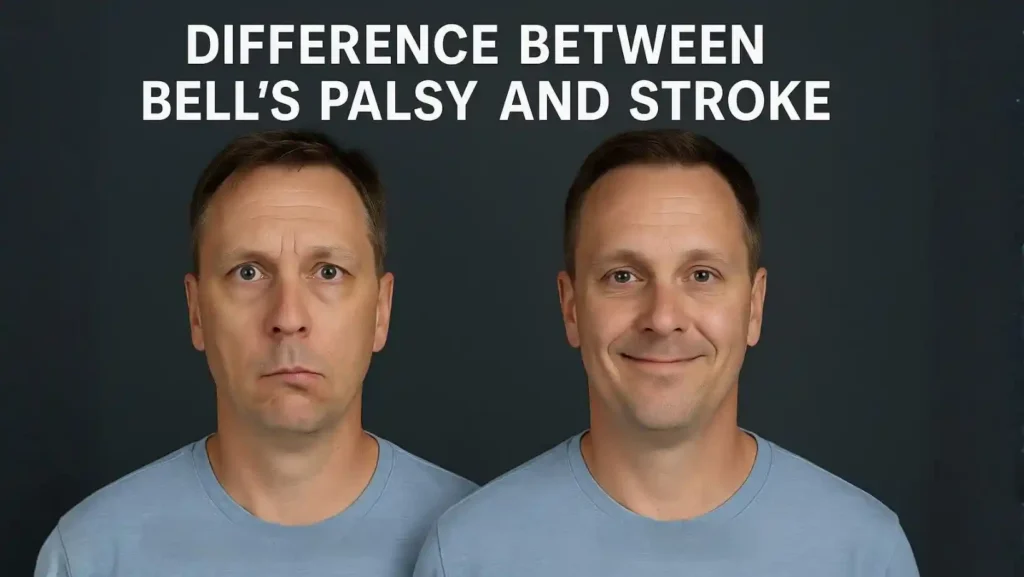
Bell’s palsy and stroke can cause a drooping face on one side. Yet the damage inside your body is not the same. Bell’s palsy is a problem of one facial nerve. A stroke is an emergency where part of your brain loses blood. If you mix up Bell’s palsy or stroke , you might delay life-saving care.
Difference Between Bell’s Palsy And Stroke
Peripheral vs Central Facial Weakness Explained
In Bell’s palsy , the problem lies in the facial nerve itself. This nerve, called cranial nerve VII, controls your facial muscles. It leaves the brainstem, runs through a narrow bony tunnel near your ear, then branches across your face. If a virus or swelling irritates this nerve, signals to the muscles drop. The result is lower motor neuron facial weakness, also called peripheral palsy.
Because the nerve is damaged after it leaves the brain, the whole half of your face can go weak. Your eyebrow, eye, cheek, and mouth on that side may barely move. This full pattern is classic Bell’s palsy vs stroke for nerve disease.
In a stroke , the damage is central. The brain tissue that sends signals down to the facial nerve gets hurt. Most often, the stroke hits fibers that control the lower face more than the forehead. In this case, you see upper motor neuron weakness, or central palsy. The brain itself has lost function, which is why stroke is far more dangerous than Bell’s palsy .
Forehead Movement Differences: Why Eyebrow Raising Helps Diagnose Stroke
Your forehead receives signals from both sides of the brain. Because of this, a mild or moderate stroke that hits only one side of the brain often spares the forehead. You can still raise both eyebrows.
So when a doctor checks Bell’s palsy or stroke , you are asked to raise your eyebrows and wrinkle your forehead.
In Bell’s palsy on the right, your right eyebrow does not move. The right forehead looks smooth. You may not close your right eye fully. In a stroke on the left side of the brain, the right corner of your mouth may droop, but both eyebrows can still lift.
How Speech, Balance, And Limb Weakness Signal Stroke, Not Bell’s Palsy
Bell’s palsy affects one nerve. It does not affect your arm, leg, or thinking. If you only have one-sided facial droop, ear pain, and eye problems, and your speech, strength, and balance stay normal, doctors consider it Bell’s palsy as a nerve issue.
Stroke , in contrast, often harms more than just the face. Because brain areas share close blood supply, the same stroke that weakens your facial muscles may also:
- Make one arm or leg weak or numb
- Change your speech, so words sound slurred or you cannot find the right words
- Affect your understanding of what others say
- Cause trouble walking, with poor balance or a sudden fall
Large studies show that face droop, arm weakness, and speech trouble appear together in most strokes.
So if you have facial droop plus limb weakness or speech change, doctors treat you as a likely stroke case until proven otherwise, not simple Bell’s palsy .
Timing Of Onset: Progressive Hours (Bell’s Palsy) Vs Sudden Seconds
In stroke , symptoms often appear in seconds or a few minutes. You may be normal, then suddenly your mouth droops and your arm will not lift. Family members often say the change was “all at once”. This pattern matches what major stroke groups describe worldwide.
In Bell’s palsy , weakness usually builds over several hours. You feel pain behind one ear or strange taste changes first. Over the course of one to two days, the face droop worsens until it reaches its peak.
There are gray zones. Rarely, Bell’s palsy can feel “sudden” to you, and small stroke can seem mild at first. Because of this overlap, experts warn that timing alone never rules out bells palsy or stroke . It only adds one more clue to Bell’s palsy vs stroke diagnosis .
Stroke Vs Bell’s Palsy Symptoms
Facial Droop Distribution: Full Side Paralysis Vs Only Lower Face Weakness
With Bell’s palsy , the entire half of your face on the affected side can look flat. That eyebrow does not rise, the eye does not close tightly, the cheek does not move, and the mouth corner hangs. You may show teeth only on the healthy side when you try to smile.
With a typical stroke , the lower face on one side is much weaker than the upper face. You can often still wrinkle your forehead and raise both brows, yet one mouth corner sags. Saliva might leak from that side, and your smile looks crooked.
FAST Stroke Signs: Facial Droop, Arm Weakness, Speech Slurring
Worldwide stroke campaigns teach the FAST rule. It is simple enough that you can use it at home.
- F means Face. You ask the person to smile. If one side of the face droops or feels numb, that is a danger sign.
- A means Arm. You ask the person to raise both arms. If one arm drifts down or feels weak, that points to stroke .
- S means Speech. You ask for a short, clear sentence. Slurred speech, strange words, or silence all signal trouble.
- T means Time. If any of these signs appear, you call emergency services at once. Treatments for stroke work best in the first few hours after onset.
Eye Tearing, Drooling, And Ear Pain, Unique To Bell’s Palsy
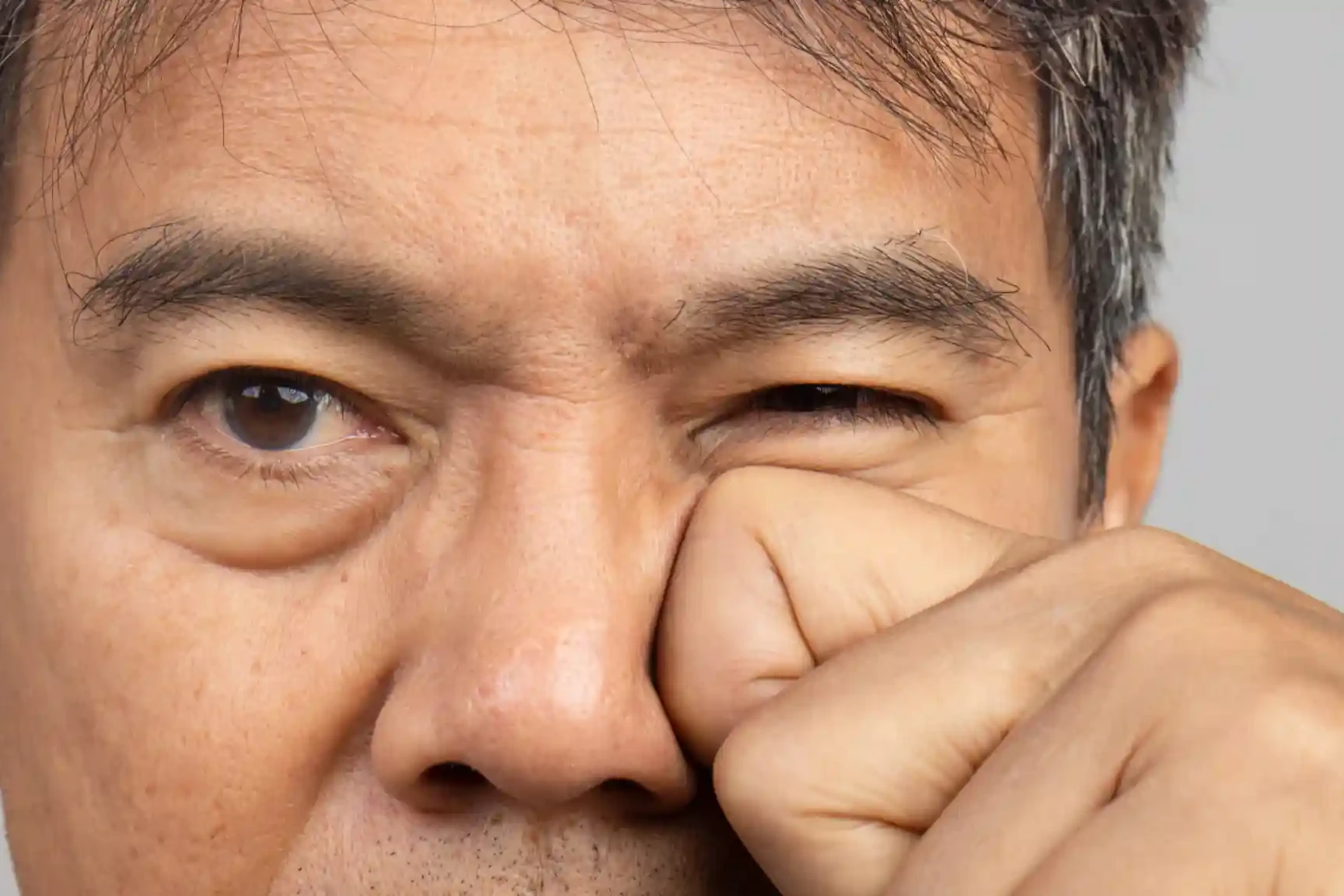
Some signs point more toward Bell’s palsy than stroke . Because the eyelid on the weak side does not close well, your eye can dry out and feel gritty. The body responds with extra tears, so the eye may water all the time.
The mouth on that side does not seal. Food and drink may spill from the corner. You might drool during meals. While drooling can appear in stroke , in Bell’s palsy it often shows up without limb weakness or language trouble.
Behind the ear on the affected side, many people feel a dull ache or sharp pain. This ear or jaw pain often starts a day or two before the face droop. It likely comes from swollen nerve tissue inside tight bone.
Headache, Confusion, And Vision Loss, Specific To Stroke
A very sudden, severe headache, especially if you call it the worst of your life, can mean bleeding inside or around the brain. Confusion, where you cannot state the date, your age, or where you are, suggests that brain tissue is not working. Sudden loss of vision in one eye, or loss of half of your visual field, also points to a brain event, not just a facial nerve problem.
These severe features do not fit simple Bell’s palsy . So when facial droop appears with headache, confusion, or vision loss, doctors treat you as a probable stroke case and rush you through stroke diagnosis scans.
Bell’s Palsy Vs Stroke Diagnosis
Neurological Examination For Cranial Nerve VII Function Testing
When you reach the emergency room with sudden facial weakness, the first step in bell’s palsy vs stroke diagnosis is a full neurological exam. The doctor does not only look at your face. They check how the whole nervous system is working.
For cranial nerve VII, the facial nerve, you are asked to lift your eyebrows, close your eyes tight, smile, show your teeth, and puff out your cheeks. In bells palsy , all movements on one side of your face are weak, from forehead to chin. In stroke , the forehead often still moves, while the lower face droops.
The doctor also tests your arms and legs. You may be asked to push, pull, hold your arms up, or walk a short distance. They listen to your speech and check your memory, attention, and sense of touch. If you have facial weakness plus arm or leg problems, or speech and thinking changes, the doctor treats it as bells palsy or stroke with high concern for stroke until scans are done.
CT Or MRI To Rule Out Ischemic Or Hemorrhagic Stroke
Because stroke can kill brain cells within minutes, brain imaging often comes next. Current guidelines from major stroke groups recommend brain imaging as soon as possible when strokesymptoms are present.
A CT scan is often the first test. It is fast and good at finding bleeding in the brain, which is called a hemorrhagic stroke . If there is bleeding, clot-busting drugs are not safe. The CT scan also helps rule out large tumors or other major brain problems.
If the CT scan shows no bleeding but your symptoms still suggest stroke , an MRI might be done. MRI can show small areas of brain damage from an ischemic stroke where a blood vessel is blocked. In some people with bells palsy , MRI may show the facial nerve lighting up when contrast dye is used, which supports a peripheral nerve problem instead of stroke .
EMG Or Nerve Conduction For Bell’s Palsy Confirmation
Electromyography, called EMG, uses tiny needles or surface sensors to study muscle activity. Nerve conduction studies use small electrical pulses on the skin to see how fast and how strong the nerve signals travel. These tests can show how severe the nerve damage is and which parts of the nerve are affected.
Research suggests that EMG and nerve conduction can help predict which bells palsy patients are more likely to have slow or incomplete recovery, although the evidence is not perfect and some studies show mixed results.
These tests are not needed in every case. For mild bells palsy , doctors often watch your progress over a few weeks. For severe weakness or unclear cases, EMG and nerve conduction give more detail and support a careful bells palsy workup.
Blood Tests To Exclude Infection, Lyme Disease, Or Autoimmune Triggers
If you live in or travel to an area with many ticks, doctors often test for Lyme disease when you arrive with facial palsy. Lyme disease can cause facial nerve weakness on one or both sides, and treatment needs antibiotics, not only steroids. Guidelines from the CDC and infectious disease experts stress this point, and they note that evidence about adding steroids in Lyme facial palsy is still limited.
Other blood tests may check your blood sugar, immune system markers, or signs of recent infections. The goal is to make sure that the difference between Bell’s palsy and stroke is an autoimmune disease, HIV, or rare nerve inflammation.
Facial Paralysis Causes
Viral Reactivation Leading To Nerve Swelling In Bell’s Palsy
Most experts think bells palsy often happens when a common virus becomes active again inside the facial nerve. Herpes simplex virus type 1, the virus that can cause cold sores, is a frequent suspect. Varicella zoster virus, which causes chickenpox and shingles, is another possibility.
The idea is that the virus irritates the nerve inside a tight bony tunnel. Swelling then compresses the nerve and blocks the signals to facial muscles, causing the one-sided weakness that defines bells palsy . Studies from nerve tissue and imaging support this model, but it is not proven in every person, so researchers still say the exact cause is partly unclear and the evidence is limited.
Ischemic Stroke Causes: Clot, Plaque, Or Embolism
An ischemic stroke happens when a blood vessel in the brain becomes blocked. This can occur when a clot forms on a fatty plaque in an artery that already has damage from high blood pressure, smoking, or high cholesterol. A clot can also travel from the heart in conditions like atrial fibrillation and then lodge in a brain artery.
When blood stops flowing, brain cells in that area do not get oxygen or nutrients. Within minutes they begin to die. If that part of the brain controls the face and arm on one side, you see the classic stroke symptoms pattern: facial droop plus arm weakness.
Hemorrhagic Stroke Causes: Vessel Rupture Or Aneurysm
A hemorrhagic stroke occurs when a weakened blood vessel in the brain breaks and bleeds. Very high blood pressure over many years is a major risk factor. Sometimes a thin walled bulge in a vessel called an aneurysm ruptures and spills blood around the brain.
The bleeding increases pressure inside the skull and damages brain tissue. You may feel a sudden severe headache, develop facial weakness, vomit, or become very drowsy. This pattern is very different from bells palsy , which does not cause sudden collapse or a “thunderclap” headache.
Because treatments for ischemic and hemorrhagic stroke are very different, scans are essential whenever Bell’s palsy or stroke is a question.
Rare Causes: Tumors, Trauma, Or Ramsay Hunt Syndrome
Not all one-sided facial weakness is Bell’s palsy . Head injuries can cut or bruise the facial nerve. Tumors in the parotid gland, skull base, or brainstem can crush the nerve slowly, leading to weakness that worsens over weeks instead of hours.
Ramsay Hunt syndrome happens when the shingles virus attacks the facial nerve near the ear. You may see small fluid-filled blisters in or around the ear, severe ear pain, and facial paralysis. Lyme disease can also cause facial palsy, sometimes on both sides, especially in children who live in high-risk areas.
Bell’s Palsy Vs Stroke Treatment
Stroke Treatments: Clot Busting Drugs, Thrombectomy, ICU Stabilization
For many ischemic strokes, guidelines from major heart and stroke groups support the use of intravenous clot-busting drugs in selected patients within a limited time from symptom onset. These medicines can reopen blocked arteries and improve outcome if used safely.
For larger clots in large brain arteries, specialists may perform mechanical thrombectomy. In this procedure, a small tube goes through your blood vessels to the blocked artery. A device then grabs or breaks up the clot so blood flow returns. Studies over the last decade show that adding thrombectomy to standard care improves survival and function in many patients, although results vary by age, clot location, and treatment delay.
After emergency treatment, many stroke patients stay in an intensive care or high dependency unit. The team watches blood pressure, sugar, breathing, and brain swelling. They also start prevention for another stroke with blood thinners or other medicines when safe. Doctors do not promise that these steps will fully reverse the stroke , but evidence shows they can reduce disability for many people.
Bell’s Palsy Treatments: Steroids, Antivirals, Eye Lubrication
Treatment for Bell’s palsy focuses on reducing nerve swelling and protecting the eye. High quality studies and guidelines support a short course of oral corticosteroids started within the first few days after symptoms begin for most adults, unless there is a reason you cannot take steroids. These medicines lower inflammation and improve the chance of full recovery.
Some doctors add antiviral medicine that targets herpes viruses. Research suggests that steroids alone already give strong benefit, and adding antivirals gives only a small extra gain in many studies. The evidence is mixed, and expert groups note that the benefit of antivirals is modest and may not apply to every case, which means the research is still limited.
Eye care is crucial in Bell’s palsy treatment when the eyelid does not close well. You usually need lubricating eye drops during the day and thicker gel or ointment at night. You may tape the eyelid closed while you sleep so the surface of the eye does not dry or get scratched. These protective steps are strongly supported by eye and neurology experts.
In Lyme-associated facial palsy, antibiotics are needed, and steroid use is more complex, since some data suggest steroids alone might worsen outcomes if infection is not treated. Here, specialist advice is important and the evidence is still being studied.
Physical Therapy For Facial Muscle Rehabilitation
As weeks pass, you may notice that Bell’s palsy improves but does not return to normal. Some people develop tightness or unwanted linked movements, such as the eye closing when they smile. In this phase, physical therapy can help retrain your facial muscles.
Therapists use gentle exercises, mirror feedback, and sometimes massage or taping to guide smoother, more balanced movement. Reviews suggest that facial therapy is safe and may help function and quality of life, although the exact best program and timing are still being studied, so the research remains limited.
People who have a stroke that affects the face also benefit from rehab. In stroke treatment , facial therapy for stroke is usually part of a broader program that includes speech, swallowing, arm, and leg training. This whole-body rehab helps you regain daily skills step by step.
When Recovery May Take Weeks Vs Lasting Disability
In Bell’s palsy , large follow-up studies show that about 70 to 85% of people recover near-normal or fully normal facial movement within three to six months, especially if they receive early steroids. Some people need longer, and a smaller group has lasting weakness or synkinesis, but most can smile and close the eye again.
In stroke , the outcome depends on the size and location of brain damage, how fast treatment began, and your overall health. Some people regain almost all function, while others have lasting weakness, speech trouble, or vision loss. Rehab improves chances, but no doctor can guarantee a full return to normal life after stroke .
FAQs
Can Bell’s Palsy Be Confused With A Stroke In The First Hour?
Yes, Bell’s palsy and stroke can look alike at the start, and even experts can struggle in the first hour. Because missing a stroke is dangerous, doctors usually treat early cases as possible stroke until scans and tests clarify the difference between Bell’s palsy and stroke .
How Do Doctors Instantly Tell If It’s A Stroke Or Bell’s Palsy?
Doctors quickly test your forehead, arms, legs, and speech, then look at brain scans. If you have limb weakness or language problems with facial droop, symptoms favor stroke , and urgent stroke diagnosis steps follow.
Can Bell’s Palsy Cause Arm Or Leg Weakness Like A Stroke?
No, Bell’s palsy affects only the facial nerve and cannot weaken your arms or legs. If you have facial droop plus limb weakness, the team must treat it as likely stroke with strong concern for stroke until proven otherwise.
How Long Does Bell’s Palsy Recovery Usually Take?
For most people with Bell’s palsy , early change appears within a few weeks, and large groups recover well by three to six months. Recovery after Bell’s palsy is usually quicker and more complete for bells palsy , although some tightness or slight weakness can remain.
Can Bell’s Palsy Happen On Both Sides Of The Face?
Yes, but it is rare. Most bells palsy cases affect one side, yet both sides can be involved in a small number of patients or with conditions like Lyme disease. When both sides are weak, doctors check for infections and immune diseases.
Are There Long Term Complications Of Bell’s Palsy?
Some people with Bell’s palsy develop lasting mild weakness, twitching, or linked movements such as the eye shutting when they smile. These problems are not stroke , but they affect comfort and appearance, so therapy, eye care, and sometimes injections may be used as Bell’s palsy treatment .
Does Bell’s Palsy Increase Your Risk Of Stroke Later?
Current research suggests bells palsy itself does not directly cause stroke , but you may still share risk factors like high blood pressure or diabetes. Controlling these risks is vital whether you had Bell’s palsy or stroke , to protect your brain and blood vessels.
Is Bell’s Palsy Contagious Or Infection-Related?
The facial weakness of Bell’s palsy is not contagious, and you cannot spread paralysis to another person. Some linked viruses can spread, but most adults already carry them. This is one more difference between Bell’s palsy and stroke , since stroke comes from blood vessel problems, not simple infection.
What Eye Care Steps Are Required With Bell’s Palsy?
With Bell’s palsy , your weak eyelid may not close fully, so you need frequent lubricating drops by day and thicker gel at night. Taping the eye during sleep, wearing glasses outdoors, and seeing an eye specialist protect vision and are key parts of Bell’s palsy treatment when facial weakness affects blinking.
About The Author

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
Dr. Chandril Chugh is a U.S.-trained neurologist with over a decade of experience. Known for his compassionate care, he specializes in treating neurological conditions such as migraines, epilepsy, and Parkinson’s disease. Dr. Chugh is highly regarded for his patient-centered approach and dedication to providing personalized care.
→ Book a consultation to discover which remedies suit your needs best.