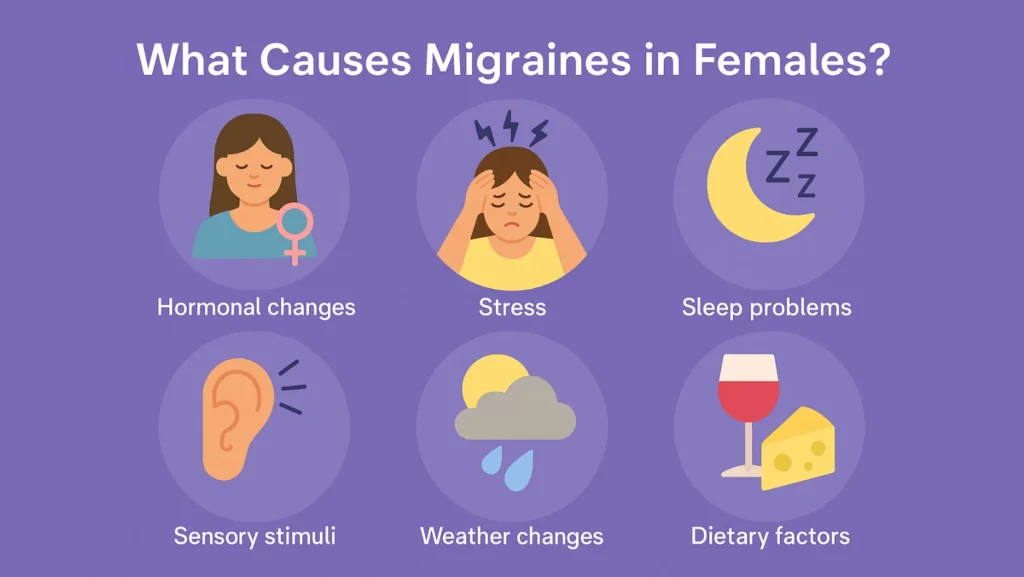
Migraines in females are more common in women than men, and the reasons go far beyond “just headaches.” They are a complex mix of hormonal changes, genetics, lifestyle factors, and even how the brain processes pain.
Understanding what are the causes of migraines in women helps in early diagnosis, prevention, and proper treatment. Let us explore the science, the triggers, and the unique role hormones play in female migraines.
A Note About Sex And Gender Differences
When talking about migraine, it is important to separate sex from gender. Biological sex influences hormonal cycles, reproductive health, and body chemistry. Gender roles, on the other hand, may impact stress levels, workload, and lifestyle choices. Both sex and gender shape female-specific migraine risk factors and influence how often migraines occur and how severe they become.
Table of Contents
ToggleWhat Is Migraine, And Why Does It Happen In Women?
A migraine is not a normal headache. It is a neurological disorder where the brain becomes hyper-sensitive to stimuli. The trigeminovascular system plays a central role, transmitting pain signals when over-activated.
Unlike a simple tension headache, migraine episodes may last from a few hours to several days and often include nausea, vomiting, and sensitivity to light or sound.
Women experience migraines at nearly three times the rate of men. The key lies in hormones, especially estrogen and progesterone, which affect reproductive hormones and brain chemistry. These hormones can make women more vulnerable to migraine episodes, particularly during times of hormonal shifts like menstruation, pregnancy, and menopause.
Why Are Migraines More Common In Females?
Studies show that female hormones lower the brain’s pain threshold, making women more likely to experience severe headaches. Genetics also plays a role, with a clear genetic predisposition to migraine found in families.
Environmental and lifestyle triggers further increase risk. Women often juggle multiple responsibilities at home and work, leading to stress, irregular sleep, and dietary changes, all of which trigger migraines. Hormonal changes combined with these migraine triggers in women explain the higher prevalence.
Migraine And Hormones: The Link Explained
Hormones are at the heart of migraines in females. Estrogen regulates serotonin, a brain chemical involved in pain sensitivity. A sudden estrogen drop migraine happens when estrogen levels fall quickly, such as before menstruation.
Progesterone and migraine are also connected. Rising or falling progesterone levels may disrupt the brain’s electrical balance. Together, these shifts explain why many women face headaches tied to hormonal cycles.
Hormonal Migraines In Females
When migraines follow a clear hormonal pattern, they are called hormonal migraines in females. These migraines often appear during puberty, worsen during periods, and sometimes improve after menopause. Tracking cycles helps doctors distinguish hormonal migraines from other types.
Migraine And The Menstrual Cycle
The migraine and menstrual cycle connection is strong. Many women notice attacks two days before and three days after their period begins. This is when estrogen levels drop the most.
A menstrual cycle headache can sometimes feel like tension or sinus pain, but true menstrual migraines are typically more severe and resistant to regular painkillers.
What Causes Menstrual Migraines?
Menstrual migraines are sharp decline in estrogen before menstruation is the main trigger. But other factors worsen these attacks:
| Trigger | Explanation |
| Estrogen drop | Sudden hormone fall around menstruation triggers brain sensitivity |
| Low magnesium | Many women have reduced magnesium during periods, which worsens headaches |
| Stress & anxiety | Emotional strain around cycles worsens pain perception |
| Poor sleep | Hormonal changes disturb sleep, leading to headaches |
| Skipped meals | Blood sugar changes increase migraine frequency |
Some women also face ovulation migraine in the middle of their cycle when hormones fluctuate again.
Pregnancy And Migraine
Pregnancy and migraine is a mixed story. In early pregnancy, migraines may worsen due to hormonal fluctuations, stress, and morning sickness. By the second and third trimesters, many women experience fewer migraines due to stable estrogen levels.
However, treatment is tricky. Most medications for migraine are unsafe in pregnancy. Natural approaches like sleep regulation, hydration, and doctor-approved supplements such as Magnesium become more important.
Migraines During Periods
Migraines during period days are some of the most disabling. The pain can last longer than regular migraines and often resists over-the-counter medicines. Women also report stronger nausea, dizziness, and fatigue during these attacks. Identifying the pattern can help doctors plan short-term preventive therapies.
Other Migraine Triggers In Women

Hormones are not the only cause. There are many daily migraine triggers in women. These include:
- Stress: Emotional stress releases brain chemicals that overstimulate nerves.
- Sleep and migraine triggers: Both too little and too much sleep disrupt brain balance.
- Diet and migraine in females: Skipped meals, dehydration, chocolate, cheese, and processed foods can trigger attacks.
- Caffeine and alcohol: Excess caffeine or sudden withdrawal can set off pain. Alcohol, especially red wine, is a strong trigger.
- Environmental triggers: Bright lights, strong perfumes, weather changes, and loud sounds activate the sensitive brain.
Tracking personal triggers helps reduce attack frequency.
Treatment For Migraine And Headaches In Females
Treating migraines requires both acute and preventive strategies.
- Acute treatment: Painkillers, triptans, and anti-nausea drugs work best when taken early in the attack.
- Preventive treatment: For frequent migraines, preventive medicines, lifestyle changes, and sometimes hormone therapy are recommended.
- Contraceptives: Some birth control pills worsen migraines, while others stabilize hormones and reduce attacks. Choosing between combined contraceptives and progesterone-only pills requires medical guidance.
- Estrogen supplementation: Used in some women to prevent hormone-related migraines.
- Magnesium: A natural supplement shown to reduce migraine frequency.
Non-medication options include yoga, meditation, and stress management. Regular meals and a stable sleep cycle are part of migraine prevention for women.
Similar Conditions And Causes Of Headaches In Females
Not every headache is migraine. Other causes include:
- Tension headaches: A pressing, band-like pain around the head.
- Sinus headaches: Pain and pressure due to sinus infections.
- Chronic migraine in women: Defined as 15 or more headache days per month.
- Migraine with aura in women: Includes visual changes, tingling, or speech issues before the pain starts.
A thorough evaluation is important to avoid misdiagnosis.
The Bottom Line
Migraines in women are not just “bad headaches.” They are linked to hormones, genes, and lifestyle. By understanding what causes headaches in females, women can work with doctors to create tailored treatment plans. Tracking the cycle, identifying triggers, and balancing hormones play key roles in reducing migraine frequency and severity.
FAQs
What causes migraines in females?
Migraines in females are mostly linked to hormonal changes, estrogen fluctuations, genetic predisposition, and lifestyle triggers like stress, sleep disruption, and diet changes.
How to diagnose migraine?
Doctors diagnose migraine through medical history, symptom patterns, family history, and ruling out other conditions. Imaging is rarely needed unless unusual symptoms suggest a secondary cause.
How do hormones affect migraines in women?
Hormones influence brain chemistry and nerve sensitivity. Estrogen drop before menstruation lowers pain threshold, while progesterone shifts also alter brain activity and trigger migraine episodes.
Why do migraines get worse during the menstrual cycle?
During menstruation, estrogen drops sharply, which destabilizes brain chemistry. Combined with stress, poor sleep, and low magnesium, it makes migraines more frequent and intense.
What causes migraines in females more than males?
Hormonal fluctuations, reproductive changes, and female biology increase risk. Added stress and lifestyle factors further explain why women suffer more frequent and severe migraines compared to men.
Can birth control pills trigger migraines in women?
Yes. Combined contraceptives with estrogen can trigger migraines in women, especially those with aura. Progesterone-only options may be safer and sometimes reduce hormonal migraine attacks.
What are common migraine triggers in females?
Triggers include stress, irregular sleep, dehydration, skipped meals, alcohol, caffeine, strong odors, bright light, and weather changes. Each woman may have unique personal triggers.
How can women prevent hormone-related migraines?
Keeping a symptom diary, eating regular meals, practicing stress control, taking magnesium, and discussing hormone therapy with a doctor can help prevent hormone-related migraines.
About The Author

Medically reviewed by Dr. Chandril Chugh, MD, DM (Neurology)
Board-Certified Neurologist
Dr. Chandril Chugh is a U.S.-trained, board-certified neurologist with expertise in diagnosing and managing neurological disorders, including migraines, epilepsy, Parkinson’s disease, and movement disorders. His clinical focus includes evidence-based neurological care and patient education.
All content is reviewed for medical accuracy and aligned with current neurological guidelines.