Have you ever felt like you’re drowning in your thoughts because there’s no one around to pull you out? Now imagine facing that while living with post-traumatic stress disorder. That’s what many people experience during periods of social isolation. Being cut off from regular contact isn’t just lonely,it can be dangerous when PTSD is involved.
In this blog, we will break down how social isolation affects people with PTSD, what really goes on in the brain, and what steps can be taken to cope and seek help. Whether you’re someone living with PTSD or supporting a loved one, this blog will help you understand the real struggles and what can be done.
Table of Contents
ToggleHow Does Social Isolation Impact PTSD Symptoms?
Being alone isn’t always peaceful. For someone with PTSD, it often means being stuck in painful memories. During social isolation, these memories have no competition. They grow stronger, repeat more often, and steal a person’s sense of safety.
Let’s take a closer look at the science behind this.
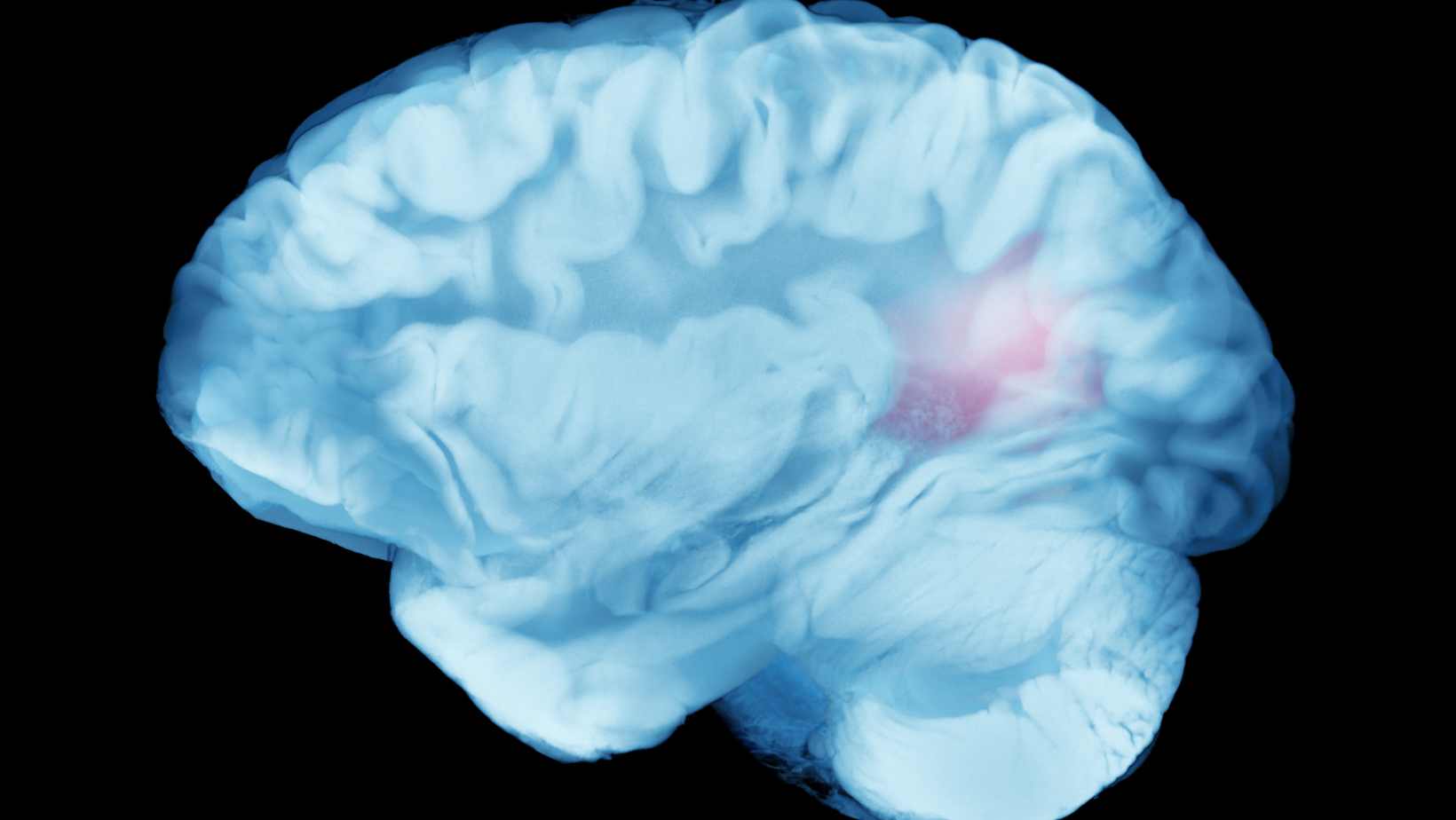
What Happens in the Brain When You’re Alone With PTSD?
The human brain is wired for connection. For people with PTSD, the brain already functions in a high-alert state. When someone faces social isolation, this response gets worse.
- The amygdala (which controls fear) becomes more active.
- The hippocampus (which handles memory) may shrink, making traumatic memories harder to manage.
- The prefrontal cortex (responsible for thinking clearly) loses control.
These changes can make people feel:
- More fearful
- More anxious
- Less in control of their thoughts
Longer periods of social isolation can even lead to structural changes in the brain.
Can Social Isolation Trigger More Flashbacks and Nightmares?
Yes, and many people have shared their stories.
When you’re isolated, your brain has fewer distractions. That means traumatic memories can rise to the surface faster.
Some real-life examples:
- A veteran reported daily flashbacks during lockdown when he couldn’t leave his house.
- A woman with childhood trauma began reliving her abuse every night while staying alone during the pandemic.
This rise in flashbacks and isolation makes even normal routines difficult.
Is There A Link Between Isolation, Depression, And PTSD?
Yes, many studies confirm this.
According to the World Health Organization (WHO):
- People with PTSD are twice as likely to suffer from depression.
- During the COVID-19 pandemic, depression rates increased by over 25% worldwide due to social isolation.
The National Institute of Mental Health (NIMH) also reports that isolation increases feelings of hopelessness and sadness, especially in PTSD patients.
Why Are People With PTSD More Vulnerable To Loneliness?
Social isolation doesn’t just happen. Many people with PTSD begin pulling away from others without even realizing it. Let’s understand why.
Does Trauma Make Social Withdrawal Worse Over Time?
Yes. Trauma teaches the brain that people aren’t safe. As time goes on:
- People avoid interactions that may trigger memories
- Fear of being misunderstood increases
- Trust gets harder to rebuild
So the more isolated someone becomes, the less likely they are to seek help. It’s a cycle that feeds itself.
What Role Do Trust Issues Play in Isolation?
People with PTSD often feel like others won’t understand them. This creates deep trust issues.
Here’s what happens:
- Past betrayal or abuse leads to fear of being judged.
- Relationships feel unsafe.
- Talking about trauma becomes nearly impossible.
That silence pushes people deeper into social isolation.
Are People With PTSD At A Higher Risk Of Suicide During Social Isolation?
Yes, sadly. Besides, the risk of developing depression or indulging in deliberate self-harm is six times higher in people with PTSD. Suicide risk goes up when there’s no support.
According to the CDC, veterans with PTSD are 1.5 times more likely to die by suicide during times of social isolation. For abuse survivors and first responders, the numbers are also high.
This shows how important it is to stay connected, even from afar.
What Are The Everyday Challenges Of Living With PTSD In Isolation?
Daily life becomes harder when no one is around to help. Simple things like eating, sleeping, or going outside may feel impossible.
How Do Triggers and Panic Attacks Go Unnoticed Without a Support System?
Triggers are hidden. Without someone to notice your reactions:
- Panic attacks can escalate quickly
- Flashbacks go unchecked
- Emotional triggers get stronger over time
This can feel terrifying and lonely.
What Happens When You Can’t Access In-Person Therapy?
Therapy is a lifeline for many. But people living in rural areas or under lockdown often can’t reach help.
Real problem areas include:
- Lack of transportation
- Closed clinics during health crises
- No internet access in remote areas
This gap in mental health support can make PTSD symptoms spiral.
Can Virtual Therapy Replace Face-To-Face Sessions?
Sometimes, yes. According to an APA survey:
- 71% of patients said virtual therapy helped them feel supported.
- PTSD patients found online CBT to be just as effective as in-person therapy.
But some people still prefer the human touch that comes with physical presence.
What Are The Best PTSD Treatment Options Available When You’re Isolated?
You don’t have to wait for a clinic visit. PTSD treatment can be anything from a simple change of habit to seeking professional help. It is different for every individual based on their coping mechanism and severity of the disease. Many PTSD treatment options are available online or by phone.
Are Teletherapy And Online CBT Effective For PTSD?
Yes, many experts support them.
The American Psychological Association (APA) found:
- Online CBT works for 60-80% of PTSD patients
- Telehealth options reduced dropout rates in therapy
Virtual help is now more reliable than ever before.
What Role Do Medications Play In Long-Term PTSD Management?
Medicines like SSRIs and anti-anxiety pills can:
- Reduce panic
- Help manage sleep
- Lower flashbacks
A doctor can guide what’s safe based on your condition.
Are There Any Emergency Helplines Or Support Services For People Struggling Alone?
Yes. These services are life-saving.
| Country | Helpline | Contact Info |
|---|---|---|
| USA | National Suicide Prevention Lifeline | 988 or 1-800-273-TALK |
| India | iCall | +91 9152987821 |
| UK | Samaritans | 116 123 |
| Australia | Lifeline | 13 11 14 |
Keep these numbers close during social isolation.
PTSD Treatments
| Method | What It Does | Key Benefit |
|---|---|---|
| Reach Out | Encourages opening up or seeking help | Early support, less isolation |
| Mindfulness | 2 mins/day of meditation or prayer | Calms anxiety, restores hope |
| Exercise | Light physical activity (e.g., yoga, walk) | Boosts mood, lowers stress |
| Psychotherapy | Custom therapy based on diagnosis | Tailored healing approach |
| Cognitive Therapy | Talk therapy to express and reframe thoughts | Clears negative patterns |
| Exposure Therapy | Safe re-exposure to trauma | Builds control, reduces fear |
| EMDR | Eye movement + trauma recall | Eases reaction, improves processing |
Now you may think that the world is coming to an end, but remember this too shall pass and it’s only after the darker cold nights, the sun feels brighter and warm.
Expert Help Is Just One Step Away: Book a Consultation Today
Living with PTSD is already hard. Facing it in silence can make it worse. You don’t have to keep suffering in silence. Whether you’re a survivor, a veteran, or a caregiver, help is available even during social isolation.
Book a private consultation with Dr. Chandril Chugh, a trusted expert in mental health support, neurology, and trauma-related care. Your recovery matters. Take the first step today.
Also Read:
FAQs
Can social isolation make PTSD worse?
Yes, social isolation can make post-traumatic stress disorder worse. It increases the chances of having frequent flashbacks, panic attacks, and deep sadness. Without daily interaction, people may feel more trapped in their trauma. Isolation reduces access to mental health support, which can delay recovery.
What are the signs of PTSD getting severe during isolation?
If someone is isolating more, having frequent nightmares, avoiding daily routines, or showing anger outbursts, these may be signs of worsening PTSD. Thoughts of self-harm or hopelessness are also serious red flags. These signs should be noticed early, especially by close family members or friends.
How do I help a friend with PTSD who refuses to socialize?
Be patient and stay in touch regularly, even with simple messages or voice notes. Let them know they are not alone. Recommend support groups or safe spaces like virtual therapy sessions, but don’t push too hard. Showing care without pressure is key.
Are there PTSD-specific apps or virtual communities that help?
Yes, several apps and online platforms are made for PTSD support. PTSD Coach, BetterHelp, and Talkspace offer chat features, exercises, and counseling. These tools give people comfort and connection during social isolation when in-person help isn’t possible.
What if my PTSD gets worse even with therapy?
If therapy doesn’t seem to help, don’t give up. It might mean a change in approach is needed. Sometimes adjusting medications or switching to a new therapist can make a difference. Keep communication open with professionals for better PTSD treatment options.
Is it normal to feel disconnected from reality when isolated with PTSD?
Yes, it’s common for people with PTSD to feel distant, numb, or detached. This disconnection is part of how the brain protects itself from pain. These feelings may grow stronger during social isolation, but they can be managed by staying in touch and using grounding techniques. Yes. Many people feel lost or “numb”. This is part of emotional triggers and trauma. Staying connected, even online, can help ease this feeling.

Dr Chandril Chugh
Dr. Chandril Chugh, a renowned American Board-Certified Neurologist, is just a click away. With years of global experience, he offers trusted neurological guidance online.
→ Book a consultation to discover which remedies suit your needs best.