National Men’s Mental Health Month: Why It’s Important | Dr. Chandril Chugh
National Men's Mental Health Month is in June. It's a big push to help men feel better mentally. Dr. Chandril Chugh, a top neurologist, talks about why men need this help.
Men often hide their mental health issues because of shame and old ideas. But this month is all about making mental health a priority for everyone. It's a chance to help men feel okay about getting help.
We learn about depression, anxiety, and stress. These issues affect men and their families a lot.
Joining in this month helps men get the support they need. We can make sure they have the help they deserve. Together, we can help men feel better and get the care they need.
Understanding Men's Mental Health Challenges
Men's mental health is often ignored, with many keeping their struggles hidden. Depression and anxiety are common among men. But, fear of being judged stops many from getting help. It's important to understand the challenges men face to support them better.
Prevalence of Mental Health Issues in Men
Statistics show a worrying trend for men's mental health. Veterans are 1.5 times more likely to die by suicide than others. Suicide is the second leading cause of death for young veterans.
Brain injuries in veterans also raise their suicide risk. Native Americans, Asian and Pacific Islanders, and veterans with brain injuries are at higher risk too.
Societal Stigma and Barriers to Seeking Help
- Men face social barriers like stigma, fear of judgment, and trouble talking about feelings. These make it hard for them to get mental health care.
- Men are less likely to be diagnosed with depression than women. This shows we need better ways to help men.
- Transgender veterans are twice as likely to commit suicide as their cisgender peers. This highlights the extra challenges the LGBTQ+ community faces.
- Men who do seek help often feel misunderstood by mental health professionals. This makes it harder for them to get the support they need.
It's key to address men's mental health needs with specific and culturally sensitive help. By tackling stigma and barriers, we can help men focus on their mental health. This way, they can get the support they deserve.
Common Mental Health Concerns for Men
Men often face unique mental health challenges. Depression and anxiety are common among them. Societal stigma and work-life balance issues play big roles.
Depression and Anxiety in Men
Depression and anxiety affect everyone, but men may show symptoms differently. Men are less likely to get help for mental health issues. They might show depression through anger or substance abuse instead of sadness.
Stress and Burnout at Work and Home
Work and family life can be very stressful for men. They face high pressure in their careers and at home. This can lead to burnout and make mental health problems worse.
- In 2021, 51.7% of women with a mental health condition received support from mental health services, while only 40% of men with a mental health condition accessed these services.
- The suicide rate among males in 2021 was around four times higher than the suicide rate among females, with men representing almost 80% of all suicides.
- Men are more likely to engage in substance misuse instead of seeking mental health care.

It's important to recognize depression, anxiety, and burnout in men. By taking care of themselves, getting help when needed, and balancing work and life, men can improve their well-being.
National men's mental health month
November is National Men's Mental Health Month. It's a time to focus on men's emotional health. This month helps remove the stigma around mental health talks, offers resources, and pushes men to care for their minds.
Many groups and health services work together to spread the word. They want to help men improve their health. This leads to happier and healthier lives for everyone.
- Men's suicide rates are 3.85 times higher than women's, according to the Centers for Disease Control and Prevention.
- Firearms account for over 54.64% of all suicide deaths in the United States.
- Younger generations, aged 18-20, are more comfortable discussing mental health concerns compared to older age groups.
This month is a big reminder that mental health is as vital as physical health. It aims to start open talks, reduce stigma, and offer help. This helps men feel okay to ask for support.

It's about tackling issues like depression, anxiety, or job stress. National Men's Mental Health Month urges men to look after their well-being. By focusing on mental health, we make a better place for men to succeed.
The Importance of Early Detection and Intervention
Early mental health detection is key for men's well-being. Recognizing signs and symptoms helps men address concerns and seek help. Watching for mood, behavior, and mental state changes is important.
Signs and Symptoms to Watch For
Some common mental health symptoms in men include:
- Persistent feelings of sadness, hopelessness, or irritability
- Difficulty concentrating or making decisions
- Increased risk-taking or impulsive behavior
- Difficulties in personal or professional relationships
- Sudden changes in sleep patterns or appetite
If you notice these symptoms, it's crucial to seek professional help.
Benefits of Seeking Professional Support
Seeking professional help for mental health offers many benefits. Treatment can help manage symptoms and improve well-being. It leads to better emotional control, stronger relationships, and more productivity.
By focusing on early detection and intervention, men can keep their mental health in check. Don't hesitate to seek support – your mental health is important.

Cognitive Behavioral Therapy for Men's Mental Health
Cognitive Behavioral Therapy (CBT) is a top choice for men's mental health. It helps men change negative thoughts and build resilience. This leads to better mental health overall.
CBT shows that our thoughts, feelings, and actions are linked. Men can learn to change bad thought patterns with a therapist's help. This can improve their feelings and actions, helping with depression, anxiety, stress, and burnout.

CBT for men's mental health is unique because it's practical and goal-focused. It's not just about the past. It's about solving today's problems with real skills.
This approach is great for men who like direct solutions. It helps them feel more comfortable seeking help.
CBT for men's mental health also helps break down barriers to seeking help. It offers a clear, proven way to improve mental health. This can encourage men to start their journey towards better mental well-being.
If you or someone you know needs mental health treatment, think about CBT. With the right support, men can manage their thoughts and feelings. This can lead to a happier, healthier life.
Building a Support Network
Having a strong support network is key for men's mental health. Family and friends, plus support groups, offer community and help. They encourage talking openly and provide guidance for mental health challenges.
Involving Family and Friends
Your loved ones are important for your mental health. Talk to them about what you're going through. Share your feelings and experiences.
Their support and understanding can greatly improve your well-being.
Joining Support Groups
- Look for local or online support groups for men's mental health. These places are safe and free from judgment. You can meet others who face similar struggles.
- Join in group talks, share your story, and learn from others. Support groups offer helpful tips and a sense of belonging.
- Think about joining the National Alliance on Mental Illness (NAMI). They have many support services and educational programs for individuals and families.
Building a strong support network helps you deal with mental health challenges. You don't have to face these alone.
Lifestyle Factors and Men's Mental Health
Your lifestyle choices are key to your mental health. Regular exercise and a balanced diet can boost your mood and stress management. These lifestyle factors can greatly improve your mental health.
Exercise and Physical Activity
Regular physical activity is great for your mental health. Activities like brisk walking or jogging can lower depression and anxiety. Try to do at least 30 minutes of exercise daily, even in short sessions.
Nutrition and Healthy Eating Habits
Your diet affects your mental health too. Eating a balanced diet with fruits, veggies, and lean proteins is good for your brain. Stay away from processed foods and sugary snacks. Focus on healthy eating habits that benefit both your body and mind.
Adding these lifestyle factors to your daily life can help your mental health. Remember, even small changes can make a big difference in your life.
Breaking the Stigma: Raising Awareness
It's important to fight the mental health stigma around men. We need to raise mental health awareness and change wrong ideas. This will help men feel okay to get help when they need it.
Men often don't talk about their mental health because of shame. They think it shows weakness or not being manly. But, mental health issues are common and can show up in many ways, like being angry or using drugs.
We can make a better place for men to care about their mental health. Events like Men's Mental Health Month and the #RealConvo campaign help. They push for talking openly, show good examples, and make it okay to get help.
When men focus on their mental health, they live better lives. They build stronger bonds and feel better overall. It's time to end the silence and let men take care of their minds without fear.
We can make a world that values men's mental health more. With learning, understanding, and listening, we can help. Let's work together to remove barriers. So, men can get help without feeling ashamed.
Workplace Mental Health Initiatives
Employers must support men's mental health at work. Good workplace mental health programs help your male employees feel better and work better.
Make sure men have access to mental health help. This could be counseling, workshops, or therapists. Talking openly about mental health helps men get help without fear.
- Offer confidential mental health services and ensure employees feel comfortable accessing them.
- Provide training for managers to help them recognize and address mental health concerns in male staff.
- Foster a culture of understanding and empathy, where men feel safe discussing their mental health challenges.
Also, help men balance work and life. Offer flexible work hours, breaks, and talk about self-care. This reduces stress and burnout.
By focusing on mental health, you help your male employees and your whole team. These efforts make your workplace better for everyone.
Conclusion
National Men's Mental Health Month is very important. It reminds us to tackle the mental health issues men face. We can help men by raising awareness and giving them resources and support.
We've talked about how common mental health problems are in men. We've also looked at why men might not talk about their feelings. Things like depression, anxiety, and stress at work are big concerns.
It's key to catch these problems early and get help. Professional support and therapy can really help. A strong support network and a healthy lifestyle are also important.
Employers can help too by making workplaces open and supportive. This helps everyone, especially men of color and diverse backgrounds. It makes healthcare fairer for all.
Let's keep working together to help men's mental health. It's not just about individual effort. It's about all of us supporting each other. We can make a world where men feel okay to talk about their feelings and live well.
FAQ
What is National Men's Mental Health Month?
National Men's Mental Health Month is a big deal. It happens every June. It's all about making men aware of their mental health.
Why is men's mental health often overlooked?
Men often hide their mental health struggles. This is because of shame and not knowing the truth. It's important to understand their challenges to help them.
What are some common mental health concerns for men?
Men deal with depression and anxiety a lot. Work and family life can make it worse. Knowing the signs helps men take care of their minds.
How can early detection and intervention help men's mental health?
Spotting mental health issues early is key. Knowing the signs and getting help is the first step. This way, men can get better and feel better.
What are the benefits of Cognitive Behavioral Therapy (CBT) for men's mental health?
CBT is a great help for men's mental health. It helps them change bad thoughts and find ways to cope. This leads to better mental health.
How can a strong support network benefit men's mental health?
Having a strong support group is vital. Family, friends, and groups can offer help and advice. They make men feel less alone and more supported.
What lifestyle factors can impact men's mental health?
Lifestyle choices matter a lot for men's mental health. Exercise, healthy eating, and stress management are key. These habits can really help men's mental health.
How can employers support men's mental health in the workplace?
Employers can make a big difference. They can offer mental health resources and counseling. This creates a supportive work environment for men's mental health.
Source Links
- Best Neurologist In Patna, Author Dr Chandril Chugh
- U.S. Army Garrison Rheinland-Pfalz highlights Men’s Mental Health Awareness Month
- Men and mental health: What are we missing?
- When Is Men’s Mental Health Awareness Month?
- Men's Health - Mental Health Awareness
Men’s Mental Health Statistics: The Numbers You Should Know | Dr. Chandril Chugh
Exploring men's mental health, we find important statistics. Mental health affects everyone, but men face unique challenges. This section will look at how common mental health problems are in men. It aims to help us better support their well-being.
Men are more likely to die by suicide than women. They also face higher rates of substance abuse. But, societal norms often stop men from getting help. It's key to tackle these issues and offer support that fits their needs.
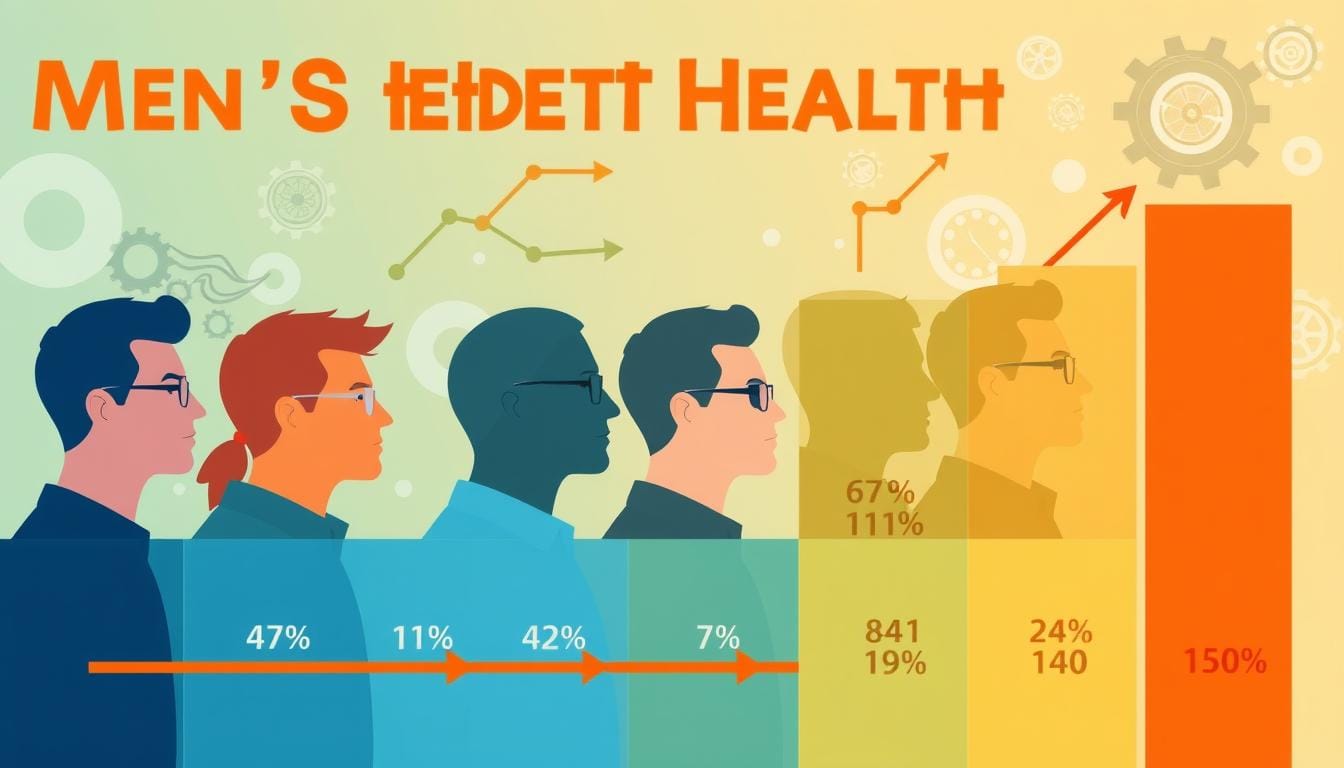
The Prevalence of Mental Health Issues in Men
Mental health problems affect people of all genders, but men face big challenges too. Anxiety and depression hit many men, with about 6 million in the U.S. dealing with depression each year. Yet, men are less likely to get help than women.
Suicide Rates and Risk Factors
Suicide rates for men are very high. Men are four times more likely to die by suicide than women. Most suicides, 79%, are men. This is due to substance abuse, feeling alone, and not wanting to ask for help.
Men also get schizophrenia more often, with 90% of cases diagnosed by 30 being male. The fear of being seen as weak stops many men from getting help. This makes the problem worse.
We need to tackle mental health issues in men head-on. We must understand the reasons behind these problems. By talking openly and making mental health services easy to find, we can help men. This way, we can build a stronger, more caring community.
Men's mental health statistics: A Closer Look at the Numbers
Men's mental health stats are quite alarming. Despite the stigma and barriers, it's key to understand these numbers. They show the big challenges men face.
The Stigma Surrounding Men's Mental Health
Men often hide their feelings due to gender norms. This "tough guy" idea, or toxic masculinity, stops them from talking about their mental health. This makes things worse.
Only about half of men with mental health issues get help, says the Anxiety & Depression Association of America (ADAA). Also, 49% of men hide their depression, and 45% think they can solve mental health problems alone, a Today Show survey found.
Societal Expectations and Toxic Masculinity
Societal norms make it hard for men to talk about their mental health. Men are more likely to use alcohol and drugs, showing a bad coping method.
Men are also more likely to be locked up for treatment and face violent crimes. They make up most of the prison population. This shows how mental health and masculinity are linked.
We must tackle the stigma and expectations around men's mental health. By understanding men's unique challenges and helping them get support, we can improve mental health for everyone.
Age-Specific Mental Health Challenges for Men
Men face different mental health challenges at different ages. It's important to understand these issues to help them better.
Young men deal with stress from school and work. They're trying to grow up. In the U.S., men die by suicide four times more than women. During COVID-19, men reported more depression and thoughts of suicide than women.
As men get older, they face new challenges. These include balancing work and life, money worries, and what society expects of them. Even when they seek help, they might not get the right care because of gender biases.
Older men have it even tougher. They deal with aging, health problems, and feeling left out. White men over 85 are at the highest risk of suicide. More men in this age group die by suicide than any other group.
To help men, we need to educate them, make resources easy to find, and change how society views masculinity and mental health.
Mental Health and Substance Abuse among Men
There's a big problem linking mental health and substance abuse in men. Men often face alcohol and drug addiction more than women. These issues can hide mental health problems, making treatment hard.
Men need special help that tackles both their mental health and addiction. This is because they face unique challenges.
Alcohol and Drug Addiction
Men are more likely to have substance use disorder than women. They might drink alone or use drugs to deal with stress or sadness. This can lead to more alcohol-related deaths and hospital visits.
Men also use marijuana more and have a higher risk of addiction. If they have PTSD, they're almost twice as likely to have a substance use disorder.
Dual Diagnosis and Co-Occurring Disorders
- About 50% of people with severe mental disorders also have substance abuse.
- 45.6 percent of adults with substance use disorder also have mental illness, like depression.
- Suicide rates are almost four times higher for men. 40 percent of these deaths involve alcohol, 30 percent opioids, and 21 percent marijuana.
Men's high rates of mental health and substance abuse issues show the need for special treatment. It must be tailored to their unique needs.
The Impact of Trauma and Adverse Childhood Experiences
Research shows that trauma and adverse childhood experiences (ACEs) deeply affect men's mental health. Events like physical or sexual abuse, neglect, or violence can lead to mental health issues. These include post-traumatic stress disorder (PTSD), depression, and substance abuse.
About two-thirds of U.S. adults have had at least one ACE in childhood. One in six adults have faced four or more ACEs. This means they have been exposed to many traumatic events.
- Some groups face more ACEs, like women, young adults, and those with lower income.
- Emotional abuse is the most common ACE. It's followed by parental separation and household substance abuse.
The effects of trauma and ACEs on men's mental health are huge. Studies show they increase the risk of depression, anxiety, and suicidal thoughts. ACEs also lead to chronic health problems and substance abuse.

It's key to understand how trauma and ACEs affect men's mental health. We need to address these issues and help men build resilience. This way, we can help them deal with the lasting effects and improve their well-being.
Mental Health and Masculinity: Redefining Strength
Traditional ideas of masculinity can block men from seeking mental health help. The idea of strength often means hiding feelings. This makes it hard for men to care for their minds and ask for help.
It's time to change what we mean by strength and masculinity. Emotional awareness, being open, and taking care of oneself are key. By embracing these, men can greatly improve their mental health.
Men with depression often want to talk about their feelings. But, they face barriers because of what society expects. This can make them feel isolated and less supported, leading to more distress.
We need a new culture that supports men emotionally. Seeing famous people like rapper Logic talk about mental health helps. Creating safe places for men to share their stories can also help break the stigma.
By changing what we mean by strength and masculinity, we can help men care for their mental health. This benefits not just men but our whole community.
Improving Access to Mental Health Resources for Men
Men often face big challenges when trying to get mental health help. Stigma, lack of awareness, and services not made for men are big hurdles. It's key to make mental health care better for men to improve their health.
Stigma is a big problem, especially for men who feel they must be tough. Men are less likely to get help because of this. They might turn to alcohol or drugs instead. We need to change these harmful ideas and support men's mental health.
Many men don't know about mental health resources or feel they don't fit. [Data] shows women get more help than men. We need to reach out more and offer services made for men.
To help men get better mental health care, we need many steps. This includes:
- Starting campaigns to reduce stigma and encourage men to get help
- Creating more mental health services for men
- Training doctors to spot and help men's mental health issues
- Working with community groups and places of worship to reach men
- Offering affordable, easy-to-use mental health resources like online groups
By working to remove barriers and make help easier to get, we can help men focus on their well-being. This is important for men's health and for our communities' strength.
The Role of Healthcare Providers in Supporting Men's Mental Health
Healthcare providers are key in helping men with their mental health. They do this by doing regular mental health checks and starting treatment early. This helps men feel less ashamed to talk about their feelings.
Checking for mental health issues during regular visits is important. It helps find problems like depression and anxiety early. Healthcare providers can make a safe space for men to talk about their feelings. This way, men can get the help they need.
- Incorporate mental health screening as a standard practice during routine check-ups and wellness visits.
- Provide referrals to mental health professionals and ensure seamless coordination of care.
- Foster an environment of trust and understanding, where men feel comfortable discussing their emotional health.
- Educate patients on the importance of proactive mental health management and the availability of various treatment options.
Starting treatment early is very important for men's mental health. Healthcare providers need to understand the challenges men face. This includes the pressure to be tough and not show emotions.
By supporting men's mental health, healthcare providers can make a big difference. They can help men feel more comfortable getting help. This can greatly improve men's health in the long run.
Community-Based Approaches to Promoting Men's Mental Health
Community-based programs are great for supporting men's mental health. They use local efforts to help men get the help they need. These programs create safe places for men to talk and support each other.
Peer support groups are a good example. They let men share their stories and learn from each other. Studies show these groups help men's mental health and get them to seek help.
- Education campaigns in the community also work well. They use messages that men can relate to. This helps men feel okay talking about their mental health.
- Initiatives that meet the needs of men in certain groups are also effective. For example, programs for men at work or in sports teams can reach them where they are.
Using community-based methods to support men's mental health is powerful. It builds a network that helps men take care of themselves. This approach can really change the way men think about their mental health, leading to better lives for everyone.

The Intersection of Men's Mental Health and Physical Health
The link between men's mental and physical health is very important. Your physical health can greatly affect your mental health, and the other way around. It's key to work on both for better health.
Issues like chronic conditions or a bad diet can hurt your mental state. Feeling stressed or anxious can also show up in your body. This means you might feel tired or have pain.
It's important to take care of both your mind and body. This way, you can improve your health and life quality. You might need to see doctors for both physical and mental health. Also, making healthy lifestyle choices is helpful.
Remember, your mental and physical health are connected. Taking care of one can help the other. By focusing on your overall health, you can make yourself happier and healthier.
Conclusion
We need to tackle the mental health issues men face. It's key to know how common these problems are and why they happen. We must also understand the barriers men have in getting help.
By working to reduce stigma and change what it means to be a man, we can help. This way, men can feel okay talking about their feelings and get the support they need.
Men's mental health is a big issue. They are more likely to die by suicide and show depression in different ways. They also find it hard to get help because of what society expects of them.
Men from different races and ethnicities face even more challenges. This is especially true if they don't have health insurance.
We can help men by changing how we see masculinity. Creating a supportive space for them to talk about their feelings is important. Research and local efforts are also key to understanding men's mental health in different places.
Improving men's mental health is not just about them. It's about making our society better for everyone. We need to work together to make a change.
FAQ
What are the unique mental health challenges that men often face?
Men often deal with substance abuse and higher suicide rates. Yet, they are less likely to seek help due to societal stigma and masculinity expectations.
How do the mental health conditions of men differ from women?
Women are more likely to face anxiety and depression. But men also struggle with these issues. They are less likely to get help than women.
What are the societal barriers that prevent men from addressing their mental health?
Traditional gender norms and expectations of masculinity can stop men from seeking help. This "tough guy" mentality makes it hard for them to talk about their feelings.
How do men's mental health challenges vary across different age groups?
Men's mental health issues change with age. Young men face stress from school and work. Middle-aged men deal with work-life balance. Older men see the effects of aging on their mental health.
What is the connection between mental health issues and substance abuse in men?
There's a strong link between mental health and substance abuse in men. They are more likely to struggle with alcohol and drug addiction. This can hide underlying mental health problems.
How do traumatic experiences impact men's mental health?
Trauma and adverse childhood experiences deeply affect men's mental health. Events like abuse or neglect can lead to PTSD, depression, and addiction.
How can redefining masculinity help address men's mental health challenges?
Changing what it means to be strong and masculine is key. It should include emotional awareness, vulnerability, and self-care. This encourages men to care for their mental health.
What are the barriers to accessing mental health resources for men?
Men face many barriers to mental health resources. Stigma, lack of awareness, and few male-friendly services are big issues. Making support more accessible and tailored to men's needs is vital.
What is the role of healthcare providers in supporting men's mental health?
Healthcare providers are crucial in supporting men's mental health. They should do routine screenings, intervene early, and create a safe space for men to talk about their feelings. This helps break down stigma and barriers.
How can community-based initiatives help promote mental health awareness and support for men?
Community programs and initiatives are effective. They include peer support groups, education campaigns, and community-driven interventions. These address the unique needs and cultural factors affecting men's mental health.
What is the relationship between men's mental and physical health?
Poor physical health, injuries, or unhealthy lifestyle choices can harm a man's mental well-being. A holistic approach that considers overall health is key for better outcomes.
Source Links
- Full text of "THE HINDU DELHI 18.09.2019"
- Males and Mental Health Stigma
- Men's Mental Health: Why 40% of men won't talk about it
- Men's Mental Health | Anxiety and Depression Association of America, ADAA
- Men’s Mental Health: Social Determinants and Implications for Services
- Men and women: statistics
Therapy Goals for Depression: Setting Yourself Up for Success | Dr. Chandril Chugh
Depression affects millions worldwide. Getting help and setting goals is key to recovery. Dr. Chandril Chugh's guide helps you manage your mental health and make progress.
Whether your depression is mild, moderate, or severe, this article has you covered. It talks about cognitive-behavioral therapy, exposure therapy, mindfulness, and lifestyle changes. These can help you feel better and improve your mood.
Cognitive Behavioral Therapy (CBT) is a proven way to fight depression. It helps you change your thoughts and feel better. Exposure therapy and mindfulness also play big roles in your recovery.
Changing your lifestyle, like exercising and eating well, helps too. Building a strong support system is also important. Remember, getting help when you need it and learning to handle setbacks are part of the journey.
Start your journey with Dr. Chandril Chugh's help. Take the first step towards a brighter future. Explore the strategies and insights in this guide.
Understanding the Cognitive Model of Depression
The cognitive model of depression says our thoughts, feelings, and actions are linked. People with depression often think negative thoughts. These thoughts can make them feel sad and upset.
Identifying Negative Thought Patterns
Those with depression might think in certain ways. For example:
- Catastrophizing: Thinking the worst will happen.
- Overgeneralizing: Seeing a negative event as a big problem in life.
- Personalization: Thinking they are to blame for everything.
Challenging and Replacing Irrational Beliefs
Cognitive-behavioral therapy (CBT) helps change these negative thoughts. It teaches people to see things more realistically. This can make them feel better and more positive.
Cognitive Defusion: Distancing from Anxious Thoughts
Cognitive defusion is a CBT technique. It helps people see their anxious thoughts as just thoughts. This makes these thoughts less powerful. It helps them face challenges more clearly.
Knowing about the cognitive model of depression helps people manage their mental health. They can work towards a more positive life.

Cognitive Behavioral Therapy: A Proven Approach
Cognitive Behavioral Therapy (CBT) is a well-known and proven way to treat depression. It helps people see how their thoughts, feelings, and actions are linked. This way, they can spot and change negative thoughts that make them feel sad.
Exploring the Principles of CBT
CBT's main ideas include spotting and changing bad thinking, trying new behaviors, and finding ways to cope. By changing their thoughts, people can handle life's tough moments better.
The Effectiveness of CBT for Depression
- Studies show CBT really helps reduce sadness and improves life for those with depression.
- CBT might need up to 20 sessions, as the National Health Services say. It works well for mild to moderate depression.
- CBT is also used for other mental health issues like anxiety, OCD, and insomnia.
- It can be used with other treatments, like medicines, to help with depression.
CBT gives people useful tools and strategies. It's a powerful way to improve mental health and help people take back control of their lives.
Therapy goals for depression
Setting clear goals is key in treating depression. These goals might include feeling better, managing emotions, and doing daily tasks. Working with a mental health expert helps create a plan that fits your needs.
Some important goals for depression therapy are:
- Lessening the number and strength of sad episodes
- Boosting mood and handling emotions better
- Doing more in daily life and being social
- Finding ways to deal with bad thoughts and feelings
- Improving life quality and feeling better overall
To reach these goals, you might:
- Spot and fight negative thoughts that lead to sadness
- Use cognitive-behavioral methods to manage symptoms
- Face scary situations to get better at dealing with them
- Use mindfulness and kindness to yourself to build emotional strength
- Make healthy lifestyle changes, like exercising and having friends
By setting clear goals, you can help yourself get better. Working with a therapist lets you tackle your depression together. This makes you feel in control and helps you beat depression.

Exposure Therapy: Facing Your Fears
Beating depression means facing what scares you. Exposure therapy helps a lot. It makes you get used to things that make you anxious. Dr. Chandril Chugh, a top neurologist, says it's a key part of getting better.
Gradual Exposure to Anxiety-Provoking Situations
Exposure therapy is about slowly facing things you avoid. Like talking to people or doing activities that make you nervous. Your therapist helps you, making sure you're safe and in charge.
By taking small steps, you challenge your fears. You learn to handle your feelings better.
Building Tolerance and Resilience
Doing exposure therapy makes you more comfortable with things that scare you. You get better at dealing with your emotions. This makes you feel more confident and strong.

Recovery isn't always easy, and you might face ups and downs. But with a good therapist and your effort, you can beat your fears. Dr. Chandril Chugh and his team are ready to help you.
Mindfulness and Self-Compassion
Overcoming depression needs a mix of approaches. Mindfulness and self-compassion are key. Mindfulness helps you stay present and accept your feelings. Self-compassion means being kind to yourself.
Studies show these methods help with depression. A big study found they reduce symptoms and stress. They also help you feel better over time.
Being kind to yourself can make a big difference. It helps you handle tough times better. This kindness can protect your emotional health.

You can add mindfulness and self-compassion to your therapy. These practices help you feel more positive. They make you stronger against depression.
Remember to be gentle with yourself as you get better. Celebrate your small wins. Mindfulness and self-compassion are powerful tools. They help you overcome depression and live a better life.
Lifestyle Changes for Sustainable Well-being
To help with your therapy, making lifestyle changes can really help. Exercise can make you feel better and think clearer. Also, getting enough sleep, eating well, and managing stress can help you feel more in control.
Incorporating Exercise and Healthy Habits
Doing physical activities like yoga or running can make you feel happier. Try to exercise for at least 30 minutes, five days a week. Eating right and sleeping well also helps your mind stay healthy.
Building a Support System
Having a strong support system is key to getting better. Talk to your family, join groups, or do things in your community. This way, you won't feel alone and you'll feel more connected.
By making healthy choices, you can help yourself get better. This way, you can live a better life and feel more fulfilled.
Seeking Professional Help
Getting help for depression can change your life. Mental health professionals like therapists and psychiatrists can help. They know how to tackle depression's tough challenges.
When to Consult a Mental Health Professional
Knowing when to get help is key. Look for signs like lasting sadness or trouble doing daily tasks. A mental health pro can offer support and create a plan just for you.
Seeing a mental health pro gives you tools to fight depression. They can help you:
- Find out why you're feeling down
- Learn ways to handle bad thoughts
- Try therapies like cognitive-behavioral therapy (CBT)
- Look into medicines to balance your brain's chemicals
- Build a support network and make healthy choices
Getting help is brave, not weak. It shows you care about your health and want a better life.
Coping with Setbacks and Maintaining Progress
Recovering from depression is not always easy. You might see progress and then face setbacks. It's important to have ways to deal with these challenges and keep moving forward.
Start by being kind to yourself. Remember, setbacks are part of the journey. Treat yourself with the same care and understanding you would offer a friend.
- Reach out to friends or a therapist. Sharing your feelings can offer new insights and make you feel less alone.
- Change your therapy goals or methods if needed. Be open to trying different ways until you find what works for you.
- Look at the progress you've made, even if it's small. Celebrate your wins to keep you motivated.
Dealing with depression setbacks and keeping up progress is ongoing. With a strong mindset and the right strategies, you can handle the ups and downs. Keep moving towards your goals.
Conclusion
Setting clear goals is key to beating depression. Understanding depression's causes helps a lot. Using therapies like cognitive-behavioral and exposure therapy is important.
Adding mindfulness and self-compassion to your life is also crucial. Making lifestyle changes can help a lot too. This way, you can take charge of your mental health.
Getting professional help is vital for lasting success. Being kind and flexible in your recovery is important. With the right help and strategies, you can beat depression and live a better life.
Focus on changing negative thoughts and building resilience. Use therapies and mindfulness to help. Remember, small steps lead to big changes.
Stay positive and surround yourself with support. Trust the journey towards a brighter future. Keep working towards your goals for depression recovery.
FAQ
What is the cognitive model of depression?
The cognitive model of depression says our thoughts, feelings, and actions are linked. People with depression often think negatively. This can make them feel sad and upset.
How can cognitive-behavioral therapy (CBT) help with depression?
CBT shows how our thoughts, feelings, and actions are connected. It helps people see and change negative thoughts that make them sad. CBT teaches new ways to think and act.
What are the key therapy goals for individuals with depression?
Therapy goals for depression are important. They include feeling less sad, managing emotions better, and doing daily activities. Goals also include learning to cope and improving life quality.
How can exposure therapy help with depression?
Exposure therapy is part of CBT. It helps people face things they avoid because of sadness. This builds confidence and helps manage emotions.
What role do mindfulness and self-compassion play in the treatment of depression?
Mindfulness helps people accept their feelings without judgment. Self-compassion is treating oneself with kindness. Both help reduce negative thoughts and improve recovery.
How can lifestyle changes contribute to the management of depression?
Lifestyle changes help manage depression. Regular exercise, healthy eating, and sleep are key. A strong support system also helps.
When should someone seek professional help for depression?
Getting help for depression is important. See a mental health professional if symptoms last long or interfere with daily life.
How can individuals cope with setbacks and maintain progress in their recovery from depression?
Recovery from depression has ups and downs. It's important to have ways to deal with challenges. Self-compassion, support, and adjusting therapy goals help keep progress.
Source Links
- Best Neurologist In Patna, Author Dr Chandril Chugh
- Cognitive Behavioral Therapy for Depression
- Cognitive Therapy for Depression
Symptoms of Depression in Men: Recognizing the Signs | Dr. Chandril Chugh
Dr. Chandril Chugh is a top mental health expert. He wants to help men understand depression better. In this article, he talks about the signs of depression in men. He aims to help you spot these signs and improve your mental health.
Depression is a complex issue that affects everyone. But, men often show different symptoms than what's commonly known. Knowing these signs can help you tackle depression and care for your mental health.
Dr. Chugh explains the emotional, physical, and mental symptoms men with depression might have. He covers sadness, fatigue, and risky behavior. By knowing these signs, you can get help and take back control of your mental health.
If you're dealing with depression or worried about someone you love, this article is for you. Dr. Chandril Chugh offers important insights and tips. Start your journey to better mental health and find a more fulfilling life.
Understanding Depression in Men
Depression is a complex mental health issue that affects everyone. But, it shows up differently in men than in women. It's important to know these differences to help men with their mental health.
Men with depression might feel sad all the time, lose interest in things they used to like, and get angry easily. They might also feel tired, have changes in appetite or sleep, and find it hard to focus. These symptoms can really affect a man's life and how he relates to others.
Men often face a big challenge because of what society expects from them. They're expected to be strong, not show emotions, and be able to handle everything on their own. This makes it hard for them to admit they need help with their mental health. So, they might not get the help they need, making things worse.
Jobs that are mostly for men, like construction or being in the military, can also make depression more likely. These jobs are stressful and can lead to trauma. This adds to the mental health challenges men already face.
It's key to understand how depression affects men differently. This knowledge helps doctors, family, and friends support men better. Together, we can make it easier for men to get the help they need for their mental health.
Emotional Symptoms of Depression in Men
Depression affects men and women in different ways. It's important to know how depression shows up in men. Men often show sadness as irritability, anger, or losing interest in fun activities.
Persistent Sadness or Emptiness
Men with depression often feel sad or empty for a long time. This feeling can last for weeks or months. It affects their daily life, work, and relationships.
They might feel hopeless, worthless, or unable to feel joy. This makes their life very hard.
Loss of Interest in Activities
Men with depression lose interest in things they used to love. They might stop doing hobbies, social activities, or even taking care of themselves. This makes them feel even more alone and sad.
Irritability and Anger
Many men with depression get irritable and angry. They might get frustrated easily, have outbursts, or act aggressively. This is a way for them to deal with their depression.
It's key to spot these signs of depression in men early. This way, we can help them get the right treatment and support. Understanding how depression shows up in men helps us support them better.

Physical Symptoms of Depression in Men
Depression can show up in many ways, not just in how we feel. Men with depression might feel very tired or have trouble sleeping. They might also notice changes in how much they eat and their weight. Spotting these signs is key to getting help.
Fatigue and Low Energy
Feeling very tired is a big sign of depression in men. Even after a full night's sleep, they might still feel exhausted. This can make it hard to do simple things and hurt their daily life.
Sleep Disturbances
Problems sleeping are common in men with depression. Some can't fall asleep or stay asleep. Others sleep too much, trying to hide from their feelings. Bad sleep can make depression worse, creating a cycle.
Changes in Appetite and Weight
Depression can also affect how much men eat and their weight. Some might eat less and lose weight, while others might eat more and gain weight. These changes can make them feel worse about themselves.
Cognitive and Behavioral Symptoms
Depression can affect a man's thinking and actions. This part talks about symptoms like trouble focusing, being indecisive, and acting recklessly. Knowing these signs can help spot depression and offer support.
Difficulty Concentrating
Men with depression often struggle to focus. This makes it hard to do well at work or enjoy hobbies. It's a common problem for those with depression.
Indecisiveness
Depression can make it hard to decide what to do. Men might put off important choices or feel stuck. Overcoming this indecisiveness is key to managing depression.
Reckless or Self-Destructive Behavior
- Some men with depression might act recklessly, like drinking too much or taking risks. They might also harm themselves.
- These actions are often a way to deal with pain or show they don't care about themselves. It's important to see and treat these behaviors as part of depression treatment.
Spotting the signs of depression in men is crucial. It helps in offering the right help and support. Understanding how depression affects thinking and actions helps everyone involved.

Symptoms of depression in men
Depression shows up differently in men than in women. Men might not show their feelings in the same way. It's important to know the signs of depression in men to get help early.
Men often feel sad or empty but might not talk about it. Instead, they might get angry or irritable. They might also stop doing things they used to love, which can make them feel even more alone.
- Persistent sadness or feelings of emptiness
- Loss of interest in activities and hobbies
- Increased irritability, anger, or hostility
Depression can also make men feel very tired or have trouble sleeping. They might eat less or more than usual, which can be a sign of depression too.
Men with depression might have trouble focusing or making decisions. They might also take risks or do things that could hurt themselves, like using drugs or alcohol. These signs can make it harder for men to see they need help.
If you or someone you care about is showing these signs, getting help is key. Getting help early can really help in fighting depression.
The Unique Challenges for Men with Depression
Men with depression often face unique challenges. These can make it hard for them to seek help and care for their mental health. [https://www.aamc.org/news/men-and-mental-health-what-are-we-missing] Societal stigmas and gender-specific barriers make it tough for men to talk about their depression.
Men often downplay or don't recognize depression symptoms. They might see it as just stress. This leads to fewer diagnoses, even though men are more likely to die by suicide or abuse substances. The fear of being seen as weak or unmanly also stops men from getting help.
- Just 1 in 3 men took medication for daily feelings of depression or anxiety, with just 1 in 4 speaking to a mental health professional.
- White men aged 85 years and older are most at risk of suicide.
- Of those who receive a schizophrenia diagnosis by the age of 30 years, 90% are men.
Men also face gender-specific barriers, like feeling they must be self-reliant. They might be unsure about psychotherapy. [https://www.aamc.org/news/men-and-mental-health-what-are-we-missing] Men are less likely to talk about their mood to doctors, which affects how they seek help.

It's important to tackle these challenges to support men's mental health. [https://www.aamc.org/news/men-and-mental-health-what-are-we-missing] Understanding the barriers men face helps us create a better environment for them to care for their mental health.
The Importance of Early Intervention
It's key to spot and tackle depression in men early on, Link Between Depression And Suicide. Early action can greatly change a man's mental health path. Spotting signs and getting help fast can lessen depression's effects and boost well-being.
Consequences of Untreated Depression
Ignoring depression can make it worse. It can hurt a man's personal and work life. It can also harm relationships and job skills, raising the risk of suicidal thoughts. The sooner depression is treated, the better.
Seeking Professional Help
- Men feeling depressed should get help from a therapist or counselor.
- A mental health expert can give a full check-up, find the cause, and create a plan just for you.
- Getting help early and right can help men take back control of their mental health. It can also make life better and lower the risk of serious problems.
Looking for professional help shows courage, not weakness. By focusing on mental health and tackling depression, men can find a more rewarding and lasting path to happiness.
Strategies for Coping with Depression
Men can fight depression by themselves, but getting help from a doctor is key. This part talks about ways to feel better, like exercising, staying connected with friends, and using mindfulness. These steps help men take charge of their mental health and feel better overall.
Exercise and Physical Activity
Exercise is a big help against depression. Try walking fast, jogging, swimming, or lifting weights. It makes you feel happier, less stressed, and healthier. Try to exercise for 30 minutes each day. Pick activities you like to keep doing them.
Social Support
Having friends and family is very important for men with depression. Talk to your loved ones about how you feel. Doing things with others, like going out or doing hobbies, makes you feel connected. It's okay to ask for help when you need it.
Mindfulness and Relaxation Techniques
Using mindfulness and relaxation can really help with depression. Try meditation, deep breathing, or yoga. These can lower stress, help you focus, and make you feel better. They help you deal with bad thoughts and feelings, making recovery easier.

Treatment Options for Depression in Men
If you're a man struggling with depression, know you have many ways to get help. You can try psychotherapy, medication, and lifestyle changes. These can help manage your symptoms and improve your well-being.
Psychotherapy
Talking to a mental health professional can really help. Cognitive-behavioral therapy (CBT) can change negative thoughts and teach coping skills. Interpersonal therapy (IPT) helps improve your relationships and communication, which can also help with depression.
Medication
Antidepressant medications, like SSRIs or SNRIs, can help. They balance your brain's chemicals to ease symptoms. It's key to work with your doctor to find the right medication and dosage for you.
Lifestyle Changes
- Regular exercise can boost your mood and well-being.
- Eat a healthy, balanced diet with nutrient-rich foods.
- Get 7-9 hours of sleep each night for better health.
- Reduce stress with relaxation techniques like meditation or mindfulness.
- Avoid too much alcohol and substance abuse, as they can make depression worse.
Exploring these treatment options for depression in men is a big step towards better mental health. With the right support and self-care, you can beat depression and live a fulfilling life.
Supporting a Loved One with Depression
When a man in your life is struggling with depression, your support can help a lot. Depression is treatable, and your help can guide them through it.
Understanding and Empathy
Start by learning about depression in men. Knowing the signs helps you talk and show empathy. Don't downplay their feelings or give advice without being asked. Just listen and understand.
Encouraging Professional Help
Encourage them to see a doctor or therapist. Men often don't want to talk about it. Your support can help them feel more comfortable.
Offer to help find a doctor or go with them to appointments. This shows you're there for them.
Creating a Supportive Environment
Depression can make people want to stay away from others. Make a caring space by checking in and inviting them to fun activities. Let them share their feelings without fear of judgment.
Don't be too hard on them. Help them take small steps towards getting better.
Supporting someone with depression takes patience and understanding. By being empathetic, encouraging help, and creating a caring space, you can help them heal.
Conclusion
As we wrap up our look at depression in men, it's clear we need a wide range of solutions. We must understand depression in men better. This way, we can help men feel okay about talking about their feelings.
It's important to know how depression affects men differently. This includes how traditional ideas of being a man can hurt them. Also, men are more likely to try to take their own lives. And, they might not react the same way to antidepressants.
We all have a role in helping men with depression. This includes everyone, from doctors to friends. By being kind and understanding, we can help men feel safe to ask for help.
Together, we can make a change. We can make a world where men feel free to talk about their feelings. This way, they can live happy and fulfilling lives.
FAQ
What are the unique symptoms of depression in men?
Depression in men can show differently. Symptoms include feeling sad or empty, losing interest in things, and getting angry easily. They might also feel tired, have trouble sleeping, or eat less.
Other signs are trouble focusing, making decisions, or acting recklessly.
How does depression in men differ from depression in women?
Depression affects both men and women but shows differently. Men might show anger or take risks more than women. Women often show sadness and withdraw more.
Why is it important to recognize depression in men?
It's key to spot depression in men early. If not treated, it can get worse. It can harm relationships, work, and even lead to suicidal thoughts.
Helping men get help can greatly improve their mental health.
What are the unique challenges men face in addressing their depression?
Men often struggle to admit they're depressed because of societal views. They might see it as weak or not masculine. They might also feel they should handle it alone.
It's important to understand and help overcome these barriers.
What are some effective coping strategies for men with depression?
Men can fight depression with self-care. Regular exercise, staying connected with friends, and using mindfulness help. These steps empower men to manage their depression.
What are the treatment options available for depression in men?
Treating depression in men needs a mix of approaches. This includes therapy, medication, and lifestyle changes. Working with a healthcare provider to find the right plan is key.
How can loved ones support a man with depression?
Supporting a man with depression means being understanding and empathetic. Encourage him to get help and create a supportive space. Be patient, listen without judging, and offer help when needed.
Source Links
- Common Women's Mental Health Issues: What To Know
- Best Neurologist In Patna, Author Dr Chandril Chugh
- Signs of Depression in Men: 13 Symptoms and What You Can Do
- Depression in Men: Symptoms and Physical Effects
Facts About Men’s Mental Health: Important Things to Know | Dr. Chandril Chugh
Men's mental health is very important but often ignored. It's key to know the mental health issues men face and how to take care of your mind. This guide will cover the facts about men's mental health, including statistics, common disorders, and the stigma around it.
The Prevalence of Mental Health Issues Among Men
Men's mental health statistics are concerning. Mental health disorders affect everyone, but men face special challenges. Knowing how common these issues are in men is key to helping them.
Rates of Common Mental Disorders in Men
Men are not spared from common mental health problems. Over 6 million men in the U.S. deal with depression each year. Many cases go unnoticed.
More than 3 million men struggle with panic disorder, agoraphobia, or other phobias. About 3.5 million Americans have schizophrenia, with 90% of them being men by age 30.
Mental Health Challenges Faced by Men of Different Ages
- Young men aged 16-24 are especially at risk. Over a quarter of them face common mental health issues.
- Men between 16 to 25 are also at high risk for bipolar disorder. Men and women are equally affected by this condition.
- Tragically, men in the U.S. die by suicide four times more often than women. They often use more lethal methods and act more impulsively.
It's vital to address mental health issues in men. This ensures everyone gets the support and resources they need for better well-being.
The Societal Stigma Surrounding Men's Mental Health
One in five adults in the United States face mental illness yearly. Yet, men struggle to seek help because of stigma. They are seen as strong, stoic, and self-reliant, making it hard to talk about feelings.
Stigma affects men in many ways, like in work, social settings, culture, and even within themselves. This leads to fewer diagnoses and less care. Sadly, men are nearly four times more likely to die by suicide than women.
Men also tend to misuse drugs and die from alcohol more often. This shows we must tackle the stigma stopping them from getting help. Programs for vulnerable groups, like homeless youth, can help break these barriers.

Challenging the stigma around men's mental health is key. It ensures everyone, no matter their gender, gets the support they need. This way, everyone can focus on their well-being and live a fulfilling life.
Facts about men's mental health
Men face unique challenges in mental health. Nearly 1 in 10 men experience depression or anxiety, but less than half seek help. Also, men are almost two times more likely to binge drink than women and three times as likely to die from alcohol abuse.
The numbers are shocking. Over a third of men (35%) have had a diagnosable mental health condition, and 77% have felt symptoms like anxiety or depression. Sadly, 40% of men have never talked about their mental health, and 29% are too embarrassed because of stigma.
The main reasons for mental health issues in men are work, finances, and health. Men are three times as likely to die by suicide compared to women, especially between 40 to 49 years old. Sadly, suicide is the biggest cause of death for men under 50.
These male mental health statistics show we need to act fast. We must help men with their mental health issues. By understanding these facts, we can make a change. We can help men feel empowered to take care of their mental health.
The Impact of Toxic Masculinity on Men's Well-being
The idea of "toxic masculinity" has become more known lately. It shows how certain ideas about being a "real man" can harm men's mental health. These ideas tell men to hide their feelings, not ask for help, and act out in risky ways. All these can hurt their well-being a lot.
Redefining Masculinity and Its Influence on Mental Health
We need to change what it means to be a man. We should challenge old ideas that say men must be tough, aggressive, and not show feelings. By showing a kinder, more open view of masculinity, men can share their feelings, ask for help, and find better ways to deal with problems.
- Letting men be real and open with their feelings can make their mental health better. It helps them talk better in relationships and feel more empathy.
- Breaking free from the need to be a certain kind of man can stop men from taking risks. It also makes them more likely to get help for their health.
- Showing different ways to feel and act can make men's lives better. It helps create a kinder, more welcoming view of being a man.
By changing what we think of masculinity, we can make a better place for men to care about their mental health. This can lead to better lives for everyone.
Recognizing Signs and Symptoms of Mental Health Issues in Men
Knowing the symptoms of mental health problems in men and warning signs of mental health issues in men is key. It helps in early treatment. Men face special challenges with their mental health. Understanding these signs helps them get the support they need.
Changes in emotional expression are a common sign. Men might find it hard to talk about their feelings. They might even hide them because of what others expect. Signs like sudden anger, irritability, or mood swings can mean something's wrong.
Physical signs like low energy, loss of appetite, and stomach problems can also point to mental health issues. Some men might turn to risky behaviors like substance abuse or dangerous actions to deal with their feelings.
It's important to remember that mental health signs can vary. Things like age, race, sexuality, and life experiences can affect how men show their mental health problems. Getting help and working to reduce stigma around men's mental health is vital.
If you or someone you know is showing these symptoms of mental health problems in men or warning signs of mental health issues in men, get help. Visit Dr. Chandril Chugh's website to learn about keeping a healthy and active mind.
The Role of Trauma and Adverse Childhood Experiences
Trauma and bad childhood experiences deeply affect men's mental health. Research shows that those who faced abuse or neglect are more likely to have mental health problems. These can include depression, anxiety, and PTSD.
Addressing Trauma to Improve Men's Mental Well-being
To help men with trauma, we need to support them. This means creating a safe space for them to open up and feel their emotions. Here's how:
- Make therapy and counseling services available that focus on trauma.
- Help men build a strong support network of friends, family, and mental health experts.
- Challenge old ideas that tell men not to show feelings or ask for help.
- Teach men about self-care and healthy ways to deal with stress, like mindfulness and exercise.
By tackling trauma and bad childhood experiences, we can help men feel better. They can then live healthier, happier lives.

The Importance of Social Support and Healthy Relationships
Research shows that strong social connections and healthy relationships are key for men's mental health. Men with good support networks and positive relationships tend to do better mentally than those without. This is important for their overall well-being.
Men often look for help with tasks or solving problems from their friends. But, both emotional and practical support are vital for their mental health. Sadly, men usually have smaller social circles and see their family and friends less. This can make them feel lonely and isolated.
It's important to tackle this issue because men with less social support tend to hide their feelings more. This is because of the traditional male role, which makes it hard for men to ask for emotional help. This can make their mental health problems worse.
To help men, we need to encourage them to:
- Grow and care for their social networks, including family and friends
- Join in on social activities and hobbies to make connections
- Make sure to talk openly and honestly in their relationships
- Ask for help from people they trust when they're struggling
- Work to make it okay for men to ask for help and support
By highlighting the importance of social support and healthy relationships, we can help men focus on their well-being. This can lead to a better life for them, both physically and mentally.
Lifestyle Factors Affecting Men's Mental Health
Lifestyle choices are key to good mental health for men. What you eat, how much you exercise, and how well you sleep matter a lot. Knowing how these choices affect your mental health helps you take care of your mind.
The Impact of Diet, Exercise, and Sleep on Mental Well-being
Eating right can greatly improve your mental state. Foods like salmon, walnuts, and flaxseeds are full of omega-3s. They help your brain work better and reduce inflammation.
Getting enough vitamins and minerals is also important. B-complex vitamins and magnesium help your brain and mood. They keep your mind sharp and balanced.
Exercise is vital for mental health too. Activities like walking, jogging, or lifting weights release happy hormones. They help fight anxiety and depression. Try to exercise for at least 30 minutes, five days a week.
Good sleep is also essential for mental health. Aim for 7-9 hours of sleep each night. A regular sleep schedule helps your body and mind rest well. Relaxation techniques like deep breathing or meditation can also improve sleep and reduce stress.
By focusing on a healthy lifestyle, you can greatly improve your mental health. Eating well, exercising regularly, and sleeping enough are key. These habits help manage stress, boost mood, and improve overall well-being.

Seeking Professional Help: Overcoming Barriers for Men
Mental health issues affect everyone, but men face special challenges in getting help. Societal stigmas, cultural beliefs, and masculine ideals make it hard for men to talk about their mental health. This can stop them from getting the help they need.
Many men think asking for help is a sign of weakness. This fear keeps them from seeking help, as they worry about being seen as less masculine. In some places, talking about mental health is seen as taboo. This makes it even harder for men to get the support they deserve.
Men often don't know when they need help because they don't understand mental health well. This lack of knowledge can lead to not getting help when it's needed. It can make the problem worse over time.
- Break down the stigma around men's mental health by starting open conversations. Show how important it is to seek help.
- Make more mental health education and resources available for men. Tailor them to meet men's unique needs and views.
- Help healthcare providers understand how men might show they're struggling with mental health. This ensures they get the right help.
- Create a community where men feel safe talking about their mental health. Make sure they won't be judged or laughed at.
By tackling these barriers and helping men value their mental health, we can make a better place for everyone. Remember, taking care of your mental health shows strength, not weakness.
Promoting Mental Health Awareness and Education for Men
It's important to tackle the stigma that stops men from getting help for their mental health. Data shows many people, including those with social anxiety and women, don't get the help they need. This is because of biases and a lack of services that fit their needs.
It's key to promote mental health awareness and education for men. This helps them spot mental health issues, get help, and care for their overall health.
To boost mental health awareness for men, projects like the WELL BEINGS project are vital. They use radio, digital content, tours, and documentaries to fight stigma. The Social Innovators Challenge also supports projects in Australia, Canada, and the UK. These projects aim to help men who are lonely or isolated.
Educating men on mental health is vital to fix the gap in mental health services. The Centers for Disease Control and Prevention say men are less likely to get help than women. By making mental health services easy to find and fitting for everyone, we can help men take care of themselves.

Promoting mental health awareness and education for men is a big step. It helps fix the gap in mental health services and outcomes. By making mental health less stigmatized, providing easy-to-find resources, and empowering men, we can make a better world for everyone.
Conclusion
This article has shown us the key facts about men's mental health. We've looked at how common mental health issues are in men. We've also seen the barriers they face and the impact of toxic masculinity.
We've talked about how trauma and bad experiences affect men. We've learned about the importance of social support and healthy relationships. And we've seen how lifestyle choices play a role in men's mental health.
Empowering men to care for their mental health is key. We need to raise awareness and educate people. We must change societal norms that stop men from seeking help.
This will help men feel supported and encouraged to take care of their mental health. It will lead to healthier lives for men. And it will benefit everyone in the community.
Remember, your mental health is as important as your physical health. Don't be afraid to ask for help or lean on your support system. Together, we can make a world where men feel comfortable and confident in caring for their emotional well-being.
FAQ
What is the prevalence of mental health issues among men?
One in eight men have a mental disorder, compared to one in five women. Young women aged 16-24 are especially affected, with over a quarter reporting a common mental health issue.
What are the common symptoms of mental health problems in men?
Symptoms include intense fear or anxiety in social situations. Men might avoid social interactions, blush, sweat, and have trouble making eye contact or starting conversations.
How does toxic masculinity impact men's mental well-being?
Societal expectations can harm men's mental health. They might feel they can't seek help or express emotions. Changing these expectations could help.
What is the connection between trauma, adverse experiences, and men's mental health?
Trauma and adverse experiences are linked to mental health issues in both men and women. Over 53% of women with mental health issues have also faced abuse. Addressing these experiences is key.
How can lifestyle factors like diet, exercise, and sleep affect men's mental well-being?
Healthy habits like diet, exercise, and sleep are important for men's mental health. Practices like breathing exercises can also help reduce stress.
What are the barriers that prevent men from seeking professional help for mental health issues?
Societal stigma and cultural beliefs make it hard for men to seek help. Many, including those with social anxiety disorder, don't get the support they need.
How can we promote mental health awareness and education for men?
We need to raise awareness and provide education. It's important to address the challenges men face. This includes promoting mental health literacy and ensuring services meet men's needs.
Source Links
- Did You Know: Unmanaged CrossFit Can Lead To Brain Stroke!
- Full text of "THE HINDU DELHI 18.09.2019"
- Men's Mental Health | Anxiety and Depression Association of America, ADAA
- Men and mental health: What are we missing?
- Males and Mental Health Stigma
Magnetic Therapy for Depression: An Alternative Treatment | Dr. Chandril Chugh
Are you fighting depression and searching for a new way to feel better? Magnetic therapy might be something to think about. Dr. Chandril Chugh is a big name in this field. He believes it could be a game-changer for those with depression.
Magnetic therapy is a new area that uses magnetic fields to help with depression. It works by balancing the brain and body. This could bring peace and happiness back into your life.
In this article, we'll look into how magnetic therapy works. We'll see if it can really help with depression. You'll learn about the science behind it and how it might change your mood. It's a new way to find happiness and well-being.
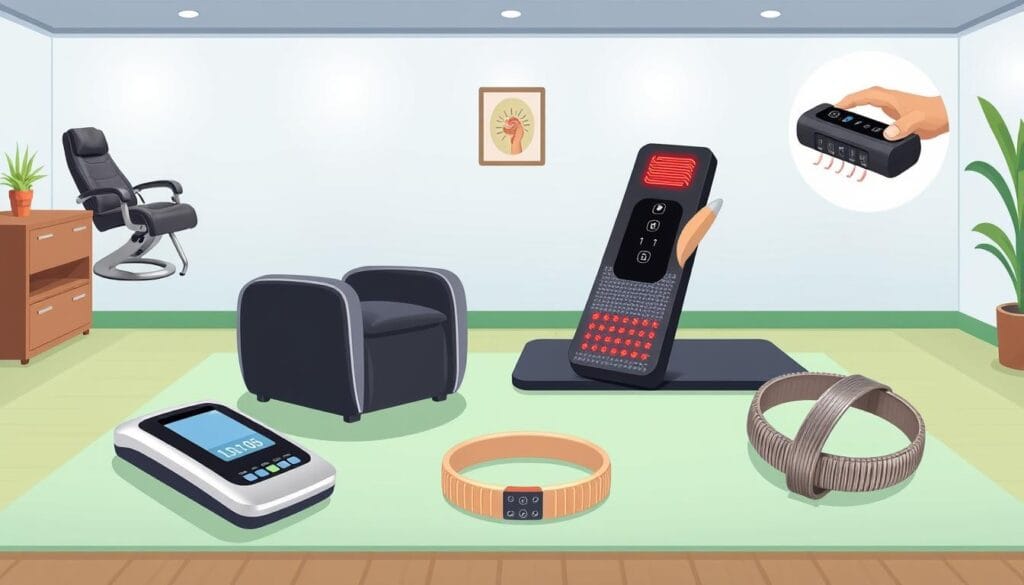
What is Magnetic Therapy for Depression?
Magnetic therapy for depression is a non-invasive treatment. It uses magnetic fields to help with depression symptoms. It works by changing the brain's activity and mood.
Understanding the Principles of Magnetic Therapy
Magnetic therapy for depression is based on the brain's electrical and magnetic properties. It uses external magnetic fields to change the brain's activity. This can affect mood and emotional processing.
The Potential Benefits of Magnetic Therapy for Depressive Disorders
Studies show magnetic therapy may help with depression. It can improve mood, motivation, sleep, and thinking. It's a safe option with fewer side effects than some medicines.
For example, Transcranial Magnetic Stimulation (TMS) was approved in 2008 for depression. Two-thirds of patients saw big improvements. Around 70% felt better for a year.
Magnetic therapy is being looked at as a safe and effective option. It could help those seeking more ways to manage their mental health.
Types of Magnetic Therapy Devices
There are many types of magnetic therapy devices for depression. These include transcranial magnetic stimulation (TMS) devices and pulsed electromagnetic field (PEMF) devices. Each has its own way of treating depression.
Transcranial magnetic stimulation (TMS) devices use electromagnetic coils. They create magnetic fields that target specific brain areas. This can help boost brain activity and fight depression. The FDA has approved TMS for treating major depressive disorder. There are different types, like standard, DASH, and TouchStar, for various needs.
Pulsed electromagnetic field (PEMF) devices, however, cover the whole body with magnetic fields. They aim to improve overall health and might help with depression too. Some PEMF devices are small and wearable, making it easy to use them every day.
The range of magnetic therapy equipment for depression keeps growing. This gives people more options to find treatments that fit their mental health needs.
The Science Behind Magnetic Therapy for Depression
Magnetic therapy for depression works through complex brain interactions. It affects how neurons fire and changes neurotransmitter levels. This can help the brain adapt and change, which is key for mood.
By focusing on mood-regulating areas, magnetic therapy might fix neural imbalances. This could help reduce depression symptoms.
How Magnetic Fields Interact with the Brain
The neuroscience of magnetic therapy shows it deeply affects brain function. Magnetic fields can change how neurons work and affect important chemicals in the brain. They also help the brain adapt and change, which is vital for mood.
Possible Mechanisms of Action in Alleviating Depressive Symptoms
Several ways magnetic therapy might help depression have been studied. It could increase key neurotransmitters, release feel-good chemicals, and boost brain adaptability. These changes can improve mood and thinking.
It might also reduce inflammation and affect the HPA axis, which is often off in depression.
Magnetic Therapy vs. Conventional Treatments for Depression
Patients now have a new option for depression: magnetic therapy. It's different from usual treatments like medicines and talk therapy. Studies show magnetic therapy might be very helpful.
Comparing the Effectiveness and Side Effects
Medicines like SSRIs and SNRIs are well-studied and work for many. But, not everyone gets better. The STAR*D study found only about a third of people got better with SSRIs. SNRIs did a bit better, with 44% getting better.
Magnetic therapy, like TMS, looks promising. It helps about two-thirds of people with depression who didn't get better with other treatments. Using brain scans to guide TMS can even help up to 80% of people.
Magnetic therapy might have fewer side effects than medicines. TMS can cause headaches or scalp feelings, but it's safer than ECT. ECT can lead to serious side effects like memory loss. Researchers are looking into safer ways to use electric current in ECT, inspired by TMS.
So, magnetic therapy might be a good choice for some. It's especially helpful for those who didn't get better with usual treatments. But, we need more research to know how it compares to other treatments.

Magnetic Therapy for Depression: An Alternative Treatment
Magnetic therapy is becoming a new way to treat depression. It's different from usual medicines because it's safe and doesn't hurt. It might help fix the brain problems that cause depression.
People who don't get better with usual treatments might find help here. It's a natural way to feel better without drugs.
The FDA says magnetic therapy is okay for treating depression. Studies show it can really help. Some people even get better completely.
Newer methods like SAINT are even better. They help almost 80% of people feel better in just five days. This shows magnetic therapy could be a great choice for treating depression.
Magnetic therapy doesn't have the bad side effects that medicines do. Some people might feel a little bit of discomfort where it's applied. But overall, it's safe and might be a good choice for treating depression.
As magnetic therapy gets better, it's important for people with depression to learn about it. Talking to a doctor about it can help. This way, people can make smart choices about their mental health.
Precautions and Potential Risks of Magnetic Therapy
Magnetic therapy is mostly safe, but there are some things to watch out for. People with pacemakers or metal implants should avoid it. Pregnant women, those with seizures, and some neurological conditions should also be careful
It's important to get help from doctors before starting magnetic therapy. Some people might feel headaches, scalp pain, or dizziness. Rarely, it could cause hearing loss, but using earplugs can help prevent this.
The biggest risk is a seizure, but it's very rare. In a big study, no one had seizures, died, or tried to kill themselves. Only about 5% of people stopped treatment because of side effects.
- Checking for seizure risks is key to avoid seizures.
- Adjusting the treatment to fit each person's needs helps prevent seizures.
- Following a special procedure to start treatment safely is important.
- People giving the treatment must watch closely for any signs of a seizure.
- They should know how to call for help if something goes wrong.
By taking these steps, magnetic therapy can be safe and helpful for many people.

Who Can Benefit from Magnetic Therapy for Depression?
Magnetic therapy for depression can help many people. It's good for those who haven't found relief with other treatments. It's also for those who don't like the side effects of usual antidepressants.
The U.S. Food and Drug Administration (FDA) says transcranial magnetic stimulation (TMS) works for depression. It's also approved for OCD, migraines, and helping people quit smoking. This shows it's a powerful tool for different health issues.
Evaluating Individual Suitability and Consulting Professionals
Seeing a doctor is key to know if magnetic therapy is for you. A psychiatrist or neurologist will check your health and suggest the best treatment.
- Getting advice from experts in magnetic therapy is important. They can give you the best care.
- Side effects of TMS include scalp pain, headaches, and muscle twitches. Rarely, it can cause seizures or hearing loss.
- As scientists learn more, TMS might get even better at helping people.
Working with your healthcare team can help you see if magnetic therapy is right for you. It's a way to manage depression and find what works best for you.
Integrating Magnetic Therapy with Other Treatment Approaches
Managing depression is best done with a mix of treatments. Magnetic therapy can be a key part of this mix. It works well with other proven treatments to help people with depression.
Using magnetic therapy, like TMS, with talk therapy can really help. Studies show that TMS and talk therapy together can make people feel better faster. This combo helps change negative thoughts and feelings.
Adding magnetic therapy to medication can also help a lot. TMS with antidepressants can make symptoms better for longer. But, it's important to talk to doctors about changing meds to avoid bad side effects.
Adding mindfulness practices, like meditation, to magnetic therapy can also help. This mix can reduce stress and improve mood. It can make magnetic therapy even more effective.
For the best results, work with doctors to mix magnetic therapy with other treatments. This way, depression can be tackled from all sides. It leads to a more complete and personal recovery plan.

Current Research and Future Directions
Scientists are studying magnetic therapy for depression a lot. They want to know how well it works over time. They also want to find out which parts of the brain it affects most.
They're looking into making treatments that fit each person's needs. This could make therapy more effective.
A study found that 61% of people with depression got better after deep TMS. Another study showed deep TMS helped keep people feeling better for a long time.
- Alternate-day dTMS with SSRIs helped people with chronic depression in a big study.
- A study looked at how often TMS should be done to help with depression.
- Another study found that a special kind of TMS helped more people than a placebo.
As we learn more, magnetic therapy might become a big part of treating depression. It could be used with new technologies like digital health tools. This could make managing depression easier.
The future of magnetic therapy for depression is bright. Researchers are working hard to make it better. They're looking at how to use it for longer and how to make it fit each person's needs.
Conclusion
Magnetic therapy is a promising option for those with depression. It uses magnetic fields to help the brain, offering a non-invasive solution. This method could improve life quality and help manage depression.
More research is needed to fully understand magnetic therapy's effects. But, it's already showing promise. It might become a key part of treating depression in the future.
Working together, doctors and patients can find the best use of magnetic therapy. It has helped many people, offering hope for those with treatment-resistant depression.
Success rates are high, from 70% to 80%. This makes magnetic therapy a valuable option for many. It's a chance to find relief from depression's heavy burden.
As magnetic therapy advances, it's important to keep up with new findings. Staying informed and talking to healthcare experts can help. This way, you can decide if magnetic therapy fits your health needs and goals.
FAQ
What is magnetic therapy and how does it work for depression?
Magnetic therapy is a new way to treat depression. It uses magnetic fields to help improve mood. This therapy might change how the brain works, helping to feel better.
What are the potential benefits of magnetic therapy for depressive disorders?
Magnetic therapy might help with feeling sad, not wanting to do things, and sleeping problems. It's safe and might have fewer side effects than other treatments.
What types of magnetic therapy devices are used to treat depression?
There are different devices for magnetic therapy. These include TMS, PEMF, and portable devices for self-use.
How do magnetic fields interact with the brain and what are the proposed mechanisms of action?
Magnetic fields might change how brain cells work. They could help with mood and thinking. This is because they might affect neurotransmitters and brain activity.
How does magnetic therapy compare to conventional treatments for depression?
Magnetic therapy might be better because it has fewer side effects. But, we need more studies to know for sure.
What are the precautions and potential risks associated with magnetic therapy?
People with pacemakers or metal implants should avoid magnetic therapy. Pregnant women and those with seizures should also be careful. Always talk to a doctor first.
Who can benefit from magnetic therapy for depression?
It's good for those who don't respond to usual treatments. Or for those who can't take antidepressants. But, a doctor must decide if it's right for you.
How can magnetic therapy be integrated with other treatment approaches for depression?
You can use magnetic therapy with therapy, lifestyle changes, and sometimes meds. This can make treatment more effective and personal.
What is the current state of research on magnetic therapy for depression, and what are the future directions?
Research is ongoing to see how well magnetic therapy works long-term. They're looking at how it affects the brain and how to make it better. They also want to use it with new technologies to help depression.
Source Links
- How To Cope With Central Pain Syndrome
- 2021 Annual Meeting | Cerebrovascular Disease and Interventional Neurology Posters
- Best Neurologist In Patna, Author Dr Chandril Chugh
- After years of depression, electromagnetic stimulation of the brain may provide relief
- Pros and Cons of TMS for Depression | Mindful Health Solutions
- TMS Therapy: What It Treats, Benefits, Side Effects, and Costs
Mental Health Rehab: When It’s Time to Consider Treatment | Dr. Chandril Chugh
Dr. Chandril Chugh is a top adult neurologist in Patna. He knows how important it is to deal with mental health quickly and fully This article will look at mental health rehab. We'll talk about when you might need treatment, the kinds of disorders that need it, and how to get the best care.
Mental health rehab is key for people with many neurological and psychological problems. This includes frontotemporal dementia and Tourette syndrome. By spotting mental health signs early and knowing the risks of not treating them, you can help your loved ones or yourself a lot.
Understanding the Need for Mental Health Rehabilitation
It's important to spot early signs of mental health problems. Small changes like trouble focusing or memory issues can mean big problems. If not treated, these can make daily life much harder.
Recognizing the Signs of Mental Health Issues
Here are some signs you might need mental health help:
- Persistent changes in mood, energy levels, or sleep patterns
- Difficulty concentrating, making decisions, or remembering information
- Withdrawal from social activities or a loss of interest in hobbies
- Unexplained physical symptoms, such as headaches or fatigue
- Significant changes in behavior or personality
Impacts of Untreated Mental Health Conditions
Ignoring mental health problems can cause big problems. People with severe mental health issues often feel unhappy and have a low quality of life. They might also lose their independence and struggle with daily tasks.
Getting help early can prevent these problems. It can improve your life and help you feel better. By facing mental health issues head-on, you can take back control and live a happier, more independent life.

Types of Mental Health Disorders Requiring Rehab
There are many mental health disorders that need rehab. These include frontotemporal dementia, Alzheimer's disease, and others. Each one has its own challenges that need special treatment.
Frontotemporal dementia affects the brain's frontal and temporal lobes. It changes behavior, personality, and language. Alzheimer's disease is the most common dementia. It causes memory loss, thinking problems, and behavior changes.
- Depression makes people feel sad, hopeless, and lose interest in things.
- Anxiety disorders include too much worry, fear, and physical symptoms.
- Bipolar disorder causes big mood swings, from being very happy to very sad.
These disorders need detailed rehab programs. They help people manage symptoms, feel better, and live independently again.
Mental health rehab: A Comprehensive Approach
For mental health rehabilitation, a complete plan is key. It needs a team of experts, like therapists and caregivers. They work together to make a treatment plan that fits the person's needs.
Evidence-based therapies are at the core. These include cognitive-behavioral therapy (CBT) and managing medications. CBT helps change bad thought patterns. Medications help with symptoms of mental health issues.
This approach also looks at other health issues. It's about treating the whole person, not just their mental health. This way, the treatment plan can help with many health problems at once.
Residential treatment programs are a big part of this plan. They offer constant support and many therapies. These programs help people grow and learn in a safe place.
In the end, every person's recovery path is different. By using proven therapies and a team of experts, mental health rehab helps people take back their lives. They learn to cope better and improve their relationships.

Stages of Frontotemporal Dementia and Treatment Options
Frontotemporal dementia (FTD) is a brain disorder that affects the frontal and temporal lobes. Knowing the stages of FTD is key for the right care and support. Let's look at the different phases and treatment choices.
Early Stages: Mild Cognitive Changes and Behavioral Shifts
In the early stages, people might find it hard to make decisions or solve problems. They might also act differently, like being less social or changing their personality. It's important to get medical help and try treatments like cognitive therapy early on.
Middle Stages: Language Difficulties and Impact on Quality of Life
As FTD gets worse, speaking and understanding can become very hard. This makes everyday life tough, especially when talking to others. Speech-language therapy can help with these issues and improve daily life.
Later Stages: Personality Changes, Memory Loss, and Severe Impairment
In the later stages, personality changes and memory loss get worse. People might lose empathy and have compulsive behaviors. A detailed care plan, including medication and support, is vital to keep their quality of life good.
It's important to try different treatments as FTD progresses. This includes medication, therapy, and support. Working with doctors, support groups, and community resources helps both the person with FTD and their caregivers.
Rehabilitation Programs and Therapies for Mental Health
Finding your way to mental health recovery can be tough. But, the right programs and therapies can help a lot. Whether you need inpatient or outpatient care, a full plan is important. It helps meet your specific needs and leads to lasting improvement.
Inpatient and Outpatient Rehabilitation Settings
Inpatient care offers a structured, intense setting for those needing constant care. It includes many therapies, medicine management, and support. This helps stabilize symptoms and starts the recovery journey.
Outpatient care lets you get treatment while keeping up with daily life. It might include weekly therapy, group counseling, and more. These services are tailored to your needs and progress.
Specialized Therapies for Mental Health Disorders
- Cognitive Therapy: Changes negative thought patterns that cause mental health problems.
- Behavioral Therapy: Works on changing behaviors and finding ways to cope with symptoms.
- Occupational Therapy: Helps with skills for daily activities and staying independent.
- Physical Therapy: Deals with physical issues from mental health, improving overall health.
- Speech Therapy: Helps with communication or swallowing problems from mental health.
These therapies offer a complete recovery plan. They cover physical, cognitive, and emotional health. This way, mental health programs can help you fully recover.
The Role of Caregivers in Mental Health Rehabilitation
Caregivers are key in mental health recovery. They offer emotional support, practical help, and educational resources. These are vital for those with mental health issues to reach their recovery goals.
Emotional support is very important. Studies show that people with supportive families do better in treatment. Caregivers create a safe space for their loved ones to talk and share feelings.
Practical help is also crucial. Caregivers help with daily tasks and healthy habits. This support makes life easier and improves well-being during mental health recovery.
Learning about mental health is important for caregivers. Knowing about mental health and treatments helps them support their loved ones better. Resources like support groups and counseling help caregivers too.
In the end, caregivers are vital for mental health recovery. Their emotional, practical, and educational support helps people achieve their goals. This way, they can get back to living a good life.
- Offer emotional support and create a safe, non-judgmental environment
- Provide practical assistance in navigating the healthcare system and managing daily tasks
- Seek caregiver education to better understand the mental health condition and available treatment options
- Access resources like support groups and counseling to cope with the challenges and maintain personal well-being
Overcoming Challenges in Mental Health Rehabilitation
Starting a mental health rehabilitation journey is both rewarding and tough. People seeking help face many obstacles. These include stigma, financial issues, and limited access to care. But, with the right help and support, these hurdles can be cleared, leading to a successful recovery.
The big challenge is the social stigma around mental illness. This makes it hard for people to ask for help, fearing judgment or being judged. It's key to spread awareness and education about mental health. This way, we can build a kinder and more understanding world.
Another big problem is not having enough access to good mental health care, especially in some areas. Mental health rehabilitation centers work to fill this gap. They offer treatments that fit each person's needs. Also, pushing for more insurance coverage and funding for mental health can help more people get the care they need.
Money can also be a big obstacle. But, many treatment centers offer help with costs. They have flexible payment plans, financial aid, and work with insurance. Patients and their families should look into these options to find what works best for them.
Keeping patients and their caregivers involved is also very important. Using therapies that focus on the patient, talking openly, and getting loved ones involved in the plan helps. This makes the person more likely to stick with their recovery plan.
By tackling these challenges and using a complete approach to mental health care, people can find their way to lasting wellness. With the right support and resources, the journey to recovery can be smoother and more successful.
Conclusion
Mental health rehabilitation helps people with mental health issues to take back their lives. It lets them reach their highest potential. Healthcare teams use a detailed, custom care plan to meet each person's needs.
This approach makes sure every patient gets the right help. It leads to a better life and recovery. It's all about focusing on the person, not just their illness.
Success in mental health care comes from combining special therapies and proven methods. Caregivers play a big role too. They offer support and help the person feel whole again.
Starting your mental health journey is a big step. It's a long-term effort, but with the right help, you can win. You can take back your life and find happiness again.
FAQ
Signs include small changes in behavior and how you think. You might notice changes in memory and focus. These changes can affect your daily life.
What are the consequences of leaving mental health conditions untreated?
Untreated mental health can lead to more brain problems. It can also change your personality and lower your quality of life.
What types of mental health disorders may require rehabilitation?
Disorders needing rehab include frontotemporal dementia and Alzheimer's. Also, depression, anxiety, and bipolar disorder may need it.
How does the comprehensive approach to mental health rehabilitation work?
A team of experts works together. They include doctors, therapists, and caregivers. They create a plan tailored to you, using proven therapies and medicines.
What are the stages of frontotemporal dementia, and what treatment options are available?
Frontotemporal dementia has three stages. Early stages show small brain changes and behavior shifts. Middle stages bring language problems and big life impacts. Later stages have big personality changes, memory loss, and severe brain problems.
Treatment includes medicines, therapy, and support. This helps manage symptoms and improve life quality.
What rehabilitation programs and therapies are available for mental health conditions?
Rehab is available in hospitals and outpatient settings. Therapies include cognitive and behavioral therapy. Also, occupational, physical, and speech therapy are options.
What is the role of caregivers in the mental health rehabilitation process?
Caregivers offer emotional support and help understand the disease. They provide practical help to those in rehab. It's also key to educate caregivers and offer them support.
What challenges may arise during the mental health rehabilitation process?
Challenges include stigma and barriers to care. Financial issues and keeping patients and caregivers involved are also big hurdles.
Source Links
- Hemiplegia Treatment: Approaches And Therapies
- Memory Loss, Behavioral Changes, and Slurred Speech in a 49-Year-Old Man
- Best Neurologist In Patna, Author Dr Chandril Chugh
- Psychiatric rehabilitation today: an overview
Men in Depression: How to Recognize and Help | Dr. Chandril Chugh
Depression is a complex mental health issue that can affect anyone. But men often find it hard to recognize and seek help. Dr. Chandril Chugh, a well-known brain specialist has worked to understand and help men with depression.
This guide will explore why men face stigma in mental health. We'll look at the signs of depression in men and how to support them. By breaking down myths, we aim to help men seek help and recover.
Depression is treatable, and men can get better with the right support. Let's talk about how to help the men in your life. Together, we can help them find the courage to seek help.
Understanding the Stigma: Why Men Struggle to Open Up
Men often face tough expectations and gender roles. These make it hard for them to share their feelings and get help for mental health. The "tough guy" idea, which values strength and not showing emotions, stops men from talking about depression and getting support.
Societal Expectations and Gender Roles
Societal stigma is a big reason men don't talk about their mental health. Men are expected to be strong, independent, and in control of their emotions. Saying they're depressed or anxious is seen as weak. This makes it hard for men to ask for help without being judged or laughed at.
The "Tough Guy" Mentality and Its Consequences
The "tough guy" idea is deeply rooted in society. It can have serious effects on men's mental health. Men who follow this idea might feel too ashamed to show their feelings or get help. This can lead to untreated depression and even death by suicide.
According to the World Health Organization, men are more than twice as likely to die by suicide than women worldwide.
To fight this stigma, we need to change old gender norms. We must encourage open talks and help men focus on their health. By tackling these societal and cultural issues, we can make a better place for men to get the help they need.
Identifying the Signs of Depression in Men
Depression shows up differently in men and women. It's key to spot the signs in men. Men often feel tired, have trouble sleeping, eat differently, and feel physical pain. These signs can be missed or misunderstood.
So, it's important for family and doctors to know how depression looks in men.
Physical Symptoms: Fatigue, Sleep Issues, and More
Depression hits 1 in 8 men at some point. Men tend to show physical signs more than emotional ones. Here are some common physical signs:
- Persistent fatigue and lack of energy
- Difficulty falling asleep or staying asleep
- Changes in appetite, such as overeating or loss of appetite
- Unexplained physical aches and pains, such as headaches or digestive problems
Life challenges like losing a loved one, job loss, abuse, or stress at work can lead to depression in men. If you see these signs, talk to a doctor.

The Unique Challenges men in depression Face
Men with depression face special challenges that make their condition worse. They often feel pressured to be strong and not show their feelings. This fear of being seen as weak can stop them from getting help.
Depression can also affect men's sense of self and their roles at home and work. They might feel like they're not living up to being the strong provider. This feeling of failure can make them ignore their own mental health needs. The shame of having mental health issues can also make them feel isolated and less likely to seek help.
- Studies show that men's fear of seeking help for depression comes from traditional masculine norms. These norms value strength, success, self-reliance, and hiding emotions.
- Men who got help for depression said it changed their views on depression. This shows how important it is to meet their specific needs.
- Fathers with mental health issues find it hard to be good parents because of depression. This can make their parenting worse and make the problem even bigger.
To help men with depression, we need a special approach. We must understand the pressures and expectations they face because of their gender. By creating a supportive and understanding space, we can help men focus on their mental health. This way, they can get the help they need to recover.
Coping Mechanisms: Unhealthy vs. Healthy Approaches
Men dealing with depression might use many coping strategies. Some are harmful, while others are helpful. It's key to know the difference.
Substance Abuse and Other Risky Behaviors
Excessive drinking or drug use is a bad way to cope for men with depression. It can lead to addiction and make mental health worse. Other harmful behaviors, like gambling or self-harm, try to hide pain but make things worse.
Positive Coping Strategies: Exercise, Therapy, and Support
Healthy coping strategies can help manage depression. Exercise, like running or lifting weights, can boost mood and reduce stress. Therapy, whether alone or with others, offers tools to handle emotions.
Having a strong support network is also crucial. Friends, family, or groups can make men feel less alone and more hopeful.
It's important to swap bad coping methods for good ones. Focus on self-care and getting the right help. This way, men can manage their depression and feel better overall.
The Impact of Depression on Relationships and Work
Depression can affect a man's life in big ways. It can strain his relationships with loved ones. Symptoms like feeling distant and irritable can make it hard to connect with others.
At work, depression can also be a big problem. It can make it hard to focus and do well in your job. This can hurt your career.
Depression can make relationships tough. It can lead to problems with intimacy and trust. It can even cause the end of long-distance relationships.
At work, depression can cause problems too. It can make you tired and unable to concentrate. This can hurt your job performance.
But, there is hope. Getting help and building a support network can help. Healthy coping strategies can also make a big difference.
Men in depression: Breaking the Silence
We must end the silence around men's depression. Society often expects men to be tough, making it hard for them to talk about their feelings. It's time to start open conversations and help men get the support they need.
Encouraging Open Dialogue and Seeking Help
About 1 in 8 men deal with depression at some point. But, men are less likely to get diagnosed than women. This is because men are often taught to hide their feelings, leading to shame and fear of seeking help.
We need to make places where men can share their feelings safely. Doctors, support groups, and educational efforts are key. They help create a supportive space for men to focus on their mental health.
- Seeing a doctor is a sign of strength, not weakness.
- Start talking about mental health in families, workplaces, and communities.
- Stop thinking depression is only a "women's issue."
- Help men take the first step to talk to mental health experts or join groups.
By ending the silence and fostering empathy, we can encourage more men to open up. This will help them seek help and work towards a better future.

Treatment Options: Therapy, Medication, and Lifestyle Changes
If you're a man struggling with depression, know that you have many treatment options. You can try therapy, medication, and lifestyle changes. These can help manage your symptoms and improve your wellbeing.
Cognitive-Behavioral Therapy and Its Benefits
Cognitive-behavioral therapy (CBT) is often recommended for men with depression. It helps you spot and change negative thoughts that lead to depression. Through CBT, you learn how to handle your emotions better and face problems head-on.
Research shows CBT can be very effective. Many men see a big drop in symptoms after 16-20 weekly sessions. A good therapist helps you understand your thoughts better and find healthier ways to deal with tough situations.
Medication is also key in managing depression. Antidepressants and mood stabilizers help balance brain chemicals that cause depression. It's crucial to work with your doctor to find the right medication and dosage for you.
Finally, making healthy lifestyle choices can boost your recovery. Regular exercise, stress management, and good sleep habits can greatly improve your mood and wellbeing.
There's no single way to treat depression in men. By trying therapy, medication, and lifestyle changes together, you can find the best way to heal and improve your life.
The Role of Family and Friends in Supporting Recovery
When a man is struggling with depression, family and friends play a big role. They offer emotional, practical, and social support. This helps him focus on his mental health and work towards wellness.
It's key for family and friends to encourage open talk. A safe and non-judgmental space lets you share feelings and thoughts freely. This understanding helps you seek help when needed.
Your loved ones can also help set healthy boundaries. They remind you to take care of yourself and stick to your treatment plan. This support is crucial, even when it's hard.
Being part of your treatment is very helpful. Family and friends can go to therapy with you. They learn about depression and how to support you. This strengthens your support network.
Remember, your recovery is a journey. The support of your loved ones is crucial. Together, you can empower each other to prioritize mental health and find healing.
Family and friends support for men with depression can change the game. Embrace their support and start your journey to help men with depression.

Preventive Measures: Fostering Mental Well-being
Good mental health is more than just treating depression. Taking steps early can stop depression in men. Stress management is key, along with regular exercise and finding a balance in life.
Stress Management, Self-Care, and Mindfulness
Self-care is important too. This includes enough sleep, eating well, and doing things you enjoy. Mindfulness helps men stay aware and in control of their feelings. This is crucial for mental health.
- Engage in regular physical activity to manage stress and boost mood
- Practice relaxation techniques, such as deep breathing, meditation, or yoga
- Prioritize a healthy work-life balance to prevent burnout
- Ensure adequate sleep, a nutritious diet, and time for leisure activities
- Incorporate mindfulness practices to enhance self-awareness and emotional regulation
By focusing on prevention, men can improve their mental health. These steps help men stay strong against depression. They also show others the importance of mental health.
Success Stories: Men Who Have Overcome Depression
Beating depression is a big journey. Many men have won this fight. Their success stories of men with depression give hope to those still fighting.
Sam, a 26-year-old MA student, battled anxious depression since his teens. He even thought about suicide and hurt himself. But he didn't give up. He got help and now excels in school and life.
Max, a 26-year-old who works in charity calls, also fought depression. It started in his teens and got worse after big life changes. Therapy and support groups helped him find his way again.
Even famous athletes like Olympic champion Michael Phelps have faced depression. In 2004, Phelps hit rock bottom. But he got better with therapy, meds, and lifestyle changes.
These men show us the strength of being open, resilient, and seeking help. Their stories encourage others to start their own journey to better mental health.

Recovery isn't always easy. Men with depression face special challenges. Yet, these stories show that with the right support and a strong will, anyone can beat depression.
Conclusion: Embracing Vulnerability and Seeking Help
As we wrap up our look at men's mental health, the message is clear. Being open and seeking help shows strength, not weakness. It's time to break down the old ideas that keep men from talking about their feelings.
Letting go of the need to be tough and being honest with yourself is a big step. It's the first step towards feeling better. Getting help from professionals and building a strong support network can help you face the challenges of depression.
Your mental health is as vital as your physical health. Taking care of your feelings, finding healthy ways to cope, and working on your recovery can lead to a better future. By being open and seeking help, you're not just helping yourself. You're also inspiring others to do the same.
FAQ
What are the societal expectations and gender roles that prevent men from seeking help for depression?
Men often feel they must be strong and not show weakness. This idea makes it hard for them to talk about depression. It's a big part of why men struggle to get help.
How can depression manifest differently in men compared to women?
Depression can show up in different ways for men and women. Men might feel tired, have trouble sleeping, or feel physical pain. These signs are often missed or misunderstood.
What unique challenges do men with depression face?
Men with depression face many challenges. They might feel they can't show weakness or burden others. Depression can also affect their identity and work life, making recovery harder.
What are the differences between healthy and unhealthy coping mechanisms for men with depression?
Men might try to hide their pain by using drugs or taking risks. But, healthier ways like exercise and talking to someone can help them feel better.
How can depression impact a man's personal and professional life?
Depression can hurt a man's relationships and work life. It can make it hard to keep up with work and connect with loved ones. It's important to talk about mental health at work.
What are the treatment options available for men struggling with depression?
Men can get help through therapy, medicine, and lifestyle changes. Therapy helps them change their thinking and face fears. Medicine and healthy habits also help manage symptoms.
How can family and friends support men with depression?
Family and friends are key in helping men with depression. They can offer emotional support and encourage seeking help. Being involved in treatment helps men feel supported.
What are some preventive measures men can take to promote their mental well-being?
Men can stay mentally healthy by managing stress and practicing self-care. This includes exercise, relaxation, and hobbies. Mindfulness helps with emotional control and purpose.
Can you share some inspiring success stories of men who have overcome depression?
The article shares stories of men who beat depression. These stories show the power of seeking help and finding new ways to cope. They offer hope and show that recovery is possible.
Source Links
- Strategies For Managing Mood Swings Effectively | Dr Chandril Chugh
- Best Neurologist In Patna, Author Dr Chandril Chugh
- Men’s Experiences of Mental Illness Stigma Across the Lifespan: A Scoping Review
- Behaviors in men that could be signs of depression
- How Does Depression Affect Romantic Relationships?
Managing Separation Anxiety in Babies: A Parent's Guide
Tearful, tantrum-filled goodbyes are common in a child's early years. Around the first birthday, many kids feel separation anxiety. They get upset when a parent or other caregiver leaves them with someone else. This feeling is normal and can be tough for both you and your child.
Understanding what your child feels and having strategies can help you both. It makes getting through this phase easier.
Separation anxiety is a natural part of a baby's growth and their bond with caregivers. By learning to handle this stage, you can help your child feel secure and confident. They'll learn to be okay even when you're not there.
Understanding Separation Anxiety in Infants
As your little one grows, they start to understand the world better. They learn that things and people are still there even when they can't see them. Around 4 to 7 months, your baby might start feeling separation anxiety. This is a normal part of their emotional growth.
What is Separation Anxiety?
Separation anxiety is when your baby feels scared or upset when you leave their sight. It shows they are getting more attached to you and worry about when you'll come back. Since they don't get time, they might feel worried and scared about your departure.
When Does It Develop?
Separation anxiety usually starts between 8 months and 1 year old. This is when they become more independent but still need you a lot. It's a key time for them to learn about the world and keep feeling safe with their parents or guardians.
Knowing when separation anxiety happens can help you support your baby during this change. By creating a caring space and using ways to calm them, you can help your baby feel secure as they grow.
Signs and Symptoms of Separation Anxiety in Babies
As a parent, it's key to know the signs of separation anxiety in your baby. This stage is common for infants. Understanding these signs helps you support your baby better.
One key sign is when your baby cries or feels distressed when you leave. They might cling to you, not wanting to be held by anyone else. They could also have trouble sleeping or wake up at night, looking for a parent or someone they know.
The way a baby reacts to being separated can depend on their personality and daily routine. More sensitive or anxious babies might feel separation anxiety more strongly. Being hungry, tired, or sick can make them feel more scared and need you more.
Knowing when your baby feels separation anxiety lets you help them through it. With patience, consistency, and love, your baby will get better at handling it. They'll become more independent and confident over time.
Factors Affecting Separation Anxiety
Separation anxiety in babies can be affected by their temperament and routine. Babies who meet caregivers other than their parents early on find it easier to handle when parents leave. But, if a baby is tired, hungry, or sick, they might find it harder.
Temperament and Routine
A baby's temperament greatly affects their separation anxiety. Some babies are more sensitive and feel more distress when parents leave. Others are more easygoing and adapt better. Also, a baby's routine can change how they feel about being separated.
Babies with a consistent schedule handle separations better than those with unpredictable routines.
Hunger, Fatigue, and Illness
Hunger, fatigue, and illness can make separation anxiety worse in babies. When a baby is hungry, tired, or sick, they find it harder to cope with a parent's departure. They need the comfort and security of their caregivers more during these times.

Understanding what affects a baby's separation anxiety helps parents support their child better. This way, parents can help their child go through this stage with more ease and confidence.
Preparing Your Baby for Separation
As a parent, you're key in helping your baby deal with separation anxiety. Start by preparing babies for separation in your daily life. Use practicing separations and creating goodbye rituals to make things easier for your baby.
Playing Peekaboo and Practicing Separations
Peekaboo is great for teaching your baby about object permanence. It shows them you'll always come back, even if they can't see you. You can also use a favorite toy to show them about being apart and coming back.
Start with short times apart and slowly make them longer. This helps your baby get used to you being away. Begin with just stepping out of the room and then increase the time as they feel more comfortable.
Establishing a Goodbye Ritual
A consistent goodbye routine can make your baby feel secure. It could be singing a song, giving a hug, or doing a special handshake. This way, your baby knows you'll return, which helps them feel better when you're apart.
Remember, every baby is different. Try various methods to see what works best for your baby. With patience and consistency, you can help your baby handle separation better.
Check out this link for more tips on preparing your baby for separation.
Handling Separation Anxiety During Departures
Managing separation anxiety during departures can be tough, but it's doable with the right steps. It's important to stay calm and consistent when leaving your child. Your feelings can affect theirs.
Staying Calm and Consistent
When it's time to leave, keep a calm face. Don't show any worry or hesitation, as it can make your baby more anxious. Instead, give a reassuring smile, a gentle hug, and a brief goodbye.
Being consistent is key. Always follow the same routine when you leave, so your baby feels secure.
Avoiding Prolonged Goodbyes
Long goodbyes can make separation anxiety worse. Your baby might think you're not ready to leave. So, aim for a quick, positive goodbye.
A simple hug, a kiss on the cheek, and a gentle reassurance that you'll be back soon can help. Sneaking away without saying goodbye can cause more distress, as your child didn't get to process the departure.
With patience and consistency, you can help your baby overcome separation anxiety during departures. By staying calm and keeping goodbyes brief, you give your little one the support and reassurance they need. This way, they can feel secure even when you're not there.
Separation anxiety in babies
Separation anxiety in babies is a big deal. The reunion is just as important as the departure. Happy reunion rituals help strengthen the bond between you and your baby. They make your baby feel safe and secure after being apart.
One simple way to make reunions special is with a warm hug. This hug can instantly calm your baby and show them you're there. Playing with a favorite toy together is another great way to bond.
Letting your baby lead the reunion is also a good idea. Some babies like a quiet hello, while others want to show you something new. Listening to what your baby wants makes reunions happier.
The main aim of these rituals is to ease separation anxiety and strengthen your bond. By doing this, your baby will feel safe, loved, and confident, even when you're apart.

Coping Strategies for Separation Anxiety
When your little one feels separation anxiety, it can be tough. But, there are ways to make it easier for them and for you too.
Using Transitional Objects
One good idea is to give your child a transitional object. This could be a favorite toy or a soft blanket. These items can be a comfort and help your child feel safe when you're apart.
Checking In During the Day
Also, checking in with your child during the day can be helpful. It makes you feel better and helps you stay calm when you leave. A quick call or video chat can make a big difference in easing separation anxiety.
Using these strategies every day can make things easier for your baby. With time and patience, they'll get better at handling being apart from you. Remember, they will learn to be more independent.
Separation Anxiety at Night
As the sun sets and bedtime comes near, separation anxiety can grow for babies. A steady bedtime routine can make this easier and get your baby ready for being apart. Activities like bath, books, and a special goodnight ritual tell your baby it's time to sleep.
Establishing a Bedtime Routine
Being consistent with bedtime activities is important. Always do the same soothing things every night. This makes your baby feel safe and know what to expect. It helps lessen separation anxiety at night.
Using Recorded Voices and Sounds to Soothe
Along with a calming bedtime routine, recorded voices and sounds can offer comfort when you're not there. Record yourself reading stories or singing lullabies. Then, play these for your baby when they feel anxious or alone. These familiar sounds can calm and reassure your baby.
With a steady bedtime routine and soothing sounds, you can help your baby deal with separation anxiety at night. Be patient and caring, and you'll make sure both you and your baby get a good night's sleep.
Conclusion
Managing separation anxiety in babies is a delicate process. It needs patience, consistency, and understanding your child's needs. By supporting your child's development and strengthening the parent-child bond, you can get through this tough time with empathy and skill. Remember, managing separation anxiety is key to your baby's growth. It helps them build trust, resilience, and learn to soothe themselves.
This phase will pass, and your child will become more secure and confident. Keep trying the strategies from this guide, adjusting them for your situation and your baby's unique nature. With time and effort, you'll see a strong, secure bond grow. This bond will be the base for your child's future relationships and well-being.
Use this chance to get closer to your little one. By managing separation anxiety, you're not just helping your child grow. You're also strengthening the parent-child bond that will last long after this hard time is over.
FAQ
What is separation anxiety in babies?
Separation anxiety is when babies get upset when a parent or caregiver leaves them with someone else. It's a normal part of growing up.
When does separation anxiety typically develop in infants?
Babies usually start feeling separation anxiety between 8 months and 1 year old. They become more independent but still worry about being apart from their parents.
What are common signs of separation anxiety in babies?
Babies with separation anxiety might cry when a parent leaves, cling in new places, cry at night, or have trouble sleeping without a caregiver nearby.
How do factors like temperament, routine, and illness affect separation anxiety?
Babies who meet other caregivers early on find it easier to handle being apart. But being tired, hungry, or sick makes it harder. A baby's personality and daily routine also play a role in how they feel about being separated.
What are some strategies to help ease separation anxiety in babies?
To ease separation anxiety, parents can play peekaboo to show they'll always come back. Sending stuffed animals on "adventures" and reuniting them with the baby helps too. Short visits with a trusted caregiver and a consistent goodbye ritual, like singing a song or giving a hug, can also help.
How can parents remain calm and consistent during separations?
Parents should stay calm and consistent when leaving their child. Showing too much emotion can make the child more anxious. Quick goodbyes with a hug and reassurance that you'll return help ease the separation. Sneaking away can cause more distress, as the child didn't get to process the departure.
How can happy reunion rituals help with separation anxiety?
Happy reunion rituals, like hugging, playing, or following the child's cues, strengthen the parent-child bond. They remind the child that being apart is sad but coming back is great.
How can transitional objects and checking in during the day help with separation anxiety?
Giving a comfort item, like a stuffed animal or blanket, can soothe a child during separations. Checking in on the child during the day provides reassurance, reduces guilt, and helps parents stay calm for the next goodbye.
How can parents manage separation anxiety at bedtime?
A consistent bedtime routine, like bath, books, and goodnight rituals, prepares the baby for being apart. Recording yourself reading or singing can also comfort the child when they're alone or scared, offering a familiar presence even when you're not there.
Source Links
- How to Ease Your Child’s Separation Anxiety
- Separation Anxiety (for Parents)
- How To Handle Separation Anxiety in Babies
Separation Anxiety Disorder in Adults
As an adult, you might feel scared and worried when you think about being away from someone you love. This feeling is known as separation anxiety disorder. It's not just for kids; many adults deal with it too. It can make everyday life and relationships harder.
Separation anxiety in adults means you're really scared of being away from someone close, like a partner, parent, or best friend. You might worry a lot about their safety or feel sick when you're apart. This anxiety can stop you from doing well at work, making friends, and being independent.
If you're facing separation anxiety, know you're not alone. Many people deal with it, and there's help available. With the right support and treatment, you can handle your feelings better. By learning about the causes, spotting the signs, and getting help, you can start to overcome separation anxiety.
What is Separation Anxiety Disorder in Adults?
Separation anxiety disorder in adults is a mental health issue. It makes people fear being away from someone they are very close to. This fear is usually for a family member or romantic partner. It can really change how an adult lives and connects with others.
Symptoms and Signs of Adult Separation Anxiety
The main signs of separation anxiety disorder in adults are:
- Feeling very worried and anxious when you're apart from someone you love
- Always thinking about bad things happening to the person you're attached to or to yourself when you're apart
- Not wanting to be alone or leave the person you're close to
- Feeling sick, having headaches, and trouble sleeping because of it
- Having nightmares about being separated
How it Affects Daily Life and Relationships
Adults with this disorder find it hard to be alone, keep up good relationships, and do well at work or school. They might avoid doing things that mean being away from their loved one. This leads to feeling ashamed, embarrassed, and helpless.
This disorder can really stop an adult from living a happy and independent life.
Causes and Risk Factors of Separation Anxiety Disorder in Adults
The exact reasons for separation anxiety in adults are still being studied. It seems to come from both genes and environment. Knowing what might increase the risk can help us understand it better.
Genetic and Environmental Influences
Some people might be more likely to feel separation anxiety because of their genes. Things that happened in childhood, like tough times or big changes, can also play a part. These events can make separation anxiety more likely in adults.
Life Events and Triggers
Big events in life can make separation anxiety worse or start it. This includes losing someone close, getting sick, or going through big changes like moving or having a child. These changes can make people feel less secure and more anxious when they're apart from loved ones.
Knowing what causes adult separation anxiety and the risk factors for separation anxiety in adults is key. By tackling these factors, people can get better and have healthier relationships.
Separation Anxiety Disorder In Adults
Excessive Worry and Physical Symptoms
Adults with separation anxiety often worry too much about being away from someone they feel close to. They might always think about their loved one's safety or fear something bad happening to them when apart. These worries can make them feel sick to their stomach, give them a fast heartbeat, or cause headaches.
Impact on Work, Social Life, and Independence
Separation anxiety can make it hard for adults to do things on their own and live normally. It can affect their work, stop them from being social or traveling alone, and make it hard to be independent. The fear of being apart can lead to feeling alone, problems in relationships, and missing out on personal and career growth.
The effects of excessive worry with separation anxiety can be big, changing an adult's life a lot. It's important to understand the issues and find ways to deal with it to keep living a full and independent life.

With the right help and treatment, adults with separation anxiety can get better. They can learn to handle their symptoms, become stronger, and get back their independence and happiness.
Recognizing Separation Anxiety in Adults
It can be hard to spot separation anxiety in adults. The signs might look like normal worries or other mental health issues. But it's key to know the usual signs of adult separation anxiety. This helps in getting the right treatment and taking back control of your life.
Common Thoughts and Behaviors
Adults with separation anxiety often worry too much about something bad happening to their loved ones. They might also worry they won't be able to handle being apart. These worries can be way too much and really get in the way of daily life and relationships.
Some common behaviors seen in adults with separation anxiety include:
- Refusing to leave home or avoiding activities that require time apart from loved ones
- Excessive texting, calling, or checking in on attachment figures to ensure their safety and wellbeing
- Experiencing intense distress or panic when faced with separation from loved ones
- Difficulty concentrating or engaging in tasks when separated from attachment figures
If you're always worried about your loved ones' safety or feel really upset when you're apart, it might be separation anxiety. It's important to recognize this and get help.
Diagnosis and Co-occurring Conditions
To diagnose separation anxiety disorder in adults, experts look at symptoms against the DSM-5 criteria. They check if the person has at least three symptoms like worrying about losing someone, not wanting to be alone, or feeling sick. These symptoms must make daily life hard for at least four weeks.
DSM-5 Criteria for Diagnosis
The DSM-5 gives clear guidelines for diagnosing separation anxiety in adults. To get a diagnosis, people must:
- Worry a lot or feel anxious about being away from someone or a place they feel attached to.
- Have a strong fear or anxiety about losing someone close or something happening to them.
- Not want to leave home or be alone because of fear of being separated.
- Have symptoms that make daily life hard or cause a lot of distress.
- Not have symptoms that fit better with another mental health issue, like a phobia or panic disorder.
Related Anxiety Disorders and Mental Health Issues
Adults with separation anxiety might also have other mental health problems, like other anxiety disorders, obsessive-compulsive disorder, or depression. It's important to understand how these conditions are linked. A mental health expert can check for other issues and plan the best treatment.
Treatment Options for Adult Separation Anxiety
Dealing with separation anxiety in adults needs a mix of methods. Cognitive behavioral therapy (CBT) is a top choice. It helps people spot and fight negative thoughts and actions that cause anxiety.
Cognitive Behavioral Therapy (CBT)
CBT for separation anxiety includes steps like facing separation bit by bit, learning coping skills, and handling anxious thoughts and feelings. This way, adults with separation anxiety can beat their fears. They can feel more independent and confident.
Medication and Combination Therapy
In some cases, medicines like selective serotonin reuptake inhibitors might be given with therapy to lessen separation anxiety symptoms. Combining CBT with medication works best for treating separation anxiety in adults.
Managing separation anxiety disorder means working with mental health experts to create a plan that fits your needs. With the right treatment, adults can control their symptoms, live better, and keep strong relationships.

Coping Strategies and Self-Help Tips
Dealing with separation anxiety as an adult can be tough. But, with the right strategies and self-help, you can manage your symptoms better. It's key to have a strong support system for adult separation anxiety.
Building a Support System
Surround yourself with people you trust, like family, friends, and loved ones who get what you're going through. They can offer emotional support, company, and help when you need it. Joining a support group, online or in person, can also make you feel less alone.
Relaxation Techniques and Mindfulness
Adding relaxation techniques to your daily life can really help with anxiety and stress from separation. Try deep breathing, meditation, or progressive muscle relaxation to calm down. Mindfulness, focusing on the present moment, can also help you deal with anxious thoughts.
Along with professional help, having a self-care routine can boost your ability to cope with self-help tips for separation anxiety in adults. Do things that make you happy, like reading, exercising, or a hobby, to help with coping strategies for adult separation anxiety. By focusing on your well-being and using effective coping methods, you can overcome separation anxiety and feel more in control.
Seeking Professional Help
If you're an adult dealing with ongoing and severe separation anxiety, it's key to get help. A mental health expert, like a therapist or counselor, can check your symptoms, give you a diagnosis, and create a plan to help you. They can help you with your separation anxiety.
When to See a Mental Health Provider
You should think about getting help if you worry too much about being apart, feel sick or have panic attacks, avoid doing things, or have trouble in your relationships and work because of your anxiety. Getting professional help can really change how you handle your symptoms and boost your well-being.
Finding the Right Therapist or Counselor
When picking a mental health provider, look for someone who focuses on anxiety disorders and works with adults with separation anxiety. This ensures you get specific and effective treatment for your issues. Spend time researching and talking to potential therapists to find one that suits your needs and likes.
Don't wait to ask for help with separation anxiety. With the right support and treatment, you can manage your symptoms and take back control of your life.
Conclusion
Separation anxiety disorder in adults is a complex issue that affects daily life and well-being. It's not just for kids; adults can feel the same fear and anxiety when away from loved ones. This condition can deeply impact your life.
Learning about the causes, signs, and treatment options helps you manage your separation anxiety. With cognitive-behavioral therapy, medication, and other methods, you can cope better. You'll learn to handle life's changes and find healthy ways to deal with separation anxiety.
Getting professional help and building a support network is key to getting better. With the right support and guidance, you can beat separation anxiety disorder. Start your journey to a more balanced life today.
FAQ
What is separation anxiety disorder in adults?
Separation anxiety disorder makes adults feel very scared or anxious when they're away from someone close, like a family member or partner. This fear can make daily life hard.
What are the main symptoms of separation anxiety disorder in adults?
Symptoms include feeling anxious when apart, worrying about the person's safety, not wanting to be alone, and having physical symptoms like nausea. Nightmares about being separated can also happen.
What causes separation anxiety disorder in adults?
It's not fully known, but it might be due to genes and past experiences. Childhood troubles, traumatic events, or big life changes could play a part.
How does separation anxiety disorder affect adults' daily lives?
It can make it hard for adults to do things on their own. It might affect their work, social life, and making decisions without needing someone else's help.
How is separation anxiety disorder recognized in adults?
Adults with this disorder worry a lot about their loved ones being in danger. They might not want to leave home, constantly check in with their partner, or avoid activities that mean being apart.
How is separation anxiety disorder in adults diagnosed?
Doctors look at symptoms to see if they meet the DSM-5 criteria. The person must have at least three symptoms that make daily life hard for over four weeks.
What are the treatment options for separation anxiety disorder in adults?
Cognitive behavioral therapy (CBT) is often the first step. It helps change negative thoughts and behaviors. Sometimes, doctors also suggest medication like SSRIs to help with symptoms.
What self-help strategies can adults with separation anxiety use?
Building a strong support network, using relaxation techniques, and having a daily routine can help. These steps can make managing separation anxiety easier.
When should an adult seek professional help for separation anxiety?
Adults should get help if their separation anxiety is severe and affects their life, relationships, and work. A mental health expert can create a treatment plan.
Source Links
- What Is Separation Anxiety Disorder?
- Separation Anxiety in Adults
- Separation anxiety in adults: Symptoms, treatment, and management