and anxiety is clear. Trauma can really hurt your mental health, leading to anxiety disorders. The type of trauma, how long it lasted, and when it happened can affect how you develop anxiety, trauma link, and mental health impact.
If you had a tough childhood, know you're not alone. Many people deal with the lasting effects of trauma. Getting help from a professional is key to managing anxiety and moving past your past.
Working on the causes of your anxiety and finding ways to cope can help you heal. You have the strength to overcome trauma and handle your anxiety in a healthy way.
Comorbidity of Anxiety and Chronic Pain
Chronic pain and anxiety often go together. Studies show a strong link between childhood trauma, anxiety, and ongoing pain. Adults who faced trauma, like abuse or neglect, are more likely to have chronic pain and anxiety later.
The Connection Between Trauma, Anxiety, and Pain
Childhood trauma can change the nervous system and brain. This can make anxiety and pain worse. People with a trauma history might worry more about physical feelings, making their pain and anxiety worse.
Research shows trauma, anxiety, and chronic pain are linked in the brain. Trauma changes how the brain handles stress and threats. This can make the brain's pain and fear centers work differently, making people more sensitive to pain.

- Childhood trauma raises the risk of chronic pain, like fibromyalgia, headaches, and back pain.
- Those with trauma history tend to feel more anxiety and panic from physical sensations.
- The cycle of pain and anxiety can get worse, where one makes the other worse.
Knowing how trauma, anxiety, and chronic pain are linked is key to finding the right treatments. This helps address the root causes of this common problem.
Treating Trauma-Related Anxiety
Childhood trauma and its effects on anxiety are serious but can be treated. The American Psychological Association (APA) suggests cognitive behavioral therapy (CBT) for anxiety from trauma. CBT helps people change negative thoughts linked to traumatic events.
Eye movement desensitization and reprocessing (EMDR) is another good therapy. It helps process traumatic memories in a new way. Prolonged exposure (PE) therapy is also useful. It slowly exposes people to what they fear to lessen avoidance and anxiety.
Cognitive Behavioral Therapy (CBT)
CBT is a therapy that focuses on changing negative thoughts and behaviors from trauma. It helps people challenge bad beliefs. This way, they can better manage their anxiety.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR uses eye movements or other stimulation to help the brain process traumatic memories. This can lessen the emotional pain of the trauma. People can see the event in a new, less distressing way.
Prolonged Exposure Therapy
Prolonged exposure therapy slowly exposes people to what they fear from the trauma. This reduces avoidance and lowers anxiety over time. By facing their fears in a safe place, people learn to handle their anxiety better.
Therapies like CBT, EMDR, and prolonged exposure are very effective for anxiety from childhood trauma. With help from a mental health expert, people can move past trauma's effects. They can regain control and feel better overall.
The Long-Term Effects of Childhood Trauma
Childhood trauma can have lasting effects on your mental and physical health. A 2019 study showed that early emotional trauma can lead to anxiety in older adults. It also linked childhood trauma to mental and physical health issues, like chronic pain.
The effects of childhood trauma highlight the need for treatment to heal. With the right support and therapies, you can move past the harm of your past. This leads to a healthier, happier life.
- Increased risk of adult mental health issues, such as anxiety, depression, and PTSD
- Higher chance of physical health impacts, including chronic pain, heart disease, and breathing problems
- Challenges in building strong relationships and staying emotionally stable
Don't let the long-term trauma effects of your childhood stop you. Seek help and begin your path to healing and strength.
Resilience and Recovery
Childhood trauma can deeply affect us, but it's key to know that both trauma and anxiety disorders can be treated. With the right support and therapies, people can build resilience and heal from past emotional and psychological wounds.
Seeking Professional Help
Getting help from a therapist who knows about trauma and anxiety is a crucial first step. These experts can tackle deep issues and give you ways to handle anxiety and stress. This helps in recovering from trauma.
Therapy and mental health care give you strategies to cope, better manage your feelings, and feel safe and in control. These are key for building resilience and beating the hurdles from childhood trauma.
With the right support from professionals and a dedication to your health, healing and moving forward is possible. You can live a life full of joy and fulfillment, even after tough times.
Heal with Expert Help from Dr. Chandril Chugh
Healing anxiety from childhood trauma is not about forgetting the past, it’s about giving your brain what it needed and never got. If you see signs of trauma in yourself or someone you love, don’t wait.
Dr. Chandril Chugh is a US-trained, board-certified neurologist who specializes in treating complex brain and emotional disorders. With years of experience, he provides expert care for those dealing with trauma, anxiety, and brain-based challenges.
If you’re tired of guessing why you feel the way you do, let Dr. Chugh help you make sense of it all.
Book your consultation with Dr. Chandril Chugh now.
FAQ
What is the link between childhood trauma and anxiety disorders?
Childhood trauma can lead to serious effects that last a lifetime. It includes physical and emotional abuse, neglect, and exposure to violence at home. This trauma is closely linked to anxiety disorders like PTSD, Generalized Anxiety Disorder, and panic attacks.
How common are anxiety disorders among individuals with a history of childhood trauma?
About 3 to 15 percent of girls and 1 to 6 percent of boys develop PTSD after a traumatic event. A 2018 study found that adults with ACEs face many mental and physical health issues, including anxiety disorders.
How do unpredictable childhood environments contribute to the development of anxiety disorders?
Unpredictable environments greatly affect anxiety disorder development. Kids in such settings often worry about their parents' presence, influence, or anger. This keeps them in a state of constant alertness, expecting the worst.
How does childhood trauma affect the perception of physical sensations?
Those who faced trauma as kids might be more sensitive to physical feelings. They might think these sensations mean something serious is wrong. This can lead to panic attacks and health anxiety.
What are the neurological changes associated with childhood trauma?
Trauma in childhood can change the brain and nervous system. The amygdala, which handles emotions, might grow or become too active. This makes people overreact to threats, causing ongoing worry and anxiety.
Is there a connection between childhood trauma, anxiety, and chronic pain?
Yes, there's a strong link between childhood trauma, anxiety, and chronic pain. Adults who went through trauma, like abuse or neglect, are more likely to have chronic pain and anxiety disorders.
What are the effective treatments for trauma-related anxiety?
Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Prolonged Exposure (PE) therapy work well. They help deal with trauma's effects and reduce anxiety.
Can the effects of childhood trauma persist into adulthood?
Yes, trauma's effects can last a long time. A 2019 study showed that early emotional trauma linked to more anxiety in older adults, even those 65 to 77 years old.
How can individuals with a history of childhood trauma find healing and resilience?
Trauma and anxiety disorders are treatable. Working with a therapist who knows about trauma and anxiety is key. They can help tackle the deep issues and teach ways to manage anxiety and stress.
Source Links
- How Childhood Trauma Relates to Present-Day Anxiety and Panic
- When Childhood Trauma Leads to Anxiety
- The Unholy Trinity: Childhood Trauma, Adulthood Anxiety, and Long-Term Pain
Exploring Different Types of Music Therapy
Have you ever noticed how a song can change your mood in seconds?
Music can make us feel many things, like happiness or sadness. It's a strong tool for healing and staying well. Music therapy uses music to help with mental, emotional, and physical health. This article will look at the many types of music therapy and how they can improve your health.
There are many types of music therapy designed to meet different needs. Whether someone is recovering from a stroke, dealing with anxiety, or managing autism, there's a form of music therapy that can help.
In this blog, we will explore the different types of music therapy, how each one works, and how they can help improve your life or the life of someone you care about.
What is Music Therapy?
Music therapy is a clinical, evidence-based treatment that uses music to help people achieve specific health goals. A trained music therapist works with individuals or groups, using music in different ways based on the person’s needs.
It has roots in Ancient Greece, where music was used to connect the body and mind.
There are many types of music therapy, and each one uses different methods to help people feel better mentally, physically, and emotionally.
The History of Music Therapy
Music therapy has been used for thousands of years. Ancient Greeks used music to treat mental illness. In the early 19th century, music's link to health became a focus of study. By 1914, music therapy was gaining attention. Surgeons found that music helped patients feel less anxious before surgery.
In modern times, it became more structured during World War I and II, when musicians played for soldiers in hospitals. The patients showed better recovery, and doctors took notice.
Today, certified music therapists use structured methods backed by science. The American Music Therapy Association (AMTA) was formed in 1998 to set professional standards.
The Benefits of Music Therapy
Before we talk about different types of music therapy, let’s understand why it helps:
- Reduces anxiety and stress
- Helps with pain management
- Supports memory and speech after brain injuries
- Improves motor skills in physical therapy
- Aids emotional expression in trauma patients
- Music therapy benefits children with autism
In one study, 68% of patients with chronic illness said music therapy reduced their pain.
Music therapy can help with anxiety, depression, PTSD, and neurological diseases like Alzheimer's. It also aids children in learning, behavior, and managing emotions.
If you're looking for relief or just want to improve your well-being, music therapy could be right for you. With a qualified music therapist, you can use music to boost your health in many ways.
Active vs. Receptive Music Therapy Interventions
In music therapy, there are two main ways therapists work: active and receptive music therapy. Each has its own benefits and goals. Knowing the differences can help you pick the right approach for you or your clients.
| Type | Description | Example Activity |
|---|---|---|
| Active | The person takes part in making music | Singing, drumming, playing guitar |
| Receptive | The person listens to music selected by a therapist | Guided music listening |
- Active music therapy means the client makes music, plays an instrument, or learns to play. It boosts self-expression, confidence, and helps develop new skills. Making music can be a powerful way to grow and heal.
- Receptive music therapy is more passive. Clients listen to music and talk about it. The therapist picks a song and the client might analyze lyrics, feel the emotions, or see pictures in their mind. This helps people understand their feelings, become more aware, and find ways to deal with tough times.
Both active and receptive music therapy interventions have their own strengths. The choice depends on what the person needs, likes, and the therapy's goals. Using both methods together can give a full music therapy experience that meets the client's many needs.
1. Guided Imagery and Music Therapy
The Bonny method of guided imagery and music (GIM) is a special way to explore your feelings and get creative insights.
This method works by blending music with a person’s inner thoughts and pictures in their mind. During a session, the person lies down in a relaxed position. The music therapist carefully chooses and plays specific music that can help the person connect with their emotions. As the music plays, the person shares the images or memories that come into their mind.
This process helps the brain move into a more relaxed, open state. It allows feelings, thoughts, or memories to come forward, especially those that might be hard to express with words. By talking about these mental images during or after the session, the person can gain new understanding about themselves.
How it helps:
- Calms the mind and body, lowering stress and anxiety
- Helps people understand and heal from emotional pain or trauma
- Boosts mental clarity, imagination, and problem-solving
- Supports therapy for PTSD, depression, and chronic stress
Guided imagery is one of the deepest types of music therapy because it reaches the parts of the mind where many strong emotions live.
This therapy is great for dealing with mental health issues like PTSD, grief, and stress. It uses music and imagination to help you see your inner world. This can lead to big changes in how you see yourself and the world.
If you want to know yourself better or help others, the Bonny method of guided imagery and music therapy is a great choice. It's a unique way to improve your mental and emotional health.
2. Analytical Music Therapy
Analytical music therapy (AMT) is a special way to look into the human mind. It uses music to help you understand yourself, your relationships, and your connection to music.
This is a talk-based therapy. The patient and therapist make music together, then talk about the thoughts and feelings that came up.
What happens during a session:
- Client plays music freely with instruments
- Therapist joins in with musical replies
- After playing, they talk about the emotions or ideas that appeared
Applications of Analytical Music Therapy
Analytical music therapy is one of the most interactive types of music therapy. It works by helping people give shape to feelings that are difficult to explain. Making music together creates a safe space where hidden emotions can rise to the surface.
Once expressed through sound, these emotions can be discussed with the therapist. This connection between music and words helps people understand their behavior, process trauma, and feel emotionally stronger.
Over time, it can lead to better mental health and deeper self-awareness. It’s often used for emotional disorders, especially when talking alone is not enough.
This type is helpful in:
- Treating depression
- Reducing anxiety
- Helping children express feelings
It's one of the best types of music therapy for emotional awareness.
It helps people with emotional, psychological, and relationship issues. If you're facing anxiety, depression, relationship problems, or just want to grow, this therapy can be deeply helpful.
3. Neurologic Music Therapy
Neurologic music therapy (NMT) is a special type of music therapy that helps people with brain and nerve problems. It works by using rhythm and sound to retrain the brain. When someone listens to or plays music in a structured way, it activates parts of the brain linked to movement, speech, and memory. Over time, this can help the brain form new connections, especially after injury.
For example, after a stroke, walking or talking may become hard. But with NMT, music patterns can guide the brain to relearn these tasks step by step. In Parkinson’s disease, rhythm can help improve balance and walking. For children with autism or those with developmental delays, NMT improves communication and focus.
Common uses include:
- Stroke recovery
- Parkinson’s disease
- Traumatic brain injury (TBI)
- Autism and developmental delays
In one study, NMT helped stroke patients walk 50% faster. It’s one of the most powerful types of music therapy for brain recovery.
4. Nordoff-Robbins Music Therapy
Nordoff-Robbins music therapy, also known as creative music therapy, helps people express themselves through music. Paul Nordoff and Clive Robbins created this therapy. They worked with people who had developmental and emotional challenges.
This therapy works well with kids, teens, and adults on the autism spectrum. It also helps those with developmental disabilities and emotional issues. Nordoff-Robbins music therapists help clients find their voice and connect with others through music.
It’s one of the interactive types of music therapy that builds confidence and communication.
The Origins of Nordoff-Robbins Therapy
Nordoff and Robbins spent nearly two decades studying music's impact on their clients. They developed the Nordoff-Robbins method. This method means the therapist plays music with the client, creating spontaneous musical experiences.
This therapy believes everyone has a musical side. It helps with self-expression, social skills, and well-being. Clients use drums and cymbals to make music together with therapists.

5. Community Music Therapy
Community music therapy brings people together to make a difference through music. It's different from one-on-one sessions. The aim is to improve life for groups, not just one person.
This method is used in many places like schools, hospitals, and community centers. It helps people feel better by making music together. This way, everyone's life gets better.
The Goals of Community Music Therapy
The main goals are:
- Promoting social inclusion and community engagement
- Enhancing group cohesion and interpersonal connections
- Empowering individuals and communities to create positive change
- Improving overall quality of life and well-being for participants
It's different from traditional music therapy. It focuses on the group's experience and music's power in groups. With a music therapist, people share music to build a stronger community and feel better.
If you want a more connected community or to enjoy music therapy with others, try community music therapy. It's a powerful way to improve your life and well-being.
6. Orff Music Therapy
Orff music therapy combines music with movement, speech, and drama. It was created by Gertrude Orff, a famous composer and educator. This therapy is great for schools, helping kids with delays or disabilities to express themselves and be creative.
The Orff-Schulwerk approach says music, movement, and language work together. By using them together, people can get better at speaking, making friends, moving, and hearing. It's really good for those who find regular music therapy hard.
Orff music therapy includes many activities, like:
- Improvising with percussion instruments
- Singing and chanting
- Dancing and moving to the music
- Storytelling and dramatic play
These fun activities help people connect more with music. They also help them express themselves and grow personally.
If you're a parent, teacher, or healthcare worker, using Orff music therapy can really help. It's a great way to support people with different needs and abilities.
Types of music therapy
Here is a table to help understand the different types of music therapy at a glance:
| Type | Main Use Case | Active or Receptive | Target Group |
| Analytical Music Therapy | Emotional exploration | Active | Teens, adults |
| Guided Imagery | Deep emotional healing | Receptive | Adults, trauma patients |
| Neurologic Music Therapy | Brain and nerve function | Active | Stroke, TBI, Parkinson’s |
| Nordoff-Robbins | Communication and interaction | Active | Children with autism |
| Orff | Creativity and physical expression | Active | Children with disabilities |
| Community | Social bonding, support | Both | Groups, marginalized people |
How to Know Which Type is Right for You?
Choosing the right types of music therapy depends on your needs.
- If you're recovering from a stroke, neurologic music therapy may help.
- If you have emotional trauma, guided imagery or analytical therapy might work better.
- For kids with special needs, Orff or Nordoff-Robbins therapy is often used.
A certified music therapist will guide you based on your goals and health needs.
Dr. Chandril Chugh's Final Words on Music Therapy
Music can be more than just a hobby. It can heal. If you or someone you love is facing emotional, mental, or physical challenges, music therapy may be a gentle, effective support.
With so many types of music therapy, it's important to choose the one that fits your unique situation. You can choose from active music-making, listening, or community music experiences.
As you finish this article, remember that everyone's path to wellness is different. Music therapy can help you reach your full potential and connect more deeply with yourself and others. Start this journey and see how music therapy can change your life.
FAQ
What is music therapy?
Music therapy is a healthcare profession. It involves a music therapist creating sessions with specific goals. These goals aim to improve mental, emotional, and physical health.
What are the benefits of music therapy?
Music therapy can help with anxiety, depression, and PTSD. It also aids in managing neurological diseases like Alzheimer's. Plus, it supports children's learning, behavior, and emotional control.
What are the different types of music therapy?
There are two main types of music therapy. Active therapy lets clients create music or learn an instrument. Receptive therapy involves listening to music and discussing it to process emotions.
What is the Bonny method of guided imagery and music therapy?
The Bonny method uses classical music and imagery for personal growth and psychological issues. It helps clients uncover hidden emotions and gain creative insights by exploring their unconscious mind.
What is analytical music therapy?
Analytical music therapy explores the client's relationships with themselves, others, and music. Clients may sing or play an instrument to express their thoughts. This helps them reflect on their unconscious feelings with the therapist.
What is neurologic music therapy?
Neurologic music therapy helps with cognitive, sensory, and motor issues from neurological diseases or injuries. It's based on research showing music stimulates the brain and promotes brain flexibility.
What is Nordoff-Robbins music therapy?
Nordoff-Robbins music therapy is an improvisational approach. Therapists and clients play instruments like drums or cymbals. It aims to help clients express themselves and improve social skills.
What is community music therapy?
Community music therapy focuses on improving life in groups through music. It aims for a better quality of life in community settings rather than just helping one person.
What is Orff music therapy?
Orff music therapy combines music with movement, speech, and sometimes drama. It's designed to enhance language skills, social abilities, motor skills, and hearing. It helps children with developmental delays and disabilities.
Source Links
- Exploring the Types of Music Therapy and How They Differ | Trala
- Types of Music Therapy
- What Is Music Therapy, and How Can It Help Me?
Music Therapy for Depression: How It Can Help
If you're fighting depression, music therapy might be a surprising way to find help. This approach is proven to be effective, easy, and affordable for dealing with depression. Music therapy uses music to change your mood and improve your well-being. It can be a key part of your mental health care.
Depression affects over 300 million people around the world. It brings feelings of constant sadness, less interest, and a lack of joy, making everyday tasks hard. But, music therapy can be a strong ally in fighting these feelings and helping you heal.
We're going to explore music therapy in depth. We'll look at how it works, its history, and the good it can do for those with depression. If you're thinking about trying it for yourself or someone you care about, learning about music therapy could show you new ways to feel better and boost your mental health.
What is Music Therapy?
Music therapy uses music to help people feel better and behave in positive ways. It's a way to improve mood and overall health. By using music, people can express themselves, manage stress, and communicate better.
The American Music Therapy Association (AMTA) says music therapy is a professional use of music to meet specific goals. Music therapists work with clients to make plans that fit their needs and likes.
Music Therapy and Mental Health
Music therapy can really help with mental health. It can lower anxiety and boost self-confidence, which is great for those dealing with depression or other mental issues. Making music yourself can make the therapy even more effective.
Music therapists use music to help clients express feelings and develop ways to cope with mental health problems. Music-making and the support from therapists make music therapy a strong way to improve mental health.
How Does Music Therapy Work?
Music therapy is a powerful tool that changes the brain in complex ways. It uses areas for rhythm, emotion, and pitch to activate the brain's reward center. This makes music therapy effective for treating mental health issues like depression.
The neuroscience of music therapy shows music can work on the limbic system. This system is key for emotions, motivation, and social skills. When you listen to music, your brain releases dopamine and endorphins. These chemicals make you feel better and more connected.
Music therapy also helps with depression by improving communication and emotional control. By making or listening to music you like, you tap into your brain's healing power. This can help balance your emotions and improve your mood.
Music therapy goes beyond usual treatments by reaching deep into the human experience. Using the neuroscience of music therapy, experts help people with depression find new ways to express themselves and process emotions. This leads to recovery and healing.
History of Music Therapy
The history of music therapy goes way back, but it became a big deal in the 20th century. It started with ancient civilizations like Ancient Greece, where music was used for healing. But the modern version of music therapy began after World War II.
The first mention of music therapy was in 1789, in an article called "Music physically considered." In the 1800s, doctors kept studying how music could help people. By the 1940s, music therapy programs were in universities, thanks to pioneers like E. Thayer Gaston. They made music therapy a recognized therapy.
The history of music therapy is an interesting story. It started with ancient healing methods and grew into a modern therapy. Today, research shows how music can help with both physical and mental health. So, the future of music therapy looks very promising.

Benefits of Music Therapy for Depression
Music therapy is a powerful way to help with depression. Studies show it has many benefits for those feeling down. It can really make a difference in someone's life.
A big study looked at 1,649 studies on music therapy. It found that music can help reduce anxiety and fight depression in adults. Music therapy helps people relax and connect with their feelings. It also helps them build stronger relationships with their therapists.
Another study looked at how music therapy affects depression. It showed that music can really help reduce symptoms of depression. It also improves how well people function and lowers anxiety in those with depression.
Music therapy has many benefits for depression. It can make people feel better, reduce stress, and help them express their feelings. It can also make social connections stronger. If you or someone you know is dealing with depression, think about trying music therapy.
Music therapy for depression
Research shows that music therapy can help with depression when used with standard treatments. It might make managing depressive symptoms more effective. Studies suggest that adding music therapy to treatment plans can lead to better results than just standard therapy.
Music Therapy Enhances Depression Treatment
A recent study found that music therapy helped more than standard treatment alone. It led to big drops in both doctor-rated and patient-reported depression. This shows music therapy could make traditional depression treatments work better.
Music therapy can be made to fit what each person likes and can work with other treatments. This makes it a great addition to managing depression.
Music therapy uses the strong link between music and emotions to help with depression. As research grows, using music therapy with standard care could become a key part of treating depression.
Music Therapy for Children and Adolescents
Music therapy is great for young people with depression. It's a fun way for them to express feelings and boost self-esteem. Music therapy helps improve their well-being.
Music therapy helps kids and teens with depression through creative play and social interaction. They get to make and perform music. This helps them learn important skills and express their feelings.
It also helps with focus, coordination, and understanding oneself. These skills are key for those facing depression.
Music therapy strengthens family bonds and builds resilience in young people. It involves families in the therapy process. This creates stronger connections and support systems, vital for recovery and well-being.

Most studies on music therapy are for adults, but it's also beneficial for young people with depression. It offers a fun, creative way to tackle emotional issues. Music therapy is a powerful tool for supporting the mental health of kids and teens.
Implementing Music Therapy
Qualified music therapists take a detailed approach to music therapy. They start by assessing your needs, strengths, and musical tastes. This includes looking at your emotional, physical, and social health, as well as your communication skills and past traumas.
Next, they work with you to set goals. Then, they design a music therapy plan just for you. This plan can be for one person or a group. It might include making music, singing, listening to tunes, or playing instruments.
Music Therapy Assessment and Program Development
A music therapy process starts with a detailed assessment by a pro. They get to know your music therapy needs and likes. This helps create a plan just for you, focusing on your goals.
During the program, the therapist checks on your progress and makes changes if needed. This teamwork makes sure the therapy fits you perfectly and meets your goals.
Future Directions in Music Therapy Research
Music therapy is growing, and researchers are looking into new ways to make it even more effective. They're focusing on several areas, like how it affects people and working together more. They also want to involve more experts, use different methods, and grow the theory behind it.
The American Music Therapy Association (AMTA) is at the forefront of this. They aim to improve research and make music therapy available to those who need it, like people with depression and anxiety. By working together and connecting with communities, music therapy can help more people in the future.
- Exploring the future of music therapy research to enhance its impact
- Emphasizing consumer-centric and collaborative research approaches
- Promoting clinician involvement and interdisciplinary collaboration
- Embracing diverse methodologies to uncover the mechanisms of music therapy
- Advancing the theoretical foundations of music therapy
- Expanding research efforts to reach more individuals in need
- Fostering strategic partnerships to increase access to music therapy services
As music therapy grows, these new directions could bring big changes. They could improve mental health and quality of life for many people. By leading in these areas, music therapy can keep changing lives and making a big difference in communities.
Conclusion
Music therapy can be a great help for people with depression. It's non-invasive and doesn't cost much. Studies show it can make people feel less anxious and happier.
It also helps improve social skills and overall well-being. More research is needed, especially for kids and teens. But, the current studies show music therapy is a good addition to treatment plans.
With more people facing mental health issues, music therapy is key. It can change how you feel and help you manage your emotions. Music therapy is a powerful tool for fighting depression.
Adding music therapy to your mental health plan can lead to better self-awareness and emotional strength. It's a step towards a happier life. Music therapy can be a big part of managing depression.
FAQ
What is music therapy?
Music therapy uses music to help people achieve their goals. It's a way to improve wellness, manage stress, and help with memory and communication. It also lets people express their feelings.
How does music therapy work?
Music therapy works by engaging the brain's emotion, motivation, and thinking centers. It helps with social skills, emotions, and movement. Music can make people feel better and build stronger relationships.
What is the history of music therapy?
Music therapy has roots in Ancient Greece. It became a formal therapy after World War II. By the 1940s, music therapy programs were available in universities.
What are the benefits of music therapy for depression?
Music therapy can reduce anxiety and depression. It helps with relaxation and improves well-being. It also helps people connect with their feelings and build relationships with therapists.
How is music therapy implemented?
Music therapists first assess a person's needs and strengths. They consider emotional, physical, and social health. Then, they work with the patient to set goals and create a music therapy plan.
This plan can be for one person or a group. It might include making music, singing, or playing instruments.
What are the future directions in music therapy research?
Future music therapy research aims to improve access and quality of services. It will focus on working with more people, including those with depression and anxiety. The American Music Therapy Association is leading this effort.
Source Links
Common Women's Mental Health Issues: What to Know
It's key to understand women's mental health since women often face more mental health issues than men. Issues like depression, anxiety, eating disorders, and hormonal problems are common. Knowing about these common mental health issues for women helps us take action to improve women's mental wellness.
Many mental disorders in women are tied to hormonal shifts. For example, depression during pregnancy and after menopause can affect a woman's mood and daily life. Women also tend to have more depression, anxiety, and eating disorders than men.
Why Women's Mental Health Matters
Women's mental health is very important. They face special challenges because of biology, society, and culture. It's key to understand gender differences in mental health to help them better.
Mental Disorders More Common in Women
Women are more likely to have mental issues like depression, anxiety disorders, and eating disorders. Hormonal changes, social stress, and other factors might play a role in this.
Unique Disorders Related to Hormonal Changes
Women also deal with mental health issues linked to hormonal shifts. This includes depression during pregnancy, premenstrual dysphoric disorder (PMDD), and depression during menopause. Knowing how hormonal changes affect women's mental health is key to good care.
By focusing on women's mental health needs, we can create better support systems. This helps improve their lives and mental well-being.
Symptoms of Mental Disorders in Women
It's key to know the signs of mental health issues in women to get the right help. Women face many emotional, psychological, and social challenges with mental health disorders. Knowing these signs can help you spot problems early and improve your mental health.
Some common symptoms of mental health issues in women include:
- Persistent feelings of sadness, hopelessness, or emptiness
- Anxiety, panic attacks, or excessive worrying
- Changes in sleep patterns, such as insomnia or oversleeping
- Significant changes in appetite, leading to weight loss or gain
- Difficulty concentrating, making decisions, or completing tasks
- Irritability, mood swings, or emotional sensitivity
- Withdrawal from social activities or relationships
- Unexplained physical symptoms, such as headaches or chronic pain
- Thoughts of self-harm or suicide
The symptoms of mental health issues in women can vary a lot. Not everyone will have the same symptoms. The severity and how long these symptoms last can also vary. If you or someone you know is showing these signs, getting professional help is key for diagnosis and treatment.
Knowing the common symptoms of mental health issues in women helps you take steps for your well-being. Remember, your mental health is as important as your physical health. It's vital to make it a priority.
Risk Factors Affecting Women's Mental Health
Many women struggle with their mental health due to various risk factors. These include social, economic, and environmental factors that affect their well-being. It's important to understand these factors to help women with their mental health needs.
Social and Economic Factors
Women often deal with more social and economic stress than men. Being a main caregiver, living in poverty, and facing workplace discrimination are some of these challenges. These issues can lead to mental health problems like depression and anxiety.
Physical and Sexual Abuse
Many women suffer from physical or sexual abuse, which greatly affects their mental health. Abuse can cause post-traumatic stress disorder (PTSD), depression, and other mental health issues. It's crucial to address how abuse impacts women's mental health.
We can improve women's mental health by recognizing and tackling these risk factors. It's key to offer support, resources, and mental health services. This helps empower women to overcome their challenges.
Mental Health and Life Events
Women go through many life changes that can affect their mental health. Important events like perinatal depression and menopause can change how they feel. These changes can be tough on their mental well-being.
Perinatal Depression
Perinatal depression is a common issue for women during pregnancy and after giving birth. It makes them feel sad, anxious, and even think about harming themselves or their baby. It's important to get help from a professional to deal with this.
Menopause and Mental Health
Going through menopause can also make women feel anxious, moody, and depressed. These feelings come from the big hormonal changes they go through. Women facing these mental health issues should talk to their doctors about how to handle them.
It's key to understand how life events and hormonal shifts affect women's mental health. Knowing the risks and getting the right support helps them get through tough times better.
Impact of COVID-19 on Women's Mental Health
The COVID-19 pandemic has deeply affected women's mental health. Women are often frontline healthcare workers and do more unpaid care work. They also work in low-paid and insecure jobs, making them more likely to face mental health issues.
Studies show the pandemic has made gender disparities worse. Women now have higher rates of depression, anxiety, and stress than men. This is because they handle household duties, childcare, and eldercare more, especially during lockdowns.
The economic effects of the pandemic have also been tough on women. Many have lost their jobs or seen their work hours cut. This financial stress adds to their mental health problems, causing feelings of isolation and hopelessness.
Women are also facing more domestic violence and abuse during the pandemic. Lockdowns make it harder for victims to get help, making their mental health worse.
The COVID-19 pandemic has had a big impact on women's mental wellbeing. We need to focus on their unique challenges to support their mental health and resilience.
Protecting and Improving Women's Mental Health
Keeping women's mental health safe and improving it is key to their overall health. Getting help from professionals and taking care of oneself are two main ways to do this. These steps are crucial for protecting and enhancing mental health.
Seeking Professional Help
Talking to mental health experts like therapists or counselors is very helpful. They offer treatments like therapy and sometimes medication for mental health issues. This support helps women find ways to cope, lessen symptoms, and improve their mental health.
Self-Care Strategies
Women can also help their mental health by taking care of themselves. This means keeping up with friends and family, staying active, and managing stress well. Self-care helps improve mental wellbeing and makes women stronger against mental health challenges.
- Maintain social connections with family and friends
- Engage in regular physical activity, such as yoga or walking
- Practice stress management techniques, like meditation or deep breathing
- Prioritize self-care activities that bring joy and relaxation
By using both professional help and self-care, women can actively work on their mental health. This leads to better overall wellbeing.
Mental Health and Poverty
Poverty greatly affects women's mental health. Studies reveal that women in poverty often face depression and anxiety. In fact, 29% of these women struggle with these issues, while only 16% of those who are not poor do.
Poverty and mental wellness are closely linked. Women in poverty often lack healthcare access and face high stress levels. These factors can lead to mental health problems. Women who have faced abuse are especially at risk.
It's vital to address poverty and women's mental health together. By understanding their challenges, we can help. This means improving mental health services, tackling community barriers, and fighting the stigma of mental illness through education.
To solve this issue, we need a comprehensive plan. By focusing on the economic factors, we can help women improve their mental health. This will strengthen our communities as a whole.
Women's Mental Health and Race/Ethnicity
Women from different racial and ethnic backgrounds face unique mental health challenges. Black, Asian, and Minority Ethnic (BAME) women often deal with racism and stigma. These issues can make mental health problems worse.
Research shows that BAME women have higher rates of mental health issues like depression and anxiety. This shows we need to focus on their mental health needs. We must provide support that fits their cultural backgrounds.
Things like income level, healthcare access, and beliefs about mental health affect BAME women's mental health. We must tackle these issues to improve their well-being. This ensures all women get the support they need to do well.
Understanding and meeting the mental health needs of women from various racial and ethnic groups is key. This approach helps create a fair and welcoming society. It ensures all women, no matter their race or ethnicity, can get the help they need for good mental health.
Mental Health Issues in Young Women and Girls
Mental health is a big concern for young women and girls. In fact, 75% of mental health problems start before they turn 24. Young women often face more mental health issues than young men.
Self-Harm and Suicide Rates
Self-harm and suicidal thoughts are rising among young women. They are more likely to harm themselves and try to take their own lives than young men. This shows that mental health problems are hitting this group hard.
Common Mental Disorders
Young women also struggle with anxiety and depression more often. These issues can really affect their life, like their school work, friends, and happiness. It's important to help them deal with these problems so they can do well.

We need to understand the challenges young women and girls face to help them. Knowing about self-harm, suicide, and common mental disorders helps us make better support plans. This way, we can make a safer and more caring place for their mental health.
Women's mental health
Women's mental health needs a full and caring approach. They deal with special challenges that affect their feelings, like hormonal shifts and social and economic issues. By knowing the mental health issues women often face and the reasons behind them, we can make plans to help them feel better.
Supporting women's mental wellness means looking at their physical, emotional, and social needs. We must see how big life events like pregnancy, childbirth, and menopause affect their mental health. It's also key to look at how social and economic issues like gender bias, domestic violence, and poverty play a part.
To protect and boost women's mental health, we need a wide-ranging strategy. This means helping women get professional help when they need it and supporting self-care like mindfulness, exercise, and being with friends. By helping women put their mental health first, we can help them deal with their unique challenges and feel better overall.
Looking after women's mental health is key to their full well-being and helping them do well in life. By taking a full approach, we can really help improve the mental health and strength of women from different backgrounds and experiences.
Conclusion
Women's mental health is a key issue that needs more focus and support. We must understand the mental health challenges women face and the factors that affect their well-being. By doing so, we can improve their mental health and resilience.
Key points from the discussion highlight how mental disorders affect women more than others. They deal with hormonal changes and life events that make things harder. It's important to offer healthcare and support that fits their needs.
Addressing gender, socioeconomic status, and race/ethnicity is key to giving women equal mental health care. This approach ensures services are comprehensive and fair.
Putting women's mental health first helps everyone. It makes communities healthier and more prosperous. By creating a supportive environment, we help women succeed and build a fairer society.
FAQ
What are the common mental health issues that affect women?
Women often deal with mental health issues like depression and anxiety. They also face unique challenges due to hormonal changes. This includes perinatal depression and premenstrual dysphoric disorder.
Why is women's mental health important?
Mental health issues are more common in women than men. They face special challenges linked to hormonal changes. It's key to understand these issues to support women's well-being.
What are the symptoms of mental disorders in women?
Women with mental health issues may show emotional, psychological, and social problems. It's important to recognize these symptoms to get the right support.
What are the risk factors that affect women's mental health?
Factors like being a caregiver or living in poverty can hurt women's mental health. Women often face these issues more than men. This can lead to depression, anxiety, and PTSD.
How do major life events and hormonal changes affect women's mental health?
Big life events like pregnancy and menopause can really affect women's mental health. Issues like perinatal depression are common during these times.
How has the COVID-19 pandemic affected women's mental health?
The COVID-19 pandemic has hit women's mental health hard. Women are often frontline healthcare workers or do unpaid care work. This increases their risk of mental health issues.
How can women protect and improve their mental health?
Women can boost their mental health by getting professional help and practicing self-care. This includes talking to therapists, taking medication, and keeping up social connections.
How does poverty affect women's mental health?
Poverty can really hurt women's mental health. 29% of poor women suffer from mental health disorders, compared to 16% of those who are not poor. Abuse adds to this risk.
How do race and ethnicity impact women's mental health?
BAME women face extra challenges that affect their mental health, like racism and stigma. They have higher rates of mental disorders than White British women. We need to tackle these disparities.
What mental health issues are young women and girls particularly vulnerable to?
Young women and girls are at high risk for mental health problems. By age 24, 75% of mental health issues start. They're more likely to experience self-harm, PTSD, and common disorders like anxiety and depression than young men.
Source Links
Statistics on Women's Mental Health: Understanding the Data
Have you ever wondered why more women seem to struggle with sadness, anxiety, or stress? What’s really going on under the surface?
In this blog, statistics on women's mental health shine a clear light on trends that matter, especially for mothers, sisters, daughters, and friends.
In this blog, we will explore real numbers and stories so you can see why these statistics on women's mental health need our full attention.
The Prevalence of Mental Health Issues among Women
Women's mental health statistics show a concerning trend. Women often face higher rates of mental health issues than men. This calls for more awareness and support for women's mental health challenges.
Anxiety and Depression Rates
Women are twice as likely to get anxiety as men. Also, one in five women has a mental disorder, while one in eight men do. This shows women are more affected by mental health problems.
Common Mental Disorders in Young Women
Young women face a high risk of mental health issues. Over a quarter (26%) of young women aged 16-24 have a mental health problem. This is almost three times the rate for young men.
Young women are the most at risk for mental illness. 25.7% have self-harmed, more than twice the rate for young men. These numbers highlight the need to focus on mental health support for young women.
Age-Based Breakdown of Mental Health Challenges in Women
| Age Group | Key Mental Health Concerns | Notable Statistics |
| Teens (12–17) | Depression, self-harm, anxiety | 26% with common disorders; 25.7% report self-harm |
| 30s–40s | Burnout, work-family stress, anxiety | Peak anxiety, high chronic stress |
| Elderly (60+) | Isolation, dementia, depression | Higher years lived with mental disability |
How does Violence and Abuse Impact on Women's Mental Health
Women's well-being is closely linked to their experiences of violence and abuse. Sadly, studies show a strong connection between their mental health and the traumas they go through.
Abuse and Mental Health Problems
Over half (53%) of women with mental health issues have also faced abuse. This shows how violence deeply affects a woman's mental and emotional health.
Trauma, PTSD, and Self-Harm
Abuse's impact goes even deeper. Almost three-quarters (78%) of women who faced severe physical and sexual violence have had life-threatening trauma. About 16% have PTSD. Sadly, over a third (36%) have tried to take their own lives, and a fifth (22%) have harmed themselves.
The connection between women's mental health and abuse is clear. We must address this issue and support survivors fully. This is key to empowering women and improving their well-being.
Barriers to Mental Health Support in Women
| Barrier Type | Key Statistics and Issues | Source |
| Stigma and Cultural Norms | Lower treatment usage among minority women | KFF, CDC |
| Financial / Geographic Access | Poor access in rural and lower-income areas | UN Women |
| Therapy and Medication Gaps | Hispanic women least likely to continue treatment | SAMHSA, MHA |

Mental Health and Poverty: The Connection for Women
Poverty has a big effect on women's mental health. Studies show a strong link between women's mental health and poverty. Women in poverty often face mental health issues, with 29% reporting disorders. This is compared to 16% of women who are not poor.
For women in poverty who have been abused, the situation gets worse. They are more likely to have poor mental health. This shows how poverty, abuse, and mental health are linked.
Helping women in poverty with their mental health is key. It helps them live better lives, keep healthy relationships, and join in community activities. By tackling this issue with strong, evidence-based plans, we can help women beat their challenges and improve their mental health.
Read: Best Vitamin Supplements for Women: Essential Nutrients for Optimal Health
COVID-19 Impact on Women’s Mental Health
| Factor | Impact | Source |
| New Cases of Anxiety (2020) | 52 million additional globally | WHO COVID-19 Impact Report |
| New Cases of Depression (2020) | 35 million additional globally | WHO COVID-19 Impact Report |
| Job Loss in Early Pandemic (US) | 11.5 million women vs 9 million men | McKinsey |
| Emotional Distress in Lockdown | 27% of women vs 10% of men reported serious distress | Pew Research Center |
Statistics on women's mental health: Disparities Among Minority Groups
Women from different backgrounds face mental health challenges, but some groups have it harder. Black, Asian, and minority ethnic (BAME) women in the U.S. deal with extra barriers. These can really affect their mental health.
Mental Health Challenges for Minority Women
Research shows BAME women often face big mental health issues. For example, 29% of Black women, 24% of Asian women, and 29% of mixed-race women have a common mental disorder. This is more than White British women (21%) and White other women (16%). These numbers show the special mental health struggles minority women go through.
- Racism and Stigma: BAME women often face more racism, discrimination, and social stigma. This can lead to more stress, anxiety, and depression.
- Socioeconomic Factors: Minority women are more likely to be poor and have less access to healthcare. These issues can hurt their mental health.
- Cultural Barriers: Some cultural beliefs in minority communities might make talking about mental health taboo. This makes it harder for women to get help and support.
We need a complete, community-focused plan to tackle these mental health issues. We must work to remove barriers and offer care that fits the culture of minority women. This way, we can help all women focus on their mental health and get the support they deserve.
Top Causes of Mental Illness in Women
| Cause | Impact and Findings | Source |
| Domestic Violence | 53% of mentally ill women experienced abuse | National Domestic Violence Hotline |
| Trauma and PTSD | 2x more likely PTSD rates in women | APA Trauma Research |
| Eating Disorders | Co-occur with anxiety/depression in 80% of cases | NIH |
Reproductive and Maternal Mental Health Concerns
Women go through many stages in their reproductive lives. Each stage brings its own mental health challenges. These issues, like premenstrual disorders, infertility, and postpartum depression, need our focus and understanding.
Premenstrual Dysphoric Disorder (PMDD)
About one in 20 women deal with Premenstrual Dysphoric Disorder (PMDD). It's a severe form of PMS that can really get in the way of life. PMDD brings on mood swings, irritability, anxiety, and depression before a woman's period.
Infertility, Baby Loss, and Postnatal Depression
Trying to become a mom can be tough on mental health. Infertility and losing a baby can make people feel hopeless and sad. Postpartum depression hits more than one in ten women in the first year after having a baby. It can make it hard to bond with the baby and connect with others.
It's important to tackle these reproductive and maternal mental health issues. We need to support women during these important times in their lives.
Read: Breastfeeding and Postpartum Depression: What You Should Know | Dr. Chandril Chugh
Recognizing Women's Strength and Resilience
Women face big challenges, but we must see their strength and resilience. Inspirational women like former First Lady Michelle Obama share wisdom on beating adversity. She said, "There is no limit to what we, as women, can accomplish." This message of empowerment helps women deal with mental health issues and reach their goals.
Women show great resilience by adapting and thriving despite challenges. A study by the Female Quotient and Cisco found many working women feel resilient in their jobs and personal lives. Women in top positions and over 45 feel especially resilient.
Being resilient is key to feeling happy at work and taking care of oneself. Women who focus on their mental health are more resilient. Creating a supportive work culture helps women's mental health and lets them shine.

Leaders are vital in making a supportive work place. Companies should focus on empathy, teamwork, and supporting workers. By valuing women's strength and resilience, we can build a fair and empowering future for everyone.
Addressing the Stigma and Barriers to Care
It's important to reduce stigma in women's mental health to help them get the support they need. Women often face barriers like societal biases and a lack of affordable, culturally-competent services. By spreading awareness and encouraging open talks, we can fight the shame and misunderstandings that stop women from caring for their mental health.
Improving Access to Mental Health Support
Women need access to mental health support that understands their needs. This means more telehealth options, more female providers, and mental health screenings during regular doctor visits. Consulting with experienced neurologists like Dr. Chandril Chugh can also help spot and treat mental health issues linked to neurological conditions.
To really help women get the mental health support they need, we must tackle the big barriers that have stopped them from focusing on their well-being. By working together to lessen stigma and make trauma-informed, culturally-responsive services more available, we can help women take control of their mental health and get the support they deserve.
- Increase awareness and understanding around the severity of mental health challenges women face
- Invest in specialized, trauma-informed mental health services for women
- Provide more accessible and gender-sensitive support options
- Integrate mental health screenings into routine medical visits
- Consult with experienced neurologists to address underlying neurological conditions
Conclusion: Empowering Women's Mental Well-being
Women's mental health is a big concern, and we need to act. We must support and empower women for their well-being. By tackling mental health issues, addressing violence, and focusing on women's unique challenges, we can make things better.
We need to break down the stigma around mental health and make support services more accessible. Women should feel safe to get the help they need without facing judgment or obstacles. With teamwork and a comprehensive approach, we can improve women's mental health solutions and make strategies for improving women's mental health work.
Putting the mental health of women first helps them and our communities too. Let's celebrate and support women's mental health. Together, we can build a future where mental health is valued by all.
FAQ
How prevalent are mental health issues among women?
Women are twice as likely to have anxiety as men. One in five women have a mental disorder, compared to one in eight men. Young women aged 16–24 show that over a quarter have a common mental health problem.
What is the connection between women's experiences of violence and abuse and their mental health?
53% of women with mental health issues have also faced abuse. Most women who have been physically and sexually abused have gone through trauma. This trauma can lead to PTSD in 16% of them.
Over a third of these women have tried to take their own life. A fifth have self-harmed.
How does poverty impact women's mental health?
Women living in poverty often have poor mental health. 29% of these women have a common mental disorder, compared to 16% of those who are not poor. Abuse adds to the mental health struggles of poor women.
What mental health challenges do minority women face?
Minority women face racism and stigma, making their mental health harder. Black, Asian, and Minority Ethnic women are more likely to have mental disorders. For example, 29% of Black women and 24% of Asian women have these disorders.
What are some of the unique reproductive and maternal mental health concerns women face?
About one in 20 women suffer from Premenstrual Dysphoric Disorder (PMDD), a severe PMS. Infertility and losing a baby can deeply affect mental health. Over 10% of women feel hopeless and grieve in the first year after having a baby.
Source Links
Exploring Mental Health in Women: Key Issues and Insights
Your mental health is key to your overall well-being. Yet, it's often overlooked, especially for women. Women face unique challenges and are more likely to struggle with mental illness than men. In fact, 1 in 5 women deal with a mental illness, while 1 in 8 men do.
But, your symptoms are often ignored by doctors. You also face big hurdles in getting good mental health care.
This article will look into the main issues and offer insights to help your mental health. We'll talk about how common mental health problems are in women, the stigma and barriers to getting care, and the mental health challenges you might face.
We'll also look at gender-specific risks and stressors, cultural views, the effects of discrimination and gender-based violence, and ways to improve mental wellness throughout your life.
By understanding women's mental health challenges, we can create a supportive environment. This way, you can focus on your mental health and get the support you need. Let's start this important journey together, exploring mental health in women and finding insights for a healthier future.
Women's Mental Health: An Overlooked Crisis
Women's mental health issues are often ignored in our society. Many women suffer from anxiety, depression, and PTSD more than men. This is not just because of biology, but also because of societal pressures and gender discrimination.
Prevalence and Impact of Mental Health Issues in Women
Women are more likely to deal with mental health problems, like clinical depression, at nearly double the rate of men. These issues deeply affect their lives, impacting relationships, work, and overall happiness. Sadly, the stigma around mental illness stops many women from getting help.
Societal Stigma and Barriers to Accessing Care
Many women face big hurdles when trying to get mental health care. Stigma, dismissive doctors, and a lack of services that understand different cultures make it hard. Money issues and other responsibilities also stop women from focusing on their mental health.
We need to tackle the big issues that cause the mental health crisis in women. By removing barriers and fighting stigma, we can help women take control of their health. This will make our society more supportive and inclusive for everyone.
Common Mental Health Challenges Faced by Women
Women's mental health is a big concern. Anxiety and depression are common among them. Women are almost twice as likely to have these issues as men. This difference can come from hormonal changes, societal pressure, and stress that affects women more.
Anxiety and Depression: Higher Rates Among Women
Anxiety and depression often go hand in hand. Women deal with these conditions a lot. Hormonal changes during the menstrual cycle, pregnancy, and menopause can make mood swings and emotional ups and downs.
Women also face high expectations from society. They have to balance work, family, and home life. This can lead to stress and burnout, making mental health problems worse.
Trauma, Stress, and Post-Traumatic Stress Disorder
Women are more likely to go through traumatic events like gender-based violence, sexual assault, and domestic abuse. These events can lead to PTSD, a serious condition with symptoms like flashbacks and anxiety. The stress and emotional burden women deal with daily can also hurt their mental health.
It's important to understand the mental health challenges women face. Knowing about these issues helps us offer better support and resources. This can help women feel empowered and improve their mental well-being.
mental health in women
Women's mental health is complex, influenced by biology, psychology, and society. Many mental health issues affect both men and women. But women often face special challenges that make their mental health worse. It's important to understand women's mental health to help them.
Anxiety and depression are big problems for women. They're more likely to have these conditions. This is due to societal pressures, hormonal changes, and daily stress.
Women are also more likely to have trauma, stress, and PTSD. Things like conflicts, relationship issues, and gender-based violence can cause these problems.
- Women often face stigma and barriers when trying to get mental health help.
- Culture can affect how women see and deal with their mental health, sometimes showing up as physical symptoms.
To help women's mental wellbeing, we need a wide-ranging approach. This means creating special programs, reducing stigma, and making help easy to get.

Understanding mental health challenges for women helps us help them better. By taking a full approach to their health, we can make their lives better.
Gender-Specific Risk Factors and Stressors
Women face unique challenges that deeply affect their mental health. These include the complexities of relationships, work-life balance, and caregiving. These factors can lead to more stress, anxiety, and depression.
Interpersonal Conflicts and Relationship Dynamics
Women's mental health is closely linked to their relationships. Dealing with family, romantic partners, and friends can be stressful. Conflicts or power imbalances add to the stress, especially the emotional and social pressures.
Caregiving Responsibilities and Work-Life Balance
Women often carry a heavy load in caregiving, whether it's for kids, parents, or others. Balancing work, home, and caregiving can cause burnout and overwhelm. This constant juggling is a big stress and anxiety source for many women.
It's important to support women in these areas to improve their mental health. By understanding their challenges and offering specific help, we can help them manage these issues better. This way, women can focus on their mental health.
Cultural and Ethnic Perspectives on Women's Mental Health
Women's mental health is shaped by the cultural norms and beliefs of their communities. In some cultures, mental illness is seen as shameful or a sign of weakness. This can make women hesitant to get help and may cause them to show mental health issues through physical symptoms.
Influence of Cultural Norms and Beliefs
It's important to understand cultural differences to help women with mental health issues. Some cultures believe mental health problems show personal weakness or divine punishment. This makes it hard for women to talk about their mental health openly.
Traditions and gender roles can also limit women's freedom and access to help, making mental health issues worse.
Somatization and Manifestation of Mental Health Issues
In many ethnic communities, mental health problems are shown through physical symptoms. Women might say they have headaches, stomach issues, or chronic pain instead of talking about their feelings. This makes it hard for doctors to see and treat the mental health issues.
Healthcare workers need to understand the different cultural views on women's mental health. This helps them see the unique challenges women from different backgrounds face. It can lead to better mental health care that helps women get the support they need and reduces the stigma around mental health.
The Impact of Discrimination and Gender-Based Violence
Gender discrimination and violence deeply affect women's mental health. They can make women feel left out, lower their self-esteem, and increase stress. Violence like domestic abuse and sexual assault can cause serious mental health issues. These include post-traumatic stress disorder (PTSD), depression, and anxiety.
It's vital to tackle these big issues and support survivors fully. We need to give them counseling, housing, childcare, legal help, and job chances. We must also work to end the stigma around mental health and offer support without judgment.
The effects of discrimination and violence on women's mental health are huge. By tackling these problems, we can help create a fairer and supportive world for women. This will help them do well in both their mental and physical health.

Remember, the harm from gender-based discrimination and violence goes beyond mental health. It can also affect their physical. We must look at how gender, mental health, and physical health connect. This is key to supporting women's full health and well-being.
Addressing Mental Health Needs Across the Lifespan
Women's mental health changes as they grow older. It's key to offer support at important life stages. For example, teenage girls face special mental health issues like anxiety and body image worries.
The time around pregnancy and after childbirth is also crucial for women's mental health. Many new moms struggle with postpartum depression. It's vital to help them during these times.
Adolescent Mental Health and Body Image Concerns
Being a teenager can be tough for girls' mental health. They deal with big changes in their bodies and feelings. Issues like anxiety, depression, and worries about how they look are common.
It's important to give teens the right help and support. This includes easy-to-use resources and ways to take care of themselves. This can help them stay mentally healthy.
Perinatal Mental Health and Postpartum Depression
The time before and after having a baby is very important for women's mental health. Many new moms feel postpartum depression. We need to make it okay to talk about these feelings.
It's crucial to make sure new moms get the help they need. Early support and good care can really help women feel better during this time.
Strategies for Promoting Mental Well-Being in Women
Women's mental health can be tough to handle, but there are ways to help. By focusing on self-care and managing stress, and building a strong support network, you can get better. These steps can make you feel stronger and healthier.
Importance of Self-Care and Stress Management
Looking after your mental health means putting your needs first. Start with self-care activities that feed your mind, body, and spirit. This includes:
- Practicing mindfulness or meditation to reduce stress and anxiety
- Engaging in regular exercise to boost mood and energy levels
- Ensuring adequate sleep and maintaining a balanced diet
- Exploring creative outlets like art, music, or journaling
Adding these strategies to your daily life can help you cope better and feel better overall.
Building Supportive Communities and Destigmatizing Mental Health
Having a circle of supportive people is key to your mental health journey. Talk to family, friends, or groups to share your feelings and find strength. Also, fighting the stigma around mental health makes it easier for women to get help.
By embracing self-care, managing stress, and valuing community, you can improve your mental health. This approach helps create a supportive space for all women.
Mental Health Resources and Support Services
Women face many mental health challenges. It's key to have resources and support. These tools help you take control of your well-being and get the help you need.
If you're dealing with anxiety, depression, trauma, or other mental health issues, there are many mental health resources for women out there. You can find therapy, counseling, support groups, and online communities. These services offer the guidance, understanding, and care you deserve.
Accessing Mental Health Support
Therapy is a crucial support service for women's mental health. Qualified therapists help you understand your feelings, develop coping strategies, and work towards healing. Many therapists offer affordable, evidence-based, and culturally-responsive care tailored to your needs.
Support groups are also a great resource. They connect you with others who get what you're going through. This can make you feel less alone and build a sense of community. These groups focus on specific issues like postpartum depression or survivors of abuse.
For those who prefer online options, there are many websites, apps, and virtual communities for women's mental health. These platforms provide information, self-care tools, and ways to connect with peers and professionals.
Remember, asking for help is a sign of strength, not weakness. By using the available mental health resources for women and support services for women's mental health, you can improve your well-being and build resilience.
Conclusion
Women's mental health is a big issue that needs our focus and action. We must understand the challenges, risk factors, and ways to support their mental health. This means tackling barriers, reducing stigma, and making sure care is culturally sensitive and trauma-aware.
By focusing on women's mental health, we help them live better lives. This benefits everyone, from families to society. The main points are clear: we need to keep spreading the word, pushing for change, and making sure women get the support they need.
Together, we can work towards a future where the conclusion on women's mental health is positive. We'll focus on progress, empowerment, and a society that cares for women's mental health. Let's use what we know to make a difference. Let's build a world that's fair, welcoming, and supports the mental health of all women.
FAQ
What are the key mental health challenges faced by women?
Women face more mental health issues than men, like anxiety and depression. Hormonal changes, societal pressure, and stress from relationships play a big role.
What are the barriers women face in accessing quality mental healthcare?
Women find it hard to get mental health help because of stigma and barriers. They might face dismissive attitudes from doctors, lack of care that fits their culture, and high costs.
How do gender-specific risk factors and stressors impact women's mental health?
Women deal with unique stress like conflicts in relationships and the heavy load of caring for others and working. This can hurt their mental health.
How do cultural and ethnic perspectives influence women's mental health?
Culture and ethnicity shape women's mental health a lot. In some cultures, mental health is seen as taboo, making women less likely to seek help.
What is the impact of discrimination and gender-based violence on women's mental health?
Discrimination and violence against women can make them feel left out and low in self-esteem. It can lead to serious mental health issues like PTSD and depression.
How can we promote mental well-being in women across different life stages?
We need to offer special support to women at different times in their lives, like when they're young, during pregnancy, and after having a baby. This helps them stay mentally healthy.
What are effective strategies for supporting women's mental health?
Helping women take care of themselves, manage stress, and have a strong support network is key. We should also work to reduce the stigma around mental health and make sure care is tailored to each woman's needs.
What mental health resources and support services are available for women?
Women can find many resources like therapy, counseling, and online groups to help with their mental health. These services should be affordable, fit their culture, and be based on solid evidence.
Source Links
- A Deeper Look: Women's Mental Health in the Workplace
- Perspectives on Global Women’s Mental Health
- Understanding and Nurturing Women's Mental Health | Thriveworks
5 Tips for Managing Sleep Apnea Insomnia
Sleep is key for your mind, body, and feelings. But, it's hard to get good sleep if you have obstructive sleep apnea (OSA). OSA makes you stop breathing for short times at night. This can lead to not getting enough sleep and increase your risk of serious health problems like heart issues and diabetes.
This article will share 5 tips to help you deal with sleep apnea insomnia. These tips can improve your sleep quality and help you take back control of your life.
Understanding Sleep Apnea and Insomnia
Sleep disorders like sleep apnea and insomnia can greatly affect your health and happiness. Knowing what causes and shows these conditions helps you find the right treatment and sleep better.
What is Sleep Apnea?
Obstructive sleep apnea (OSA) is a common sleep issue. It happens when your airway partly or fully blocks, making you stop breathing for short times at night. This blockage is due to your throat muscles relaxing, which keeps airways open.
OSA leads to waking up often, not sleeping enough, and health problems if not treated.
Causes and Symptoms of Sleep Apnea Insomnia
Symptoms of sleep apnea insomnia include feeling very tired during the day, having trouble focusing, memory issues, and loud snoring. Things that might make you more likely to have sleep apnea include being overweight, having a family history of it, drinking too much alcohol, and certain body features like a narrow airway or big tongue.

It's crucial to deal with sleep apnea and insomnia quickly. They can raise the risk of high blood pressure, heart disease, and stroke. By knowing the causes and signs of these sleep problems, you can work on better sleep and health.
Establishing a Consistent Sleep Schedule
Keeping a regular sleep schedule is key for those with sleep apnea insomnia. Try to go to bed and wake up at the same time every day, even on weekends. This helps your brain and body get into a routine, which leads to better sleep.
Importance of Sleep Hygiene
Good sleep hygiene can make a big difference in how well you sleep. Stay away from blue light from devices before bed, as it can mess with your sleep cycle. Instead, do calming things like reading, stretching, or meditation to get ready for sleep.
Creating a Relaxing Sleep Environment
Your bedroom's setup is key to good sleep. Make it cool, dark, and quiet for a calm space. Choose comfy bedding, like a supportive mattress and pillows, to help your body relax fully at night.

By sticking to a regular sleep schedule, following good sleep habits, and making your bedroom sleep-friendly, you're on the right path. These steps can help you manage your sleep apnea insomnia and boost your sleep quality.
Using a Continuous Positive Airway Pressure (CPAP) Machine
The best way to treat sleep apnea is with a CPAP machine. This device sends air pressure into the airway, keeping it open. It stops the throat from closing during sleep. It's important to find a CPAP mask and machine that fit you well for the best results.
CPAP machines have many options, like auto-adjusting pressure and different settings for breathing in and out. They also have special features for different types of sleep apnea. Using your CPAP machine every day, even when you're traveling or taking naps, is key to keeping your airways open.
Keeping your CPAP machine clean and replacing parts on time is crucial. The right CPAP mask, like nasal, nasal pillow, full-face, or hybrid, can greatly improve your comfort. This makes it easier to stick with the treatment.
Working with your doctor or sleep specialist is important for using your CPAP correctly. They can help with issues like mask leaks, skin irritation, or trouble falling asleep with the mask on.
With the right CPAP and consistent use, you can manage your sleep apnea well. This improves your sleep quality and lowers the risks of breathing problems.

Optimizing Sleep Positioning
Your sleep position can greatly affect sleep apnea and snoring. [https://drchandrilchugh.com/blog/ways-to-reduce-stress-amidst-hectic-lifestyle/] Sleeping on your side is best because it lessens apnea and snoring.
Benefits of Side Sleeping
Sleeping on your side is good for those with sleep apnea. It keeps your airways open and lowers the chance of blockage. Studies link side sleeping to fewer sleep apnea episodes.
Stomach and Back Sleeping Considerations
Sleeping on your stomach can be good, but make sure your neck is in line with the right pillow. Avoid sleeping on your back if you can, as it might make sleep apnea worse. If you must sleep on your back, try using a wedge pillow or an adjustable bed frame to keep your airways open.

Finding the right sleep position is key to managing sleep apnea and snoring. Try different positions and talk to your healthcare provider for advice.
Exploring Dental Appliances for Sleep Apnea
For people with mild to moderate sleep apnea, dental appliances can be a good choice instead of CPAP therapy. These custom mouthguards, like MADs or TSDs, move the lower jaw forward slightly. This helps keep the airway open by tightening the throat muscles and tissues during sleep.
CPAP is the top treatment for sleep apnea, but dental appliances are an option for those who find CPAP hard to use or uncomfortable. Research shows MADs can cut down on breathing stops, snoring, and daytime sleepiness. TSDs also help reduce breathing pauses and make people feel less tired during the day.
About 90% of sleep apnea patients prefer MADs over TSDs, showing they are easier to use and more comfortable. For kids with sleep apnea, RME devices often help reduce symptoms and even cure it in some cases. Combining surgery with RME has been shown to work better than just one treatment alone.
Even though CPAP is the main treatment for sleep apnea, dental appliances are a good alternative for those looking for something more comfortable. With help from a dentist, people can see how these custom devices can help manage sleep apnea and improve their life quality.
Choosing the Right Pillow and Mattress
Finding the right pillow and mattress is key for those with sleep apnea insomnia. The right sleep setup can ease symptoms, boost sleep quality, and offer comfort.
Pillow Selection for Different Sleep Positions
Your pillow should match your sleep position. Side sleepers do well with a thick pillow that keeps the neck aligned and reduces shoulder pressure. Back sleepers might like a thinner pillow, while stomach sleepers should choose an even thinner one for spinal alignment. CPAP users might prefer pillows with special indents for the mask.
Mattress Considerations for Sleep Apnea
A supportive mattress that fits your sleep position can ease pressure points and enhance sleep quality. Mattresses last about 10 years, making them a big investment in your sleep. If your mattress is over a decade old and doesn't support you well, it's time for a new one.

Choosing the right pillow and mattress can greatly improve sleep for those with sleep apnea insomnia. Tailoring your sleep setup to your needs can lead to better sleep and health.
Humidifying Your Bedroom
Keeping the right humidity in your bedroom is key for good sleep, especially if you use a CPAP machine for sleep apnea. Dry air can make sleep apnea worse, causing discomfort and problems with your CPAP therapy. A humidifier can help by keeping your mouth and throat moist.
Importance of Humidity for CPAP Users
Many CPAP machines have built-in humidifiers. But, some people might need an extra humidifier in their bedroom. This ensures the air stays moist, preventing dryness in dry places. It's important to clean your humidifier often to stop mold and bacteria from growing, which can harm your sleep.
The Environmental Protection Agency says the best humidity for sleeping is 40% to 60%. This range helps you sleep comfortably without dry or too humid air bothering you.

Adding a humidifier to your bedtime routine can make your sleep better and support your CPAP therapy. This easy step can greatly improve your sleep quality and health, helping you manage sleep apnea better.
Making Lifestyle Changes for Better Sleep
Healthy habits can make sleep apnea symptoms better. Keeping a healthy weight with a balanced diet and exercise helps. This is because extra fat can block the airways, making sleep apnea worse.
Even kids can get sleep apnea. It's more common in obese adults because of fat blocking the airways.
Weight Management and Exercise
Weight loss, especially around the neck, can help breathing during sleep. Exercise improves sleep quality and oxygen levels. It also makes sleep apnea symptoms less severe.
Studies show exercise is good for people with sleep apnea.
Avoiding Alcohol and Smoking
It's important to avoid alcohol and quit smoking. These habits can make snoring and poor sleep worse. Alcohol affects the muscles in the upper airway and can lead to weight gain.
Experts suggest not drinking alcohol for 3 to 4 hours before bedtime. Smoking is more common in people with sleep apnea, but the exact link is still being studied.
By making lifestyle changes like managing weight, exercising, and avoiding alcohol and smoking, sleep quality can improve for those with sleep apnea.

Trying Alternative Therapies
If you're having trouble sleeping because of sleep apnea, you might look into other treatments. Traditional methods like CPAP machines and dental devices work well. But, some other ways might also help.
Playing Wind Instruments and Singing
Playing wind instruments and singing could be an interesting option. These activities require special breathing skills. This can make the muscles in your upper airway stronger, which might lessen sleep apnea symptoms.
For example, playing the didgeridoo, a wind instrument from Australia, has helped some people sleep better. It made them feel less tired during the day and reduced apnea episodes.
Even though there's not much proof, trying these methods might be helpful along with your usual treatments. Always talk to your doctor before starting any new therapy. They can tell you about the good and bad parts.
- Herbal remedies like valerian, chamomile, and
- Acupuncture and relaxation techniques such as meditation and yoga
- CBD and cannabis products
- Sleep hypnosis
Always talk to your doctor before trying any new therapies. This makes sure they're safe and right for you.
Sleep apnea insomnia
Sleep apnea and insomnia often go together. The breathing stops and sleep issues from sleep apnea can cause chronic insomnia. [https://www.verywellhealth.com/insomnia-vs-sleep-apnea-5213997] It's important to find and fix the sleep apnea to improve sleep quality and daily life.
Health conditions, medicines, and lifestyle can lead to sleep apnea insomnia. Working with a doctor to find and manage these factors is key to solving the problem.
Diagnosing Sleep Apnea Insomnia
Doctors use questionnaires, sleep diaries, and actigraphy to diagnose insomnia and sleep apnea. A full check-up is needed to see if someone has both insomnia and sleep apnea (COMISA).
- Chronic insomnia affects roughly 1 in 3 people.
- 25–30% of men have sleep apnea, alongside 9–17% of women.
- Any individual who has either insomnia or sleep apnea has a 30–50% chance of having the other condition.
Treating Sleep Apnea Insomnia
Treating sleep apnea insomnia needs a full approach. Changing lifestyle habits, like keeping a regular sleep schedule and having a calming bedtime routine, can help. CPAP therapy might not work well for everyone, so other treatments like dental appliances could be used.
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a good treatment for those with COMISA. It helps with the mental issues that cause insomnia. It's important to work with a healthcare provider to get a treatment plan that covers both sleep apnea and insomnia.
Seeking Medical Treatment
If your sleep apnea symptoms don't get better or get worse, you should see a doctor. Talk to a healthcare provider, like a sleep specialist. They can check you out and suggest the best treatment.
When to Consult a Doctor
You should think about seeing a doctor if you notice any of these signs:
- Loud, frequent snoring that disrupts your sleep or your partner's sleep
- Daytime fatigue or sleepiness that interferes with your daily activities
- Difficulty breathing or gasping for air during sleep
- Frequent nighttime awakenings or difficulty staying asleep
- High blood pressure or other cardiovascular issues
Treatment Options for Sleep Apnea
Your doctor might suggest different ways to help with your sleep apnea, such as:
- Continuous Positive Airway Pressure (CPAP) devices to keep airways open while you sleep
- [Oral appliances] that move the jaw or tongue to stop airway blockage
- Surgical treatments to fix issues that cause sleep apnea
Getting diagnosed and treated early is key to avoiding serious health problems from sleep apnea.
Conclusion
Managing sleep apnea insomnia means making changes in your life, getting medical help, and trying new therapies. Start by keeping a regular sleep schedule. Use a CPAP machine as directed and sleep in a way that helps you breathe better. Also, choose healthy habits to fight sleep apnea insomnia and get back to good sleep.
Working with your doctor is key to beating sleep apnea insomnia. Together, create a plan that fits your specific needs. With the right approach and support, you can sleep better, feel healthier, and lower the risks linked to sleep problems.
Finding better sleep might take time and effort, but you can do it. Stay committed and try different ways to tackle sleep apnea insomnia. Putting your sleep first and taking steps to manage it can greatly improve your health and happiness.
FAQ
What is sleep apnea?
Obstructive sleep apnea (OSA) is a sleep disorder. It happens when the airway partly or fully blocks. This causes you to stop breathing for short periods at night.
What are the symptoms of sleep apnea insomnia?
Symptoms include feeling very tired during the day, trouble focusing, and memory issues. You might also snore loudly.
How can I establish a consistent sleep schedule?
It's important to keep a regular sleep schedule. Try to go to bed and wake up at the same time every day. This helps your body and brain get into a healthy sleep cycle.
What is a CPAP machine and how does it help with sleep apnea?
A CPAP machine is a key treatment for sleep apnea. It sends air pressure into your airway to keep it open. This stops your throat from closing during sleep.
How does sleep positioning affect sleep apnea?
Sleeping on your side is best for sleep apnea. It helps lessen apnea and snoring. Sleeping on your stomach can also help, but back sleeping might make it worse.
Can oral appliances be used to treat sleep apnea?
Yes, for mild to moderate sleep apnea, oral devices can be an option instead of CPAP. These devices move your lower jaw forward to open your airway at night.
How can the right pillow and mattress help with sleep apnea?
The right pillow and mattress can greatly improve sleep apnea. Side sleepers need a thick pillow for neck alignment and comfort. CPAP users might prefer special pillows designed for their devices.
How can a humidifier help with sleep apnea?
A humidifier can make your bedroom more comfortable for sleep apnea and CPAP users. Dry air can make your mouth and throat dry, which can be uncomfortable and affect your CPAP therapy.
What lifestyle changes can improve sleep apnea symptoms?
Healthy habits can help with sleep apnea. Eating well and exercising can reduce sleep apnea severity. Avoiding alcohol and quitting smoking is also key to better sleep quality.
Can alternative therapies help with sleep apnea?
Yes, activities like playing wind instruments and singing might help with sleep apnea. These activities strengthen your upper airway muscles, which can lessen sleep apnea symptoms.
When should I seek medical treatment for sleep apnea?
If your symptoms don't get better or get worse, see a doctor. A sleep specialist can check you and suggest the right treatment.
Source Links
- Healthy Tips for Sleeping Better with Sleep Apnea | Banner
- 20 Tips to Reduce Your Sleep Problems
- Sleep apnea - Diagnosis and treatment - Mayo Clinic
- Insomnia vs. Sleep Apnea: Symptoms, Diagnosis, Treatment
- Insomnia and Sleep Apnea - What Are They?
Effective Solutions for Extreme Sleep Apnea
If you're dealing with severe extreme sleep apnea, you're not alone. This condition means you stop breathing for long periods during sleep. It can lead to serious health issues if not treated. But, there are ways to manage and treat it.
This guide will cover diagnosis and treatment options for extreme sleep apnea. We'll look at CPAP therapy, oral appliances, surgery, and lifestyle changes. Knowing these options can help you get better sleep and improve your health.
If you're new to severe sleep apnea or have had it for years, this article is for you. It offers the info and advice you need to find the right treatment. By tackling this issue, you can sleep better and lower your risk of other health problems like heart disease, stroke, and diabetes.
Diagnosis of Extreme Sleep Apnea
Diagnosing extreme sleep apnea starts with a detailed look at your symptoms and sleep history. Your doctor will first do a physical exam and ask about your sleep patterns, snoring, and how tired you feel during the day. If they think you might have sleep apnea, you'll be sent to a sleep specialist for more tests.
Symptoms and Sleep History
To diagnose extreme sleep apnea, your symptoms and sleep history are checked first. Signs include loud snoring, gasping or choking while asleep, waking up often, and feeling very tired during the day. Your doctor will also ask about your sleep habits, like how long you sleep and how rested you feel in the morning.
Sleep Testing and Polysomnography
If your symptoms and sleep history point to possible extreme sleep apnea, your doctor will suggest a sleep study, or polysomnography. This test is done overnight in a sleep center and tracks your breathing, oxygen levels, heart rate, and more. The test results help figure out how severe your sleep apnea is and what treatment you need.
For some, a home sleep test might be an option to diagnose sleep apnea. These tests use portable devices to check your breathing and oxygen levels at home. But, a sleep study at a center is usually preferred if you might have central sleep apnea.
Treatment Options for Extreme Sleep Apnea
For those with moderate to severe sleep apnea, continuous positive airway pressure (CPAP) therapy is often the best choice. CPAP machines send a steady flow of air pressure. This keeps the airways open and stops apnea and snoring.
Continuous Positive Airway Pressure (CPAP) Therapy
CPAP therapy is the top treatment for extreme sleep apnea. It uses a mask or nosepiece to give a constant air pressure. This keeps the airways open all night, improving sleep quality. Studies show CPAP is very effective in handling sleep apnea symptoms.
Other Airway Pressure Devices
If CPAP doesn't work well, there are other options. Auto-CPAP adjusts the air pressure to match your breathing. Bilevel positive airway pressure (BPAP) gives more pressure when you breathe in and less when you breathe out.

The choice between CPAP and other devices depends on your sleep apnea severity, your preferences, and your doctor's advice. Getting the right treatment is key to lowering the risks of sleep apnea, like heart disease and stroke.
Oral Appliances for Extreme Sleep Apnea
For some people with mild to moderate sleep apnea, oral appliances can be an option instead of CPAP therapy. These devices are custom-made and prescribed by a dentist. They move the jaw forward to stop the tongue and soft tissues from blocking the airway while sleeping. They're not as powerful as CPAP for severe sleep apnea but can be easier for some patients.
Mandibular advancement devices (MADs) are the top choice for treating sleep apnea. They move the lower jaw forward to open the airway. For those who can't use MADs, tongue-stabilizing devices (TSDs) are an option.
- Custom-made oral appliances give the best results for sleep apnea, beating over-the-counter options.
- They work best for people with mild to moderate sleep apnea who can't use CPAP machines.
- Oral appliance therapy is less effective than CPAP but can still help some people.
It's key to know that oral appliances aren't right for everyone. They're not good for people with central sleep apnea, kids with breathing problems, or those with severe sleep apnea. Regular check-ins with a dentist or sleep expert are needed to see how well the device is working and to handle any side effects.

Surgical Interventions
When treatments like CPAP therapy or oral appliances don't work, surgery might be the last choice. These surgeries aim to fix the body parts that cause sleep apnea.
Tissue Removal and Shrinkage
Removing or shrinking throat tissue can help open up the airway. This includes uvulopalatopharyngoplasty (UPPP), which cuts the uvula and soft palate. Or laser-assisted uvulopalatoplasty (LAUP), which uses a laser to make the uvula and soft palate smaller.
Jaw Repositioning and Implants
Moving the jaw can also widen the airway. Maxillomandibular advancement moves the upper and lower jaws forward. Implants can also support the tongue, keeping it from blocking the airway at night.
Nerve Stimulation Procedures
- Hypoglossal nerve stimulation puts a device in to help keep the airway open by electrically stimulating the tongue muscles.
- Lingual tonsillectomy removes tissue at the base of the tongue to improve airflow.
Surgery for sleep apnea is usually a last choice but can help some people. It's important to think about the risks and benefits before deciding.

Therapies for Central Sleep Apnea
Central sleep apnea happens when the brain doesn't control breathing during sleep. It's different from obstructive sleep apnea, where the airway gets blocked. Treating this condition involves addressing health issues and trying special therapies.
Treating Underlying Medical Conditions
First, find and treat health problems that cause central sleep apnea. Issues like heart failure, stroke, kidney disease, and neurological disorders can lead to it. Fixing these problems can help improve sleep breathing.
Adaptive Servo-Ventilation (ASV)
Adaptive servo-ventilation (ASV) is a therapy for central sleep apnea. It watches your breathing and changes air pressure to keep it steady at night. This is great for people with heart failure or other conditions causing central sleep apnea.
Other treatments like continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BPAP) can also help. These devices support breathing and stop pauses during sleep.
Combining treatment for underlying conditions with therapies like ASV can greatly improve sleep and health. It's important to work with your healthcare team to find the best treatment for you.
Lifestyle and Home Remedies for Extreme Sleep Apnea
If you're dealing with extreme sleep apnea, making lifestyle changes and trying home remedies can help a lot. By focusing on your weight, exercise, and medication use, you can help manage your condition. This can also improve how well you sleep.
Weight Loss and Exercise
Carrying extra weight can make sleep apnea worse. Losing a few pounds through healthy eating and regular exercise can ease your symptoms. Activities like brisk walking, swimming, or strength training can also help.
These exercises strengthen your muscles that help you breathe. This makes it easier to breathe while you sleep.
Avoiding Alcohol and Certain Medications
Drinking alcohol and some medications, like sedatives, can relax your throat muscles. This can make sleep apnea worse. Try to limit or avoid these substances.
Instead, stick to a regular sleep schedule, use relaxation techniques, and live a healthy lifestyle. This can help reduce your symptoms.
By making these lifestyle changes and trying home remedies, you can take charge of your sleep apnea. This can also boost your overall health and well-being.

Extreme Sleep Apnea in Children
Sleep apnea is not just for adults; kids can have it too. It can be caused by big tonsils or adenoids, face shape issues, or other health problems. To treat it in kids, doctors use CPAP therapy, oral devices, and surgery to fix the root cause.
Kids with sleep apnea may snore, stop breathing, and have trouble sleeping. They might also be restless. If not treated, it can lead to high blood pressure, high cholesterol, and even prediabetes.
Some kids are more at risk, like those with Down syndrome or certain birth defects. Cerebral palsy and a family history of sleep apnea also increase the risk. In rare cases, it can cause growth problems or even death.
It's important to catch and treat sleep apnea early to help kids grow and learn well. About 7 to 11 percent of kids have a sleep disorder, but many might not know they have it. Around 1 to 5 percent of kids have obstructive sleep apnea, especially African American kids.
Treatments for kids with severe sleep apnea include CPAP machines, oral devices, losing weight, and surgery. Doctors might send kids for tests like a sleep study to figure out the best treatment.

If your child shows signs of sleep apnea, talk to your healthcare team. They can help diagnose and treat it. With the right care, kids with severe sleep apnea can get better and live a healthy life.
Risks and Complications of Untreated Extreme Sleep Apnea
Not treating sleep apnea can lead to serious health issues. High blood pressure is a big risk, which can cause heart disease and stroke. Untreated sleep apnea is also linked to diabetes and sudden cardiac death.
People with extreme sleep apnea may feel tired all day, have trouble thinking clearly, and live a lower quality life. The constant sleep disruptions can affect focus, mood, and overall health.
Men are 2 to 3 times more likely to get obstructive sleep apnea than women. Smoking and being older also increase the risk.
Untreated sleep apnea can affect others too. It can make partners sleep poorly, leading them to sleep elsewhere. It also raises the risk of car and workplace accidents, affecting society as a whole.
To avoid these problems, people with extreme sleep apnea should work with their doctors to find the right treatment. This might include using a CPAP machine, making lifestyle changes, or other treatments.
Addressing extreme sleep apnea early can protect your health and the health of your loved ones. The dangers of not treating it are too great to ignore.
Integrative Approaches to Extreme Sleep Apnea Management
Some people with extreme sleep apnea find help in integrative or holistic treatments. These methods can lessen stress, enhance sleep, and work alongside other treatments. They offer a full approach to managing sleep apnea.
Yoga is one such method. It helps with relaxation and breathing. Meditation and mindfulness are also good for the mind.
Acupuncture is another option. It's a traditional Chinese medicine technique. It aims to ease sleep apnea symptoms by targeting specific body points.
- Herbal remedies and supplements, like valerian root and melatonin, might be tried under a doctor's advice. They can help with sleep and relaxation.
- Changing your lifestyle is also key. This includes managing weight, exercising, and avoiding alcohol and some drugs. These changes can be part of a full treatment plan.
These integrative methods aren't a replacement for medical care. Yet, they can be a big help for some with extreme sleep apnea. By mixing traditional and holistic treatments, people can create a well-rounded plan. This plan tackles the complex nature of sleep apnea.
Choosing the Right Treatment Plan
Choosing the right treatment for extreme sleep apnea means looking at several things. These include how severe your condition is, what you prefer, and the good and bad of each therapy. It's important to work with a team of healthcare experts. This team should include a sleep specialist, your main doctor, and possibly a dentist or ENT specialist. They will help create a sleep apnea treatment plan just for you.
Factors to Consider
When picking a sleep apnea treatment, think about these important factors in treatment:
- The severity of your sleep apnea, based on sleep studies and doctor checks
- Your personal likes and lifestyle, like if you can use a CPAP machine or if you're okay with surgery
- The good and bad of each treatment, like how well it works, how comfy it is, and any side effects
- Your overall health and any other health issues that might affect treatment choices
Working with Your Healthcare Team
Working with your healthcare team is key to finding the best sleep apnea treatment plan for you. Your team might include:
- A sleep specialist, who can give a full check-up and suggest the best treatment choices
- Your main doctor, who can manage any other health issues and keep an eye on your health during treatment
- A dentist or ENT specialist, who might help with fitting and checking oral devices or surgery
By working with your healthcare team, you can get a sleep apnea treatment plan that fits your needs. This way, you can get the best results.
Monitoring and Adjusting Therapy
Managing extreme sleep apnea often means keeping a close eye on your therapy. You'll need to check in with your healthcare team, have follow-up sleep studies, and adjust your CPAP settings or other treatments as needed. This careful monitoring helps keep your therapy working well and lets you make changes quickly to get the best results.
It's important to meet regularly with your sleep specialist or doctor. They can look at your symptoms, check your sleep study results, and adjust your treatment plan if needed. Sometimes, you might need more sleep studies to see how well your therapy is working and if your sleep apnea is getting better or worse.
If you're using CPAP therapy, your healthcare team might need to change the pressure or try different masks to make sure they fit right and are comfortable. For oral appliances, seeing your dentist regularly is key to check how well they fit and work. You might need to get your appliance adjusted to keep it effective.
Keeping an eye on your sleep apnea treatment and making changes when needed can really help you get the best results. By working with your healthcare team, you can make sure your therapy keeps working well and improve your sleep and daily life.
Remember, managing severe sleep apnea is an ongoing process. Your treatment plan might change over time. Stay alert, talk openly with your healthcare providers, and be open to trying different treatments until you find the one that works best for you.
Living with Extreme Sleep Apnea
Living with extreme sleep apnea can be tough. But, you can make it easier with the right strategies and support. These can help you sleep better and lessen the effects of sleep apnea.
Improving Sleep Quality
Creating a calm sleep area is key for those with extreme sleep apnea. This means keeping the room cool, quiet, and dark. It also means making sure your bed is comfy for sleep.
Good sleep habits also help. Stick to a regular sleep schedule and avoid screens before bed. These steps can make your sleep better.
Managing Daytime Fatigue
Feeling tired during the day is a big issue for many with sleep apnea. To fight this, take regular breaks and stay active. Even a short walk can help increase your energy and health.
Being proactive in managing your sleep apnea and making lifestyle changes can greatly improve your life. Always talk to your healthcare team to find what works best for you.
Support Resources for Extreme Sleep Apnea
Finding help for [sleep apnea](https://www.resmed.co.in/sleep-apnea) can be easier with support from patient groups, online forums, and local clubs. These resources offer important info, support from peers, and advice for those with this ongoing issue. Meeting others who know what it's like to live with extreme sleep apnea can be very uplifting.
Being part of a [sleep apnea community](https://www.resmed.co.in/sleep-apnea) helps you find support, share stories, and learn new ways to cope with others who understand your struggles. These groups host events, share learning materials, and link people with doctors and support services.
Local sleep apnea groups also meet in person, offering a chance to connect with community members. They provide emotional support, useful tips, and a feeling of belonging for those dealing with extreme sleep apnea.
Talking to a healthcare expert is key to finding the best [sleep apnea support resources](https://www.resmed.co.in/sleep-apnea). They can guide you to local groups, advocacy organizations, and other resources to help you and your family cope with the condition.
You don't have to go through extreme sleep apnea alone. Connect with the [sleep apnea community](https://www.resmed.co.in/sleep-apnea) and use the support available to better manage your condition and enhance your life quality.
Conclusion
Extreme sleep apnea is a serious issue that needs a detailed and tailored approach. It's important to understand the different ways to diagnose and treat it. This includes CPAP therapy, oral devices, surgery, and changing daily habits. People with sleep apnea can work with their doctors to find the best solution and get better sleep.
Studies have shown many ways to treat extreme sleep apnea. These include surgery, CPAP machines, oral devices, and upper airway stimulation. This variety means doctors can create a plan that fits each patient's needs. This increases the chance of long-term success.
With the right support and strategies, people with extreme sleep apnea can improve their health and life quality. By using the available treatments and working with their doctors, they can beat the challenges of this condition. They can then enjoy deep, refreshing sleep.
FAQ
What is extreme sleep apnea and how is it diagnosed?
Extreme sleep apnea is a serious sleep disorder where breathing stops many times during sleep. Doctors first check your symptoms and sleep history. Then, they use tests like an overnight sleep study to watch your breathing and oxygen levels.
What are the treatment options for extreme sleep apnea?
For severe sleep apnea, CPAP therapy is often the best choice. If CPAP doesn't work, other devices like auto-CPAP or BPAP might be tried. For milder cases, oral appliances can help keep the airway open.
When are surgical interventions considered for extreme sleep apnea?
Surgery might be an option if other treatments don't work. This includes removing throat tissue, moving the jaw, or implanting devices to help control throat muscles.
How can lifestyle changes and home remedies help manage extreme sleep apnea?
Changing your lifestyle can help with sleep apnea. This means losing weight, exercising regularly, and avoiding alcohol and certain drugs that relax the throat muscles.
What are the risks and complications of untreated extreme sleep apnea?
Not treating sleep apnea can lead to serious health issues. These include high blood pressure, heart disease, stroke, diabetes, and even sudden death. It can also cause fatigue, brain fog, and a poor quality of life during the day.
How can integrative and holistic approaches be used to manage extreme sleep apnea?
Some people find help in holistic methods like yoga, meditation, and acupuncture. These can reduce stress, improve sleep, and work alongside other treatments.
How can I work with my healthcare team to develop the best treatment plan for my extreme sleep apnea?
Choosing the right treatment for sleep apnea depends on many factors. Work with a team including sleep specialists, primary care doctors, and specialists like dentists or ENTs. They can help create a plan that fits your needs.
How can I manage the ongoing care and monitoring of my extreme sleep apnea treatment?
Keeping up with sleep apnea treatment means regular check-ins and adjustments. This might include sleep studies and changes to your CPAP or oral appliance settings. Staying vigilant helps keep your treatment working well.
What resources are available to help me manage the challenges of living with extreme sleep apnea?
There are many resources to help with sleep apnea. Look for patient groups, online forums, and local support groups. They offer information, support, and advice for living with this condition.
Source Links
- Obstructive sleep apnea - Diagnosis and treatment - Mayo Clinic
- 6 Home Remedies for Sleep Apnea
- Sleep apnea - Diagnosis and treatment - Mayo Clinic
- Sleep Apnea: What It Is, Causes, Symptoms & Treatment
- Severe Sleep Apnea: Symptoms, Risk Factors, Treatment, and More
- Sleep Apnea Treatments: Lifestyle Changes, Oral Appliances, and Surgery
- Oral Appliances for Sleep Apnea: Benefits and How They Work
- Oral Appliances in Obstructive Sleep Apnea